Abstract
Traditional ultrasound teaching is normally delivered using large, costly and often quite advanced cart-based systems. These carts are often large systems on wheels, usually limited to the departments that own them i.e. clinics, wards or radiology. Portability has been further improved by the development of laptop style systems, which are easier to wheel in-between patients/departments. In our experience and anecdotally, many of these systems can be intimidating to the novice and can lead to early attrition or poor uptake of ultrasound into clinical practice. Carts can also restrict the amount of training deliverable to practitioners, as they are limited in number due to cost and can take quite some time to boot up, reducing convenience.
This dogma is being progressively changed with the advent of smaller handheld devices, some clearly within the financial grasps of most practitioners, and even to the point of medical schools offering students their own personal device.1,2 This relative inexpensiveness can lead to the purchase of these devices for novelty and convenience, over need. Obvious caution is needed in these circumstances, but with increased ease of purchase, better availability and inbuilt simplicity, ultrasound learning can be seamlessly integrated into day-to-day practice.
This review discusses how one of the most disruptive innovations in modern medicine is changing ultrasound from a classic imaging modality to become integrated as the fifth pillar of clinical examination, and how these new devices can serve as springboards to more advanced ultrasound training. In fact, within what has become a bigger area of clinical examination, things are getting smaller.
Keywords: Ultrasound, point of care ultrasound, point of care, handheld ultrasound, pocket ultrasound, training
Traditional clinical examination – A dying art?
There is no debate regarding the fact that medicine has relied upon the traditional four pillars of clinical examination for millennia. It must be borne in mind that the arrival stethoscope was not simply adopted overnight. In fact, it underwent a similar scrutiny to our modern ultrasound (US) devices. It now unquestionably forms the fourth pillar of clinical examination, and has opened up a wealth of further possibility into the mysteries of disease processes with auscultation. As this tradition propagated over the years, there was simply no debate regarding the fact that its dogma settled into a firm and undebatable foundation. Any new drug or technology in medicine faces such a cacophony of scrutiny now; yet no one seemed to debate a new examination technique, after all, it was cheap and harmless?!
There is no replacement for a good set of examination skills amongst practitioners, but there is still debate over the usefulness, sensitivity and specificity of some traditional modalities of diagnosis.3,4 Sadly, many forms of physical examination may indeed be a thing of the past. This is particularly so, as many of our highly experienced, widely practiced colleagues have gone, or will soon retire. We also face a world where there are so many other available diagnostic tests, our trainees/students now defer to these as the first choice over a thorough examination.
Indeed, there is still debate over the inclusion of US into everyday practice, but evidence emerging tells us that US may be superior to traditional examination in many ways.5–12 Although there is significant bias from both authors in writing this, we feel that embracing US and its inclusion into all physical examinations is merely grasping the opportunity to stay ahead of the game. Technology is continually advancing in medicine, and at some pace, therefore failure to grasp this could be adding a disservice to our patients. US certainly fits into this statement. The stethoscope came along, allowing us to ‘hear into the body’, now handheld US permits us to ‘see into the body’. This fifth pillar forms a bridge between a clinical examination of a chest and a computed tomography (CT) of the chest, but with the patient in front of us; and no transport or upheaval elsewhere.
Handheld devices
Portable US solutions have been continuously evolving and as a result, continue to challenge the place of the stethoscope. Insonation, as the fifth pillar of clinical examination, has become a true reality.13 It has transported US from the radiology department/US laboratory, direct to the patient; whether on the intensive care unit (ICU), the hospital ward, in their general practitioner (GP) surgery or at the roadside in the prehospital environment.
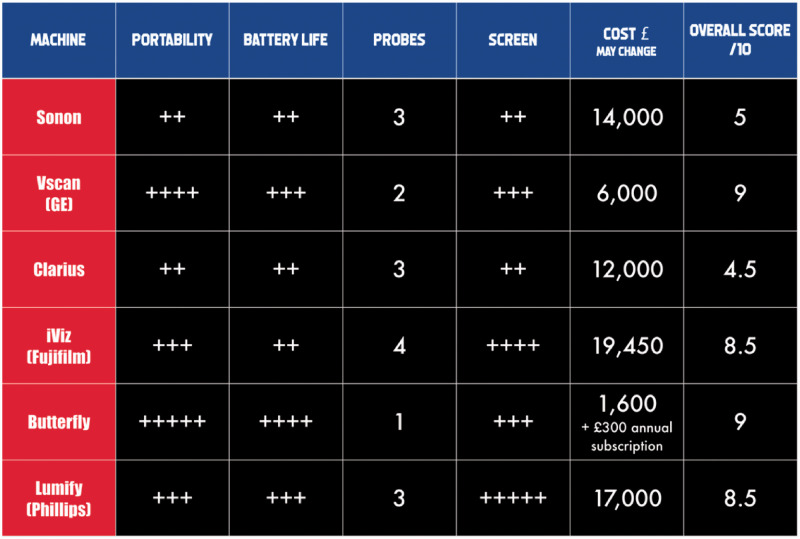
There is often confusion/debate as to which device is most fit-for-purpose. Figure 1 delineates some of the most popular devices and their attributes. Many of the devices have been tried and tested in order to clear up confusion as to which to purchase for institutions or individuals. We wish to point out that these reviews are written by a small subset of clinicians and they do. Not directly compare cart-based devices.14
Figure 1.
