Abstract
Background/Objectives:
To compare surgical outcomes between vulnerable nursing home (NH) residents and matched community-dwelling older adults undergoing surgery for bladder and bowel dysfunction.
Design:
Retrospective cohort study.
Participants:
A total of 55,389 NH residents and propensity matched (based on procedure, age, sex, race, comorbidity, and year) community-dwelling older adults undergoing surgery for bladder and bowel dysfunction [female pelvic surgery, transurethral resection of the prostate, suprapubic tube placement, hemorrhoid surgery, rectal prolapse surgery]. Individuals were identified using Medicare claims and the Minimum Data Set (MDS) for NH residents between 2014–2016.
Measurements:
Thirty-day complications, 1-year mortality, and weighted changes in healthcare resource utilization (hospital admissions, emergency room visits, office visits) in the year before and after surgery.
Results:
NH residents demonstrated statistically significant increased risk of 30-day complications [60.1% v. 47.2%; RR 1.3 (95% CI 1.3–1.3)] and 1-year mortality [28.9% vs 21.3%; RR 1.4 (95% CI 1.3–1.4)], compared to community-dwelling older adults. NH residents also demonstrated decreased healthcare resource utilization, compared to community-dwelling older adults, changing from 3.9 to 1.9 (vs.1.1 to 1.0) hospital admissions, 11 to 10.1 (vs. 9 to 9.7) office visits, and 3.4 to 2.2 (vs. 1.9 to 1.9) emergency room visits from the year before to after surgery.
Conclusion:
Despite matching on several important clinical characteristics, NH residents demonstrated increased rates of 30-day complications and 1-year mortality after surgery for bowel and bladder dysfunction, while demonstrating decreased healthcare resource utilization. These mixed findings suggest that outcomes may be more varied among vulnerable older adults and warrant further investigation.
Introduction
Bladder and bowel dysfunction, defined herein as urinary retention, female pelvic floor disorders [i.e., urinary incontinence and pelvic organ prolapse (POP)], rectal prolapse, and hemorrhoids, are common conditions in older men and women that greatly negatively impact health related quality of life (HRQOL). These problems can be extremely life altering, resulting in loss of dignity, and potentially leading to skin breakdown, falls, other injuries and morbidity.1 Further, these conditions can be so intolerable to older adults that one cohort of hospitalized patients with serious illness rated these conditions as states worse than death.2 While the mainstays of treatment for bladder and bowel dysfunction are behaviorally based, these treatments are often unsatisfactory and patients often look to surgical options for relief.
Despite these being considerably “minor” or “low risk” surgeries, however, there are little to no data demonstrating the safety and efficacy of such procedures among the oldest adults. This is particularly true among nursing home residents, who represent the most frail subset of the older population, and who are at increased risk both for these disorders and for poor surgical outcomes due to the underlying states of vulnerability and physical dependency that led to institutionalization in the first place. While surgery may be the only “cure” for these bothersome conditions in some individuals, there is a lack of data to help guide physicians in determining which older adults may benefit from surgery and which may be harmed.
We designed a retrospective cohort study using data from the Minimum Data Set (MDS) for Nursing Home Residents and Medicare inpatient and outpatient claims to evaluate and compare short- and long-term outcomes between nursing home residents and propensity-matched community-dwelling older adults undergoing surgery for bladder and bowel dysfunction between 2014 and 2016. By matching on important clinical factors such as age and comorbidity, we expect to see worse outcomes among nursing home residents, likely attributable to their underlying vulnerabilities. Findings from this study will further inform the surgical decision-making process.
Methods
Subjects and Databases
We utilized a 100% cohort of Medicare beneficiaries undergoing our procedures of interest for bladder and bowel dysfunction from 2014–2016. Specifically, we used the Medicare Inpatient file, Outpatient file, Carrier file, Medicare Denominator file, and the Minimum Data Set (MDS) for Nursing Home Residents in order to include all fee-for-service care for Medicare beneficiaries ages 66 and older undergoing these procedures during this time period. The International Classification of Diseases, Ninth Revision (ICD-9) and Tenth Revision (ICD-10) procedure codes and Current Procedural Terminology Codes (CPT4) were used to identify procedures according to the following categories: female pelvic surgery (including surgery for stress urinary incontinence and pelvic organ prolapse), transurethral resection of the prostate (TURP), suprapubic tube (SPT) placement, hemorrhoid surgery, and rectal prolapse surgery (listed in Supplemental Table 1).
