Abstract
Introduction:
Pre-exposure prophylaxis (PrEP) is effective in preventing HIV among adherent users. However, PrEP uptake among transgender women is low and current Centers for Disease Control and Prevention (CDC) prescribing guidelines are not specific to transgender women. Self-perceived risk for HIV among those PrEP indicated is not well understood.
Methods:
This cross-sectional analysis includes 1,293 transgender women screened at baseline from March 2018 to May 2020 for a multisite, prospective cohort study. We compared the prevalence of PrEP indication using current CDC prescribing criteria vs. transgender women-specific criteria developed by study investigators with community input. We identified factors associated with study specific PrEP indication as well as factors associated with self-perceived low to no HIV risk among those PrEP indicated. We also calculated descriptive statistics to depict the PrEP care continuum.
Results:
PrEP indication prevalence using transgender women-specific criteria was 47% (611), 155 more than were identified using the CDC criteria. Eighty-three percent were aware of PrEP, among whom 38% had ever used PrEP. Among PrEP ever-users, 63% were using PrEP at the time of the study. There was 66% of current PrEP users who reported 100% adherence within the prior 7 days. Among those PrEP indicated, 13% were using and adherent to PrEP at the time of the study. Over half (55%) of PrEP-indicated participants had low or no self-perceived HIV risk.
Conclusions:
These findings suggest further guidance is needed for healthcare providers in prescribing PrEP to transgender women. Greater uptake and adherence are also needed for optimal effectiveness.
Keywords: transgender women, PrEP indication, Health Belief Model, self-perceived risk, HIV prevention
Introduction
Transgender women experience a disproportionate burden of HIV, with an estimated prevalence of around 14–28%.1,2 Pre-exposure prophylaxis (PrEP) has been established as a highly efficacious means for preventing HIV acquisition,3–5 even in the presence of hormone therapy.6 However, there is still a dearth of evidence concerning the effectiveness of PrEP among transgender women. Although, there is research that has explored facilitators and barriers to oral, daily PrEP usage as well as acceptability of PrEP among transgender women, much of this research has grouped this population with cisgender men who have sex with men (MSM).7,8 Additionally, this work has not explored the role of self-perceived HIV acquisition risk in the context of PrEP use. Thus, there is a need to focus on PrEP implementation efforts among transgender women and identify means to improve PrEP uptake.
Given the high burden of HIV among transgender women, PrEP uptake is likely to have high impact in reducing acquisition for those who are sexually active (or PrEP indicated). 9 The social marginalization and oppression experienced by transgender women have simultaneously led to increased risk of HIV acquisition (compared to the general population) and decreased access to HIV prevention services.10 Social exclusion (e.g., from formal employment and education) and unmet need for gender affirmation are associated with increased behavioral risk factors for HIV acquisition such as engagement in sex work and condomless receptive anal sex.11 Adverse childhood events, which are more prevalent among transgender people than cisgender people,12 have also been associated with high HIV acquisition risks.13 However, uptake of oral, daily PrEP remains low among transgender women.11 Furthermore, current PrEP indication guidelines from the Centers for Disease Control and Prevention (CDC) are not specific to transgender women as they only explicitly provide criteria for cisgender men who have sex with men (MSM), heterosexually active cisgender men and women, and people who inject drugs.14 Although the guidelines acknowledge that transgender people could potentially benefit from PrEP,14 no guidelines have been developed specifically for transgender women despite being one of the most affected populations in the U.S. HIV epidemic. In practice, the CDC PrEP prescribing criteria for MSM are often applied to transgender women.
Along with the need for PrEP prescribing criteria that are specific to transgender women, it is also important to ensure that those who are indicated for PrEP are aware of their risk of HIV acquisition. Behavioral models, such as the Health Belief Model, posit that a person’s perceived risk for adverse health is important in determining whether or not they will adopt a given health intervention.15 Such models suggest that an individual’s self-perceived threat for a given disease, along with their perception of the level of efficacy of a health intervention for that disease, will dictate whether or not they will adopt a given health behavior.15 Thus, it is possible that transgender women who are behaviorally indicated for PrEP use, but who do not perceive themselves as being at risk for HIV acquisition, may be less likely to inquire about or start using PrEP. Research is needed to evaluate perceived risk for HIV acquisition among transgender women in relation to PrEP indication.
This analysis evaluates the use of PrEP prescribing criteria that are specific to the HIV acquisition risks of transgender women and the self-perceived risk for HIV among these women. We also report levels of engagement throughout the PrEP care continuum. These analyses aim to identify gaps in PrEP engagement among transgender women and potential opportunities where PrEP messaging may be improved for this population.
