Abstract
Objective:
To summarize the literature on prevalence, impact, and contributing factors related to diagnostic error in the pediatric intensive care unit (PICU).
Data Sources:
Search of PubMed, EMBASE, and the Cochrane Library up to December 2019.
Study Selection:
Studies on diagnostic error and the diagnostic process in pediatric critical care were included. Non-English studies with no translation, case reports/series, studies providing no information on diagnostic error, and studies focused on non-PICU populations, a single condition/disease or a single diagnostic test/tool were excluded.
Data Extraction:
Data on research design, objectives, study sample, and results pertaining to the prevalence, impact, and factors associated with diagnostic error was abstracted from each study.
Data Synthesis:
Using independent tiered review, 396 abstracts were screened and 17 studies (14 full-text, 3 abstracts) were ultimately included. Fifteen of 17 studies (88%) had an observational research design. Autopsy studies (autopsy rates were 20%−47%) showed a 10%−23% rate of missed major diagnoses; 5%−16% of autopsy-discovered diagnostic errors had a potential adverse impact on survival and would have changed management. Retrospective record reviews reported varying rates of diagnostic error from 8% in a general PICU population to 12% among unexpected critical admissions and 21%−25% of patients discussed at PICU morbidity and mortality conferences. Cardiovascular, infectious, congenital, and neurologic conditions were most commonly misdiagnosed. Systems (40%−67%), cognitive (20%−33%), and both systems and cognitive (40%) factors were associated with diagnostic error. Limited information was available on the impact of misdiagnosis.
Conclusions:
Knowledge of diagnostic errors in the PICU is limited. Future work to understand diagnostic errors should involve a balanced focus between studying the diagnosis of individual diseases and uncovering common system- and process-related determinants of diagnostic error.
Keywords: pediatrics, critical care, diagnosis, diagnostic error, misdiagnosis, patient safety
INTRODUCTION
In its 2015 landmark report, the National Academies of Sciences, Engineering, and Medicine (NASEM) defined diagnostic error as the failure to establish an accurate and timely explanation of a patient’s health problem or to communicate that explanation to the patient (1). The risk of diagnostic error in pediatric critical care is potentially high given the need for immediate delivery of complex care by multi-disciplinary teams to critically ill children who cannot participate in their own care (2). Diagnosing acutely ill children can be difficult because children vary widely in age and development, are dependent on their caregivers to articulate their symptoms, and can be ill from a broad range of problems of varying severity (3).
The objective of this study is to summarize the literature on diagnostic error in the pediatric intensive care unit (PICU) with regard to their prevalence, impact and contributing factors. Through a comprehensive literature search and analysis, we aim to describe the state of the science, identify gaps in knowledge, and inform future directions for research necessary to understand and prevent diagnostic error and mitigate associated harm to critically ill children and their families.
MATERIALS AND METHODS
We performed a systematic review to summarize literature on diagnostic errors in the PICU. This study was reported in accordance with PRISMA guidelines (4) (see Supplemental Digital Content 1).
Search Strategy
With the assistance of a trained librarian, we searched PubMed, EMBASE, and the Cochrane Library through December 17, 2019 for all studies on diagnostic error and the diagnostic process in pediatric critical care settings/populations. We began with no language limitations. Search terms included “misdiagnosis,” “diagnostic errors,” “diagnostic delay,” “intensive care unit, pediatric,” “pediatric intensive care unit,” “PICU,” “critical care,” and “pediatrics.”
Review and Inclusion/Exclusion Criteria
Three authors with expertise in critical care medicine and the evaluation of diagnostic errors served as reviewers. Abstracts were screened by one reviewer (C.C.) to exclude duplicate articles and case reports/case series. Two reviewers (C.C., J.W.C.) then independently reviewed each abstract and excluded studies describing non-PICU populations, focused on a single condition/disease or a single diagnostic test/tool, focused on treatment, with no original data, and studies not focused on diagnostic error or the diagnostic process. A third reviewer (J.C.F.) adjudicated all disagreements by the two reviewers. After a full article review, additional studies were excluded by consensus based on the above criteria and non-English language studies without English translations were excluded. We did not contact authors or identify unpublished studies.
Data Abstraction and Synthesis
Each article’s full text was reviewed and we collected data on research design, primary objective, and study population. We reviewed each study for available data on the prevalence of diagnostic error (proportion), taking into account the relevant denominator and how diagnostic error was determined, common misdiagnosed medical conditions, and time to discovery of error. When available, we also collected data on the consequences of diagnostic error including morbidity and mortality. Autopsy studies in particular, described discrepancies between autopsy and clinical findings using the Goldman classification system (5), wherein missed major diagnoses are categorized as Class I and II diagnostic errors. Class I errors had a potential adverse impact on survival and would have changed medical management, while Class II errors had no potential impact on survival and would not have changed therapy. We noted proportions reported in each class accordingly.
Data were also collected concerning factors associated with diagnostic error. We used NASEM’s conceptual model, which characterizes the diagnostic process as a complex, patient-centered collaborative activity that involves information gathering and clinical reasoning with the goal of explaining a patient’s health problem (6). The diagnostic process occurs over time and within the context of a larger health care work system. Within the process are cognitive, systems, or combined cognitive/systems factors that can affect diagnostic outcomes. Cognitive factors contributing to misdiagnosis include errors in clinical reasoning and knowledge gaps, while systems factors include organizational vulnerabilities including structural and workflow issues (7).
We did not formally assess the risk of bias of individual studies. We were unable to perform quantitative data synthesis due to the heterogeneity of studies included, both in terms of research design and included subject populations.