Long-term nursing home residents were identified via the MDS file. The MDS is a quarterly assessment of all nursing home residents in the United States who received Medicare or Medicaid benefits. For the purposes of this study, nursing home residents were considered to be long-term if they had completed at least 2 or more consecutive assessments more than 90 days apart during the 12 months prior to their bladder or bowel procedure, consistent with our prior published methodology.3
Outcome Measures
There were three primary outcomes of this study: (1) 30-day complications; (2) 1-year mortality; and (3) changes in resource utilization in the year follow surgery. Thirty-day complications were identified using ICD-9 and corresponding ICD-10 diagnosis codes extracted from the Inpatient and Outpatient Medicare claims, consistent with the existing literature.4,5 Complications included infection, cardiovascular, renal, pulmonary, nervous system including stroke, deep venous thrombosis or pulmonary embolism, delirium, wound complications, postoperative hemorrhage, postoperative shock, complications secondary to anesthesia, other complications, and reoperation. One-year mortality was determined using the date of death from the Medicare Denominator file. Resource utilization was defined as the number of inpatient hospitalizations, emergency room (ER) visits,6 and outpatient office visits in the year before and after surgery based on the Inpatient, Outpatient and Carrier Medicare claims, where appropriate.
Covariates
Demographic data including age, sex and race were obtained from the Medicare Inpatient, Outpatient, Carrier, and Master Beneficiary Summary files. Comorbidity information was abstracted from the Medicare Inpatient and Outpatient files and the MDS, and was used to calculate the Charlson Comorbidity Index Score, consistent with the literature.7
Statistical Analysis
Propensity score matching was performed in order to address measurable confounders of the association of poor outcomes with community-dwelling older adults versus nursing home residents undergoing the bladder and bowel procedures of interest. Propensity scores are the predicted probabilities from a logistic regression model predicting community-dwelling older adults versus nursing home residents. We matched the two groups based on procedure type, age, sex, race, Charlson Score, and the calendar year wherein the procedure was performed using caliper matching without replacement (caliper width of 0.05 standard deviations of the logit propensity) to derive a matched sample.8 While we recognize that matching cannot adjust for frailty and other unmeasurable higher-level factors that lead to nursing home care, it can account for the measurable clinical factors noted herein and in a manner that makes fewer assumptions than a multiple regression approach.9 In order to ensure the effectiveness of the propensity score balancing, we compared standardized mean differences in each predictor before and after matching. After acceptable matching was achieved, we used Generalized Estimating Equations (GEEs) to assess 30-day complications and 1-year mortality with the primary predictor of nursing home versus community-dwelling status in the matched sample. Models were adjusted for procedure type, age group, race, Charlson score, and calendar year. Kaplan Meier survival curves were created to illustrate differences in 1-year survival trends between the two groups with a p value derived from a log-rank test.
Data on healthcare resource utilization in the year before and after surgery are presented in figures with standard error bars. Of note, hospitalizations pertaining to the surgical encounter were counted during the “before surgery” period. In order to account for mortality within the year following surgery, data are weighted based on the number of days that each individual was alive during this time period. We computed estimates and confidence intervals for the outcomes of interest.
A two-sided p was considered to be statistically significant for all analyses. Analyses were performed using SAS Institute statistical software, v. 9.4.
Results
The characteristics of the un-matched cohort of all individuals undergoing surgery for bladder and bowel dysfunction are shown in Supplemental Table 2. There were 429,309 individuals in total, of which 21,600 (5.0%) were nursing home residents and 407,709 (95.0%) were community-dwelling older adults. The characteristics of our propensity matched cohort are shown in Table 1, consisting of a total of 55,389 individuals matched 1:2 whereby there were 18,463 nursing home residents and 36,926 community-dwelling older adults. Collectively, 47.8% of individuals in our cohort underwent TURP, 38.7% underwent SPT placement, 5.4% underwent female pelvic surgery, 5.0% underwent hemorrhoid surgery, and 3.2% underwent rectal prolapse surgery. The mean age of the cohort was 80.5 years, 79.8% were male, 88.2% were white, and mean Charlson Score was 4.6. Additionally, 34.6% of the cohort had surgery in the inpatient setting, 52.5% in the outpatient hospital setting, 3.9% in an ambulatory surgery center, and 3.8% in the office setting.
