ABSTRACT
Transrenal urine cell-free DNA (cfDNA) is a promising tuberculosis (TB) biomarker, but is challenging to detect because of the short length (<100 bp) and low concentration of TB-specific fragments. We aimed to improve the diagnostic sensitivity of TB urine cfDNA by increasing recovery of short fragments during sample preparation. We developed a highly sensitive sequence-specific purification method that uses hybridization probes immobilized on magnetic beads to capture short TB cfDNA (50 bp) with 91.8% average efficiency. Combined with short-target PCR, the assay limit of detection was ≤5 copies of cfDNA in 10 ml urine. In a clinical cohort study in South Africa, our urine cfDNA assay had 83.7% sensitivity (95% CI: 71.0 to 91.5%) and 100% specificity (95% CI: 86.2 to 100%) for diagnosis of active pulmonary TB when using sputum Xpert MTB/RIF as the reference standard. The detected cfDNA concentration was 0.14 to 2,804 copies/ml (median 14.6 copies/ml) and was inversely correlated with CD4 count and days to culture positivity. Sensitivity was nonsignificantly higher in HIV-positive (88.2%) compared to HIV-negative patients (73.3%), and was not dependent on CD4 count. Sensitivity remained high in sputum smear-negative (76.0%) and urine lipoarabinomannan (LAM)-negative (76.5%) patients. With improved sample preparation, urine cfDNA is a viable biomarker for TB diagnosis. Our assay has the highest reported accuracy of any TB urine cfDNA test to date and has the potential to enable rapid non-sputum-based TB diagnosis across key underserved patient populations.
KEYWORDS: DNA hybridization, DNA purification, PCR, cell-free DNA, diagnostics, sample preparation, transrenal DNA, tuberculosis, urine
INTRODUCTION
Tuberculosis (TB) is the leading cause of global mortality due to infectious disease, with an estimated 10 million cases and 1.4 million deaths in 2019 (1). An estimated 30% of TB cases remain undiagnosed or unreported, in part due to limitations in rapid diagnostics (1). Current TB tests rely on sputum samples, which are difficult to collect from people living with HIV, severely ill patients, and children, and may not detect extrapulmonary TB (EPTB). Rapid sputum-based tests (e.g., smear microscopy, Xpert MTB/RIF) also have lower sensitivity in these same underserved patient populations, who more often have paucibacillary TB (2–4). A WHO consensus meeting identified a rapid, non-sputum-based test as one of the highest priority target products for TB diagnostics (5).
Urine is an attractive alternate sample for TB diagnosis because it is easy to collect and poses minimal TB transmission risk. In patients with active TB disease, TB-specific cell-free DNA (cfDNA) fragments are released into the blood, a fraction of which are filtered through the kidneys and excreted in the urine as transrenal cfDNA (6–8). TB-specific cfDNA has been detected in urine from both HIV-negative and HIV-positive patients with pulmonary TB, but diagnostic sensitivities have been inconsistent (0 to 79%) (8–13). High variability in methodology and subsequent performance across studies have limited the understanding of TB urine cfDNA and hindered its clinical implementation (14, 15).
Urine cfDNA is a challenging target due to the short length and low concentration of TB-specific fragments. While plasma cfDNA has a peak fragment length of 167 base pairs (bp), urine cfDNA is more fragmented (7, 16, 17). Recently, new sequencing library preparation methods revealed that very short, formerly undetectable fragments compose a larger fraction of cfDNA than previously realized (18–21). The majority of urine cfDNA fragments, regardless of origin, are <100 bp, with the peak fragment length ranging from 30 to 110 bp (16, 17, 21, 22). Although the fragment length of TB cfDNA specifically has not yet been characterized, bacterial cfDNA is expected to be especially fragmented (peak <60 bp) because it is less protected by DNA-associated proteins than human cfDNA (21, 23).
The low-to-moderate sensitivities reported in previous TB urine cfDNA studies are likely due in part to sample preparation and/or amplification methods that are suboptimal for short urine cfDNA (6, 14). We hypothesized that we could increase the sensitivity of cfDNA-based TB diagnosis by improving recovery of short cfDNA during the DNA extraction step. We developed a highly sensitive sequence-specific purification method that uses DNA probes immobilized on magnetic beads to extract TB-specific cfDNA via hybridization. By combining sequence-specific purification with short-target PCR, we can reliably detect ≤5 copies of short (50 bp) cfDNA in 10 ml urine (24).
Here, we determined for the first time the diagnostic accuracy of our TB cfDNA assay in clinical urine specimens from adults with active pulmonary TB. Our results demonstrate the advantages of our sequence-specific purification approach, contribute to the growing evidence needed to establish urine cfDNA as a TB biomarker, and will serve as the foundation for future clinical studies in expanded populations (e.g., children, individuals with EPTB).
MATERIALS AND METHODS
Study design and participants.
Participants were consecutively enrolled at Edendale Hospital in Pietermaritzburg, South Africa (approved by the University of KwaZulu-Natal Biomedical Research Ethics Committee, number BE475/18). Adults (≥18 years old) meeting the case definition for active pulmonary TB were recruited. As a control group, adult inpatients at Edendale Hospital with excluded diagnosis for active TB disease were concurrently enrolled. The characteristics of the South Africa control group closely matched the TB-positive study population (i.e., patients seeking hospital care, many HIV-positive, likely included participants with latent TB and Bacillus Calmette–Guérin vaccination). Because the TB burden at the enrollment site in South Africa is high, however, there was a risk of enrolling patients with undiagnosed TB in the control group. To differentiate any potential false positives due to undiagnosed TB, a separate healthy control group was enrolled at the University of Washington, Seattle, USA (approved by the University of Washington Institutional Review Board, number 48840). Participants were adults (≥18 years old) with low risk of TB exposure, as defined by birth in a country with low TB risk and no history of diagnosis of latent TB, treatment for active or latent TB, or living with an individual with active TB. All participants provided written informed consent. Samples were deidentified prior to testing at the University of Washington, where this study was conducted.
Case definitions.
TB-positive participants (South Africa) were defined as those with a positive sputum Xpert MTB/RIF (Cepheid, Sunnyvale, CA, USA) result within 5 days of enrollment and the presence of one or more TB symptoms (fever, night sweats, cough, and/or weight loss). Xpert MTB/RIF rather than Xpert MTB/RIF Ultra was used as the reference standard because Xpert MTB/RIF Ultra cartridges were not available at Edendale Hospital, a regional health care facility, at the time of participant enrollment (February to July 2019). Patients with >72 h of anti-TB treatment were excluded. TB-negative participants (South Africa) had a primary diagnosis other than TB and no clinical suspicion for TB. Healthy controls (USA) were recruited on a volunteer basis and were not seeking medical care.
Clinical data, sputum testing, and urine lipoarabinomannan (LAM) testing.
Clinical data were collected for all participants enrolled in South Africa. These included date of birth, gender, weight, height, self-reported TB history, presence of TB symptoms (fever, night sweats, cough, and/or weight loss), TB treatment duration, HIV test result, and CD4+ cell count (for participants living with HIV only). Expectorated sputum was submitted to the South African National Health Laboratory System (NHLS) for confirmatory solid and liquid mycobacterial culture and acid-fast bacilli (AFB) smear microscopy. Mycobacterial culture was performed at the NHLS Provincial TB Reference Laboratory using both Middlebrook 7H11 solid agar medium and the liquid Bactec mycobacterial growth indicator tube (MGIT) 960 system (BD, Franklin Lakes, NJ, USA) for each sputum sample. Cultures were incubated for up to 42 days. Culture plates were read at 3 and 6 weeks, and Mycobacterium tuberculosis was identified from solid or liquid cultures using niacin and nitrate testing. Participants were considered culture-positive with growth from either the solid or liquid culture. Smear microscopy was performed in the NHLS Laboratory at Edendale Hospital on decontaminated samples using both Ziehl-Neelsen and Auramine stains and considered positive if either stain revealed AFB. Urine (60 μl) was tested using Alere Determine TB LAM Ag (Abbott Laboratories, Chicago, USA). Collection of clinical data, sputum testing, and urine LAM testing were not done for healthy controls enrolled in the USA.
Urine collection and storage for cfDNA analysis.
