Abstract
Background
There are multiple options for the treatment of thumb carpometacarpal joint osteoarthritis (CMC1 OA), with evidence for pain relief and improved function. Although simple trapeziectomy has the lowest complication risk, tendon suspension of the first metacarpal and interposition is still the most commonly used surgical procedure in patients with CMC1 OA. Although there are several reports of good short-term results after trapeziectomy and tendon suspension-interposition arthroplasty, few studies have evaluated long-term outcomes. This study is one of the largest and longest follow-up evaluations of a cohort of patients with CMC1 OA who were treated with trapeziectomy and suspension-interposition arthroplasty, capturing 96% of the original cohort for evaluation.
Questions/purposes
(1) After trapeziectomy and tendon suspension surgery, what are the long-term, patient-reported outcomes and clinical measurements (strength and ROM); and in unilateral procedures, how do these parameters compare with those of the contralateral hand that was not operated on? (2) What is the mean subsidence (unloaded trapezial space), and does pinch strength correlate with the amount of subsidence?
Methods
From 1998 to 2005, 130 patients underwent trapeziectomy and abductor pollicis longus (APL) suspension-interposition arthroplasty for CMC1 OA at one orthopaedic department. During this period, 15 patients were treated with CMC1 arthrodesis and four were treated with implant arthroplasty, for a total of 149 patients. The surgeons used APL suspensionplasty for most patients, based on age and expected postoperative function; they also employed this procedure to avoid hardware or implant failure issues. The 100 living patients were asked to participate in this retrospective study, 96% (96) of whom were enrolled. The mean age at surgery was 58 ± 7 years. The patients completed a two-item thumb pain scale (modified from the SF-36 body pain scale), a hand pain VAS (average level of pain experienced over the week preceding measurement), and the 11-item QuickDASH. Patient-reported outcomes data were obtained from all 96 patients, and 83% (80) of patients underwent bilateral hand radiography and a physical examination at a mean follow-up of 17 ± 2.4 years. We calculated outcome data for each patient, and in 39 patients with unilateral surgery and intact contralateral CMC1 joint, we compared the operated side with the contralateral side. We compared our outcome data with that from the Swedish National Quality Registry for Hand Surgery (HAKIR), noting comparable outcomes for pain and QuickDASH scores.
Results
At long-term follow-up after trapeziectomy and APL suspension surgery, the mean thumb pain score was 19 ± 26, hand pain VAS score 23 ± 25, and QuickDASH score 26 ± 21. In the patients with unilateral surgery and intact contralateral CMC1 joint, the thumb pain score for the operated side was lower than the contralateral side, specifically 19 ± 25 compared with 29 ± 30 (mean difference -9.8 [95% CI -19.5 to -0.2]; p = 0.045); hand pain VAS score was 24 ± 23 versus 30 ± 25 (mean difference -6.1 [95% CI -15.2 to 3.1]; p = 0.19), and the QuickDASH score was 27 ± 19. Grip strength showed no differences between the operated and contralateral sides (mean 16.7 ± 7.3 kg versus 16.6 ± 6.9 kg, mean difference 0.1 [95% CI -1.6 to 1.8]; p = 0.90), while pinch was different (4.4 ± 1.4 versus 5.0 ± 1.5 kg, mean difference -0.6 [95% CI -0.9 to -0.3]; p = 0.001). The mean trapezial space was 4.4 ± 2.2 mm, and there was no association between the trapezial space and pinch strength (0.07 kg [95% CI -0.04 to 0.18] per mm of space; p = 0.17).
Conclusion
The finding of comparable pain and function between operated and unoperated sides at long-term follow-up suggests that trapeziectomy and tendon suspension-interposition arthroplasty provides predictable outcomes, and surgeons can use these data to counsel patients that surgery can potentially return them to comparable use. However, as patients often have asymptomatic radiographic OA on the contralateral side, future studies are needed to examine the impact of asymptomatic disease on function.
Level of Evidence
Level IV, therapeutic study.
Introduction
Surgery for the arthritic thumb carpometacarpal (CMC1) joint has been focused on removal of the trapezium, combined with procedures to suspend the first metacarpal using expendable tendons [23, 24, 31]. Tendon suspension using the flexor carpi radialis tendon to reconstruct the palmar oblique ligaments was initially described in response to reports of weakness and painful metacarpal subsidence with simple soft tissue interposition [6]. Although trapeziectomy alone is supported by evidence [8, 13, 14], tendon suspension of the first metacarpal with interposition is still the most commonly used surgical procedure in patients with CMC1 osteoarthritis (OA) [36]. One commonly used technique is abductor pollicis longus (APL) tendon suspension-interposition arthroplasty, with the advantage of surgery through a single incision [26, 28, 30]. Although there are reports of improvement in pain and function after APL arthroplasty [17, 20], the two studies with mean follow-up of 13 and 15 years had a high loss of follow-up of the original cohort and minimal physical examination measures [4, 25].
It is well known that first metacarpal subsidence is seen on postoperative radiographs after trapeziectomy [29]. Although some studies have shown no effect of subsidence on pinch or grip [37], a comparison of trapeziectomy alone with trapeziectomy and ligament reconstruction demonstrated a relationship between loss of trapezial space and pinch strength [10]. Another study showed that radigraphic outcomes after trapeziectomy alone compared with trapeziectomy/ligament reconstruction indicated a greater degree of arthritic change at the distal scaphoid and base of the first metacarpal, but that this finding did not correlate with patient-rated outcomes [27].
