ABSTRACT
Objective:
Describe the medium-term safety of the tension free vaginal tape obturator (TVT-O) procedure in terms of complications, cure and changes in quality of life (QoL) after the surgery.
Materials and methods:
Descriptive historical cohort that included women over 18 years of age who underwent TVT-O due to objectively proven stress urinary incontinence, urethral hypermobility or mixed urinary incontinence in which the stress component predominated, confirmed on urodynamic testing between July 2013-April 2017, in a reference hospital located in the city of Murcia Spain. Women with previous anti-incontinence surgery, concomitant vaginal surgery and planning pregnancy were excluded. Follow-up was determined for each patient based on the time elapsed between surgery and the time when the research protocol was applied. Complications were stratified according to the modified Clavien-Dindo classification; also we evaluated subjective cure rate, quality of life using the ICIQ-SF score, before and after surgery.
Results:
The mean age was 52.6 (SD± 10.5) years and 80.1% of patients were at least overweight. The incidence of complications at 12 months was: 8.3% (12/144). We did not detect complications after this period in the followed patients at 24, 36 and 48 months. The subjective cure determined at 12, 24, 36 and 48 months was 62.5% (90/144), 59.09% (55/88), 50.81% (31/61) and 50% (7/14), respectively. There was a significant improvement in quality of life, as determined by the ICQ-SF mean score before and after surgery (13.76[6,34] vs 3.84[5.76]; p<0.05).
Conclusions:
The TVT-O surgery is a safe therapy associated with a low complication incidence at 12 months, an acceptable subjective cure rate in stress urinary incontinence, and quality-of-life improvement. Classifications of complications related to the insertion of the prosthesis and of those inherent to surgery, such as urinary tract infection, are required.
Keywords: Urinary incontinence, stress urinary incontinence, quality of life, suburethral sling
RESUMEN
Objetivo:
Describir la seguridad a mediano plazo del procedimiento con el cabestrillo suburetral transobturador dentro-fuera (en inglés: tension free vaginal tape obturator TVT-O) en términos de: complicaciones, cura y cambios en la calidad de vida después de la cirugía.
Materiales y métodos:
Cohorte histórica descriptiva que incluye mujeres mayores de 18 años intervenidas de TVT-O por incontinencia urinaria de esfuerzo (IUE) objetivamente comprobada, hipermovilidad uretral o incontinencia urinaria mixta en la que predominó el componente de esfuerzo, confirmada en prueba urodinámica entre julio del 2013 y abril del 2017 en un hospital de referencia ubicado en la ciudad de Murcia, España. Se excluyeron mujeres con cirugía previa de incontinencia, cirugía vaginal concomitante y planificación del embarazo. El seguimiento se determinó para cada paciente por el tiempo transcurrido desde la cirugía hasta el momento en que se aplicó el protocolo de investigación. Las complicaciones se estratificaron según la clasificación de Dindo-Clavien modificada, además, se evaluaron la tasa de curación subjetiva y la calidad de vida mediante el International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF) antes y después de la cirugía.
Resultados:
La edad media de las pacientes fue de 52,59 (DE±10,46) años, el 80,1 % tenía al menos sobrepeso. La incidencia de complicaciones en los primeros 12 meses fue del 8,3%. No detectamos complicaciones después de este periodo en las pacientes seguidas a 24, 36 y 48 meses. La curación subjetiva determinada a los 12, 24, 36 y 48 meses fue del 62,5% (90/144), 59,09% (55/88), 50,81% (31/61) y 50% (7/14), respectivamente. Hubo una mejoría significativa en la calidad de vida, en términos de puntuación media ICQ-SF antes y después de la cirugía (13,76 [6,34] vs 3,84 [5,76]; p < 0,05).
Conclusiones:
El TVT-O es una terapia segura, con baja tasa de complicaciones a los 12 meses, aceptable tasa de curación subjetiva de la IUE y una mejora en la calidad de vida. Se necesitan clasificaciones de complicaciones relacionadas con la inserción de la prótesis y que incluyan complicaciones inherentes a la cirugía, como la infección del tracto urinario.
