Purpose of review
The paper aims to provide an overview of the psychological and behavioural impacts of the COVID-19 pandemic, with a focus on variations in behavioural response in different geographical areas due to the existence of different social-cultural contexts.
Recent findings
Whilst anxiety, depression and economic stressors are common findings worldwide, specific behavioural responses are heavily influenced by government stances, misinformation, conspiratorialism and competing demands of resource scarcity. This has led to very different understandings of the pandemic even in geographically close areas, and more so when comparing disparate regions such as Africa, South America and Europe. The paper also comments on the absence of robust evidence regarding increases of suicidality and violence on a global level, whilst noting evidence certainly exists in specific regions.
Summary
The psychological and behavioural impact of COVID is heavily influenced by the local lens. Beyond a very broad brush approaches, expected behaviours from one area cannot easily be extrapolated to others. Where possible, clinicians should be guided by local data, ideally placing expectations of responses in a cultural context.
Keywords: behavioural, conspiratorialism, COVID, global, misinformation
INTRODUCTION
The purpose of this review is to provide a broad overview of behavioural and psychological responses to the COVID-19 pandemic amongst the general adult population. It first discusses globally relevant phenomena including emotional responses, suicidality, violence and conspiratorialism. It then discusses geographical variations of response, taking into account cultural, political and economic factors. Particular note is made of areas under-represented in literature.
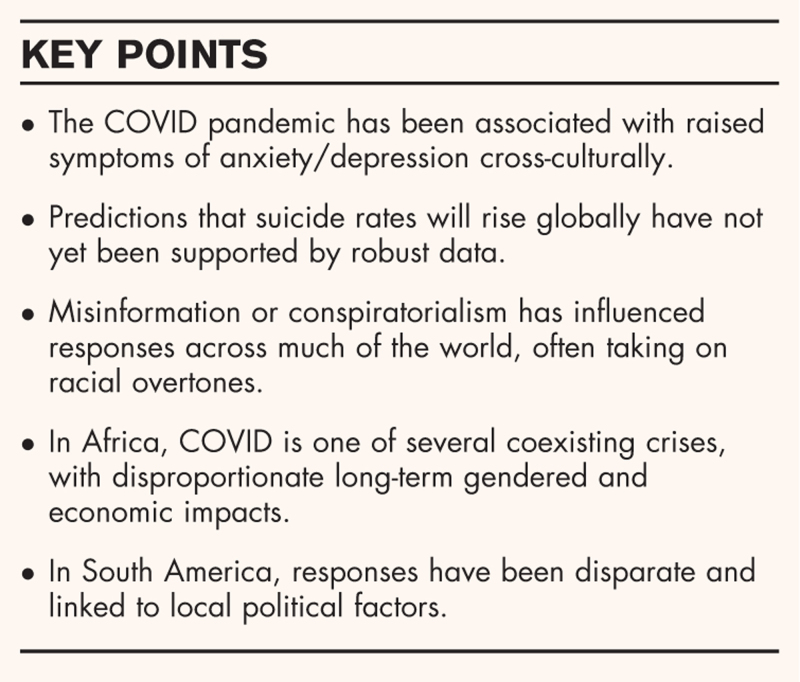
Box 1.
no caption available
GLOBAL COMMONALITIES
Many responses of the general population to the COVID-19 pandemic match predictions based on previous respiratory epidemics. Systematic reviews have shown a cross-culturally raised prevalence of symptoms of anxiety and depression [1▪,2▪▪,3]. Individual studies suggested higher risks sometimes linked to the female gender and lower socio-economic status [4▪,5▪]. There are global concerns about both direct risks of infection and longer-term economic consequences. Social distancing has disrupted traditional means of dealing with mortality-related grief potentially causing its prolongation; though the breadth of that impact is filtered through age demographics [6▪–8▪]. It has also been linked to negative changes in diet and exercise [9▪▪]. Unfortunately attempts to globally aggregate such information have been skewed by disproportionate national representation due to the staggered chronology of the pandemic.
Many attempts to assess the COVID-linked emotional valences focused upon social networks. These have shown online discourse focused upon fear and anger, although positive emotions were also noted [10,11▪,12]. Given unequal global social media uptake, it is unclear how representative this is of the global population. Preexisting temperament has been demonstrated to affect behaviour and distress related to the pandemic. One study suggested depressive, anxious and cyclothymic temperaments and insecure-anxious attachment predisposed to developing significant distress [13▪]. A further study of COVID-19 recoverees concurred with this [14]. Openness, conscientiousness, agreeableness and neuroticism, alongside actual and perceived COVID risk, contributed to likelihood to shelter in place [15▪▪]. Preexisting temperament includes a genetic component, which has also been shown to affect COVID-distress response [16].
Based on previous epidemics, predictions of social isolation, and rising unemployment there was a belief suicide rates would rise [17,18▪,19,20▪▪]. This is little evidence this eventuated, particularly in socioeconomically advantaged countries [21,22,23▪,24▪]. It has been posited a ‘pulling together’ phenomenon may have accounted for initially reduced suicide rates in countries such as Norway or Japan [24▪]. There was a similar expectation of increased levels of partner violence, based on factors including increased exposure to perpetrators, stress, increased alcohol consumption, and reduced access overstretched support or emergency services. However whilst there has been significant regional evidence, there is a paucity of high-quality data on the topic [25,26▪▪].
A rise in conspiratorialism mediated by governmental actions was commonplace. It has been suggested that high volumes of information, the presence of negative emotions and external blame attribution increased conspiratorialism, whilst raised perception of self-control reduced it [27▪▪]. It was suggested preventive behaviours were supported by conspiratorial individuals more when not government driven, although mitigated by concerns of risk to self [28▪▪]. Studies showed negative links between belief in conspiracies and health protective behaviours [29▪]. It has not been uncommon for COVID-linked misinformation to adopt racial overtones. As COVID is often asymptomatic, racial traits may have been used to identify purported carriers Social stigma has appeared to spread along racial and class lines rather than actual infection status [30▪,31]. There are suggestions scapegoating is further exacerbated by online bots, with the points of division subject to regional variation. For example, American bots focused on race and nationality, whereas Phillippine bots focused on gender and religion [32]. Finally, perceptions of scarcity and uncertainty appeared to drive panic buying behaviours, reported in countries including the USA, UK, India, China and North Korea [33]. Suggested contributing factors include perceived threats, scarcity, and fears of the unknown, which trigger purchasing as an attempt to reassert control. All would be common in a combined pandemic and global recession [34▪▪]. An overall increase in alcohol and substance use has also been noted, although less than predicted by expert opinion [26▪▪].
