Abstract
Objectives
This study aims to explore the knowledge, attitudes and practices (KAP) of the population in the United Arab Emirates (UAE) regarding microbiota and the main factors affecting its composition.
Design/setting
A cross-sectional study, using a self-administered questionnaire, was conducted from May 2018 to September 2018, recruiting participants in public venues via convenience sampling.
Participants
UAE residents (aged 18 years and above) who spoke either Arabic or English.
Results
419 responses were completed and analysed using SPSS V.24. Only 29.3% (n=94) of the participants who defined microbiota correctly had good knowledge. There was a significant difference in knowledge among different age groups (p=0.004) and educational levels (p<0.001). Multiple linear regression (MLR) model indicated that being a university student and a healthcare professional (HCP) are the only significant predictors regarding microbiota knowledge (p=0.014 and p<0.001, respectively). Of the respondents who claimed to be aware of probiotics, only 9.1% (n=15) exhibited good knowledge. MLR model showed that being a postgraduate and an HCP are the only significant predictors for probiotics knowledge (p=0.016 and p<0.001, respectively). 42.4% (n=143) and 34.6% (n=28) of the non-medical and HCP participants, respectively, use antibiotics without a prescription. None of the respondents, with or without a medical background, demonstrated good attitudes and practices toward the use of antibiotics.
Conclusion
Despite the fact that the participants had a basic understanding of microbiota and probiotics, the overall knowledge was substandard. Additionally, the respondents engaged in improper practices that alter the microbiota composition, especially via antibiotics misuse. Campaigns should target the general population as well as HCPs to upheave their overall KAP.
Keywords: epidemiology, public health, public health
Strengths and limitations of this study.
A pilot study was conducted, and standardisation sessions were held to ensure a consistent and uniform data collection process.
The participants in this study were randomly selected and the questionnaires were self-administered after explaining the aims of the study to the participants and providing them with an information sheet.
Convenience sampling was used in this study, which could affect the generalisability of the results.
The study included only the three largest cities of the UAE: Abu Dhabi, Dubai and Sharjah; hence, the results might not be representing the UAE population wholly.
The correlation between socioeconomic status and the participants’ perception was not explored.
Introduction
The human body is a host to a wide variety of microorganisms that outnumber the human body cells; recent research estimates that for every human cell there are 1.3 bacterial cells in our body; yet they coexist in a dynamic fashion. This estimate does not consider the viruses, fungi and phage that exist in our body, which equal or outnumber the bacterial estimate. These microorganisms, known as microbiota or microflora, share a harmonious relationship with human body cells, in which both depend on the other for survival.1
The microbiota in the human body confers immunity against various diseases by acting as a physical barrier against pathogens, preventing their colonisation by consuming the available nutrients and producing antimicrobial substances. The gastrointestinal tract (GIT) microbiota consists of more than 35 000 bacterial species, the majority of which are obligate anaerobes.2
The composition of the microflora is host specific and subject to alterations throughout the individual’s life.2 As such, each person’s microbiotic composition is unique, and influenced by factors such as age, sex, diet, hygiene, environment and antibiotic use.3 Furthermore, imbalances in the GIT microbiota are associated with obesity and several diseases, such as type 2 diabetes mellitus.4 5 It is estimated that around 40% of the UAE population are either prediabetic or diabetic.6
Using external supplementation of beneficial microorganisms, in the form of probiotics, helps to preserve and restore the proper intestinal microflora balance.7 The WHO defines probiotics as ‘live microorganisms which when administered in adequate amounts confer a health benefit on the host’.8 Probiotics are available in the form of food, beverages and drugs. Moreover, probiotic products contain different strains of beneficial bacteria such as Lactobacillus and Bifidobacterium that can colonise the GIT achieving a healthier balance of microflora.9
Additionally, probiotics have been shown to have either prophylactic or adjuvant therapeutic effects on a vast spectrum of infective and non-infective diseases, such as inflammatory bowel disease (IBD), irritable bowel syndrome, Helicobacter pylori infection, gastroenteritis, respiratory tract infections, lactose intolerance, oral candidiasis, urinary tract infection, colon cancer and breast cancer.10–18 Furthermore, probiotics have been attributed to lowering blood cholesterol levels and treating psychiatric illnesses.19
In the literature, misuse of antibiotics is well documented; it leads to a disruption in the GIT microbiota composition and a state of dysbiosis.20 21 Recent studies have pivoted towards showing the benefits of faecal microbiota transplant (FMT) as an alternative to antibiotics, in cases of recurrent or refractory Clostridium difficile superinfection or as a preventative prophylactic measure.22–24
To the best of our knowledge, no previous studies have explored the public’s understanding of microbiota and its influencing factors, in the UAE. It is essential to determine the knowledge, attitudes and practices (KAP) of the population regarding microbiota and its influencing factors to explore the baseline knowledge to allow for targeted awareness campaigns to shed light on the significance of the issue. Thus, this study aims to explore the KAP of the UAE’s population regarding microbiota and the factors affecting its composition, especially probiotics and antibiotics.