Palabras clave: incontinencia urinaria, incontinencia urinaria de esfuerzo, calidad de vida, cabestrillo suburetral
INTRODUCTION
The International Continence Society defines urinary incontinence (UI) as any involuntary leakage of urine 1. There are two main subtypes of urinary incontinence: stress incontinence and urgency incontinence 2. Stress urinary incontinence (SUI) is the complaint of involuntary loss of urine on effort or physical exertion including sporting activities, or on sneezing or coughing 1.
For the most inclusive definitions of urinary incontinence ('ever' 'any' or 'at least once in the past 12 months'), Milson et al. describe prevalences ranging between 5% and 69%. However, a prevalence of 25% to 45% has been reported by most studies. In addition, prevalence increases with age, being as high as 40% in women over 70 years of age. 3. The human and financial burden of urinary incontinence is high 4 and is associated with significant worsening of quality of life (QoL) 5.
Symptoms of incontinence and/or its impact on QoL can be assessed in a number of ways. Questionnaires completed by patients themselves and which have been shown to be valid and reliable are recommended 6. The International Consultation on Incontinence Questionnaire Short-Form (ICIQ-SF) developed in 2004, is a simple clinical instrument for assessing symptoms, prevalence, perceived cause of UI, and its impact on QoL. It can also be used to evaluate outcomes in clinical research as well as in routine clinical practice 7. The questionnaire consists of three items that assess the severity of incontinence plus one item intended as a guide to the causes of the urinary incontinence. The higher the score, the higher impairment 8. This was the first short questionnaire for the diagnosis of UI validated in Spain. The psychometric properties of the ICIQ-SF questionnaire have been studied and shown to be satisfactory, allowing it to be recommended in routine clinical practice for the initial diagnosis of UI. Its brevity and simple scoring and interpretation characteristics render it useful for UI detection in any healthcare setting, as well as in epidemiological studies 9. The International Consultation on Incontinence committee validated the use of this questionnaire, with a grade A recommendation 6.
Pelvic floor muscle training is widely recommended as first-line conservative management for the treatment of SUI in women 10. However, evidence shows that long-term adherence is poor and half of the patients progress to surgery 11. For patients requiring surgery, the American Urological Association supports five procedures: the use of injectable fillers, laparoscopic suspensions (laparoscopic Burch colpo-suspension), mid-urethral slings, pubovaginal slings, and open retropubic suspensions 12. Mid-urethral sling (MUS) procedures, such as tension- free vaginal tape (TVT) and inside-out transobturator tape, also called tension free vaginal tape obturator (TVT-O), are the most common approaches to the surgical treatment of SUI with urethral hypermobility 13. MUS has been the most widely investigated surgical treatment shown to have a good safety profile for SUI in women. Regardless of the route of insertion, slings are highly effective in the short and medium term. They also have a positive impact on QoL improvement and subjective cure rates of 62-98%, with the use of the transobturator route in women with SUI 13. In terms of effectiveness, obesity and older age have been associated with lower cure rates of MUS surgery at 1 and 5 years 14,15. In fact, there is no agreement in the European Guidelines of UI regarding the outcome of incontinence surgery in obese women 16.
Regarding complications, moderate quality evidence shows low overall reported rates of tape related complications, such as erosion of the tape into the vagina, at about 2% for both routes of tape insertion. Risks associated with surgical correction include hemorrhage, pain, infection, de novo urgency, urinary retention, and treatment failure 17. With the exception of groin pain, fewer adverse events occur when the transobturator approach is used. When medial-to-lateral versus lateral-to-medial insertion transobturator techniques are compared, there is no evidence to support the use of one approach over the other 13. However, reporting of longer-term results data in clinical trials is required 18,19.
With the aim of providing information on medium term results, the objective of this study is to describe safety outcomes between 1 and 4 years after the TVT-O procedure in terms of complications, cure and changes in quality of life after surgery.
MATERIALS AND METHODS
Design, and population: A descriptive historical cohort study. We included women over 18 years of age who underwent TVT-O surgery due to objectively proven SUI, urethral hypermobility or mixed urinary incontinence in which the stress component predominated, confirmed on urodynamic test, between July 2013 and April 2017, at the Reina Sofia General University Hospital in Murcia, Spain, a general public health institution affiliated to the College of Murcia, located in the reference health area VII of the Region (Murcia / East), that serves a population of 200,892 users. We excluded women with previous anti-incontinence surgery, concomitant vaginal surgery, urethral surgery, pelvic irradiation, and planning pregnancy. Non-probabilistic consecutive sampling was used. All patients that underwent TVT-O surgery and fulfilled the inclusion and exclusion criteria were part of the sample size.