RESULTS
Our initial literature search yielded 396 publications. After screening, independent review of abstracts, and final review of each article’s available text, we identified 17 studies for inclusion (14 full-text, 3 had only abstracts available from conference proceedings) (Figure). Of the 17 studies included,15 had an observational study design. Thirteen studies included PICU patients as subjects while the rest included PICU clinicians. Thirteen studies provided information on the prevalence of diagnostic error, most commonly from autopsies or chart reviews. Eight studies provided some information on factors associated with diagnostic error, while only 3 studies had data on consequences. See Supplemental Digital Content 2 for a list of all included studies and the type of information on diagnostic errors each provided.
Figure. Flow diagram of study identification, screening, and inclusion.
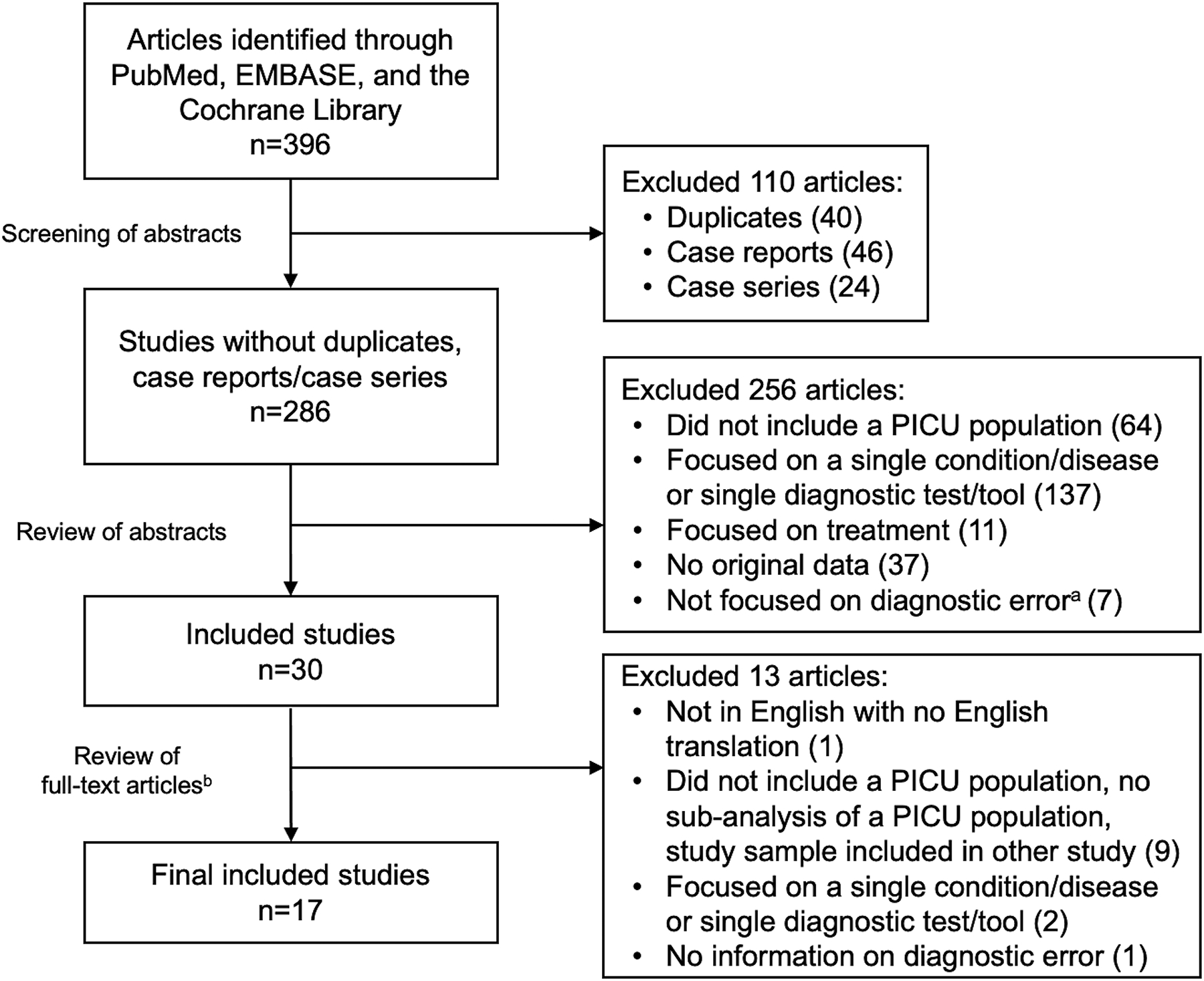
PICU – pediatric intensive care unit
aStudies excluded that were not focused on diagnostic error included education-related studies, outcomes studies, and work on other types of error.
bThree studies included in the final cohort had only abstracts available.
Prevalence of Diagnostic Error
Autopsy Studies
The most comprehensive autopsy study we identified was Custer et al.’s systematic review of 7 studies of patients who died in PICUs. This study found that missed major diagnoses (Class I and II) occurred in 20% of autopsied cases; 6% of all errors were categorized as Class I (8). Autopsy studies overall showed that in the general autopsied PICU population, the most common major missed diagnoses (Class I and II) were cardiovascular conditions, infections, and congenital malformations (8–11) (Table 1). Common examples included unidentified catastrophic hemorrhage/thrombosis, missed bacterial sepsis/meningitis, and inadequate delineation of congenital heart disease anatomy (8–11).
Table 1.