Methodology
Study design and target population
A descriptive, cross-sectional study was conducted to assess the KAP of the UAE population on the role of microbiota in disease and the factors affecting its composition. The inclusion criteria consisted of UAE citizens and residents, aged 18 years and above, who spoke either English and/or Arabic as those are the only languages spoken by the researchers in the study. Visitors to the UAE and tourists were excluded from the study. Non-probability, convenience sampling was used to recruit participants from public venues in the three largest cities of the UAE (Abu Dhabi, Dubai and Sharjah) between the months of25 May and September 2018. These cities are the cultural and commercial hubs of the country and comprise most of the UAE population. A minimum sample size of 385 was calculated based on 5% marginal error and 50% prevalence using the following formula: , where n=sample size, p=expected prevalence and SE=sampling error.
Questionnaire development
A self-administered questionnaire was developed after reviewing the literature and multiple international studies.7 20 26–28 The questionnaire was developed in English and translated into Arabic. It consisted of 44 questions divided into four sections dealing with: demographics (4 questions), knowledge of microbiota (29 questions) and attitudes and practices toward microbiota (11 questions). It contained 5-item Likert scales, true and false, and multiple-choice questions. Before proceeding with data collection, standardisation sessions were held, through which the researchers agreed on a consistent and uniform method of data collection.
Patient and public involvement
Members of the public were involved in the development of the questionnaire and the outcome measures. Prior to the commencement of the survey, the English questionnaire was piloted on 10 individuals and the Arabic version on 7. This allowed for cognitive testing of the questionnaire among members of the public to improve the quality of the questions by helping identify questions, words or phrases that were ambiguous or difficult to understand. Based on the feedback, the questionnaire was modified and edited by the authors to eliminate any ambiguity. Data obtained from the pilot was not included in the data analysis. Following that, members of the public were recruited to take part in the survey. The results of the study will be shared via awareness campaigns and open access publications.
Data collection and analysis
During data collection, the researchers were available to clarify any doubts the participants had, and the study aims were verbally explained to them. An information sheet was provided stating that completion of the questionnaire indicates agreement to join the study. There were no names or signatures taken to ensure the anonymity of the participants in this study. Confidentiality was maintained as the collected data were only available to the researchers.
Data analysis was conducted via IBM SPSS V.24. The study demographic data included sex, age, level of education and occupation. The normality of the scale data was visualised and statistically tested using the Kolmogorov-Smirnov test. Comparison of the mean scores among groups was carried out by analysis of variance and Student’s t-test, since the parametric assumptions were fulfilled. Additionally, categorical data were outlined as frequencies and percentages and compared using χ2 test. Valid percentages were reported to account for missing data. Correct answers for the knowledge questions were awarded a point, whereas incorrect answers or skipped questions were awarded no points. Five-item Likert scales were collapsed into 3-item scales and awarded 1, 2 or 3 points accordingly when analysing attitudes and practices of probiotics and antibiotics. To assess knowledge, a score was calculated based on the participants’ responses. A point was given for either affirming a true statement or disagreeing with a false one, and a total score was calculated. Accordingly, participants who achieved total scores of >66%, 33%–66% and <33% were classified into groups of ‘good’, ‘average’ and ‘poor’, respectively. The same scoring system was used in assessing respondents’ attitudes and practices. To identify the significant predictors of microbiota and probiotic knowledge, stepwise multiple linear regression (MLR) was performed. The variables associated with the dependent variable, with a p value of ≤0.05, were entered in the model. Prior to performing the analysis, assumptions of MLR were tested. A p value of ≤0.05 was considered to be statistically significant. The methodological quality of this study was assessed using Strengthening the Reporting of Observational Studies in Epidemiology Scale.
Results
Demographics
Out of 480 questionnaires distributed, a total of 450 questionnaires were completed by respondents, yielding a response rate of 93.8%; however, 31 responses were omitted secondary to incompletion or missing data. Hence, 419 questionnaires were analysed. More than half of the participants were female (58.7%, n=246) and almost half were less than 30 years of age (45.2%, n=187). With regards to educational background, most of the participants were university graduates (51.0%, n=213). Nearly a fifth of the sample (19.4%, n=81) were healthcare professionals (HCPs) from various backgrounds, including doctors, nurses, pharmacists, etc (table 1).
Table 1.
Demographic distribution of the participants
| Demographics | n (%)* |
| Sex | |
| Male | 173 (41.3%) |
| Female | 246 (58.7%) |
| Age (years) | |
| 18–29 | 187 (45.2%) |
| 30–39 | 80 (19.3%) |
| 40–49 | 73 (17.6%) |
| 50+ | 74 (17.9%) |
| Level of education | |
| Below university | 69 (16.5%) |
| University student | 136 (32.5%) |
| University graduate | 213 (51.0%) |
| Occupation | |
| Arts | 35 (8.4%) |
| Business | 67 (16.0%) |
| Education | 43 (10.3%) |
| Engineering and IT | 78 (18.7%) |
| Government | 54 (12.9%) |
| Medical field | 81 (19.4%) |
| Others | 60 (14.4%) |
*Valid percentages to account for the missing data.