Table 1.
Cohort characteristics of nursing home residents and propensity matched community-dwelling older adults. SMD=Standard Mean Difference.
| Variable Name | Total | Nursing Home | Community-Dwelling | P value | SMD |
|---|---|---|---|---|---|
|
| |||||
| All Subjects, N (%) | 55389 (100.0) | 18463 (33.3) | 36926 (66.7) | ||
| Propensity score mean ± SD | 0.2 ± 0.1 | 0.2 ± 0.1 | 0.2 ± 0.1 | 0.726 | 0.0032 |
|
| |||||
| Procedure Group, N (%): | |||||
| Female pelvic surgery | 2982 (5.4) | 994 (5.4) | 1988 (5.4) | 1.000 | 0.0000 |
| Transurethral resection of prostate | 26448 (47.8) | 8816 (47.8) | 17632 (47.8) | 0.0000 | |
| Suprapubic tube placement | 21429 (38.7) | 7143 (38.7) | 14286 (38.7) | 0.0000 | |
| Hemorrhoid | 2757 (5.0) | 919 (5.0) | 1838 (5.0) | 0.0000 | |
| Rectal prolapse | 1773 (3.2) | 591 (3.2) | 1182 (3.2) | 0.0000 | |
|
| |||||
| Age, N (%) | |||||
| Age, Mean ± SD | 80.5 ± 7.6 | 80.3 ± 7.7 | 80.6 ± 7.5 | <0.001 | −0.0423 |
| 66–69 | 5537 (10.0) | 2055 (11.1) | 3482 (9.4) | <0.001 | 0.0560 |
| 70–74 | 8892 (16.1) | 3045 (16.5) | 5847 (15.8) | 0.0179 | |
| 75–79 | 11021 (19.9) | 3609 (19.6) | 7412 (20.1) | −0.0132 | |
| 80–85 | 12353 (22.3) | 3981 (21.6) | 8372 (22.7) | −0.0268 | |
| ≥85 | 17586 (31.8) | 5773 (31.3) | 11813 (32.0) | −0.0155 | |
|
| |||||
| Sex, N (%) | |||||
| Male | 44220 (79.8) | 14740 (79.8) | 29480 (79.8) | 1.000 | 0.0000 |
| Female | 11169 (20.2) | 3723 (20.2) | 7446 (20.2) | 0.0000 | |
|
| |||||
| Race, N (%) | |||||
| White | 48872 (88.2) | 16235 (87.9) | 32637 (88.4) | 0.042 | −0.0140 |
| Black | 4209 (7.6) | 1403 (7.6) | 2806 (7.6) | 0.0000 | |
| Other | 2308 (4.2) | 825 (4.5) | 1483 (4.0) | 0.0224 | |
|
| |||||
| Charlson Score, N (%) | |||||
| Mean ± SD | 4.6 ± 3.4 | 4.6 ± 3.4 | 4.5 ± 3.3 | 0.002 | 0.0281 |
| 0 | 5305 (9.6) | 1665 (9.0) | 3640 (9.9) | 0.014 | −0.0287 |
| 1–2 | 12348 (22.3) | 4114 (22.3) | 8234 (22.3) | −0.0004 | |
| 3–4 | 12607 (22.8) | 4257 (23.1) | 8350 (22.6) | 0.0106 | |
| ≥5 | 25129 (45.4) | 8427 (45.6) | 16702 (45.2) | 0.0083 | |
|
| |||||
| Procedure year, N (%) | |||||
| 2014 | 18846 (34.0) | 6282 (34.0) | 12564 (34.0) | 1.000 | 0.0000 |
| 2015 | 17925 (32.4) | 5975 (32.4) | 11950 (32.4) | 0.0000 | |
| 2016 | 18618 (33.6) | 6206 (33.6) | 12412 (33.6) | 0.0000 | |
30-Day Complications
Thirty-day complications are shown in Supplemental Table 3. Nursing home residents demonstrated a mean of 1.1 ± 1.2 complications, compared to a mean of 0.9 ± 1.2 complications among community-dwelling older adults (p<0.001). Of note, 60.1% and 47.2% of nursing home residents and community-dwelling older adults had at least one complication, respectively (p<0.001). The most common complication was infection (in 43.4% vs. 30.7%, p<0.001) followed by cardiovascular (20.2% vs. 14.8%, p<0.001), renal (13.8% vs. 13.1%, p=0.019), and pulmonary complications (14.9% vs. 10.3%, p<0.001), for nursing home vs. community-dwelling, respectively.