We therefore asked: (1) After trapeziectomy and tendon suspension surgery, what are the long-term, patient-reported outcomes and clinical measurements (strength and ROM); and in unilateral procedures, how do these parameters compare with those of the contralateral hand that was not operated on? (2) What is the mean subsidence (unloaded trapezial space), and does pinch strength correlate with the amount of subsidence?
Patients and Methods
Study Design and Setting
This single-center, restrospective study was conducted at one orthopaedic department, with clinical and surgical appointments at both Hässleholm and Kristianstad Hospitals in southern Sweden. The department is the primary facility for hand surgery in northeastern Skåne (population during the study period: 180,000 people). From our surgery registry, we identified all adults who had been treated with any type of surgical procedure with a diagnosis code for primary CMC1 OA (ICD-10 codes M18.0 and M18.1) from January 1, 1998 through December 31, 2005. All medical records (paper and later electronic) were examined, and relevant data were extracted.
Participants
We identified 149 patients who underwent surgery for CMC1 OA during the time period (Fig. 1). The six hand orthopaedic surgeons at this center primarily performed trapeziectomy and APL suspension as the procedure of choice in patients older than 50 years, based on the evidence at that time, with arthrodesis offered to those with manual labor or agricultural occupations. Fifteen patients had CMC1 fusion and four had implant arthroplasty. The remaining 87% (130 of 149) of the original patients who underwent trapeziectomy and APL suspension-interposition arthroplasty were potentially eligible for inclusion.
Fig. 1.
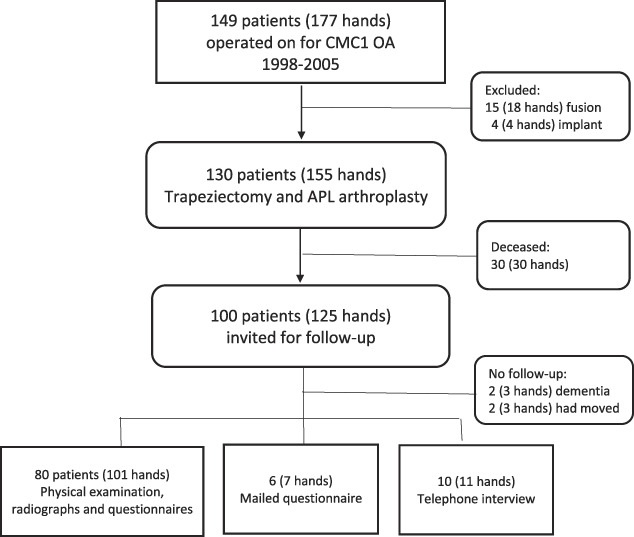
This flowchart shows the enrollment of patients in this study.
Accounting for all Patients
Of the original 130 patients, 23% (30) were deceased. In August 2018, information about the study was sent by mail to all living patients. Each patient was then contacted by telephone by a research nurse or a hand occupational therapist and asked to attend the hospital for a clinical and radiographic evaluation. Of the 100 eligible patients 80% (80) attended a follow-up examination at the hospital (conducted between September 2018 and December 2018). In addition, 6% (6 of 100) completed questionnaires and 10% (10 of 100) answered part of the questionnaire through a telephone interview with the research nurse or hand therapist, for a combined total of 96% (96 of 100) of patients who answered patient-reported outcomes measures. Radiographic analysis was performed on postoperative radiographs in 83% (80 of 96). Of the remaining patients, 2% (2 of 100) had moved to unknown addresses and could not be contacted, and 2% (2 of 100) had dementia and lived in a care facility (Fig. 1). Written informed consent was obtained from all patients who attended the examination and those who responded to the mailed questionnaires; patients who agreed to a telephone interview provided verbal consent.
Description of Study Population
The final study cohort of 96 patients was composed of 89 women and seven men, with a mean age at surgery of 58 years (Table 1). The surgical side was evenly divided between right and left; 99% (95 of 96 patients) reported being right-hand dominant. Of the 80 patients who attended their examination, there were 73 women and seven men with a mean age at follow-up of 74 ± 6 years (Table 1).
Table 1.
Characteristics of patients treated with trapeziectomy and abductor pollicis longus suspensionplasty
| Patient characteristics | All first operated thumbs | ||||||||
| Physical examination, full PROMs, and radiographs | Full PROMs | Single PROM | Unilateral trapeziectomy and intact contralateral thumb carpometacarpal (CMC1) joint | ||||||
| All | Alla | Women | Men | Allb | Allc | All | Women | Men | |
| Number of patients | 96 | 80 | 73 | 7 | 6 | 10 | 39 | 33 | 6 |
| Side, % (n) | |||||||||
| Right | 50 (48) | 49 (39) | 49 (36) | 43 (3) | 50 (3) | 60 (6) | 49 (19) | 52 (17) | 33 (2) |
| Left | 50 (48) | 51 (41) | 51 (37) | 57 (4) | 50 (3) | 40 (4) | 51 (20) | 48 (16) | 67 (4) |
| Age at surgery | 58 ± 6 | 58 ± 6 | 58 ± 6 | 62 ± 8 | 58 ± 6 | 59 ± 7 | 60 ± 6 | 60 ± 5 | 62 ± 8 |
| Age at follow-up | 74 ± 7 | 74 ± 6 | 74 ± 6 | 79 ± 8 | 76 ± 7 | 76 ± 7 | 76 ± 6 | 76 ± 6 | 78 ± 8 |
| Follow-up length | 16.8 ± 2.3 | 16.8 ± 2.4 | 16.8 ± 2.4 | 17.3 ± 2.6 | 16.8 ± 2.1 | 16.9 ± 2.1 | 16.3 ± 2.3 | 16.8 ± 2.3 | 16.9 ± 2.6 |
Data are presented as mean ± SD years, unless otherwise specified.
