Abstract
Background:
Poor mental health may hinder diet quality in pregnancy.
Objective:
This study 1) examined whether stress and depressive symptoms are associated with diet quality (via Healthy Eating Index (HEI)-2015 total scores and dietary intake of food groups/nutrients that align with HEI-2015 components) and 2) tested race as a moderator in the relationship between mental health and diet quality.
Design:
This was a cross-sectional analysis of baseline data from a randomized controlled trial collected January 2015—January 2019 in Columbia, South Carolina. Trained staff administered demographic and psychosocial questionnaires and conducted anthropometric measures. Participants completed two 24-hour dietary recalls which were self-administered (one on-site, one at home).
Participants:
The Health in Pregnancy and Postpartum study was a randomized controlled trial targeting excessive gestational weight gain among pregnant women with overweight/obesity (N=228).
Main outcome measures:
HEI-2015 total scores and food groups/nutrients that align with HEI-2015 were calculated.
Statistical analyses performed:
Multiple linear regression models were used to estimate the relationship between mental health and HEI-2015 total scores and dietary intake of food groups/nutrients that align with HEI-2015 components. Multiplicative interaction terms of stress or depressive symptoms with race were used to determine moderation.
Results:
Participants’ diet quality was suboptimal (M=52.0 ± 11.7, range 27–85). Stress was negatively associated with HEI-2015 total scores (crude but not adjusted model). Stress scores were positively associated with consumption of dairy, refined grains, and added sugars and negatively associated with total protein foods. Depressive symptoms were positively associated with consumption of dairy, refined grains, and saturated fats. Race was not a moderator.
Conclusions:
Diet quality was poor overall, but stress and depressive symptoms were not associated with HEI-2015 total scores in adjusted models. Excluding dairy, stress and depressive symptoms were associated with the consumption of food groups/nutrients related to worse diet quality. These relationships should be examined longitudinally to help establish causality and inform future interventions.
Keywords: stress, depression, mental health, diet quality, pregnancy
Introduction
Optimal diet quality is important for both maternal and child health.1,2 Pregnancy can be a time of increased stress3 and depressive symptoms and stress have been closely linked.4 Specifically, depressive symptoms and stress have been associated with poor diet quality in pregnancy,5 but both are understudied modifiable factors that may act as barriers to improving diet quality in pregnancy.6
Few studies have examined associations between stress, depressive symptoms, and diet quality in pregnancy using the Healthy Eating Index-2015 (HEI-2015).7 Furthermore, there are few studies that examine these associations among racially diverse samples of women who began pregnancy with overweight or obesity.8 The HEI-2015 is reliable and valid for all segments of the population for which the USDA Food Patterns are appropriate, including pregnant women.9–11 Therefore, using the HEI-2015 is ideally suited for examining diet quality in pregnant women from diverse racial/ethnic backgrounds.
To address these gaps, the objectives of this study were to 1) determine whether stress scores and depressive symptoms are associated with diet quality among a racially diverse sample of pregnant women in South Carolina (SC) with overweight or obesity, and 2) test whether race moderates the relationships between mental health (i.e., stress and depressive symptoms) and diet quality. It was hypothesized that pregnant women with higher stress scores and depressive symptoms would have lower HEI-2015 total scores and greater consumption of HEI-2015 components that are commonly overconsumed (i.e., sodium, refined grains, saturated fats, and added sugars). Additionally, it was hypothesized that African-American (AA) women would have higher levels of stress and depressive symptoms, and these would be associated with lower HEI-2015 total scores and higher consumption of sodium, refined grains, saturated fats, and added sugars compared to White women. This hypothesis was informed by Davis and colleagues’ framework for stress reactivity and maternal obesity development in pregnancy, which posits that AA women experience disproportionate amounts of chronic stress due to social disadvantages (e.g., discrimination, single parenthood, and poverty).12
Methods
The Health in Pregnancy and Postpartum (HIPP) study was a randomized controlled trial examining the efficacy of a theory-based behavioral lifestyle intervention to reduce excessive gestational weight gain (GWG) among White and AA pregnant women with overweight or obesity, as compared to a standard care intervention. The HIPP study is registered in clinicaltrials.gov (NCT02260518). As seen in Figure 1, there were 1,578 women who were initially eligible, 686 who were fully eligible, 270 who completed the baseline visit, and 228 who were randomized and included in the sample. This paper reports a cross-sectional analysis of demographic, mental health, and dietary data measured at baseline (N=228). Baseline assessments for this analysis were conducted from January 2015 to January 2019.
Figure 1.