Supplemental Table 4 demonstrates the unadjusted 30-day complication rate of each procedure group stratified by whether or not the subject lived in a nursing home. Rates of 30-day complications were 60.1% in nursing home residents compared to 47.2% in community-dwelling older adults (p<0.0001). Subjects undergoing suprapubic tube placement had the highest rates of 30-day complications (62.5% for nursing home residents versus 53.5% for community-dwelling older adults, p<0.0001), and subjects undergoing female pelvic surgery had the lowest rates of 30-day complications (34.3% for nursing home residents versus 29.1% for community-dwelling older adults, p<0.0001).
Table 2 shows the relative risk of various factors associated with 30-day complications. Of note, nursing home residents had an increased adjusted relative risk [aRR 1.3 (95% CI 1.3–1.3; p<0.001)] of having a 30-day complication compared to matched community-dwelling older adults. This finding was significant for all procedures examined, with SPT placement having the highest aRR of 1.6 (95% CI 1.5–1.6, p<0.001) compared to female pelvic surgery. Older age, non-white race, and increasing Charlson score were also associated with increased RR of 30-day complications (see Table 2 for values).
Table 2:
Relative risk associated with 30-day complications, adjusted for calendar year.
| Variable Name | Basic Statistics |
P value | Univariate Model RR |
Multivariate Model RR |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Observed N (%) | Event # (%) | RR & 95% CI | P value | Global P value | RR & 95% CI | P value | Global P value | ||
|
| |||||||||
| Total | 55389 (100.0) | 28510 (51.5) | |||||||
|
| |||||||||
| Cohort Group | |||||||||
| Community-Dwelling | 36926 (66.7) | 17411 (47.2) | <0.001 | Ref. | <0.001 | Ref. | <0.001 | ||
| Nursing Home (NH) | 18463 (33.3) | 11099 (60.1) | 1.3 (1.3 – 1.3) | <0.01 | 1.3 (1.3 – 1.3) | <0.01 | |||
|
| |||||||||
| Procedure type | |||||||||
| Female pelvic surgery | 2982 (5.4) | 1022 (34.3) | <0.001 | Ref. | <0.001 | Ref. | <0.001 | ||
| Transurethral resection of prostate (TURP) | 26448 (47.7) | 13358 (50.5) | 1.5 (1.4 – 1.6) | <0.001 | 1.3 (1.3 – 1.4) | <0.001 | |||
| Suprapubic tube placement (SPT) | 21429 (38.7) | 12100 (56.5) | 1.7 (1.6 – 1.7) | <0.001 | 1.6 (1.5 – 1.6) | <0.001 | |||
| Hemorrhoid | 2757 (5.0) | 1120 (40.6) | 1.2 (1.1 – 1.3) | <0.001 | 1.1 (1.0 – 1.2) | 0.005 | |||
| Rectal prolapse | 1773 (3.2) | 910 (51.3) | 1.5 (1.4 – 1.6) | <0.001 | 1.4 (1.3 – 1.5) | <0.001 | |||
| Age Group | |||||||||
| 65–69 | 5537 (10.0) | 2736 (49.4) | <0.001 | Ref. | <0.001 | Ref. | <0.001 | ||
| 70–74 | 8892 (16.1) | 4356 (49.0) | 1.0 (0.7 – 1.0) | 0.619 | 1.0 (1.0 – 1.0) | 0.526 | |||
| 75–79 | 11021 (19.9) | 5445 (49.4) | 1.0 (1.0 – 1.0) | 0.993 | 1.0 (1.0 – 1.1) | 0.034 | |||
| 80–85 | 12353 (22.3) | 6256 (50.6) | 1.0 (1.0 – 1.1) | 0.130 | 1.1 (1.0 – 1.1) | <0.001 | |||
| ≥85 | 17586 (31.7) | 9717 (55.3) | 1.1 (1.1 – 1.2) | <0.001 | 1.2 (1.2 – 1.2) | <0.001 | |||
| Race | |||||||||
| White | 48872 (88.2) | 24919 (51.0) | <0.001 | Ref. | <0.001 | Ref. | <0.001 | ||
| Non-white | 4209 (7.6) | 2358 (56.0) | 1.1 (1.1 – 1.1) | <0.001 | 1.1 (1.1 – 1.1) | <0.001 | |||
| Charlson score groups | |||||||||
| 0 to 1 | 10712 (19.3) | 3920 (36.6) | <0.001 | Ref. | <0.001 | Ref. | <0.001 | ||
| 2 | 19548 (35.3) | 9435 (48.3) | 1.3 (1.3 – 1.4) | <0.001 | 1.3 (1.3 – 1.3) | <0.001 | |||
| ≥3 | 25129 (45.4) | 15155 (60.3) | 1.7 (1.6 – 1.7) | <0.001 | 1.7 (1.6 – 1.7) | <0.001 | |||
Note: percentages represent row percentages.