Some of the features of a few of the market-leading devices. (Taken from www.criticalcarenorthampton.com13).
The history of medical US dates to just after World War II. The first handheld battery-powered US equipment became available in 1975.15 It was not until early 2000 however, that truly pocket-sized equipment became available and affordable enough to become begin entering routine clinical use.
Reluctance and caution
Many hospitals have challenged the security of image processing of these devices. Such devices may be fine for use in non-clinical educational settings, but bringing personal devices into clinical environments for either diagnostic or educational purposes, without appropriate approval, may lead to trouble. Amongst many, integration with their storage systems has been a bureaucratic challenge, more than a logistical one. To ‘dot the I’s and cross the t’s’, purchase of such probes/portable devices may involve departmental administration, information technology (IT), information governance, risk management and clinical engineering departments. Hospital encrypted devices can be utilised in order to tighten security and remotely wiped should any go missing, thus clearing out any patient identifiable data held within.
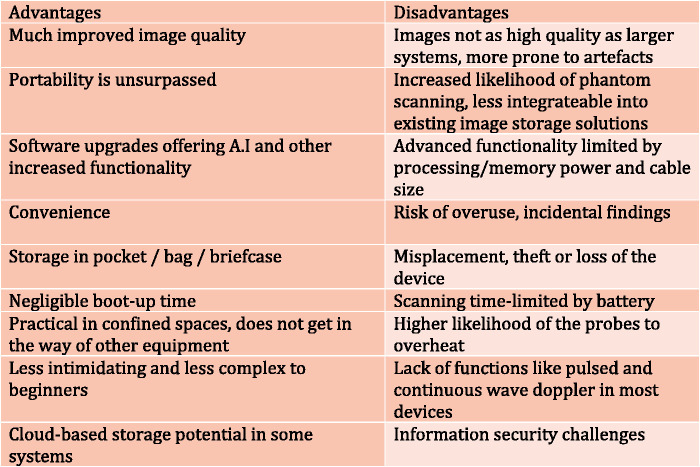
As well as this, and the limitations pertained to in Figure 3, portable handheld devices are currently incapable of generating the same image quality one might expect from a larger device. If this is not borne in mind from the outset, the naive sonographer could mismanage patients based imagining versus imaging, or indeed what they may be missing buried by a poor image on a small screen.
Figure 3.
Advantages and disadvantages of many portable ultrasound devices.
With the increasing frequency/convenience of usage, so may follow transmission of contaminants between patients. This requires users to be vigilant with scrupulous decontamination of probes, and the devices themselves. On the other hand, stethoscopes have long been recognised as sources of contamination.16,17
While handheld devices can improve cost effectiveness, through their low cost and ability to direct patients to appropriate diagnostic tests faster and in some cases avoid resource demanding transport to advanced imaging.18 But, this has not yet been translated into improved patient-oriented outcomes. There is also a risk that false positives and incidental findings increase resource consumption. Examinations must be focused towards answering defined and limited questions, and the limitations of the equipment and practitioner should be considered.
Examinations with handheld devices may deprive patients of the correct diagnostic investigations in less experienced hands. Hubris must be avoided, and the devices should be utilised as tools for rule-in, rather than rule-out.
Patient experience
Some argue that US examinations remove true patient contact. We would argue the contrary, handheld US brings the diagnostic test back into the hands of the treating clinician at the patient’s bedside. The practitioner has their hands on the patient and they are able to continue communicating and talking to them as they acquire the images they need. Placement of a stethoscope onto a patient’s chest normally requires quiet, so the practitioner can auscultate, leaving the patient in the dark. US is quite the opposite, often with the practitioner able to complete a history whilst performing insonation. Patients can also be further engaged in the process as the acquired images are displayed and explained to them in real time.19 This may proffer proof of pathology and promote increased compliance with the physician’s advice. Not only this, it may ease the path to obtaining further more detailed testing/imaging, with little obstruction to the referral from the receiving department/clinical speciality with this information in the armoury. When was the last time a doctor or practitioner described a murmur or attempted to explain a clinical sign to their patients?