GEOGRAPHICAL VARIATION
Africa
The psychosocial challenges of the African response to COVID have been very different from those in the Western World, with COVID presenting as one of a multiplicity of crises. Whilst quarantining in some African countries has led to increased levels of loneliness, in others it can seem economically unfeasible [35,36▪]. This is particularly true in countries with food scarcity. Adherence to guidelines has often had to compete with other life necessities, such as in Sub-Saharan Africa where hygiene has been hampered by shortages of clean water [37]. Regarding guideline implementation, much of the information provided within Africa has been identified as inadequate and often recycled from previous epidemics [38]. Due partially to low levels of internet access and health literacy, the impacts of the infodemic in Africa has been filtered through religious and community leaders [36▪]. This has provoked development of cultural innovations, such as the provision of information in easily memorised song form in Ghana [39]. On occasions treatment is available, trust is likely impeded by the vast African market for counterfeit and substandard drugs. This is estimated to be worth approximately $30.5 billion, with 18.7% of drugs substandard [40,41]. The potential for fake vaccines is a particular concern. Whilst the Lome initiative addressing this was signed in January 2020, by the time the pandemic struck safeguards were not fully implemented [42]. Economically, the close ties between China and Africa via importation and mining predicts a rise in local commodity prices. Combined with the simultaneous withdrawal of Chinese investment, cessation of tourism and a reduction in oil prices this has potentially disastrous psychosocial impact for communities established during the Sino-African boom [43▪].
The gendered impacts of COVID have been particularly stark in Africa. Disruption to education and its associated protections have disproportionately affected females. In Kenya, there has been a sharp increase in adolescents presenting to health facilities, with the causative abuse being referred to as a ‘shadow pandemic’ [44]. Reduced African access to contraceptives due to lockdowns is expected to contribute to seven million unintended pregnancies [45▪]. Despite these factors, morbidity and mortality rates in Africa have been favourable compared to Europe and the United States, potentially due to a low average population age and a COVID-protective climate [46]. Africa is thus likely to represent an area where the long-term societal impacts of COVID are disproportionate to its physical health sequelae.
Asia
A preponderance of early COVID studies focused on China, and the impacts from strict lockdowns imposed by the centralised government. These showed increases in anxiety and depressive symptoms that were more significant in women and worsened with lockdown [47,48▪]. Some later studies have interestingly reported further worsening of symptoms in the ‘resolution’ phase of COVID, potentially due to economic impacts [49▪]. In contrast to China's legally enforced lockdown, Japanese law generally only grants governments the power of request in administering lockdowns, with adherence dependent on peer pressure [50]. Japan may have been expected to traverse the pandemic well due its robust health system, preexisting mask use and socially distanced customs. However by the late 2020 COVID was spreading rapidly nonetheless. Blame was cast upon guideline fatigue and a governmental program to increase domestic tourism [51]. This reversal led to increased levels of psychological distress, alongside a reversal in the initial decline in suicide rates [52,53,54▪]. It was noted that much of the increase in suicide rate was found amongst females and younger workers, with these groups disproportionately affected by unemployment.
Despite a high initial disease burden, experience with the 2015 MERS outbreak left South Korea well-positioned for COVID. It is suggested this experience helped to drive adherence even with non governmentally enforced guidelines [55]. The pandemic was generally localised to specific clusters, with the extent of psychosocial distress linked to local COVID prevalence [56▪]. In Thailand, early surveys showed good understanding of COVID and its prevention alongside low levels of community transmission [57▪]. Early response was also marked by levels of community volunteering higher than global norms [58]. Whilst initially Thai citizens received COVID-related information heavily from social media, studies suggested over time they were more likely to receive it from television, with concomitant increases in evidence-based behaviour. Interestingly, anxiety levels were not consistently affected by gender [59]. Follow-up studies have not been repeated since Thailand's second wave. The impact of COVID on the subcontinent has been well studied and will not be discussed in depth. Despite locking down 1.3 billion people, within India social distancing recommendations were often difficult to follow amongst the urban poor [60▪▪]. Sudden lockdowns caused forced movement of migrant workers, second only in scale to the 1947 partition. Such workers were often isolated and particularly socially vulnerable [60▪▪,61]. Postquarantine ostracisation further exacerbated this [62]. Despite localised success stories, much of India reports heightened COVID-linked anxiety and economic insecurity [63▪]. In Bangladesh, urban respondents reported an income drop of 75%, with associated reduction in food intake [64] In the Dhaka slums, crowding was endemic, water security variable, and up to 16 families may share a bathroom. Following new government charges for tests and fake testing scandals, testing rates dropped, rendering information unreliable even for researchers, let alone the average citizen [65]. Like India, Pakistan has struggled with misinformation, including theories COVID is an anti-Muslim conspiracy [66]. One survey showed 82% of participants were concerned that social media was driving panic [67]. Due to fear of COVID-linked stigma, residents in some areas were hesitant to seek assistance for other medical conditions [68▪▪]. As in other areas of the globe, altruistic fear for family outweighed fear for self, and economic impacts limited guideline adherence.
Europe and North America
North American and European components of studies generally matched global trends regarding raised levels of anxiety, low mood, violence and fears of economic disruption, with associated impacts on diet and exercise [2▪▪,3,9▪▪,69]. These will consequently not be described in detail. However, one significant factor driving differences was the United States government response to COVID, which has been described as ‘maladaptive denial’ of both facts and implications [70▪]. Belief in the pandemic became linked to political affiliation, with mask wearing becoming a political statement [70▪,71]. Preexisting divisions exacerbated under the combined strain of the pandemic and events such as the death of George Floyd. Rather than the virus acting as a ‘great equaliser’, black communities bore a disproportionate number of cases of COVID [72▪]. This was complicated by their lower trust levels in medical professions [73]. It was suggested that the online-heavy nature of American society rendered in particularly vulnerable to misinformation-driven division. In contrast, Canada underwent a ‘rare moment of cross-partisan consensus’ [74]. Rather than absolute scepticism, opposition supporters split between whether there had been a government over or under reaction [75▪]. Canada and the USA nevertheless shared increased racially motivated violence and discrimination against people of East Asian background [76–78]. Though many surveyed linked this only to recent rhetoric, this echoed historical themes associating Asians with infection [79].