Participants were asked to provide a convenience urine sample (50 to 200 ml) at the time of enrollment and/or an early morning first-void sample the morning after enrollment. The samples were not obtained midstream. As soon as possible after collection, urine was mixed with EDTA and Tris-HCl pH 7.5 to final concentrations of 25 mM and 10 mM, respectively. Urine was stored in DNA LoBind tubes (Eppendorf, Hamburg, Germany) at −20°C at the collection site until shipping. Samples were shipped on dry ice to the University of Washington, where they were stored at −80°C until analysis. Immediately before analysis, urine was thawed at 37°C and centrifuged at 8,000 × g for 5 min to pellet cell debris. The cell-free urine supernatant was transferred to new 15-ml DNA LoBind tubes (Eppendorf) and characterized using Fisherbrand 10-SG Urine Reagent Strips (Thermo Fisher Scientific, Waltham, MA, USA) to measure the levels of glucose, bilirubin, ketone, specific gravity, blood, pH, protein, urobilinogen, nitrite, and leukocytes.
Purification of TB cfDNA from urine using sequence-specific hybridization capture.
Transrenal urine cell-free DNA (cfDNA) was extracted in triplicate from 10-ml urine samples (3 × 10-ml samples for each participant), with individual replicates for each participant processed on separate days. TB-specific urine cfDNA was extracted using our in-house sequence-specific hybridization capture method, as described previously (24). We have published a detailed, user-ready protocol at http://dx.doi.org/10.17504/protocols.io.bep4jdqw.
Immobilization of capture probes on magnetic beads. Dynabeads MyOne Streptavidin C1 (Thermo Fisher) were washed three times with an equal volume of high-salt wash buffer (1 M NaCl, 10 mM Tris-HCl [pH 8.0], 0.05% [vol/vol] Tween 20) and resuspended in an equal volume of high-salt wash buffer. Dual biotinylated capture probes BP1 and BP2 (Table 1), targeting opposite strands of the double-stranded IS6110 target region, were premixed in low-EDTA Tris-EDTA (TE) buffer to a concentration of 50 μM each. Then, 25 pmol of each probe (0.5 μl of probe mix) per 50 μl bead equivalent was added to the beads. The beads were immediately vortexed and rotated for 15 min at room temperature to immobilize capture probes on the beads. The beads were washed three times with an equal volume of high-salt wash buffer and resuspended in an equal volume of high-salt wash buffer.
TABLE 1.
Probe, primer, and target sequences
| Oligonucleotide | Sequencea |
|---|---|
| Dual biotinylated capture probe number 1 (BP1) | 5′-/52-Bio/AAAAAAAAAAAAAAAAAAAACAGACCTCACCTATGTGT/3SpC3/-3′ |
| Dual biotinylated capture probe number 2 (BP2)b | 5′-/52-Bio/AAAAAAAAAAAAAAAAAAAACCCTGCCCAGGTCGA/3SpC3/-3′ |
| Forward primer | 5′-CGAACCCTGCCCAGGTCGA-3′ |
| Reverse primer | 5′-GTA+GCAGA+CCTCACCTATGTGT-3′ |
| IS6110 target (40 bp) | 5′-CGAACCCTGCCCAGGTCGACACATAGGTGAGGTCTGCTAC-3′ |
| IS6110 reverse complement (40 bp) | 5′-GTAGCAGACCTCACCTATGTGTCGACCTGGGCAGGGTTCG-3′ |
| Synthetic positive control (50 bp) | 5′-CGAACCCTGCCCAGGTCGACACCATTCAACACATAGGTGAGGTCTGCTAC-3′ |
| Synthetic positive control reverse complement (50 bp) | 5′-GTAGCAGACCTCACCTATGTGTTGAATGGTGTCGACCTGGGCAGGGTTCG-3′ |
/52-Bio/ indicates dual biotin modification; /3SpC3/indicates carbon spacer; “+X” indicates LNA base. Target-specific probe binding sequences are underlined. A synthetic spacer region introduced to differentiate the synthetic positive control from the endogenous Mycobacterium tuberculosis complex-specific target sequence (IS6110) is in boldface. All DNA sequences were ordered HPLC-purified from Integrated DNA Technologies (Coralville, IA, USA).
BP2 targets the opposite strand (reverse complement) of the DNA strand targeted by BP1.
Sequence-specific capture of TB cfDNA. Aliquots of 2.5 ml of 5 M NaCl (final concentration 1 M), 127 μl of 10% (vol/vol) Tween 20 (final concentration 0.1%), and 50 μl of prepared beads were added to each 10-ml urine sample and gently mixed. The samples were denatured in a heat block set to 120°C for 15 min, so that the urine reached a temperature of >90°C. TB cfDNA was hybridized to capture probes by rotation at room temperature for 30 min.
Washing to remove urine and non-target DNA. Samples were centrifuged for 5 min at 5,000 × g to pellet beads. All but 1 ml of supernatant was removed and discarded. Beads were resuspended in the remaining supernatant and transferred to 1.5-ml DNA LoBind tubes (Eppendorf). The tubes were placed on an Invitrogen Dynamag-2 magnetic rack (Thermo Fisher) for 1 min and the remaining supernatant was discarded. The beads were washed twice with 1 ml high-salt wash buffer and once with 1 ml low-salt wash buffer (15 mM NaCl, 10 mM Tris-HCl [pH 8.0]). For each wash, the tubes were inverted 10 to 20 times, or until no bead aggregate was left on the tube walls, briefly spun down, and placed on the magnetic rack for 1 min before removing the wash buffer. After the final wash step, beads were spun down and any residual buffer was removed.
Elution of purified TB cfDNA. Purified TB cfDNA was eluted using 20 μl of freshly prepared 20 mM NaOH. Beads were mixed with NaOH by vortexing, briefly spun down, and placed on the magnetic rack. The eluate was transferred directly to PCR wells and partially neutralized with 3.5 μl 100 mM HCl.
Amplification of TB-specific urine cfDNA using short-target PCR.
The entire output (∼24 μl) from each 10-ml urine sample was analyzed in a single PCR well. Each 50-μl reaction contained 1.25 U OneTaq Hot Start DNA polymerase (New England BioLabs [NEB], Ipswitch, MA, USA), 1× OneTaq GC reaction buffer (NEB) (80 mM Tris-SO4, 20 mM [NH4]2SO4, 2 mM MgSO4, 5% glycerol, 5% dimethyl sulfoxide, 0.06% IGEPAL CA-630, and 0.05% Tween 20, pH 9.2), 0.8 mM dNTPs (NEB), 0.4× EvaGreen (Biotium, Fremont, CA, USA), 200 nM forward primer (Table 1), and 200 mM reverse primer (Table 1). Quantitative PCR (qPCR) was carried out in a CFX96 Touch real-time PCR detection system (Bio-Rad Laboratories, Hercules, CA, USA) using an initial incubation period of 94°C for 3 min, followed by 45 amplification cycles of 94°C for 30 s, 64°C for 30 s, and 68°C for 1 min. Quantification cycle (Cq) values were determined using the CFX Maestro software version 1.1 (Bio-Rad Laboratories) at a threshold of 500 relative fluorescent units (RFU) and recovered copies were calculated using a standard curve run with each PCR. PCR products were confirmed by postamplification melt curve analysis from 65°C to 95°C in 0.5°C increments every 5 s.
Criteria for positive samples.
Criteria for positive samples were set prior to analysis, and the assay operator was blinded to the clinical status of the samples until after processing was complete and sample calls were made. Individual replicates were ruled as positive if ≥1 single-stranded DNA copy of TB cfDNA was detected and the melt temperature (Tm) matched that of the expected native TB amplicon (76°C). Individual replicates were ruled as negative if insufficient TB cfDNA was detected (<1 copy of single-stranded DNA) and/or the Tm did not match that of the expected native TB amplicon. To allow for expected occasional PCR drop-out of low-concentration samples, a sample was ruled as positive if at least two of three replicates, analyzed on different days, were positive based on the above definitions. Samples with zero or one positive replicates were ruled as negative.
PCR primer design, controls, and precautions to prevent false positives.
We designed PCR primers targeting the insertion sequence IS6110, which is an established target for TB diagnosis present at multiple, variable copy number across ∼99% of Mycobacterium tuberculosis complex strains (25). Our PCR primers (Table 1) amplify a short 40-bp target within a subregion of IS6110 that is conserved and specific to the Mycobacterium tuberculosis (MTB) complex (26). To avoid false positives due to nonspecific amplification, we used locked nucleic acid (LNA) bases to precisely match the Tm of the primers and selected an annealing temperature (Ta) slightly above the primer Tm to encourage specific amplification without compromising amplification efficiency. The final primer set and optimized PCR conditions result in an average PCR efficiency of 97.1% (95% confidence interval [CI]: 95.7 to 98.6%) and no amplification of no-template controls (NTCs) or 10 ng of human genomic DNA up to at least 45 cycles. To avoid false positives due to contamination, we maintained good laboratory practices to limit contamination (e.g., separating pre- and post-PCR rooms, regular decontamination of work surfaces and pipettes, sterile filtered pipette tips, aliquoting reagents into single-use volumes). In addition, we designed the synthetic positive control (50 bp, used as a spike-in control during extraction and for PCR standard curves) to be amplifiable by the same primer pair but distinguishable from the endogenous TB target sequence (40 bp) by melt analysis (Table 1) so that any potential contamination with the positive control would not result in false positives. Every experiment included a positive control (pooled TB-negative urine spiked with 103 copies of double-stranded DNA synthetic positive-control template [Table 1]) and a negative control (water without spiked target) that were run throughout the extraction process alongside clinical urine samples. PCR NTCs (n = 3) were also included in each experiment.