Sonographers often turn their backs on patients when adjusting settings on the large cart-based devices. Granted, this can lead to patient detachment from the examination. Handheld devices can bridge this gap, whereby fewer complex alterations are possible while with the patient, and with no need to turn away. We feel pocket devices permit improved patient engagement and satisfaction with the examination. The manner in which examinations using these devices takes place, very much maintains the tradition of clinical examination. Rather than hand percussion of the chest, for example, we now use handheld US to insonate the body.
Ergonomics
Many US systems are bulky, requiring rearrangement of the bed space. Many busy ICU’s, emergency departments (EDs) and wards have space at a premium. A cart can be intimidating to patients, much like the dentist’s chair. A practitioner appearing with a less intimidating handheld device can be a welcomed change.
Repetitive strain injuries are becoming a real problem amongst sonographers, as they contort around a limited space in order to get the probe to the patient.20,21 Handhelds permit a more comfortable examination set, with minimal movement and enhanced ergonomic balance.
Why might these devices be the key to future training?
Handheld US devices might be better viewed as tools to extend the physical examination, rather than tools for comprehensive diagnostics. They can also be a stepping stone for those training to become competent in advanced US applications, providing the initial training in image acquisition.22 We must again state that they are limited by the image quality they can provide, both with screen size and the available memory to process a higher image quality series. Acceptance of this fact by practitioners and learners will promote an added safety net when it comes to making clinical decisions informed by handhelds.
As mentioned, larger cart-based devices can be cumbersome and intimidating, with all of the complex knobs, sliders, as well as generally much longer boot time than handheld devices. Starting out in US requires a mastery of the basics. Agreed, many of the advanced functions of larger carts can be turned off when not required for basic training, but over-complexity can lead to failure to grasp basics as the novice is buried within ‘knobology’.
In our opinion, portable handheld devices offer a window in. Most are extremely intuitive to beginners, with many mirroring the skillset required to operate most mobile phones/tablets (swiping, zooming, dragging and operation of menus). These skills are almost reflexive; certainly, to the younger generation of medical practitioners. Thus, utilising a basic inbuilt skillset may give novices a real head-start. Most can operate an android or apple-based phone; most can therefore intuitively operate many of these handheld devices.