1-year mortality
Supplemental Table 4 demonstrates the unadjusted 1-year mortality rates of each procedure group stratified by whether or not the subject lived in a nursing home. Rates of 1-year mortality were 28.9% in nursing home residents compared to 21.3% in community-dwelling older adults (p<0.0001). Subjects undergoing suprapubic tube placement had the highest 1-year mortality rates (36.5% for nursing home residents versus 27.8% for community-dwelling older adults, p<0.0001), and subjects undergoing female pelvic surgery had the lowest 1-year mortality rates (10.1% for nursing home residents versus 5.6% for community-dwelling older adults, p<0.0001).
Table 4 shows the adjusted relative risk of 1-year mortality. Nursing home residents, compared to community-dwelling older adults, demonstrated increased risk of 1-year mortality [aRR 1.4 (95% CI 1.3–1.4; p<0.001)]. This risk was highest for SPT placement [aRR 3.9 (95% CI 3.4–4.4; p<0.001)] and increased with increasing age, Charlson score, and non-white race (see Table 3 for values).
Table 3.
Relative risk associated with 12-month mortality, adjusted for year.
| Variable Name | Basic Statistics |
P value | Univariate Model RR |
Multivariate Model RR |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Observed N (%) | Event # (%) | RR & 95% CI | P value | Global P value | RR & 95% CI | P value | Global P value | ||
|
| |||||||||
| Total | 55389 (100.0) | 13203 (23.8) | |||||||
|
| |||||||||
| Cohort Group | |||||||||
| Community Dwelling | 36926 (66.7) | 7865 (21.3) | <0.001 | Ref. | <0.001 | Ref. | <0.001 | ||
| Nursing Home (NH) | 18463 (33.3) | 5338 (28.9) | 1.4 (1.3 – 1.4) | <0.001 | 1.4 (1.3 – 1.4) | <0.001 | |||
|
| |||||||||
| Procedure type | |||||||||