Knowledge of microbiota
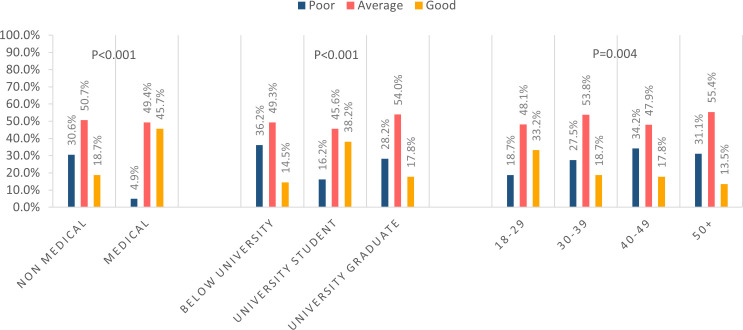
76.6% (n=321) of the participants were able to correctly define microbiota as ‘living bacteria inside a human body’. However, less than a third (29.3%, n=94) of those who defined microbiota correctly had good basic understanding on the topic and more than half (54.5%, n=175) had average knowledge. There was a significant difference in knowledge between those who defined microbiota correctly and who did not (p<0.001). Those who defined microbiota incorrectly were 6.2 times (95% CI 2.62 to 14.69) more likely to have poor or average knowledge when compared with those who defined it correctly. 52.2% (n=218) of the participants believed that having any bacteria in the nose is dangerous; additionally, 62.8% (n=263) believed that having bacteria in the intestines will lead to diarrhoea (table 2). Most of the participants, across all age groups, had average knowledge regarding microbiota. Only 33.2% (n=62) of the 18–29 years age group, 18.7% (n=15) of the 30–39 years age group, 17.8% (n=13) of the 40–49 years age group and 13.5% (n=10) of the above 50 years age group achieved a good knowledge score (p=0.004) (figure 1).
Table 2.
Knowledge of participants regarding microbiota
| Statements |
True | False | I do not know |
| n (%) | n (%) | n (%) | |
| Having bacteria in our nose is dangerous | 133 (31.8%) | 200 (47.8%) | 85 (20.3%) |
| Having bacteria in the intestines will cause diarrhoea | 161 (38.4%) | 156 (37.2%) | 102 (24.3%) |
| Having bacteria in the mouth will cause bad breath | 257 (61.3%) | 83 (19.8%) | 79 (18.9%) |
| Having bacteria on our skin is normal | 356 (85.0%) | 40 (9.5%) | 23 (5.5%) |
| It is good to have bacteria in our intestines | 258 (61.6%) | 72 (17.2%) | 88 (21.0%) |
| Microbiota can cause disease | 239 (57.0%) | 65 (15.5%) | 114 (27.2%) |
| Microbiota can protect against disease | 258 (61.6%) | 46 (11.0%) | 115 (27.4%) |
| Microbiota improves one’s mood and state of mind | 66 (15.8%) | 118 (28.3%) | 233 (55.9%) |
| Microbiota is mainly composed of chemicals | 50 (12.0%) | 238 (57.3%) | 127 (30.6%) |
Figure 1.
Knowledge of microbiota across the different demographic groups, including occupation, level of education and age.
Regardless of the level of education, most participants showed average knowledge on microbiota; however, university students had slightly better overall knowledge compared with the other groups (p<0.001) (figure 1). Surprisingly, almost half of the HCPs had average knowledge (49.4%, n=40). There was a significant difference between knowledge of HCPs and non-HCPs (p<0.001) (figure 1). MLR model indicated that being a university student and an HCP are the only significant predictors regarding microbiota knowledge (p=0.014 and p<0.001, respectively).
Pertaining to knowledge of the probiotics, the results showed that most of the population were not aware of the term probiotics (60.4%, n=252); of those who claimed to be, only 38.8% (n=64) correctly identified probiotics as ‘microorganisms’. Educational campaigns and social media were the most frequently reported sources of information on probiotics among the participants (20.8%, n=60% and 20.4%, n=59 respectively). Only 22.9% (n=96) were aware that antibiotics are not made from probiotics and only 17.4% (n=73) recognised that probiotics and antibiotics can be used together. Only 4.3% of the participants (n=18) had a good current understanding of probiotics, while the majority had basic information (62.5%, n=262). There was a significant difference between the knowledge of those who claimed to be aware of probiotics and those who were not (p<0.001). Interestingly, only 9.1% (n=15) of the respondents who claimed to be aware of probiotics had good knowledge, whereas more than half (51.5%, n=85) had average knowledge. Additionally, non-medical respondents were 9.6 times (95% CI 3.48 to 26.44) more likely to have poor or average knowledge regarding probiotics compared with HCPs. MLR model showed that being a postgraduate and an HCP are the only significant predictors for probiotics knowledge (p=0.016 and p<0.001, respectively).