Twenty-one patients had the same procedure on the contralateral hand during the study period (1998-2005), 16 patients had the same procedure on the contralateral hand outside the study period (6 before and 10 after), and two patients had contralateral CMC1 fusion before the study period.
All women, responded to all scales through mailed questionnaires (Fig. 1); one patient had the same procedure on the contralateral hand during the study period.
All women, responded to the thumb pain scale through telephone interview (Fig. 1); one patient had the same procedure on the contralateral hand during the study period, and two patients had contralateral CMC1 fusion before the study period; PROM = patient-reported outcome measure.
In the study cohort, two hands underwent revision after not responding to fusion (6 and 15 months after attempted fusion).
Description of Treatment and Surgery
Before surgery, all patients had received at least 2 months of nonoperative treatment (splinting, activity modification, and therapy). Surgery was performed by six different specialists in hand surgery or orthopaedics according to a previously described technique [3, 28, 34]. Briefly, the trapezium was removed through a dorsoradial incision, the first extensor compartment was released, and a distally based strip of the APL was passed through a slit in the flexor carpi radialis and then sutured to itself to form a suspensory support, with the remaining tendon placed into the trapeziectomy space.
Aftercare
Postoperatively, patients were immobilized in a thumb spica cast for 4 to 5 weeks, followed by routine hand therapy.
Variables, Outcome Measures, Data Sources, and Bias
Patient-reported Outcome Measures
The patients completed questionnaires including measures of pain and activity limitations. Pain in the thumb was measured with a two-item thumb pain scale, and pain in the hand was evaluated on a VAS. The two-item thumb pain scale is modified from the two-item SF-36 body pain scale, as described in a previous study [17], and asks about the severity of pain in the thumb (six response choices ranging from “none” to “very severe”) and about whether the pain caused activity limitations (five response choices ranging from “not at all” to “extremely”). The scale’s two items have identical response choices to the SF-36 bodily pain scale items, and they are scored from 0 to 100 using the same scoring algorithm, but the final score is reversed (lower score is better) to match the other scores. The minimum clinically important difference (MCID) has not been determined for this adapted measure; however, for the SF-36 bodily pain scale, it has been estimated to be 7.8 in patients with lower extremity OA [1]. For hand pain VAS, the patient was asked to rate the average severity of pain in the hand during the past week on a scale from 0 (no pain) to 100 (most severe pain) [5], with an estimated MCID of 13 [12]. Upper extremity–related activity limitations were measured with the 11-item QuickDASH questionnaire, scored from 0 (best) to 100 (worst) [15], with an MCID of 6.8 [18]. The questionnaires were completed at the hospital immediately before the examination or returned by mail (for those who only responded to the questionnaire). All questionnaires were completed under the supervision of hand therapists.
Physical Examination
Each patient underwent a physical examination performed by one of two experienced hand occupational therapists, using validated methods to obtain objective measurements [21]. Grip strength was measured on both hands using a Jamar dynamometer (Sammons-Preston) on setting 2, with the mean of three trials recorded for each hand. Thumb key pinch was similarly measured using a strain gauge (Baseline). Measurement of ROM (in °) was performed with a handheld goniometer and included thumb interphalangeal and metacarpophalangeal flexion and extension and radial abduction, as well as wrist flexion, extension, radial deviation, and ulnar deviation. Thumb opposition was measured as the distance (in mm) to the base of the small finger.
Radiography
A radiographic examination of both wrists, hands, and thumbs (with no loading or grip) was performed. The radiographs were evaluated by a single examiner (JMW), a fellowship-trained hand surgeon who was blinded to the patient’s responses to the questionnaire and results of the physical examination, and who was not involved in their treatment. The examiner measured the height of the trapezial space (in mm) as the distance from the distal articular surface of the scaphoid to the proximal margin of the first metacarpal; the capitate length was used to obtain standardized scaling because radiography was performed with varied focal distances. The examiner graded osteoarthritic change at the scaphotrapezoid joint [27] using the Kellgren-Lawrence classification [19].
Comparative Referent Cohorts
Because the patient-reported outcome measures used at follow-up were not available preoperatively, we obtained data from two referent cohorts from the Swedish National Quality Registry for Hand Surgery (HAKIR) [2]. The specialized hand surgery departments in Sweden register all surgeries in the HAKIR registry using ICD-10 codes and Scandinavian surgical codes. Patient-reported outcome data are collected preoperatively and 1 year postoperatively, including the QuickDASH and three questions about pain: pain on load, pain on motion without load, and pain at rest, scored on a scale with 10-point increments of 0 to 100 (lower is better) [22, 35]. In the present study, we used preoperative registry data (pain and QuickDASH) for all patients in the same age span as the study cohort who were treated from 2011 to 2019 for CMC1 OA with trapeziectomy and any type of tendon suspension-interposition arthroplasty (because the indication for surgery is usually similar, irrespective of the type of tendon used). We also obtained 1-year postoperative registry data for patients treated specifically with trapeziectomy and APL suspension-interposition arthroplasty.