| Female pelvic surgery | 2982 (5.4) | 212 (7.1) | <0.001 | Ref. | <0.001 | Ref. | <0.001 | ||
| Transurethral resection of prostate (TURP) | 26448 (47.7) | 5525 (20.9) | 2.9 (2.6 – 3.4) | <0.001 | 2.4 (2.1 – 2.7) | <0.001 | |||
| Suprapubic tube placement (SPT) | 21429 (38.7) | 6582 (30.7) | 4.3 (3.8 – 4.9) | <0.001 | 3.9 (3.4 – 4.4) | <0.001 | |||
| Hemorrhoid | 2757 (5.0) | 521 (18.9) | 2.7 (2.3 – 3.1) | <0.001 | 2.2 (1.9 – 2.6) | <0.001 | |||
| Rectal prolapse | 1773 (3.2) | 363 (20.5) | 2.9 (2.5 – 3.4) | <0.001 | 2.4 (2.1 – 2.8) | <0.001 | |||
|
| |||||||||
| Age Group | |||||||||
| 65–69 | 5537 (10.0) | 876 (15.8) | <0.001 | Ref. | <0.001 | Ref. | <0.001 | ||
| 70–74 | 8892 (16.1) | 1670 (18.8) | 1.2 (1.1 – 1.3) | <0.001 | 1.2 (1.2 – 1.3) | <0.001 | |||
| 75–79 | 11021 (19.9) | 2187 (19.8) | 1.3 (1.2 – 1.4) | <0.001 | 1.4 (1.3 – 1.5) | <0.001 | |||
| 80–85 | 12353 (22.3) | 2883 (23.3) | 1.5 (1.4 – 1.6) | <0.001 | 1.6 (1.5 – 1.8) | <0.001 | |||
| ≥85 | 17586 (31.7) | 5587 (31.8) | 2.0 (1.9 – 2.1) | <0.001 | 2.3 (2.1 – 2.4) | <0.001 | |||
|
| |||||||||
| Race | |||||||||
| White | 48872 (88.2) | 11660 (23.9) | 0.374 | Ref. | 0.364 | Ref. | <0.001 | ||
| Others | 4209 (7.6) | 1019 (24.2) | 1.0 (1.0 – 1.1) | 0.607 | 1.1 (1.0 – 1.2) | 0.001 | |||
|
| |||||||||
| Charlson score groups | |||||||||
| 0 to 1 | 10712 (19.3) | <0.001 | Ref. | <0.001 | Ref. | <0.001 | |||
| 2 | 19548 (35.3) | 3854 (19.7) | 1.5 (1.4 – 1.6) | <0.001 | 1.4 (1.4 – 1.5) | <0.001 | |||
| ≥3 | 25129 (45.4) | 7929 (31.6) | 2.4 (2.3 – 2.5) | <0.001 | 2.5 (2.4 – 2.6) | <0.001 | |||
Note: percentages represent row percentages.
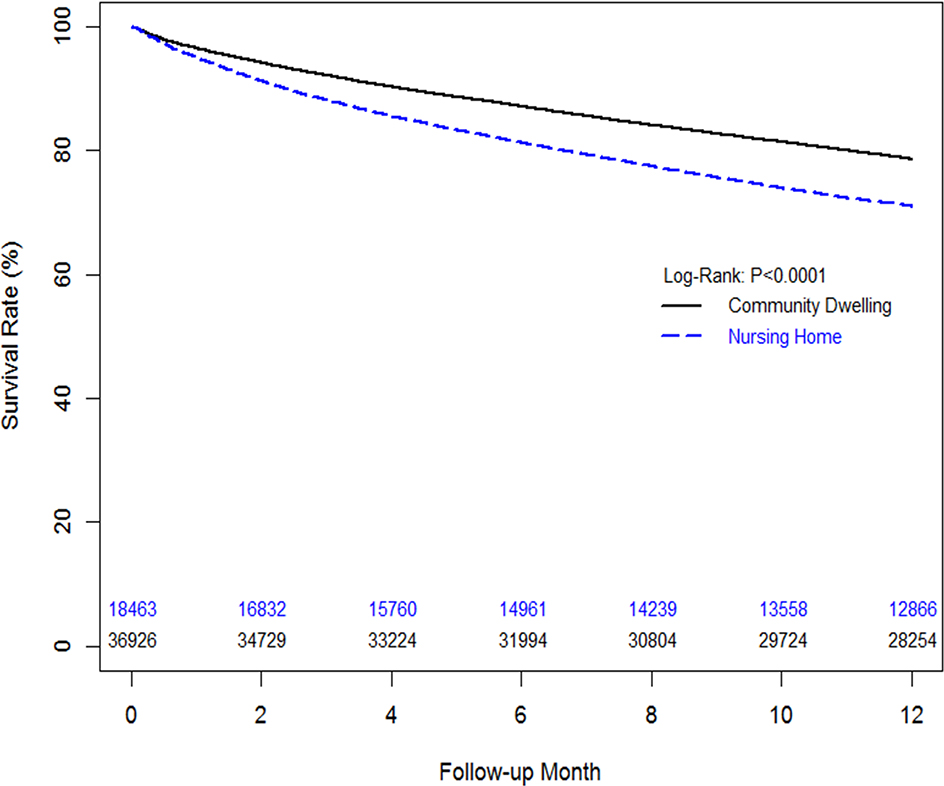
Estimated 1-year survival (Figure 1) was 78.6% for nursing home residents and 71.0% for community-dwelling older adults, p<0.001.
