Abstract
This report describes and contextualizes the high prevalence of mental health conditions (MHC) among Minnesota 2019 EVALI patients by examining the prevalence of MHC and associations between MHC and e-cigarette or vaping product (EVP) use in Minnesota population surveys.
Investigators reviewed medical records for 140 EVALI patients to determine history of MHC. History of MHC and EVP use in the general population was estimated using self-reported measures and screening tools from two population-based surveys, the 2019 Minnesota Student Survey (MSS) and the 2018 Minnesota Behavioral Risk Factor Surveillance Survey (MN-BRFSS).
Some 64.3% of EVALI patients had an MHC. In both Minnesota population surveys, MHCs were common among people who used EVP. The odds of MHC among youth aged <18 were higher among those who reported current EVP use compared with those did not report EVP use. Similarly, the odds of depression were higher among adults who reported current EVP use compared with those who did not.
Clinicians treating patients with EVALI should consider evaluating the need for, and providing indicated referrals to, post-discharge mental health services for their patients.
Introduction
A multistate outbreak of e-cigarette, or vaping, product-use associated lung injury (EVALI) was identified in the United States in summer 2019. During their investigation of the outbreak, Minnesota Department of Health (MDH) epidemiologists noted a high prevalence of underlying mental health conditions (MHC), including anxiety, depression, and other psychiatric diagnoses among confirmed and probable EVALI patients. Additionally, some of these patients noted during interview that they had been using e-cigarette, or vaping, products (EVP) with the intention of alleviating MHC symptoms. Finally, language about alleviating MHC symptoms was noted on packaging (Figure) of some EVP that EVALI patients had submitted to MDH’s Public Health Laboratory for testing. All three of these observations from the outbreak investigation process raised questions not only about a potential association between MHC and EVALI, but about a potential association between MHC and EVP use in the general Minnesota population.
FIGURE.
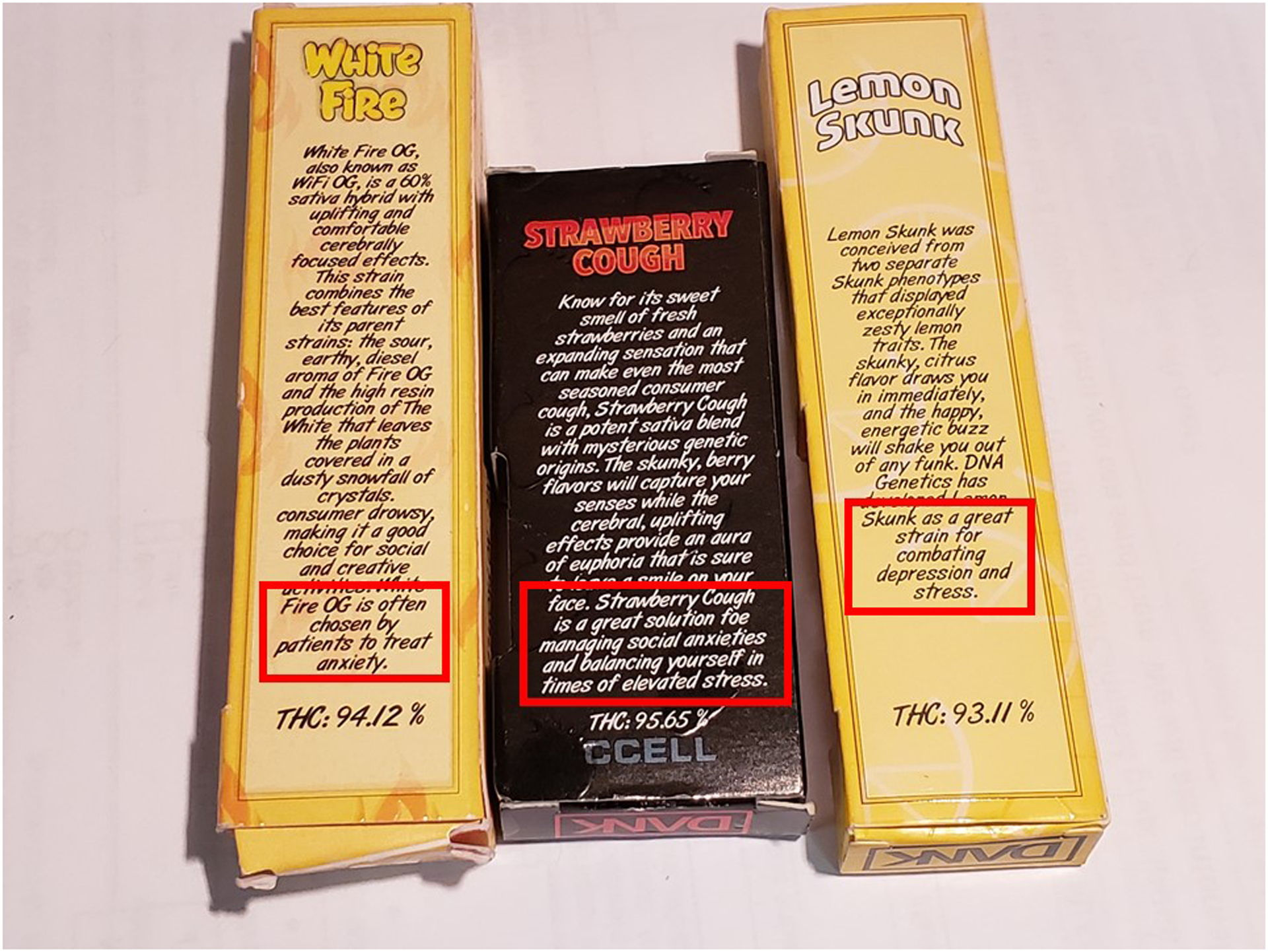
Examples of labels on illicit tetrahydrocannabinol-containing e-cigarette, or vaping, product packaging submitted to the Minnesota Department of Health by e-cigarette, or vaping, product-use associated lung injury patients that specifically reference symptoms associated with mental health conditions
In order to better describe the prevalence of MHC among Minnesota EVALI patients, medical records for all 140 confirmed and probable patients were reviewed. In order to contextualize these findings with observations from the general Minnesota population, two population-based surveys, the 2019 Minnesota Student Survey (MSS) and the 2018 Minnesota Behavioral Risk Factor Surveillance Survey (MN-BRFSS), were used to estimate the prevalence of MHC and EVP use among youths and adults.
