Abstract
Background
In 2019, 1.5 billion international tourist trips were counted worldwide. Germany, with 70.8 million vacations lasting ≥ 5 days, was one of the populations most willing to travel. These days, even elderly and multimorbid persons regularly travel long-distance, which can be associated with significant health risks. By advising travelers and implementing preventive measures, the risk of illness can be reduced significantly.
Methods
A selective survey of PubMed was performed to identify publications on medical advice for travelers between 2000 and 2020. We included guidelines, studies, and recommendations that mainly deal with the preventive aspects of travel medicine and have a high level of practical relevance and the highest possible level of evidence. Previously published guidelines (based on the GRADE criteria) were adopted, and recommendations not based on the results of scientific studies were characterized as Good Clinical Practice (GCP).
Results
Many medical recommendations for travelers still rely on individualized, experience-based, or consensus-based assessments. Apart from a review of medical history and vaccination status, a risk analysis is performed, travel fitness is evaluated individually, and a prevention plan is designed. Particular attention is devoted to malaria prophylaxis, vector protection, and traveler’s diarrhea. Medical advice before travel is especially important for the elderly, children, pregnant women, the chronically ill, long-term and adventure travelers as well as migrants from malaria-endemic areas who are returning home.
Conclusion
The health risks associated with travel can be minimized by specialist medical advice. Many recommendations are empirical in nature and require further research.
In 2019, 1.5 billion tourist trips were recorded worldwide (1). Germany, with 70.8 million tourist trips lasting longer than 5 days, was one of the nations most willing to travel. This willingness to travel is also increasingly seen among older and multimorbid individuals (1). Since there are no comprehensive systematic surveys on travel-related diseases in Germany, apart from the data provided by a handful of sentinel centers, it is difficult to draw valid conclusions about disease frequencies and entities (2). In a systematic literature review including nine studies from the USA and Europe, the proportion of travelers that acquired illness in the years 1985–2016 was 6–87% at an average trip duration of 8–21 days (3). Many of the relevant travel-related diseases, such as travelers’ diarrhoea, skin disorders, as well as vector-borne and vaccine-preventable diseases, can be prevented or their risk reduced (4– 6).
cme plus
This article has been certified by the North Rhine Academy for Continuing Medical Education. The questions on this article can be found at http://daebl.de/RY95. The submission deadline is 27 May 2022.
Participation is possible at cme.aerztebatt.de
Method
A selective literature search was conducted in PubMed for publications in the period 2000–2020. The search included guidelines from scientific societies, as well as studies and recommendations primarily dealing with the preventive aspects of travel medicine (pretravel advice, vaccinations, fitness to travel, malaria prevention, vector protection, and prevention of travelers’ diarrhea), while at the same time having high practical relevance and the highest possible level of evidence. Evidence was evaluated according to recommendations of the Agency for Healthcare Research and Quality (AHRQ). Previously published recommendations (based on GRADE [Grading of Recommendations, Assessment, Development and Evaluation] criteria) were adopted. Treatment methods that have been tried and tested in practice, as well as recommendations not based on the results of scientific studies, were characterized as Good Clinical Practice (GCP).
Procedure regarding medical advice for travelers
In routine practice, a structured and standardized approach has proven its worth (GCP) (7– 9). Ideally, the consultation should take place 6, but at least 4, weeks prior to the travel start date, in order that certain travel vaccinations, for instance, can be completed. Even in the case of last-minute trips, important preventive measures such as health advice, malaria prevention, and vaccinations can still be carried out or initiated.
Cost clarification and consultation mandate
At the time of scheduling the appointment, or at the very latest before the consultation begins, the traveler should be made aware of the fees that will be incurred (individual healthcare services)—even though many health insurance funds now cover the cost of travel vaccinations and malaria prophylaxis (10).
Travel analysis
In addition to destination and time period, important information includes: route(s), stopovers, reason, type and duration of the trip, means of transport used, (hotel) accommodation, previous travel experiences, and activities planned (for example, trekking, diving). Ideally, a detailed travel itinerary is provided.
Patient history and vaccination status
In order to carry out a risk analysis, a detailed medical history is required, including chronic, current, and travel-related illnesses (for example, fear of flying, kinetosis), previous surgical procedures, immune and vaccination status, medication, allergies, previous vaccination side effects and drug intolerances (for example, malaria prophylaxis), as well as pregnancy and health insurance status abroad.
Risk analysis and assessing fitness to travel
The assessment of fitness to travel is based on the risk of decompensation during travel (GCP). Important factors in this regard include medical care at the travel destination, risks of infection, standards of hygiene, climate, and potential preventive measures. Fitness for diving should be determined by a qualified diving physician (certified, for example, by the German Society for Diving and Hyperbaric Medicine [GTÜM]), taking into account the relevant recommendations (11).
To determine fitness to fly, it is important to assess the patient’s overall clinical status. Exclusion criteria can be found in the airlines’ conditions of carriage or in the International Air Transport Association (IATA) catalog (12). A British guideline and the US Centers for Disease Control and Prevention (CDC) also provide valuable information (13, 14). The following situations are examples of potential exclusion criteria:
Highly contagious (untreated) infectious diseases
Unstable angina pectoris
Anemia (Hb level <8.5 g/dL)
Within 3 days of acute myocardial infarction
Pneumothorax
Fresh or unsplit plaster cast
Acute bleeding
Acute psychoses within the preceding 30 days
Pregnancy beyond 36 weeks (GCP).
According to a survey conducted in Germany of 2010 individuals aged over 14 years, 3% suffer from a fear of flying (aviophobia) (15). In the case of aviophobia, it can be helpful to actively address the subject of flying and fear (psychoeduction) and practice relaxation techniques in advance of travel (16). A seat on the aisle or near the aircraft wings should be preferred (GCP). In a randomized controlled trial with 69 participants, internet-based exposure treatment (NO-FEAR Airlines) was effective in all endpoints, such as the index score on the Fear of Flying Scale, compared to the control group (score difference: -17.23, p < 0.001; effect size: -1.51; 95% confidence interval [CI]: [-2.13; -0.71]) (17).
Children under the age of 5 years and pregnant women should not travel to malaria-endemic regions. An initial manifestation of malaria during pregnancy can pose significant risks to the mother and fetus (18). Young children can develop life-threatening organ complications such as cerebral malaria within hours of the first symptoms—or the disease manifests atypically (for example, without fever), thereby hampering the rapid initiation of treatment (19). Due to the risk of fetal malformations, pregnant women should also avoid traveling to areas with Zika virus outbreaks (20). Epilepsy patients should have long-term, stable seizure control and carry sufficient medication (GCP).
Individual prophylaxis plan
An individual prophylaxis plan includes the standard vaccinations recommended by the German Standing Commission on Vaccination (STIKO), as well as any travel-specific vaccinations indicated (table 1) (21, 22). In the case of contraindications to yellow fever vaccination or other vaccinations, a medical exemption certificate can be issued.