Prevalence of Diagnostic Error in the Pediatric Intensive Care Unit
| Authors | Year | Research Design | Relevant Sample | Prevalence of Diagnostic Error | Types of Most Commonly Misdiagnosed Conditions |
|---|---|---|---|---|---|
| Autopsy Studies | |||||
| Custer JW, et al. (8) | 2015 | Systematic review of 7 PICU autopsy studies | 498 PICU patients with autopsies included in 7 studies (47% autopsy rate) | 20% major diagnostic error rate (6% Class I, 14% Class II)a | 45% infection, 29% vascular events, 10% congenital malformations (among Class I and II errors*) |
| Widmann R, et al. (9) | 2017 | Retrospective cohort | 39 patients with autopsies admitted to a single PICU (20% autopsy rate) | 6% major diagnostic error rate (2% Class I, 4% Class II)a | 38% congenital malformations, 25% vascular, 25% infection (among Class I and II errors*) |
| Carlotti AP, et al. (10) | 2016 | Retrospective cohort | 123 patients with autopsies admitted to a single PICU | 23% major diagnostic error rate (16% Class I, 7% Class II)a | 71% cardiovascular, 14% infection, 7% cancer (among Class I and II errorsa); 14% of major diagnostic errors were undiagnosed complications of care/surgery |
| Blanco C, et al. (11) | 2014 | Retrospective cohort | 54 patients admitted to a single PICU who required ECMO | 54% major diagnostic error rate (74% Class I, 28% Class II)a | 65% cardiovascular, 10% infection, 4% neurologic (among Class I and II errors*) |
| Retrospective Cohort Studies | |||||
| Cifra CL, et al. (12) | 2018 | Retrospective cohort - chart review using the Safer Dx Instrument | 50 patients non-electively admitted to a single PICU (consecutive admissions) | 8% diagnostic error rate in the first 12 hours of PICU admission | 50% neurologic, 50% infection |
| Davalos MC, et al. (13) | 2017 | Retrospective cohort - chart review using the Safer Dx Instrument | 214 patients admitted to a single PICU (selected from cohorts hypothesized to be at high risk for diagnostic error) | 12% overall diagnostic error rate; 30% of diagnostic errors were among patients transferred from an acute care floor and required hemodynamic and invasive respiratory support within the first 24 hours of PICU admission | 31% neurologic, 31% infection, 19% gastrointestinal |
| Cifra CL, et al. (14) | 2014 | Retrospective cohort - review of conference minutes, chart review, review of incident reports | 96 patients discussed at a single PICU’s morbidity and mortality conference | 21% diagnostic error rate; diagnostic error comprised 7% of all adverse events | Not specified |
| Cifra CL, et al. (15) | 2015 | Retrospective cohort - review of conference minutes, chart review | 96 patients discussed at a single PICU’s morbidity and mortality conference | 21% diagnostic error rate | 35% vascular, 30% neurologic, 20% infection, 20% cardiac |
| Frey B, et al. (16) | 2018 | Retrospective cohort - review of conference minutes | 48 patients discussed at a single PICU’s morbidity and mortality conference | 25% overall diagnostic error rate; 66% of autopsied patients had a discrepancy between clinical diagnosis and autopsy findings | Not specified overall Among autopsied patients: 38% vascular, 33% genetic/metabolic, 29% infection |
| Fink AZ, et al. (17) | 2018 | Retrospective cohort | 575 radiographs of patients admitted to a single PICU | 46% discrepancy rate in interpretation of radiographs between PICU clinicians and radiologists; 13% were actionable discrepancies | Most common actionable discrepancies: 35% line/tube placement, 18% lung findings, 15% air leak |
| Nesterova GV, et al. (18) | 2010 | Retrospective cohort | 460 radiographs of patients admitted to a single PICU | 7% discrepancy rate in interpretation of radiographs between PICU clinicians and radiologists; 9% were actionable discrepancies | Overall most common discrepancies: 30% air space disease, 27% atelectasis, 24% effusion |
| Other Studies | |||||
| Labib JR, et al. (19) | 2019 | Quasi-experimental pre-test/post-test design | 215 incident reports submitted regarding the care of 918 patients admitted to 4 PICUs | 5% diagnostic errors detailed in incident reports | Infection (not quantified) |
| Bhat PN, et al. (20) | 2018 | Cross-sectional survey | 200 pediatric cardiac ICU clinicians | 79% of respondents reported encountering ≥ 5 diagnostic errors yearly; 65% of respondents reported encountering ≥ 5 harmful diagnostic errors yearly | 37% medication side effects, 21% psychiatric conditions, 17% sepsis |
PICU - pediatric intensive care unit, ECMO - extra-corporeal membrane oxygenation
According to the Goldman classification, missed major diagnoses are categorized as Class I and II diagnostic errors. Class I errors had a potential adverse impact on survival and would have changed medical management, while Class II errors had no potential impact on survival and would not have changed therapy (5).
Retrospective Cohort Studies
Retrospective cohort studies had wide variation in study samples (denominators used in calculations of diagnostic error rates), data sources, and data collection procedures (Table 1). Only one study drew from a general PICU population of consecutive patents admitted, showing an 8% diagnostic error rate within the first 12 hours of PICU admission; 75% of patients were diagnosed correctly between 1–3 days after admission (12). Another study identified diagnostic errors within hypothesized high-risk PICU cohorts and found an overall diagnostic error rate of 12% (13). Infectious and neurologic conditions were most commonly misdiagnosed (12, 13), particularly highlighting delays in diagnosing septic shock and elevated intracranial pressure.