Practices and attitudes regarding microbiota
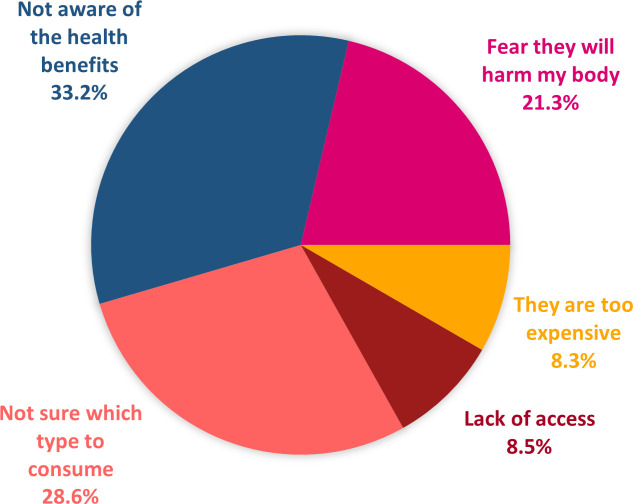
Only 17.8% of the participants (n=74) reported to have previously consumed probiotics, whereas the majority did not and have no interest in doing so (44.5%, n=185). Furthermore, being unaware of the health benefits of probiotics was the most common barrier to taking them (45.7%, n=187). Other barriers included safety concerns (29.3%, n=120) and lack of information on probiotic use (39.5%, n=161) (figure 2).
Figure 2.
General barriers against probiotics as stated by the participants.
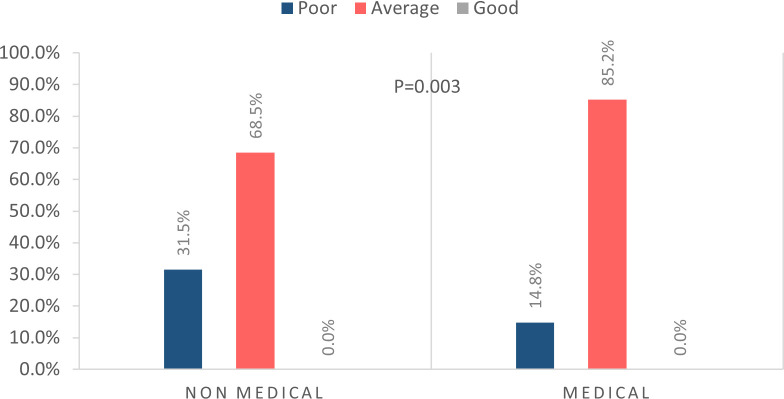
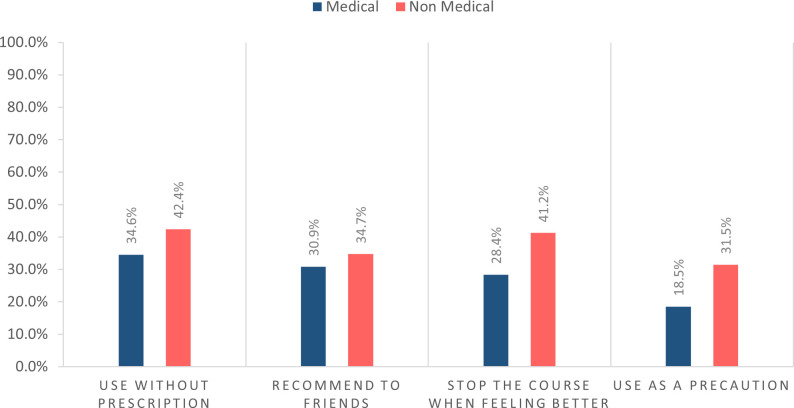
While none of the respondents, with or without a medical background, demonstrated good attitudes and practices towards the use of antibiotics, those with a medical background had better practices and attitudes compared with other occupations (p=0.003) (figure 3). Alarmingly, 42.4% (n=143) and 34.6% (n=28) of the non-medical and HCP participants, respectively, admitted they used antibiotics without a prescription. Additionally, 41.2% (n=139) of the non-medical participants admitted to stopping the course of antibiotics as soon as they feel better (figure 4). Just over half of the population were unlikely to take faecal pills to treat diarrhoea (53.2%, n=222) secondary to bacterial infections such as C. difficile.
Figure 3.
Attitudes and practices of healthcare professionals compared with non-medical participants regarding antibiotics use.
Figure 4.
Antibiotics practices of the medical and non-medical participants.
Discussion
Despite the participants’ awareness of microbiota and its basic definition, they lacked good knowledge regarding its role in protecting against disease and boosting one’s immunity. More than half of the participants believed that having bacteria in the nose is dangerous and worried that the presence of microorganisms in the intestines may cause diseases such as diarrhoea. This demonstrates that there are misconceptions among people regarding bacteria’s role in the human body.
Interestingly, age seems to play an important role in shaping people’s knowledge on this topic. Contrary to our expectations, respondents belonging to the older age groups were less versed on the matter when compared with the younger population. This can be attributed to younger people having increased exposure to the internet and social media on a regular basis. Furthermore, university students seemed to have better knowledge, than other educational groups, regarding microbiota.