Methods
Study design and setting
The American Cohort to Study HIV Acquisition Among Transgender Women (known to participants as the LITE study) is a multi-site observational cohort study enrolling HIV-negative transgender women (N=1293 as of May 2020) across the southern and eastern U.S. The cohort includes two arms: a site-based cohort (N=747) in six eastern and southern U.S. cities (Atlanta, Baltimore, Boston, Miami, New York City, and Washington, DC) and an online cohort (N=546) in over 50 metropolitan areas throughout the eastern and southern United States. The purpose of the study is to follow participants over a two-year period to estimate HIV incidence and describe factors associated with HIV acquisition. Participants complete socio-behavioral surveys and biological testing for HIV on a quarterly basis for site-based participants and every six months for online cohort participants. Participants in the site-based cohort also receive annual STI testing (syphilis, gonorrhea, and chlamydia) and biospecimen collection. Survey topics for both the online and site-based cohorts span domains of: sociodemographic characteristics, gender affirmation and pride, general health, sexual health and behaviors, mental health and substance use, social experiences including violence, discrimination, and social support. Study design and implementation were informed by ongoing discussions with a Community Advisory Board with membership spanning the cohort’s geographic region and through formative research.16,17 Methods associated with the site-based cohorts are previously described in the published protocol.18 The present analysis is a secondary analysis utilizing cross-sectional data from baseline study visits completed between March 2018 and May 2020. All study procedures were reviewed and approved by the Johns Hopkins School of Medicine Institutional Review Board (IRB) for all study sites.
Participant selection
Participants were recruited via online advertisements on social media and dating apps (both cohorts) and via traditional convenience sampling methods including peer referral, fliers, and referrals from clinics and community-based organizations (site-based cohorts only). Eligibility criteria included being ages 18 years or older; endorsing a trans feminine identity based on a two-step measure of being assigned male at birth and identifying as female, gender non-conforming, non-binary, or being on the trans-feminine spectrum; residing in one of the six site-based cities (site-based cohort) or one of the 50 eastern and southern cities (online cohort); testing negative for antibodies to HIV upon screening via oral specimen testing (online cohort) or the OraSure HIV self-test (site-based cohort); speaking English and/or Spanish language; and providing consent to participate in at least the baseline study visit.
Outcomes of interest
PrEP indication definition
This manuscript compares the CDC’s definition of PrEP indication used for MSM, which are often applied to transgender women, to a definition developed by LITE study investigators with community input and based on HIV risk factors that are more specific to transgender women. The current CDC PrEP prescribing criteria include having any cisgender male sex partners in the last 6 months, not being in a monogamous sexual partnership with a known HIV negative cisgender male, and at least one of the following: any anal sex without a condom in the last 6 months or having an STI within the last 6 months (Table 1).14 Given the frequency of follow-up and recall periods in the LITE study, laboratory-confirmed or self-reported STI diagnosis in the last 3 months and condomless sex during last sexual encounter were used as proxies for these CDC indicators. PrEP indication criteria suggested by the LITE study investigators with community input (in addition to the CDC criteria) include: a) recent sex work (within the prior 3 months), b) use of post exposure prophylaxis (PEP), c) recent sex with a partner living with HIV or of unknown HIV status (within the last 3 months), and d) needle-sharing when injecting drugs within the last 12 months. Participants reported “yes” or “no” for each of these criteria on the social-behavioral survey.
Table 1.
Comparing CDC and LITE Study PrEP prescribing criteria
| PrEP Indication Criteria | |
|---|---|
|
| |
| CDC (MSM specific) | Study specific criteria for TGW (italicized) |
|
| |
| • Current negative HIV serostatus | • Current negative HIV serostatus |
| • Any cisgender male sex partner within the last 6 months | • Any cisgender male sex partner within the last 6 months |
| • Not in a monogamous sexual partnership with an HIV negative cisgender male | • Not in a monogamous sexual partnership with an HIV negative cisgender male |
| And at least one of the following: | And at least one of the following: |
| ➢ Anal sex without a condom within the last 6 months | ➢ Anal sex without a condom within the last 6 months |
| ➢ Having an STI within the last 6 months | ➢ Having an STI within the last 6 months |
| ➢ Report current sex work (within the last 3 months) | |
| ➢ Reported use of post-exposure prophylaxis (PEP) | |
| ➢ Sex with a partner living with HIV within the last 3 months | |
| ➢ Sex with a partner of unknown HIV status with in the last 3 months | |
| ➢ Needle sharing of injection drugs within the last 12 months | |
Self-perceived risk for HIV acquisition
Perceived risk of HIV acquisition was measured by the question: “How high do you think your risk for HIV infection is?”, with answer choices of no risk, low, medium, or high risk. For this analysis, we dichotomized responses to combine “no” or “low” risk to a low-risk category versus high risk if they reported “medium” or “high” risk.
Variables of interest
We examined age, race, education, employment, health insurance, income level, drug use, social support, homelessness, adverse childhood experiences, and experiences of psychological violence for associations with PrEP indication. Age was dichotomized to compare those above vs. below the age of 30 (the median age was 28, thus we chose to consider those below age 30 as “young” participants). Low income was defined as living below the federal poverty line. Social support was measured through a modified version of the California Health Interview Survey Social Support Index in which participants answered five questions (e.g., “How often have you had someone available to take care of you if you are sick?”) and provided responses on a 5-point Likert scale ranging from 0 (None of the time) to 4 (All of the time) with response totals ranging from 0–20. Response totals above 10 were categorized as “high” social support (Cronbach alpha: 0.87).19 We used the Drug Abuse Screening Test (DAST)-1020 to screen for drug use disorder based on activity within the last 12 months. The DAST provides a score from 1–10, and scores of 3 or greater are classified as moderate to severe substance use disorder (Cronbach alpha: 0.72). We also used the CDC’s Behavioral Risk Factor Surveillance System’s Adverse Childhood Experience (ACE) questionnaire, which measures instances of child abuse or neglect.21 ACE scores ranged from 0–8, and the higher the score, the greater the number of reported adverse childhood events (Cronbach alpha: 0.64). Responses were dichotomized with those reporting 3 or fewer ACEs in the “low” adverse child experience group and those reporting 4 or more in the “high” adverse child experience group. Participants also reported whether or not they experienced any occurrence of psychological violence within the last 3 months. This was defined as any occurrence in which a participant had been insulted, belittled, intimidated, or threatened to disclose their gender identity to others without their consent.