Three studies focused on diagnostic errors identified in volunteered cases discussed at the PICU morbidity and mortality conference (MMC) (14–16), thus they were unable to provide a true estimate of diagnostic error prevalence in the general PICU population. Overall, studies from MMC cases showed that 21%−25% of discussed patients had diagnostic errors, comprising 7%−25% of all adverse events identified. The most common misdiagnosed conditions were vascular and neurologic disease (14–16).
Two studies reported a 7%−46% rate of discrepancies in interpretation of radiographs (chest and abdominal x-rays) between PICU physicians and radiologists. Among discrepancies, 9%−13% were found to be actionable and led to a change in management (17, 18). Common actionable discrepancies included failure to recognize line/tube malposition and misinterpretation of air space disease and atelectasis (17, 18).
Other Studies
A prospective study aiming to improve incident reporting in PICUs showed that diagnostic errors comprised 5% of all reported adverse events (19). Another study surveyed provider and nursing staff in pediatric cardiac ICUs regarding diagnostic errors that they were involved in; 79% of respondents self-reported ≥5 diagnostic errors per year. The most common reported missed conditions were medication side effects, psychiatric diagnoses, and infections (20).
Impact of Diagnostic Error
Only three studies shed light on the consequences of diagnostic error for patients and none illustrated the impact of diagnostic errors on PICU clinicians. In one study, 60% of diagnostic errors caused patient harm, with 25% severe enough to have potentially contributed to death (15). In the survey of pediatric cardiac ICU clinicians,16% of respondents perceived that ≥5 diagnostic errors cause severe permanent harm per year (20). Diagnostic errors discussed at MMCs all prompted interventions to mitigate future errors (16).
Factors Associated with Diagnostic Error
We found no studies systematically examining breakdowns in the PICU diagnostic process, although 8 studies identified factors contributing to diagnostic error (Table 2).
Table 2.
Factors Associated with Diagnostic Error in the Pediatric Intensive Care Unit
| Authors | Year | How Factors Contributing to Diagnostic Error Were Determined | Most Common Factors Associated with Diagnostic Error |
|---|---|---|---|
| Cognitive Factors | |||
| Bhat PN, et al. (20) | 2018 | Self-reported perceptions of pediatric cardiac ICU clinicians | Inadequate data assessment; Anchoring on one diagnosis; Provider inexperience |
| Cifra CL, et al. (15) | 2015 | Analysis at PICU morbidity and mortality conference | Problems in hypothesis generation (inadequate differential diagnoses) |
| Cifra CL, et al. (12) | 2018 | Retrospective chart review using a standard validated tool to determine occurrence of diagnostic error | Suboptimal diagnostic evaluations given available clinical information |
| Su L, et al. (21) | 2015 | Qualitative review of clinical videos in real time at the bedside | Unexpected clinical events; False reassurance from the presence of other clinicians; Lack of specialized knowledge |
| Fischer JE, et al. (22) | 2003 | Retrospective chart review | Conditions that can present along a spectrum of acuity (e.g., sepsis) |
| Systems Factors | |||
| Cifra CL, et al. (12) | 2018 | Retrospective chart review using a standard validated tool to determine occurrence of diagnostic error | Night shift admissions |
| Bhat PN, et al. (20) | 2018 | Self-reported perceptions of pediatric cardiac ICU clinicians | Delays in obtaining diagnostic studies due to inability to travel off-unit for unstable patients; Suboptimal care coordination related to deficiencies in communication and teamwork; Frequent interruptions to workflow |
| Combined Cognitive and Systems Factors | |||
| Avesar M, et al. (23) | 2019 | Analysis of clinician behavior during simulated clinical vignettes | Work environment and culture (systems) influence clinicians’ decisions to challenge existing diagnosis (cognitive) |
| Cifra CL, et al. (24) | 2017 | Analysis of ethnographic data (clinician observations and interviews) gathered during patient admission to the PICU | The characteristics of referral communication between clinicians, patterns of communication of patient data by trainees to intensivists, and manner in which health information technology organizes and presents clinical data (systems) influences intensivists’ diagnostic decision-making (cognitive) |
PICU - pediatric intensive care unit
Cognitive Factors
Two studies showed that 20%−33% of diagnostic errors were due to clinicians’ cognitive errors (15, 16)—these included inadequate data assessment and anchoring (20), problems in hypothesis generation (inadequate differential diagnoses) (15), and suboptimal diagnostic evaluations given available clinical information, especially information from the patient history (12).
One study using video review of PICU clinicians’ bedside actions in real-time illustrated cognitive errors leading to substantial delays in recognizing acute, life-threatening conditions. These included diagnostic delays when an acute condition is unexpected (e.g., delay in recognizing unanticipated cardiac arrest), diagnostic delays due to false reassurance from the mere presence of other PICU staff at the bedside despite objective data showing patient deterioration, and diagnostic errors due to lack of expertise (e.g., non-experts have difficulty discerning changes in cardiac rhythm if a patient had a baseline abnormal rhythm) (21). Cognitive challenges were also prominent when PICU clinicians were confronted with conditions that can present with a wide spectrum of acuity such as infection/sepsis (22).
Systems Factors
The same two studies as above also showed that 40%−67% of diagnostic errors were the result of systems problems (15, 16). One study reported that night shift admission may be associated with diagnostic error, and that discrepancies between documented PICU admission and discharge diagnoses may be used as a flag for misdiagnosis (12). Pediatric cardiac ICU clinicians reported that the most common systems breakdowns involved delays in obtaining diagnostic studies due to inability to travel off-unit for unstable patients and suboptimal care coordination related to deficiencies in communication and teamwork (20).