Statistical analysis.
Sensitivity and specificity were calculated using a positive sputum Xpert MTB/RIF result and the presence of one or more TB symptoms as the reference standard. The 95% confidence intervals for sensitivity and specificity were calculated using the hybrid Wilson/Brown method. Sensitivities were compared across groups using Fisher’s exact test. The detected cfDNA concentration was calculated based on the sample means of cfDNA-positive samples. Detected cfDNA concentrations were compared across groups using the Mann-Whitney test. Correlations with detected cfDNA concentration were assessed using Spearman’s correlation coefficient. Odds ratios were compared to a value of 1 using Fisher’s exact test, with 95% confidence intervals determined using the Baptista-Pike method. All statistical analysis was conducted using GraphPad Prism v8.1.2 (San Diego, CA, USA) with a significance level of 0.05.
RESULTS
Analytical performance of sequence-specific TB cfDNA assay.
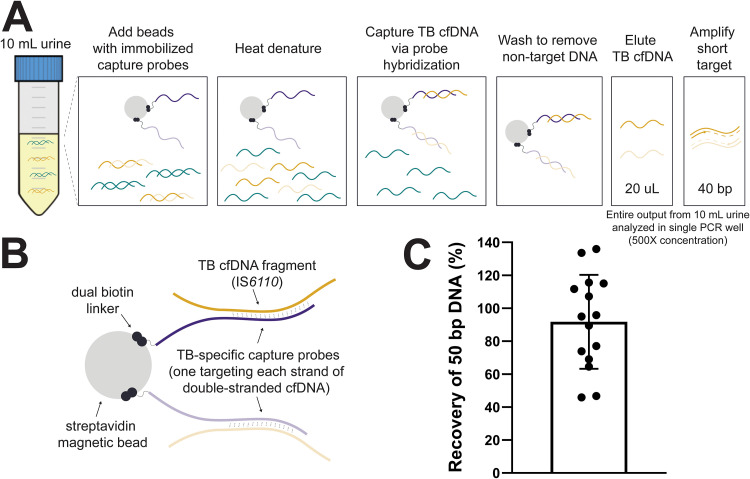
An overview of our cfDNA assay is shown in Fig. 1A and B. Recovery of the spiked-in positive control was 91.8% (95% CI: 75.9 to 107.6%) across 15 independent experiments (Fig. 1C).
FIG 1.
Capture and detection of short cfDNA fragments in urine using sequence-specific purification and short-target PCR. (A) Overview of sequence-specific purification and short-target PCR (40 bp) protocol for TB cfDNA. (B) Schematic illustrating details of capture probe design targeting the MTB complex-specific insertion element IS6110. (C) Near-complete recovery of short TB-specific DNA spiked into urine using sequence-specific purification. A positive control (103 copies of 50-bp double-stranded DNA in 10 ml pooled urine) was included throughout each experiment alongside clinical samples. The recovery of the positive control was calculated as a percentage of the input (mean ± standard deviation [SD], n = 15). Key design features, assay optimization, and additional analytical characterization of our sequence-specific purification method for cfDNA are reported in reference 24.
Study participants.
We enrolled 73 participants across two sites, the Edendale Hospital in South Africa (49 TB-positive, 10 TB-negative) and the University of Washington in the USA (14 healthy controls with low risk of TB exposure). Participant demographic and clinical data are summarized in Table 2.
TABLE 2.
Summary of study participantse
| Parameter | TB-positivea patients (South Africa) | TB-negative controls (South Africa) | Healthy controls (USA) |
|---|---|---|---|
| Total (no.) | 49 | 10 | 14 |
| Female (no. [%]) | 22 (44.9%) | 8 (80.0%) | 5 (35.7%) |
| Male (no. [%]) | 27 (55.1%) | 2 (20.0%) | 9 (64.3%) |
| Age, median yrs (IQR) | 38 (31–48) | 32 (30.25–37.25) | 26.5 (24–28.75) |
| Height, median m (IQR) | 1.68 (1.65–1.70) | 1.60 (1.59–1.68) | NA |
| Weight, median kg (IQR) | 55 (48–63) | 57 (52–70) | NA |
| HIV status (no. [%]) | |||
| HIV-positive | 34 (69.4%) | 10 (100.0%) | NA |
| HIV-negative | 15 (30.6%) | 0 (0.0%) | NA |
| CD4+ T-cell count median cells/mm3b (IQR) | 85 (42–345) | 318 (257–746) | NA |
| History of prior TB (no. [%]) | |||
| No | 32 (65.3%) | 6 (60.0%) | 14 (100.0%) |
| Yes | 17 (34.7%) | 4 (40.0%) | 0 (0.0%) |
| TB treatment status (no. [%]) | |||
| Treatment-naïve | 36 (73.5%) | NA | NA |
| Some treatmentc | 13 (26.5%) | NA | NA |
| TB culture result (no. [%]) | |||
| Culture-positive | 34 (69.4%) | 0 | NA |
| Culture-negative | 8 (16.3%) | 9 (90.0%) | NA |
| No culture result | 7 (14.3%) | 1 (10.0%) | NA |
| Days to culture positivityd (median [IQR]) | 13.5 (8.0–17.0) | NA | NA |
| AFB smear result (no. [%]) | |||
| Smear-positive | 19 (38.8%) | 0 (0.0%) | NA |
| Smear-negative | 25 (51.0%) | 5 (50.0%) | NA |
| No smear result | 5 (10.2%) | 5 (50.0%) | NA |
| Alere urine LAM result (no. [%]) | |||
| LAM-positive | 15 (30.6%) | 0 (0.0%) | NA |
| LAM-negative | 34 (69.4%) | 10 (100.0%) | NA |
TB-positive patients were defined as those with a positive Xpert MTB/RIF result and the presence of one or more TB symptoms.
CD4 count was measured for HIV-positive patients only.
All participants had ≤72 h of treatment.
For mycobacterial growth indicator tube (MGIT) culture only.
TB, tuberculosis; AFB, acid-fast bacilli; LAM, lipoarabinomannan; NA, not applicable.
Sensitivity and specificity of sequence-specific TB cfDNA assay.
A summary of the diagnostic accuracy of our TB urine cfDNA assay is given in Table 3. Full results for each participant, including paired clinical data, urine characteristics, and detected cfDNA concentration, are given in Data Set S1 in the supplemental material. Using sputum Xpert MTB/RIF as the reference standard, we detected TB-specific urine cfDNA with 83.7% sensitivity (n = 41/49; 95% CI: 71.0 to 91.5%) and 100% specificity (n = 24/24; 95% CI: 86.2 to 100%). No TB-specific cfDNA was detected in the urine of TB-negative controls in South Africa (n = 10) or healthy controls in the USA (n = 14).
TABLE 3.
Sensitivity and specificity of TB urine cfDNA assaye
| Parameter | No. cfDNA-positive/no. TB-positive | % Sensitivity (95% CIa) | No. cfDNA-negative/no. TB-negative | % Specificity (95% CIa) |
|---|---|---|---|---|
| Totalb | 41/49 | 83.7 (71.0–91.5) | 24/24 | 100 (86.2–100) |
| HIV status | ||||
| HIV-positive | 30/34 | 88.2 (73.4–95.3) | 10/10 | 100 (72.3–100) |
| HIV-negative | 11/15 | 73.3 (48.1–89.1) | 0/0 | NA |
| CD4+ countc | ||||
| ≤200 cells/mm3 | 20/22 | 90.9 (72.2–99.4) | 1/1 | 100 (51.0–100) |
| >200 cells/mm3 | 10/12 | 83.3 (55.2–97.0) | 9/9 | 100 (70.1–100) |
| Sputum culture result | ||||
| Positive | 30/34 | 88.2 (73.4–95.3) | 0/0 | NA |
| Negative | 6/8 | 75.0 (40.9–95.6) | 9/9 | 100 (70.1–100) |
| AFB sputum smear result | ||||
| Positive | 19/19 | 100 (83.2–100) | 0/0 | NA |
| Negative | 19/25 | 76.0 (56.6–88.5) | 5/5 | 100 (56.6–100) |
| Alere urine LAM result | ||||
| Positive | 15/15 | 100 (79.6–100) | 0/0 | NA |
| Negative | 26/34 | 76.5 (60.0–87.6) | 10/10 | 100 (72.3–100) |
| TB treatment status | ||||
| Treatment-naïve | 28/36 | 77.8 (61.9–88.3) | 10/10 | 100 (72.3–100) |
| Some treatmentd | 13/13 | 100 (77.2–100) | 0/0 | NA |
| Genderb | ||||
| Female | 18/22 | 81.8 (61.5–92.7) | 13/13 | 100 (77.2–100) |
| Male | 23/27 | 85.2 (67.5–94.1) | 11/11 | 100 (74.1–100) |
95% confidence intervals for sensitivity and specificity were calculated using the hybrid Wilson/Brown method.