Procedure: During September 2019, we reviewed all medical and surgical records of patients operated consecutively for TVT-O surgery from July 2013 to April 2017, available in the hospital's surgical statistics database. In order to reduce missing data bias, we used inclusive keywords like urinary incontinence, TVT-O, TVT, colposuspension, midurethral sling. The surgeries were performed by two experienced urogynecologists using the medial-to-lateral transobturator approach, once the informed consent for surgery had been understood and signed.
The diagnosis of SUI was made in our Institution based on medical history, physical examination with the patient lying or standing to demonstrate urine leakage, the Marshall-Bonney test, the Q tip test to evaluate urethral hypermobility, abdominal, perineal and digital examination of the vagina and rectum, along with assessment of any associated pelvic organ prolapse (POP). Urodynamic testing was performed in cases with storage symptoms and suspected of having mixed urinary incontinence.
Using the "Selene" software, the principal investigators recorded baseline demographic data, detrusor overactivity (DO), ICIQ-SF before and after surgery, and perioperative complications. This system is encrypted and protected from outsiders. The descriptive data were collected and anonymity was ensured by patient data encoding to confidential numbers in a rising pattern that were entered in an electronic worksheet. Perioperative complications were documented and classified by urology residents (investigators) based on the modified Clavien- Dindo grading system 18 as next described. Grade I: any deviation from the normal postoperative course without the need for pharmacological treatment or surgical, endoscopic, and radiological interventions; Grade II: requiring pharmacological treatment with drugs other than such allowed for grade I complications; Grade III: requiring surgical, endoscopic or radiological intervention; Grade IIIa: intervention not under general anesthesia; Grade IIIb: intervention under general anesthesia; Grade IV: life-threatening complication requiring intermediate/intensive care unit management; Grade IVa: single organ dysfunction (including dialysis); Grade IVb: multiorgan dysfunction; Grade V: death. Complications were also classified according to the Classification of Complications Related Directly to the Insertion of Prostheses (Meshes, Implants, Tapes) or Grafts in Female Pelvic Floor Surgery by the International Urogynecological Association (IU/International Continence Society (ICS) 19. This is a category, time, and site (CTS) classification that includes the following categories: 1. Vaginal complication-no epithelial separation: prominence (e.g., due to wrinkling or folding) or contraction (shrinkage); 2. Vaginal complication - (smaller) exposure: A smaller (1 cm or less) degree of vaginal epithelial separation is involved; 3. Vaginal complication- (larger) exposure or extrusion: A larger degree (> 1 cm) of vaginal epithelial separation or prosthesis or graft extrusion is involved; 4. Urinary tract compromise or perforation; 5. Rectal or Bowel compromise or perforation; 6. Skin and/or musculoskeletal complications; 7. Patient hematoma or systemic compromise. These categories are further subclassified into A: Asymptomatic, B: Symptomatic, C: infection, D: Abscess. Site: S0: Systemic complications (no specific site); S1: Vaginal: area of suture line; S2: Vaginal: away from the vaginal suture line; S3: Trocar passage; S4: Other skin or musculoskeletal site; S5: Intra-abdominal. Time T1: Intraoperative - 48 hr; T2: 48 hr - 2 months; T3: 2-12 months; T4: Over 12 months. The data were entered into the electronic worksheet once the patients were classified.
Eligible patients were then contacted by telephone and an appointment was scheduled in the outpatient clinic during the months of September 2019 to November 2019, to ask women if they had experienced 'urine loss or leak when they coughed, laughed, sneezed, lifted, exercised, etc.' in the previous 7 days. Women were also asked to review and complete a postoperative validated and translated Spanish version of the ICIQ-SF, available in pdf on the website of the Spanish Association of Urology, in order to evaluate subjective cure and QoL. We sought to reduce the risk of information bias through the application of the ICIQ-SF and the Marshall-Bonney tests during follow-up. Subjective cure was measured by questionnaire and was defined by an ICIQ-SF score = 0.
Follow-up was determined for each patient based on the time elapsed since the surgery until the time of the appointment, when they also filled out the ICIQ-SF.