Combined Cognitive and Systems Factors
One study showed that 40% of misdiagnoses resulted from both cognitive and systems failures (15). Two additional studies illustrate this by showing that the diagnostic process includes contextual and social factors that are still poorly understood. One study showed that rudeness of transferring clinicians during PICU handoffs resulted in unwillingness of clinicians to challenge an inaccurate diagnosis (23). Focused ethnography in the PICU showed that referral communication for PICU admission, synthesis and communication of patient data by trainees to intensivists, and health information technology all contribute to intensivists’ diagnostic decision-making (24).
DISCUSSION
This systematic review demonstrates the large gap in our knowledge of diagnostic error in the PICU. It also illustrates the challenges of synthesizing data from a limited number of studies with heterogeneous study designs, study samples, data sources, and data collection procedures. Nevertheless, this review affirms that diagnostic errors are an important problem in pediatric critical care and further inquiry into how diagnostic errors occur is warranted to prevent and mitigate them in critically ill children. We outline the major gaps in the literature identified and propose future research directions to address these gaps to improve diagnosis in the PICU (Table 3).
Table 3.
Gaps in Knowledge on Diagnostic Error in the Pediatric Intensive Care Unit and Recommended Future Directions in Research
| Gaps in Knowledge |
|---|
| Much information on diagnostic error is limited to PICU mortalities due to over-reliance on autopsy studies |
| Unknown prevalence of diagnostic error across a large general PICU population and across subpopulations (e.g., cardiac ICU, trauma, sepsis patients) |
| Little known about the impact of diagnostic error on PICU patients, their families, clinicians, and organizations |
| No conceptual model of the diagnostic process in pediatric critical care, which leaves gaps in our understanding of factors involved in the diagnostic process and potential vulnerabilities in diagnostic decision-making |
| Future Directions in Research |
| Continue efforts to increase autopsy rates in the PICU while decreasing reliance on autopsy studies as the main source of information on diagnostic error |
| Conduct large multi-center studies including relevant PICU subpopulations to characterize diagnostic error epidemiology |
| Identify PICU populations, situations, and processes that are at increased risk for diagnostic error |
| Conduct studies to determine the impact of diagnostic error including physical, psychological, and financial harm to patients, families, clinicians, and organizations |
| Develop standard diagnostic error identification and analysis frameworks that PICUs can incorporate into existing patient safety programs |
| Study the diagnostic process in the PICU and develop/adapt existing conceptual models of diagnosis to the pediatric critical care setting |
| Balance focus between studying the diagnosis of individual diseases and studying common underlying system-related causes of diagnostic error |
| Leverage a variety of research methods to study diagnostic error in the PICU; integrate and triangulate findings from different methods if possible |
| Follow standard research methodology when possible (e.g., standard methods of chart review) to make findings comparable across studies |
PICU - pediatric intensive care unit
Gaps in Current Knowledge
The prevalence of diagnostic errors varied widely but were comparable to adult studies. Autopsy studies showed diagnostic error rates of 10%−23% in children (8–10) vs. 23% in adults (25) and record reviews (using similar chart review tools) showed diagnostic error rates of 8%−12% in children (12, 13) vs. 7% in adults (26). Autopsy studies were the dominant source of epidemiological data on diagnostic errors in the PICU despite having autopsy rates of only 20%−48%, limiting most of our knowledge of diagnostic error to patients who died in-hospital.
Retrospective cohort studies included samples that may be more representative of the general PICU population, which can provide estimates of diagnostic error that contribute not only to mortality but also to morbidity in PICU patients. For example, misdiagnosed neurologic disease are common diagnostic errors outside of autopsy studies (12, 13, 15). However, we were unable to identify multicenter studies describing diagnostic error epidemiology in large PICU populations which could have parsed differences in prevalence of error across PICU subgroups. Patient samples in the smaller retrospective studies varied significantly. Many studies narrowly focused on populations potentially at higher risk for error in order to more efficiently use available research resources since chart review requires significant time, effort, and expertise. Data sources and data collection procedures also varied widely, affecting results.
We found little information on the impact of diagnostic errors on critically ill children. In general adult and pediatric populations, diagnostic errors exact high financial costs, resulting in billions of dollars in payouts for malpractice claims (27–29) in addition to the unmeasured costs of extra care as a consequence of errors. Diagnostic errors can also be psychologically devastating to families, who report feelings of guilt and helplessness when they perceive that they were unable to advocate for their loved ones (30).
Identifying factors associated with diagnostic error in the PICU could provide insights into how and why diagnostic errors occur and pave the way for targeted surveillance and intervention. Early work on diagnostic error has traditionally categorized them into cognitive errors, systems problems, or both. However, disentangling cognitive- from systems-related factors may be difficult, as shown in a few studies in this review. The cognitive work of diagnosis occurs within and is affected by the ICU work system consisting of the critical care team, their tasks, technologies, unit and organizational factors, and the physical environment (6, 31). These complex interrelationships are illustrated in conceptual models of the diagnostic process (2, 6, 32), however no PICU-specific model exists. There is growing consensus that identifying specific failures in the diagnostic process, as opposed to classifying errors as cognitive- or systems-based, may make misdiagnosis easier to address (33). Moreover, different diagnostic errors likely share specific vulnerabilities in the diagnostic process, thus addressing them may prevent several diagnostic errors with common etiologies.
Future Directions in Research
Autopsies provide a useful way to identify missed diagnoses and efforts to obtain them should be invigorated (34). However, scientific advances will require knowledge beyond autopsies as the main source of information regarding diagnostic error. At the unit level, we need to develop and promote processes to identify and analyze diagnostic error that PICUs can incorporate into current patient safety programs (35). Recent work show that diagnostic errors can be surfaced by traditional incident reporting (36) and examined in detail using modified adverse event analysis tools at the morbidity and mortality conference (35).
