Abstract
Background
The Kyrgyz Republic (Kyrgyzstan) is one of few countries in Eastern Europe and Central Asia to provide methadone within its prisons, but uptake of this program has been suboptimal, in part because methadone uptake may have personal or social risks and consequences. Decision aids are evidence-based strategies that are designed to inform the patient’s choice by objectively providing information that incorporates patient preferences.
Methods
We conducted qualitative interviews in Kyrgyz and Russian with currently and formerly incarcerated people (n=36) in Kyrgyzstan from October 2016 to September 2018. Interviews explored factors influencing methadone utilization in prisons. Transcripts were coded by five researchers using content analysis. A secondary thematic analysis was conducted to determine factors specific to initiation or continuation of methadone treatment in prisons.
Results
We identified six interrelated themes affecting an individual’s decision to initiate or continue methadone treatment: 1) informal prison governance (incarcerated people governing themselves); 2) informal prison economy; 3) perceived and objective benefits of methadone treatment; 4) perceived and objective side effects of methadone treatment; 5) distrust of formal prison administration (medical and correctional staff); and 6) desire for a “cure” from addiction.
Conclusion
Respondents’ perceptions about benefits, side effects, and addiction as a curable disease are not consistent with the available evidence. An evidence-based, informed decision-making aid would need to address the six themes identified here, of which several are specific to the Kyrgyz prison context. Unlike decision aids elsewhere, the unique aspects of incarceration itself alongside the informal governance system strongly present within Kyrgyz prisons will need to be incorporated into decisional processes to promote HIV prevention and treatment in a region with high rates of HIV transmission and mortality.
Keywords: Eastern Europe and Central Asia (EECA), HIV, injection drug use, methadone, prisons, criminal subculture, informal governance
Introduction
As of the most recent Global Burden of Disease study, over 26 million people were diagnosed with opioid use disorder (OUD) worldwide, and the number of people who use drugs is growing (Degenhardt et al., 2018). This increase is associated with overdose deaths (Hedegaard et al., 2020; Rehm & Shield, 2019) and HIV and viral hepatitis transmission (Degenhardt et al., 2017).
Incarceration acts to concentrate people who inject drugs (PWID) and people with infectious diseases like HIV, making prisons an important touchpoint for prevention and treatment of both OUD and HIV (Dolan et al., 2016; Kamarulzaman et al., 2016). Due to policies criminalizing drug use, an estimated 58% of the global population of PWID experience incarceration at some point in their lives (Degenhardt et al., 2017). In countries where data exist, within-prison drug injection practices, especially with unsterile injecting equipment, are common (Azbel et al., 2016, 2018; Culbert et al., 2015; Izenberg et al., 2014), leading to large-scale infectious disease risk associated with injecting in prison (Altice et al., 2016).
Unfortunately, most countries do not have any form of medication for OUD available in their prisons (Harm Reduction International, 2019; Kamarulzaman et al., 2016). Methadone is listed as an essential medicine by the World Health Organization; it is the gold standard for treatment of OUD and key to preventing HIV in PWID. Methadone is an opioid agonist that activates µ-opioid receptors, thereby alleviating withdrawal symptoms and reducing cravings without inducing euphoria. It has a number of medical and social benefits, including substantially reducing opioid use and injection, fatal and non-fatal overdoses, transmission of HIV and HCV, and criminal behaviour; additionally, those who take methadone report increased capacity for maintaining employment and health-related quality of life (Degenhardt et al., 2019). OUD is a chronic, relapsing medical condition, and international guidelines recommend methadone for long-term maintenance (Kampman et al., 2015). These guidelines suggest that decisions regarding treatment cessation should be collaborative, involving both patient and provider when the patient has been stabilised.
Since 2010, Eastern Europe and Central Asia (EECA) has been one of the only regions of the world in which HIV incidence is steadily increasing, fuelled by high rates of injection drug use; currently, EECA has one of the highest HIV incidence and mortality rates worldwide (Joint United Nations Programme on HIV/AIDS, 2020). Countries in EECA have taken vastly different approaches to tackling intersecting epidemics of HIV, hepatitis, mass incarceration, and OUD. The Russian Federation, for example, has criminalised the use of methadone and other medications for OUD without exception (Heimer, 2018). Uzbekistan and Turkmenistan have followed Russia’s example (Harm Reduction International, 2019). Where methadone is allowed, the coverage is exceptionally low and is available only in pilot programs.
In 2002, the Kyrgyz Republic (Kyrgyzstan) introduced the first pilot within-prison methadone program in the region and expanded it in 2008 to multiple prisons (International Harm Reduction Association, 2008). Within-prison drug injection is prevalent in Kyrgyzstan; at least half of incarcerated people are estimated to inject drugs (Azbel et al., 2016). Despite the need for, and wide availability of, methadone therapy in Kyrgyz prisons, uptake of methadone in Kyrgyzstan’s prisons is low. As of the most recent available data, only 7% of eligible people in Kyrgyz prisons were enrolled in the methadone program (Azbel et al., 2016). Mathematical modelling from Ukraine, an EECA country with a similar OUD epidemic to that of Kyrgyzstan, suggests that at least 50% coverage of eligible patients in prison is required to avert 20% of all HIV cases in that country (Altice et al., 2016). Other modelling studies suggest that scaling up methadone in prisons would avert new HIV infections and deaths in multiple international settings (Degenhardt et al., 2019).
Given the low coverage of methadone in prisons, one tool that has the potential to increase the number of people who initiate methadone is the deployment of an evidence-based decision aid. Decision aids help patients make informed choices based on objective information and their personal values, and thus are an important strategy to guide patient-centred care. Decision aids can take different forms, including booklets, DVDs, or interactive tools like mobile applications. Previous studies have shown that using decision aids, often termed “informed decision-making” (IDM), may support patients to make more values-congruent choices (Stacey et al., 2017). Crucially, a previous systematic review found that decision aids for health treatment and screening decisions relating to a wide variety of medical conditions have reported improved overall health outcomes without any major adverse consequences (Stacey et al., 2017). Newly published research suggests that providing accurate information by trained interventionists may facilitate decisions about OUD treatment in the US (Mooney et al., 2020), including in the prison context (Banta-Green et al., 2020), but there are no evidence-based decision aids for within-prison OUD currently available outside of the US context.
Here, we determine context-specific factors that must be considered when designing a decision aid for the Kyrgyz prison context. Prison settings in many countries of the former Soviet Union share history, similarly organized criminal subcultures, and beliefs surrounding addiction and addiction treatment; government responses to drug use and criminal organization in prisons have also been similar in these countries (Bryuhnov et al., 2019; Latypov et al., 2014; Polonsky, Azbel, Wegman, et al., 2016; Polonsky, Azbel, Wickersham, et al., 2016; “The Global Encyclopaedia of Informality, Volume 2,” 2018). Due to these similarities, a future decision aid may be exportable to countries elsewhere in the region, increasing the uptake of the most effective infection-prevention strategy among people who inject drugs and curtailing the spread of HIV in a region where HIV incidence is increasing (Joint United Nations Programme on HIV/AIDS, 2020).
Methods
Qualitative interviews were conducted between October 2016 and September 2018 in one women’s and two men’s medium-security prisons near Bishkek, Kyrgyzstan, that had the highest prevalence of drug injection according to a biobehavioural study (Azbel et al., 2016). Methods for data collection have been previously described (Meyer et al., 2020). Briefly, individuals were invited to participate if they met the following inclusion criteria: 1) were incarcerated at one of the three stated prisons in Kyrgyzstan, 2) met DSM-V criteria for OUD, 3) had a release date within six months and 4) were 18 years of age or older.
The prison administration provided a list of all incarcerated people within six months of release and we initially called participants randomly from the list and informed them about the study. Eventually, participants were asked to refer others. Sampling was purposeful to include both methadone participants and non-participants, people with varying experiences with drug injection and incarceration, and people from multiple social statuses in the prison hierarchy. All participants provided written consent. During consent procedures, research assistants outlined the purpose of the study (to learn about how people experiencing incarceration manage choices surrounding drug injection and/or addiction treatment). Importantly, research assistants made clear that this study was not affiliated with the prison administration, that interviews would be anonymous, and that participants could withdraw from the study at any point.