Methods
EVALI patients
EVALI became reportable to MDH on August 12, 2019. During August 15–December 23, 2019, MDH interviewed EVALI patients or their proxies for cases reported by clinicians to MDH during August 8–December 16, 2019.1 Patients were identified as confirmed or probable EVALI cases using the standardized case definition provided by the Centers for Disease Control and Prevention.2 MDH also reviewed patient medical records to ascertain history of MHC, including anxiety, depression, and other psychiatric diagnoses, and history of medication commonly indicated for MHC. Other psychiatric diagnoses included attention-deficit/hyperactivity disorder, attention deficit disorder, specified and unspecified eating disorders, adjustment disorder, borderline personality disorder, post-traumatic stress disorder, bipolar disorder, panic disorder, obsessive-compulsive disorder, psychotic disorder, schizoaffective disorder, unspecified personality disorder, and schizophrenia. To reduce potential confounding, substance-use disorders were not counted as MHC.
Population surveys
Prevalence estimates of MHC and current EVP use (defined as an answer of “every day,” “most days,” or “some days” to the question, “during the past 30 days, on how many days did you use an e-cigarette or electronic vaping product?”) among Minnesota school-attending adolescents were obtained from the 2019 Minnesota Student Survey (MSS).3 MSS is a census-style statewide computer survey of fifth-, eighth-, ninth-, and 11th-graders conducted every three years in the spring. Survey responses from 125,228 students (response rate 64%) from grades 8, 9, and 11, who were between the ages of 12 and 19 years were analyzed, including 624 (0.5%) students aged 18–19 years. Respondents were identified as having “any” MHC if they answered “yes” to the question, “Have you ever been diagnosed with a long-term mental health problem?” Anxiety and depression symptoms were assessed using the 2-Item Generalized Anxiety Disorder questionnaire (GAD-2) and 2-Item Patient Health Questionnaire (PHQ-2).4,5 Anxiety or depression was defined as a score of ≥3 on the GAD-2 and PHQ-2, respectively.
Prevalence estimates of depression and current EVP use among adults were obtained from the 2018 Minnesota Behavioral Risk Factor Surveillance Survey (MN-BRFSS), an annual, state-based telephone survey of noninstitutionalized U.S. adults aged ≥18 years.6 In 2018, a total of 16,990 people responded to MN-BRFSS (51.0% combined landline and cell phone weighted response rate). Current EVP use was defined as an answer of “every day,” “most days,” or “some days” to the question, “during the past 30 days, on how many days did you use an e-cigarette or electronic vaping product?” Respondents were identified as having depression if they answered “yes” to the question, “Have you ever been told you have a depressive disorder?” Appropriate indicators for “any” MHC and anxiety were not available.