The considerable resources of the pediatric critical care research community supported by growing institutional and government support for diagnostic error research (38, 39) could be leveraged to conduct large multicenter studies to investigate the epidemiology and impact of diagnostic error. This work is necessary to identify the PICU populations at increased risk for diagnostic error and misdiagnosis-related harm and will lay the foundation for future work on developing targeted interventions. Additionally, both quantitative and qualitative approaches should be used to study diagnostic error thus creating richer data to help triangulate and confirm research findings (40). Standard or widely-accepted research methods and tools should be used as much as possible (e.g., use of the Revised Safer Dx Instrument to guide chart review (41)) to allow for valid comparisons across studies.
Accurate and timely diagnosis in the PICU hinges only partly on intensivists’ biomedical knowledge and clinical reasoning (2, 33). Many contextual and social factors that affect diagnosis in pediatric critical care exist and are poorly understood. In addition to studying the characteristics of high-risk PICU populations, specific circumstances that render patients vulnerable to diagnostic error warrant evaluation. For example, studies show that diagnostic discordance occurs commonly in pediatric inter-hospital transfers (42) – this may be a promising PICU cohort to study in terms of improving transitions of care to prevent misdiagnosis.
We identified several types of clinical conditions that seem to be at risk for diagnostic error. Much of the effort thus far to improve diagnosis in the PICU involve disease-specific approaches, such as research on biomarkers (43), imaging innovations at the bedside (44), and refinement of diagnostic criteria for selected conditions (45). This disease-oriented approach is necessary because diseases have unique pathophysiology; however, an exclusive focus on selected diseases would neglect a substantial proportion of misdiagnoses. Many diagnostic errors are underpinned by common diagnostic process missteps and systems vulnerabilities that require disease-agnostic approaches to address. To identify vulnerabilities in pediatric critical care diagnosis, it is important to study the diagnostic process and adapt existing conceptual models of diagnosis (2, 6, 32) to create PICU-specific approaches and frameworks. Thus, we advocate for a balanced strategy that combines biomedical discovery with multidisciplinary research into the PICU diagnostic process and care delivery systems that cut across unique diseases (46).
This work has several limitations. Studies included were heterogeneous, thus findings were challenging to synthesize. Among autopsy studies, there was potential for selection bias given that autopsy rates were <50%. Among retrospective chart review studies, there was wide variation in data sources and data collection procedures, which may have resulted in different determinations of diagnostic error and contributory factors. Studies were also conducted at different centers with varying capacities for staffing including trainee oversight, diagnostic testing, and other organizational factors, which may have affected reported diagnostic error rates. We did not formally assess or restrict the quality of included studies and there is a possibility that authors may have misclassified diagnostic errors. Despite these limitations, our results on the prevalence and types of diagnostic error are similar to those found in the adult ICU. This work shows which gaps need to be addressed and informs future work on improving diagnosis in pediatric critical care.
CONCLUSIONS
There is a large gap in our knowledge of diagnostic errors in the PICU, though we do know that diagnostic errors are common and cause harm in critically ill children. Future directions include the development of local programs to identify and analyze diagnostic errors and the creation of research opportunities that involve a balanced focus between studying the diagnosis of individual diseases and describing common underlying system- and process-related determinants of diagnostic error. All of these actions can advance our understanding of how diagnostic errors occur in the PICU and help prevent and mitigate their impact on our patients and their families.
Supplementary Material
Research in Context.
Research to understand diagnostic errors has advanced in the past decade but little is known about diagnostic errors in critically ill children.
Harmful diagnostic errors occur up to 48% more often in intensive care than in the general inpatient wards, but specific factors in critical care that predispose patients to diagnostic error remain unknown.
This systematic review summarizes current knowledge of diagnostic errors in the pediatric intensive care unit and proposes research directions to mitigate diagnostic error-related harm.
What This Study Adds.
Diagnostic errors are a serious and prevalent problem in pediatric critical care but persistent knowledge gaps of how and why they occur remain.
Strategies to close these knowledge gaps include identifying errors extending beyond autopsies, multicenter efforts to delineate diagnostic error epidemiology, and employing disease-agnostic approaches that account for underlying systems and process factors affecting PICU diagnosis.
PICU leaders and staff can develop local programs to identify and analyze diagnostic errors. PICU collaboratives and professional organizations can support multidisciplinary work balancing disease-oriented research with systems-oriented investigations into the PICU care delivery processes that affect diagnosis.
ACKNOWLEDGMENTS
The authors thank Heather Healy (clinical education librarian) for her assistance in performing a systematic electronic search of databases to identify articles for inclusion in this study. We also thank Sonali Ramesh and Victoria Vivtcharenko for their assistance in retrieving and organizing articles.
Conflicts of Interest and Source of Funding:
Dr. Cifra is supported by the Agency for Healthcare Research and Quality (AHRQ) through a K08 grant (HS026965) and an internal start-up grant from the University of Iowa Carver College of Medicine Department of Pediatrics. Dr. Singh is supported by the VA Health Services Research and Development Service (Presidential Early Career Award for Scientists and Engineers USA 14-274), the VA National Center for Patient Safety, the AHRQ (R01HS27363), the Gordon and Betty Moore Foundation, and the Houston VA HSR&D Center for Innovations in Quality, Effectiveness and Safety (CIN 13-413). The content is solely the responsibility of the authors and does not necessarily represent the official views of the AHRQ. The remaining authors declare no conflicts of interest.