Since the topic of microbiota is mostly of concern to HCPs and medical students, it is especially important for them to be more knowledgeable on the topic, compared with the general population. Despite our results showing that HCPs have better knowledge, it is not significantly higher than that of non-medical personnel.
Probiotics
As expected, awareness of the term ‘probiotics’ and what it constitutes was limited. More than 75% of the participants in our study were unaware of the difference between probiotics and antibiotics and had misconceptions regarding their use. Therefore, it was not surprising that an overwhelming majority (>80%) believed that probiotics and antibiotics can never be used together.
Regrettably, almost all participants failed to display good knowledge regarding probiotics, including HCPs. This highlights the importance of educating HCPs on probiotics and the advantages it might provide to their patients. Two meta-analyses reported a reduction in the incidence and duration of respiratory tract infections of viral origin, with probiotic use.29 30 Additionally, two randomised controlled trials showed that critically ill patients on mechanical ventilation developed substantially less ventilator-associated pneumonia when using probiotics compared with placebo.31 32 Probiotics have also shown excellent results in patients with allergies, atopic diseases, asthma and IBD.17 25 33
The number of published papers examining the knowledge of the general public regarding probiotics is very limited, with the majority looking at the knowledge of college students and HCPs. In accordance with our study, a study conducted in Saudi Arabia found that the public’s knowledge towards probiotics is very limited, just over 25%.34 This is in contrast to a study conducted in Nigeria, assessing knowledge among HCPs, which showed that around 72% of respondents were aware of probiotics.7 In India, a study conducted among college students found that 88.7% of participants were knowledgeable on probiotics composition.27 Furthermore, a study conducted on college students in the Philippines revealed that participants had a good level of knowledge about probiotics and its consumption.35 There is an obvious disparity between the knowledge of the general public when compared with HCPs and college students.
Most of our respondents would not consider taking probiotics and were not even willing to learn about them indicating a poor attitude among the UAE society toward probiotics. This finding was similar to an Australian study, where more than 40% of the participants demonstrated poor behaviours and practices towards probiotics.36 However, the participants may have not been aware that they are already consuming probiotics in the form of dairy food such as yoghurt and other types of food like miso, pickles, kimchi and sauerkraut. It would be essential to investigate this to determine if the community actually has negative attitudes towards probiotics consumption.
The use of FMT as a treatment is still being explored, multiple studies have reported positive results in clinical trials. There has been a shift in recent years in the modes of delivery of FMT from oesophagogastroduodenoscopy, nasogastric/jejunal/duodenal tubes, colonoscopy, retention enema to oral capsule.37–39 However, patients’ perspective in using FMT as a treatment modality remains to be further studied to identify the factors that improve attitudes and practices. In our study, more than half of the population were unlikely to take faecal pills, to treat diarrhoea. No other studies seem to have explored the acceptability of FMT in the community; however, the receptivity of probiotic pills in a study conducted in China among patients with Crohn’s disease showed that around 80% of non-refractory patients were willing to seek FMT as a possible cure or to achieve better clinical results.40 Another recent study in Germany, investigating general approval of FMT as an alternative treatment for obesity, revealed that more than half of the participants were willing to undergo FMT.41
Antibiotics
Antibiotic misuse can be worrying as it could lead to antibiotic resistance, which is a public health crisis. Since antibiotics interfere with normal microbial homeostasis, it is extremely important to address the general population’s unhealthy attitudes and practices towards antibiotic consumption. Alarmingly, not a single respondent in this study exhibited good attitudes nor practices regarding antibiotics, including HCPs. This demonstrates the gravity of the situation and the need for action to be taken towards rectifying this. Inappropriate practices included prophylactic antibiotic use, using antibiotics without a prescription, and not completing the antibiotic course.
Unfortunately, antibiotic misuse is a global concern. Several studies have investigated the public’s negative practices and behaviours regarding antibiotics. A study in the UAE’s capital, Abu Dhabi, indicated that almost half of the public admitted to taking antibiotics without a prescription.42 Additionally, a local study and an Italian one demonstrated that about a third of participants used antibiotics without a prescription.43 44 Moreover, an Indian study demonstrated that around 20% of medical students abruptly stop the antibiotic course on improvement of their symptoms and give the unused medications to their friends. High rates of improper practices among medical students were also reported despite their adequate knowledge, indicating a disparity in the application of their knowledge.45 Furthermore, a study conducted in Jordan found that more than 60% of respondents admitted to not completing the antibiotic course.46
Significance of results and future recommendations
In the Middle East and North Africa region, the topic of microbiota has not been extensively explored. International studies have recently linked gut microbiota dysbiosis with multiple diseases, including, diarrhoea, obesity, diabetes and IBD. Very recently, a case series from China showed that some patients with COVID-19 demonstrated gut microbial dysbiosis; this further highlights that even during the current pandemic, there is a need to place more emphasis on the topic of microbiota and the factors affecting its composition, which could lead to dysbiosis.47 Ongoing research explores methods of using probiotics as a way of restabilising the balance of microbiota to resolve disease. Hence, public knowledge is essential to promote the use of probiotics and decrease antibiotics misuse.