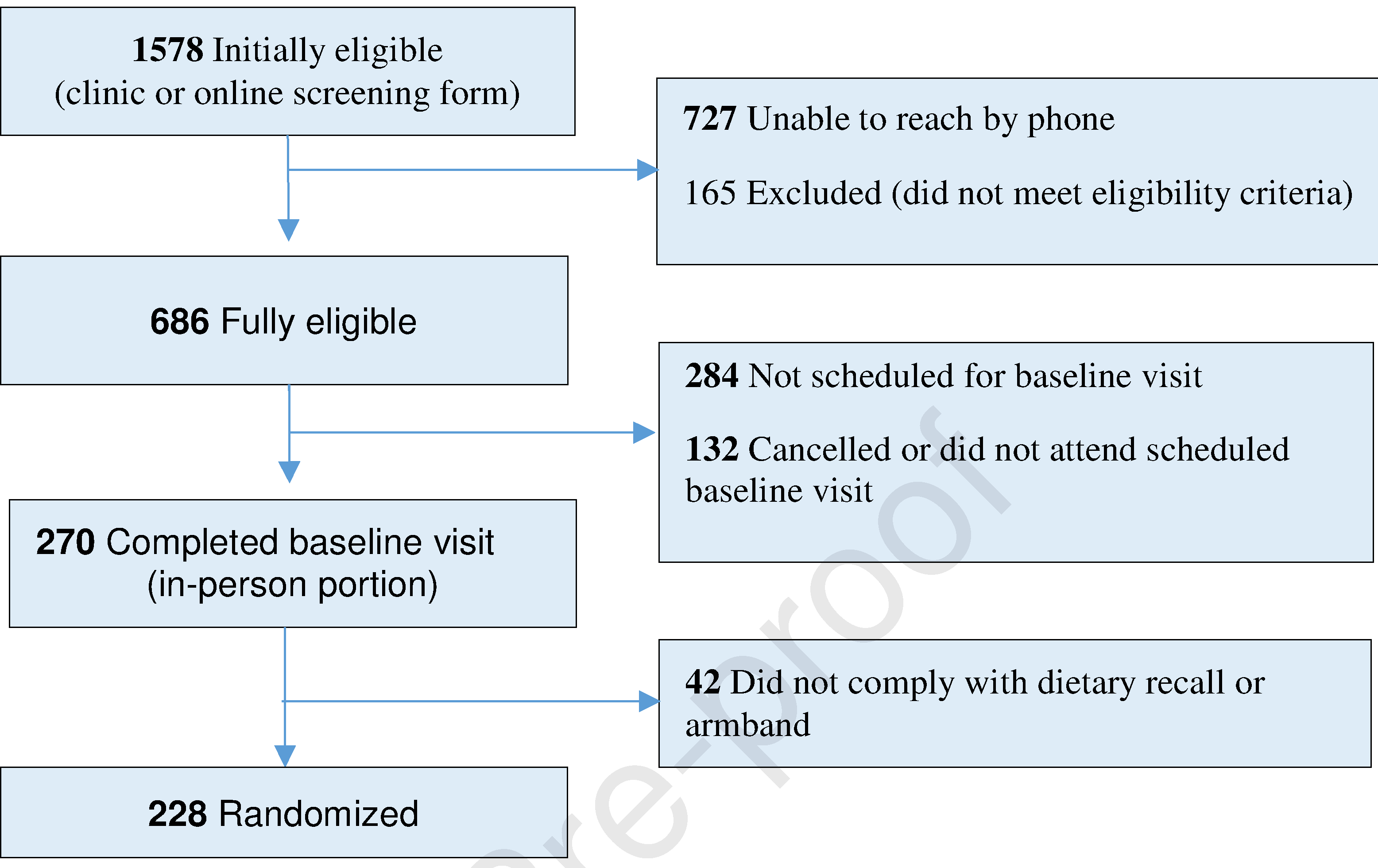
Health in Pregnancy and Postpartum (HIPP) study recruitment flow chart, January 2015 to January 2019, Columbia, SC
A full description of HIPP study methods have been published elsewhere.13 In brief, women were recruited to participate primarily through 13 obstetrics and gynecology (OB/GYN) clinics in the greater Columbia, SC area and adjacent counties, with some self-referrals in response to community and social media advertisements. Women were eligible if they: (a) were between 18–44 years of age, (b) self-identified as White or Black/AA, (c) could read and speak English, (d) had no plans to move outside of the geographic area in the next 18 months, (e) were ≤ 16 weeks gestation, and (f) had a pre-pregnancy body mass index (BMI) ≥ 25 kg/m2 and a pre-pregnancy weight ≤ 370 pounds. Women were excluded if they had contraindications to physical activity during pregnancy.14 Eligible women who met inclusion criteria and completed a baseline measurement visit were included in these analyses, regardless of their long-term participation in the intervention. The research was conducted in accordance with prevailing ethical principles and Institutional Review Boards at the participating university and health care systems approved the study protocol. All women provided written informed consent to participate.
Measures
At the baseline visit, demographic, psychosocial, and anthropometric measures were collected by the interviewer, while the 24-hour dietary recalls were self-administered after measurement staff provided instructions to participants on how to complete it as described below. A staff member was there to answer any questions during the first recall. If the participant had literacy challenges or did not have access to the internet for their second recall, measurement staff conducted an interviewer-administered recall over the phone. Baseline demographic variables were categorized as follows: age (18–24 years, 25–29 years, 30–34 years, 35–42 years), race (White or AA/Black), education (high school diploma/GED or less, some college, and college degree or higher), annual household income (<$35,000, $35,000-$49,900, $50,000− $74,900, $75,000+), parity (nulliparous or multiparous), marital status (married or not married), enrollment in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC)15 (not enrolled or enrolled), and pre-pregnancy weight status (overweight or obese). Pre-pregnancy BMI was calculated from participants’ self-reported pre-pregnancy height and weight. Questionnaires (except the 24-hour recalls) were administered by trained research staff.