Measured variables: Baseline demographic data, age, weight, height, and BMI (kg/m2). Clinical data at the time of surgery such as pelvic organ prolapse, incontinence severity and detrusor overactivity (DO) were recorded. Complications were defined according to the modified Clavien-Dindo classification and the Classification of Complications Related Directly to the Insertion of Prostheses (Meshes, Implants, Tapes) or Grafts in Female Pelvic Floor Surgery by the International Urogynecological Association (IUGA)/ International Continence Society (ICS). We evaluated subjective cure rate and Qol using the ICIQ-SF score before and after surgery. The terms used in this study follow the standardized terminology for female pelvic floor disorders of the IUGA/ICS joint report 2.
Statistical analysis: Descriptive statistics of the clinical and demographic variables of patients are shown using raw data. Mean and standard deviation (SD) or median and rank were calculated for continuous data, according to normal or not normal distribution, using the Kolgomorov-Smirnov test. We described the incidence of complications, failure and quality of life on different follow-up months 12,24,36 and 48. Discrete variables were summarized as proportions. Continuous variables were analyzed using the paired Student test. All analyses were performed using the Statistical Package for the Social Sciences (SPSS) software version 20.0 for Windows (SPSS Inc., Chicago, IL, USA). A p value of <0.05 was selected to indicate statistical significance.
Ethical issues: The Hospital Institutional Research Board approved the study protocol on June 30, 2020. Confidentiality of patient's identity was assured.
RESULTS:
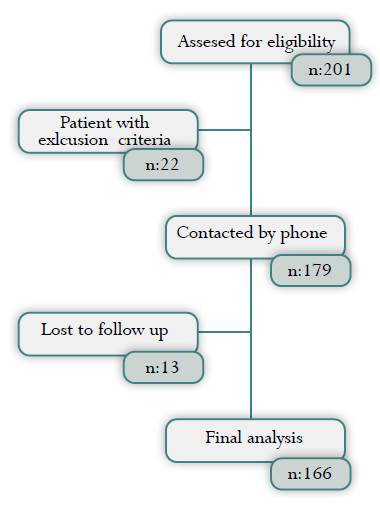
A total of 201 consecutive patients underwent TVT-O surgery, 22 women had exclusion criteria (5 had previous anti-incontinence surgery, 17 had concomitant vaginal surgery), and 13 of 179 patients (7%) were lost to follow-up (9 did not attend the consultation appointment, 4 did not complete the ICIQ-SF), resulting in 166 (82%) individuals included in the analysis (Fig 1). Of all patients in our historical cohort, n: 144, 88, 61 and 14 were seen at 12, 24, 36 and 48 months, respectively.
Figure 1. Flow diagram for the patients analyzed in this study.
At the time of surgery, mean age was 52.59 years (SD ± 10.46), mean BMI 29.65 kg/m2 (SD ± 5.25), 133 (80.1%) had a BMI ≥ 25 kg/m2. They had a median of 3 (IQR ± 2) previous pregnancies and a median of 2 (IQR ± 1) vaginal deliveries. Eighty-four (50%) patients underwent urodynamic testing before surgery for stress-predominant mixed incontinence, and 30 (18,07%) were found to have Detrusor overactivity (DO) (Table 1).
Table 1. Sociodemographic characteristics of women underwent TVT-O surgery in the General University Hospital Reina Sofia of Murcia, Spain 2013- 2017 (n= 166).
| Characteristics | n (%) |
|---|---|
| Age* | 52.59 (±10.46) |
| BMI (kg/m2)* | 29.65 (±5.25) |
| BMI | |
| Normal weight (18,5-24,9 kg/m2) ** | 33 (19.9%) |
| Overweight (25,0 - 29,9 kg/m2) ** | 56 (33.7%) |
| Obesity (≥ 30 kg/m2) ** | 77 (46.4%) |
| Presence of DO ** | 39 (18.07%) |
BMI= body mass index; DO= detrusor overactivity
* Mean and SD= standard deviation
** Absolute number ( Proportions %)
The complications incidence during the first 12 months, was 8.33% (12/144); no complications have been recorded to date after that point. Our findings, according to the Clavien-Dindo classification, were: 9 (5.42%) Clavien I; 7 had pain, with 6 cases of groin pain (3.62) and 1 (0.6%) spinal headache; 1 (0.6%) urinary tract infection (UTI) and 1 (0.6%) bleeding. Another 3 were Clavien IIIa, including 1 (0.6%) sling extrusion (SE), 1 (0.6%) bladder outlet obstruction (BOO), and 1 (0.6%) bladder perforation, all of which required surgical intervention. According to the IUGA-ICS classification of mesh, tape, and graft surgery complications, groin pain was the most frequent complication (3.62%) (Table 3).