Statistical analysis
Proportions of any MHC, anxiety, and depression by sex among EVALI patients were compared using Pearson’s chi-square test (α = 0.05). For both MSS and MN-BRFSS surveys, percentages and odds ratios (ORs) of self-reported MHC diagnoses and symptoms were calculated. MN-BRFSS data were weighted to account for the complex sampling design. We tested associations for effect modification by sex. For associations with evidence of effect modification (α = 0.05), sex-stratified ORs were calculated. For associations without evidence of effect modification, ORs were adjusted for sex. All statistical analyses were performed using SAS® (version 9.4; SAS Institute, Cary, North Carolina).
Results
EVALI patients
During August 8–December 16, 2019, a total of 140 confirmed and probable EVALI patients were reported to MDH; median age was 22 years (interquartile range: 18–32.5 years), and 89 (63.6%) patients were male. Ninety (64.3%) EVALI patients had a history of any MHC; 75 (83.3%) of these 90 EVALI patients were prescribed at least one medication commonly indicated for MHC before seeking care for EVALI. Among 34 EVALI patients aged <18 years (range: 13–17), 61.8% had any MHC, including 58.8% who had anxiety, and 35.3% who had depression. Among these 34 adolescent patients, prevalence of any MHC, anxiety, and depression did not significantly differ between female and male patients (75.0% vs 50.0%, p = 0.13 [prevalence of any MHC]; 75.0% vs 44.4%, p = .07 [anxiety]; and 43.8% vs 27.8%, p = 0.33 [depression]) (Table 1).
TABLE 1.
Mental health conditions (MHCs) among 140 Minnesota patients with e-cigarette, or vaping, product-use associated lung injury, by sex and age — August-December 2019
| Any MHC, including anxiety, depression, and other psychiatric diagnoses* (%) | Anxiety (%) | Depression (%) | |
|---|---|---|---|
| Total | 90/140 (64.3) | 78/140 (55.7) | 66/140 (47.1) |
| Prescribed medication commonly indicated for MHC | 75/90 (83.3) | 67/78 (85.9) | 56/66 (84.9) |
| Male | 48/89 (53.9) | 39/89 (43.8) | 34/89 (38.2) |
| Female | 41/50 (82.0) | 38/50 (76.0) | 31/50 (62.0) |
| Other | 1/1 (100) | 1/1 (100) | 1/1 (100) |
| Aged <18 years | 21/34 (61.8) | 20/34 (58.8) | 12/34 (35.3) |
| Male | 9/18 (50.0) | 8/18 (44.4) | 5/18 (27.8) |
| Female | 12/16 (75.0) | 12/16 (75.0) | 7/16 (43.8) |
| ≥18 years | 69/106 (65.1) | 58/106 (54.7) | 54/106 (50.9) |
| Male | 39/71 (54.9) | 31/71 (43.7) | 29/71 (40.8) |
| Female | 29/34 (85.3) | 26/34 (76.5) | 24/34 (70.6) |
| Other | 1/1 (100) | 1/1 (100) | 1/1 (100) |
Other psychiatric diagnoses included attention-deficit/hyperactivity disorder, attention deficit disorder, specified and unspecified eating disorders, adjustment disorder, borderline personality disorder, post-traumatic stress disorder, bipolar disorder, panic disorder, obsessive-compulsive disorder, psychotic disorder, schizoaffective disorder, unspecified personality disorder, and schizophrenia.
Among 106 EVALI patients aged ≥18 years (range 18–75), 65.1% had any MHC, 54.7% had anxiety, and 50.9% had depression. Prevalence of any MHC was higher among adult women than adult men (85.3% vs 54.9%; p <0 .01), as was anxiety (76.5% vs 43.7%; p < 0.01), and depression (70.6% vs. 40.8%; p < 0.01) (Table 1).