Ethical Approval
Ethical approval for this single-center retrospective study was obtained from the institutional review board of Lund University, Lund, Sweden (approval number 2018/485).
Statistical Analysis, Study Size
We provide descriptive data as means and SD or proportions as appropriate. For each patient-reported outcome measure, we calculated a scale score for all patients who responded to that scale, including those who only responded to the mailed questionnaire or only the telephone interview (Fig. 1).
For estimating the association between the trapezial space and pinch strength, we used a linear mixed-effects regression model. The exposure of interest was trapezial space in mm and the outcome was pinch strength in kg. The model was adjusted for potential confounders: age at surgery, gender, and side (right or left). In a second model, we adjusted for follow-up time. In a third model, we additionally adjusted for pain in the thumb as potential mediator and for scaphotrapezoid OA grade as a potential confounder of the pain-strength association. The residual diagnostics confirmed good fit of all models.
Results
Patient-reported Outcomes and Clinical Findings
In the 96 patients, including those with partial patient-reported outcomes, the thumb pain scale score was 19 ± 26, while 86 patients provided full patient-reported outcomes data, which showed a hand pain VAS score of 23 ± 25 and QuickDASH score of 26 ± 21 (Table 2). In the 39 patients with unilateral surgery, a comparison with the side that had not undergone previous surgery (that is, the intact CMC1 joint) demonstrated lower thumb pain scale scores (operated side: 19 ± 25, contralateral side: 29 ± 30, mean difference -9.8 [95% CI -19.5 to -0.2]; p = 0.045) but similar hand pain VAS scores (24 ± 23 versus 30 ± 25, mean difference -6.1 [95% CI -15.2 to 3.1]; p = 0.19). The mean QuickDASH score was 27 ± 19. For the thumb pain scale a score of 0 (no pain or related activity limitations) was recorded in 58% (56 of 96) of patients and score below 30 in 15% (14 of 96) of patients. The pain and QuickDASH scores were generally similar to the 1-year postoperative scores in the national hand surgery registry (HAKIR) cohort (Table 3).
Table 2.
Patient-reported outcomes measures for patient cohorts
| Patient-reported instrument | All first-operated thumbs | Unilateral trapeziectomy and intact contralateral carpometacarpal (CMC1) joint | |||
| Operated hand (n = 96)a | Operated hand (n = 39) | Unoperated hand (n = 39) | Mean difference (95% CI) | p valueb | |
| Thumb pain scale | 19 ± 26 | 19 ± 25 | 29 ± 30 | -9.8 (-19.5 to -0.2) | 0.045 |
| Hand pain VAS | 23 ± 25 | 24 ± 23 | 30 ± 25 | -6.1 (-15.2 to 3.1) | 0.19 |
| QuickDASH | 26 ± 21 | 27 ± 19 | NA | NA | NA |
Data are presented as mean ± SD, unless otherwise specified; score range: 0 (best) to 100 (worst).
Data from 96 patients for the thumb pain scale and from 86 patients for the other two scales (Fig. 1).
Paired t-test; QuickDASH = 11-item Disabilities of the Arm, Shoulder and Hand scale.
Table 3.
Referent cohorts from the Swedish quality registry for hand surgery (HAKIR) and the study cohort
| Comparative factors/measures | Registry (HAKIR) referent cohorts | Study cohort | ||||
| Preoperativea | 1-year postoperativeb | 13-21 years postoperativec | ||||
| Women (n = 656) | Men (= 146) | Women (n = 44) | Men (n = 15) | Women (n = 73) | Men (n = 7) | |
| Age at surgery in years | 59 ± 7 | 62 ± 5 | 59 ± 8 | 65 ± 7 | 58 ± 6 | 62 ± 8 |
| Side | ||||||
| Right | 49 (323) | 40 (59) | 57 (25) | 40 (6) | 49 (36) | 43 (3) |
| Left | 51 (333) | 60 (87) | 43 (19) | 60 (9) | 51 (37) | 57 (4) |
| Pain at rest | 52 ± 25 | 45 ± 26 | 14 ± 23 | 3 ± 5 | ||
| Pain on motion without load | 60 ± 21 | 51 ± 23 | 19 ± 23 | 6 ± 13 | ||
| Pain on load | 77 ± 16 | 73 ± 19 | 31 ± 29 | 14 ± 20 | 19 ± 26d | 17 ± 29d |
| QuickDASH | 57 ± 16 | 48 ± 16 | 29 ± 24 | 12 ± 12 | 27 ± 22 | 17 ± 15 |
Data presented as % (n) or mean ± SD; score range: 0 (best) to 100 (worst).
Registry patients who had undergone trapeziectomy and any type of tendon interposition arthroplasty.
Registry patients who had specifically undergone trapeziectomy and abductor pollicis longus suspension-interposition arthroplasty.
Study patients who completed all patient-reported outcome measures at physical examination or through mailed questionnaire (Fig. 1).
2-item thumb pain scale score, range 0 (best) to 100 (worst).