Table 1. Overview of the most important travel vaccinations.
| Vaccination | Minimum age | Standard vaccination schedule or basic immunization (BI), route of administration | Immunity starting from |
| Hepatitis A | 1–18 years, depending on the vaccine | 1 × i.m. | > 2 weeks after BI |
| Hepatitis B | From birth | 0–1–6 months i. m. | > 4 weeks after BI |
| Hepatitis A + B | 1–16 years, depending on the vaccine | 0–1–6 months i. m. | > 2 or 4 weeks after BI |
| TBE | 1–16 years, depending on the vaccine | 0–14 days to 9 months (after 2nd vaccine) i. m. | 2 weeks after 2nd vaccination for the current season |
| 0–1–5 months (after 2nd vaccine) i. m. | |||
| Meningococcal serogroups A, C, W135, Y | 6 weeks to 2 years, depending on the vaccine | 1 × i.m. | > 1 week after BI |
| Meningococcal serogroup B | 2 months or 10 years,depending on the vaccine | 0–1 months i.m. or 0–6 months i. m. | Immediately after BI (2nd vaccination) |
| Rabies | From birth | 0–7–21 (28) days i.m.,rapid schedule *1 : 0–3–7 days i. m. | 2–4 weeks after BI |
| Polio | 2 months | 0–1–2 months i.m. | Immediately after BI (3rd dose) |
| Yellow fever | 9 months | 1 × s.c. preferred, see product information for i.m. injection | 10 days after BI (consider for entry date) |
| Japanese encephalitis (JE) | 2 months | 0–28 days i.m., children < 3 years receive half-doses, rapid schedule*2: 0–7 days i. m. | 4 weeks after BI |
| Typhoid fever | 2 years (injectable vaccine) | 1 × i.m. | 14 days after BI |
| 5 years (oral vaccination) | 0–2–4 days, orally; there should be a minimum interval of 3 days between the 3rd vaccination dose and start of malaria prophylaxis | > 10 days after BI | |
| Typhus + hepatitis A | 16 years | 1 × i.m. | > 2 weeks after BI |
| Cholera | 2–7 years, depending on the vaccine | 1 x or 0–7(–14) days orally, maximum of 6-week interval between doses, otherwise new vaccination | 7–10 days after BI, for at least 6 months |
Overview of the vaccines most frequently used in Germany for travel medicine. The product information of the respective vaccines should be assessed prior to vaccination. A detailed and continuously updated summary, including rapid vaccination schedules and information on boosters, can be found in tabular form on the website of the authors’ institution (www.uniklinikum-leipzig.de/einrichtungen/medizinische-klinik-2/infektions-und-tropenmedizin); for further details see (22).
*1 Only for adults aged 18–65 years (if the conventional pre-exposure prophylaxis schedule cannot be completed before the required vaccine protection within 21 or 28 days)
*2 Only for adults aged 18–65 years (if the conventional schedule cannot be completed before the required vaccine protection within 28 days)
i.m., intramuscular; s.c., subcutaneous
For some destinations, it is essential to prescribe malaria chemoprophylaxis and recommend suitable repellents (23). In a small number of situations, for example, in the case of immunosuppression, chronic inflammatory bowel disease (IBD), or short trips involving high risk of infection, the prescription of prophylactic antibiotics can be considered (GCP). The carbonic anhydrase inhibitor acetazolamide is able to prevent acute mountain sickness (AMS) with a moderate level of evidence (relative risk [RR]: 0.47; [0.39; 0.56]; systematic review, 16 studies; 2301 participants) (24). When traveling to regions where there is high risk for travelers’ diarrhea (for example, South and South-East Asia, Egypt), no first-aid kit should be without preparations for oral rehydration solutions (ORS) (25).
Deep vein thrombosis (DVT) prophylaxis using compression stockings and/or low-molecular-weight heparins or direct oral anticoagulants (DOACs; off-label use) is indicated in high-risk patients traveling on flights lasting more than 3 h—but is not generally recommended (26, 27). According to the randomized controlled trial (RCT) LONFLIT 5 JAP, the incidence rate of DVT with and without compression stockings was 0.97% versus 5.8%, respectively (p<0.0025; [28]). In the likewise randomized controlled LONFLIT3 study, the incidence rate of DVT with and without prophylactic heparinization was 0% versus 4.8%, respectively (p < 0.05; [29]). There are no RCTs to date on the use of DOACs in this indication (30).
For the prevention of seasickness and motion sickness, anticholinergics (for example, transdermal scopolamine) and antihistamines such as dimenhydrinate can be prescribed (31).
Education
The central aim of the consultation is to provide risk information based, as far as possible, on evidence, as well as to impart destination-specific health literacy skills. German nationals can only use the European Health Insurance Card, found on the back of the national health insurance card, to obtain medical services in travel destinations within the EU or in contracting countries (32). Good international health insurance should include pre-existing conditions, provide assistance services, and ensure “medically advisable and justifiable repatriation” (32).
In many countries, there are relevant health risks over and above infectious diseases, for example, as a result of road traffic, pollution, crime, and terrorism. The German Federal Foreign Office and other institutions provide information in this regard (list of information with useful internet addresses at www.uniklinikum-leipzig.de/einrichtungen/medizinische-klinik-2/infektions-und-tropenmedizin).
The consultation also includes instructions on hygiene and behavioral measures, as well as first aid in special situations, such as following animal bites, fever, diarrhea, or during stays at high altitudes. For example, rapid ascent to high altitudes (> 2500 m) can cause acute altitude sickness (AMS), the prevalence of which—depending on the study, age, absolute altitude reached, as well as the rate of ascent—can be as high as 30–45% even at moderate altitudes (3500 m) (33). If warning symptoms such as nausea, headache, or reduced performance fail to prompt a rapid descent, high-altitude cerebral edema (HACE) or high-altitude pulmonary edema (HAPE) may occur (34).
Climate-related illnesses such as heat stroke, heat exhaustion/syncope, hypothermia, and frostbite can be prevented by means of a combination of acclimatization, appropriate behavior, suitable clothing, and sufficient intake of fluids, electrolytes, and food (GCP).
Time differences of more than 5 h result in disruption of the circadian rhythm in the form of jet lag (35). It has proven effective in practice to allow 1 day of adjustment time for every two time zones crossed on eastbound flights and 50% less when traveling westbound (GCP). In addition to sufficient sleep, it is considered beneficial to immediately participate in the local daily rhythm of the destination (involving time spent in daylight), avoid alcohol and sleeping pills, and refrain from strenuous activities during the first days of travel (12, 36). According to a systematic review with integrated meta-analysis, immediate-release melatonin (0.5–5 mg/day) is effective for the prevention and treatment of jet lag from a time difference of 5 h (RR jet lag score > 60: 0.5; [0.25; 0.74]; number needed to treat [NNT]: 2) (37, 38). As a physiological neurohormone, melatonin synchronizes the day–night rhythm via central and peripheral oscillators.
Finally, travelers should be familiar with the “ABC” of sun protection: avoidance, clothing, and sunscreen (39, 40).
Advice on follow-up care
The patient being consulted must be aware that travel-related illnesses can develop even after their trip. The most important warning signs and symptoms that should prompt (specialist) medical clarification are listed in Box 1. For example, any unexplained fever up to 4 months after returning from a malaria-endemic area requires clarification within 24 h.
BOX 1. Warning symptoms and signs.