Within Europe, COVID-related worries began as consistently high, but decreased during reopening. Loneliness was more prevalent in youth [80▪▪]. Inactivity and negative dietary changes linked to quarantine, including emotional eating, were noted in much of Europe [9▪▪,81,82,83▪,84]. Some countries reported a differing perception of time within lockdown [85▪▪]. Whilst early in the pandemic in Western Europe there was increased political support for status quo institutions and democracy, by April the 5G coronavirus conspiracy had reached the same online footprint as information supporting quarantine measures. One Polish study suggested 56% of the population believed at least one COVID-linked conspiracy theory, whereas in Britain telephone engineers were directly assaulted [86,87,88▪▪,89▪▪]. In contrast with America, when British antiscientism rose it appeared to be outside partisan divides; this may also be true in other European areas [90].
Oceania
Oceania has been a region lesser affected by COVID. Nations including Micronesia, Samoa and Vanuatu remained transmission free, whereas Kiribati, Palau, Tonga and Tuvalu remain virus free [91]. Kirbati and Palau nonetheless instituted states of emergency. Research on COVID's psychological impacts in these countries is scarce. New Zealand was lauded for exemplary pandemic management, utilising a ‘go early go hard’ strategy to eliminate community transmission whilst incidentally reducing all cause-mortality [92,93▪,94,95▪▪]. Initial restrictions were the highest of any high-income country [96]. Lockdown surveys of distress, wellbeing and violence paralleled international trends, though some showed higher happiness with quarantine conditions [93▪,95▪▪]. There has been little published research into New Zealand mental health since local elimination of COVID. Australia, whilst initially managing COVID well, has struggled with repeated lockdowns. Due to the distances involved, the closure of state borders, and the local nature of clusters, experiences within Australia appear highly varied. Initial psychological responses paralleled other Western Countries, including socioeconomic vulnerabilities. Gender influence was also noted [22,97,98]. An exception to the Oceania trend is Papua New Guinea, where misinformation has reduced uptake of the ‘new normal’. This was exacerbated by political divisions, including the leader of the opposition calling for a suspension of vaccine provision, citing natural Papuan immunity [99]. In this climate is unclear if efforts to modify cultural practises that risk COVID spread, such as haus krai rites, will be successful.
South America
The psychological reaction to COVID in South America has been disparate and politically driven. In Brazil, the president argued against self-isolation and that Brazilians had the strength to ward off the virus [100▪▪]. Limited water supplies and rampant disinformation led to the virus disproportionately harming the socioeconomically disadvantaged. This is particularly true amongst enclaves of quilombolas, and indigenous groups recently identified as ‘at risk of genocide’, who have perceived COVID as an existential threat [101]. In other areas, drug dealers and militia enforced social distancing measures, forming para-states. In contrast, Chilean public health measures were widespread, albeit impaired by housing shortages, profound social unrest and high levels of alcohol and substance abuse. Despite the potentially mitigating public support of lockdowns, COVID appears to have worsened moods, sensations of loneliness, and to have only further exacerbated economic anxiety [102,103,104▪▪]. In Argentina, studies had shown the populace preferred low levels of social distance than other countries, holding numerous customs that could thus spread COVID. There was a suggestion this may leave them unusually susceptible to distancing-related loneliness, though this has not been robustly demonstrated [105,106▪]. Whilst the populace has broadly accepted restrictions, notably regularly applauding health workers during the early pandemic, implementation was marred by concerns of associated gendered violence, mandating a governmental response [107▪].
CONCLUSION
Whilst experiences of anxiety, low mood and fears of economic instability exist worldwide, considerable regional variation remains. In some countries, COVID is one crisis amongst many, whilst in others the argument is whether it is a crisis at all. Variable government attitudes, misinformation and resource scarcity appear three major factors that contribute to geographical differences in psychosocial response worth further investigation.
Acknowledgements
None.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1▪.Krishnamoorthy Y, Nagarajan R, Saya G, Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res 2020; 293:113382. [DOI] [PMC free article] [PubMed] [Google Scholar]; An early meta-analysis of 171,571 participants in regards to anxiety and depression. Studies were largely from China and of poor quality but helped to set the baseline expectation for impacts of COVID.
- 2▪▪.Cénat J, Blais-Rochette C, Kokou-Kpolou C, et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res 2021; 295:113599.doi:10.1016/j.psychres.2020.113599. [DOI] [PMC free article] [PubMed] [Google Scholar]; A meta-analysis, with several non-Chinese countries included. Found no differences in mental health between Healthcare Workers and the general populace. Also found no overall difference based on gender, though some differences were noted in Western and Middle-Eastern studies.
- 3.Necho M, Tsehay M, Birkie M, et al. Prevalence of anxiety, depression, and psychological distress among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Int J Soc Psychiatry 2021; doi:10.1177/00207640211003121. [DOI] [PubMed] [Google Scholar]
- 4▪.Mazza C, Ricci E, Biondi S, et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Health 2020; 17:3165. [DOI] [PMC free article] [PubMed] [Google Scholar]; An Italian study that drew associations between sociodemographic variables and DASS-21 scores during the COVID-19 outbreak. Described a link between female gender and increased DASS-21 during COVID.
- 5▪.Wang GY, Tang SF. Perceived psychosocial health and its sociodemographic correlates in times of the COVID-19 pandemic: a community-based online study in China. Infect Dis Poverty 2020; 9:148. 10.1186/s40249-020-00770-8 [DOI] [PMC free article] [PubMed] [Google Scholar]; A cross-sectional online survey intending to measure hopelessness, loneliness and depression. Discusses the psychosocial impacts of COVID-19 on China well.
- 6▪.Verdery AM, Smith-Greenaway E, Margolis R, Daw J. Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proc Natl Acad Sci USA 2020; 117:17695–17701. [DOI] [PMC free article] [PubMed] [Google Scholar]; Identifies the ripple effect of COVID deaths on the population, which helps to highlight the multiplicative impact of bereavement in disadvantaged communities.
- 7▪.Cardoso É, Silva B, Santos J, Lotério L, et al. The effect of suppressing funeral rituals during the COVID-19 pandemic on bereaved families. Rev Lat Am Enfermagem 2020; 28:e3361.doi:10.1590/1518-8345.4519.3361. [DOI] [PMC free article] [PubMed] [Google Scholar]; A small thematic analysis of online documents from bereaved families during the pandemic that lays out common themes regarding reaction to disrupted funeral rituals.