PrEP care continuum
In the survey, participants reported whether or not they had heard of daily, oral PrEP, if they had ever taken PrEP, if they were currently using PrEP, and how adherent they were in their PrEP use. Self-reported PrEP use in the last 30 days prior to the survey was classified as current PrEP use. Adherence to daily, oral PrEP was defined as not missing a dose of PrEP medication within the last 7 days prior to the survey. This level of adherence is based on lack of evidence that any dosing less than 7 pills in 7 days is protective for individuals using exogenous hormones.22
Analysis
PrEP indication
We compared the number of additional participants that would be indicated for PrEP when using the study specific PrEP indication definition compared to the CDC’s definition. We then conducted bivariable and multivariable analyses to determine factors associated with having indications for PrEP using our revised criteria for transgender women. We estimated adjusted prevalence ratios (aPR) using a multivariable Poisson regression model with robust variance adjusting for race/ethnicity, education, health insurance, drug use, lifetime housing stability, ACEs score, experiences of psychological violence victimization within the last 3 months, and study site. To build the multivariable model, we conducted Pearson’s chi-squared tests for each variable and selected those that were statistically significant at a 0.10 alpha level. We excluded poverty level and employment status as they were highly correlated with education.
Self-perceived HIV risk among PrEP indicated participants
Among those who were PrEP indicated based on those criteria, we repeated the same model building procedures in order to identify factors associated with reporting self-perceived low HIV risk. The variables for this model included age (i.e., being < or >=30 years of age), education level, substance use, social support, lifetime housing stability, and ACEs score. We also calculated descriptive statistics to characterize the PrEP care continuum, tabulating the percentage of participants who were aware of PrEP, had health insurance coverage, currently used PrEP, and were adherent to PrEP among those who were PrEP indicated based on transgender-specific criteria. Study site and current PrEP use (within the last 30 days) were included in the model. All analyses were conducted using Stata 15 software.23
Results
Descriptive characteristics
As of May 2020, there were 1293 participants who had a negative HIV test enrolled in the baseline visit. Among this group, 57% were younger than 30 years of age, 14% identified as Non-Hispanic/Latinx Black, 28% reported less than a high school education, and 72% endorsed low perceived HIV acquisition risk (Table 2). Eleven percent of participants reported current PrEP use at the time of enrollment.
Table 2.
Socio-demographics of TGW by PrEP indication status (n=1293) (as of 5/1/2020)
| Demographics | Total=1293 | PrEP Indication by CDC= 456 | Transgender Enhanced PrEP Indication = 155 | p-value |
|---|---|---|---|---|
| Study site | N (%) | N (%) | N (%) | 0.99 |
| Baltimore, MD | 78 (6) | 38 (8) | 12 (8) | |
| Boston, MA | 170 (13) | 52 (11) | 16 (10) | |
| New York, NY | 221 (17) | 90 (20) | 34 (22) | |
| Atlanta, GA | 64 (5) | 30 (7) | 9 (6) | |
| Miami, FL | 92 (7) | 43 (9) | 15 (10) | |
| Washington D.C. | 122 (9) | 48 (11) | 14 (9) | |
| Online | 546 (42) | 155 (34) | 55 (36) | |
| Age | ||||
| <30 years of age | 735 (57) | 284 (62) | 76 (49) | |
| >=30 years of age | 554 (43) | 172 (38) | 79 (51) | 0.004 |
| Race | ||||
| Non-Hispanic/Latinx White | 676 (53) | 184 (41) | 58 (38) | |
| Non-Hispanic/Latinx Black | 174 (14) | 93 (21) | 20 (13) | |
| Hispanic/Latinx (any race) | 109 (9) | 54 (12) | 23 (15) | 0.08 |
| Other | 317 (25) | 120 (27) | 52 (34) | |
| Education | ||||
| High school or less | 360 (28) | 164 (36) | 56 (37) | 0.96 |
| Some college or more | 921 (72) | 290 (64) | 98 (64) | |
| Employment | ||||
| No employment | 517 (41) | 190 (43) | 63 (42) | |
| Employed (Part-time) | 279 (22) | 105 (24) | 40 (27) | |
| Employed (Full-time) | 457 (36) | 151 (34) | 47 (31) | 0.71 |
| Health Insurance | ||||
| Yes | 1036 (80) | 350 (78) | 116 (76) | 0.65 |
| No | 243 (19) | 101 (22) | 37 (24) | |
| Low Income | ||||
| Below Poverty level | 418 (38) | 164 (42) | 73 (52) | 0.06 |
| Above Poverty level | 675 (62) | 224 (58) | 69 (49) | |
| Drug Abuse Screening Test | ||||
| Above moderate drug use | 361 (28) | 148 (33) | 62 (41) | 0.08 |
| Below moderate drug use | 917 (72) | 303 (67) | 91 (60) | |
| Social Support | ||||
| Low social support score | 568 (45) | 197 (44) | 81 (54) | 0.04 |
| High social support score | 684 (55) | 249 (56) | 69 (46) | |
| Ever Experienced Homelessness | ||||
| Yes | 557 (44) | 238 (53) | 81 (53) | 0.93 |