Stress was measured using Cohen’s 4-item Perceived Stress Scale (PSS), which is a global measure of perceived stress designed to assess the degree to which situations in the previous month were perceived as stressful.16 Responses were indicated on a 5-point Likert-type scale, ranging from 0 (never) to 4 (very often), with possible scores ranging from 0 to 16. Higher scores indicated more perceived stress.
Depressive symptoms were measured using the 10-item Edinburgh Prenatal/Postnatal Depression Scale (EPDS), a widely-used self-report scale that has been validated for use during pregnancy and postpartum.17 Respondents rated how often in the past seven days they experienced the described thoughts or feelings on a 4-point Likert-type scale, ranging from 0 (never) to 3 (very often), with possible scores ranging from 0 to 30. Higher scores indicated more depressive symptoms.
Participants completed two unannounced 24-hour dietary recalls (one weekday and one weekend day, which included Fridays) at baseline through the National Cancer Institute’s (NCI) Automated Self-Administered 24-hour Dietary Recall (ASA24) online system.18 Two unannounced days were used to reduce potential bias. The ASA24 is a web-based dietary assessment tool that provides nutrient analysis of all foods and beverages reported during the data collection timeframe.18 The food groups and other dietary components needed to calculate HEI-2015 scores were provided by ASA24.
The two dietary recalls per participant were averaged and then scored using the simple HEI-2015 scoring algorithm method via SAS code provided by the NCI19 to generate HEI-2015 scores, which measure adherence to the 2015–2020 Dietary Guidelines for Americans (DGAs).9 The HEI-2015 includes 13 components, including nine adequacy components (i.e., total fruits, whole fruits, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant proteins, and fatty acids), which are dietary aspects that need to be increased. There are four moderation components (i.e., refined grains, sodium, added sugars, and saturated fats), which are dietary aspects that need to be limited/reduced. The maximum HEI-2015 total score is 100 points, with higher scores indicating better diet quality.
Statistical Analyses
Descriptive statistics were used to summarize participants’ sociodemographic characteristics, stress, depressive symptoms, and diet quality at baseline. Independent samples t-tests were used to test for mean differences in continuous variables by race. The χ2 test was used to examine differences in the proportion of categorical characteristics by race.
Multiple linear regression models were used to predict HEI-2015 total scores and intake of food groups/nutrients that align with HEI-2015 components. Stress and depressive symptoms were the independent variables and were modeled separately as continuous variables. Potential confounders were chosen a priori based on existing literature and included maternal race, educational attainment, age, marital status, parity, WIC enrollment, and pre-pregnancy BMI.5,20– 22WIC enrollment was used as a proxy for low-income since financial burden is a requirement to receive WIC benefits.23 Multiplicative interaction terms were used to determine if race moderated the relationship between stress, depressive symptoms, and diet quality in adjusted models. Beta coefficients and standard errors for significant models are presented. For all analyses, a P-value <0.05 indicated statistical significance. Statistical analyses were performed using SAS® software, version 9.4.24
Results
Study population.
Participants (n=228) were racially diverse (56% White, 44% AA), primarily married (67%), more than a third were 30–34 years old (37%), and almost a quarter of women (24%) were enrolled in WIC (Table 1). The sample was well-educated, since most women (59%) earned a college degree or higher. More than half of women had at least one child (57%) and just over half (52%) were classified as obese at the start of their pregnancy. The mean gestational age was 12.5 weeks (±2.4 weeks). Overall, participants had low levels of stress (M=4.7±3.2, range 0–14), low levels of depressive symptoms (M=5.9±4.5, range 0–20), and suboptimal HEI-2015 total scores (M=52.0 ± 11.7, range 27–85). Race differences in demographic characteristics are reported in Table 1. Average consumption of food groups/nutrients that align with HEI-2015 components are reported in Table 2. HEI-2015 component scores are reported in Table 3.
Table 1.