Population surveys
Among all MSS respondents, prevalence of any self-reported MHC diagnosis, anxiety, and depression was 30.3%, 35.3%, and 27.6%, respectively, for females; and was 15.9%, 16.2%, and 16.8%, respectively, for males (Table 2). Among MSS respondents reporting current EVP use, prevalence of any self-reported MHC diagnosis, anxiety, and depression was 50.8%, 45.5%, and 52.9%, respectively, for females; and was 26.6%, 27.9%, and 26.5%, respectively, for males (Table 2). Among MSS respondents, 16% of male and 18% of female students reported current EVP use. Odds of any MHC diagnosis, depression, and anxiety were significantly higher among those who reported current EVP use (Table 2). ORs were higher among female students [any MHC: 2.97 (2.85, 3.11); depression: 2.46 (2.35, 2.57); anxiety: 2.73 (2.61, 2.86)] than among male students [any MHC: 2.22 (2.10, 2.35); depression: 2.26 (2.14, 2.39); anxiety: 2.21 (2.09, 2.33)] (Table 2).
TABLE 2:
Prevalence of mental health conditions (MHCs) and odds of MHC by e-cigarette or vaping product (EVP) use — 2019 Minnesota Student Survey (MSS)†and 2018 Minnesota Behavioral Risk Factor Surveillance Survey (MN-BRFSS)§
| MHC Variable | Survey | Age Group | Prevalence of MHC among all respondents (%) | Prevalence of MHC among respondents reporting current EVP use (%) | Prevalence of MHC among respondents NOT reporting current EVP USE (%) | Current EVP use |
|---|---|---|---|---|---|---|
| Any MHC | 2019 MSS | 12–19 | Male: 15.9 | Male: 26.6 | Male: 13.7 | 2.22 (2.10, 2.35) |
| Female: 30.3 | Female: 50.8 | Female: 25.8 | 2.97 (2.85, 3.11) | |||
| Anxiety | 2019 MSS | 12–19 | Male: 16.2 | Male: 27.9 | Male: 14.0 | 2.21 (2.09, 2.33) |
| Female: 35.3 | Female: 45.5 | Female: 31.3 | 2.46 (2.35, 2.57) | |||
| Depression | 2019 MSS | 12–19 | Male: 16.8 | Male: 26.5 | Male: 14.6 | 2.26 (2.14, 2.39) |
| Female: 27.6 | Female: 52.9 | Female: 23.4 | 2.73 (2.61, 2.86) | |||
| Depression | 2018 MN-BRFSS | 18–65+ | Overall: 17.6 | Overall: 32.5 | Overall: 17.0 | 2.75 (2.20, 3.43) (Adjusted for sex) |
MSS is a statewide computer survey of fifth, eighth, ninth, and 11th grade students conducted every three years. Fifth graders were not asked about EVP use and not included in this analysis.
MN-BRFSS is an annual, state-based telephone survey of noninstitutionalized U.S. adults aged ≥18 years.
Among all adult MN-BRFSS respondents, prevalence of depression was 17.6%. (Table 2). Among adult MN-BRFSS respondents who reported current EVP use, the prevalence of depression was 32.5% (Table 2). Among MN-BRFSS respondents, 5% of male and 2% of female adults reported current EVP use. Adjusting for sex, odds of self-reported depression were significantly higher [OR = 2.75 (2.20, 3.43)] among respondents who reported current EVP use, compared with those who did not (Table 2).
Discussion
Approximately two-thirds of Minnesota EVALI patients had evidence of a past medical history of any MHC. Among adult EVALI patients, MHC prevalence was higher among females than males. The majority of EVALI patients with MHC had been prescribed at least one medication commonly indicated for MHC before seeking care for EVALI. These findings reinforce CDC’s guidance to clinicians that EVALI patients might benefit from evaluations for MHC to determine post-discharge support needs, including assuring social support and access to mental health and substance-use disorder services.7
Among respondents to the 2019 MSS and 2018 MN-BRFSS, both youth and adults who reported current EVP use were significantly more likely to report history or symptoms of MHC than those who did not report current EVP use. These findings align with those of other cross-sectional analyses that have investigated MHC and EVP use in large, population-based samples.8,9 For example, among respondents to the 2016 National Health Interview Survey, those who self-reported MHC were 2–3 times more likely to report EVP ever use and current use, compared with respondents who did not report MHC.7 In another large, nationally representative adult sample, Cummins et al. found that regardless of smoking status, respondents with self-reported MHC were approximately twice as likely to have tried e-cigarettes as those without MHC.8 The survey data collection tools referenced in these studies do not ask respondents to distinguish between nicotine-containing EVP use and tetrahydrocannabinol (THC)-containing EVP use.