- 8▪.Eisma M, Tamminga A. Grief before and during the COVID-19 pandemic: multiple group comparisons. J Pain Symptom Manag 2020; 60:e1–e4. [DOI] [PMC free article] [PubMed] [Google Scholar]; An attempt to quantitatively test whether grief levels are higher in a pandemic, and whether recent loss during a pandemic yielded more severe grief reactions than a similar loss before the pandemic.
- 9▪▪.Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 International Online Survey. Nutrients 2020; 12:1583. [DOI] [PMC free article] [PubMed] [Google Scholar]; An online international survey suggesting reduced exercise and more unhealthy eating habits during COVD-19 restrictions. Interestingly reported a reduction in binge drinking.
- 10.Medford R, Saleh S, Sumarsono A, et al. An ‘Infodemic’: leveraging high-volume twitter data to understand early public sentiment for the coronavirus disease 2019 outbreak. Open Forum Infect Dis 2020; 7:ofaa258. 10.1093/ofid/ofaa258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11▪.Lwin MO, Lu J, Sheldenkar A, et al. Global sentiments surrounding the COVID-19 pandemic on twitter: analysis of twitter trends. JMIR Public Health Surveill 2020; 6:e19447.Published 2020 May 22. doi:10.2196/19447. [DOI] [PMC free article] [PubMed] [Google Scholar]; Analysis of 20,325,929 tweets from 7,033,158 unique users stratified by emotion over time, showing initial fear and anger and gradual emergence of positive emotions.
- 12.Xue J, Chen J, Hu R, et al. Twitter discussions and emotions about the COVID-19 pandemic: machine learning approach. J Med Internet Res 2020; 22:e20550.URL: https://www.jmir.org/2020/11/e20550 DOI: 10.2196/20550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13▪.Moccia L, Janiri D, Pepe M, et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav Immun 2020; 87:75–79. [DOI] [PMC free article] [PubMed] [Google Scholar]; Measures Kessler-10 psychological distress scale scores against measures of affective temperament and attachment style to identify predictors of distress in a sample of 500 Italian individuals.
- 14.Janiri D, Kotzalidis GD, Giuseppin G, et al. Psychological distress after covid-19 recovery: reciprocal effects with temperament and emotional dysregulation. An exploratory study of patients over 60 years of age assessed in a postacute care service. Front Psychiatry 2020; 11:590135.doi: 10.3389/fpsyt.2020.590135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15▪▪.Götz FM, Gvirtz A, Galinsky AD, Jachimowicz JM. How personality and policy predict pandemic behavior: understanding sheltering-in-place in 55 countries at the onset of COVID-19. Am Psychol 2021; 76:39–49. [DOI] [PubMed] [Google Scholar]; Draws links between big-5 personality factors, stringency of government policy and tendency to shelter in place, using a sample of 101,005 individuals across 55 countries.
- 16.Rimfeld K, Malanchini M, Allegrini A, et al. Genetic correlates of psychological responses to the COVID-19 crisis in young adult twins in Great Britain. Behav Genet 2021; 51:110–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson NP, Mueller J. Updating the accounts: global mortality of the 1918-1920 ‘Spanish’ influenza pandemic. Bull Hist Med 2002; 76:105–115. [DOI] [PubMed] [Google Scholar]
- 18▪.Banerjee D, Kosagisharaf JR, Sathyanarayana Rao TS. ’The dual pandemic’ of suicide and COVID-19: a biopsychosocial narrative of risks and prevention. Psychiatry Res 2021; 295:113577.doi:10.1016/j.psychres.2020.113577. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper, from early in the pandemic, explains why it is likely that COVID-19 will significant drive up rates of suicide. It outlines several theoretical models for suicide, and highlights risk factors for suicide that worsen in a pandemic.
- 19.Kahil K, Cheaito MA, El Hayek R, et al. Suicide during COVID-19 and other major international respiratory outbreaks: a systematic review. Asian J Psychiatr 2021; 56:102509.doi:10.1016/j.ajp.2020.102509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20▪▪.John A, Pirkis J, Gunnell D, et al. Trends in suicide during the covid-19 pandemic. BMJ 2020; 371:m4352.doi:10.1136/bmj.m4352. [DOI] [PubMed] [Google Scholar]; A concise summary of the absence of consistent evidence of overall increased suicidality linked to COVID.
- 21.15 Faust J, Shah S, Du C, et al. Suicide deaths during the COVID-19 stay-at-home advisory in Massachusetts, March to May 2020. JAMA Network Open 2021; 4:e2034273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leske S, Kõlves K, Crompton D, et al. Real-time suicide mortality data from police reports in Queensland, Australia, during the COVID-19 pandemic: an interrupted time-series analysis. Lancet Psychiatry 2021; 8:58–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23▪.John A, Okolie C, Eyles E, et al. The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: a living systematic review [version 1; peer review: 1 approved, 2 approved with reservations]. F1000Research 2020; 9:1097. 10.12688/f1000research.25522.1 [DOI] [PMC free article] [PubMed] [Google Scholar]; A living systematic review including case studies, cross sectional studies and modelling reviews. Highlights the limited quality of evidence in assessing changes in suicidality and the inability to make causal statements. Limited by many of the sources being preprint reviews or of poor quality.
- 24▪.Ueda M, Nordström R, Matsubayashi T. Suicide and mental health during the COVID-19 pandemic in Japan. J Public Health (Oxf) 2021; doi: 10.1093/pubmed/fdab113. [DOI] [PMC free article] [PubMed] [Google Scholar]; Highlights increase in suicide rates within specific Japanese subgroups such as homemakers and high school students and provides cultural context; illustrates the cultural variability of suicidality as a COVID response.
- 25.Mittal S, Singh T. Gender-based violence during COVID-19 pandemic: a mini-review. Front Glob Womens Health 2020. 4.doi: 10.3389/fgwh.2020.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26▪▪.Abdo C, Miranda EP, Santos CS, et al. Domestic violence and substance abuse during COVID19: a systematic review. Indian J Psychiatry 2020; 62: Suppl S3: 337–342. [DOI] [PMC free article] [PubMed] [Google Scholar]; Identifies the lack of evidence of increased domestic violence linked to COVID, but outlines why this may reflect difficulties in reporting rather than an absence of violence.