Table 3. Type of complications according IUGA/ICS classification in women underwent to TVT-O surgery in the General University Hospital Reina Sofia of Murcia, Spain 2013- 2017. (n=166).
| Complication* | n (%) | Category | Time | Site |
|---|---|---|---|---|
| Pain | 6 (3.62) | 1B | T2 | S3 |
| Bleeding | 1 (0.60) | 7A | T1 | S5 |
| SE | 1 (0.60) | 3B | T2 | S1 |
| BP | 1 (0.60) | 4A | T1 | S3 |
| BOO | 1 (0.60) | 4B | T2 | S1 |
SE= sling extrusion; BP= bladder perforation; BOO= bladder outlet obstruction.
* Urinary tract infection and has not been included into the classification.
Table 2. Type of complications according to modified Clavien-Dindo classification in women underwent to TVT-O surgery in the General University Hospital Reina Sofia of Murcia, Spain 2013- 2017. (n=166).
| n (%) | ||
|---|---|---|
| Complications | 12 (7.22) | |
| Clavien-Dindo | ||
| I | Pain | 7 (4.22) |
| UTI | 1 (0.60) | |
| Bleeding | 1 (0.60) | |
| IIIa | SE | 1 (0.60) |
| BP | 1 (0.60) | |
| BOO | 1 (0.60) | |
UTI= urinary tract infection; SE= sling extrusion; BP = bladder perforation; BOO= bladder outlet obstruction.
Table 4. Quality of Life using the ICIQ-SF score in women underwent to TVT-O surgery in the General University Hospital Reina Sofia of Murcia, Spain 2013- 2017. (n=166).
| ICIQ-SF score | ||||
|---|---|---|---|---|
| n | Mean (SD) | p value | ||
| Overall preoperative | 13.76 (6.34) | 0.01 | ||
| Overall postoperative | 3.84 (5.76) | |||
| DO | Preoperative | 30 | 16.67 (5.48) | 0.03 |
| Postoperative | 30 | 6.87 (7.28) | ||
ICIQ-SF - the short form of International Consultation on Incontinence Questionnaire; SD- standard deviation; DO= detrusor overactivity
Cure rate and QoL: The subjective cure rate (ICIQ-SF score = 0) determined at 12, 24, 36 and 48 months was 62.5% (90/144), 59.09% (55/88), 50.81% (31/61) and 50% (7/14), respectively. Regarding QoL, the ICIQ-SF score at the time of surgery was 13.76 (SD ± 6.34). ICIQ-SF mean scores found after surgery were 3.73 (SD ± 5.58) at 12 months, 3.94 (SD ± 5.61) at 24 months, 4.87(SD ± 6.04) at 36 months and 3.84 (SD ± 4.27) at 48 months. There were significant differences between ICIQ-SF scores before and after surgery (13.76 [SD ± 6.34] vs 3.84 [SD ± 5.76]; p<0.05).
DISCUSSION
The incidence of complications during the first 12 months was: 8.3% (12/144). The subjective cure rate of SUI with inside-out TVT-O varied from 62.5% at 12 months to 50% at 48 months, while there was a significant clinical improvement in QoL from a preoperative mean score of 13.76 to 3.84 at 48 months.
Postoperative complication rates of 27% have been reported in TVT-O surgery 20,21, higher than our results. However, complication rates similar to ours have been shown in Latin America 22. We found a lower rate of early UTI (0.6%) than reported in the literature (1-2.9%) after TVT-O surgery 21-23. It is important to emphasize that the IUGA/ICS classification of Complications Related Directly to the Insertion of Prostheses or Grafts in Female Pelvic Floor Surgery does not include urinary tract infection 24, which is an important procedure-related complication.