Copyright Form Disclosure:
Dr. Cifra’s institution received funding from the National Institutes of Health and the National Institute for Child Health and Human Development. She received funding from the Agency for Healthcare Research and Quality as a subcontract via MedStar Health Research Institute (AHRQ) and received support for article research from the AHRQ. Dr. Singh received support for article research from the government. Drs. Custer and Facker have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.National Academies of Sciences, Engineering, and Medicine: Summary. In: Improving Diagnosis in Health Care. Washington, D.C.: The National Academies Press; 2015. p. 1–18. [Google Scholar]
- 2.Bergl PA, Nanchal RS, Singh H: Diagnostic Error in the Critically III: Defining the Problem and Exploring Next Steps to Advance Intensive Care Unit Safety. Ann Am Thorac Soc 2018; 15:903–907 [DOI] [PubMed] [Google Scholar]
- 3.Roland D, Snelson E: “So why didn’t you think this baby was ill?” Decision-making in acute paediatrics. Arch Dis Child Educ Pract Ed 2019; 104:43–48 [DOI] [PubMed] [Google Scholar]
- 4.Moher D, Liberati A, Tetzlaff J, et al. : Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009; 339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldman L, Sayson R, Robbins S, et al. : The value of the autopsy in three medical eras. N Engl J Med 1983; 308:1000–1005 [DOI] [PubMed] [Google Scholar]
- 6.National Academies of Sciences, Engineering, and Medicine: The diagnostic process. In: Improving Diagnosis in Health Care. Washington, D.C.: The National Academies Press; 2015. p. 31–80. [Google Scholar]
- 7.Singh H, Graber ML, Kissam SM, et al. : System-related interventions to reduce diagnostic errors: a narrative review. BMJ Qual Saf 2012; 21:160–170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Custer JW, Winters BD, Goode V, et al. : Diagnostic Errors in the Pediatric and Neonatal ICU: A Systematic Review*. Pediatr Crit Care Med 2015; 16:29–36 [DOI] [PubMed] [Google Scholar]
- 9.Widmann R, Caduff R, Giudici L, et al. : Value of postmortem studies in deceased neonatal and pediatric intensive care unit patients. Virchows Arch 2017; 470:217–223 [DOI] [PubMed] [Google Scholar]
- 10.Carlotti APCP, Bachette LG, Carmona F, et al. : Discrepancies Between Clinical Diagnoses and Autopsy Findings in Critically Ill Children: A Prospective Study. Am J Clin Pathol 2016; 146:701–708 [DOI] [PubMed] [Google Scholar]
- 11.Blanco C, Steigman C, Probst N, et al. : Discrepancies between autopsy and clinical findings among patients requiring extracorporeal membrane oxygenator support. ASAIO J 2014; 60:207–210 [DOI] [PubMed] [Google Scholar]
- 12.Cifra CL, TenEyck P, Dawson JD, et al. : Piloting methods to determine factors associated with diagnostic error on admission to a pediatric intensive care unit. New Orleans, LA: Diagnosis; 2018. 5(4):eA80 [Google Scholar]
- 13.Davalos MC, Samuels K, Meyer AND, et al. : Finding Diagnostic Errors in Children Admitted to the PICU. Pediatr Crit Care Med 2017; 18:265–271 [DOI] [PubMed] [Google Scholar]
- 14.Cifra CL, Jones KL, Ascenzi J, et al. : The morbidity and mortality conference as an adverse event surveillance tool in a paediatric intensive care unit. BMJ Qual Saf 2014; 23:930–938 [DOI] [PubMed] [Google Scholar]
- 15.Cifra CL, Jones KL, Ascenzi JA, et al. : Diagnostic Errors in a PICU: Insights from the Morbidity and Mortality Conference. Pediatr Crit Care Med 2015; 16:468–476 [DOI] [PubMed] [Google Scholar]
- 16.Frey B, Doell C, Klauwer D, et al. : The Morbidity and Mortality Conference in Pediatric Intensive Care as a Means for Improving Patient Safety. Pediatr Crit Care Med 2016; 17:67–72 [DOI] [PubMed] [Google Scholar]
- 17.Fink AZ, Levin TL, Blumfield E, et al. : Discrepancies in Radiograph Interpretation Between Pediatric Radiologists and Pediatric Intensivists in the Pediatric or Neonatal Intensive Care Unit. J Am Coll Radiol 2018; 15:1580–1586 [DOI] [PubMed] [Google Scholar]
- 18.Nesterova GV, Leftridge CA Jr, Natarajan AR, et al. : Discordance in interpretation of chest radiographs between pediatric intensivists and a radiologist: impact on patient management. J Crit Care 2010; 25:179–183 [DOI] [PubMed] [Google Scholar]
- 19.Labib JR, Kamal Elden NM, Hegazy AA, Labib NA. Incident Reporting System in Pediatric Intensive Care Units of Cairo Tertiary Hospital: An Intervention Study. Arch Pediatr Infect Dis 2019;7(4):e91774. [Google Scholar]
- 20.Bhat PN, Costello JM, Aiyagari R, et al. : Diagnostic errors in paediatric cardiac intensive care. Cardiol Young 2018; 28:675–682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Su L, Kaplan S, Waller M: Video review produces insight into diagnostic errors. Diagnosis 2015; 2:eA29–eA30 [Google Scholar]
- 22.Fischer JE, Seifarth FG, Baenziger O, et al. : Hindsight judgement on ambiguous episodes of suspected infection in critically ill children: poor consensus amongst experts? Eur J Pediatr 2003; 162:840–843 [DOI] [PubMed] [Google Scholar]