Through their affordability, handheld US devices are also increasingly employed by medical schools both as part of the clinical point of care US curriculum, but also as tools for demonstrating functional anatomy. This can lead to paradoxical situations where students enter clinical practice and are more competent than their superiors in US.23
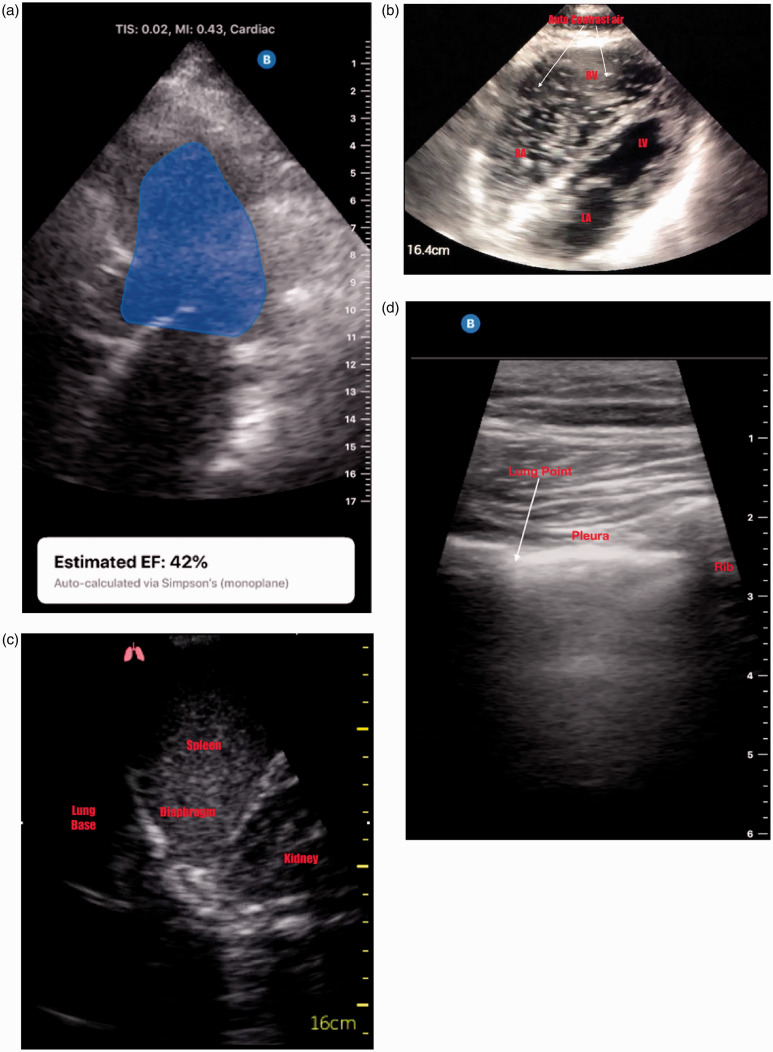
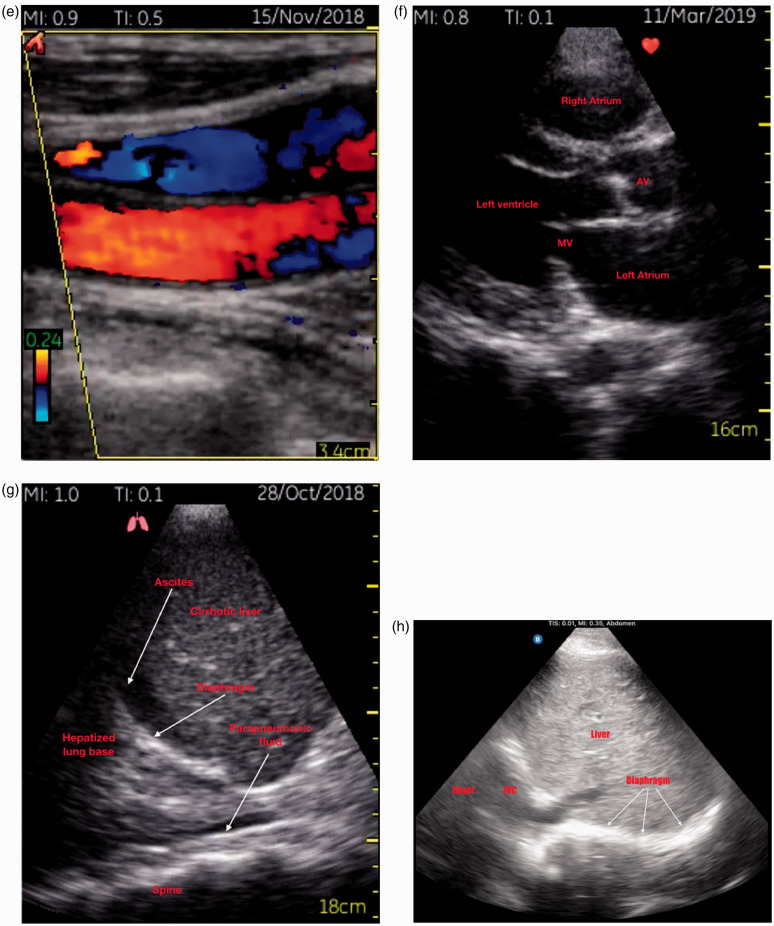
There is also a certain degree of palpable excitement when a novice picks up and discovers they are able to obtain a very rapid, basic image set with a device they can hold in their hand, (akin to a stethoscope or the palpating hand) (Figure 2). Therein, the examiner forms a new connection with the patient.
Figure 2.
Various images obtained from two popular portable handheld devices. (a) Apical four-chamber view with auto ejection fraction calculation. (b) Apical four-chamber view with saline auto-contrast demonstration in right heart during adrenaline minijet administration for cardiac arrest. (c) Left lung base scan demonstrating relevant anatomy. (d) Scan of the upper chest wall demonstrating a lung point where normal pleural sliding meets the interface with the non-sliding part of the pneumothorax. (e) Colour flow Doppler across jugular vein and carotid artery. (f) Normal parasternal long axis view of the heart. (g) Right lung base/right upper quadrant view showing cirrhotic liver, ascites and parapneumonic fluid. (h) Subcostal diaphragm scan used later to perform M-mode for excursion fraction calculation in a weaning patient.
Some of the advantages and disadvantages of these devices are shown in Figure 3.
The approach to training – Starting with a foundation in the basics
The dream state would be that every medical student/foundation doctor/more experienced doctor, have their own device. Due to financial constraints within the National Health Service (NHS), this certainly cannot be made a reality yet. However, the experienced mentor who does own a handheld can utilise it to fantastic effect when integrated into training.
The first step in learning to use US is image acquisition, which is, in essence, a practical skill and as such, requires hours and hours of training of eye–hand coordination to become competent and professing that, ‘Imagining has become imaging’. Introductory courses and workshops are beneficial and inspirational, but it is the repetitive and frequent use in clinical practice that truly leads to competency (experiential and context-based learning). Handheld devices afford ease of use, convenience, a lack of intimidation and accessibility, reducing the threshold for training.