Interviews were conducted both before and after release from prison. Within-prison interviews were conducted in a private room situated on the border between the incarcerated people’s living quarters and the administrative territory of the prison. Such a location was intentionally chosen to ensure maximal comfort on the part of the participants who may feel uncomfortable interfacing too closely with the prison administration (Slade & Azbel, 2020). Interviews were conducted in Russian and/or Kyrgyz, depending on the participant’s preference, and participants were given non-monetary supplies for their time (in the form, primarily, of hygienic products). Trained research assistants (including LA) conducted the interviews, which lasted, on average, 45 minutes and were audio-recorded. Interviews were transcribed, translated, and back-translated to ensure understanding (Brislin, 1970).
Interview guides were in-depth and evolved over time to include a variety of topics that emerged as relevant from previous interviews. The following topics were prominent in interviews: 1) Personal accounts of addiction management and plans for release; 2) Structures of “informal governance” (governance by incarcerated people themselves) and the function of the obshchak [word to describe both the prison hierarchy system and the lawmakers/enforcers of that system]; 3) Meaning of methadone and methadone vs. heroin injection and 4) Challenges managing drug-related risk during community re-entry.
Participants were recruited from a subsample of incarcerated people who met the above criteria and who enrolled in a study that offered methadone and post-release observation (study MATLINK). Overall, 36 people who met inclusion criteria were approached for supplemental qualitative interviews, and all consented to participate. Qualitative data were linked to a baseline structured survey that was completed 6 months before release to the community. Follow-up interviews were collected from 13 of these people immediately post-release, 5 people completed the first follow-up interviews (at 6 months), and 1 person completed the second follow-up interview (at 12 months).
Coding was initially conducted using an inductive approach to identify themes in the interview data. This thematic analysis was guided by the risk environment framework (Rhodes, 2002). The coding of these interviews is discussed in a previous paper (Meyer et al., 2020). For the present paper, the authors used thematic analysis to sub-code the data, guided by the theoretical framework put forward by Muthulingam and colleagues for assessing patient preferences about treatment for OUD (Muthulingam et al., 2019), paying close attention to factors that have been previously identified as relevant to decision aid development.
Ethical approval for the qualitative interviews was provided by the Yale University Human Investigations Committee (IRB). Yale’s review process included an incarcerated person as a representative. The study was also approved by the US Department of Health and Human Services, Office for Human Research Protections (OHRP). Ethical approval was also provided by the Committee on Bioethics under the Global Research Institute in Kyrgyz Republic and the University of Illinois at Chicago.
Results
Respondents
Table 1 provides a description of the 36 participants. Respondents were predominantly male (14 female, 22 male), ranging in age from 26 to 60, who had been PWID for between 1 and 40 years. Twenty had used methadone at some point; 15 had never used it (one respondent’s methadone use status was unknown).
Table 1.
Demographic characteristics of respondents.
| Gender | Years on methadone | Hierarchy Status | Age | Duration of current incarceration (years) | Lifetime number of incarcerations | Number of years injecting |
|---|---|---|---|---|---|---|
| Male | < 1 year | missing | 56 to 60 | 3 to 4 | 5 | 21 to 25 |
| Male | 8 | Poryadochnyi | 46 to 50 | 1 to 2 | 5 | 11 to 15 |
| Male | 2 | Obizhennyi | 36 to 40 | 1 to 2 | 4 | 11 to 15 |
| Female | 8 | N/A | 46 to 50 | 7 to 8 | 3 | 16 to 20 |
| Female | 4 | N/A | 46 to 50 | 1 to 2 | 4 | 16 to 20 |
| Female | N/A | N/A | 41 to 45 | 3 to 4 | 4 | 16 to 20 |
| Female | 4 | N/A | 46 to 50 | 5 to 6 | 4 | 16 to 20 |
| Male | < 1 year | Poryadochnyi | 31 to 35 | 3 to 4 | 1 | 11 to 15 |
| Male | 3 | Neput’ | 36 to 40 | 1 to 2 | 1 | 16 to 20 |
| Female | 2 | N/A | 31 to 35 | 3 to 4 | 5 | 1 to 5 |
| Male | N/A | Poryadochnyi | 31 to 35 | 5 to 6 | 2 | 11 to 15 |
| Female | 8 | N/A | 31 to 35 | 3 to 4 | 1 | 6 to 10 |
| Male | N/A | Neput’ | 41 to 45 | 5 to 6 | 5 | 6 to 10 |
| Male | N/A | Neput’ | 41 to 45 | 3 to 4 | > 7 | 16 to 20 |
| Male | N/A | Obizhennyi | 41 to 45 | 3 to 4 | 1 | 6 to 10 |
| Male | 3 | Neput’ | 46 to 50 | 1 to 2 | 4 | 21 to 25 |
| Male | 1 | Neput’ | 41 to 45 | 3 to 4 | 4 | 21 to 25 |
| Female | missing | N/A | 31 to 35 | 1 to 2 | 2 | 6 to 10 |
| Male | < 1 year | Obizhennyi | 51 to 55 | 3 to 4 | 4 | 31 to 35 |
| Male | N/A | Poryadochnyi | 46 to 50 | 5 to 6 | 7 | 36 to 40 |
| Female | 4 | N/A | 56 to 60 | 5 to 6 | 4 | 21 to 25 |
| Male | N/A | Obizhennyi | 26 to 30 | 5 to 6 | 4 | 1 to 5 |
| Male | N/A | Poryadochnyi | 18 to 25 | 3 to 4 | 6 | 11 to 15 |
| Female | N/A | N/A | 41 to 45 | 3 to 4 | 1 | 1 to 5 |
| Male | 5 | Poryadochnyi | 31 to 35 | 3 to 4 | 7 | 16 to 20 |
| Male | N/A | missing | 46 to 50 | 3 to 4 | 6 | missing |
| Female | N/A | N/A | 36 to 40 | 5 to 6 | 6 | 16 to 20 |
| Male | N/A | Poryadochnyi | 36 to 40 | 3 to 4 | 5 | 16 to 20 |
| Male | N/A | Poryadochnyi | 36 to 40 | 3 to 4 | 7 | 6 to 10 |
| Male | N/A | Neput’ | 56 to 60 | 1 to 2 | 4 | 1 to 5 |
| Female | 1 | N/A | 51 to 55 | 3 to 4 | 1 | 1 to 5 |
| Female | 3 | N/A | 46 to 50 | 3 to 4 | 4 | 6 to 10 |
| Male | < 1 year | Poryadochnyi | 36 to 40 | 1 to 2 | 5 | 16 to 20 |
| Female | 8 | N/A | 31 to 35 | 7 to 8 | 1 | 6 to 10 |
| Female | 4 | N/A | 36 to 40 | 3 to 4 | 7 | 11 to 15 |
| Male | N/A | Obizhennyi | 26 to 30 | 5 to 6 | 3 | 1 to 5 |
Note that women’s prisons do not participate in the hierarchy system, and therefore for female respondents, hierarchy status is listed as “Not applicable” (N/A). For those who have never used methadone, years on methadone is listed as N/A. “Missing” indicates that the data was not provided during the interview.
Themes
Responses generally fit into one of six interconnected themes (Figure 1): informal prison governance, informal prison economy, benefits of methadone treatment, side effects of methadone treatment, distrust of the formal prison administration, or desire for a “cure” for OUD.
Figure 1.