In the 80 patients who had follow-up examinations, the mean grip strength on the surgical side was 17.0 ± 7.1 kg, and mean pinch strength was 4.4 ± 1.5 kg (Table 4). In patients with unilateral surgery and intact contralateral CMC1 joint, the mean grip strength was 16.7 ± 7.3 kg in the operated side versus 16.6 ± 6.9 kg in the contralateral side (mean difference 0.1 [95% CI -1.6 to 1.8]; p = 0.90), while pinch strength was less in the operated side at 4.4 ± 1.4 kg versus 5.0 ± 1.5 kg (mean difference -0.6 [95% CI -0.9 to -0.3]; p = 0.001). Thumb and wrist ROM showed no differences between operated and unoperated sides (p > 0.05), with the exception of wrist extension with a mean 62° ± 11° on the operated side versus 58° ± 9° on the unoperated side (mean difference 3.6° [95% CI 0.5° to 6.8°]; p = 0.03). In patients with both thumbs operated on during the study period, patient-reported outcomes, physical measures, and radiographic findings were similar on both sides (see Supplementary Table 1; Supplemental Digital Content 1, http://links.lww.com/CORR/A564).
Table 4.
Physical examination measures
| Physical examination measure | All first operated thumbs | Unilateral trapeziectomy and intact contralateral CMC1 joint | |||
| Operated hand (n = 80)a | Operated hand (n = 39) | Unoperated hand (n = 39) | Mean difference (95% CI) | p valueb | |
| Strength in kg | |||||
| Grip | 17.0 ± 7.1 | 16.7 ± 7.3 | 16.6 ± 6.9 | 0.1 (-1.6 to 1.8) | 0.90 |
| Key pinch | 4.4 ± 1.5 | 4.4 ± 1.4 | 5.0 ± 1.5 | -0.6 (-0.9 to -0.3) | 0.001 |
| ROM in ° | |||||
| Thumb | |||||
| IP extensionc | 11 ± 11 | 12 ± 10 | 13 ± 16 | 1.4 (-2.9 to 5.7) | 0.51 |
| IP flexion | 64 ± 12 | 62 ± 12 | 62 ± 11 | 0.6 (-3.0 to 4.3) | 0.73 |
| MCP extensionc | 15 ± 14 | 14 ± 16 | 10 ± 19 | -4.0 (-9.2 to 1.3) | 0.13 |
| MCP flexion | 39 ± 13 | 39 ± 12 | 42 ± 14 | -3.5 (-8.0 to 1.1) | 0.13 |
| Palmar abduction | 39 ± 10 | 38 ± 11 | 38 ± 10 | 0 (-2.5 to 2.5) | > 0.99 |
| Radial abduction | 42 ± 7 | 41 ± 8 | 41 ± 7 | -0.9 (-3.0 to 1.1) | 0.36 |
| Opposition deficit (mm)d | 0 (0, 10) | 0 (0, 10) | 0 (0, 5) | 0 (0, 0) | 0.27 |
| Wrist | |||||
| Flexion | 61 ± 12 | 61 ± 13 | 59 ± 13 | 2.1 (-1.9 to 6.1) | 0.29 |
| Extension | 61 ± 11 | 62 ± 11 | 58 ± 9 | 3.6 (0.5 to 6.8) | 0.03 |
| Radial deviation | 22 ± 12 | 24 ± 13 | 22 ± 7 | 2.5 (-2.2 to 7.1) | 0.28 |
| Ulnar deviation | 40 ± 9 | 39 ± 9 | 41 ± 9 | -1.7 (-3.8 to 0.4) | 0.12 |
Data presented as mean ± SD, unless otherwise specified.
Data from 80 patients who attended clinical and radiographic examination (Fig. 1).
Paired t-test.
Values represent hyperextension; MCP fusion in three hands (two in unilateral group), and MCP extension deficit (> 10°) was present in one hand.
Values are median (quartiles) distance to base of small finger; median difference (quartiles); CMC1 = thumb carpometacarpal; IP = interphalangeal; MCP = metacarpophalangeal.
Subsidence and Strength
The mean trapezial space was 4.4 ± 2.2 mm, and there was no association between the trapezial space and pinch strength (0.07 kg [95% CI -0.04 to 0.18] per mm of space; p = 0.17) when adjusted for age, gender, side, pain, and OA grade. The results did not change when the model was adjusted for the time since surgery (0.05 kg [95% CI -0.07 to 0.17] per mm of space; p = 0.19); thus, there was no association between first metacarpal subsidence and pinch strength. Scaphotrapezoid joint Kellgren-Lawrence OA Grades 2 to 4 were seen in 72% (57 of 79) of the joints (Table 5). Among the 39 patients with unilateral trapeziectomy and unoperated contralateral CMC1 joint, scaphotrapezoid OA Grade 2 to 4 was observed in 67% (26 of 39) of the operated hands and 87% (34 of 39) of the contralateral hands.
Table 5.
Radiographic osteoarthritis (OA) in the scaphotrapezoid joint
| All operated hands | Unilateral trapeziectomy and intact contralateral CMC1 joint | ||
| OA gradea | (n = 79)b | Operated-on hand (n = 39) | Nonoperated-on hand (n = 39) |
| 0 | 11 (9) | 10 (4) | 10 (4) |
| 1 | 16 (13) | 23 (9) | 3 (1) |
| 2 | 32 (25) | 31 (12) | 33 (13) |
| 3 | 29 (23) | 21 (8) | 28 (11) |
| 4 | 11 (9) | 15 (6) | 26 (10) |
Data presented as % (n).