The authors regularly teach on ward rounds with handheld devices.24 It is there at each bed space. It is there when the mentor attends sick patients on the wards taking the trainee with them. It is there when assessing cardiac activity during cardiac arrest attendance. It brings US into every area, so that the trainee experiences it, literally at point-of-care.
Carts are undeniably present in other areas external to the ICU, but require knowledge of functionality and must be booted up before scanning can commence. On the ICU ward round, the cart must be transported from bed space to bed space, often consuming a lot of space in amongst pumps and other machines.
Pathologies – Go and look!
There are a wealth of sono-anatomical variances, sono-pathologies and interesting findings to be witnessed. Instructing the trainee to attend a bed space and ‘see what you saw’, would require them to find the cart, boot it up and take it to the patient. Not the most convenient of situations. One pulled from the mentor’s pocket at the bed space and handed to the trainee there and then, is certainly as convenient as getting them to auscultate for a murmur, palpate for a mass or percuss for stony dullness at a lung base.
A real morale boost can be gained by the novice as they see the pleural effusion that was not visible on the chest X-ray, they catch the ascites in full view or see why the patient was struggling to breathe; there are the concomitant B-lines and a failing left ventricle (LV). The sono-pathological link has been made; the clinical signs have been taken to memory with a visual reinforcement of what they read about in books.25 The torch has been shone inside the patient and has similarly lit up the world of understanding for the novice.
Anatomy and physiology
Textbooks are read and images are taken to memory. But, there is no replacement for seeing what you read about in practice. Handheld US certainly paves the way for this process. Pleura are visualised, neuroanatomy is seen as blocks are performed, spleens, livers, kidneys and hearts are brought to life in 2D form right before their eyes. That mid-diastolic murmur or raised jugular venous pressure (JVP) is all explained now. The reason for the patient’s breathlessness is clear! The association with sono-anatomy, prosection anatomy and textbook anatomy is solidified.26
Physiology can be taught and illustrated visually at the bedside. The gastric antrum distends as the naso-gastric (NG) feed commences or as the subject takes a drink, the gallbladder empties as a fatty meal is taken. Medical therapy is guided by sound. The mentor adjusts the diuretic dose as the B-lines disappear over hours in the fluid overloaded patient. The reason for dobutamine versus noradrenaline is explained, as the failing LV cannot work any harder against afterload. The fluid boluses and noradrenaline doses are adjusted according to inferior vena cava diameters and left ventricular cavity eyeballing. The reason passive leg raise works can be seen as vessels fill, heart rates fall on the screen and the LV appears fuller.
Is this a passing fad…doesn’t US cause delays?
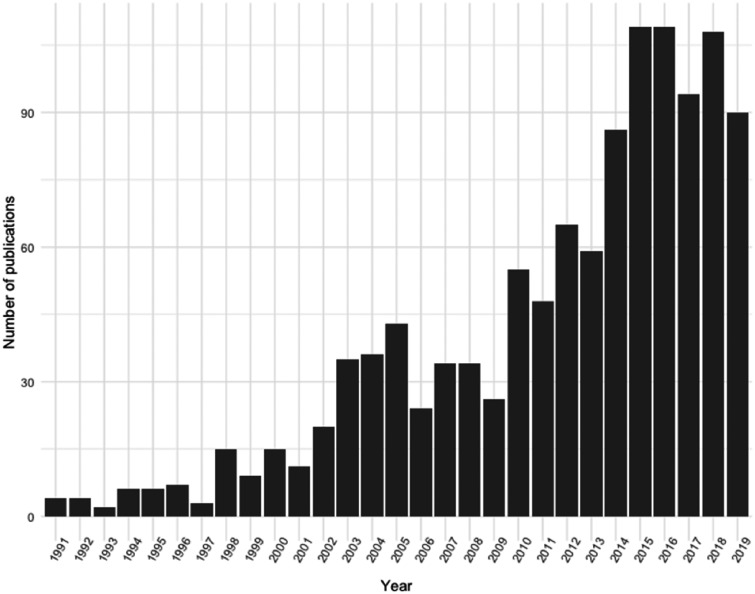
It can be true to say that there have been many technological innovations that have gripped medical practice, many of which passed like ships in the wind. But, portable US is here to stay. There has been a wealth of publications regarding this easy access modality and there also seems to have been an exponential uptake of such devices over the last five years (Figure 4).27 Many individuals have their own device and many units/specialities use them in daily practice.
Figure 4.