Healthy controls enrolled in the USA were included in total specificity and gender-specific specificity, but not in the remaining specificities.
CD4 count was measured for HIV-positive patients only.
All participants had ≤72 h of treatment.
TB, tuberculosis; AFB, acid-fast bacilli; LAM, lipoarabinomannan; cfDNA, cell-free DNA; NA, not applicable.
Sensitivity was nonsignificantly higher in HIV-positive patients compared to HIV-negative patients (88.2% [n = 30/34; 95% CI: 73.4 to 95.3%] versus 73.3% [n = 11/15; 95% CI: 48.1 to 89.1%]; P = 0.23). Sensitivity was similar in HIV-positive patients with CD4 counts of ≤200 and >200 cells/mm3 (90.9% [n = 20/22; 95% CI: 72.2 to 99.4%] versus 83.3% [n = 10/12; 95% CI: 55.2 to 97.0%]; P = 0.60). Sensitivity was 77.8% (n = 28/36; 95% CI: 61.9 to 88.3%) in treatment-naive patients. If a positive sputum culture result was also required for the TB case definition, total sensitivity increased to 88.2% (n = 30/34; 95% CI: 73.4 to 95.3%). We detected TB-specific cfDNA in the urine of all patients with positive AFB sputum smear (n = 19/19) and/or Alere urine LAM (n = 15/15) results. Sensitivity remained high in smear-negative (76.0% [n = 19/25; 95% CI: 56.6 to 88.5%]) and LAM-negative (76.5% [n = 26/34; 95% CI: 60.0 to 87.6%]) patients. The reduction in sensitivity for smear-negative patients compared to smear-positive patients was significant (P = 0.029), while that for LAM-negative compared to LAM-positive patients was not (P = 0.087). See Table S1 for statistical analysis of sensitivity across groups. Due to the relatively small sample size of this study, the power of these subgroup comparisons was limited and the statistical analyses should be interpreted accordingly. Subsequent, more highly powered studies are needed to conclusively compare cfDNA detection sensitivity across subgroups.
We evaluated factors associated with TB cfDNA positivity and found that only a positive AFB smear result was significantly associated with a positive TB cfDNA result (odds ratio >1, P = 0.029). HIV status, CD4 count, treatment status, culture result, and LAM result were not significantly associated with a positive urine cfDNA result (Table S2).
Quantification of TB-specific cfDNA concentration in urine.
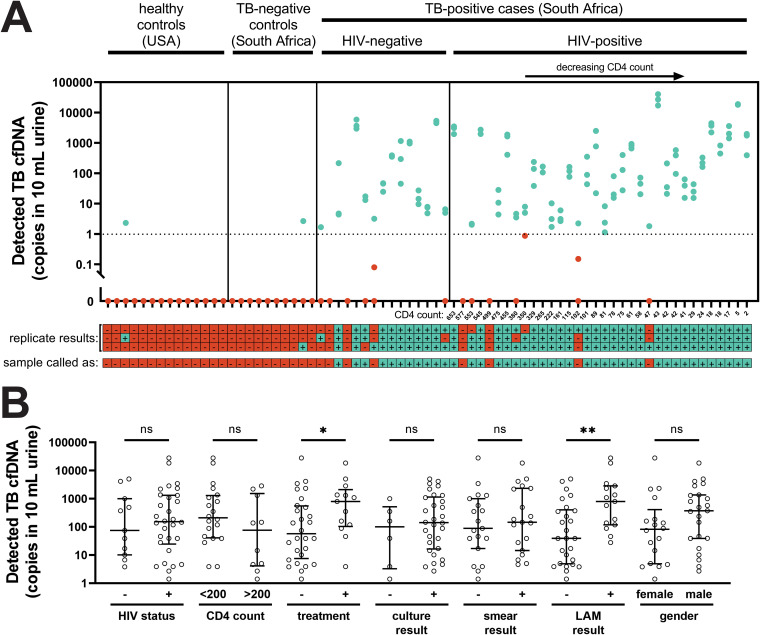
The detected TB-specific cfDNA concentration was variable and skewed toward low concentrations, with a median of 146 copies in 10 ml urine (Table 4). The cfDNA concentration had a moderate inverse correlation with CD4 count (−0.43 [95% CI: −0.68 to −0.10; P = 0.011]) (Fig. 2A) and days to culture positivity (−0.36 [95% CI: −0.64 to −0.0060; P = 0.041]) (Fig. S1), but no significant correlation with days of anti-TB treatment (1 to 3 days), AFB smear score, or Alere urine LAM score (Table S3). The cfDNA concentration was higher in patients with some treatment compared to treatment-naive patients (P = 0.045) and in urine LAM-positive patients compared to urine LAM-negative patients (P = 0.0045), but was not significantly different in patients grouped by HIV status, CD4 count, culture result, smear result, or gender (Fig. 2B).
TABLE 4.
Detected concentrations of TB-specific urine cfDNA
| Patient group | Median no. copies in 10 ml urine (IQR)a | Range of copies in 10 ml urinea |
|---|---|---|
| Total | 146 (17–1,092) | 1.4–28,044 |
| TB treatment statusb | ||
| Treatment-naïve | 57 (7.6–557) | 1.4–28,044 |
| Some treatmentc | 796 (104–2,111) | 3.9–18,543 |
| Alere urine LAM resultd | ||
| Positive | 796 (119–2,851) | 28–28,044 |
| Negative | 39 (4.9–404) | 1.4–5,021 |
Concentration for each sample is given as copies of single-stranded DNA in 10 ml urine, which was calculated based on the mean across n = 3 technical replicates.
Detected cfDNA concentration was higher in patients with some treatment (Mann-Whitney, p = 0.045).
All participants had ≤72 h of treatment.
Detected cfDNA concentration was higher in patients with a positive urine LAM result (Mann-Whitney, p = 0.0045).
FIG 2.
Detected concentrations of TB-specific urine cfDNA. (A) Concentration of TB cfDNA detected in each participant’s urine, stratified by HIV status and ranked by CD4 count. There was a moderate inverse correlation between CD4 count and detected TB cfDNA concentration (Spearman’s r = −0.43 [95% CI: −0.68 to −0.10], P = 0.011), but TB cfDNA could be detected regardless of HIV status and CD4 count. Each dot represents one of three replicates processed on different days for each sample. Note that dots representing replicates with similar detected concentrations may overlap. Replicates called as positive are shown in cyan and replicates called as negative are shown in red. The dashed line indicates the 1 copy per 10 ml threshold used to define positive replicates. The legend below the plot indicates cfDNA detection status by replicate (considered positive if ≥1 copy of single-stranded DNA was detected with melt temperature matching that of the expected IS6110 amplicon) and by sample (considered positive if ≥2 of 3 replicates were positive). (B) Comparison of detected TB cfDNA concentration across groups (bars indicate median and interquartile range [IQR] of sample means of cfDNA-positive samples). The detected TB cfDNA concentration was significantly higher in patients with some treatment compared to treatment-naive patients, and in LAM-positive patients compared to LAM-negative patients (* indicates Mann-Whitney P < 0.05; ** indicates Mann-Whitney P < 0.01), but was not affected by HIV status, CD4 count, culture result, smear result, or gender (ns indicates not significant). See Table S4 for calculated P values for each comparison.
DISCUSSION
Improved detection of short cfDNA in urine using sequence-specific purification.
To maximize sensitivity of TB urine cfDNA detection, it is essential to use methods designed to detect low concentrations of short fragments (6, 14, 15). Decreasing the minimum target length is expected to improve cfDNA diagnostic sensitivity (8, 27–29). For example, decreasing PCR amplicon length by a modest 10 bp (49 bp to 39 bp) led to more than 10-fold increase in detected TB-specific cfDNA (29). Critically, in addition to amplifying short targets, sample preparation methods must also extract short cfDNA from urine with high efficiency. Conventional silica-based DNA extraction methods have lower recovery of short fragments and are thus not optimal for urine cfDNA (30).