Unexplained fever (particularly following a stay in a malaria-endemic area)
Diarrhea with bloody stools or fever
Chronic (> 4 weeks) diarrhea
Rash
Petechiae
Chronic (> 4 weeks), non-healing skin lesions
Lymphadenopathy
Hepato-/splenomegaly
B-symptoms
Unexplained blood count changes (for example, eosinophilia, thrombocytopenia, leukocytopenia)
Unexplained elevation of liver values
Unexplained (chronic) cough and persistent respiratory symptoms
Myalgia, arthralgia
Paresthesia, CNS symptoms
Bleeding diathesis
Preventive measures
Medications and first-aid kit
Not all travel destinations allow travelers to bring medications into the country. If travelers are taking various active substances and medical items (for example, syringe needles) with them, it may be advisable to obtain a medical certificate (GCP). Ideally, this should be written in the languages of the countries to be visited/transited, but at least in English. Important medications and an informative medication list should always be carried in hand luggage; travelers should ensure that they take double the amount with them, distributed if possible over several pieces of luggage.
If the journey involves a time shift of more than three time zones, dosages of long-term medication(s), for example insulin and cortisone preparations, initially need to be adjusted (GCP): westbound air travel increases dose requirements due to the “longer day,” whereas the “shorter day” with eastbound air travel reduces requirements (e1).
Box 2 provides an overview of the tried and tested first-aid kit.
BOX 2. Recommendations on additional basic items in a first-aid kit (indication/products).
-
Wounds, blisters, fractures/distortions
Three gauze bandages 4/6/8 cm wide, respectively
One packet of sterile gauze
Cotton swabs
Band-aids 4 and 6 cm wide; two rolls (50 cm) of adhesive plaster in widths of 1.25 and 2.5 cm, respectively
Two elasticated bandage wraps 8 and 10 cm wide, respectively
3–4 wound closure strips for cuts
Antiseptic wound gel or solution (e.g., povidone iodine, octenidine)
Tweezers
Tape, blister plasters, special padding material for plasters
A universal splint (foldable; in aluminum or plastic)
Triangular cloth
-
Hygiene, prevention, medical aids
Mouth/nose protection masks
Hand disinfectant (e.g., in gel form), preferably alcohol-based
Condoms
2–3 pairs of protective gloves
Scissors
Safety pin
Sufficient sunscreen agents (at least SPF 20; for children and fair-skinned people, at least SPF 30)
One emergency blanket (reflective)
Where applicable, ear drops for scuba divers for the prevention of otitis externa (containing ethanol, glycerol, glacial acetic acid)
-
Insect bites and stings
Tick tweezers/fixing pin
Corticosteroid cream
Antihistamine cream (also available combined with hydrocortisone)
-
Pain and fever
At least 10 tablets each of paracetamol/ibuprofen/novaminsulfone*1
Thermometer
For severe pain > 10 tramadol capsules (50 mg) or 10 tilidine tablets (50/4 mg)
-
Diarrhea
Electrolyte mix for adults and children (in powder form to mix, and in fruit flavor for children)
Racecadotril, tannin albuminate/ethacridine lactate, loperamide (only as emergency medication)
Azithromycin, if necessary rifaximin/rifamycin (only after an appropriate risk–benefit assessment and in the case of non-invasive, non-bloody diarrhea without fever)
-
Abdominal pain (cramping)
5–10 butylscopolaminium bromide tablets
-
Nausea, vomiting, kinetosis
5–10 dimenhydrinate chewable tablets or 5–10 metoclopramide tablets, against kinetosis; alternatively, ginger tablets/chewing gum or scopolamine plaster
-
Cough
10 dihydrocodeine extended-release tablets or noscapine
-
Sunburn, skin and lip care/protection
Bamipine lactate or flumetasone; dexpanthenol (skincare)—as gel, lotion, or spray
Sunscreen cream/pen (SPF 30–50)
-
Insect bite protection
Repellents, preferably containing DEET or icaridin (as a precaution, purchased in home country); where appropriate, permethrin to treat clothing/mosquito net
-
Malaria protection
Sufficient supply of tablets for malaria chemoprophylaxis or emergency treatment (purchased at a licensed pharmacy in home country to avoid counterfeits)
-
Individual own requirements/medication, doctor’s letter
Sufficient quantities of regular medications
Sun glasses and, where applicable, spare glasses
Where applicable, spare contact lenses and care products
Where applicable, monitoring devices (blood pressure, blood glucose, INR)*2
-
Acute mountain sickness (AMS) and high-altitude cerebral edema (HACE)
10 dexamethasone tablets 8 mg*3
-
High-altitude pulmonary edema (HAPE)
10 nifedipine extended-release tablets 20 mg*3
-
Angina
4–6 nitroglycerin capsules, nitroglycerin spray
-
Medical aids and devices
Disposable syringes, 1–2 in each size: 2/5/10 mL, disposal hypodermic needles, 1–2 in different sizes (where applicable, with medical certificate)
Tourniquet
Rescue sheet (for evacuation of persons)
Stethoscope
Torch/penlight, alternatively, cellphone LED light
*1 No acetylsalicylic acid (ASS) due to risk of bleeding or complications (e.g., in the case of Dengue fever), ibuprofen also not recommended in suspected Dengue fever
*2 Where necessary, medical certificate and medication package inserts, doctor’s letter in several languages, consider storage conditions (temperature range!) for medications and monitoring devices
*3 Information regarding indicated additional descent
AMS, acute mountain sickness, HACE, high-altitude cerebral edema; HAPE, high-altitude pulmonary edema; INR, international normalized ratio
Malaria prophylaxis
In Germany, approximately 1000 cases of imported malaria were registered annually between 2014 and 2019 (> 90% from sub-Saharan Africa) (e2). More than 70% of all imported cases involved the potentially life-threatening Plasmodium falciparum malaria. In 2019, of 814 cases with incomplete follow-up, only two deaths due to Plasmodium falciparum were registered (e2, e3).
The risk and severity of disease depend on numerous factors, including, among others, prevention compliance (23, e4– e8). According to a systematic review, the following adherence factors are beneficial for malaria prophylaxis:
Higher age of travelers
Shorter travel duration
Good (previous) experiences with tolerability of anti-malarial drugs
Going on a holiday rather than a business or adventure trip
Seeking pretravel advice (e9).
Recommendations on prophylaxis should always be tailored to the individual (23). Consistent adherence to all preventive measures does not guarantee absolute safety—not even guideline-compliant malaria chemoprophylaxis is able to ensure this (for example, effectiveness of atovaquone/proguanil compared to placebo: 95.8%, [91.5; 97.9]; meta-analysis, 10 RCTs, 4539 participants) (e10).
The following measures can be recommended for antimalarial prophylaxis (14, 23, e11, e12):
Exposure prophylaxis
Long-term chemoprophylaxis
Standby emergency treatment.
Insect bites should be consistently avoided around the clock (GCP). When traveling to high malaria risk areas, regular chemoprophylaxis is additionally indicated as a general rule (Table 2, eTable, eFigure) (23).