The overall knowledge of the UAE population regarding microbiota and its influencing factors is lacking. This poor knowledge can be attributed to multiple factors, including lack of access to information, inadequate awareness campaigns and the substandard level of knowledge among HCPs. As such, educational and health-promoting campaigns tackling the benefits of microbiota, its role in conferring immunity against diseases and the main factors affecting its composition would upheave the overall knowledge of the UAE community.
Even though this study did not explore the KAP of the different HCPs, further studies could investigate the different backgrounds and educational levels among HCPs, to determine the gaps and areas that need to be focused on through awareness campaigns. Regrettably, the HCPs in our study did not demonstrate sufficient knowledge regarding microbiota. In society, HCPs are viewed as role models of the healthcare system; however, our HCP respondents themselves had bad attitudes and engaged in unhealthy practices involving antibiotics. To rectify this, HCPs must update their knowledge. This can be achieved by attending special courses, workshops and seminars as well as lecture series for professional development on microbiota and its influencing factors to keep up with the current trends in healthcare. Seeking consultation from HCPs regarding appropriate probiotic and antibiotic use should be encouraged. This is especially important as HCPs play a major role in ensuring an appropriate level of knowledge among the general population, ultimately leading to better attitudes and practices. Additionally, further emphasis needs to be placed on the topic of microbiota in medical and health-related schools to ensure that students acquire adequate knowledge for the purpose of educating the general population in the future.
Another way to reach the UAE public is via social media, which was found to be a major source of information regarding probiotics in our study. While internet and social media usage has many benefits, the information shared on such platforms, especially medical, might not always be reliable. Henceforth, care should be taken to monitor and update these resources on a regular basis, to provide accurate knowledge on probiotic forms, health benefits, natural sources and appropriate consumption. Hence, if used correctly, these resources can positively contribute to the society, by promoting health education.
Limitations
This study used convenience sampling, which might affect the generalisability of the results. Physical mail is not a common mode of communication in the UAE and home visits are not an appropriate method of data collection in this conservative society. Additionally, only the three largest cities, Abu Dhabi, Dubai and Sharjah, were included in the study, which might further affect the generalisability of the results. However, since the UAE is a metropolitan country, we expect the results to be representative of the UAE population. Finally, we did not explore how the difference in socioeconomic status might affect the perception of the participants nor did we investigate the plausible difference in KAP of the local versus the expatriate communities in the UAE.
Conclusion
The overall KAP of the UAE population regarding microbiota and factors affecting it are low. Most participants had wrong perception about the role of microbiota in the body, and their ability to confer illnesses. Additionally, they were not aware about what probiotics comprised of or the health benefits of probiotics. Furthermore, the participants had poor attitudes and engaged in bad practices regarding antibiotics. Hence, it is important to emphasise the role of microbiota in disease and to educate the population, especially HCPs, on the topic.
Supplementary Material
Acknowledgments
The authors thank Dr Amal Hussein from the Department of Family and Community Medicine and Behavioural Sciences at the University of Sharjah for her continuous support throughout the project.
Footnotes
HJB and SFA contributed equally.
Contributors: HJB: contributed to the conception and design of the study, critically revised the manuscript and provided valuable feedback. SFA, HRR and MAA: drafted and tested the questionnaire, participated in data collection, performed the statistical analysis, contributed to writing the manuscript, critically revised the manuscript and provided valuable feedback. SKA: drafted and tested the questionnaire, participated in data collection and performed the analysis.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study was approved by the Research Ethics Committee at the University of Sharjah (number: REC-18-01-31-03-S). Information sheet was provided to the participants that stated that completion of the questionnaire indicates agreement to join the study.