Figure 1.
Kaplan Meier curve comparing 1-year mortality between nursing home residents and matched community-dwelling older adults undergoing surgery for bladder and bowel dysfunction
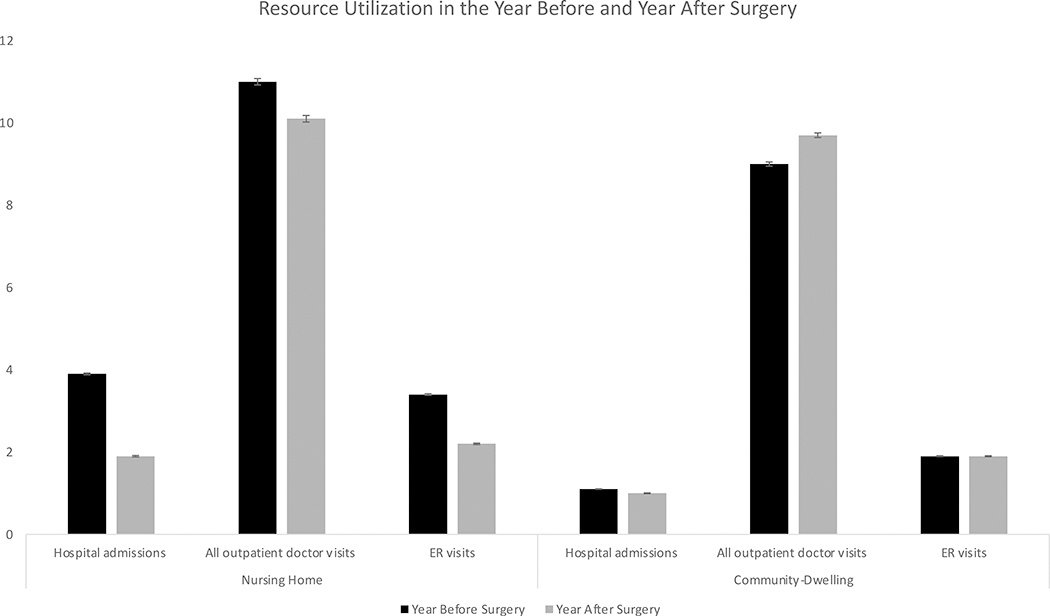
Healthcare Resource Utilization
Figure 2 illustrates weighted counts of healthcare resource utilization (i.e., hospital admissions, outpatient office visits, and ER encounters) in the year before and after surgery among nursing home residents and community-dwelling older adults. Nursing home residents demonstrated marked decreases in all three types of healthcare resource utilization pre- and post-surgery, decreasing from 3.9 to 1.9 hospital admissions, from 11 to 10.1 outpatient doctor visits, and from 3.4 to 2.2 ER visits. Community-dwelling older adults, on the contrary, demonstrated only a modest decrease for number of hospital admissions from 1.1 to 1, an increase in number of outpatient doctor visits from 9 to 9.7, and no change in the number of ER visits from 1.9 to 1.9. Rates of unadjusted healthcare utilization are reported by procedure group and stratified by whether or not the subject lives in a nursing home in Supplemental Table 4.
Figure 2:
Resource Utilization in the Year Before and Year After Surgery in nursing home and community-dwelling older adults with standard errors shown. All p values <0.001.
Discussion
Nursing home residents demonstrated increased relative risk of 30-day complications and 1-year mortality compared to community-dwelling older adults, despite matching on key characteristics such as procedure type, age, sex, race, comorbidity and year. Regardless of these worse outcomes, however, nursing home residents also demonstrated decreases in resource utilization, as measured by fewer hospitalizations, emergency room visits, and office visits in the year following surgery, compared to the year preceding it, suggesting that there may be some potential benefits of surgery in carefully selected older adults.