Table 2. Medications for malaria prophylaxis or standby emergency treatment, modified from (23).
| Dosage of antimalarial drugs for prophylaxis and treatment in adults | ||
| Medication | Prophylaxis | Standby emergency treatment (SBET) |
| Atovaquone/proguanil*1 | From 40 kg BW: 1 tablet daily (= 250/100 mg); between 1–2 days before and 7 days after stay in a malaria area | From 40 kg BW: 4 tablets (= 1000/400 mg) as a single daily dose on 3 consecutive days |
| Doxycycline*2 | 1 Tablet daily (= 100 mg); between 1–2 days before and 4 weeks after stay in a malaria area | Suitable only as part of combination therapy |
| Mefloquine*3 | • Special precautions to be followed according to the product information; – Under 90 kg BW: 1 tablet per week (= 250 mg) – From 90 kg BW: 1½ tablets per week (= 375 mg) – From 120 kg BW: 2 tablets per week (= 500 mg) • Between 1–3 weeks before and 4 weeks after stay in a malaria area |
No longer recommended: approval in Germany withdrawn in 2016 |
| Artemether/lumefantrine*4 | Not suitable | From 35 kg BW: initial 4-tablet dose (= 80/480 mg); followed by 4-tablet doses after 8, 24, 36, 48, and 60 h |
| Dihydroartemisinin–piperaquine*5 | Not suitable | • Currently not approved for SBET*5 • Therapeutic dose in uncomplicated malaria: 4 tablets (= 1 280/160 mg) daily on 3 consecutive days |
Overview of the most important medications for malaria chemoprophylaxis and standby emergency treatment (SBET). Attention should be paid to the product information. A dosing table according to body weight for children can be found in the eTable
*1 To be taken with food (including dairy products) at the same time every day
*2 To be taken with food and plenty of fluid, not together with dairy products; formally off-label use; the monohydrate formulation has better gastrointestinal tolerability
*3 For first-time mefloquine prophylaxis, start 2–3 weeks before departure to malaria area and check tolerability
*4 To be taken with food (including dairy products)
*5 To be taken with fluid between meals. Need for ECG monitoring due to QTc prolongation. Piperaquine is a weak CYP3A4 inhibitor. No more than two treatments permitted within a 12-month period. Due to piperaquine’s long elimination half-life, no second treatment should be performed within 2 months of the first treatment cycle. Not suitable for the treatment of complicated Plasmodium falciparum malaria.
BW, body weight; SBET, standby emergency treatment
eTable. Weight-adjusted dosage recommendations on medications for malaria prophlaxis*1 modified from (23).
| Body weight (kg) | Age | Tablets/day Atovaquone/proguanil 62.5/25 mg (junior)*2 | Tablets/dayDoxycycline 100 mg*2 | Tablets/week Mefloquine 250 mg*2 |
| 5–9 | < 4 months | ½ (up to 8 kg BW, off-label use) | – | ⅛ tablet |
| 9–11 | 4–11 months | ¾ (from 8 kg BW, off-label use) | – | ¼ tablet |
| 11–15 | 1–2 years | 1 | – | ¼ tablet |
| 15–19 | 3–4 years | 1 | – | ¼ + ⅛ tablet |
| 19–25 | 5–7 years | 1; or 2 from 21 kg BW | – | ½ tablet |
| 25–36 | 8–10 years | 2; or 3 from 31 kg BW | ½ | ½–¾ tablet |
| 36–50 | 11–13 years | 3 ‘junior’ tablets; or 1 tablet for adults (250/100 mg) from 40 kg BW | ¾ | ¾–1 tablet |
| > 50 | > 13 years | 1 tablet for adults (250/100 mg) | 1 | 1 tablet |
*1 Atovaquone/proguanil (‚junior‘ formulation), doxycycline and mefloquine.
*2 A commercially available pill splitter is recommended for pill splitting. Attention should always be paid to the respective valid product information.
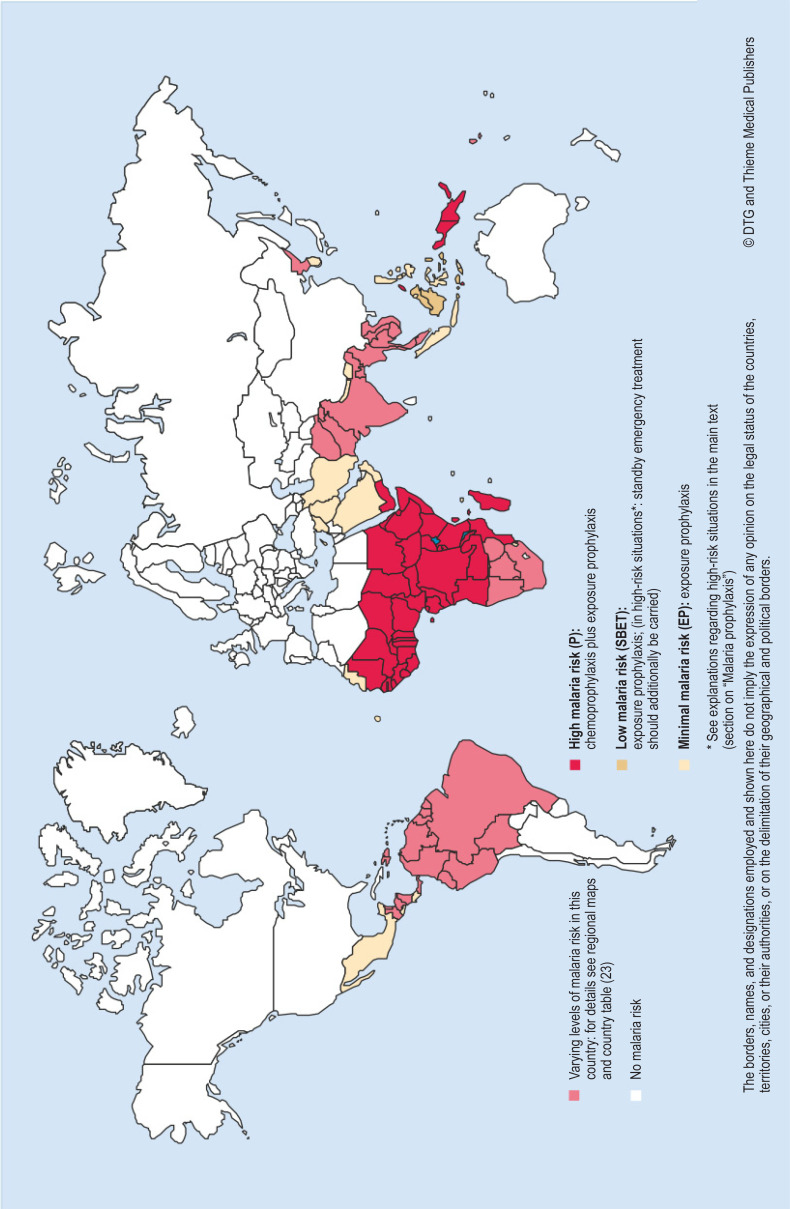
eFigure.
Recommendations on malaria prevention according to the German Society for Tropical Medicine, Travel Medicine and Global Health (DTG): overview map
Reprinted with kind permission of the German Society for Tropical Medicine, Travel Medicine and Global Health (DTG) and Thieme Medical Publishers.
The criteria for standby emergency treatment (SBET) have been heavily restricted in the current guidelines, since travelers often encounter problems with its use. According to a meta-analysis by Tan et al., the overall pooled prevalence of indicated SBET among 26,403 travelers was only 2.5% ([1.1; 4.3%]; seven prospective cohort studies [e13]). If one assumes a malaria incidence of < 0.001% for low-incidence countries, the number needed to prescribe (NNP) is between 370 and 981 in order for SBET to be used in a judicious manner (e13). Added to this is the fact that many tourist regions are able to ensure the provision of ever better medical care (23). Therefore, SBET should only be prescribed for trips lasting longer than 7 days to areas with a low risk of malaria and poor medical care.
Vector control
To avoid insect and tick bites, as well as related diseases, the following measures of exposure prophylaxis are generally recommended (23, e14):
Topical repellents (table 3)
Spatial repellents and insecticide sprays
Light-colored, full-length, and closed clothing
Bed nets—if necessary treated with insecticide
Behavioral measures.