We aimed to increase the diagnostic sensitivity of TB urine cfDNA detection by improving recovery of short cfDNA during the DNA extraction step. We developed a sequence-specific purification method that uses hybridization capture probes immobilized on magnetic beads to extract short cfDNA with high analytical sensitivity. We have previously demonstrated that sequence-specific purification improves recovery of short cfDNA fragments (25 to 150 bp) from urine compared to alternate urine cfDNA extraction methods, including a protocol used for TB urine cfDNA (31). In a recent paper detailing our sequence-specific purification method, we described its key features, provided a user-ready protocol, and thoroughly characterized its analytical performance (24). In this study, our sequence-specific approach recovered nearly all target-specific 50-bp positive-control DNA (91.8% average recovery) and was in some clinical specimens able to detect down to a single copy of TB cfDNA in 10 ml of urine.
Diagnostic accuracy and comparison to previous TB urine cfDNA studies.
In this study, we tested our sequence-specific TB cfDNA assay in clinical urine specimens for the first time. The sensitivity and specificity of our assay for diagnosis of active pulmonary TB were 84% and 100%, respectively, the highest reported diagnostic accuracy of a TB cfDNA test. For comparison, previous TB urine cfDNA studies are summarized in Table 5 (8–12). For a comprehensive review of previous studies, refer to reference 14.
TABLE 5.
Comparison to previous studies targeting urine cfDNA for pulmonary TB diagnosisa
| First author | Year | DNA extraction |
PCR amplicon length (bp) | Effective urine vol analyzed (ml)b | Proportion of smear-negative participantsc | % Sensitivity (proportion) |
% Specificity (proportion) | ||
|---|---|---|---|---|---|---|---|---|---|
| Method | Designed for short urine cfDNA? | HIV-negative patients | HIV-positive patients | ||||||
| Cannas (8) | 2008 | Wizard silica resin | Claimed, but we have identified limitations (<35% recovery of ≤150-bp DNA)d | 129/67 (nested) | 0.35 | 2/43 | 79 (34/43) | 100 (23/23) | |
| Peter (12)e | 2012 | Xpert cartridge | No | 192 (Xpert) | NR | NR | NA | 8 (3/38) | NA |
| Fortún (13) | 2014 | NR | No | NR (AMTD) | NR | NR | 18 (5/28) | NA | |
| Bordelon (11) | 2017 | Dynabeads MyOne Silane | No | 67 | 0.1–0.5 | NR | 0 (0/33) | 0 (0/31) | |
| Labugger (9) | 2017 | Unspecified silica resinf | Claimed (33% recovery of 75-bp DNA)g | 38 | 1.6 | 4/10 | 64 (7/11) | NA | 100 (8/8) |
| Patel (10) | 2018 | Unspecified silica resinf | Claimed (∼50% recovery of gDNA)h | 38 | NR | 45/175 | 40 (36/90) | 45 (38/84) | 89 (210/237) |
| Oreskovic (this study) | 2021 | Sequence-specific purification | Yes (>90% recovery of 50-bp DNA) | 40 | 10 | 30/49 | 73 (11/15) | 88 (30/34) | 100 (24/24) |
Included studies specifically targeted urine cell-free DNA for pulmonary TB diagnosis. Studies analyzing cell-associated DNA, plasma cfDNA, or EPTB were excluded. Studies targeting plasma cfDNA were excluded here but reported 65%/93% (50), 29%/100% (50), and 45%/67% (51) sensitivity/specificity. NR, not reported; NA, not applicable; Xpert, Xpert MTB/RIF assay (Cepheid); AMTD, amplified Mycobacterium tuberculosis direct test (Hologic); gDNA, TB genomic DNA.
Calculated based on the urine input volume, elution volume, and PCR input volume.
Given as proportion of TB-positive participants who had a negative sputum smear microscopy result. cfDNA detection sensitivity may be lower in smear-negative patients compared to smear-positive patients.
We found that the Wizard silica method had low recovery of short fragments (<35% for 40–150 bp) and was dependent on urine composition (i.e., pH and nontarget DNA concentration) (31).
Peter et al. tested both whole urine and the insoluble fraction of urine concentrated by centrifugation. Only results from whole urine testing are listed here because cfDNA is expected to be in the soluble fraction of centrifuged urine.
Labugger et al. and Patel et al. used a silica resin-based method similar to that used by Cannas et al., but did not specify the resin or binding buffer.
Estimated based on the reported average of 1.6 cycle delay for extraction calibration curves compared to PCR calibration curves for genomic DNA and a 75-bp target.
Estimated based on reported approximate 1 cycle delay for extraction calibration curves compared to PCR calibration curves for genomic DNA.
Prior studies showed potential for detection of TB-specific urine cfDNA in HIV-positive and HIV-negative patients, but had variable sensitivity due to sample preparation and/or amplification methods suboptimal for short targets (6, 14, 15). Cannas et al. used an in-house silica resin method (based on Promega Wizard DNA purification resin) reportedly designed to improve binding of short cfDNA, but did not report its analytical performance (e.g., percent recovery) (8). While the Wizard method improves upon conventional silica-based methods, our past testing revealed limited recovery (<35%) of ≤150-bp fragments (31). It was also highly dependent on urine composition and is likely to fail in samples with high pH and/or low non-target-DNA concentrations (31). Labugger et al. and Patel et al. used a similar silica resin-based method, but did not specify the resin or binding conditions (9, 10). It is possible that their method suffers from similar limitations as the Wizard method used by Cannas et al., although we could not experimentally verify this. They reported recoveries of approximately 30 to 50% and limits of detection of 3 copies/ml (75-bp target) (9) and 1.25 copies/ml (TB gDNA containing up to 42 target repeats) (10). Our sequence-specific purification method increases percent recovery by 2-fold or more and improves the limit of detection to ≤0.5 copies/ml of 50-bp cfDNA (with a positivity cutoff threshold of 0.1 copies/ml used here). Our method allows the full volume eluted from a 10-ml urine extraction to be amplified in a single PCR well, maximizing sensitivity for detection of low-concentration samples.
Past studies also enrolled few smear-negative participants, and thus have not tested the ability to detect urine cfDNA in individuals with paucibacillary TB who stand to benefit most from a non-sputum-based test. In particular, the most promising study by Cannas et al. included only 5% (2/43) smear-negative participants (8). Our results indicate that cfDNA detection sensitivity is higher in smear-positive compared to smear-negative individuals, so enrollment biased toward smear-positive participants may lead to an overestimation of assay sensitivity. In contrast, we demonstrated higher sensitivity while including 61% (30/49) smear-negative participants. Because Xpert MTB/RIF has reduced sensitivity (67%, pooled) in smear-negative, culture-positive sputum samples (2), our study is still limited in that it likely does not include Xpert-negative individuals with the lowest sputum bacterial loads.
Although not directly tested here, an added benefit of our sequence-specific approach is that it may help ensure specificity by removing nontarget DNA. Sequence-specific purification has been used to improve sensitivity of TB diagnosis from sputum by removing high concentrations of nontarget DNA that can lead to downstream amplification inhibition (32), but has not been applied in urine where the primary advantage of non-target-DNA removal would be to reduce the likelihood of downstream nonspecific amplification. Confirming specific amplification of short targets without the footprint for a fluorescent detection probe can be difficult, but the added layer of specificity offered by sequence-specific purification may aid in overcoming this challenge.
Comparison to existing rapid TB tests.
Our urine cfDNA assay has the potential to diagnose TB in individuals who may be missed by other rapid tests (e.g., smear microscopy, urine LAM). We detected TB-specific cfDNA in the urine of all smear-positive and LAM-positive patients. Importantly, sensitivity remained high in both smear-negative (76.0%) and LAM-negative (76.5%) patients. The target product profile for a rapid biomarker-based non-sputum-based TB test outlines the optimal requirements for pulmonary TB in adults as ≥98% sensitivity for smear-positive TB, ≥68% sensitivity for smear-negative TB, and ≥80% sensitivity for HIV-associated TB (5). Our results suggest that, by employing an optimized extraction method with demonstrated high efficiency for short fragments, urine cfDNA-based assays have the potential to achieve sufficient sensitivity to meet these criteria and improve diagnostic accuracy compared to smear microscopy.