- 27▪▪.Kim S, Kim S. Searching for general model of conspiracy theories and its implication for public health policy: analysis of the impacts of political, psychological structural factors on conspiracy beliefs about the COVID-19 Pandemic. Int J Environ Res Public Health 2021; 18:266.https://doi.org/ijerph18010266 [DOI] [PMC free article] [PubMed] [Google Scholar]; Acts as a primer to political, psychological and social structural factors driving COVID-19 conspiracy theories. Identifies 19 variables that appear to affect individual belief in conspiracy theories within the Korean context; many of these may be more broadly applicable.
- 28▪▪.Marinthe G, Brown G, Delouvée S, Jolley D. Looking out for myself: Exploring the relationship between conspiracy mentality, perceived personal risk, and COVID-19 prevention measures. Br J Health Psychol 2020; 25:957–980. [DOI] [PMC free article] [PubMed] [Google Scholar]; Discusses the ways in which people with conspiratorial mentality tend to engage in behaviour, the high impact of who recommends the behavior, and the tendency to follow extreme but not nonextreme health behaviors. Also notes the suppressive impact of the direct threat of COVID; potentially highlighting better ways to communicate with conspiratorial individuals.
- 29▪.Allington D, Duffy B, Wessely S, et al. Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency [published online ahead of print, 2020 Jun 9]. Psychol Med 2020. 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]; A series of UK based questionnaire surveys on COVID-related beliefs outling links between social media use and belief in conspiracy theory, and negative correlations regarding health-protective behavior and belief in conspiracy theories.
- 30▪.Katherine J. Roberto, Andrew F. Johnson, Beth M. Rauhaus. Stigmatization and prejudice during the COVID-19 pandemic. Adm Theory Praxis 2020; 42:364–378. [Google Scholar]; Discusses psychological factors behind COVID-linked stigmatisation and racism, and provides a rapid overview of antiasian xenophobia linked to COVID and its impacts.
- 31.Bhanot D, Singh T, Verma SK, Sharad S. Stigma and discrimination during COVID-19 pandemic. Front Public Health 2021; 8:577018.doi: 10.3389/fpubh.2020.577018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Joshua Uyheng, Kathleen M. Carley. Bots and online hate during the COVID-19 pandemic: case studies in the United States and the Philippines. J Comput Soc Sci 2020; 3:445–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arafat SMY, Kar SK, Menon V, et al. Panic buying: an insight from the content analysis of media reports during COVID-19 pandemic. Neurol Psychiatry. Brain Res 2020; 37:100–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34▪▪.Yuen KF, Wang X, Ma F, Li KX. The psychological causes of panic buying following a health crisis. Int J Environ Res Public Health 2020; 17:3513.Published 2020 May 18. doi:10.3390/ijerph17103513. [DOI] [PMC free article] [PubMed] [Google Scholar]; A systematic review of literature to synthesise the main psychological themes that lead to panic buying, alongside suggestion of strategies to curb future panic buying that would be applicable to the pandemic.
- 35.Padmanabhanunni A, Pretorius TB. The unbearable loneliness of COVID-19: COVID-19-related correlates of loneliness in South Africa in young adults. Psychiatry Res 2021; 296:113658.doi:10.1016/j.psychres.2020.113658, 10.1016/j.psychres.2020.113658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36▪.Coetzee BJ, Kagee A. Structural barriers to adhering to health behaviours in the context of the COVID-19 crisis: considerations for low- and middle-income countries. Glob Public Health 2020; 15:1093–1102. [DOI] [PubMed] [Google Scholar]; Utilises the theoretical domains framework to outline challenges to making behavioral changes related to COVID, outlining the impacts of environmental context, employment, risk salience, information access, demographic factors and sociopolitical context.
- 37.Anim DO, Ofori-Asenso R. Water scarcity and COVID-19 in sub-Saharan Africa. J Infect 2020; 81:e108–e109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Seytre B. Erroneous communication messages on COVID-19 in Africa. Am J Trop Med Hyg 2020; 103:587–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thompson RGA, Nutor JJ, Johnson JK. Communicating awareness about COVID-19 through songs: an example from Ghana. Front Public Health 2021; 8:607830.Published 2021 Jan 18. doi:10.3389/fpubh.2020.607830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.World Health Organization. (2017). WHO global surveillance and monitoring system for substandard and falsified medical products: executive summary. Geneva, World Health Organization. Retrieved from: https://www.who.int/medicines/regulation/ssffc/publications/gsmsreport-sf/en/ Accessed 1 April 2021. [Google Scholar]
- 41.Schneider M, Ho Tu Nam N. Africa and counterfeit pharmaceuticals in the times of COVID-19. J Intellect Proper Law Pract 2020; 15:417–448. [Google Scholar]
- 42.Adepoju P. African nations to criminalise falsified medicine trafficking. Lancet 2020; 395:324.doi:10.1016/s0140-6736(20)30244-0. [DOI] [PubMed] [Google Scholar]
- 43▪.African Union. Impact of the coronavirus (COVID 19) On The African Economy. 2020; Addis Ababa: African Union, https://au.int/sites/default/files/documents/38326-doc-covid-19_impact_on_african_economy.pdfhttps://au.int/sites/default/files/documents/38326-doc-covid-19_impact_on_african_economy.pdf. Accessed April 1, 2020. [Google Scholar]; Outlines the impacts of COVID on the economy in Africa, including potential long term consequences including withdrawal of foreign investment, unemployment, healthcare crisis, social unrest, security challenges and potential food shortages. Whilst it does not lay out the mental health impacts, these could be extrapolated.
- 44. African Institute for Development Policy. Adolescents age 10-19 presenting with pregnancy at health facilities – extract from Kenya Health Information system. 2020. [Data file] Retrieved from https://www.afidep.org/publication/adolescents-age-10-19-presentingwith-pregnancy-at-health-facilities/ Accessed 1 April 2021. [Google Scholar]
- 45▪.Cousins S. COVID-19 has ‘devastating’ effect on women and girls. The Lancet 2020; 396:301–302. [DOI] [PMC free article] [PubMed] [Google Scholar]; A snapshot summary of the international impacts on reproductive health and gender based violence arising from the pandemic.
- 46.Njenga MK, Dawa J, Nanyingi M, et al. Why is there low morbidity and mortality of COVID-19 in Africa? Am J Trop Med Hyg 2020; 103:564–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tian F, Li H, Tian S, et al. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48▪.Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020; 17:1729. [DOI] [PMC free article] [PubMed] [Google Scholar]; An early Chinese online survey using snowball sampling techniques. Sample included 1210 respondent, found moderate to severe anxiety in 28.8%; 75.2% worried about family contracting COVID. Female gender was associated with higher rates of stress, anxiety and depression.