| No | 720 (56) | 215 (47) | 72 (47) | |
| Adverse Childhood Experiences | ||||
| Low adverse childhood experiences | 693 (55) | 229 (51) | 67 (45) | 0.16 |
| High adverse childhood experiences | 571 (45) | 217 (49) | 83 (55) | |
| Recent Threat of Violence (within last 3 months) | ||||
| Yes | 508 (47) | 205 (55) | 67 (44) | 0.75 |
| No | 570 (53) | 171 (45) | 85 (56) |
Enhanced PrEP Indication refers to participants who were considered to be indicated for PrEP based on study criteria but not based on CDC criteria
Differences in level of PrEP indication based on study vs. CDC criteria
Out of the 1293 participants, 456 (35%) participants (Table 2) were indicated for PrEP based on CDC criteria compared to 611 (47%) participants using the enhanced criteria for transgender women. Thus, an additional 155 participants were reclassified as PrEP indicated when using the enhanced study criteria. Thus overall, the prevalence of PrEP indication was 12% higher based on the enhanced study criteria compared to the CDC criteria. Those who were PrEP indicated based on transgender women-specific criteria were more likely to be age 30 years or older (p=0.004) and were more likely to report low social support (p=0.04) than those indicated by CDC criteria only. A greater percentage of these participants also had an income below the federal poverty level (52% vs. 42%) and more reported above moderate to severe drug use (41% vs. 33%); however, these differences were not statistically significant (p=0.06 and p=0.08, respectively).
In multivariable analyses, participants who were Non-Hispanic/Non-Latinx Black (PR: 1.53, 95% CI: 1.28, 1.83), Hispanic/Latinx (PR: 1.76, 95% CI: 1.47, 2.11), or Other race (PR: 1.39, 95% CI: 1.19, 1.62) were more likely to be PrEP indicated compared to Non-Hispanic/Non-Latinx White participants. Those who reported moderate to severe drug use (PR: 1.34, 95% CI: 1.19, 1.52), lifetime homelessness (PR: 1.15, 95% CI: 1.02, 1.29), or a recent (within the last 3 months) occurrence of psychological violence (PR: 1.19, 95% CI: 1.06, 1.34) were more likely to be PrEP indicated. Geographic location, participation in the online cohort, and education were inversely associated with PrEP indication (see Table 3).
Table 3.
Socio-demographics associated with LITE Study specific PrEP indication in TGW (N=1293)
| Demographics | PR [95% CI] | P-value | aPR [95% CI] | P-value |
|---|---|---|---|---|
| Study Site | ||||
| Baltimore, MD | ref | -- | ref | -- |
| Boston, MA | 0.62 [0.49, 0.80] | <0.001 | 0.77 [0.60, 1.00] | 0.05 |
| New York, NY | 0.88 [0.71, 1.07] | 0.20 | 0.87 [0.71, 1.06] | 0.16 |
| Atlanta, GA | 0.95 [0.74, 1.22] | 0.70 | 1.02 0.79, 1.33] | 0.86 |
| Miami, FL | 0.98 [0.78, 1.24] | 0.89 | 0.90 [0.71, 1.15] | 0.39 |
| Washington D.C. | 0.79 [0.62, 1.01] | 0.06 | 0.87 [0.69, 1.11] | 0.26 |
| Online | 0.60 [0.49, 0.73] | <0.001 | 0.78 [0.63, 0.96] | 0.02 |
| Race | ||||
| Non-Hispanic/Latinx White | ref | -- | ref | -- |
| Non-Hispanic/Latinx Black | 1.81 [1.43, 2.31] | <0.001 | 1.53 [1.28, 1.83] | <0.001 |
| Hispanic/Latinx | 1.97 [1.61, 2.41] | <0.001 | 1.76 [1.47, 2.11] | <0.001 |
| Other | 1.52 [1.16, 1.98] | 0.002 | 1.39 [1.19, 1.62] | <0.001 |
| Education | ||||
| High school or less | ref | -- | ref | -- |
| Some college or more | 0.69 [0.66, 0.72] | <0.001 | 0.82 [0.72, 0.92] | 0.001 |
| Health Insurance | ||||
| No | ref | -- | ref | -- |
| Yes | 0.79 [0.71, 0.89] | 0.96 [0.84, 1.09] | 0.52 | |
| Drug Abuse Screening Test | ||||
| Below moderate drug use | ref | -- | ref | -- |
| Above moderate drug use | 1.35 [1.14, 1.61] | 0.001 | 1.34 [1.19, 1.52] | <0.001 |
| Ever experienced homelessness | ||||
| No | ref | -- | ref | -- |
| Yes | 1.44 [1.34, 1.54] | <0.001 | 1.15 [1.02, 1.29] | 0.025 |
| Adverse Childhood Experiences | ||||
| Low adverse childhood experiences | ref | -- | ref | -- |
| High adverse childhood experiences | 1.23 [1.11, 1.37] | <0.001 | 1.04 [0.93, 1.18] | 0.48 |
| Recent occurrence of psychological violence (less than 3 months) | ||||
| No | ref | -- | ref | -- |
| Yes | 1.23 [1.06, 1.43] | 0.006 | 1.19 [1.06, 1.34] | 0.003 |
High prevalence of self-perceived low HIV risk among those PrEP indicated
Among the 504 participants with available data on self-perceived HIV risk and who were indicated for PrEP based on the study criteria, 55% perceived themselves as being of low or no risk for HIV infection (Table 4). This percentage remained the same after excluding participants who reported current PrEP usage (i.e., PrEP use within the last 30 days). Being below the age of 30 (PR: 1.26, 95% CI: 1.04, 1.53) and having high social support (PR: 1.20, 95% CI: 1.00, 1.47) were associated with higher prevalence of self-perceived low or no HIV risk. Having moderate to severe drug use was associated with higher self-perceived HIV risk (PR: 0.81, 95% CI: 0.66, 0.99).