Unlike urine LAM tests, which have insufficient sensitivity, particularly in HIV-negative individuals (33), cfDNA tests have the potential to diagnose TB regardless of HIV status and CD4 count. We observed slightly higher sensitivity in HIV-positive (88.2%) compared to HIV-negative (73.3%) patients, but the difference was nonsignificant and the number of HIV-negative patients was small. Despite a moderate inverse correlation between CD4 count and detected TB-specific cfDNA concentration, there was no significant difference in sensitivity for HIV-positive patients with CD4 counts of ≤200 compared to >200 cells/mm3. Although the small sample sizes led to large confidence intervals that may obscure some meaningful differences, and future studies are needed to conclusively compare cfDNA detection sensitivity across HIV-positive and HIV-negative subgroups, our results suggest that urine cfDNA is detectable across a wider patient population than urine LAM.
In contrast, the commercially available Alere Determine TB LAM test has 42% pooled sensitivity in HIV-positive individuals, with sensitivity inversely proportional to CD4 cell count (34). The WHO only recommends its use in people living with HIV but not as a general screening test for TB (35). Ongoing efforts aim to improve urine LAM detection sensitivity. The Fujifilm SILVAMP TB LAM test improves sensitivity relative to Alere LAM in both HIV-positive (70% versus 42%) and HIV-negative (53% versus 11%) individuals (36, 37). As antigen-based tests, however, LAM assays may not be able to achieve the sensitivity afforded by nucleic acid amplification tests. On the other hand, a critical advantage of LAM assays over cfDNA is their ease of sample processing. The cfDNA assay described here is not yet suitable for use in most clinically relevant settings, and will require substantial simplification in order to compete with existing rapid TB tests.
Contributions to evidence for urine cfDNA as a biomarker for TB.
To date, usefulness of urine cfDNA as a biomarker for TB has been limited, in part due to inconsistent methods and results in previous TB urine cfDNA studies. Our study contributes to the evidence for urine cfDNA as a TB biomarker in two ways: (i) demonstration of the feasibility of high sensitivity and specificity with optimal preanalytical methods and (ii) development of a reliable, quantifiable method to further study TB urine cfDNA. Previous TB urine cfDNA studies have focused on measuring diagnostic accuracy, and have mostly neglected to report TB urine cfDNA concentrations. Labugger et al. measured concentrations for a limited number of treatment-naive individuals (n = 7), which ranged from 1 to 41 copies/ml (median 6.5 copies/ml) (9). Here, we quantified TB-specific cfDNA to better estimate the clinical range (<1 to 2,804 copies/ml; median 14.6 copies/ml), and have conducted analyses to determine which variables correlate with cfDNA concentration. We found that cfDNA concentration was higher in LAM-positive patients compared to LAM-negative patients, but LAM result did not affect cfDNA sensitivity. We detected cfDNA in all patients who had recently initiated TB treatment, with a higher concentration compared to treatment-naive patients, supporting the possibility of using cfDNA for treatment monitoring, as suggested previously (9). Upon initiation of a successful treatment regimen, cfDNA concentration may temporarily increase due to bactericidal activity, followed by a slow decline as the infection is cleared (9). Our study did not show a correlation between days of treatment and cfDNA concentration, but only included participants with ≤3 days of treatment and did not monitor individual participants over time.
Although cfDNA was detectable regardless of HIV status or CD4 count, the detected concentration had a moderate inverse correlation with CD4 count. We also found that cfDNA concentration had a moderate inverse correlation with days to culture positivity, suggesting that levels of excreted cfDNA may be related to bacterial burden. We observed no correlation with AFB sputum smear score or Alere urine LAM score, but the sample sizes for these analyses were small. We anticipate that our assay can be used to continue to study TB urine cfDNA trends across subgroups and answer important unresolved questions regarding optimal sample collection techniques, processing methods, and storage conditions that have been the focus of recent work (38–40). As a caveat, the cfDNA concentrations measured by our assay may be confounded by the variable copy number of IS6110 (0 to 25 copies) (25) and by differences in participants’ hydration status. In the future, strain typing and normalizing cfDNA concentration to urine creatinine may help better elucidate trends in cfDNA concentration.
Study limitations and future work.
TB symptoms were required in addition to a positive Xpert result for the TB case definition to reduce the risk of a false-positive Xpert result, but it is possible that some could still have occurred. Using the strictest TB-positive criteria, requiring both positive Xpert and positive culture, would result in a nonsignificant increase in cfDNA sensitivity (to 88%). Several TB-positive, cfDNA-negative samples (false negatives) narrowly missed the cfDNA positivity cutoff, suggesting the opportunity for future improvement in clinical sensitivity. We are currently pursuing two approaches to further improve our assay’s ability to detect low cfDNA concentrations: (i) a reduction in PCR target length (to 25 bp using an ultrashort PCR design described in reference 31) and (ii) multiplexing to target multiple genomic regions. Multiplexing will have the additional benefit of improving inclusivity by enabling detection of TB strains lacking IS6110.
This study serves as a valuable demonstration of the feasibility of our sequence-specific approach in adults with active pulmonary TB, but the sample size and scope were limited. Future studies will seek to further validate our assay and better compare sensitivity across subgroups using larger sample sizes (including more HIV-negative participants and negative controls). Subsequent work will also include expanded populations, specifically those underserved by current rapid sputum-based tests (including individuals with Xpert-negative TB, children, and patients with EPTB). TB-specific cfDNA has been detected in the urine (13) and plasma (41–43) of individuals with EPTB, including a case study of a child with tubercular otitis media (44), but there have not yet been any prospective studies in children.
Our assay also currently requires a trained user, laboratory equipment, and significant hands-on time. In the future, we aim to simplify our laboratory-based test into a format more suitable for use in resource-limited settings, possibly by adapting technologies in development for silica-based magnetic bead purification for sequence-specific purification. Promising technologies for assay simplification include those that employ immiscible phase filtration (45–48) and high-gradient magnetic separation (49). Because existing technologies cannot accommodate large input sample volumes, the 10-ml volume required for our assay may pose a significant challenge for assay simplification. Ideally, further improvements to the analytical sensitivity (ultrashort PCR and/or multiplexing, as described above) will allow for a reduction in sample volume. Alternatively, magnetic beads can be concentrated manually by centrifugation or a semiautomated device (such as the nRichDx system) prior to processing on a downstream automated device.
In conclusion, sequence-specific purification improves recovery of short urine cfDNA and increases the sensitivity of adult pulmonary TB diagnosis from urine cfDNA. Our assay has the highest reported accuracy of any TB urine cfDNA test to date and has the potential to enable urine-based TB diagnosis across sputum-scarce and paucibacillary populations. This study will lay the foundation for expanded clinical studies and future development of a rapid test. In addition, our work serves as a valuable contribution to the clinical evidence for urine cfDNA as a biomarker for TB. The ability to diagnose TB across key underserved populations (e.g., children, people living with HIV, individuals with EPTB) using urine samples would address an urgent need that was identified as one of the highest priority gaps in TB diagnostics (5). A sensitive urine-based test built upon the sequence-specific purification method described here could significantly contribute to improving sample availability, expanding access to rapid TB diagnosis, and controlling the TB epidemic.
ACKNOWLEDGMENTS
We are grateful to study participants for their contributions to this research. We thank the KwaZulu-Natal Department of Health and the staff of Edendale Hospital for their partnership, and Norman D. Brault and James Lai for their contributions to the early development of the sequence-specific purification method.
Research reported in this publication was funded by the Bill and Melinda Gates Foundation under award number OPP1152864 and the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under award number R21AI125975. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This research was funded in part by a 2018 CFAR developmental grant from the University of Washington/Fred Hutch Center for AIDS Research, and an NIH-funded program under award number AI027757, which is supported by the following NIH Institutes and Centers: NIAID, NCI, NIMH, NIDA, NICHD, NHLBI, NIA, NIGMS, NIDDK. A.O. was supported by funding from the National Science Foundation Graduate Research Fellowship Program. The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Footnotes
Supplemental material is available online only.
Contributor Information
Paul K. Drain, Email: pkdrain@uw.edu.
Barry R. Lutz, Email: blutz@uw.edu.