A web of science search for publications on ‘handheld ultrasound’, ‘hand carried ultrasound’ and ‘pocked sized ultrasound’.22
Proponents of US will clearly spend many hours incorporating it into their daily practice, which may be irritating to some. There have been phrases stated … ‘they’ll scan because they can’, ‘how will a scan benefit this patient’, ‘Is that necessary here’, or ‘this will delay the ward round!’ The key is to scan patients where there is an indication, and this does come with experience, (as with any slick, targeted clinical examination). The great benefit of handheld US is the ability to change a presumed diagnosis or direct the patient to a more appropriate further examination. It also permits earlier correction of therapy, possibly also sparing the patient unnecessary radiation or transportation elsewhere in order that a test is performed.28 This is clearly beneficial and can justify any delay to a ward round.
Some advocate incorporation of US into the ward round ‘on the -fly’, whilst others choose to re-visit the patient and perform a ‘point of care ultrasound (POCUS) round’, at a later point. There are advantages and disadvantages to both of these approaches and it all depends on the mentor as to which they choose. The important aspect to this for the trainee is to realise that its benefits are there to be embraced and that everyone within the team can be engaged with the process.
Developing a safer practitioner
Teaching a foundation in good bedside POCUS, early, may also promote safer medical practice for patients, particularly for those undergoing interventional procedures. We know that the use of US minimises the complication rates associated with intercostal drain insertion versus blind techniques.29,30 We also know that the use of US to guide placement of regional anaesthesia is more or less the gold standard now, as is its use to place indwelling vascular cathetars.31,32
A suggested approach
Manage expectations – no one can master US in two weeks, it can take months. None of us was instantly proficient with our stethoscopes or ophthalmoscopes.
Familiarity – the beginner should learn about what the device can do by using it on themselves or volunteers. Once the pinches, swipes, modes and probes the handheld offers are familiar, the patient examination becomes far easier, and the sonographer more proficient. No one wants to be selecting/deselecting modes, over gaining or trying to frantically measure structures during the scan. Familiarity breeds competence, but equally complacency too. The user should operate and accept the device has limitations, as discussed earlier.
Support – the mentor is key. The knowledge, experience and enthusiasm of the experienced sonographer will embed the same in the novice. Palpable enthusiasm and excitement in US will rub off and hopefully, a new breed of sonographer will emerge over time. The handheld can now afford trainees with the opportunities the carts perhaps did not, as they were too complex, were being used or took up too much space.
Focus on a few – pick only a few applications and clinical questions most relevant to your/their practice and focus on this to start with. It may be that this initial scope is limited due to the handheld’s capabilities.
Start behind the scenes – encourage pre-reading, encourage reference to free open access medicine (FOAM) sites and other training resources.33–36 Encourage the trainee to take the device away and look at it/watch video resources where it is being used by others in practice. Encourage the trainee to look at specimen images.
Get the numbers up – Scan as many patients as possible as often as possible. Start ideally alongside the mentor/sonographer. Target known/existing pathology when possible (i.e. gallstones, deep venous thrombosis (DVT) in a vascular clinic, pleural effusions, poor LVs, etc.). Maximize hands-on probe time and learn to escalate to the carts when there are further questions to be answered limited by the handheld. Psychomotor skills and spatial orientation can be challenging to master.
Compare and confirm – it is well worth advising the trainee to scan patients where there are other forms of confirmatory/non-confirmatory testing already available (i.e. consultative US, CT), to compare their findings.
Get a story – Ensure the trainee obtains a full background on each patient; this gives true context to the point of care scanning and instils training in putting together the history, prior examination findings and a targeted insonation. It also gives the trainee more of a ‘real-life’, approach to scanning, as they will when attending patients with the handheld device once confident to do so.
Keep a log – log, save and review all images with the mentor. This allows the trainee to hone their image acquisition/interpretation skills It also provides evidence when coming to accredit via their chosen pathway.
Keep it up – the key to mastery of US is to maintain the enthusiasm. The mentor: mentee relationship should be a strong one, in order to encourage and nurture the skillset. Using a handheld device to inform critical treatment decisions can often be met with cynicism. ‘Sometimes even ultrasound cannot penetrate the deaf ears of pessimists’. Therefore, it is vital that certainly initially those decisions are backed up by the second opinion of experts. The novice and even experienced practitioner who observes the ‘phone a friend’ approach, will go far!
So where does the evidence lie?