Kellgren-Lawrence grading, range 0 (no OA) to 4 (most severe OA).
One patient had undergone fusion of the scaphotrapezoid joint before follow-up.
Other Relevant Findings
Three patients underwent subsequent revision surgery because of pain; two with repeated tendon interposition arthroplasty (using the extensor carpi radialis longus and APL at 18 and 21 months post index surgery, respectively), and one with fusion of the first metacarpal base to the second metacarpal and scaphotrapezoid fusion at 42 months after APL suspensionplasty. No other major complications occurred.
Discussion
OA of the base of the thumb is common and disabling, and it can be treated with either nonoperative or operative means [32]. When nonoperative measures are not effective, studies have shown that surgical removal of the trapezium, with or without tendon suspension or interposition to stabilize the first metacarpal, is a reliable treatment for pain relief and return of function in the short- and medium-term [7, 9, 13]. What is not known is whether the effect of surgery is lasting and durable, or whether these results degenerate with a later decrease in function over time. This study was performed to evaluate the long-term effect of surgical treatment of CMC1 OA. Our findings confirm that patients can expect function comparable to that of their unoperated hand and low levels of pain at a mean of 17 years after surgery. In addition, the risk of surgical revision was very low.
Limitations
This study’s limitations include a study group drawn from a single center with evaluation of a single surgical technique, the choice of which may have been influenced by selection bias by the operating surgeons. Although some patients underwent other surgical procedures during the study period (CMC1 fusion and implant arthroplasty), these constituted only 13% (19 of 149) of all patients treated for CMC1 OA during that period, indicating lower risk of selection bias. In addition, the procedures were performed at the region’s primary referral center by different hand and orthopaedic surgeons, which supports the generalizability of our findings. We believe that the range in patient ages and the use of a technique with literature support [16], particularly at the time of surgery, are all mitigating factors.
We did not obtain standardized preoperative measures of pain and function, limiting the ability to stringently evaluate response to surgery in this cohort. We included data from the Swedish National Quality Registry for Hand Surgery (HAKIR), with a specific focus on surgery for CMC1 OA. Based on a similar age and gender distribution and geographic similarity to this cohort, we believe that the quality registry data provide comparable measurements and can thus be used to provide preoperative estimates of self-rated function and to compare postoperative outcomes. Using within-patient comparisons of the operated hand with the unoperated contralateral hand may not be a valid comparison, as the other hand may be affected by osteoarthritis or other disease and is not an age-matched nonarthritic hand. However, in this subgroup, the patient had not presented for care of the contralateral hand, and thus they can be theorized to potentially have milder symptoms compared with the operative side. A further limitation is the loss of a small percentage of the original cohort to follow-up, but the use of telephone and mail contact allowed us to include standardized outcomes data for some of these patients.
Patient-reported Outcomes and Clinical Findings
This study demonstrated that patients treated with trapeziectomy/APL suspensionplasty achieved functional outcomes and pain comparable to the unoperated side. In addition, these patient-reported outcomes are comparable to the DASH and VAS scores in analogous studies [4, 13, 33], suggesting that this procedure yields results similar to simple trapeziectomy and other forms of ligament reconstruction. Evaluation of strength and range of motion showed overall comparable results between operated and unoperated sides, except a mean pinch strength difference of 0.6 kg less on the operative side, with 3.6° greater extension. Although the small amount of extension difference is likely not clinically important, the difference in pinch may reflect previously reported slight loss of pinch postoperatively [13] or surgery on the nondominant hand.
Overall, there is a paucity of long-term outcomes data available for this procedure or indeed for any of the trapeziectomy-suspension techniques. The existing studies are limited by loss of approximately 50% of the original cohort to follow-up [4, 25] and demonstrated very similar mean QuickDASH scores of 21 and VAS pain scores of 1.6 at minimum 10-year (mean 13-year) follow-up [25].
A comparison with a cohort from the Swedish National Quality Registry for Hand Surgery showed that the follow-up QuickDASH scores in the study cohort (mean of 27 in women and 17 in men) did not differ substantially from the 1-year postoperative scores in the National Quality Registry for Hand Surgery cohort (mean of 29 in women and 12 in men). The pain scores were more difficult to compare because the National Quality Registry for Hand Surgery provided separate pain scores (pain on load, pain on motion without load, and pain at rest) whereas our study cohort provided the thumb pain score (modified from the SF-36 body pain score, which incorporates pain-related activity limitations) and average VAS score for hand pain. However, the mean thumb pain scores in the study cohort were generally similar to those in the registry cohort. The fact that function and pain scores are consistent among studies is important information in setting patient and surgeon expectations. The results of the present study, which show that patients had some residual pain and activity limitations at a mean of 17 years postsurgery, can be used to counsel patients with regard to expectations. There remain several unanswered questions, which include differential effects of various surgeries on strength, pain, and patient-reported outcomes; this would be best addressed by a long-term prospective comparative trial to specifically compare trapeziectomy alone with ligament reconstruction and other forms of treatment.