Table 3. Important repellents/insecticides available in Germany.
| Active ingredient concentration | Repels mosquitoes for up to | Age restriction | Use during pregnancy |
| DEET (diethyltoluamide) | |||
| 30% | 6 h | From 3 years*1 | Insufficient data according to the manufacturer |
| 50% | 8 h | From 2 years*1 | |
| Icaridin | |||
| 20% | 6–12 h | From 6 months or 2 years depending on product*1 | Possible depending on product (also while breastfeeding) |
| IR3535 (ethyl butylacetylaminopropionate, EBAAP) | |||
| 10% | 4 h | From 2 months | Possible |
| 20% | 6 h | From 1 year | Possible |
| Oil of lemon eucalyptus (e.g., p-menthane-3,8-diol,, PMD) | |||
| 30% | 6 h | From 1 year | Not specified |
| Permethrin (insecticide to treat textiles [clothing and bed nets]) | |||
| 2% | 4 weeks | From 3 years | Possible |
| 5% | 4 weeks | From 3 years | Not specified |
Overview of important insect and tick repellents available in Germany.
Travelers should read the package leaflet before use. Not all repellents work equally well against mosquitoes, ticks, and bugs. The respective package leaflets provide information on this. The periods of duration of protection indicated for the individual repellents may vary according to environmental and personal factors. It is not uncommon for similar-sounding trade names to disguise different active ingredients. The table provides a non-evaluative selection of possible examples of products on the German market (modified from [23]).
*1 DEET (30–50%) and icaridin are approved for use from as early as 2 months of age in many countries (e.g., Great Britain, USA).
Repellents should not be applied until sunscreen products have had time to become effective (GCP). Particularly in malaria-endemic areas, it is beneficial to avoid outdoors at dusk and during the night as far as possible, and to instead stay indoors in mosquito-proof air-conditioned rooms, ideally protected by window and door grilles (e15, e16).
Prophylaxis and primary treatment of travelers’ diarrhea
Acute travelers’ diarrhea (TD) represents one of the most frequent health disorders experienced during long-distance travel, occurring in 10–40% of travelers in the first 2 weeks, depending on the destination, local microepidemiology, and style of travel (e17, e18). This applies in particular to South and Southeast Asia, as well as to West and Central Africa; backpackers tend to be more at risk than travelers staying in hotels (e19). The established rule of prevention “boil it, peel it, cook it, or forget it!” harbors problems of adherence and evidence. Nevertheless, travelers should be urged to observe good food and hand hygiene for plausibility reasons (GCP). Despite all “precautionary measures” and even when staying in five-star hotels, it is not always possible to definitively prevent TD (e19). According to a systematic evidence review process in 2017 conducted by the International Society of Travel Medicine (ISTM), antibiotics should not be routinely used for TD prevention due to potential side effects and resistance induction (strong level of recommendation, low to very low level of evidence), although they could prevent an estimated 58–88% of all TD episodes (e20). Having said that, they can be considered for high-risk travelers (for example, those with inflammatory bowel disease [IBD] or immunosuppression) (strong recommendation, low to very low level of evidence) (e20). If indicated, rifaximin or bismuth subsalicylate (not available in Germany) are recommended for prophylaxis (strong recommendation, low to high level of evidence). According to a meta-analysis of four RCTs and 879 people, taking a daily dose of 400–600 mg of rifaximin can reduce the risk of disease by 47.8% ([37.5; 61.0], p < 0.001) (e21). Fluoroquinolones are not recommended by the ISTM for TD prevention due to potential side effects and high resistance selection pressure (strong recommendation, low to very low level of evidence) (e20). However, no antibiotic is currently approved for this indication. The evidence for prebiotics and probiotics in TD prevention is poor; only Saccharomyces boulardii has shown convincing effects to date (risk reduction: 79%, [72; 87], p < 0.001) (e22).
The effectiveness of live attenuated oral cholera vaccines through cross-protection in non-cholera-related TD is low (off-label use, maximum effectiveness: 7%; indeed, according to one Cochrane review, there was no significant effect at all) (e23, e24). Therefore, these vaccines should be reserved primarily for travelers staying in cholera outbreak areas or cholera-endemic regions with the most basic hygienic conditions (cholera prevention rate of approximately 85–90%) (e25, e26).
TD is predominantly bacterial in nature (72–80%, of which 28–42% are caused by enterotoxigenic Escherichia coli, ETEC) and is self-limiting within 48 h in over 50% of travelers, but nevertheless causes changes to travel plans and activities in 12–46% of those affected (e18, e19, e27). Severity is classified into:
Mild (does not interfere with planned activities)
Moderate (distressing and interferes with planned activities)
Severe (heavily incapacitating, any form of bloody and/or febrile diarrhea) (e20).
Antibiotics should not be used in mild TD (strong recommendation, moderate level of evidence) (e20). Instead, loperamide or bismuth subsalicylate (not available in Germany) can be considered in adults (strong recommendation, moderate level of evidence) (e20). Antibiotic treatment may be performed for moderate TD (weak recommendation, moderate level of evidence), whereas it should be performed for severe TD (strong recommendation, high level of evidence) (e20). For empirical treatment, azithromycin is the preferred antibiotic, or rifaximin or rifamycin in the case of non-invasive pathogens. Fluoroquinolones can be considered with limitations (caution: high resistance rates in South/Southeast Asia) as a single dose or over 3 days (strong recommendation, high level of evidence) (e20).
This notwithstanding, a German consensus recommendation deems the enkephalinase inhibitor racecadotril to be the treatment of first choice—despite the lack of relevant studies on uncomplicated TD—since it does not affect the self-cleaning function of the intestine (in contrast to loperamide), can be used in all age groups, and has a lower interaction potential (e28). Activated charcoal (medicinal charcoal), although often found in first-aid kits, is not recommended by the ISTM or the German consensus paper due to a lack of efficacy studies.
Advice for risk groups
There are particular requirements on travel advice for the elderly, children, pregnant women, the chronically ill, long-term and adventure travelers (GCP), as well as migrants from malaria-endemic areas visiting friends and relatives (VFR). The latter group has a 2.82-fold increased risk of contracting malaria (95% CI [1.42; 5.92]) due to failure to take (sufficient) prophylaxis (e29).
According to §4 of the German Ordinance on Preventive Occupational Health Care (ArbMedVV) (e30), travelers are required to seek consultation with an occupational or tropical physician (German Social Accident Insurance [DGUV] principle G35) before or after occupational travel to countries with increased health risks. The employer bears the costs.
Questions on the article in issue 21/2021:
Medical Advice for Travelers
The submission deadline is 27 May 2022. Only one answer is possible per question. Please select the answer that is most appropriate.
Question 1
As a general rule, which individuals should be advised against traveling to malaria-endemic areas?
Pregnant women and women aged over 50 years
Men aged over 50 years and women aged under 20 years
Pregnant women and children aged under 5 years
Patients with chronic inflammatory bowel disease
Patients at risk of thrombosis
Question 2
What was the incidence of deep vein thrombosis in the LONFLIT3 randomized controlled trial with prophylactic heparinization versus no prophylaxis?
0% versus 4.8%
1% versus 5.8%
3% versus 7.5%
2% versus 10%
5% versus 7.2%
Question 3
What is the time to onset of immunity following yellow fever vaccination?