As we strive to introduce POCUS into training as early as possible, it must be mentioned that outcome data for it is in its relative infancy. A recent ED trial utilising POCUS to manage shocked patients did not yield any survival benefit Vs those who received the usual care.37 The same result was borne out in a second trial focussing on survival outcomes using POCUS in cardiac arrest versus usual care; no purported survival benefit.38 Finally, the third in this trial series found that ED cardiac arrest patients with cardiac activity on POCUS had improved clinical outcomes as compared with patients not receiving POCUS, and patients with no activity on POCUS.39 Outcome data for the use of POCUS within the ICU setting are slowly emerging. A recent study showed that regular incorporation of POCUS into morning ICU rounds was associated with shortened duration of mandatory ventilation (MV) and length of stay in ICU. This may have been due to associated reduced fluid administration.40
Conclusion
When properly mentored with a solid governance infrastructure, the addition of a fifth pillar into the traditional examination subset with insonation can only benefit our patients. POCUS is not a replacement for a good physical examination, nor is it a replacement for detailed full-scale imaging. Portable or pocket US devices have advanced with vigour; smaller, faster, better and infinitely more convenient to practitioners, forming an ideal springboard to advancing both experienced and novice sonographers. Could the panacea for all patients, in the future, be an US-assisted clinical examination augmented by pocket devices? The stethoscope added benefit to so many, but US may now replace it. The examination sphere is getting larger as the devices get smaller. Is ‘from pocket to POCUS’, the future of US training and indeed clinical examination…we think so!
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Jonathan N Wilkinson https://orcid.org/0000-0001-6175-4576
References
- 1.https://www.itnonline.com/content/mount-sinai-school-medicine-gives-pocket-ultrasound-devices-its-students (accessed 2 November 2019).
- 2.https://www.mobihealthnews.com/news/north-america/uc-irvine-medical-school-gifts-butterfly-handheld-ultrasounds-its-whole-class (accessed 3 November 2019).
- 3.Elder A, Japp A, Verghese A. How valuable is physical examination of the cardiovascular system? Br Med J 2016; 354: i3309. [DOI] [PubMed] [Google Scholar]
- 4.Herrle SR, Corbett EC, Jr, Fagan MJ, et al. Bayes’ theorem and the physical examination: probability assessment and diagnostic decision making. Acad Med 2011; 86: 618–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehta M, Jacobson T, Peters D, et al. Handheld ultrasound versus physical examination in patients referred for transthoracic echocardiography for a suspected cardiac condition. JACC Cardiovasc Imaging 2014; 7: 983–990. [DOI] [PubMed] [Google Scholar]
- 6.Mjolstad OC, Dalen H, Graven T, et al. Routinely adding ultrasound examinations by pocket-sized ultrasound devices improves inpatient diagnostics in a medical department. Eur J Intern Med 2012; 23: 185–191. [DOI] [PubMed] [Google Scholar]
- 7.Skjetne K, Graven T, Haugen BO, et al. Diagnostic influence of cardiovascular screening by pocket-size ultrasound in a cardiac unit. Eur J Echocardiogr 2011; 12: 737–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haji DL, Royse A, Royse CF. Review article: clinical impact of non-cardiologist-performed transthoracic echocardiography in emergency medicine, intensive care medicine and anaesthesia. Emerg Med Australas 2013; 25: 4–12. [DOI] [PubMed] [Google Scholar]
- 9.Goonewardena SN, Gemignani A, Ronan A, et al. Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging 2008; 1: 595–601. [DOI] [PubMed] [Google Scholar]
- 10.Prinz C, Voigt JU. Diagnostic accuracy of a hand-held ultrasound scanner in routine patients referred for echocardiography. J Am Soc Echocardiogr 2011; 24: 111–116. [DOI] [PubMed] [Google Scholar]
- 11.Panoulas VF, Daigeler AL, Malaweera ASN, et al. Pocket-size hand-held cardiac ultrasound as an adjunct to clinical examination in the hands of medical students and junior doctors. Eur Heart J Cardiovasc Imaging 2013; 14: 323–330. [DOI] [PubMed] [Google Scholar]
- 12.Kobal SL, Trento L, Baharami S, et al. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol 2005; 96: 1002–1006. [DOI] [PubMed] [Google Scholar]
- 13.Narula J, Chandrashekhar Y, Braunwald E. Time to add a fifth pillar to bedside physical examination: inspection, palpation, percussion, auscultation, and insonation. JAMA Cardiol 2018; 3: 346–350. [DOI] [PubMed] [Google Scholar]
- 14.Wilkinson JN, et al. The final battle – portable ultrasound devices, https://criticalcarenorthampton.com/2019/04/15/the-final-battle-portable-ultrasound-devices/2019 (accessed 8 November 2019).
- 15.Portable Ultrasound, https://en.wikipedia.org/wiki/Portable_ultrasound (accessed 11 November 2019).