Table 4.
Factors associated with self-perceived low risk for HIV acquisition among PrEP indicated TGW (N=504)
| Demographics | PR [95% CI] | P-value | aPR [95% CI] | P-value |
|---|---|---|---|---|
| Study Site | ||||
| Baltimore, MD | ref | -- | ref | -- |
| Boston, MA | 1.05 [0.72, 1.54] | 0.79 | 1.01 [0.68, 1.52] | 0.95 |
| New York, NY | 1.07 [0.77, 1.50] | 0.68 | 1.12 [0.79, 1.59] | 0.51 |
| Atlanta, GA | 1.17 [0.78, 1.74] | 0.45 | 1.05 [0.68, 1.62] | 0.82 |
| Miami, FL | 1.05 [0.72, 1.55] | 0.79 | 1.09 [0.73, 1.63] | 0.68 |
| Washington D.C. | 1.06 [072, 1.55] | 0.78 | 1.00 [0.67, 1.49] | 0.996 |
| Online | 1.20 [0.87, 1.65] | 0.27 | 1.09 [0.78, 1.53] | 0.60 |
| Age | ||||
| >=30 years of age | ref | -- | ref | -- |
| <30 years of age | 1.21 [1.05, 1.39] | 0.007 | 1.26 [1.04, 1.53] | 0.02 |
| Education | ||||
| High school or less | ref | -- | ref | -- |
| Some college or more | 1.17 [0.97, 1.41] | 0.10 | 1.11 [0.91, 1.36] | 0.29 |
| Drug Abuse Screening Test | ||||
| Below moderate drug use | ref | -- | ref | -- |
| Above moderate drug use | 0.78 [0.70, 0.87] | <0.001 | 0.81 [0.66, 0.99] | 0.04 |
| Social Support | ||||
| Low | ref | -- | ref | -- |
| High | 1.32 [1.12, 1.55] | 0.001 | 1.22 [1.00, 1.47] | 0.05 |
| Ever experienced homelessness | ||||
| No | ref | -- | ref | -- |
| Yes | 0.75 [0.67, 0.83] | <0.001 | 0.85 [0.70,1.03] | 0.10 |
| Adverse Childhood Experiences | ||||
| Low adverse childhood experiences | ref | -- | ref | -- |
| High adverse childhood experiences | 0.86 [0.73, 1.01] | 0.08 | 0.95 [0.79, 1.14] | 0.57 |
| Currently using PrEP? (within the last 30 days) | ||||
| No | ref | -- | ref | -- |
| Yes | 0.84 [0.69, 1.03] | 0.09 | 0.86 [0.69, 1.06] | 0.16 |
PrEP care continuum among transgender women
Among the 611 participants who were indicated for PrEP based on study criteria, 83% were aware of PrEP (Figure 1). Among those aware of PrEP, 38% had ever taken PrEP prior to the study. Sixty-three percent of those who had ever taken PrEP were using PrEP at the time of the study, and 66% of PrEP users reported 100% adherence within the prior 7 days of the survey (ultimately 13% of those indicated for PrEP). This summary of the PrEP care continuum was similar when using CDC criteria (see Appendix). There were 25 participants who reported using PrEP at the time of screening; however, they were not indicated for PrEP at the time of participation based on study criteria.
Figure 1.