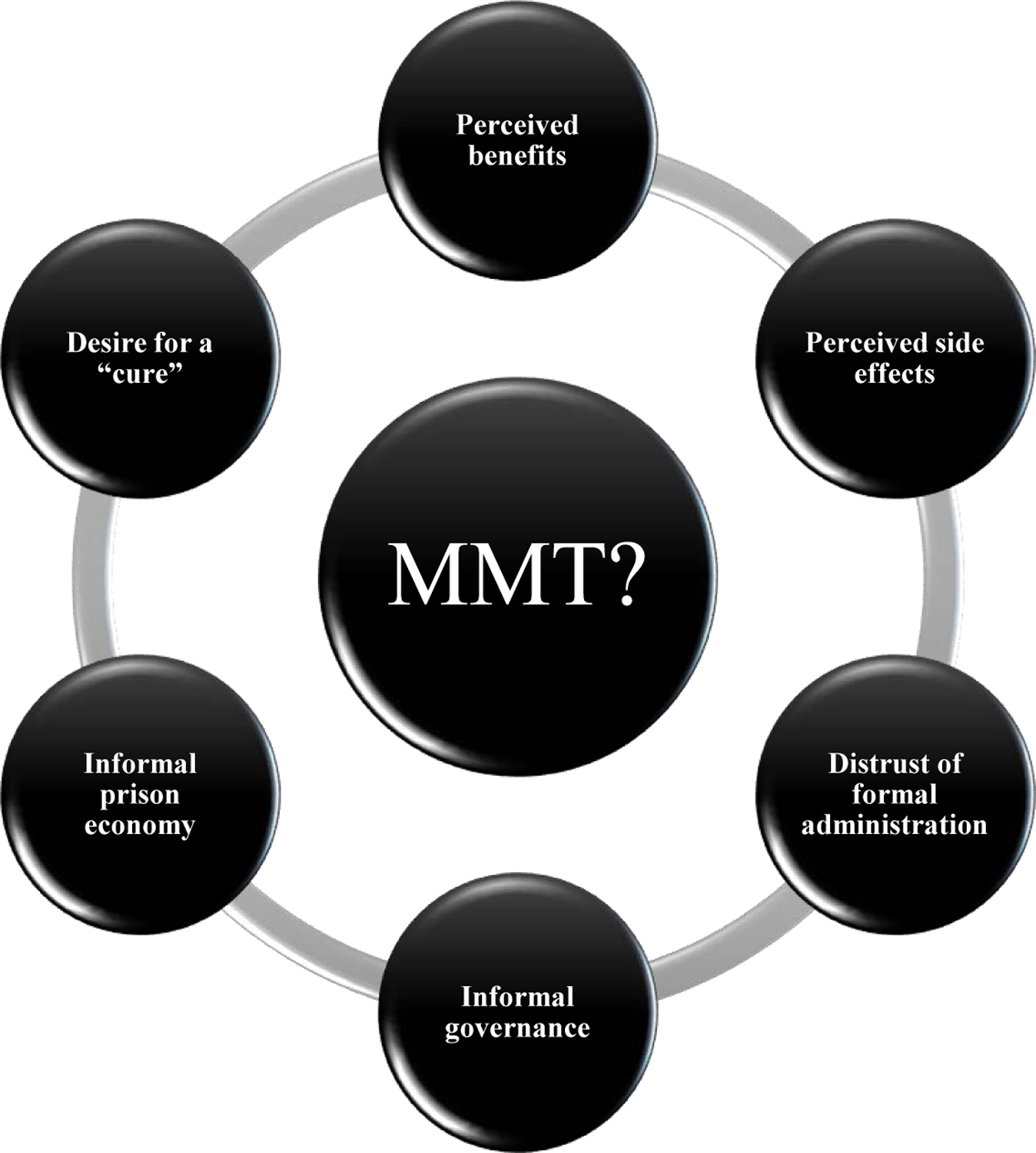
A schematic representation of the six interrelated themes identified in relation to methadone uptake among people who inject drugs in Kyrgyz prisons.
Informal Prison Governance
Men’s prisons were informally governed by the obshchak (literal translation (lit.) “common fund”) and led by the vor (lit. “thief,” member of a gang known as the “thieves-in-law”), perpetuating a strict prison hierarchy system (Figure 2). Among the general body of incarcerated people, the top of the hierarchy was made up of the poryadochnye (singular poryadochnyi), lit. “the decent ones,” followed by neputi (singular neput’), lit. “the ones who lost the way,” and finally obizhennye (singular obizhennyi), lit. “the ones who have offended.” Of the 22 male respondents in this study, 9 were poryadochnye, 6 were neputi, and 5 were obizhennye (2 had an unknown hierarchy status).
Figure 2.
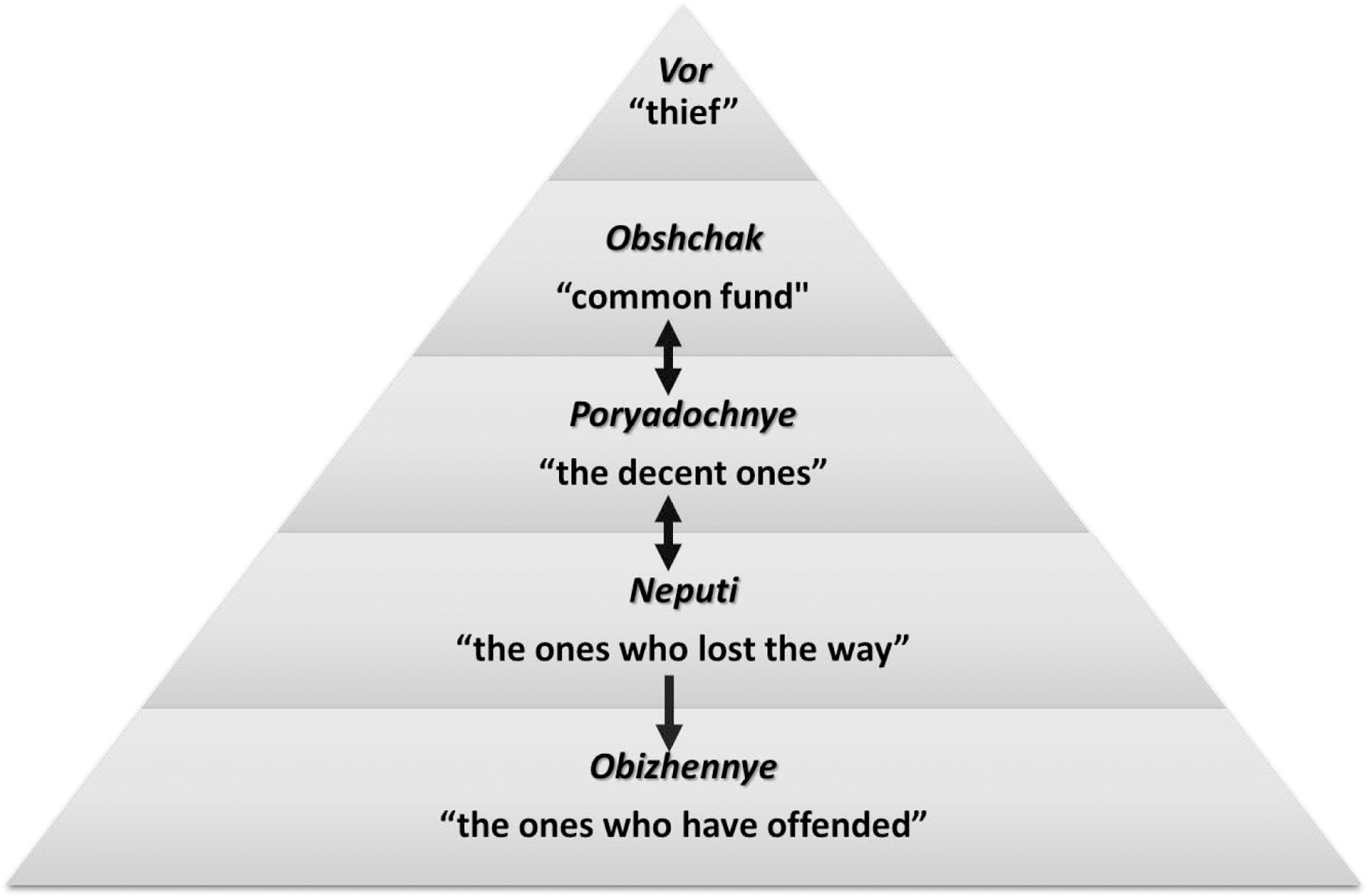
A strict prison hierarchy regulated life in men’s prisons. Both the hierarchy itself and the people who enforced it were referred to as the obshchak (lit. “common fund”). The hierarchy was governed by the vor (lit. “thief,” a member of the gang known as the “thieves-in-law”). Enforcing the vor’s wishes was the obshchak, consisting of deputies, overseers, and enforcers of the system’s strict laws. Among the rest of the prison population, the hierarchy consisted of the poryadochnye (lit. “the decent ones”), followed by the neputi (lit. “the ones who lost the way”) and obizhennye (lit. “the ones who have offended”). One could move between hierarchy classes, except for the obizhennye, who were permanently relegated to that category, often for crimes seen as especially heinous (for example, paedophilia or homosexuality). Incarcerated people in different levels of the hierarchy followed strict rules that outlined when and how they could interact.