In a prospective single center randomized trial conducted in Spain using the ICIQ-SF and the Sandvik Severity Index (SSI), the subjective cure rate reported at 12 months was 70.1% for the transobturator approach 23. Likewise, a recent systematic review (SR) showed subjective cure rates ranging from 62% to 98% at 12 months 13, similar to our subjective cure rate (62.5%) at the same time postoperative time point. The medium-term (1-5 years) subjective cure rates range from 82% to 91% 13. Subjective cure rates of SUI after TVT-O of 94% and 81% at 36 and 48 months, respectively, have been described (21,25), in contrast with the results obtained in our study, in which we found a subjective cure rate of 50.8% and 50% at 36 and 48 months, respectively.
Regarding QoL, ICIQ-SF mean scores of 0.91-2.3 have been described 12 months after sling placement using the transobturator approach, with a drop of 6.61-12.2 points in the postoperative score. This reflects a subjective improvement in QoL 23,26. We found ICIQ-SF mean scores of 3.73 (SD ± 5.58) at 12 months, with a difference of 10.03 points before and after surgery, translating into a subjective improvement in QoL and patient satisfaction. An ICIQ-SF mean score of 4 has been described at 36 months of follow-up in patients taken to TVT-O surgery 21, similar to the result obtained in our study 4.87 (SD ± 6.04) at the same time point. We found a significant improvement of 9.92 points in the ICIQ-SF at 48 months after TVT-O surgery, slightly higher than previously described. It should be noted that the ICIQ-SF is a restrictive tool in terms of cure rate, because the remaining 37.3% (ICIQ-SF≥ 1) that not achieved cure, showed a significant improvement in QoL.
Points of strength of this study are (i) a homogeneous study population with the exclusion of women with other associated surgical procedures (ii); the subjective outcomes obtained by the use of validated questionnaire before and after surgery. Conversely, we acknowledge that a limitation of this study could be the historical cohort design plus the fact that we did not consider the objective cure rate, the maximum urethral closure pressure, or the assessment of voiding or storage symptom after surgery. In addition to this, we had an important lost of follow up at 24, 36, and 48 months. Besides, the presence of DO could be a confounding factor, since we included patients with mixed urinary incontinence in which the stress component predominated; this might represent a limitation and makes it difficult to generalize the results. Consequently, long-term controlled randomized prospective studies are required.
CONCLUSIONS
TVT-O surgery represents a safe therapy at 12 months, with a low complication rate and an acceptable subjective cure rate in SUI. The overall patient satisfaction and objective outcomes should be standardized and reassessed at each postoperative visit. QoL questionnaires are essential components of incontinence research. Further investigations to compare different subjective cure evaluations after mesh surgery will be of interest. Classifications of complications related to prosthesis insertion and those inherent to surgery such as urinary tract infection are required.
ACKNOWLEDGMENTS
Members of the urology department of the Reina Sofia General University Hospital of Murcia, for allowing the surgery and making this research possible.
FUNDING:
None.
AUTHOR'S CONTRIBUTIONS:
Florencio Manuel Marín-Martínez: Had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design, acquisition of data, data analysis and interpretation, drafting of the manuscript, critical review of the manuscript for important intellectual content, statistical analysis. Julián Oñate-Celdrán: Study concept and design, data acquisition, data analysis and interpretation, critical review of the manuscript for important intellectual content.
Olimpia Molina-Hernández: Study concept and design, data acquisition, data analysis and interpretation, critical review of the manuscript for important intellectual content.
Miriam Artes-Artes: Study concept and design, data acquisition, data analysis and interpretation, critical review of the manuscript for important intellectual content.
Emny Rochelle Bobadilla-Romero: Study concept and design, data acquisition, data analysis and interpretation, critical review of the manuscript for important intellectual content.
Víctor Javier García-Porcel: Study concept and design, data acquisition, data analysis and interpretation, critical review of the manuscript for important intellectual content.
Pablo Luis Guzmán-Martínez: Study concept and design, data acquisition, data analysis and interpretation, critical review of the manuscript for important intellectual content.
Angel Andreu-García: Study concept and design, data acquisition, data analysis and interpretation, critical review of the manuscript for important intellectual content.
Carlos Sánchez-Rodríguez: Study concept and design, data acquisition, data analysis and interpretation, critical review of the manuscript for important intellectual content.
Damián García-Escudero: Study concept and design, data acquisition, data analysis and interpretation, critical review of the manuscript for important intellectual content.