- 16.Russotto V, Cortegiani A, Raineri SM, et al. Bacterial contamination of inanimate surfaces and equipment in the intensive care unit. J Intens Care 2015; 3: 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marinella MA, Pierson C, Chenoweth C. The stethoscope: a potential source of nosocomial infection? Arch Intern Med 1997; 157: 786–790. [DOI] [PubMed] [Google Scholar]
- 18.Greaves K, et al. The use of hand-carried ultrasound in the hospital setting—a cost-effective analysis. J Am Soc Echocardiogr 2005; 18: 620–625. [DOI] [PubMed] [Google Scholar]
- 19.Portable Ultrasound, improves patient understanding, quality of care, https://www.beckershospitalreview.com/quality/portable-ultrasound-improves-patient-understanding-quality-of-care.html (accessed 11 November 2019).
- 20.Coffin C. Work-related musculoskeletal disorders in sonographers: a review of causes and types of injury and best practices for reducing injury risk. DOI: 10.2147/RMI.S34724 (accessed 2 November 2019).
- 21.Harrison G, Harris A. Work-related musculoskeletal disorders in ultrasound: can you reduce risk? Ultrasound 2015; 23: 224–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mulvagh SL, et al. Handheld ultrasound devices and the training conundrum: how to get to seeing is believing. J Am Soc Echocardiogr 2014; 27: 310–313. [DOI] [PubMed]
- 23.Decara JM, Kirkpatrick JN, Spencer KT, et al. Use of hand-carried ultrasound devices to augment the accuracy of medical student bedside cardiac diagnoses. J Am Soc Echocardiogr 2005; 18: 257–263. [DOI] [PubMed] [Google Scholar]
- 24.https://uk.reuters.com/video/2019/10/02/doctor-diagnoses-his-own-cancer-with-an?videoId=607443258 (accessed 6 November 2019).
- 25.Bobek E, Tversky B. Creating visual explanations improves learning. Cogn Res Princ Implic 2016; 1: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Swamy M, Searle RF. Anatomy teaching with portable ultrasound to medical students. BMC Med Educ 2012; 12: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saxhaug L. A web of science search for publications on “handheld ultrasound”, “hand carried ultrasound” and “pocked sized ultrasound” (formulated 1 November 2019).
- 28.Andersen GN, et al. Diagnostic influence of routine point-of-care pocket-size ultrasound examinations performed by medical residents. J Ultrasound Med 2015; 34: 627–636. [DOI] [PubMed] [Google Scholar]
- 29.Grogan DR, et al. Complications associated with thoracentesis. A prospective, randomized study comparing three different methods. Arch Intern Med 1990; 150: 873–877. [DOI] [PubMed] [Google Scholar]
- 30.Raptopoulos V, et al. Factors affecting the development of pneumothorax associated with thoracentesis. RSAJR Am J Roentgenol 1991; 156: 917–920. [DOI] [PubMed] [Google Scholar]
- 31.Barrington MJ. Did ultrasound fulfill the promise of safety in regional anesthesia? Curr Opin Anaesthesiol 2018; 31: 649–655. [DOI] [PubMed] [Google Scholar]
- 32.Sazdov D. Comparative analysis of ultrasound guided central venous cathetarization compared to blind cathetarization. Pril (Makedon Akad Nauk Umet Odd Med Nauki) 2017; 38: 107–114. [DOI] [PubMed] [Google Scholar]
- 33.www.criticalcarenorthampton.com.
- 34.www.lifeinthefastlane.com.
- 35.www.5minutesono.com.
- 36.www.thepocusalas.com.
- 37.Atkinson PR, Milne J. Does point-of-care ultrasonography improve clinical outcomes in emergency department patients with undifferentiated hypotension? An international randomized controlled trial from the SHoC-ED investigators. Ann Emerg Med 2018; 72: 478–489. [DOI] [PubMed] [Google Scholar]
- 38.Beckett N, Atkinson PR. Is there an association between the use of cardiac ultrasound and survival outcomes in patients arriving to the emergency department in cardiac arrest? The second sonography in hypotension and cardiac arrest in the emergency department (SHOC-ED 2) study. Cambridge University Press 2016; 18: S70. [Google Scholar]
- 39.Atkinson PR, Beckett N, French J, et al. Does point-of-care ultrasound use impact resuscitation length, rates of intervention, and clinical outcomes during cardiac arrest? A study from the sonography in hypotension and cardiac arrest in the emergency department (SHoC-ED) investigators. Cureus 2019; 11: e4456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen DZ, Hong Y. Incorporation of point-of-care ultrasound into morning round is associated with improvement in clinical outcomes in critically ill patients with sepsis. J Clin Anesth 2018; 48: 62–66. [DOI] [PubMed] [Google Scholar]