- 49▪.Wang M, Zhao Q, Hu C, et al. Prevalence of psychological disorders in the COVID-19 epidemic in China: a real world cross-sectional study. J Affect Disord 2021; 281:312–320. [DOI] [PMC free article] [PubMed] [Google Scholar]; Chinese cross sectional study of 5676 respondents. Some participants surveyed during outbreak, others during remission of the outbreak. Being in the remission was associated with greater prevalence of severe anxiety and depression. Female respondents had a higher risk of depression and anxiety than males.
- 50.Tanaka M. Covid-19 Japan Update: Legal Framework of the State of Emergency in Japan (Covid-19 Japan Updates Vol 3) City-Yuwa Partners. 2020. Retrieved from https://www.cityyuwa.com/english/COVID-19/shared/pdf/COVID-19_vol3.pdf Accessed 1 April 2021. [Google Scholar]
- 51.Anzai A, Nishiura H. ‘Go To travel’ campaign and travel-associated coronavirus disease 2019 cases: a descriptive analysis. J Clin Med 2021; 10:398. 10.3390/jcm10030398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nishimura Y, Ochi K, Tokumasu K, et al. Impact of the COVID-19 pandemic on the psychological distress of medical students in Japan: cross-sectional survey study. J Med Internet Res 2021; 23:e25232.doi:10.2196/25232, 10.2196/25232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kimura M, Kimura K, Ojima T. Relationships between changes due to COVID-19 pandemic and the depressive and anxiety symptoms among mothers of infants and/or preschoolers: a prospective follow-up study from pre-COVID-19 Japan. BMJ Open 2021; 11:e044826.doi:10.1136/bmjopen-2020-044826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54▪.Tanaka T, Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat hum behav 2021; 5:229–238. [DOI] [PubMed] [Google Scholar]; Exploration of the rebound in suicide rates in Japan's second wave. Increase was noted particulary in Japanese housewives, and further noted that only cities with low suicide rates had significant increases in suicide rates. The suggestion that the effect of the pandemic is to increase suicidality in ‘low risk’ categories, and reasons that the quarantine may have been protective, is explored.
- 55.Juhwan Oh, Jong-Koo Lee, Dan Schwarz, et al. National Response to COVID-19 in the Republic of Korea and Lessons Learned for Other Countries. Health Syst Reform 2020; 6:e1753464.DOI:10.1080/23288604.2020.1753464. [DOI] [PubMed] [Google Scholar]
- 56▪.Kim M, Park I-H, Kang Y-S, et al. Comparison of psychosocial distress in areas with Different COVID-19 prevalence in Korea. Front Psychiatry 2020; 11:1318.doi:10.3389/fpsyt.2020.593105. [DOI] [PMC free article] [PubMed] [Google Scholar]; An online study of 1500 Korean individuals utilising GAD-7, PHQ-9 and a perceived stress scale alongside reported experiences. Comparison was made between areas of high-COVID prevalence and lower. Whilst GAD-7 and PHQ-9 responses were similar between regions, once beyond an incidence threshold stress, sleep and eating disturbances were significantly raised.
- 57▪.Goodwin R, Wiwattanapantuwong J, Tuicomepee A, Suttiwan P, et al. Anxiety, perceived control and pandemic behaviour in Thailand during COVID-19: results from a national survey. J Psychiatr Res 2021; 135:212–217. [DOI] [PMC free article] [PubMed] [Google Scholar]; Survey of 1000 individuals in Thailand measuring anxiety, knowledge of COVID, control and nature of pandemic behaviors. Repeated an earlier survey- compared to this, found that levels of anxiety were similar but that levels of perceived control had dropped. More anxious individuals were noted to perform less evidence based behaviors.
- 58.Marome W, Shaw R. COVID-19 response in Thailand and its implications on future preparedness. Int J Environ Res Public Health 2021; 18:1089. 10.3390/ijerph18031089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Goodwin R. Anxiety and public responses to covid-19: early data from Thailand. J Psychiatr Res 2020; 129:118–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60▪▪.Sengupta S, Jha M. Social policy, COVID-19 and impoverished migrants: challenges and prospects in locked down India. Int J Commun Soc Dev 2020; 2:152–172. [Google Scholar]; The paper outlines in detail the experiences of the migrant workers and informal who experienced the two-month COVID lockdown, noting the homelessness, violence and economic instability that were associated.
- 61.Choudhari R. COVID 19 pandemic: mental health challenges of internal migrant workers of India. Asian J Psychiatr 2020; 54:102254.doi:10.1016/j.ajp.2020.102254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jha SS, Lahiri A. Domestic migrant workers in India returning to their homes: emerging socioeconomic and health challenges during the COVID-19 pandemic. Rural Remote Health 2020; 20:6186.doi: 10.22605/RRH6186. Epub 2020 Nov 20. PMID: 33213180. [DOI] [PubMed] [Google Scholar]
- 63▪.Dubey S, Biswas P, Ghosh R, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr 2020; 14:779–788. [DOI] [PMC free article] [PubMed] [Google Scholar]; A broad commentary piece on the impacts of COVID, noting corona-stigma, quarantine, isolation, the infodemic, predominantly comparing China and India.
- 64.Rahman HZ, Matin I et al. ‘Livelihoods, Coping, and Support during the Covid-19 Crisis’. Dhaka, Bangladesh: PPRC. 2020. Retrieved from: https://knowledge4policy.ec.europa.eu/publication/livelihoods-coping-support-during-covid-19-crisis_en. Accessed 1 April 2021. [Google Scholar]
- 65.Cousins S. Bangladesh's COVID-19 testing criticised. Lancet 2020; 396:591.doi:10.1016/s0140-6736 (20)31819-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Khan YH, Mallhi TH, Alotaibi NH, et al. Threat of COVID-19 vaccine hesitancy in pakistan: the need for measures to neutralize misleading narratives. Am J Trop Med Hyg 2020; 103:603–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Balkhi F, Nasir A, Zehra A, Riaz R. Psychological and behavioral response to the coronavirus (COVID-19) pandemic. Cureus 2020; 12:e7923.doi: 10.7759/cureus.7923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68▪▪.Ahmed SAKS, Ajisola M, Azeem K, et al. Improving Health in Slums Collaborative. Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: results of pre-COVID and COVID-19 lockdown stakeholder engagements. BMJ Glob Health 2020; 5:e003042.doi: 10.1136/bmjgh-2020-003042. [DOI] [PMC free article] [PubMed] [Google Scholar]; A multinational series of interviews in seven slum communities, conducted before and during the pandemic. Major limitations in mental health support was noted, combined with reduction of services, increased poverty and increased stigma in seeking medical help. Residents were instead turning more to self treatment or home remedies.