Mabel Coromoto Suarez-Pineda: Study concept and design, data acquisition, data analysis and interpretation, critical review of the manuscript for important intellectual content.
Pedro Valdelvira-Nadal: Study concept and design, data acquisition, data analysis and interpretation, critical review of the manuscript for important intellectual content.
REFERENCES
- 1.D’Ancona C, Haylen B, Oelke M, Abranches-Monteiro L, Arnold E, Goldman H, et al. The International Continence Society (ICS) report on the terminology for adult male lower urinary tract and pelvic floor symptoms and dysfunction. Neurourol Urodyn. 2019;38(2):433–477. doi: 10.1002/nau.23897. [DOI] [PubMed] [Google Scholar]
- 2.Haylen BT, De Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26. doi: 10.1007/s00192-009-0976-9. [DOI] [PubMed] [Google Scholar]
- 3.Milsom I, Altman D, Cartwright R, Lapitan MC, Nelson R, Sjostrom S, et al. Abrams P, Cardozo L, Wagg A, Wein A. Incontinence 6th International Consultation on Incontinence. 6. Tokyo: Tokyo: International Continence Society; Sep, 2017. Incontinence; pp. 1–142.https://www.ics.org/publications/ici_6/Incontinence_6th_Edition_2017_eBook_v2.pdf [Google Scholar]
- 4.Coyne KS, Wein A, Nicholson S, Kvasz M, Chen CI, Milsom I. Economic burden of urgency urinary incontinence in the United States: A systematic review. J Manag Care Pharm. 2014;20(2):130–140. doi: 10.18553/jmcp.2014.20.2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krhut J, Gärtner M, Mokris J, Horcicka L, Svabik K, Zachoval R, et al. Effect of severity of urinary incontinence on quality of life in women. Neurourol Urodyn. 2018;37(6):1925–1930. doi: 10.1002/nau.23568. [DOI] [PubMed] [Google Scholar]
- 6.Donovan J, Bosch R, Gotoh M, Jackson S, Naughton M, Radley S, et al. Symptom and quality of life assessment. Incontinence 3rd Int Consult Incontinence. 2005. pp. 519–584. [Google Scholar]
- 7.Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: A brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23(4):322–330. doi: 10.1002/nau.20041. [DOI] [PubMed] [Google Scholar]
- 8.Busquets M, Serra R. Validación del cuestionario international consultation on incontinence questionnaire short-form (ICIQ-SF) en una población chilena usuaria del fondo nacional de salud (FONASA) Rev. Med. Chile. 2012;140(3):340–346. doi: 10.4067/S0034-8872012000300009. [DOI] [PubMed] [Google Scholar]
- 9.Espuña Pons M, Rebollo Álvarez P, Puig Clota M. Validación de la versión española del International Consultation on Incontinence Questionnaire-Short Form. Un cuestionario para evaluar la incontinencia urinaria. Med Clin (Barc) 2004;122(8):288–292. doi: 10.1016/S0025-7753(04)74212-8. [DOI] [PubMed] [Google Scholar]
- 10.Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2018;10(10):CD005654–CD005654. doi: 10.1002/14651858.CD005654.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bø K, Kvarstein B, Nygaard I. Lower urinary tract symptoms and pelvic floor muscle exercise adherence after 15 years. Obstet Gynecol. 2005;105(5):999–1005. doi: 10.1097/01.AOG.0000157207.95680.6d. [DOI] [PubMed] [Google Scholar]
- 12.Dmochowski RR, Blaivas JM, Gormley EA, Juma S, Karram MM, Lightner DJ, et al. Update of AUA Guideline on the Surgical Management of Female Stress Urinary Incontinence. J Urol. 2010;183(5):1906–1914. doi: 10.1016/j.juro.2010.02.2369. [DOI] [PubMed] [Google Scholar]
- 13.Ford AA, Rogerson L, Cody JD, Aluko P, Ogah JA. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev. 2017;7(7):CD006375–CD006375. doi: 10.1002/14651858.CD006375.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brennand EA, Tang S, Birch C, Murphy M, Ross S, Robert M, et al. Five years after midurethral sling surgery for stress incontinence: obesity continues to have an impact on outcomes. Int Urogynecol J. 2017;28(4):621–628. doi: 10.1007/s00192-016-3161-y. [DOI] [PubMed] [Google Scholar]