Immediate
5 Days
10 Days
3 Weeks
4 Weeks
Question 4
How many cases of malaria were imported to Germany annually between 2014 and 2019?
Approximately 50
Approximately 200
Approximately 500
Approximately 1000
Approximately 2000
Question 5
In the case of oral vaccination against which disease is it important, when administering the third dose, to ensure that an interval of at least 3 days is allowed prior to the start of malaria prophylaxis?
Polio
Chickenpox
Yellow fever
Typhoid fever
Hepatitis A and B
Question 6
Acute altitude sickness can cause nausea, headaches, and reduced performance. Life-threatening complications are possible. In this context, what does the abbreviation HACE stand for?
High-altitude coronary embolism
High-altitude coronary embolism
High-altitude chronic encephalitis
High-altitude crisis and endocarditis
High-altitude cerebral edema
Question 7
Which of the following analgesics are not recommended in Dengue fever due to a risk of complications?
Tilidine
Acetylsalicylic acid
Pethidine
Novaminsulfon
Tramadol
Question 8
What advice should be given regarding repellents for insect bite prevention?
Repellents with DEET (purchased in Germany) should be used
Repellents should preferably be purchased at the travel destination
Use of repellents should preferably be avoided
Repellents should not contain icaridin
Plant-based repellents are preferred
Question 9
Travelers’ diarrhea is a frequent problem during long-distance travel, particularly to South and Southeast Asia, as well as North, West, and Central Africa. When is the use of antibiotics recommended?
For prophylaxis as early as 2 days before the start of travel
For prophylaxis beginning on the day of arrival at the travel destination
For prophylaxis beginning 2 days after arrival at the travel destination
For the treatment of severe travelers’ diarrhea
Antibiotics are contraindicated in travelers’ diarrhea
Question 10
Which medication is recommended for both malaria prophylaxis and standby emergency treatment (SBET)?
Mefloquine
Artemether/lumefantrine
Doxycycline
Dihydroartemisinin–piperaquine
Atovaquone/proguanil
Acknowledgments
Translated from the original German by Christine Rye.
Footnotes
Conflict of interests
Dr. Wendt received reimbursement of congress fees and travel costs, as well as speaker’s honoraria from the Centrum für Reisemedizin.
Prof. Lübbert received reimbursement of travel cost and speaker’s honoraria from the Centrum für Reisemedizin.
The remaining authors declare that no conflict of interests exists.
References
- 1.Deutscher Reiseverband (DRV) (ed.) Der Deutsche Reisemarkt: Zahlen und Fakten 2019. www.drv.de/public/Downloads_2019/Archiv_Reisen_in_Zahlen/20-04-03_DRV_ZahlenFakten_2019.pdf (last accessed on 5 July 2020) [Google Scholar]
- 2.Wilder-Smith A, Boggild AK. Sentinel surveillance in travel medicine: 20 years of GeoSentinel publications (1999-2018) J Travel Med. 2018;25 tay139. doi: 10.1093/jtm/tay139. [DOI] [PubMed] [Google Scholar]
- 3.Angelo KM, Kozarsky PE, Ryan ET, Chen LH, Sotir MJ. What proportion of international travellers acquire a travel-related illness? A review of the literature. J Travel Med. 2017;24tax046 doi: 10.1093/jtm/tax046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schlagenhauf P, Weld L, Goorhuis A, et al. Travel-associated infection presenting in Europe (2008-12): an analysis of EuroTravNet longitudinal, surveillance data, and evaluation of the effect of the pre-travel consultation. Lancet Infect Dis. 2015;15:55–64. doi: 10.1016/S1473-3099(14)71000-X. [DOI] [PubMed] [Google Scholar]
- 5.Warne B, Weld LH, Cramer JP, et al. Travel-related infection in European travelers, EuroTravNet 2011. J Travel Med. 2014;21:248–254. doi: 10.1111/jtm.12120. [DOI] [PubMed] [Google Scholar]
- 6.Gautret P, Cramer JP, Field V, et al. Infectious diseases among travellers and migrants in Europe, EuroTravNet 2010. Euro Surveill. 2012;17 20205. [PubMed] [Google Scholar]
- 7.Mazolla R, Klinsing U, Lambertz U, Schmolz G, Wallacher B, Zabel P. Manual Reisemedizin praktisch: Reisemedizinische Sprechstunde Qualitätszirkel Reisemedizin. 2nd ed. Düsseldorf 2014. www.fachgesellschaft-reisemedizin.de/aktivitaeten/wissenschaftliche-arbeit/manual-reisemedizin-praktisch.html (last accessed on 18 February 2021) [Google Scholar]
- 8.Freedman DO, Chen LH, Kozarsky PE. Medical considerations before international travel. N Engl J Med. 2016;375:247–260. doi: 10.1056/NEJMra1508815. [DOI] [PubMed] [Google Scholar]
- 9.Aw B, Boraston S, Botten D, et al. Travel medicine: What’s involved? When to refer? Can Fam Physician. 2014;60:1091–1103. [PMC free article] [PubMed] [Google Scholar]
- 10.Centrum für Reisemedizin (CRM) Kostenerstattung von Reiseimpfungen durch Krankenversicherungen. www.crm.de/krankenkassen/kk_tabelle_kassen.htm (last accessed on 30 December 2020) [Google Scholar]
- 11.Tetzlaff K, Klingmann C, Muth CM, Piepho T, Welslau W. Gesellschaft für Tauch- und Überdruckmedizin (GTÜM) und Österreichische Gesellschaft für Tauch- und Hyperbarmedizin (ÖGTH) Gentner. Stuttgart: 2014. Checkliste Tauchtauglichkeit: Untersuchungsstandards und Empfehlungen der Gesellschaft für Tauch- und Überdruckmedizin (GTÜM) und der Österreichischen Gesellschaft für Tauch- und Hyperbarmedizin (ÖGTH). 2nd ed. [Google Scholar]
- 12.International Air Transport Association (IATA) Medical Manual: 12th Edition. www.iata.org/en/publications/medical-manual/ (last accessed on 30 December 2020) [Google Scholar]
- 13.Ahmedzai S, Balfour-Lynn IM, Bewick T, et al. Managing passengers with stable respiratory disease planning air travel: British Thoracic Society recommendations. Thorax. 2011;66(Suppl 1):i1–i30. doi: 10.1136/thoraxjnl-2011-200295. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention (CDC) University Press. Oxford Oxford: 2020. Travel by Air, Land & Sea. In: Brunette G, Nemhauser J (eds.): CDC Yellow Book 2020—Health information for international travel. [Google Scholar]
- 15.Statistika Wie ist Ihre Einstellung zum Thema Fliegen? GfK-Befragung 2008. https://de.statista.com/statistik/daten/studie/1265/umfrage/einstellung-zum-thema-fliegen/ (last accessed on 30 December 2020) [Google Scholar]