- 69.Bhutani S, vanDellen MR, Cooper JA. Longitudinal weight gain and related risk behaviors during the COVID-19 pandemic in adults in the US. Nutrients 2021; 13:671.doi: 10.3390/nu13020671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70▪.Weidner C, II, Nelson L. The role of power-addiction and maladaptive denial in the US federal COVID-19 response. Int J Public Leadersh 2020; 17:19–38. [Google Scholar]; Weidner succinctly outlines the political pressures that led to the behavioral splits and COVID-denial within America.
- 71.Motta M, Stecula D, Farhart C. How right-leaning media coverage of COVID-19 facilitated the spread of misinformation in the early stages of the pandemic in the US. Can J Polit Sci 2020; 53:335–342. [Google Scholar]
- 72▪.Poteat T, Millett G, Nelson LE, Beyrer C. Understanding COVID-19 risks and vulnerabilities among black communities in America: The Lethal Force of Syndemics. Ann Epidemiol 2020; 47:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]; Outlines the historical and political factors leading the racialisation of COVID, assisting in better understanding how the community has reacted.
- 73.Alang S, McAlpine DD, Hardeman R. Police brutality and mistrust in medical institutions. J Racial Ethn Health Disparities 2020; 7:760–768. [DOI] [PubMed] [Google Scholar]
- 74.Merkley E, Bridgman A, Loewen PJ, et al. A rare moment of cross-partisan consensus: elite and public response to the COVID-19 pandemic in Canada. Can J Polit Sci 2020; 53:311–318. [Google Scholar]
- 75▪.Pickup M, Stecula D, van der Linden C. Novel coronavirus, old partisanship: COVID-19 attitudes and behaviours in the United States and Canada. Can J Polit Sci 2020; 53:357–364. [Google Scholar]; A brief paper that highlights that whilst partisan lean may heavily affect perceptions of a crisis, that it is significantly less likely to directly affect behavior.
- 76.Cheah C, Wang C, Ren H, et al. COVID-19 racism and mental health in Chinese American Families. Pediatrics 2020; 146:e2020021816.doi:10.1542/peds.2020-021816. [DOI] [PubMed] [Google Scholar]
- 77.Xu J, Sun G, Cao W, et al. Stigma, discrimination, and hate crimes in Chinese-speaking world amid covid-19 pandemic. Asian J Criminol 2021; 16:51–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kong, J, Ip J et al. A Year of Racist Attacks: Anti Asian racism across Canada one year into the COVID-19 Pandemic. Toronto, Canada. Chinese Canadian National Council Toronto Chapter. 2020. Available online from: https://mcusercontent.com/9fbfd2cf7b2a8256f770fc35c/files/35c9daca-3fd4-46f4-a883-c09b8c12bbca/covidracism_final_report.pdf. Accessed 1 April 2021. [Google Scholar]
- 79.White A. Historical linkages: epidemic threat, economic risk, and xenophobia. Lancet 2020; 395:1250–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80▪▪.Varga T, Bu F, Dissing A, Elsenburg L, et al. Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: a longitudinal analysis of 200,000 Western and Northern Europeans. Lancet Regional Health 2021; 2:100020. [DOI] [PMC free article] [PubMed] [Google Scholar]; A study of 200,000 individuals over 4 countries measuring worry, loneliness, precautionary behaviors and COVID-linked experiences. Demonstrates a downwards trend for worries over time, identifies general similarities in trends. Loneliness was more common in youth, women, and those with history of mental illness. The Netherlands showed lower levels of worry and loneliness.
- 81.Papandreou C, Arija V, Aretouli E, et al. Comparing eating behaviours, and symptoms of depression and anxiety between Spain and Greece during the COVID-19 outbreak: cross-sectional analysis of two different confinement strategies. Eur Eat Disord Rev 2020; 28:836–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Brailovskaia J, Cosci F, Mansueto G, et al. The association between depression symptoms, psychological burden caused by Covid-19 and physical activity: an investigation in Germany, Italy, Russia, and Spain. Psychiatry Res 2021; 295:113596.doi: 10.1016/j.psychres.2020.113596. Epub 2020 Nov 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83▪.Coulthard H, Sharps M, Cunliffe L, van den Tol A. Eating in the lockdown during the Covid 19 pandemic; self-reported changes in eating behaviour, and associations with BMI, eating style, coping and health anxiety. Appetite 2021; 161:105082.doi: 10.1016/j.appet.2020.105082. Epub 2021 Jan 18. [DOI] [PMC free article] [PubMed] [Google Scholar]; A UK study of 620 individuals reporting changes to eating patterns during lockdown. Increases in high energy dense food consumption overall were noted, associated particularly with health anxiety, prelockdown eating behavior and female gender. Higher BMI was associated with emotional eating. For many other behaviors the majority of people reported nil change.
- 84.Bemanian M, Mæland S, Blomhoff R, et al. Emotional eating in relation to worries and psychological distress amid the COVID-19 pandemic: a population-based survey on adults in Norway. Int J Environ Res Public Health 2020; 18:130.doi: 10.3390/ijerph18010130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85▪▪.Droit-Volet S, Gil S, Martinelli N, et al. Time and Covid-19 stress in the lockdown situation: Time free, "Dying" of boredom and sadness. PLoS One 2020; 15:e0236465.Published 2020 Aug 10. doi:10.1371/journal.pone.0236465. [DOI] [PMC free article] [PubMed] [Google Scholar]; A study of 4634 French participants on subjective experience of time in COVID, an area much discussed in the media but little studied. Compared against stress levels, anxiety and emotional dimensions. TIme appeared to slow with decreased happiness and increased boredom, rather than directly with stress.
- 86.Duplaga M. The determinants of conspiracy beliefs related to the COVID-19 pandemic in a nationally representative sample of internet users. Int J Environ Res Public Health 2020; 17:7818.doi: 10.3390/ijerph17217818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jolley D, Paterson J. Pylons ablaze: Examining the role of 5G COVID-19 conspiracy beliefs and support for violence. Br J Soc Psychol 2020; 59:628–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88▪▪.Bol D, Giani M, Blais A, Loeweb P. The effect of COVID-19 lockdowns on political support: Some good news for democracy? Eur J Polit Res 2020; 60:497–505. [Google Scholar]; An online survey of 15 European countries that encompassed both early and immediately prelockdown. Showed increased support of the status quo. Little evidence this is due to a rally round-the-flag or increased airtime driven effects. Suggests that main mechanism is retrospective performance evaluation, ie. citizens understanding the benefits of confinement.