Baseline demographic and psychosocial characteristics of Health in Pregnancy and Postpartum (HIPP) participants (N=228), January 2015 to January 2019, Columbia, South Carolina
| Characteristic a | Total (n=228), n | Total % | White (n=127; 56%) | African-American b (n=101; 44%) | p-value |
|
| |||||
| Age in years, % | 0.02 | ||||
| 18–24 | 39 | 17.1 | 11.0 | 24.8 | |
| 25–29 | 63 | 27.6 | 26.0 | 29.7 | |
| 30–34 | 85 | 37.3 | 43.3 | 29.7 | |
| 35–42 | 41 | 18.0 | 19.7 | 15.8 | |
| Marital Status, % | <0.0001 | ||||
| Married | 152 | 66.7 | 84.2 | 44.6 | |
| Not married | 76 | 33.3 | 15.8 | 55.4 | |
| Education level, % | 0.02 | ||||
| High school or less | 28 | 12.3 | 8.7 | 16.8 | |
| Some college | 65 | 28.5 | 24.4 | 33.7 | |
| College degree/higher | 135 | 59.2 | 66.9 | 49.5 | |
| Annual household income, % c | <0.0001 | ||||
| <$35,000 | 66 | 29.0 | 15.8 | 45.5 | |
| $35,000–$49,900 | 31 | 13.7 | 12.6 | 14.9 | |
| $50,000–$74,900 | 44 | 19.4 | 22.0 | 15.8 | |
| $75,000+ | 86 | 37.9 | 48.8 | 23.8 | |
| WIC, % | <0.0001 | ||||
| Not enrolled | 174 | 76.3 | 89.8 | 59.4 | |
| Enrolled (parent and/or child receives food) | 54 | 23.7 | 10.2 | 40.6 | |
| Parity, % | 0.89 | ||||
| Nulliparous | 98 | 43.0 | 42.5 | 43.6 | |
| Multiparous | 130 | 57.0 | 57.5 | 56.4 | |
| Pre-pregnancy weight status, %d | 0.08 | ||||
| Overweight (BMI 25.0–29.9 kg/m2) | 110 | 48.2 | 53.5 | 41.6 | |
| Obese (BMI ≥ 30 kg/m2) | 118 | 51.8 | 46.5 | 58.4 | |
| Group randomization, % | 0.79 | ||||
| Intervention | 114 | 50.0 | 51.2 | 48.5 | |
| Standard Care | 114 | 50.0 | 48.8 | 51.5 | |
|
| |||||
| Characteristic e , Mean ± SD | Total | White | African-American | p-value | |
|
| |||||
| Age (years), range 18–42 | 29.7 ± 5.1 | 30.5 ± 4.5 | 28.6 ± 5.5 | 0.005 | |
| Gestational age (weeks), range 7–20 | 12.5 ± 2.4 | 12.2 ± 2.2 | 13.0 ± 2.6 | 0.01 | |
| Perceived stressf, range 0–14 | 4.7 ± 3.2 | 4.5 ± 3.0 | 5.0 ± 3.6 | 0.23 | |
| Depressive symptomsf, range 0–20 | 5.9 ± 4.5 | 5.6 ± 4.0 | 6.4 ± 5.0 | 0.16 | |
The χ2 test was used to examine differences in the proportion of categorical characteristics by race.
Includes two participants who indicated both AA and White as their race.
Percentages less than 100% due to a refused response.
Based upon self-reported pre-pregnancy height and weight.
Independent samples t tests were used to test for mean differences in continuous demographic characteristics by race.
Higher scores = greater perceived stress or depressive symptoms. Ranges reported are ranges observed in the study sample.
Table 2.
Health in Pregnancy and Postpartum (HIPP) participants’ (N=228) baseline Healthy Eating Index-2015 (HEI-2015) component intakes and total scoresa by race, January 2015 to January 2019, Columbia, South Carolina
| HEI-2015 Components | All (n=228) M ± SD | White (n=127) M ± SD | African-American (n=101) M ± SD | p-valueb |
|---|---|---|---|---|
|
| ||||
| Adequacy Components c | ||||
| Total Vegetables (cups) | 1.7 ± 1.1 | 1.8 ± 1.2 | 1.7 ± 1.1 | 0.46 |
| Greens and Beans (cups) | 0.3 ± 0.5 | 0.3 ±0.4 | 0.3 ± 0.5 | 0.86 |
| Total Fruits (cups) | 1.1 ± 1.1 | 1.0 ±1.0 | 1.1 ± 1.2 | 0.47 |
| Whole Fruits (cups) | 0.7 ± 0.9 | 0.8 ± 0.8 | 0.7 ± 0.9 | 0.58 |
| Whole Grains (oz.) | 0.7 ± 0.8 | 0.8 ± 0.8 | 0.5 ± 0.8 | 0.04 |
| Dairy (cups) | 1.7 ± 1.1 | 1.9 ± 1.2 | 1.5 ± 1.0 | 0.01 |
| Total Protein Foods (oz.) | 6.0 ± 3.4 | 5.7 ± 3.1 | 6.4 ± 3.7 | 0.10 |
| Seafood and Plant Proteins (oz.) | 1.3 ± 1.8 | 1.2 ± 1.6 | 1.4 ± 2.0 | 0.58 |
| Ratio of Unsaturated Fat to Saturated Fat | 1.9 ± 0.5 | 1.7 ± 0.4 | 2.0 ± 0.6 | <0.01 |
| Moderation Components d | ||||
| Sodium (mg) | 3661.8 ± 1322.0 | 3807.5 ± 1377.5 | 3478.5 ± 1231.0 | 0.06 |
| Refined Grains (oz.) | 5.3 ± 2.5 | 5.7 ± 2.5 | 4.8 ± 2.5 | 0.01 |
| Saturated Fats (g) | 26.2 ± 11.3 | 27.8 ± 25.7 | 24.2 ± 22.2 | 0.02 |
| Added Sugars (tsp eq.) | 14.7 ± 11.1 | 16.8 ± 12.3 | 12.1 ± 8.6 | <0.01 |
| Total Score | 52.0 ± 11.7 | 51.3 ± 12.1 | 52.7 ± 11.1 | 0.36 |
Scores reflect intake values averaged across 2 days.
Independent samples t-tests were used to test for mean differences in HEI-2015 components and total scores.
Adequacy components- dietary components that should be increased.
Moderation components- dietary components that should be consumed in moderation.
Table 3.