Strict rules governed how and when different levels within the hierarchy could interact. Participation in the methadone program challenged these norms, and overseers would watch the program closely to ensure that no violations of the system occurred. In the methadone program, people were required to take methadone in order of social status: first poryadochnye, followed by neputi, and finally obizhennye. Overseers would monitor the proceedings closely to ensure that the order was followed and that people in different social classes did not drink from the same glasses (particularly poryadochnye, who were at greatest risk of losing social standing by virtue of their high position).
Provided that they could follow the obshchak’s strict rules, respondents were able to participate in the methadone program. Violation of these rules, however, risked a lowering of one’s position in the hierarchy and subsequent social ostracism. “Now it’s mainly obizhennye and neputi on methadone. There are very few poryadochnye…In Belovodsk, [one of the other prisons], really, there’s this law, those who go on methadone, they’re sent to the live with the [neputi] right away” (poryadochnyi, male, 36–40 years old, formerly on methadone). While the use of methadone itself did not necessarily result in the lowering of rank in all prisons, prison culture mandated that members of higher status avoid interaction with those lower in the hierarchy. Because of this, higher-ranked people were often reluctant to enter the methadone program at the same time or in the same place as lower-ranked clients.
Notably, this restriction was limited to those incarcerated in men’s prisons—women’s prisons did not follow this hierarchy. Instead, women’s prisons defined who were the most respected members of the prison community by age and abstaining from certain behaviours; as one respondent explained, “how do you get the status of a respected person? You have to be worthy of it, right? This means not running around, gossiping, not selling out anyone and not backstabbing, dirty. And you’ll be a respected person. Plus [that applies] not just in prison” (female, 41–45 years old, never on methadone).
Informal Prison Economy
Some respondents described heroin as a type of currency within the prison’s informal governance system. By providing methadone for free to participants, the formal administration disrupted the economic order that the obshchak had created within the prison. One respondent described that in his prison, one of the obshchak’s edicts prohibited the use of methadone. “In prisons, drugs are a currency. That’s another reason why the obshchak is against methadone. Because methadone is for free, you don’t have to work. You go there, no problem, they pour it for you, you drink it, you don’t have to do anything, while you have to work for heroin” (poryadochnyi, male, 36–40 years old, formerly on methadone).
Since heroin was one of the main forms of currency within the prison (Rhodes et al., 2019), methadone program participants were excluded from some of the social capital associated with heroin trade and distribution. Common items like tea, cigarettes, and food, which incarcerated people bartered in exchange for heroin, were out of reach for many methadone program participants. Further, methadone program participants were forced to live in separate barracks from non-participants, intensifying the social distance between them. Because of the strong social value placed on contribution to the informal prison economy, entering the methadone program would often break trust between participants and non-participants. Some non-participants reported distrust of those using methadone, although the strength of this feeling was site-dependent and varied based on individual prison culture.
Perceived Benefits of Methadone
Limiting disease spread was a common theme in responses, as was decreased death due to overdose. Respondents expressed a desire to be free from dependence on heroin and the negative health and social implications of OUD. They used methadone to limit symptoms of withdrawal and promote a healthy work and personal life. One person explained that for him, methadone was a path to a better life. “It’s a very good medication, very, I don’t know why it’s like that in Kyrgyzstan, if I were president, I would allow it in Kazakhstan and in Russia, for drug addicts it’s like a way out. Especially for those who are tired of being addicts, you get tired, very tired, the same problems, you get up in the morning, shoot up, find them, and to find them, you have to find money first, and it’s not that simple, such problems, plus the police is near, walking next to you, they take away money... Yes, methadone is for me some kind of a breather for me, it’s very good, and in all these years I’ve come to understand that if it were available sooner, I would have sooner, maybe my life would have turned out differently, if methadone were available sooner” (poryadochnyi, male, 56–60 years old, on methadone).
In contrast, people who used heroin, relative to being on methadone, were frequently described as committing crimes, especially theft. According to respondents, friends and neighbours would avoid people who used heroin. Methadone was a solution, and many respondents described methadone as a stabilizing force in their lives. As one respondent stated, “From heroin, you get sick, you walk around looking for it. All these troubles start. Police. Spending money. You’re humiliating yourself in front of people. You steal from someone… You won’t be accepted by others. People, neighbours, they’ll be avoiding you. That’ why I think it’s better to go on methadone. You get up in the morning, drink tea, go [take your] methadone and then work, you’re not sick, it’s good, normal” (poryadochnyi, male, 31–35 years old, on methadone). Methadone was frequently linked to a calmer demeanour. It was believed to improve mood and outlook on life, as well as save its recipients money.
Perceived Side Effects of Methadone
Reported side effects were numerous and severe. A common complaint was that methadone prevents the person from getting high even with the addition of heroin. “For some reason, methadone has different potencies,” one respondent explained. “...for example, a month ago, it was totally different. There was nothing like that. For the last 2–3 weeks it has been... it is not just me, you may ask anyone taking it here, just ask, everyone would say it is not potent. That’s it. It is too soft. It is hard for me to explain what I feel, my feeling, how I feel all that, but basically, it’s not potent, too soft” (poryadochnyi, male, 41–45 years old, on methadone). Methadone did not allow for one of the key benefits of heroin—euphoria. Respondents emphasised that they did not get high while using methadone and therefore were not interested in continuing treatment.
As a “synthetic” medication (as opposed to heroin, which is plant-derived and therefore considered more “natural” (Rozanova et al., 2018)), methadone was believed to cause everything from bone aches, to liver burns, to turning one’s internal organs into “goo.” One respondent described participants in the methadone program at her prison, saying, “Well, people see, they know, hear about how this ends, how these women suffer, they can’t for half an hour, an hour in the toilet for number one, their whole internal organs system gets messed up, and people draw conclusions for themselves” (female, 41–45 years old, never on methadone). There was also a common belief that methadone is more addictive than heroin and leads to worse withdrawal symptoms. This perception discouraged respondents from initiating methadone, since they were often seeking recovery from OUD, which they perceived as not taking any opioids at all (Azbel et al., 2017).
Some respondents were afraid that methadone would kill them. One respondent reported that “everyone died who started taking methadone, everyone whom I knew. Those who joined the methadone program. One guy gave it up and died, the other started taking it occasionally and died as well right here” (obizhennyi, male, 51–55 years old, formerly on methadone). Similarly, another described, “I just see that with this methadone method, they just start dying. Well at first, of course it’s good, it’s all going well, like clockwork, he’s blooming and thriving, but one fine day, he just drops dead, a corpse” (obizhennyi, male, 41–45 years old, never on methadone). Importantly, many people entered the in-prison methadone program while seeking treatment for other health conditions, like tuberculosis, that would sometimes prove fatal.