References
- 1.Sender R, Fuchs S, Milo R. Are we really Vastly Outnumbered? revisiting the ratio of bacterial to host cells in humans. Cell 2016;164:337–40. 10.1016/j.cell.2016.01.013 [DOI] [PubMed] [Google Scholar]
- 2.Sekirov I, Russell SL, Antunes LCM, et al. Gut microbiota in health and disease. Physiol Rev 2010;90:859–904. 10.1152/physrev.00045.2009 [DOI] [PubMed] [Google Scholar]
- 3.Duda-Chodak A, Tarko T, Satora P, et al. Interaction of dietary compounds, especially polyphenols, with the intestinal microbiota: a review. Eur J Nutr 2015;54:325–41. 10.1007/s00394-015-0852-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Acosta A, Camilleri M. Gastrointestinal morbidity in obesity. Ann N Y Acad Sci 2014;1311:42–56. 10.1111/nyas.12385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qin J, Li Y, Cai Z, et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 2012;490:55–60. 10.1038/nature11450 [DOI] [PubMed] [Google Scholar]
- 6.Hamoudi R, Saheb Sharif-Askari N, Saheb Sharif-Askari F, et al. Prediabetes and diabetes prevalence and risk factors comparison between ethnic groups in the United Arab Emirates. Sci Rep 2019;9:17437. 10.1038/s41598-019-53505-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Otuto Amarauche C, Amarauche CO. Assessing the awareness and knowledge on the use of probiotics by healthcare professionals in Nigeria. J Young Pharm 2016;8:53–5. 10.5530/jyp.2016.1.12 [DOI] [Google Scholar]
- 8.Fao J, Working WHO, Report G. Guidelines for the evaluation of probiotics in food 2002:1–11https://www.who.int/foodsafety/fs_management/en/probiotic_guidelines.pdf
- 9.Iannitti T, Palmieri B. Therapeutical use of probiotic formulations in clinical practice. Clin Nutr 2010;29:701–25. 10.1016/j.clnu.2010.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sihra N, Goodman A, Zakri R, et al. Nonantibiotic prevention and management of recurrent urinary tract infection. Nat Rev Urol 2018;15:750–76. 10.1038/s41585-018-0106-x [DOI] [PubMed] [Google Scholar]
- 11.Shahbazi R, Yasavoli-Sharahi H, Alsadi N, et al. Probiotics in treatment of viral respiratory infections and neuroinflammatory disorders. Molecules 2020;25. 10.3390/molecules25214891. [Epub ahead of print: 22 Oct 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shenoy A, Gottlieb A. Probiotics for oral and vulvovaginal candidiasis: a review. Dermatol Ther 2019;32:e12970. 10.1111/dth.12970 [DOI] [PubMed] [Google Scholar]
- 13.Oak SJ, Jha R. The effects of probiotics in lactose intolerance: a systematic review. Crit Rev Food Sci Nutr 2019;59:1675–83. 10.1080/10408398.2018.1425977 [DOI] [PubMed] [Google Scholar]
- 14.Vitellio P, Celano G, Bonfrate L, et al. Effects of Bifidobacterium longum and Lactobacillus rhamnosus on Gut microbiota in patients with lactose intolerance and persisting functional gastrointestinal symptoms: a randomised, double-blind, cross-over study. Nutrients 2019;11. 10.3390/nu11040886. [Epub ahead of print: 19 Apr 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhu R, Chen K, Zheng Y-Y, et al. Meta-analysis of the efficacy of probiotics in Helicobacter pylori eradication therapy. World J Gastroenterol 2014;20:18013–21. 10.3748/wjg.v20.i47.18013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mendoza L. Potential effect of probiotics in the treatment of breast cancer. Oncol Rev 2019;13:422. 10.4081/oncol.2019.422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saez-Lara MJ, Gomez-Llorente C, Plaza-Diaz J, et al. The role of probiotic lactic acid bacteria and bifidobacteria in the prevention and treatment of inflammatory bowel disease and other related diseases: a systematic review of randomized human clinical trials. Biomed Res Int 2015;2015:1–15. 10.1155/2015/505878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Didari T, Mozaffari S, Nikfar S, et al. Effectiveness of probiotics in irritable bowel syndrome: updated systematic review with meta-analysis. World J Gastroenterol 2015;21:3072. 10.3748/wjg.v21.i10.3072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sarkar A, Lehto SM, Harty S, et al. Psychobiotics and the manipulation of Bacteria-Gut-Brain signals. Trends Neurosci 2016;39:763–81. 10.1016/j.tins.2016.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thursby E, Juge N. Introduction to the human gut microbiota. Biochem J 2017;474:1823–36. 10.1042/BCJ20160510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Malik B, Bhattacharyya S. Antibiotic drug-resistance as a complex system driven by socio-economic growth and antibiotic misuse. Sci Rep 2019;9:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mullish BH, Quraishi MN, Segal JP, et al. The use of faecal microbiota transplant as treatment for recurrent or refractory Clostridium difficile infection and other potential indications: joint British Society of Gastroenterology (BSG) and Healthcare Infection Society (HIS) guidelines. Gut 2018;67:1920–41. 10.1136/gutjnl-2018-316818 [DOI] [PubMed] [Google Scholar]
- 23.Shen NT, Maw A, Tmanova LL, et al. Timely use of probiotics in hospitalized adults prevents Clostridium difficile infection: a systematic review with meta-regression analysis. Gastroenterology 2017;152:1889–900. 10.1053/j.gastro.2017.02.003 [DOI] [PubMed] [Google Scholar]