Health in Pregnancy and Postpartum (HIPP) participants’ (N=228) baseline Healthy Eating Index-2015 (HEI-2015) total scores and component scores, January 2015 to January 2019, Columbia, South Carolina.
| Participants’ Component Scores | |||||
|---|---|---|---|---|---|
| HEI-2015 Component | Standard for Achieving Maximum Score | Maximum Score | All | White | African-American |
|
| |||||
| ← Mean score±SD → | |||||
| Adequacy a | |||||
| Total Vegetables | ≥1.1 cup equiv. per 1,000 kcal | 5.0 | 3.5 ± 1.4 | 3.5 ± 1.4 | 3.5 ± 1.4 |
| Greens and Beans | ≥0.2 cup equiv. per 1,000 kcal | 5.0 | 2.6 ± 2.2 | 2.6 ± 2.1 | 2.5 ± 2.3 |
| Total Fruits | ≥0.8 cup equiv. per 1,000 kcal | 5.0 | 2.8 ± 1.9 | 2.7 ± 1.8 | 2.9 ± 1.9 |
| Whole Fruits | ≥0.4 cup equiv. per 1,000 kcal | 5.0 | 2.8 ± 2.1 | 3.0 ± 2.0 | 2.5 ± 2.2 |
| Whole Grains | ≥1.5 oz equiv. per 1,000 kcal | 10.0 | 2.3 ± 2.6 | 2.6 ± 2.6 | 2.0 ± 2.6 |
| Dairy | ≥1.3 cup equiv. per 1,000 kcal | 10.0 | 6.3 ± 2.8 | 6.6 ± 2.5 | 5.9 ± 3.0 |
| Total Protein Foods | ≥2.5 oz equiv. per 1,000 kcal | 5.0 | 4.4 ± 1.0 | 4.3 ± 1.0 | 4.5 ± 1.0 |
| Seafood and Plant Proteins | ≥0.8 oz equiv. per 1,000 kcal | 5.0 | 2.3 ± 2.2 | 2.4 ± 2.1 | 2.2 ± 2.2 |
| Ratio of Unsaturated Fat to Saturated Fat | (PUFAs + MUFAs)/SFAs ≥2.5 | 10.0 | 4.7 ± 3.2 | 4.2 ± 2.9 | 5.3 ± 3.4* |
| Moderation b | |||||
| Sodium | ≤1.1 gram per 1,000 kcal | 10.0 | 2.1 ± 2.6 | 2.2 ± 2.5 | 2.0 ± 2.7 |
| Refined Grains | ≤1.8 oz equiv. per 1,000 kcal | 10.0 | 6.0 ± 3.3 | 5.7 ± 3.2 | 6.3 ± 3.3 |
| Saturated Fats | ≤8% of energy | 10.0 | 5.0 ± 3.0 | 4.7 ± 2.9 | 5.3 ± 3.2 |
| Added Sugars | ≤6.5% of energy | 10.0 | 7.1 ± 2.8 | 6.7 ± 3.0 | 7.7 ± 2.5* |
| Total Score | 52.0 ± 11.7 | 51.3 ± 12.1 | 52.7 ± 11.1 | ||
Adequacy components-dietary components that should be increased.
Moderation components-dietary components that should be consumed in moderation.
p < 0.05
Diet quality, stress, and depressive symptoms.
The first aim was to examine if stress scores and depressive symptoms were associated with HEI-2015 total scores and food groups/nutrients that align with HEI-2015 components. Stress was negatively associated with HEI-2015 total scores in the crude model only. In terms of food groups/nutrients that align with HEI-2015 components, higher levels of stress were associated with greater consumption of dairy products (including all milk products, such as fluid milk, yogurt, cheese, and fortified soy beverages) [β (SE) 0.05 (0.02); p=0.02], refined grains [β (SE) 0.14 (0.05); p=0.01], and added sugars [β (SE) 0.61 (0.23; p=0.01)]. Additionally, higher levels of stress were associated with lower consumption of total protein foods (including meat, poultry, seafood, nuts, seeds, soy products, and legumes) [β (SE) −0.19 (0.07); p=0.01] (models not shown). Stress was not significantly associated with any other food group/nutrient aligned with HEI-2015 components.
Overall, depressive symptoms were not significantly related to HEI-2015 total scores in either the crude or adjusted analyses. Regarding food groups/nutrients that align with HEI-2015 components, higher levels of depressive symptoms were associated with greater consumption of dairy [β (SE) 0.06 (0.02); p<0.001], refined grains [β (SE) 0.11 (0.04); p<0.01], and saturated fats [β (SE) 0.44 (0.17); p=0.01] (models not shown). Depressive symptoms were not significantly associated with any other food group/nutrient aligned with HEI-2015 components.
Moderation analyses.
Aim 2 tested for moderation. Race did not moderate the relationships between stress and diet quality or depressive symptoms and diet quality, controlling for key covariates.