Christine Y. Turenne, St. Boniface Hospital
REFERENCES
- 1.World Health Organization. 2020. Global tuberculosis report 2020. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 2.Horne DJ, Kohli M, Zifodya JS, Schiller I, Dendukuri N, Tollefson D, Schumacher SG, Ochodo EA, Pai M, Steingart KR. 2019. Xpert MTB/RIF and Xpert MTB/RIF Ultra for pulmonary tuberculosis and rifampicin resistance in adults. Cochrane Database Syst Rev 2019:CD009593. doi: 10.1002/14651858.CD009593.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Detjen AK, DiNardo AR, Leyden J, Steingart KR, Menzies D, Schiller I, Dendukuri N, Mandalakas AM. 2015. Xpert MTB/RIF assay for the diagnosis of pulmonary tuberculosis in children: a systematic review and meta-analysis. Lancet Respir Med 3:451–461. doi: 10.1016/S2213-2600(15)00095-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kohli M, Schiller I, Dendukuri N, Dheda K, Denkinger CM, Schumacher SG, Steingart KR. 2018. Xpert MTB/RIF assay for extrapulmonary tuberculosis and rifampicin resistance. Cochrane Database Syst Rev 2018::CD012768. doi: 10.1002/14651858.CD012768.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. 2014. High-priority target product profiles for new tuberculosis diagnostics: report of a consensus meeting. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 6.Green C, Huggett JF, Talbot E, Mwaba P, Reither K, Zumla AI. 2009. Rapid diagnosis of tuberculosis through the detection of mycobacterial DNA in urine by nucleic acid amplification methods. Lancet Infect Dis 9:505–511. doi: 10.1016/S1473-3099(09)70149-5. [DOI] [PubMed] [Google Scholar]
- 7.Botezatu I, Serdyuk O, Potapova G, Shelepov V, Alechina R, Molyaka Y, Anan’ev V, Bazin I, Garin A, Narimanov M, Knysh V, Melkonyan H, Umansky S, Lichtenstein A. 2000. Genetic analysis of DNA excreted in urine: a new approach for detecting specific genomic DNA sequences from cells dying in an organism. Clin Chem 46:1078–1084. doi: 10.1093/clinchem/46.8.1078. [DOI] [PubMed] [Google Scholar]
- 8.Cannas A, Goletti D, Girardi E, Chiacchio T, Calvo L, Cuzzi G, Piacentini M, Melkonyan H, Umansky SR, Lauria FN, Ippolito G, Tomei LD. 2008. Mycobacterium tuberculosis DNA detection in soluble fraction of urine from pulmonary tuberculosis patients. Int J Tuber Lung Dis 12:146–151. [PubMed] [Google Scholar]
- 9.Labugger I, Heyckendorf J, Dees S, Häussinger E, Herzmann C, Kohl TA, Richter E, Rivera-Milla E, Lange C. 2017. Detection of transrenal DNA for the diagnosis of pulmonary tuberculosis and treatment monitoring. Infection 45:269–276. doi: 10.1007/s15010-016-0955-2. [DOI] [PubMed] [Google Scholar]
- 10.Patel K, Nagel M, Wesolowski M, Dees S, Rivera-Milla E, Geldmacher C, Dheda K, Hoelscher M, Labugger I. 2018. Evaluation of a urine-based rapid molecular diagnostic test with potential to be used at point-of-care for pulmonary tuberculosis: Cape Town cohort. J Mol Diagn 20:215–224. doi: 10.1016/j.jmoldx.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Bordelon H, Ricks KM, Pask ME, Russ PK, Solinas F, Baglia ML, Short PA, Nel A, Blackburn J, Dheda K, Zamudio C, Cáceres T, Wright DW, Haselton FR, Pettit AC. 2017. Design and use of mouse control DNA for DNA biomarker extraction and PCR detection from urine: application for transrenal Mycobacterium tuberculosis DNA detection. J Microbiol Methods 136:65–70. doi: 10.1016/j.mimet.2017.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peter JG, Theron G, Muchinga TE, Govender U, Dheda K. 2012. The diagnostic accuracy of urine-based Xpert MTB/RIF in HIV-infected hospitalized patients who are smear-negative or sputum scarce. PLoS One 7:e39966. doi: 10.1371/journal.pone.0039966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fortún J, Martín-Dá P, G´Omez-Mampaso E, Gonzá Lez-García A, Barbolla I, G´Omez-García I, Wikman P, Ortíz J, Navas E, Cuartero C, Gijón D, Gijón G, Moreno S. 2014. Extra-pulmonary tuberculosis: differential aspects and role of 16S-rRNA in urine. Int j Tuber Lung Dis 18:478–485. doi: 10.5588/ijtld.13.0555. [DOI] [PubMed] [Google Scholar]
- 14.Fernández-Carballo BL, Broger T, Wyss R, Banaei N, Denkinger CM. 2018. Toward the development of a circulating free DNA-based in-vitro diagnostic test for infectious diseases: a review of evidence for tuberculosis. J Clin Microbiol 57:e01234-18. doi: 10.1128/JCM.01234-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marangu D, Devine B, John-Stewart G. 2015. Diagnostic accuracy of nucleic acid amplification tests in urine for pulmonary tuberculosis: a meta-analysis. Int j Tuber Lung Dis 19:1339–1347. doi: 10.5588/ijtld.15.0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tsui NBY, Jiang P, Chow KCK, Su X, Leung TY, Sun H, Chan KCA, Chiu RWK, Lo YMD. 2012. High resolution size analysis of fetal DNA in the urine of pregnant women by paired-end massively parallel sequencing. PLoS One 7:e48319. doi: 10.1371/journal.pone.0048319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Markus H, Zhao J, Contente-Cuomo T, Stephens MD, Raupach E, Odenheimer-Bergman A, Connor S, McDonald BR, Moore B, Hutchins E, McGilvrey M, de la Maza MC, Van Keuren-Jensen K, Pirrotte P, Goel A, Becerra C, Von Hoff DD, Celinski SA, Hingorani P, Murtaza M. 2021. Analysis of recurrently protected genomic regions in cell-free DNA found in urine. Sci Transl Med 13:eaaz3088. doi: 10.1126/scitranslmed.aaz3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burnham P, Kim MS, Agbor-Enoh S, Luikart H, Valantine HA, Khush KK, De Vlaminck I. 2016. Single-stranded DNA library preparation uncovers the origin and diversity of ultrashort cell-free DNA in plasma. Sci Rep 6:27859. doi: 10.1038/srep27859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Snyder MW, Kircher M, Hill AJ, Daza RM, Shendure J. 2016. Cell-free DNA comprises an in vivo nucleosome footprint that informs its tissues-of-origin. Cell 164:57–68. doi: 10.1016/j.cell.2015.11.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sanchez C, Snyder MW, Tanos R, Shendure J, Thierry AR. 2018. New insights into structural features and optimal detection of circulating tumor DNA determined by single-strand DNA analysis. NPJ Genom Med 3:31. doi: 10.1038/s41525-018-0069-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burnham P, Dadhania D, Heyang M, Chen F, Westblade LF, Suthanthiran M, Lee JR, De Vlaminck I. 2018. Urinary cell-free DNA is a versatile analyte for monitoring infections of the urinary tract. Nat Commun 9:2412. doi: 10.1038/s41467-018-04745-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheng THTT, Jiang P, Tam JCWW, Sun X, Lee W-S, Yu SCYY, Teoh JYCC, Chiu PKFF, Ng C-F, Chow K-M, Szeto C-C, Chan K, Chiu RWKK, Dennis Lo YM, Lo YMD. 2017. Genomewide bisulfite sequencing reveals the origin and time-dependent fragmentation of urinary cfDNA. Clin Biochem 50:496–501. doi: 10.1016/j.clinbiochem.2017.02.017. [DOI] [PubMed] [Google Scholar]
- 23.Yao W, Mei C, Nan X, Hui L. 2016. Evaluation and comparison of in vitro degradation kinetics of DNA in serum, urine and saliva: a qualitative study. Gene 590:142–148. doi: 10.1016/j.gene.2016.06.033. [DOI] [PubMed] [Google Scholar]
- 24.Oreskovic A, Lutz B. 2021. Ultrasensitive hybridization capture: reliable detection of <1 copy/mL short cell-free DNA from large-volume urine samples. PLoS One 16:e0247851. doi: 10.1371/journal.pone.0247851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.del Carmen Menéndez M, Samper S, Otal I, García MJ. 2012. IS6110 the double-edged passenger, p 59–88. In Cardona P-J (ed), Understanding tuberculosis—deciphering the secret life of the bacilli. InTech Open. [Google Scholar]