To potentiate the effects of methadone and get high, methadone program participants would frequently combine their methadone with another illegal medication, Dimedrol (diphenhydramine, an antihistamine) (Meyer et al., 2020). Dimedrol potentiates soporific effects of methadone and was easily available in the prisons, often provided by the prison guards or medical staff themselves. However, Dimedrol use was forbidden by the obshchak, a provision indicative of a deep conflict between the formal prison administration and the informal prison governance. To those not taking methadone, the combined effects of methadone and Dimedrol made methadone program participants look like zombies, slaves, or lifeless individuals without autonomy. As one respondent described, “Well, I don’t know, just looking at [people who take methadone], how they’re killing themselves, I don’t feel like it, I still feel like living…Well, I don’t know, before, they are walking around like zombies [due to methadone and] Dimedrol” (poryadochnyi, male, 36–40 years old, never on methadone). Dimedrol use was often seen as intrinsic to methadone program participation, and the obshchak used this fallacy to demonize methadone. As one respondent described, “When they looked from the side of the obshchak, aha, those on methadone basically don’t want to work, they pour methadone, what else do they need, aha, they follow up with Dimedrol” (poryadochnyi, male, 36–40 years old, on methadone).
Distrust of Formal Administration
Concerns about the methadone program were punctuated by a deep and abiding distrust of prison administration. Doctors were considered agents of the state who therefore failed to look out for the best interests of the incarcerated people. Respondents often feared that methadone would lead the person on treatment to become overly dependent on these doctors. When asked what the purpose of the methadone program was, one respondent explained that it was a plot run by the doctors. “To kill, as simply as that, kill all the drug addicts, robbers and murderers (laughter). That’s what I think basically, because many countries refused methadone, many countries. There’s only our Kyrgyzstan left, we have many drug addicts” (obizhennyi, male, 41–45 years old, never on methadone). The belief that methadone leads to death was a common one, as was the description of doctors as fundamentally untrustworthy.
Overall, the prison administration, including its medical staff, was considered unreliable and unable to provide for the basic needs of incarcerated people. As one respondent explained, “conflicts happen because of something between the administration and the obshchak, it’s mainly [Essentials or necessities that the administration is required to provide for incarcerated people]. They can’t give us our essentials. Even, even a jacket, shoes, rations, bread, sugar, oil… toothbrushes, soap for washing… they can’t… soap for washing for the fourth month, we can’t take soap. We can’t take household soap. They can’t give us. There” (poryadochnyi, male, 31–35 years old, on methadone). Given the formal prison administration’s frequent inability to provide even essential goods, methadone program participants feared that the supply of methadone might be interrupted or costs might increase and the prison would stop providing the service.
Desire for a “Cure”
Many respondents, especially those planning to be released soon, wished to taper off methadone over time. They believed that once they were no longer using methadone, their addiction would be “cured” and they would be “normal.” Taking methadone meant that one was still an addict. As one participant reported, “I would like to give up methadone, use nothing at all. I would go to church, pray, for example, I have such desire. I want to get out, get my passport, find a job, go to church, repent, become a believer, change my life completely. I want that. I would like to find a man, get married, have a normal life. Even though I would not have children, I would adopt someone. I want a normal life, for at least 10–15 years” (female, 36–40 years old, on methadone).
Social factors played heavily into the desire to cease opioid use. “Well, after all, I’m not alone in the world. I’m not descended from an ape. I have parents, relatives. They don’t know about this. Even how… the parents, fine, my parents would understand, right. Friends, parents, they’ll understand. How would they look at you, even relationships, right, my parents could even lose, right, relationships with people they know. ‘Oh, their son is a drug addict.’ Well, each has his [issues] …In general, right, I want to change something in my life. Before it’s too late. To get released, to find a job. Well, to start afresh, right. To try, right, to start things afresh...Well, basically I don’t even really want to [take methadone] after my release” (obizhennyi, male, 31–35 years old, on methadone).
Respondents expressed confusion and dismay when doctors disregarded their wishes to stop methadone. As one respondent reported, “[My dose] is too much for me, too much. Because when methadone was good, as I said, 120 [mg]... it was 130. It was too much; I should not have. I asked her repeatedly: ‘Please, taper my dose.’ And she used to say: ‘You raise it as you please, and then taper it.’ And I said: ‘That was in the past, when I wanted to raise the dose. Now I have no desire to raise it, now I would like to... taper it a bit.’ ‘You should think it over, because you will come back later and ask me to raise it once again.’ ‘No, I would not. I swear, really, why don’t you believe me? I would not ask you again’” (poryadochnyi, male, 31–35 years old, on methadone). In the prisons studied, methadone program participants were required to provide regular urine samples, and any samples found to contain illicit drugs led to an increase of the participant’s methadone dose, regardless of the participant’s wishes. However, many methadone program participants expressed frustration that their doses were being increased, because they believed that doctors were denying them the opportunity for a “normal” life.
Discussion
To inform development of a decision aid in Kyrgyz prisons, we have performed a secondary analysis of thematically coded interview data from three Kyrgyz prisons to identify factors that may influence methadone uptake in prisons. We identified six themes: (1) informal prison governance, (2) informal prison economy, (3) perceived benefits of methadone treatment, (4) perceived side effects of methadone treatment, (5) distrust of formal prison administration, and (6) desire for a “cure” from addiction (Figure 1). While these six themes are distinct in terms of their relationship to methadone uptake, they are deeply interconnected. For example, the informal prison economy relies on the obshchak to facilitate transactions between parties and reinforce the use of heroin as a currency. Similarly, a deep distrust of formal administration permeated descriptions of methadone’s side effects, since some respondents believed that methadone was part of a state plot to kill PWID.
Previous studies have demonstrated a need for deeper understanding of the relationship between informal (led by incarcerated people) and formal (led by prison administration) systems of prison governance in designing a within-prison methadone program in EECA (Altice et al., 2016; Azbel et al., 2017; Rozanova et al., 2018). This study incorporates interviews from sources within the “red” zones (governed by formal administration) and “black” zones (governed by the obshchak) of the Kyrgyz prisons participating in this study. Additionally, this study uses a framework based on IDM, the idea that with decision aids, physicians and patients can work together to find the best treatment for a given patient, increasing patient satisfaction and obtaining better health outcomes (Stacey et al., 2017). This study builds upon ongoing work in the US to develop decision aids for OUD (Mooney et al., 2020; Muthulingam et al., 2019). Additionally, previous US- and Malaysia-based studies have suggested a need for decision aids and informed decision making with PWID experiencing incarceration (Banta-Green et al., 2020; Mukherjee et al., 2016). To our knowledge, however, this is the first such study to inform decision aids in the EECA context.
Unpacking the relationships between the obshchak and the formal prison administration in Kyrgyzstan is crucial to addressing methadone uptake and, by extension, to influencing the HIV risk environment in Kyrgyz prisons. Because methadone is currently provided by the formal prison administration, it is at odds with the obshchak. Methadone program participants are far less likely than non-participants to work for the obshchak in exchange for heroin, disrupting the informal prison economy. Additionally, many respondents expressed fear that methadone was part of a state-based plot to kill people with substance use disorders. We strongly suggest incorporating an understanding of these formal administration vs. obshchak dynamics into any future decision aid tool, especially since methadone uptake can lead to social ostracism for incarcerated people believed to be collaborating with the formal prison administration. Critically, any decision aid tool should be available both within and outside of the prison’s “red” zones. If available within the “black” zones of the prison as well, this decision aid may be less likely to be perceived as a strategy of the state. Additionally, members of different hierarchy levels live in different areas of the prison. Providing different methadone distribution locations in barracks occupied by each hierarchy level could alleviate some of the logistical difficulties of providing methadone to people in different levels of the hierarchy. Additionally, bringing methadone distribution to “black” regions could alleviate the perception of methadone as a tool of the state. However, until methadone becomes part of the informal prison economy in a manner akin to the present obshchak-run heroin distribution system, this intervention may have limited effectiveness.