Discussion
Diet quality among HIPP participants was poor overall with an average HEI-2015 score of 52 out of 100. This is notably lower than the average HEI-2010 score of 63 previously observed among a large cohort of US pregnant women;25 however, their participants were mostly White (69%) and just over half of their participants (51%) had BMIs that fell within the normal weight category, making the HIPP sample unique. This study found that stress and depressive symptoms were not associated with lower HEI-2015 total scores among HIPP participants after controlling for key covariates. Findings from previous studies have been mixed. Some studies that have examined associations between mental health and diet quality scores in pregnancy have found that higher stress and/or depressive symptoms are associated with lower diet quality scores in pregnancy.5,26 Alternatively, Omidvar and colleagues found that neither depressive symptoms nor pregnancy-specific stress were significantly associated with healthy nutrition scores as measured by the Health-Promoting Lifestyle Profile.21 Stress and depressive symptoms among HIPP participants were generally low (average stress score of 5 out of 16; average depressive symptoms score of 6 out of 30) could have contributed to the null associations between mental health and HEI-2015 total scores. In a sample of pregnant women with more variability in stress and depressive symptoms scores, there might have been significant inverse associations between stress, depressive symptoms, and HEI-2015 total scores. Previous studies that observed significant associations were comprised of women from Pakistan26or majority Hispanic women in Texas;5,6 whereas AA women have been typically underrepresented.5,6 It is critical that AA women and women of other races and ethnicities are adequately represented in future studies in order to gain a better understanding of the contextual factors that influence diet quality and develop culturally-appropriate interventions to improve diet quality.
In terms of food groups/nutrients that align with HEI-2015 components, results showed that higher levels of stress were significantly associated with greater consumption of dairy, refined grains, and added sugars and lower consumption of total protein foods. With the exception of dairy, these findings support previous research that found that pregnant women who experience high stress levels are more likely to eat simple carbohydrates (i.e., refined grains and added sugars), which reduces their dietary quality throughout pregnancy.22 This eating pattern could be due to how individuals respond to stress as Lobel and colleagues found that pregnancy-specific stress significantly predicted unhealthy eating.27 Hurley and colleagues found that general stress was associated with greater consumption of protein in pregnancy; however, pregnancy-specific stress was associated with reduced protein and meat intake.22 Since pregnancy-specific stress and general stress have different relationships with aspects of diet quality in pregnancy,22 additional research is needed to clarify these relationships. Regarding refined grains and added sugars, Hurley and colleagues found that higher stress was associated with higher intake of breads and foods from the fats, oils, sweets, and snack group,22 which aligns with the current study’s findings.
In terms of depressive symptoms, higher levels of depressive symptoms were significantly associated with greater consumption of dairy, refined grains, and saturated fats. These findings around fat consumption support previous research that found higher depressive symptoms were associated with higher fat intake among pregnant women with overweight or obesity,8 including greater fast-food intake.28,29 Regarding dairy consumption, Miyake and colleagues found that greater yogurt intake was independently associated with a lower prevalence of depressive symptoms during pregnancy; however, they found no relationship between all dairy products and depressive symptoms.30 Since research on the relationship between depressive symptoms and dairy consumption during pregnancy is limited, this deserves further exploration in future studies.
Race did not moderate any of the relationships between stress or depressive symptoms and HEI-2015 total scores or food groups/nutrients that align with HEI-2015 components. It was hypothesized AA women would have higher levels of stress and depressive symptoms, and these would be associated with lower HEI-2015 total scores and higher consumption of sodium, refined grains, saturated fats, and added sugars compared to White women. This was based on Davis’ framework for stress reactivity and maternal obesity development in pregnancy posits that AA women experience disproportionate amounts of chronic stress due to social disadvantages (e.g., discrimination, single parenthood, and poverty).12 The lack of moderation by race could be due to comparable stress and depressive symptoms between AA and White participants, as well as AA women’s lower consumption of refined grains, saturated fats, and added sugars than their White counterparts. Furthermore, AA women in this study were generally well-educated (50% with a college degree or higher) and 40% had annual household incomes over $50,000. Future studies with greater variability in mental health can examine race as a moderator.
Limitations
HIPP participants’ stress and depressive symptoms scores were low overall, stress and depressive symptoms scores had limited variability, and scores were comparable between AA and White women which may have restricted the ability to detect significant associations with overall diet quality. Furthermore, this study’s cross-sectional design does not allow for the examination of mental health and diet quality at multiple time-points during pregnancy, or for the temporal association to be determined. It is plausible that mental health and diet quality have a bi-directional relationship,31 highlighting the need for large-scale, longitudinal study designs that examine stress, depressive symptoms, and diet quality at multiple time-points to determine the temporal and directional nature of this association.20 This study used two days of 24-hour recalls and it could be beneficial to assess additional days of dietary intake when examining diet in relation to health.32Since HIPP participants’ diet quality is lower than that of a large cohort of US pregnant women25 and the study used baseline data from a randomized trial, the sample may not be representative of all pregnant women with overweight or obesity in SC or the US. Study participants included only White and AA women, so findings may be not generalizable to other races or ethnicities. Additionally, the study’s sample size could be a limitation, especially for examining moderation by race, and the literature could benefit from having a larger study with a similar racial profile examine the associations between mental health and diet quality in pregnancy.
Strengths
This study addresses an important gap in the literature by examining stress and depressive symptoms as potential barriers to achieving optimal diet quality. The current study’s large percentage of AA women is a strength since very few studies have examined associations between stress and depressive symptoms with diet quality in pregnancy with more than 20% of African-Americans represented in their sample;8,28 however, their assessments of diet quality were limited to brief screeners assessing fat, fruit, vegetable, and fast-food intake through rapid screening tools compared to a comprehensive diet quality index score derived from multiple 24-hour recalls.
This study’s use of the HEI-2015 to assess diet quality is a strength because it standardizes the methods used through density standards,10 controls for diet quantity,10 and is reliable and valid for all segments of the population for which the USDA Food Patterns are appropriate,9 including pregnant women.