- 16.Oakes M, Bor R. The psychology of fear of flying (part II): a critical evaluation of current perspectives on approaches to treatment. Travel Med Infect Dis. 2010;8:339–363. doi: 10.1016/j.tmaid.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 17.Campos D, Bretón-López J, Botella C, et al. Efficacy of an internet-based exposure treatment for flying phobia (NO-FEAR Airlines) with and without therapist guidance: a randomized controlled trial. BMC Psychiatry. 2019;19 doi: 10.1186/s12888-019-2060-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McKinney KL, Wu HM, Tan KR, Gutman JR. Malaria in the pregnant traveler. J Travel Med. 2020;27 doi: 10.1093/jtm/taaa074. taaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schlagenhauf P, Haller S, Wagner N, Chappuis F. Malaria und Kinder, die reisen - Prophylaxe und Therapie. Ther Umsch. 2013;70:323–333. doi: 10.1024/0040-5930/a000411. [DOI] [PubMed] [Google Scholar]
- 20.Vouga M, Chiu Y-C, Pomar L, et al. Dengue, Zika and chikungunya during pregnancy: pre- and post-travel advice and clinical management. J Travel Med. 2019;26 doi: 10.1093/jtm/taz077. taz077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ständige Impfkommission. Empfehlungen der Ständigen Impfkommission beim Robert Koch-Institut - 2019/2020. www.rki.de/DE/Content/Infekt/Impfen/Impfkalender/Impfkalender_node.html (last accessed on 18 February 2021) [Google Scholar]
- 22.Rothe C, Rosenbusch D, Alberer M, et al. Vaccinations for international travel - clinical practice recommendations. Flugmedizin, Tropenmedizin, Reisemedizin. 2020;2:58–79. [Google Scholar]
- 23.Rothe C, Rosenbusch D, Alberer M, et al. Recommendations for antimalarial prophylaxis. Flugmedizin, Tropenmedizin, Reisemedizin. 2020;4:163–197. [Google Scholar]
- 24.Nieto Estrada VH, Molano Franco D, Medina RD, Gonzalez Garay AG, Martí-Carvajal AJ, Arevalo-Rodriguez I. Interventions for preventing high altitude illness: Part 1. Commonly-used classes of drugs. Cochrane Database Syst Rev. 2017 doi: 10.1002/14651858.CD009761.pub2. CD009761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gross M. Das gehört in die Reiseapotheke. MMW Fortschr Med. 2016;158:44–45. doi: 10.1007/s15006-016-8206-0. [DOI] [PubMed] [Google Scholar]
- 26.Bonetti N, Beer JH. Die Thrombose im Gepäck. Ther Umsch. 2016;73:573–581. doi: 10.1024/0040-5930/a000840. [DOI] [PubMed] [Google Scholar]
- 27.Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF) Prophylaxe der venösen Thromboembolie (VTE) https://www.awmf.org/uploads/tx_szleitlinien/003-001l_S3_VTE-Prophylaxe_2015-10-abgelaufen_01.pdf (last accessed on 30 December 2020) [Google Scholar]
- 28.Belcaro G, Cesarone MR, Nicolaides AN, et al. Prevention of venous thrombosis with elastic stockings during long-haul flights: the LONFLIT 5 JAP study. Clin Appl Thromb Hemost. 2003;9:197–201. doi: 10.1177/107602960300900303. [DOI] [PubMed] [Google Scholar]
- 29.Cesarone MR, Belcaro G, Nicolaides AN, et al. Venous thrombosis from air travel: the LONFLIT3 study: prevention with aspirin vs low-molecular-weight heparin (LMWH) in high-risk subjects: a randomized trial. Angiology. 2002;53:1–6. doi: 10.1177/000331970205300101. [DOI] [PubMed] [Google Scholar]
- 30.Chamnanchanunt S, Rojnuckarin P. Direct oral anticoagulants and travel-related venous thromboembolism. Open Med (Wars) 2018;13:575–582. doi: 10.1515/med-2018-0085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koch A, Cascorbi I, Westhofen M, Dafotakis M, Klapa S, Kuhtz-Buschbeck JP. The neurophysiology and treatment of motion sickness. Dtsch Arztebl Int. 2018;115:687–696. doi: 10.3238/arztebl.2018.0687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bundesministerium für Gesundheit (BMG) Online-Ratgeber Krankenversicherung: Versicherungsschutz im Ausland. www.bundesgesundheitsministerium.de/krankenversicherung-im-ausland.html (last accessed on 5 July 2020) [Google Scholar]
- 33.Kriemler S, Bürgi F, Wick C, et al. Prevalence of acute mountain sickness at 3500 m within and between families: a prospective cohort study. High Alt Med Biol. 2014;15:28–38. doi: 10.1089/ham.2013.1073. [DOI] [PubMed] [Google Scholar]
- 34.Luks AM, Swenson ER, Bärtsch P. Acute high-altitude sickness. Eur Respir Rev. 2017;26 doi: 10.1183/16000617.0096-2016. 160096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cingi C, Emre IE, Muluk NB. Jetlag related sleep problems and their management: a review. Travel Med Infect Dis. 2018;24:59–64. doi: 10.1016/j.tmaid.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 36.Bin YS, Postnova S, Cistulli PA. What works for jetlag? A systematic review of non-pharmacological interventions. Sleep Med Rev. 2019;43:47–59. doi: 10.1016/j.smrv.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 37.Herxheimer A, Petrie KJ. Melatonin for the prevention and treatment of jet lag. Cochrane Database Syst Rev. 2002;30 doi: 10.1002/14651858.CD001520. CD001520. [DOI] [PubMed] [Google Scholar]
- 38.Tordjman S, Chokron S, Delorme R, et al. Melatonin: pharmacology, functions and therapeutic benefits. Curr Neuropharmacol. 2017;15:434–443. doi: 10.2174/1570159X14666161228122115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pavicic T, Steckmeier S, Kerscher M, Korting HC. Evidenz-basierte Kosmetika: Konzept und Anwendung bei den Zielstellungen lichtgeschädigter Altershaut und Xerosis. Wien Klin Wochenschr. 2009;121:431–439. doi: 10.1007/s00508-009-1204-9. [DOI] [PubMed] [Google Scholar]
- 40.Yeager DG, Lim HW. What‘s New in Photoprotection: a review of new concepts and controversies. Dermatol Clin. 2019;37:149–157. doi: 10.1016/j.det.2018.11.003. [DOI] [PubMed] [Google Scholar]
- E1.Edalat A, Roth D. Gesund und fit über den Wolken: Pharmazeutische Beratung von Flugreisenden. Deutsche Apothekerzeitung (DAZ) 2015;24 [Google Scholar]
- E2.Robert Koch-Institut. Infektionsepidemiologische Jahrbuch meldepflichtiger Krankheiten für 2019. Robert Koch-Institut 2019. www.rki.de/DE/Content/Infekt/Jahrbuch/Jahrbuch_2019.html (last accessed on 22 April 2021) [Google Scholar]
- E3.Robert Koch-Institut. Infektionsepidemiologische Jahrbuch meldepflichtiger Krankheiten für 2019. Robert Koch-Institut 2020. www.rki.de/DE/Content/Infekt/Jahrbuch/Jahrbuecher/2019.html (last accessed on 18 February 2021) [Google Scholar]