In the Kyrgyz prison context, a potential methadone program participant’s hierarchy status (Figure 2) should be a key factor in the decision-making algorithm. A person’s standing in the hierarchy will determine the logistics of taking methadone. For example, neputi will usually receive methadone after poryadochnye, and they will take from different cups. More importantly, one’s hierarchical standing will determine the potential consequences of entering a methadone program. Poryadochnye entering methadone treatment risk social isolation and violence for violating the obshchak’s rules at some prisons. Obizhennye, who are at the lowest position on the hierarchy, risk far less in terms of violating social norms. Particularly in “black” prisons, a regular supply of heroin is available to poryadochnye and others willing to work for the obshchak. Given that Kyrgyzstan provides needle/syringe exchange programs (NSP) within prisons, a decision aid could potentially present continued heroin use with safe injection practices (Ferri et al., 2006; Stöver & Hariga, 2016; Uchtenhagen, 2011) as a feasible alternative to methadone for harm reduction among PWID.
While the obshchak is an important decision-making factor for methadone uptake in men’s prisons, this same system does not exist in the women’s prison. For context, there is only one women’s prison in Kyrgyzstan, and women represent 4.2% of the national prison population (“World Prison Brief: Kyrgyzstan,” 2019). The hierarchy in the women’s prison is much less regimented than in the men’s prisons. For example, a woman might have lower social status because she steals from other incarcerated people, has personal hygiene issues, or is an informant to the formal prison administration. Given the lack of the obshchak in the women’s prison, heroin is less widely available there relative to men’s prisons. This may explain why a previous study has found that within-prison drug injection is significantly less prevalent among women (Azbel et al., 2018). Previous research has also suggested that because heroin is less widely available in the women’s prison, methadone is more socially acceptable (Meyer et al., 2020). Ten of the 14 female participants in this study had used methadone, compared to 10 of 22 male participants (Table 1); however, female respondents expressed the same health-related beliefs and negative attitudes about methadone as the male participants.
Therefore, in addition to providing information localised to one’s hierarchy standing for incarcerated men, an EECA decision aid should address methadone-related beliefs specific to this context, many of which are not supported by clinical literature. These include many different ideas about physical side effects of the medication. Methadone has been associated with some of the more mild side effects described, including constipation, fatigue, nausea, weight loss, and itchy skin (Haber et al., 2017). Constipation is a common side effect of methadone use; however, respondents often perceived this side effect as an indication that methadone rendered internal organs dysfunctional. Other mild side effects (such as problems with urination), as well as the most severe side effects described (massive disruption to internal organs, death) have not been reported in clinical trials; a decision aid could help dispel some of the myths about side effects of methadone.
Several respondents reported that people they knew who joined the methadone program died. Though some methadone program participants did die, the high prevalence of HIV, tuberculosis and other co-morbidities is high and it is unclear that the respondents connected death from methadone to a comorbidity. Notably, many people who enter the methadone program do so upon connecting to the healthcare system for another reason, such as a tuberculosis diagnosis. Thus, comorbidities and underlying infections appear frequently among people in the methadone program (Altice et al., 2016), creating a perception among the wider prison community that methadone causes sickness and death. A decision aid would play a key role in educating the prison population on the likelihood of sickness, death, or any given side effect as well as reasonable health benefits to expect from participating in a methadone program. Additionally, in the EECA prison context, methadone is often combined with other substances, particularly Dimedrol (Meyer et al., 2020), so side effects listed should include information about effects of combining methadone with other substances.
The most immediate future use of study results is to guide the content and design of a context-specific decision aid to help incarcerated people choose whether to enter an in-prison methadone treatment program. Decision aids, which may exist as phone apps, brochures, training sessions, or other content-delivery mechanisms, consist of three central components: (1) information, (2) deliberation, and (3) implementation/delivery/execution of the decision. Given that many respondents expressed a desire to taper their methadone prior to release, information on the chronic, relapsing nature of OUD will be a critical component of a future decision aid. Participants reported that leaving methadone was part of their trajectory toward a “normal” life. Therefore, a decision aid should emphasise that prior methadone program participants have found that methadone promoted social relationships and decreased criminality in their lives, as reported by previous studies (Gourlay et al., 2005; Marsch, 1998). Moreover, in the absence of methadone, relapse to illicit opioid use is common, occurs soon after release, and is associated with poor linkage and retention in care for other comorbid conditions (e.g., HIV) (Loeliger, Altice, Ciarleglio, et al., 2018; Loeliger, Altice, Desai, et al., 2018; Loeliger, Meyer, et al., 2018; Merrall et al., 2010). Clinical providers should be careful to explain that methadone is not a short-term therapy or cure for OUD, but rather a component of a long-term treatment plan for a chronic relapsing condition.
This decision aid could be created using choice-based conjoint analysis, a strategy to help people make complex decisions by weighing multiple factors (Bridges et al., 2011). Incarcerated people could theoretically be using methadone alone, methadone in combination with Dimedrol, heroin alone, or a combination of methadone and heroin, with or without Dimedrol. Conjoint analysis starts by breaking a potential treatment option into attributes: for example, effects on hierarchy status, need for heroin for economic reasons, importance of being high, effects on social relationships both within and outside of prison, etc. By comparing profiles with different combinations of attributes in a series of questions, conjoint analysis can determine which option will likely match best with an individual’s priorities. In this context, such a strategy could allow incarcerated people to evaluate factors named here (i.e., a desire for a “normal” life, hierarchy status, potential side effects, etc.) to determine whether methadone (or heroin from the obshchak) is a good option for them.
While this work informs elements to be considered in a decision aid for incarcerated people in this context, some other important considerations would include risks and benefits of methadone relative to injecting opioids within prison. For example, risks of overdose or transmission of HIV or HCV would be weighed against potential demotion within the prison hierarchy. Additionally, a decision aid must consider continuity issues after release from prison, considering the extraordinary risks present during this transition. Findings in this study also suggest modifications that the prison might consider in terms of methadone delivery, including in program location (i.e., Is methadone distribution located in a “red” zone or “black” zone? Do obizhennye and poryadochnye receive methadone from the same location, and if so, do the groups use the same cups/pens/serving hatch?). Other factors to consider in methadone distribution include involvement of the obshchak and Dimedrol availability.
This future decision aid may be translatable to locations outside of Kyrgyzstan. Informal prison governance has been described in many countries of the former Soviet Union (“The Global Encyclopaedia of Informality, Volume 2,” 2018). Systems of self-governance within prisons have also been described in other countries throughout the world, such as in Northern Ireland and Brazil (Butler et al., 2020). Additionally, many of the negative attitudes and concerns that participants in this study expressed about methadone have already been observed in multiple international settings. One systematic review found that myths about methadone’s negative health effects exist in the United States, Australia, China, Canada, Ukraine, the United Kingdom, Malaysia, Iran, and Switzerland, just to name a few (Cioe et al., 2020). A Canadian study using qualitative interviews found that methadone patients were seen as incompetent, untrustworthy “junkies” who were using methadone to get high (Woo et al., 2017)—all stereotypes very similar to those described by study respondents in Kyrgyzstan. Researchers in China found that many community members believed that methadone was a way for “addicts” to get high, and most believed that methadone patients had undesirable social characteristics (Deng et al., 2020). Given the prevalence of myths and stigma surrounding methadone, as well as the existence of informal prison governance in diverse international prison contexts, findings from this study may be applicable to within-prison decision aids in a variety of countries.
Limitations of this study include that the interviews focused on injection-related HIV risk and methadone access within prison and after release; they did not delve deeply into sociocultural and structural barriers to care. Additionally, since this was a secondary analysis of data, the original interviews did not ask questions specific to decision aid development. Finally, the implementation of a decision aid in this context will likely change the environment studied, potentially rendering some of these conclusions no longer true.
Eventually, this research and a subsequent decision aid may help inform future interventions in the area, as well as suggest changes to current methadone program implementation.
Funding
This work was supported by the National Institute of Drug Abuse (R21 DA042702, Meyer; R01 DA029910, Altice), the National Institute for Mental Health (T32 MH020031, Bromberg), and the Fogarty International Center (D43 TW010540, Bromberg).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing Interests Statement
The authors declare that they have no competing interests. They do not have any direct or indirect connections with the alcohol, gambling, tobacco, or pharmaceutical industries.