Conclusions
Overall, HIPP participants’ diet quality was poor and stress and depressive symptoms were not associated with HEI-2015 total scores in adjusted models. Stress and depressive symptoms were associated with greater consumption of food groups/nutrients that should be limited or consumed in moderation (i.e., refined grains, added sugars, and saturated fats) and greater consumption of dairy products. Stress was also associated with lower consumption of protein foods. These relationships should be examined longitudinally to help establish causality and inform future pregnancy lifestyle interventions.
Research Snapshot.
Research Question:
Are stress and depressive symptoms associated with HEI-2015 total scores and consumption of food groups/nutrients that align with HEI-2015 components in a sample of pregnant women in South Carolina?
Key Findings:
In this cross-sectional analysis of baseline data from the Health in Pregnancy and Postpartum Study (n=228), diet quality was poor. Mental health was not associated with HEI-2015 total scores in adjusted models. Stress was positively associated with dairy, refined grains, and added sugars and negatively associated with total protein foods consumption. Depressive symptoms were positively associated with dairy, refined grains, and saturated fat consumption.
Funding:
This study was supported by an NIH diversity supplement grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD078407) and was partially supported by a SPARC Graduate Research Grant from the Office of the Vice President for Research at the University of South Carolina.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest/Competing interests: The authors declare that they have no conflict of interest.
Contributor Information
Alycia K. Boutté, Department of Health Promotion, Education, and Behavior Graduate Trainee, Prevention Research Center Arnold School of Public Health University of South Carolina 915 Greene Street, Discovery 1 Room 529 Columbia, SC 29208.
Gabrielle M. Turner-McGrievy, Department of Health Promotion, Education, and Behavior Arnold School of Public Health University of South Carolina 915 Greene Street, Discovery 1 Room 552 Columbia, SC 29208.
Sara Wilcox, Department of Exercise Science Director, Prevention Research Center Arnold School of Public Health University of South Carolina 921 Assembly Street, Public Health Research Center 117 Columbia, SC 29208.
Jihong Liu, Department of Epidemiology and Biostatistics Arnold School of Public Health University of South Carolina 915 Greene Street, Discovery 1 Room 459 Columbia, SC 29208.
Jan M. Eberth, Department of Epidemiology and Biostatistics Deputy Director, SC Rural Health Research Center Arnold School of Public Health University of South Carolina 915 Greene Street, Discovery 1, Room 234 Columbia, SC 29208.
Andrew T. Kaczynski, Department of Health Promotion, Education, and Behavior Co-Investigator, Prevention Research Center Arnold School of Public Health University of South Carolina 915 Greene Street, Discovery 1 Room 545 Columbia, SC 29208.
References
- 1.Phillips C, Johnson NE. The impact of quality of diet and other factors on birth weight of infants. The American Journal of Clinical Nutrition. 1977;30(2):215–225. [DOI] [PubMed] [Google Scholar]
- 2.Stuebe AM, Oken E, Gillman MW. Associations of diet and physical activity during pregnancy with risk for excessive gestational weight gain. Am J Obstet Gynecol. 2009;201(1):58.e1–58.e8. 10.1016/j.ajog.2009.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Devine CM, Bove CF, Olson CM. Continuity and change in women’s weight orientations and lifestyle practices through pregnancy and the postpartum period: the influence of life course trajectories and transitional events. Social Science & Medicine. 2000;50(4):567–582. 10.1016/S0277-9536(99)00314-7 [DOI] [PubMed] [Google Scholar]
- 4.Hammen C. Stress and Depression. Annual Review of Clinical Psychology. 2005;1(1):293–319. 10.1146/annurev.clinpsy.1.102803.143938 [DOI] [PubMed] [Google Scholar]
- 5.Fowles ER, Stang J, Bryant M, Kim S. Stress, Depression, Social Support, and Eating Habits Reduce Diet Quality in the First Trimester in Low-Income Women: A Pilot Study. Journal of the Academy of Nutrition and Dietetics. 2012;112(10):1619–1625. 10.1016/j.jand.2012.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fowles ER, Bryant M, Kim S, et al. Predictors of Dietary Quality in Low-Income Pregnant Women: A Path Analysis. Nursing Research. 2011;60(5):286–294. 10.1097/NNR.0b013e3182266461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berube LT, Messito MJ, Woolf K, Deierlein A, Gross R. Correlates of Prenatal Diet Quality in Low-Income Hispanic Women. Journal of the Academy of Nutrition and Dietetics. 2019;119(8):1284–1295. 10.1016/j.jand.2019.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang M-W, Brown R, Nitzke S, Smith B, Eghtedary K. Stress, Sleep, Depression and Dietary Intakes Among Low-Income Overweight and Obese Pregnant Women. Matern Child Health J. 2015;19(5):1047–1059. 10.1007/s10995-014-1604-y [DOI] [PubMed] [Google Scholar]