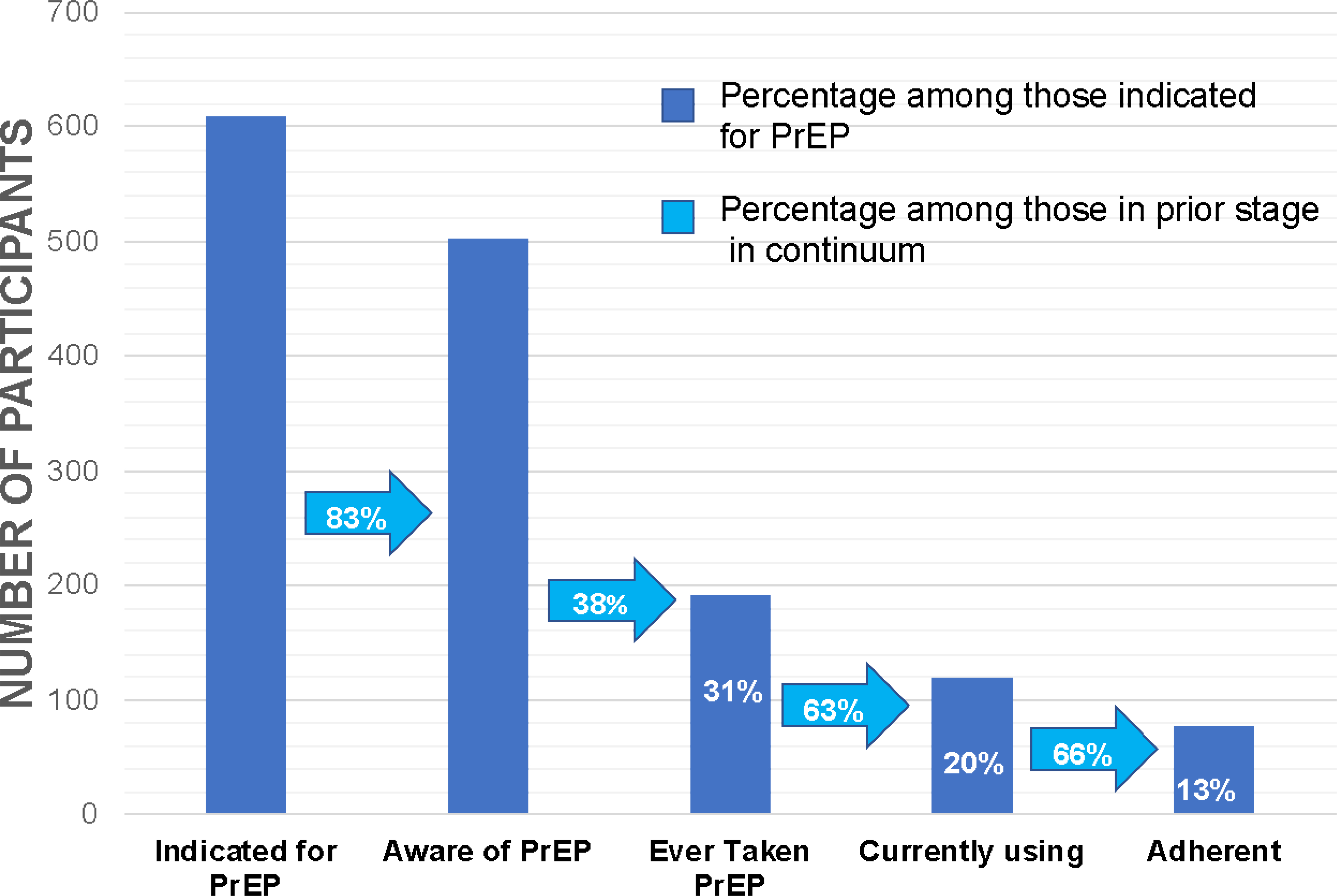
PrEP Care Continuum among participants with indications for PrEP based on LITE study criteria, May 2020
Discussion
In this study we found that there would be an additional 12% of study participants who would be PrEP indicated using prescribing criteria specific to transgender women compared to using the current, CDC prescribing criteria. These participants could potentially benefit from PrEP if health practitioners used evidence-based PrEP indication criteria specific to the HIV risk factors of transgender women. This finding highlights the importance for health practitioners to become educated on these specific criteria to identify and prescribe PrEP to transgender women more efficiently. Additionally, participants who were identified by transgender women-specific criteria for PrEP use were those who may experience greater risk environments as they had lower social support, higher levels of poverty, and higher substance use. Thus, using these specific prescribing criteria may identify transgender women subgroups with higher unmet need for PrEP. These findings suggest that guidelines must include criteria that are specific to transgender women (as well as other transgender or gender non-binary individuals) to accurately determine PrEP indication in these populations and increase PrEP access among those who can benefit the most.
Being Non-Hispanic/Latinx Black, Hispanic/Latinx, having above average drug use, ever being homeless, or having a recent (within the last 3 months) occurrence of psychological violence were associated with a higher prevalence of PrEP indication. These factors (i.e., racial and ethnic minority status, substance use, homelessness, and psychological violence) have also been shown in related literature to be associated with having less access to healthcare.24,25 This lack of access would thus hinder transgender women from engaging with a healthcare professional who would be able to prescribe PrEP, or even identify them as candidates for PrEP use.