- E4.Kotepui M, Kotepui KU, Milanez GDJ, Masangkay FR. Prevalence of and risk factors for severe malaria caused by Plasmodium and dengue virus co-infection: a systematic review and meta-analysis. Infect Dis Poverty. 2020;134 doi: 10.1186/s40249-020-00741-z. doi: 10.1186/s40249-020-00741-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E5.Kotepui M, Kotepui KU, Milanez GD, Masangkay FR. Prevalence of severe Plasmodium knowlesi infection and risk factors related to severe complications compared with non-severe P knowlesi and severe P. falciparum malaria: a systematic review and meta-analysis. Infect Dis Poverty. 2020;106 doi: 10.1186/s40249-020-00727-x. doi: 10.1186/s40249-020-00727-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E6.Diouf I, Rodriguez Fonseca B, Caminade C, et al. Climate variability and malaria over West Africa. Am J Trop Med Hyg. 2020;102:1037–1047. doi: 10.4269/ajtmh.19-0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E7.Singh Parihar R, Bal PK, Kumar V, et al. Numerical modeling of the dynamics of malaria transmission in a highly endemic region of India. Sci Rep. 2019;9 doi: 10.1038/s41598-019-47212-6. 11903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E8.Rossati A, Bargiacchi O, Kroumova V, Zaramella M, Caputo A, Garavelli PL. Climate, environment and transmission of malaria. Infez Med. 2016;24:93–104. [PubMed] [Google Scholar]
- E9.Ahluwalia J, Brooks SK, Weinman J, Rubin GJ. A systematic review of factors affecting adherence to malaria chemoprophylaxis amongst travellers from non-endemic countries. Malar J. 2020;19 doi 10.1186/s12936-020-3104-4. doi: 10.1186/s12936-020-3104-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E10.Nakato H, Vivancos R, Hunter PR. A systematic review and meta-analysis of the effectiveness and safety of atovaquone proguanil (Malarone) for chemoprophylaxis against malaria. J Antimicrob Chemother. 2007;60:929–936. doi: 10.1093/jac/dkm337. [DOI] [PubMed] [Google Scholar]
- E11.Bundesamt für Gesundheit (BAG), Expertenkomitee für Reisemedizin (EKRM) Malariaschutz für Kurzzeitaufenthalter: Richtlinien und Empfehlungen. 2016-OEG-04. www.bag.admin.ch/dam/bag/de/dokumente/mt/i-und-b/richtlinien-empfehlungen/empfehlungen-risikogruppen-risikosituationen/malariaschutz-kurzzeitaufenthalter-bis-3-monate.pdf.download.pdf/malaria-2016-kurzzeit.pdf (last accessed on 2 January 2021) [Google Scholar]
- E12.World Health Organization (WHO) Malaria. https://www.who.int/news-room/fact-sheets/detail/malaria (last accessed on 2 January 2021) [Google Scholar]
- E13.Tan R, Elmers J, Genton B. Malaria standby emergency treatment (SBET) for travellers visiting malaria endemic areas: a systematic review and meta-analysis. J Travel Med. 2019;26 doi: 10.1093/jtm/taz027. taz027. [DOI] [PubMed] [Google Scholar]
- E14.Wendt S, Paquet D, Schneider A, Trawinski H, Lübbert C. Durch Mücken übertragbare Erkrankungen. CME. 2020;17:51–70. [Google Scholar]
- E15.Alpern JD, Dunlop SJ, Dolan BJ, Stauffer WM, Boulware DR. Personal protection measures against mosquitoes, ticks, and other arthropods. Med Clin North Am. 2016;100:303–316. doi: 10.1016/j.mcna.2015.08.019. [DOI] [PubMed] [Google Scholar]
- E16.Centers for Disease Control and Prevention (CDC) University Press. Oxford Oxford: 2020. Mosquitoes, Ticks & Other Arthropods. In: Brunette G, Nemhauser J (eds.): CDC Yellow Book 2020—Health information for international travel. [Google Scholar]
- E17.Pitzurra R, Steffen R, Tschopp A, Mutsch M. Diarrhoea in a large prospective cohort of European travellers to resource-limited destinations. BMC Infect Dis. 2010;231 doi: 10.1186/1471-2334-10-231. doi: 10.1186/1471-2334-10-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E18.Steffen R. Epidemiology of travellers‘ diarrhea. J Travel Med. 2017;24:S2–S5. doi: 10.1093/jtm/taw072. [DOI] [PubMed] [Google Scholar]
- E19.Steffen R, Hill DR, DuPont HL. Traveler‘s diarrhea: a clinical review. JAMA. 2015;313:71–80. doi: 10.1001/jama.2014.17006. [DOI] [PubMed] [Google Scholar]
- E20.Riddle MS, Connor BA, Beeching NJ, et al. Guidelines for the prevention and treatment of travelers‘ diarrhea: a graded expert panel report. J Travel Med. 2017;24:S57–S74. doi: 10.1093/jtm/tax026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E21.Ng QX, Ho CYX, Shin D, Venkatanarayanan N, Chan HW. A meta-analysis of the use of rifaximin to prevent travellers‘ diarrhoea. J Travel Med. 2017;24 doi: 10.1093/jtm/tax025. doi: 10.1093/jtm/tax025. [DOI] [PubMed] [Google Scholar]
- E22.McFarland LV, Goh S. Are probiotics and prebiotics effective in the prevention of travellers‘ diarrhea: a systematic review and meta-analysis. Travel Med Infect Dis. 2019;27:11–19. doi: 10.1016/j.tmaid.2018.09.007. [DOI] [PubMed] [Google Scholar]
- E23.Hill DR, Ford L, Lalloo DG. Oral cholera vaccines: use in clinical practice. Lancet Infect Dis. 2006;6:361–373. doi: 10.1016/S1473-3099(06)70494-7. [DOI] [PubMed] [Google Scholar]
- E24.Ahmed T, Bhuiyan TR, Zaman K, Sinclair D, Qadri F. Vaccines for preventing enterotoxigenic Escherichia coli (ETEC) diarrhoea. Cochrane Database Syst Rev. 2013 doi: 10.1002/14651858.CD009029.pub2. CD009029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E25.Jelinek T, Kollaritsch H. Vaccination with Dukoral against travelers‘ diarrhea (ETEC) and cholera. Expert Rev Vaccines. 2008;7:561–567. doi: 10.1586/14760584.7.5.561. [DOI] [PubMed] [Google Scholar]
- E26.Chen WH, Cohen MB, Kirkpatrick BD, et al. Single-dose live oral cholera vaccine CVD 103-HgR protects against human experimental infection with vibrio cholerae O1 El Tor. Clin Infect Dis. 2016;62:1329–1335. doi: 10.1093/cid/ciw145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E27.Jiang ZD, DuPont HL. Etiology of travellers’ diarrhea. J Travel Med. 2017;24:S13–S16. doi: 10.1093/jtm/tax003. [DOI] [PubMed] [Google Scholar]
- E28.Jelinek T, Nothdurft H-D, Haditsch M, Weinke T. Konsensuspapier Therapie der akuten Reisediarrhö Eine Praxisempfehlung für die Reiseberatung. MMW Fortschr Med. 2017;159:4–11. doi: 10.1007/s15006-017-9293-2. [DOI] [PubMed] [Google Scholar]
- E29.Marasinghe DH, Cheaveau J, Meatherall B, et al. Risk of malaria associated with travel to malaria-endemic areas to visit friends and relatives: a population-based case-control study. CMAJ Open. 2020;8:E60–E68. doi: 10.9778/cmajo.20190070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E30.Deutsche Gesetzliche Unfallversicherung (DGUV) Handlungsanleitung für die arbeitsmedizinische Vorsorge. https://dtg.org/images/Fortbildung/Zertifikate/Arbeitsaufenthalt/Handlungsanleitung_G_35_GUV-I_504-35_1_.pdf (last accessed on 5 October 2020) [Google Scholar]