An important limitation of this study is the inability of the 2019 MSS and 2018 MN-BRFSS survey instruments to distinguish between use of nicotine-containing EVP and THC-containing EVP.1 Although the majority of EVALI patients reported using THC-containing EVP, MSS and MN-BRFSS respondents could have used mostly nicotine- or cannabidiol (CBD)-containing EVP. Therefore, we are unable to determine whether the high prevalence of MHC among EVALI patients and the association between EVP and MHC in the general population represent the same association. To more fully understand this association and its implications for population health, more research is needed to examine the role that specific EVP substances (e.g., illicit THC-containing EVPs vs nicotine-containing EVPs) play in the association with MHC. Additionally, because the study samples and data collection methods differ fundamentally from each other, prevalence of MHC should not be directly compared between samples. However, the similarity of findings within each of these disparate samples makes a strong case for an association between MHC and EVP use. Another limitation is the use of self-reported data to estimate the population prevalence of MHC. Because of social stigma around MHC, MSS respondents and MN-BRFSS respondents might have been less likely to report MHC. Similarly, EVALI patients may not have volunteered history of MHC to their physicians during lung injury treatment.
Conclusions
Clinicians treating patients with EVALI should consider evaluating the need for post-discharge mental health services for their patients, especially if the patient reports having used EVP intending to manage MHC-related symptoms. These post-discharge mental health services could include assuring social support and access to mental health and substance-use disorder services. Further research is warranted to examine underlying factors driving the observed association between EVP use and MHC among the general population youth and adults.
Acknowledgments
Muneera Hassan, Minnesota Department of Health; Anna Lynn, Minnesota Department of Health; Molly Meyer, Minnesota Department of Health; Kari Gloppen, Minnesota Department of Health; Deborah Anderson, PharmD, Minnesota Poison Control System; Elisabeth Bilden, MD, Essentia Health-Saint Mary’s Medical Center, Duluth, Minnesota; Anne Griffiths, MD, Children’s Hospital, Minneapolis, Minnesota; Sakina Naqvi, MD, M Health Fairview Health Services, Saint Paul, Minnesota; Travis Olives, MD, Hennepin Healthcare and Minnesota Poison Control System; staff members and leadership of the Minnesota Department of Public Health; Minnesota clinicians; interviewed lung injury patients.
This report was supported in part by an appointment to the Applied Epidemiology Fellowship Program administered by the Council of State and Territorial Epidemiologists (CSTE) and funded by the Centers for Disease Control and Prevention (CDC) Cooperative Agreement Number 1NU38OT000297-01-00.
Footnotes
None of the authors have any conflict of interest to disclose.
References
- 1.Taylor J, Wiens T, Peterson J, Saravia S, Lunda M, Hanson K, et al. Characteristics of E-cigarette, or Vaping, Products Used by Patients with Associated Lung Injury and Products Seized by Law Enforcement — Minnesota, 2018 and 2019. MMWR Morb Mortal Wkly Rep 2019;68:1096–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. 2019. Lung Injury Surveillance Primary Case Definition (CDC) – September 18, 2019. Office on Smoking and Health Website. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease/health-departments/index.html#primary-case-def. Accessed September 19, 2019.
- 3.Minnesota Department of Education. 2019 Minnesota Student Survey. Roseville (MN). 2019. [Google Scholar]
- 4.Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic meta-analysis. General Hospital Psychiatry. 2016;39:24–31. [DOI] [PubMed] [Google Scholar]
- 5.Arroll B, Goodyear-Smith F, Crengle S, Gunn J, Kerse N, Fishman T, et al. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Annals of Family Medicine. 2010; 8(4):348–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System Survey Data. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. 2019. [Google Scholar]
- 7.Evans ME, Twentyman E, Click ES, Goodman AB, Weissman DN, Kiernan E, et al. Update: Interim Guidance for Health Care Professionals Evaluating and Caring for Patients with Suspected E-cigarette, or Vaping, Product Use–Associated Lung Injury and for Reducing the Risk for Rehospitalization and Death Following Hospital Discharge — United States, December 2019. MMWR Morb Mortal Wkly Rep 2020; 68:1189–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bianco CL. Rates of electronic cigarette use among adults with a chronic mental illness. Addictive Behaviors. 2019; 89:1–4. [DOI] [PubMed] [Google Scholar]
- 9.Cummins SE, Zhu SH, Tedeschi GJ, Gamst AC, Myers MG. Use of e-cigarettes by individuals with mental health conditions. Tobacco Control. 2014;23 Suppl 3(Suppl 3):iii48–iii53. [DOI] [PMC free article] [PubMed] [Google Scholar]