The study also found a high proportion (over half) of those indicated for PrEP had reported that they had no or low risk of acquiring HIV, even after analytically excluding participants who reported PrEP use. This is consistent with literature which suggests that perceived susceptibility HIV can be a critical barrier in the uptake of PrEP.26 Factors associated with no or low HIV risk were reporting younger age, greater educational levels, and high social support. Although younger age, higher levels of education, and high social support are factors traditionally associated with better health outcomes, HIV incidence is increasing faster among adolescents and young adults and are priority groups for HIV prevention.27 Generally, these findings confirm the greater need for health practitioners to proactively engage with these patient populations and to increase opportunities for transgender women to learn about and access PrEP. PrEP interventions to improve HIV risk perceptions may benefit from reaching the social networks of younger age transgender women and those with high social support.
We also found that among all participants who had indications for PrEP, there was a low proportion who were currently using and adherent to daily, oral PrEP at the time of the study (13%). Even though most participants with indications for PrEP were aware of PrEP (83%), only 38% had ever taken a medication regimen at the time of the study. Thus, there is a need for more PrEP implementation efforts among transgender women, including comprehensively identifying and counseling those who could most benefit from PrEP and exploring ways to support adherent usage once PrEP is prescribed.
This study had several strengths and limitations. A strength is that it uses one of the largest samples of transgender women (over 1200) recruited across multiple metropolitan areas in the eastern and southern U.S. Also, although there have been several studies exploring PrEP indications among transgender women, this is one of the only studies to explore the level of self-perceived low HIV risk among those who have indications for PrEP. A limitation of the data is that over 100 participants with indications for PrEP did not report their “self-perceived” risk and were not included in this analysis. While this represents less than 10% of the sample, study findings concerning factors associated with self-perceived low or no HIV risk may not reflect all participants with indications for PrEP. Additionally, it is possible that the self-perceived HIV risk variable is misclassified since it was measured through self-report and prior research suggest that respondents tend to under report HIV risks.28 Nonetheless, this further affirms the point that participants who may benefit from PrEP may not self-select themselves to seek care. Also, although we included occurrence of sharing needles during injection drug use as part of criteria for study specific PrEP indications, we did not include occurrences of sharing needles when injecting silicone, fillers, or when injecting hormones. However, we recommend for practitioners to consider any reported needle-sharing practices when considering PrEP indication for transgender women.
Conclusions
This study found that expanding current CDC PrEP prescribing criteria to be specific to transgender women can identify a sizeable number of additional women who could benefit from PrEP. Both PrEP uptake and adherence, however, are low among transgender women who are indicated for PrEP, which is matched by low self-perceived risk for HIV acquisition. These findings highlight the need for transgender women to receive individualized PrEP recommendations and effective education concerning the benefits of PrEP to support PrEP uptake and adherence among those who need it most.
Supplementary Material
Acknowledgements:
The authors would like to express their gratitude to the transgender women who took part in this study. This study would not be possible without their participation. We also acknowledge the work of the entire American Cohort To Study HIV Acquisition Among Transgender Women team: Andrea Wirtz (multiple PI; Johns Hopkins University (JHU)); Sari Reisner (multiple PI; Harvard University); Keri Althoff (JHU); Chris Beyrer (JHU); James Case (JHU); Erin Cooney (JHU); Oliver Laeyendecker (JHU); Megan Stevenson (JHU) and Jeffrey Herman (JHU); Tonia Poteat (University of North Carolina); Kenneth Mayer (Fenway Health); Asa Radix (Callen-Lorde Community Health Center); Christopher Cannon (Whitman-Walker Health); W. David Hardy (Whitman-Walker Health); Jason Schneider (Emory University and Grady Hospital); Sonya Haw (Emory University and Grady Hospital); Allan Rodriguez (University of Miami); Andrew Wawrzyniak (University of Miami); the incredible research teams at each study site; and the LITE community advisory board, including the following individuals: Sherri Meeks, Flora Marques, Sydney Shackelford, Nala Toussaint, and SaVanna Wanzer, as well as those who have remained anonymous.
Sources of Support: Research reported in this publication was jointly supported by the National Institute of Allergy and Infectious Diseases, the National Institute of Mental Health, and the National Institute of Child Health and Human Development of the National Institutes of Health under Award Number UG3/UH3AI133669 (ALW and SLR). Research reported in this publication was also supported by HIV/AIDS, Hepatitis, STD, and TB Administration (HAHSTA), Washington DC Department of Health. The LITE study is also appreciative of support from the CFAR at partner institutions, including JHU (P30AI094189), Emory University (P30AI050409), Harvard University (P30AI060354), DC CFAR (P30AI117970), and the University of Miami (P30AI073961). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or HAHSTA.
Footnotes
Conflicts of Interest
There are no conflicts of interest to declare among the authors.