Have you obtained ethical approval for the conduct of your study?
Yes.
Sources
- Altice FL, Azbel L, Stone J, Brooks-Pollock E, Smyrnov P, Dvoriak S, Taxman FS, El-Bassel N, Martin NK, Booth R, Stöver H, Dolan K, & Vickerman P (2016). The perfect storm: incarceration and the high-risk environment perpetuating transmission of HIV, hepatitis C virus, and tuberculosis in Eastern Europe and Central Asia. In The Lancet (Vol. 388, Issue 10050, pp. 1228–1248). Lancet Publishing Group. 10.1016/S0140-6736(16)30856-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azbel L, Polonsky M, Wegman M, Shumskaya N, Kurmanalieva A, Asanov A, Wickersham JA, Dvoriak S, & Altice FL (2016). Intersecting epidemics of HIV, HCV, and syphilis among soon-to-be released prisoners in Kyrgyzstan: Implications for prevention and treatment. International Journal of Drug Policy, 37, 9–20. 10.1016/j.drugpo.2016.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azbel L, Rozanova J, Michels I, Altice FL, & Stöver H (2017). A qualitative assessment of an abstinence-oriented therapeutic community for prisoners with substance use disorders in Kyrgyzstan. Harm Reduction Journal, 14(1), 1–9. 10.1186/s12954-017-0168-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azbel L, Wegman MP, Polonsky M, Bachireddy C, Meyer J, Shumskaya N, Kurmanalieva A, Dvoryak S, & Altice FL (2018). Drug injection within prison in Kyrgyzstan: elevated HIV risk and implications for scaling up opioid agonist treatments. International Journal of Prisoner Health, 14(3), 175–187. 10.1108/IJPH-03-2017-0016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banta-Green CJ, Williams JR, Sears JM, Floyd AS, Tsui JI, & Hoeft TJ (2020). Impact of a jail-based treatment decision-making intervention on post-release initiation of medications for opioid use disorder. Drug and Alcohol Dependence, 207. 10.1016/j.drugalcdep.2019.107799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridges JFP, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, Johnson FR, & Mauskopf J (2011). Conjoint analysis applications in health - A checklist: A report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value in Health, 14(4), 403–413. 10.1016/j.jval.2010.11.013 [DOI] [PubMed] [Google Scholar]
- Brislin RW (1970). Back-translation for cross-cultural research. Journal of Cross-Cultural Psychology, 1(3), 185–216. 10.1177/135910457000100301 [DOI] [Google Scholar]
- Bryuhnov AA, Kutyakin SA, & Napkhanenko IP (2019). Historical and criminological analysis of the state of opposition to thieves in law and criminal authorities in prisons in the late 80s-early 90s of the XX century. Философия Права, 2(89). https://cyberleninka.ru/article/n/istoriko-kriminologicheskiy-analiz-sostoyaniya-protivodeystviya-voram-v-zakone-i-kriminalnym-avtoritetam-v-mestah-lisheniya-svobody-v/viewer [Google Scholar]
- Butler M, Slade G, & Dias CN (2020). Self-governing prisons: Prison gangs in an international perspective. Trends in Organized Crime, 1–16. 10.1007/s12117-018-9338-7 [DOI] [Google Scholar]
- Cioe K, Biondi BE, Easly R, Simard A, Zheng X, & Springer SA (2020). A systematic review of patients’ and providers’ perspectives of medications for treatment of opioid use disorder. Journal of Substance Abuse Treatment, 119. 10.1016/j.jsat.2020.108146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culbert GJ, Waluyo A, Iriyanti M, Muchransyah AP, Kamarulzaman A, & Altice FL (2015). Within-prison drug injection among HIV-infected male prisoners in Indonesia: A highly constrained choice. Drug and Alcohol Dependence, 149, 71–79. 10.1016/j.drugalcdep.2015.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Charlson F, Ferrari A, Santomauro D, Erskine H, Mantilla-Herrara A, Whiteford H, Leung J, Naghavi M, Griswold M, Rehm J, Hall W, Sartorius B, Scott J, Vollset SE, Knudsen AK, Haro JM, Patton G, Kopec J, … Vos T (2018). The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet Psychiatry, 5(12), 987–1012. 10.1016/S2215-0366(18)30337-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Grebely J, Stone J, Hickman M, Vickerman P, Marshall BDL, Bruneau J, Altice FL, Henderson G, Rahimi-Movaghar A, & Larney S (2019). Global patterns of opioid use and dependence: harms to populations, interventions, and future action. In The Lancet (Vol. 394, Issue 10208, pp. 1560–1579). Lancet Publishing Group. 10.1016/S0140-6736(19)32229-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P, Stone J, Cunningham EB, Trickey A, Dumchev K, Lynskey M, Griffiths P, Mattick RP, Hickman M, & Larney S (2017). Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. The Lancet Global Health, 5(12), e1192–e1207. 10.1016/S2214-109X(17)30375-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng Q, Hu M, Yu F, Liu Q, Hao W, Wu Q, & Luo T (2020). A Community-Based Investigation of Stigma Toward Individuals Receiving Methadone Maintenance Treatment in China: A Randomized Case Vignette Study. Frontiers in Psychiatry, 11, 601266. 10.3389/fpsyt.2020.601266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan K, Wirtz AL, Moazen B, Ndeffo-mbah M, Galvani A, Kinner SA, Courtney R, McKee M, Amon JJ, Maher L, Hellard M, Beyrer C, & Altice FL (2016). Global burden of HIV, viral hepatitis, and tuberculosis in prisoners and detainees. Lancet, 388(10049), 1089–1102. 10.1016/S0140-6736(16)30466-4 [DOI] [PubMed] [Google Scholar]
- Ferri M, Davoli M, & Perucci CA (2006). Heroin maintenance treatment for chronic heroin-dependent individuals: A Cochrane systematic review of effectiveness. Journal of Substance Abuse Treatment, 30(1), 63–72. 10.1016/j.jsat.2005.09.003 [DOI] [PubMed] [Google Scholar]
- Gourlay J, Ricciardelli L, & Ridge D (2005). Users’ experiences of heroin and methadone treatment. Substance Use and Misuse, 40(12), 1875–1882. 10.1080/10826080500259497 [DOI] [PubMed] [Google Scholar]
- Haber PS, Elsayed M, Espinoza D, Lintzeris N, Veillard AS, & Hallinan R (2017). Constipation and other common symptoms reported by women and men in methadone and buprenorphine maintenance treatment. Drug and Alcohol Dependence, 181, 132–139. 10.1016/j.drugalcdep.2017.09.024 [DOI] [PubMed] [Google Scholar]
- Harm Reduction International. (2019). Global State of Harm Reduction: 2019 updates | Harm Reduction International. https://www.hri.global/global-state-of-harm-reduction-2019 [Google Scholar]
- Hedegaard H, Miniño AM, & Warner M (2020). Drug Overdose Deaths in the United States, 1999–2018. NCHS Data Brief, 356, 1–8. https://www.cdc.gov/nchs/data/databriefs/db273_table.pdf#1. [PubMed] [Google Scholar]
- Heimer R (2018). The Policy-Driven HIV Epidemic Among Opioid Users in the Russian Federation. In Current HIV/AIDS Reports (Vol. 15, Issue 3, pp. 259–265). Current Medicine Group LLC 1. 10.1007/s11904-018-0395-y [DOI] [PubMed] [Google Scholar]
- International Harm Reduction Association. (2008). The Global State of Harm Reduction 2008. https://www.hri.global/files/2010/06/16/GSHRFullReport1.pdf
- Izenberg JM, Bachireddy C, Wickersham JA, Soule M, Kiriazova T, Dvoriak S, & Altice FL (2014). Within-prison drug injection among HIV-infected Ukrainian prisoners: Prevalence and correlates of an extremely high-risk behaviour. International Journal of Drug Policy, 25(5), 845–852. 10.1016/j.drugpo.2014.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. (2020). UNAIDS Data 2020. Programme on HIV/AIDS. https://www.unaids.org/en/resources/documents/2020/unaids-data [PubMed]