Subsidence and Strength
Our study showed some thumb subsidence, as well as mild or moderate signs of arthrosis at the scaphotrapezoid joint, but there was no relationship between pinch strength and subsidence. First metacarpal subsidence is common after trapeziectomy and has not been shown to be associated with impingement or poor outcomes [11]. A previous study reported there was no correlation between the amount of subsidence and pinch or grip in 13 patients evaluated at 32 months postoperatively [37]; however, a comparative study of 22 patients with trapeziectomy alone versus 34 patients treated with a ligament reconstruction and tendon interposition demonstrated a relationship between ligament reconstruction and improved pinch strength [10]. A recent study indicated radiographic signs of increased degeneration of the pseudoarthrosis between the distal scaphoid and base of the first metacarpal in patients who underwent trapeziectomy only compared with those who were treated with ligament reconstruction and tendon interposition [27]. Taken together, these findings underscore our lack of knowledge about how best to measure radiographic outcomes and what is clinically relevant. Further studies of dynamic pinch on imaging and radiographic factors in the peritrapezial joints are needed.
Conclusion
This long-term follow-up study of patients treated with trapeziectomy and abductor pollicis longus tendon suspension for CMC1 OA at a mean of 17 years postoperatively indicates that patients generally have sustained decrease in pain and functional use of the operated hand with a very low revision rate; however, outcome measurements indicate some residual pain and activity limitations. These long-term outcomes are comparable to other surgical procedures that involve trapeziectomy and can help clinicians in setting patient expectations for the longevity of surgical treatment of CMC1 OA. In addition, these findings can guide future prospective research to investigate the true impact of suspension techniques on clinical and radiographic outcomes.
Supplementary Material
Acknowledgments
We thank David C. Landy MD, PhD, for his assistance with statistical analysis.
Footnotes
Each author certifies that neither he nor she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was obtained from Lund University, Lund, Sweden (approval number 2018/485).
This work was performed at Lund University, Lund, Sweden.
Contributor Information
Aleksandra Turkiewicz, Email: aleksandra.turkiewicz@med.lu.se.
Martin Englund, Email: martin.englund@med.lu.se.
Jon Karlsson, Email: jon.karlsson@vgregion.se.
Marianne Arner, Email: marianne.arner@gmail.com.
Isam Atroshi, Email: isam.atroshi@med.lu.se.
References
- 1.Angst F, Stucki G, Aeschlimann A. Quality of life assessment in osteoarthritis. Expert Rev Pharmacoecon Outcomes Res. 2003;3:623-636. [DOI] [PubMed] [Google Scholar]
- 2.Arner M. Developing a national quality registry for hand surgery: challenges and opportunities. EFORT Open Rev. 2016;1:100-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Atroshi I, Axelsson G, Nilsson EL. Osteotomy versus tendon arthroplasty in trapeziometacarpal arthrosis: 17 patients followed for 1 year. Acta Orthop Scand. 1998;69:287-290. [DOI] [PubMed] [Google Scholar]
- 4.Avisar E, Elvey M, Wasrbrout Z, Aghasi M. Long-term follow-up of trapeziectomy with abductor pollicis longus tendon interposition arthroplasty for osteoarthritis of the thumb carpometacarpal joint. J Orthop. 2013;10:59-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Breivik H, Borchgrevink PC, Allen SM, et al. Assessment of pain. Br J Anaesth. 2008;101:17-24. [DOI] [PubMed] [Google Scholar]
- 6.Burton RI, Pellegrini VD., Jr.Surgical management of basal joint arthritis of the thumb. Part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg Am. 1986;11:324-332. [DOI] [PubMed] [Google Scholar]
- 7.Catalano L, Horne LT, Fischer E, Barron OA, Glickel SZ. Comparison of ligament reconstruction tendon interposition and trapeziometacarpal interposition arthroplasty for basal joint arthritis. Orthopedics. 2008;31:228. [DOI] [PubMed] [Google Scholar]
- 8.Davis TR, Brady O, Dias JJ. Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint: a study of the benefit of ligament reconstruction or tendon interposition. J Hand Surg Am. 2004;29:1069-1077. [DOI] [PubMed] [Google Scholar]
- 9.Davis TR, Pace A. Trapeziectomy for trapeziometacarpal joint osteoarthritis: is ligament reconstruction and temporary stabilisation of the pseudarthrosis with a kirschner wire important? J Hand Surg Eur Vol. 2009;34:312-321. [DOI] [PubMed] [Google Scholar]
- 10.De Smet L, Sioen W, Spaepen D, van Ransbeeck H. Treatment of basal joint arthritis of the thumb: trapeziectomy with or without tendon interposition/ligament reconstruction. Hand Surg. 2004;9:5-9. [DOI] [PubMed] [Google Scholar]
- 11.Downing ND, Davis TR. Trapezial space height after trapeziectomy: mechanism of formation and benefits. J Hand Surg Am. 2001;26:862-868. [DOI] [PubMed] [Google Scholar]
- 12.Gallagher EJ, Liebman M, Bijur PE. Prospective validation of clinically important changes in pain severity measured on a visual analog scale. Ann Emerg Med. 2001;38:633-638. [DOI] [PubMed] [Google Scholar]