- 89▪▪.Vériter S, Bjola C, Koops J. Tackling COVID-19 disinformation: internal and external challenges for the European Union. Hague J Dipl 2020; 15:569–582. [Google Scholar]; Outlines the scale of COVID-disinformation facing the EU, including the manner in which it was blocking out correct information. Discusses the longer term impacts to culture and behavior, its appeal and the need for cognitive resilience.
- 90.Maher P, MacCarron P, Quayle M. Mapping public health responses with attitude networks: the emergence of opinion-based groups in the UK's early COVID-19 response phase. Br J Soc Psychol 2020; 59:641–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.World Health Organisation. World Health Organisation COVID 19 Dashboard Data Table. 2021. [Data File] Available online from: https://covid19.who.int/WHO-COVID-19-global-table-data.csv. Accessed 1 April 2021. [Google Scholar]
- 92.Jefferies S, French N, Gilkison C, Graham G, et al. COVID-19 in New Zealand and the impact of the national response: a descriptive epidemiological study. Lancet Public Health 2020; 5:e612–e623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93▪.Every-Palmer S, Jenkins M, Gendall P, et al. Psychological distress, anxiety, family violence, suicidality, and wellbeing in New Zealand during the COVID-19 lockdown: a cross-sectional study. PLoS One 2020; 15:e0241658.Published 2020 Nov 4. doi:10.1371/journal.pone.0241658. [DOI] [PMC free article] [PubMed] [Google Scholar]; Online survey of 2416 individuals during the New Zealand lockdown. 30.3% scored above moderate distress on the K10; rates slightly higher in females. Specifically queried positive experiences linked to lockdown. 81% of the sample were happy with lockdown living circumstances; most respondents found it easy to maintain contact with those outside of home.
- 94.Kung S, Doppen M, Black M, et al. Reduced mortality in New Zealand during the COVID-19 pandemic. Lancet 2021; 397:25.doi:10.1016/S0140-6736(20)32647-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95▪▪.14 Faulkner J, O’Brien W, McGrane B, et al. Physical activity, mental health and well being of adults during initial COVID-19 containment strategies: a multicountry cross-sectional analysis,. J Sci Med Sport 2021; 24:320–326. [DOI] [PMC free article] [PubMed] [Google Scholar]; Multinational comparison in changes in exercise and wellbeing during early COVID-containment via an online survey. Depression, stress and anxiety were lower in New Zealand compared to other countries. UK and Australia showed the greatest negative change in exercise behavior, NZ the least. Men and young adults more likely to have negative exercise changes.
- 96.Hale T, Angrist N, Goldszmidt R, et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat Hum Behav 2021; 5:529–538. [DOI] [PubMed] [Google Scholar]
- 97.Fisher J, Tran T, Hammarberg K, et al. Mental health of people in Australia in the first month of COVID-19 restrictions: a national survey. Med J Aust 2020; 213:458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hammarberg K, Tran T, Kirkman M, Fisher J. Sex and age differences in clinically significant symptoms of depression and anxiety among people in Australia in the first month of COVID-19 restrictions: a national survey. BMJ Open 2020; 10:e042696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Government of Papua New Guinea Leader of the Opposition. Media statement marape and ministers must be first in line. Waigani: Papua New Guinea National Parliament; 2021. [Google Scholar]
- 100▪▪.Ortega F, Orsini M. Governing COVID-19 without government in Brazil: ignorance, neoliberal authoritarianism, and the collapse of public health leadership. Glob Public Health 2020; 15:1257–1277. [DOI] [PubMed] [Google Scholar]; An overview of the political, psycho-cultural and religious trends leading to denialism within areas of Brazil. Provides both cross-cultural context and the common psychological mechanisms by which uncomfortable knowledge is managed on a state level and why populations often accept them, potentially extrapolatable to other contexts.
- 101.Polidoro M, de Assis Mendonça F, Meneghel SN, et al. Territories under siege: risks of the decimation of indigenous and Quilombolas peoples in the context of COVID-19 in South Brazil. J Racial Ethn Health Disparities 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Caqueo-Urízar A, Urzúa A, Aragón-Caqueo D, et al. Mental health and the COVID-19 pandemic in Chile. Psychol Trauma 2020; 12:521–523. [DOI] [PubMed] [Google Scholar]
- 103.Fischman P, Irarrazaval M. Debate: Mental health, social crisis and the COVID-19 pandemic in Chile. Child Adolesc Ment Health 2020; 25:256–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104▪▪.Blukacz A, Cabieses B, Markkula N. Inequities in mental health and mental healthcare between international immigrants and locals in Chile: a narrative review. Int J Equity Health 2020; 19:197. 10.1186/s12939-020-01312-2 [DOI] [PMC free article] [PubMed] [Google Scholar]; Provides a narrative review of the mental healthcare inequities present in Chile. This includes commentary on the rigidity of the social structure, the need for social capital and the deficits and discrimination in health coverage, including ‘rationing’ through prioritisation of diseases. Whilst not explicitly COVID-focused, identifies many of the weaknesses that were struck by the pandemic.
- 105.Torrente F, Yoris A, Low DM, et al. Sooner than you think: a very early affective reaction to the COVID-19 pandemic and quarantine in Argentina. J Affect Disord 2021; 282:495–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106▪.Gokmen Y, Turen U, Erdem H, Tokmak İ. National preferred interpersonal distance curbs the spread of COVID-19: a cross-country analysis. Disaster Med Public Health Prep 2020. 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]; Utilises data regarding national based distance preferences regarding intimate, personal, social and public distances and compares this with national spreads of COVID-19. Highlights the importance of prexisting cultural behavior patterns on pandemics.
- 107▪.Polischuk L, Fay D. Administrative response to consequences of COVID-19 emergency responses: observations and implications from gender-based violence in Argentina. Am Rev Public Admin 2020; 50:675–684. [Google Scholar]; Outlines levels of gender-based violence in Argentina linked to the pandemic, highlighting underlying structural causes. Describes and critiques governmental responses to limit this on a national and provincial level.