- 26.Hellyer TJ, Desjardin LE, Assaf MK, Bates JH, Cave MD, Eisenach KD. 1996. Specificity of IS6110-based amplification assays for Mycobacterium tuberculosis complex. J Clin Microbiol 34:2843–2846. doi: 10.1128/JCM.34.11.2843-2846.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Su Y-H, Wang M, Block TM, Landt O, Botezatu I, Serdyuk O, Lichtenstein A, Melkonyan H, Tomei LD, Umansky S. 2004. Transrenal DNA as a diagnostic tool: important technical notes. Ann N Y Acad Sci 1022:81–89. doi: 10.1196/annals.1318.014. [DOI] [PubMed] [Google Scholar]
- 28.Shekhtman EM, Anne K, Melkonyan HS, Robbins DJ, Warsof SL, Umansky SR. 2009. Optimization of transrenal DNA analysis: detection of fetal DNA in maternal urine. Clin Chem 55:723–729. doi: 10.1373/clinchem.2008.113050. [DOI] [PubMed] [Google Scholar]
- 29.Melkonyan HS, Feaver WJ, Meyer E, Scheinker V, Shekhtman EM, Xin ZH, Umansky SR. 2008. Transrenal nucleic acids: from proof of principle to clinical tests. Ann N Y Acad Sci 1137:73–81. doi: 10.1196/annals.1448.015. [DOI] [PubMed] [Google Scholar]
- 30.Boom R, Sol C, Salimans MM, Jansen C, Wertheim-van Dillen P, van der Noordaa J. 1990. Rapid and simple method for purification of nucleic acids. J Clin Microbiol 28:495–503. doi: 10.1128/JCM.28.3.495-503.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oreskovic A, Brault ND, Panpradist N, Lai JJ, Lutz BR. 2019. Analytical comparison of methods for extraction of short cell-free DNA from urine. J Mol Diagnostics 21:1067–1078. doi: 10.1016/j.jmoldx.2019.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reed JL, Basu D, Butzler MA, McFall SM. 2017. XtracTB Assay, a Mycobacterium tuberculosis molecular screening test with sensitivity approaching culture. Sci Rep 7:3653. doi: 10.1038/s41598-017-03930-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Minion J, Leung E, Talbot E, Dheda K, Pai M, Menzies D. 2011. Diagnosing tuberculosis with urine lipoarabinomannan: systematic review and meta-analysis. Eur Respir J 38:1398–1405. doi: 10.1183/09031936.00025711. [DOI] [PubMed] [Google Scholar]
- 34.Bjerrum S, Schiller I, Dendukuri N, Kohli M, Nathavitharana RR, Zwerling AA, Denkinger CM, Steingart KR, Shah M. 2019. Lateral flow urine lipoarabinomannan assay for detecting active tuberculosis in people living with HIV. Cochrane Database Syst Rev 2019:CD011420. doi: 10.1002/14651858.CD011420.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Health Organization. 2019. Lateral flow urine lipoarabinomannan assay (LF-LAM) for the diagnosis of active tuberculosis in people living with HIV: policy update (2019). World Health Organization, Geneva, Switzerland. [Google Scholar]
- 36.Broger T, Nicol MP, Sigal GB, Gotuzzo E, Zimmer AJ, Surtie S, Caceres-Nakiche T, Mantsoki A, Reipold EI, Székely R, Tsionsky M, van Heerden J, Plisova T, Chikamatsu K, Lowary TL, Pinter A, Mitarai S, Moreau E, Schumacher SG, Denkinger CM. 2020. Diagnostic accuracy of 3 urine lipoarabinomannan tuberculosis assays in HIV-negative outpatients. J Clin Invest 130:5756–5764. doi: 10.1172/JCI140461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Broger T, Sossen B, Du Toit E, Kerkhoff AD, Schutz C, Ivanova Reipold E, Ward A, Barr DA, Macé A, Trollip A, Burton R, Ongarello S, Pinter A, Lowary TL, Boehme C, Nicol MP, Meintjes G, Denkinger CM. 2019. Novel lipoarabinomannan point-of-care tuberculosis test for people with HIV: a diagnostic accuracy study. Lancet Infect Dis 19:852–861. doi: 10.1016/S1473-3099(19)30001-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Murugesan K, Hogan CA, Palmer Z, Reeve B, Theron G, Andama A, Somoskovi A, Steadman A, Madan D, Andrews J, Croda J, Sahoo MK, Cattamanchi A, Pinsky BA, Banaei N. 2019. Investigation of preanalytical variables impacting pathogen cell-free DNA in blood and urine. J Clin Microbiol 57:e00782-19. doi: 10.1128/JCM.00782-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee EY, Lee E-J, Yoon H, Lee DH, Kim KH. 2020. Comparison of four commercial kits for isolation of urinary cell-free DNA and sample storage conditions. Diagnostics 10:234. doi: 10.3390/diagnostics10040234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Augustus E, Van Casteren K, Sorber L, van Dam P, Roeyen G, Peeters M, Vorsters A, Wouters A, Raskin J, Rolfo C, Zwaenepoel K, Pauwels P. 2020. The art of obtaining a high yield of cell-free DNA from urine. PLoS One 15:e0231058. doi: 10.1371/journal.pone.0231058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yamamoto M, Ushio R, Watanabe H, Tachibana T, Tanaka M, Yokose T, Tsukiji J, Nakajima H, Kaneko T. 2018. Detection of Mycobacterium tuberculosis-derived DNA in circulating cell-free DNA from a patient with disseminated infection using digital PCR. Int J Infect Dis 66:80–82. doi: 10.1016/j.ijid.2017.11.018. [DOI] [PubMed] [Google Scholar]
- 42.Lyu L, Li Z, Pan L, Jia H, Sun Q, Liu Q, Zhang Z. 2020. Evaluation of digital PCR assay in detection of M.tuberculosis IS6110 and IS1081 in tuberculosis patients plasma. BMC Infect Dis 20:657. doi: 10.1186/s12879-020-05375-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang J, Han X, Liu A, Bai X, Xu C, Bao F, Feng S, Tao L, Ma M, Peng Y. 2017. Use of digital droplet PCR to detect Mycobacterium tuberculosis DNA in whole blood-derived DNA samples from patients with pulmonary and extrapulmonary tuberculosis. Front Cell Infect Microbiol 7:369. doi: 10.3389/fcimb.2017.00369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Petrucci R, Lombardi G, Corsini I, Visciotti F, Pirodda A, Cazzato S, Landini MP, Dal Monte P. 2015. Use of transrenal DNA for the diagnosis of extrapulmonary tuberculosis in children: a case of tubercular otitis media. J Clin Microbiol 53:336–338. doi: 10.1128/JCM.02548-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Neto MF, Butzler MA, Reed JL, Rui X, Fisher MJ, Kelso DM, McFall SM. 2017. Immiscible phase filter extraction and equivalent amplification of genotypes 1–6 of hepatitis C RNA: the building blocks for point-of-care diagnosis. J Virol Methods 248:107–115. doi: 10.1016/j.jviromet.2017.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Creecy A, Russ PK, Solinas F, Wright DW, Haselton FR. 2015. Tuberculosis biomarker extraction and isothermal amplification in an integrated diagnostic device. PLoS One 10:e0130260. doi: 10.1371/journal.pone.0130260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Guckenberger DJ, Pezzi HM, Regier MC, Berry SM, Fawcett K, Barrett K, Beebe DJ. 2016. Magnetic system for automated manipulation of paramagnetic particles. Anal Chem 88:9902–9907. doi: 10.1021/acs.analchem.6b02257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Berry SM, Pezzi HM, LaVanway AJ, Guckenberger DJ, Anderson MA, Beebe DJ. 2016. AirJump: using interfaces to instantly perform simultaneous extractions. ACS Appl Mater Interfaces 8:15040–15045. doi: 10.1021/acsami.6b02555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pearlman SI, Leelawong M, Richardson KA, Adams NM, Russ PK, Pask ME, Wolfe AE, Wessely C, Haselton FR. 2020. Low-resource nucleic acid extraction method enabled by high-gradient magnetic separation. ACS Appl Mater Interfaces 12:12457–12467. doi: 10.1021/acsami.9b21564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ushio R, Yamamoto M, Nakashima K, Watanabe H, Nagai K, Shibata Y, Tashiro K, Tsukahara T, Nagakura H, Horita N, Sato T, Shinkai M, Kudo M, Ueda A, Kaneko T. 2016. Digital PCR assay detection of circulating Mycobacterium tuberculosis DNA in pulmonary tuberculosis patient plasma. Tuberculosis (Edinb) 99:47–53. doi: 10.1016/j.tube.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 51.Click ES, Murithi W, Ouma GS, McCarthy K, Willby M, Musau S, Alexander H, Pevzner E, Posey J, Cain KP. 2018. Detection of apparent cell-free M. tuberculosis DNA from plasma. Sci Rep 8:645. doi: 10.1038/s41598-017-17683-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig. S1, Tables S1 to S4. Download JCM.00074-21-s0001.pdf, PDF file, 393 KB (392.8KB, pdf)
Data Set S1. Download JCM.00074-21-s0002.xlsx, XLSX file, 31 KB (30KB, xlsx)