- Kamarulzaman A, Reid SE, Schwitters A, Wiessing L, El-Bassel N, Dolan K, Moazen B, Wirtz AL, Verster A, & Altice FL (2016). Prevention of transmission of HIV, hepatitis B virus, hepatitis C virus, and tuberculosis in prisoners. Lancet, 388(10049), 1115–1126. 10.1016/S0140-6736(16)30769-3 [DOI] [PubMed] [Google Scholar]
- Kampman K, Comer S, Cunningham C, Fishman MJ, Gordon A, Langleben D, Nordstrom B, Oslin D, Woody G, Wright T, & Wyatt S (2015). The ASAM National Practice Guidelines For the Use of Medications in the Treatment of Addiction Involving Opioid Use. The ASAM National Practice Guideline, 40. https://www.asam.org/docs/default-source/practice-support/guidelines-and-consensus-docs/asam-national-practice-guideline-supplement.pdf?sfvrsn=96df6fc2_24 [Google Scholar]
- Latypov A, Grund JP, El-Bassel N, Platt L, Stöver H, & Strathdee S (2014). Illicit drugs in Central Asia: What we know, what we don’t know, and what we need to know. In International Journal of Drug Policy (Vol. 25, Issue 6, pp. 1155–1162). Elsevier. 10.1016/j.drugpo.2014.09.015 [DOI] [PubMed] [Google Scholar]
- Loeliger KB, Altice FL, Ciarleglio MM, Rich KM, Chandra DK, Gallagher C, Desai MM, & Meyer JP (2018). All-cause mortality among people with HIV released from an integrated system of jails and prisons in Connecticut, USA, 2007–14: a retrospective observational cohort study. The Lancet HIV, 5(11), e617–e628. 10.1016/S2352-3018(18)30175-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeliger KB, Altice FL, Desai MM, Ciarleglio MM, Gallagher C, & Meyer JP (2018). Predictors of linkage to HIV care and viral suppression after release from jails and prisons: a retrospective cohort study. The Lancet HIV, 5(2), e96–e106. 10.1016/S2352-3018(17)30209-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeliger KB, Meyer JP, Desai MM, Ciarleglio MM, Gallagher C, & Altice FL (2018). Retention in HIV care during the 3 years following release from incarceration: A cohort study. PLoS Medicine, 15(10). 10.1371/journal.pmed.1002667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsch LA (1998). The efficacy of methadone maintenance interventions in reducing illicit opiate use, HIV risk behavior and criminality: A meta-analysis. Addiction, 93(4), 515–532. 10.1046/j.1360-0443.1998.9345157.x [DOI] [PubMed] [Google Scholar]
- Merrall ELC, Kariminia A, Binswanger IA, Hobbs MS, Farrell M, Marsden J, Hutchinson SJ, & Bird SM (2010). Meta-analysis of drug-related deaths soon after release from prison. In Addiction (Vol. 105, Issue 9, pp. 1545–1554). Blackwell Publishing Ltd. 10.1111/j.1360-0443.2010.02990.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer JP, Culbert GJ, Azbel L, Bachireddy C, Kurmanalieva A, Rhodes T, & Altice FL (2020). A qualitative study of diphenhydramine injection in Kyrgyz prisons and implications for harm reduction. Harm Reduction Journal, 17(1), 1–9. 10.1186/s12954-020-00435-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney LJ, Valdez J, Cousins SJ, Yoo C, Zhu Y, & Hser YI (2020). Patient decision aid for medication treatment for opioid use disorder (PtDA-MOUD): Rationale, methodology, and preliminary results. Journal of Substance Abuse Treatment, 108, 115–122. 10.1016/j.jsat.2019.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherjee TI, Wickersham JA, Desai MM, Pillai V, Kamarulzaman A, & Altice FL (2016). Factors associated with interest in receiving prison-based methadone maintenance therapy in Malaysia. Drug and Alcohol Dependence, 164, 120–127. 10.1016/j.drugalcdep.2016.04.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthulingam D, Bia J, Madden LM, Farnum SO, Barry DT, & Altice FL (2019). Using nominal group technique to identify barriers, facilitators, and preferences among patients seeking treatment for opioid use disorder: A needs assessment for decision making support. Journal of Substance Abuse Treatment, 100, 18–28. 10.1016/j.jsat.2019.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polonsky M, Azbel L, Wegman MP, Izenberg JM, Bachireddy C, Wickersham JA, Dvoriak S, & Altice FL (2016). Pre-incarceration police harassment, drug addiction and HIV risk behaviours among prisoners in Kyrgyzstan and Azerbaijan: Results from a nationally representative cross-sectional study. Journal of the International AIDS Society, 19, 20880. 10.7448/IAS.19.4.20880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polonsky M, Azbel L, Wickersham JA, Marcus R, Doltu S, Grishaev E, Dvoryak S, & Altice FL (2016). Accessing methadone within Moldovan prisons: Prejudice and myths amplified by peers. International Journal of Drug Policy, 29, 91–95. 10.1016/j.drugpo.2015.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, & Shield KD (2019). Global Burden of Disease and the Impact of Mental and Addictive Disorders. In Current Psychiatry Reports (Vol. 21, Issue 2). 10.1007/s11920-019-0997-0 [DOI] [PubMed] [Google Scholar]
- Rhodes T (2002). The ‘risk environment’: a framework for understanding and reducing drug-related harm. International Journal of Drug Policy, 13(2), 85–94. [Google Scholar]
- Rhodes T, Azbel L, Lancaster K, & Meyer J (2019). The becoming-methadone-body: on the onto-politics of health intervention translations. Sociology of Health & Illness, 0(0), 1618–1636. 10.1111/1467-9566.12978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozanova J, Morozova O, Azbel L, Bachireddy C, Izenberg JM, Kiriazova T, Dvoryak S, & Altice FL (2018). Perceptions of Health-Related Community Reentry Challenges among Incarcerated Drug Users in Azerbaijan, Kyrgyzstan, and Ukraine. Journal of Urban Health, 95(4), 508–522. 10.1007/s11524-018-0256-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade G, & Azbel L (2020). Managing drugs in the prisoner society: heroin and social order in Kyrgyzstan’s prisons. Punishment and Society, 146247452095628. 10.1177/1462474520956280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL, Eden KB, Holmes-Rovner M, Llewellyn-Thomas H, Lyddiatt A, Thomson R, & Trevena L (2017). Decision aids for people facing health treatment or screening decisions. In Cochrane Database of Systematic Reviews (Vol. 2017, Issue 4). John Wiley and Sons Ltd. 10.1002/14651858.CD001431.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stöver H, & Hariga F (2016). Prison-based needle and syringe programmes (PNSP) – Still highly controversial after all these years. Drugs: Education, Prevention and Policy, 23(2), 103–112. 10.3109/09687637.2016.1148117 [DOI] [Google Scholar]
- The Global Encyclopaedia of Informality, Volume 2. (2018). In Ledeneva A (Ed.), The Global Encyclopaedia of Informality, Volume 1. 10.14324/111.9781911307907 [DOI] [Google Scholar]
- Uchtenhagen AA (2011). Heroin maintenance treatment: From idea to research to practice. Drug and Alcohol Review, 30(2), 130–137. 10.1111/j.1465-3362.2010.00266.x [DOI] [PubMed] [Google Scholar]
- Woo J, Bhalerao A, Bawor M, Bhatt M, Dennis B, Mouravska N, Zielinski L, & Samaan Z (2017). “Dont judge a book by its cover”: A qualitative study of methadone patients’ experiences of stigma. Substance Abuse: Research and Treatment, 11, 1178221816685087. 10.1177/1178221816685087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Prison Brief: Kyrgyzstan. (2019). In Institute for Crime & Justice Policy Research. https://www.prisonstudies.org/country/kyrgyzstan