- 13.Gangopadhyay S, McKenna H, Burke FD, Davis TR. Five- to 18-year follow-up for treatment of trapeziometacarpal osteoarthritis: a prospective comparison of excision, tendon interposition, and ligament reconstruction and tendon interposition. J Hand Surg Am. 2012;37:411-417. [DOI] [PubMed] [Google Scholar]
- 14.Gray KV, Meals RA. Hematoma and distraction arthroplasty for thumb basal joint osteoarthritis: minimum 6.5-year follow-up evaluation. J Hand Surg Am. 2007;32:23-29. [DOI] [PubMed] [Google Scholar]
- 15.Gummesson C, Atroshi I, Ekdahl C. The quality of reporting and outcome measures in randomized clinical trials related to upper-extremity disorders. J Hand Surg Am. 2004;29:727-734. [DOI] [PubMed] [Google Scholar]
- 16.Heyworth BE, Jobin CM, Monica JT, et al. Long-term follow-up of basal joint resection arthroplasty of the thumb with transfer of the abductor pollicis brevis origin to the flexor carpi radialis tendon. J Hand Surg Am. 2009;34:1021-1028. [DOI] [PubMed] [Google Scholar]
- 17.Jorheim M, Isaxon I, Flondell M, Kalen P, Atroshi I. Short-term outcomes of trapeziometacarpal artelon implant compared with tendon suspension interposition arthroplasty for osteoarthritis: a matched cohort study. J Hand Surg Am. 2009;34:1381-1387. [DOI] [PubMed] [Google Scholar]
- 18.Kazmers NH, Qiu Y, Yoo M, et al. The minimal clinically important difference of the promis and quickdash instruments in a nonshoulder hand and upper extremity patient population. J Hand Surg Am. 2020;45:399-407 e396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee HJ, Kim PT, Deslivia MF, et al. Results of abductor pollicis longus suspension ligamentoplasty for treatment of advanced first carpometacarpal arthritis. Clin Orthop Surg. 2015;7:372-376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li L, Li Y, Wu C, Zhang X. Test-retest reliability of tip, key, and palmar pinch force sense in healthy adults. BMC Musculoskelet Disord. 2020;21:189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Merskey H. The perception and measurement of pain. J Psychosom Res. 1973;17:251-255. [DOI] [PubMed] [Google Scholar]
- 23.Nylen S, Johnson A, Rosenquist AM. Trapeziectomy and ligament reconstruction for osteoarthrosis of the base of the thumb. A prospective study of 100 operations. J Hand Surg Br. 1993;18:616-619. [DOI] [PubMed] [Google Scholar]
- 24.Pellegrini VD., Jr.Osteoarthritis of the trapeziometacarpal joint: the pathophysiology of articular cartilage degeneration. I. Anatomy and pathology of the aging joint. J Hand Surg Am. 1991;16:967-974. [DOI] [PubMed] [Google Scholar]
- 25.Pomares G, Delgrande D, Dap F, Dautel G. Minimum 10-year clinical and radiological follow-up of trapeziectomy with interposition or suspensionplasty for basal thumb arthritis. Orthop Traumatol Surg Res. 2016;102:995-1000. [DOI] [PubMed] [Google Scholar]
- 26.Robinson D, Aghasi M, Halperin N. Abductor pollicis longus tendon arthroplasty of the trapezio-metacarpal joint: surgical technique and results. J Hand Surg Am. 1991;16:504-509. [DOI] [PubMed] [Google Scholar]
- 27.Salem HM, Davis TR. Degenerative change at the pseudarthrosis after trapeziectomy at 6-year follow-up . Clin Orthop Relat Res. 2014;472:1160-1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sigfusson R, Lundborg G. Abductor pollicis longus tendon arthroplasty for treatment of arthrosis in the first carpometacarpal joint. Scand J Plast Reconstr Surg Hand Surg. 1991;25:73-77. [DOI] [PubMed] [Google Scholar]
- 29.Soejima O, Hanamura T, Kikuta T, Iida H, Naito M. Suspensionplasty with the abductor pollicis longus tendon for osteoarthritis in the carpometacarpal joint of the thumb. J Hand Surg Am. 2006;31:425-428. [DOI] [PubMed] [Google Scholar]
- 30.Thompson J. Surgical treatment of trapeziometacarpal arthrosis. Adv Orthop Surg. 1986;10:105-120. [Google Scholar]
- 31.Thomsen NO, Jensen CH, Nygaard H. Weilby-burton arthroplasty of the trapeziometacarpal joint of the thumb. Scand J Plast Reconstr Surg Hand Surg. 2000;34:253-256. [DOI] [PubMed] [Google Scholar]
- 32.Van Heest AE, Kallemeier P. Thumb carpal metacarpal arthritis. J Am Acad Orthop Surg. 2008;16:140-151. [DOI] [PubMed] [Google Scholar]
- 33.Wang T, Zhao G, Rui YJ, Mi JY. Outcomes of modified trapeziectomy with ligament reconstruction tendon interposition for the treatment of advanced thumb carpometacarpal arthritis: two-year follow-up. Medicine (Baltimore). 2018;97:e0235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weilby A. Tendon interposition arthroplasty of the first carpo-metacarpal joint. J Hand Surg Br. 1988;13:421-425. [DOI] [PubMed] [Google Scholar]
- 35.Wilcke M, Roginski M, Astrom M, Arner M. A registry based analysis of the patient reported outcome after surgery for trapeziometacarpal joint osteoarthritis. BMC Musculoskelet Disord. 2020;21:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wolf JM, Delaronde S. Current trends in nonoperative and operative treatment of trapeziometacarpal osteoarthritis: a survey of us hand surgeons. J Hand Surg Am. 2012;37:77-82. [DOI] [PubMed] [Google Scholar]
- 37.Yang SS, Weiland AJ. First metacarpal subsidence during pinch after ligament reconstruction and tendon interposition basal joint arthroplasty of the thumb. J Hand Surg Am. 1998;23:879-883. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