- 15.Brennand EA, Tang S, Williamson T, Birch C, Murphy M, Robert M, et al. Twelve-month outcomes following midurethral sling procedures for stress incontinence: Impact of obesity. BJOG An Int J Obstet Gynaecol. 2015;122(12):1705–1712. doi: 10.1111/1471-0528.13132. [DOI] [PubMed] [Google Scholar]
- 16.EAU Guidelines . Edn Present EAU Annu Congr Amsterdam. 2020. [Google Scholar]
- 17.Gomes CM, Carvalho FL, Bellucci CHS, Hemerly TS, Baracat F, de Bessa Jr J, et al. Update on complications of synthetic suburethral slings. Int Braz J Urol. 2017;43(5):822–834. doi: 10.1590/s1677-5538.ibju.2016.0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Serati M, Braga A, Caccia G, Torella M, Ghezzi F, Salvatore S, et al. TVT-O for treatment of pure urodynamic stress urinary incontinence: Efficacy and adverse effects at 13-years follow-up. Neurourol Urodyn. 2020;39(5):1423– 1429. doi: 10.1002/nau.24358. [DOI] [PubMed] [Google Scholar]
- 19.Serati M, Braga A, Athanasiou S, Tommaselli GA, Caccia G, Torella M, et al. Tension-free Vaginal Tape-Obturator for Treatment of Pure Urodynamic Stress Urinary Incontinence: Efficacy and Adverse Effects at 10-year Follow-up. Eur Urol. 2017;71(4):674–679. doi: 10.1016/j.eururo.2016.08.054. [DOI] [PubMed] [Google Scholar]
- 20.Zhang Z, Zhu L, Xu T, Lang J. Retropubic tensionfree vaginal tape and inside-out transobturator tape: a long-term randomized trial. Int Urogynecol J. 2016;27(1):103–111. doi: 10.1007/s00192-015-2798-2. [DOI] [PubMed] [Google Scholar]
- 21.Zullo MA, Schiavi MC, Luffarelli P, Prata G, Di Pinto A, Oliva C. TVT-O vs. TVT-Abbrevo for stress urinary incontinence treatment in women: a randomized trial. Int Urogynecol J. 2020;31(4):703–710. doi: 10.1007/s00192-019-04077-7. [DOI] [PubMed] [Google Scholar]
- 22.Echavarría-Restrepo LG, Trujillo-Gallego LF, Hurtado- Arango CM, Gómez-Londoño M, Isaza-Sierra IC, Montoya-Vélez LP. Six months follow up of females treated with medium tension-free urethral slings for Urinary Stress Incontinence between 2007 and 2009 at the Pontificia Bolivariana teaching hospital in the city of Medellin, Colombia. Historical cohort. Rev Colomb Obstet Ginecol. 2011;62(3):237–243. doi: 10.18597/rcog.210. [DOI] [Google Scholar]
- 23.Fernandez-gonzalez S, Martinez E, Lin X, Amat L. Contasure-needleless® compared with Monarc® for the treatment of stress urinary incontinence. Int Urogynecol J. 2016;28(7):1077–1084. doi: 10.1007/s00192-016-3231-1. [DOI] [PubMed] [Google Scholar]
- 24.Haylen BT, Freeman RM, Swift SE, Cosson M, Davila GW, Deprest J, et al. An international urogynecological association (IUGA)/international continence society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic flo. Neurourol Urodyn. 2011;30(1):2–12. doi: 10.1002/nau.21036. [DOI] [PubMed] [Google Scholar]
- 25.Liapis A, Bakas P, Creatsas G. Efficacy of insideout transobturator vaginal tape (TVTO) at 4 years follow up. Eur J Obstet Gynecol Reprod Biol. 2010;148(2):199–201. doi: 10.1016/j.ejogrb.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 26.Masata J, Svabik K, Zvara K, Hubka P, Toman A, Martan A. Comparison of the efficacy of tension-free vaginal tape obturator (TVT-O) and single-incision tensionfree vaginal tape (AjustTM) in the treatment of female stress urinary incontinence: a 1-year follow-up randomized trial. Int Urogynecol J. 2016;27(10):1497–1505. doi: 10.1007/s00192-016-3012-x. [DOI] [PubMed] [Google Scholar]