- 24.Goldenberg JZ, Yap C, Lytvyn L, et al. Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children. Cochrane Database Syst Rev 2017;12:CD006095. 10.1002/14651858.CD006095.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lise M, Mayer I, Silveira M. Use of probiotics in atopic dermatitis. Rev Assoc Med Bras 2018;64:997–1001. 10.1590/1806-9282.64.11.997 [DOI] [PubMed] [Google Scholar]
- 26.Chukwu E, Nwaokorie F, Yisau J, et al. Assessment of the knowledge and perception of probiotics among medical science students and practitioners in Lagos state. Br J Med Med Res 2015;5:1239–46. 10.9734/BJMMR/2015/13676 [DOI] [Google Scholar]
- 27.Sharma R, Gupta S, Gupta D, et al. Awareness and knowledge about probiotics among college students. J Pure Appl Microbiol 2019;13:2201–8. 10.22207/JPAM.13.4.33 [DOI] [Google Scholar]
- 28.DST P, Huang JH, MHM L. Knowledge, attitudes and practices towards antibiotic use in upper respiratory tract infections among patients seeking primary health care in Singapore. BMC Fam Pract 2016;17:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hao Q, Lu Z, Dong BR, et al. Probiotics for preventing acute upper respiratory tract infections. Cochrane Database Syst Rev 2011:CD006895. 10.1002/14651858.CD006895.pub2 [DOI] [PubMed] [Google Scholar]
- 30.King S, Glanville J, Sanders ME, et al. Effectiveness of probiotics on the duration of illness in healthy children and adults who develop common acute respiratory infectious conditions: a systematic review and meta-analysis. Br J Nutr 2014;112:41–54. 10.1017/S0007114514000075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morrow LE, Kollef MH, Casale TB. Probiotic prophylaxis of ventilator-associated pneumonia: a blinded, randomized, controlled trial. Am J Respir Crit Care Med 2010;182:1058–64. 10.1164/rccm.200912-1853OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zeng J, Wang C-T, Zhang F-S, et al. Effect of probiotics on the incidence of ventilator-associated pneumonia in critically ill patients: a randomized controlled multicenter trial. Intensive Care Med 2016;42:1018–28. 10.1007/s00134-016-4303-x [DOI] [PubMed] [Google Scholar]
- 33.Mennini M, Dahdah L, Artesani MC, et al. Probiotics in asthma and allergy prevention. Front Pediatr 2017;5:165. 10.3389/fped.2017.00165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Allah HAA, S. PM. The knowledge and perceptions regarding probiotics among the people of Al-Qassim region, Saudi Arabia. Jhms 2019;2. 10.31014/aior.1994.02.03.56 [DOI] [Google Scholar]
- 35.Mejia WB, Sheree A, Barrion A. Cronicon knowledge and consumption of probiotic foods of selected students in Laguna, Philippines. EC Nutrition 2019;14:452–9. [Google Scholar]
- 36.Khalesi PhD S, Vandelanotte PhD C, Thwaite BSc T, et al. Awareness and attitudes of gut health, probiotics and prebiotics in Australian adults. J Diet Suppl 2021;18:418–32. 10.1080/19390211.2020.1783420 [DOI] [PubMed] [Google Scholar]
- 37.Stallmach A, Steube A, Grunert P. Fecal microbiota transfer: reliable indications, donor screening, and modes of application. Dtsch Arztebl Int 2020;117:31–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Du C, Luo Y, Walsh S, et al. Oral fecal microbiota transplant capsules are safe and effective for recurrent Clostridioides difficile infection: a systematic review and meta-analysis. J Clin Gastroenterol 2021;55:300–8. 10.1097/MCG.0000000000001495 [DOI] [PubMed] [Google Scholar]
- 39.Wang J-W, Kuo C-H, Kuo F-C, et al. Fecal microbiota transplantation: review and update. J Formos Med Assoc 2019;118 Suppl 1:S23–31. 10.1016/j.jfma.2018.08.011 [DOI] [PubMed] [Google Scholar]
- 40.Xu L, Zhang T, Cui B, et al. Clinical efficacy maintains patients’ positive attitudes toward fecal microbiota transplantation. Medicine 2016;95:e4055. 10.1097/MD.0000000000004055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gundling F, Roggenbrod S, Schleifer S, et al. Patient perception and approval of faecal microbiota transplantation (FMT) as an alternative treatment option for obesity. Obes Sci Pract 2019;5:68–74. 10.1002/osp4.302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Abasaeed A, Vlcek J, Abuelkhair M, et al. Self-Medication with antibiotics by the community of abu dhabi Emirate, United Arab Emirates. J Infect Dev Ctries 2009;3:491–7. 10.3855/jidc.466 [DOI] [PubMed] [Google Scholar]
- 43.Abduelkarem AR, Othman AM, Abuelkhair ZM, et al. Prevalence of self-medication with antibiotics among residents in United Arab Emirates. Infect Drug Resist 2019;12:3445–53. 10.2147/IDR.S224720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Napolitano F, Izzo MT, Di Giuseppe G, et al. Public knowledge, attitudes, and experience regarding the use of antibiotics in Italy. PLoS One 2013;8:e84177. 10.1371/journal.pone.0084177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Khan A K A, Banu G, KK R. Antibiotic resistance and Usage-A survey on the knowledge, attitude, perceptions and practices among the medical students of a southern Indian teaching hospital. J Clin Diagn Res 2013;7:1613–6. 10.7860/JCDR/2013/6290.3230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Suaifan GA RY, Shehadeh M, Darwish DA. A cross-sectional study on knowledge, attitude and behavior related to antibiotic use and resistance among medical and non-medical university students in Jordan. African J Pharm Pharmacol 2012;6:763–70. [Google Scholar]
- 47.Xu K, Cai H, Shen Y. Management of COVID-19: the Zhejiang experience. Zhejiang Da Xue Xue Bao Yi Xue Ban 2020;49:147–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request.