- 9.U.S. Department of Health and Human Services, U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans.; 2015. Accessed February 6,2018. https://health.gov/dietaryguidelines/2015/resources/2015-2020_Dietary_Guidelines.pdf
- 10.Krebs-Smith SM, Pannucci TE, Subar AF, et al. Update of the Healthy Eating Index: HEI-2015. Journal of the Academy of Nutrition and Dietetics. 2018;118(9):1591–1602. 10.1016/j.jand.2018.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reedy J, Lerman JL, Krebs-Smith SM, et al. Evaluation of the Healthy Eating Index-2015. Journal of the Academy of Nutrition and Dietetics. 2018;118(9):1622–1633. 10.1016/j.jand.2018.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis EM, Stange KC, Horwitz RI. Childbearing, stress and obesity disparities in women: a public health perspective. Matern Child Health J. 2012;16(1):109–118. 10.1007/s10995-010-0712-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilcox S, Liu J, Addy CL, et al. A randomized controlled trial to prevent excessive gestational weight gain and promote postpartum weight loss in overweight and obese women: Health In Pregnancy and Postpartum (HIPP). Contemporary Clinical Trials. 2018;66:51–63. 10.1016/j.cct.2018.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Canadian Society for Exercise Physiology. PARmed-X for Pregnancy. Physical Activity Readiness Medical Examination. Published online 2015. Accessed August 25, 2020. http://www.csep.ca/cmfiles/publications/parq/parmed-xpreg.pdf
- 15.U.S. Department of Agriculture. Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) Accessed October 12, 2020. https://www.fns.usda.gov/wic
- 16.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of health and social behavior. Published online 1983:385–396. [PubMed] [Google Scholar]
- 17.Gibson J, McKenzie-McHarg K, Shakespeare J, Price J, Gray R. A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatrica Scandinavica. 2009;119(5):350–364. 10.1111/j.1600-0447.2009.01363.x [DOI] [PubMed] [Google Scholar]
- 18.National Cancer Institute. ASA24® Respondent Website Methodology. Published 2017. Accessed August 25, 2020. https://epi.grants.cancer.gov/asa24/respondent/methodology.html
- 19.National Cancer Institute. Healthy Eating Index SAS Code. Published July 24, 2020. Accessed October 31, 2020. https://epi.grants.cancer.gov/hei/sas-code.html
- 20.Baskin R, Hill B, Jacka FN, O’Neil A, Skouteris H. The association between diet quality and mental health during the perinatal period. A systematic review. Appetite. 2015;91:41–47. 10.1016/j.appet.2015.03.017 [DOI] [PubMed] [Google Scholar]
- 21.Omidvar S, Faramarzi M, Hajian-Tilak K, Nasiri Amiri F. Associations of psychosocial factors with pregnancy healthy life styles. PLoS One. 2018;13(1):e0191723. 10.1371/journal.pone.0191723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hurley KM, Caulfield LE, Sacco LM, Costigan KA, Dipietro JA. Psychsocial influences in dietary patterns during pregnancy. Journal of the American Dietetic Association. 2005;105(6):963–966. [DOI] [PubMed] [Google Scholar]
- 23.South Carolina Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) Benefits.gov. Published 2018. Accessed November 1, 2018. https://www.benefits.gov/benefit/2046
- 24.SAS Institute Inc. SAS/STAT (Version 9.4).SAS Institute Inc.; 2013. [Google Scholar]
- 25.Bodnar LM, Simhan HN, Parker CB, et al. Racial or Ethnic and Socioeconomic Inequalities in Adherence to National Dietary Guidance in a Large Cohort of US Pregnant Women. Journal of the Academy of Nutrition and Dietetics. 2017;117(6):867–877.e3. 10.1016/j.jand.2017.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saeed A, Raana T, Muhammad Saeed A, Humayun A, Saeed AM. Effect of antenatal depression on maternal dietary intake and neonatal outcome: a prospective cohort. Nutrition Journal. 2016;15:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lobel M, Cannella DL, Graham JE, DeVincent C, Schneider J, Meyer BA. Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychology. 2008;27(5):604–615. 10.1037/a0013242 [DOI] [PubMed] [Google Scholar]
- 28.Chang M-W, Brown R, Nitzke S. Fast Food Intake in Relation to Employment Status, Stress, Depression, and Dietary Behaviors in Low-Income Overweight and Obese Pregnant Women. Matern Child Health J. 2016;20(7):1506–1517. 10.1007/s10995-016-1949-5 [DOI] [PubMed] [Google Scholar]
- 29.Fowles ER, Timmerman GM, Bryant M, Kim S. Eating at Fast-Food Restaurants and Dietary Quality in Low-Income Pregnant Women. Western Journal of Nursing Research. 2011;33(5):630–651. 10.1177/0193945910389083 [DOI] [PubMed] [Google Scholar]
- 30.Miyake Y, Tanaka K, Okubo H, Sasaki S, Arakawa M. Intake of dairy products and calcium and prevalence of depressive symptoms during pregnancy in Japan: a cross-sectional study. BJOG. 2015;122(3):336–343. 10.1111/1471-0528.12972 [DOI] [PubMed] [Google Scholar]
- 31.Molyneaux E, Poston L, Khondoker M, Howard LM. Obesity, antenatal depression, diet and gestational weight gain in a population cohort study. Archives of Women’s Mental Health. 2016;19(5):899–907. 10.1007/s00737-016-0635-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Cancer Institute. 24-hour Dietary Recall (24HR) At a Glance | Dietary Assessment Primer. Accessed October 27, 2020. https://dietassessmentprimer.cancer.gov/profiles/recall/