References
- 1.Becasen JS, Denard CL, Mullins MM, Higa DH, Sipe TA. Estimating the prevalence of HIV and sexual behaviors among the US transgender population: a systematic review and meta-analysis, 2006–2017. American journal of public health. 2019;109(1):e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baral SD, Poteat T, Strömdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. The Lancet infectious diseases. 2013;13(3):214–222. [DOI] [PubMed] [Google Scholar]
- 3.Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. New England Journal of Medicine. 2010;363(27):2587–2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murnane PM, Celum C, Nelly M, et al. Efficacy of pre-exposure prophylaxis for HIV-1 prevention among high risk heterosexuals: subgroup analyses from the Partners PrEP Study. AIDS (London, England). 2013;27(13). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murnane PM, Brown ER, Donnell D, et al. Estimating efficacy in a randomized trial with product nonadherence: application of multiple methods to a trial of preexposure prophylaxis for HIV prevention. American journal of epidemiology. 2015;182(10):848–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grant RM, Pellegrini M, Defechereux PA, et al. Sex Hormone Therapy and Tenofovir Diphosphate Concentration in Dried Blood Spots: Primary Results of the Interactions Between Antiretrovirals And Transgender Hormones Study. Clinical Infectious Diseases. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grant RM, Anderson PL, McMahan V, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. The Lancet infectious diseases. 2014;14(9):820–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Golub SA, Gamarel KE, Rendina HJ, Surace A, Lelutiu-Weinberger CL. From efficacy to effectiveness: facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in New York City. AIDS patient care and STDs. 2013;27(4):248–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuhns LM, Reisner SL, Mimiaga MJ, Gayles T, Shelendich M, Garofalo R. Correlates of PrEP indication in a multi-site cohort of young HIV-uninfected transgender women. AIDS and Behavior. 2016;20(7):1470–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sevelius JM. Gender affirmation: A framework for conceptualizing risk behavior among transgender women of color. Sex roles. 2013;68(11–12):675–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sevelius JM, Deutsch MB, Grant R. The future of PrEP among transgender women: the critical role of gender affirmation in research and clinical practices. Journal of the International AIDS Society. 2016;19:21105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schnarrs PW, Stone AL, Salcido R Jr, Baldwin A, Georgiou C, Nemeroff CB. Differences in adverse childhood experiences (ACEs) and quality of physical and mental health between transgender and cisgender sexual minorities. Journal of psychiatric research. 2019;119:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Campbell JA, Walker RJ, Egede LE. Associations between adverse childhood experiences, high-risk behaviors, and morbidity in adulthood. American journal of preventive medicine. 2016;50(3):344–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Service CfDCaPUPH. Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 Update: a clinical practice guideline. In: Service CfDCaPUPH, ed2018. [Google Scholar]
- 15.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health education quarterly. 1988;15(2):175–183. [DOI] [PubMed] [Google Scholar]
- 16.Wirtz AL, Cooney EE, Chaudhry A, Reisner SL. Computer-Mediated communication to facilitate synchronous online focus group discussions: feasibility study for qualitative HIV research among transgender women across the United States. Journal of medical Internet research. 2019;21(3):e12569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reisner SL, Chaudhry A, Cooney E, Garrison-Desany H, Juarez-Chavez E, Wirtz AL. ‘It all dials back to safety’: A qualitative study of social and economic vulnerabilities among transgender women participating in HIV research in the USA. BMJ open. 2020;10(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wirtz AL, Cooney EE, Stevenson M, et al. Digital Epidemiologic Research on Multilevel Risks for HIV Acquisition and Other Health Outcomes Among Transgender Women in Eastern and Southern United States: Protocol for an Online Cohort. JMIR Res Protoc. 2021;10(4):e29152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Survey CHI. CHIS 2003 Adult Questionnaire. In. Los Angeles, CA: UCLA Center for Health Policy Research; 2011. [Google Scholar]
- 20.Bohn M, Babor T, Kranzler H. Validity of the Drug Abuse Screening Test (DAST-10) in inpatient substance abusers. Problems of drug dependence. 1991;119:233–235. [Google Scholar]
- 21.Bynum L, Griffin T, Riding D, et al. Adverse childhood experiences reported by adults-five states, 2009. Morbidity and Mortality Weekly Report. 2010;59(49):1609–1613. [PubMed] [Google Scholar]
- 22.Shieh E, Marzinke M, Fuchs E, et al. Transgender women on estrogen have significantly lower tenofovir/emtricitabine concentrations during directly observed dosing when compared to cis men. Paper presented at: AIDS RESEARCH AND HUMAN RETROVIRUSES2018. [Google Scholar]
- 23.LLC S. Stata 15 base reference manual. 2017.
- 24.Lester H, Bradley CP. Barriers to primary healthcare for the homeless: the general practitioner’s perspective. The European Journal of General Practice. 2001;7(1):6–12. [Google Scholar]
- 25.Bolton LB, Giger JN, Georges CA. Structural and racial barriers to health care. ANNUAL REVIEW OF NURSING RESEARCH. 2004;23:39–58. [PubMed] [Google Scholar]
- 26.Felsher M, Szep Z, Krakower D, Martinez-Donate A, Tran N, Roth AM. “I Don’t Need PrEP Right Now”: A Qualitative Exploration of the Barriers to PrEP Care Engagement Through the Application of the Health Belief Model. AIDS Education and Prevention. 2018;30(5):369–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brennan J, Kuhns LM, Johnson AK, et al. Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. American journal of public health. 2012;102(9):1751–1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Norwood MS, Hughes JP, Amico KR. The validity of self-reported behaviors: methods for estimating underreporting of risk behaviors. Annals of epidemiology. 2016;26(9):612–618. e612. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