- 23.Avesar M, Erez A, Essakow J, et al. : The effect of rudeness on challenging diagnostic error: a randomized controlled simulation trial. Crit Care Med 2019; 47(1):682 [Google Scholar]
- 24.Cifra CL, Dukes KC, Reisinger HS, et al. : Using ethnography to understand the diagnostic process in a pediatric intensive care unit. Diagnosis 2017; 4:eA115 [Google Scholar]
- 25.Winters B, Custer J, Galvagno SM Jr, et al. : Diagnostic errors in the intensive care unit: a systematic review of autopsy studies. BMJ Qual Saf 2012; 21:894–902 [DOI] [PubMed] [Google Scholar]
- 26.Bergl PA, Taneja A, El-Kareh R, et al. : Frequency, Risk Factors, Causes, and Consequences of Diagnostic Errors in Critically Ill Medical Patients: A Retrospective Cohort Study. Crit Care Med 2019; 47:e902–e910 [DOI] [PubMed] [Google Scholar]
- 27.Saber Tehrani AS, Lee H, Mathews SC, et al. : 25-Year summary of US malpractice claims for diagnostic errors 1986–2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf 2013; 22:672–680 [DOI] [PubMed] [Google Scholar]
- 28.Gupta A, Snyder A, Kachalia A, et al. : Malpractice claims related to diagnostic errors in the hospital. BMJ Qual Saf 2017;27(1):bmjqs-2017–006774 [DOI] [PubMed] [Google Scholar]
- 29.Carroll AE, Buddenbaum JL: Malpractice Claims Involving Pediatricians: Epidemiology and Etiology. Pediatrics 2007; 120:10–17 [DOI] [PubMed] [Google Scholar]
- 30.Giardina TD, Haskell H, Menon S, et al. : Learning From Patients’ Experiences Related To Diagnostic Errors Is Essential For Progress In Patient Safety. Health Aff 2018; 37:1821–1827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O’Hara S, Klar RT, Patterson ES, et al. : Macrocognition in the Healthcare Built Environment (mHCBE): A Focused Ethnographic Study of “Neighborhoods” in a Pediatric Intensive Care Unit. HERD 2018; 11:104–123 [DOI] [PubMed] [Google Scholar]
- 32.Singh H, Sittig DF: Advancing the science of measurement of diagnostic errors in healthcare: the Safer Dx framework. BMJ Qual Saf 2015; 24:103–110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Graber ML: Progress understanding diagnosis and diagnostic errors: thoughts at year 10. Diagnosis 2020;7(3):151–159 [DOI] [PubMed] [Google Scholar]
- 34.Liao JM, Singh H: Reviving the Autopsy as a Diagnostic Error–Reduction Tool. Lab Med 2013; 44:186–190 [Google Scholar]
- 35.Singh H, Bradford A, Goeschel C: Operational measurement of diagnostic safety: state of the science. Diagnosis 2020July25:/j/dx.ahead-of-print/dx-2020–0045/dx-2020–0045.xml. doi: 10.1515/dx-2020-0045. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 36.Marshall TL, Ipsaro AJ, Le M, et al. : Increasing Physician Reporting of Diagnostic Learning Opportunities. Pediatrics 2021; 147(1):e2019400. [DOI] [PubMed] [Google Scholar]
- 37.Reilly JB, Myers JS, Salvador D, et al. : Use of a novel, modified fishbone diagram to analyze diagnostic errors. Diagn Berl Ger 2014; 1:167–171 [DOI] [PubMed] [Google Scholar]
- 38.Coalition to Improve Diagnosis [Internet].Soc Improve Diagn Med [cited 2021 Jan 12] Available from: https://www.improvediagnosis.org/coalition/
- 39.Lujan BR: Improving Diagnosis in Medicine Act of 2019 [Internet].2019; [cited2021 Jan 12] Available from: https://www.congress.gov/bill/116th-congress/house-bill/5014/text
- 40.Zwaan L, Singh H: The challenges in defining and measuring diagnostic error. Diagn Berl Ger 2015; 2:97–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Singh H, Khanna A, Spitzmueller C, et al. : Recommendations for using the Revised Safer Dx Instrument to help measure and improve diagnostic safety. Diagnosis 2019; 6(4):315–323 [DOI] [PubMed] [Google Scholar]
- 42.Philpot C, Day S, Marcdante K, et al. : Pediatric interhospital transport: diagnostic discordance and hospital mortality. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc 2008; 9:15–19 [DOI] [PubMed] [Google Scholar]
- 43.Lautz AJ, Dziorny AC, Denson AR, et al. : Value of Procalcitonin Measurement for Early Evidence of Severe Bacterial Infections in the Pediatric Intensive Care Unit. J Pediatr 2016; 179:74–81.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Valla FV, Young DK, Rabilloud M, et al. : Thigh Ultrasound Monitoring Identifies Decreases in Quadriceps Femoris Thickness as a Frequent Observation in Critically Ill Children. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc 2017; 18:e339–e347 [DOI] [PubMed] [Google Scholar]
- 45.Khemani RG, Smith LS, Zimmerman JJ, et al. : Pediatric acute respiratory distress syndrome: definition, incidence, and epidemiology: proceedings from the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc 2015; 16:S23–40 [DOI] [PubMed] [Google Scholar]
- 46.Zwaan L, Singh H: Diagnostic error in hospitals: finding forests not just the big trees. BMJ Qual Saf 2020; 29(12):961–964 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