While our study cohort represented the oldest and most comorbid of individuals undergoing surgery for bladder and bowel dysfunction in the United States, those residing in nursing homes experienced significantly higher rates of 30-day complications and 1-year mortality. There are many possible explanations as to why this may be the case, as nursing home residents often have underlying vulnerabilities that require institutionalization in the first place. Some examples of these vulnerabilities include frailty, functional and cognitive impairment, and underlying social vulnerabilities such as the absence of a caregiver or being unmarried and/or living alone.10
Limited data reporting 30-day complications among nursing home residents and highly comorbid older adults undergoing our procedures of interest exist in the literature. We previously reported 30-day complications among older women undergoing inpatient pelvic organ prolapse surgery to be 16.2% and 3.9% among nursing home and community-dwelling older adults, respectively.3 This is much lower than our combined 30-day mortality rates of 60.1% and 47.2% reported in this study, however, this higher rate likely is driven by some of the other procedures reported herein.
We previously reported 1-year mortality rates ranging from 29% to 50% among nursing home residents undergoing relatively “minor” urologic procedures, including TURP, SPT placement, breast cancer surgery, cystoscopy, bladder biopsy, transurethral resection of bladder tumor, and removal of ureteral obstruction.11–13 In this study, 1-year mortality among nursing home residents was 28.9%, consistent with the lower mortality procedures reported above.
We previously studied a similar cohort of older adults undergoing major abdominal surgery for bleeding duodenal ulcers, cholecystectomy, appendectomy, and colectomy, finding similarly higher rates of mortality (reported at 30-days) among nursing home residents compared to community-dwelling older adults. In this study, 30-day mortality was as high as 42% versus 26% for bleeding duodenal ulcers, 32% versus 13% for colectomy, 12% versus 2% for appendectomy, and 11% versus 3% for cholecystectomy.14 Our reported 1-year mortality rates of 28.9% in nursing home residents versus 21.3% in community-dwelling older adults undergoing surgery for bladder and bowel dysfunction, were appropriately lower compared to those reported in patients undergoing major abdominal surgery. These differences are likely attributable to the fact that our study represents older adults undergoing elective procedures to improve health related quality of life, as opposed to the types of procedures performed in the prior study done on an urgent or emergent basis for sometimes life-threatening conditions.
Our findings on improved resource utilization among nursing home residents undergoing surgery for bladder and bowel dysfunction are a novel contribution to the literature. Of note, these findings were adjusted for the amount of time that individuals were alive in the year following surgery, as to not negatively skew the results. Interestingly, while we found that rates of hospitalization, emergency room visits, and outpatient doctor visits were higher among nursing home residents compared to community-dwelling older adults, the nursing home residents overall demonstrated reduction in utilization of each of these healthcare resources in the year following surgery. This is in contrast to resource utilization among community-dwelling older adults, which even increased for the number of outpatient doctor visits in the year following surgery. While the underlying reasons behind these differences are beyond the scope of this study, these findings are interesting and warrant further investigation. One potential interpretation of these findings is that performing surgery for bladder and bowel dysfunction among carefully selected nursing home residents may result in some benefits due to their potential satisfaction with improved health related quality of life following surgery. Another potential explanation is that older adults living in nursing homes benefit from supportive care that community-dwelling older adults lack, potentially keeping them out of the hospital, emergency room, and office settings.
This study should be interpreted with certain limitations in mind. First, by nature of using billing data as the substrate of our analyses, we lack important clinical and qualitative factors that may be important and influential in surgical decision-making, particularly since we are studying procedures that are performed to improve quality of life. Certainly, future studies that are able to leverage this type of information are needed in order to add important clinical and patient-driven factors to our existing study. However, these more qualitative types of studies are limited to much smaller patient cohorts, while this study is unique in that it is a national sample inclusive of all nursing home residents and corresponding older and highly comorbid adults that would be difficult and impossible to recruit to such a study on this level. Second, our study population only includes individuals who underwent surgery for bladder and bowel dysfunction and excludes individuals with similar conditions who chose not to undergo surgery or who may not have been surgical candidates. To this effect, our population likely represents a positive selection bias towards the nursing home residents (and their corresponding matched counterparts) who were better surgical candidates, thereby excluding less healthy individuals. Furthermore, our reported findings likely represent conservative estimates of complications and mortality.
Conclusions
This study demonstrated increased rates of 30-day complications and mortality in nursing home residents compared to community-dwelling older adults, despite matching on key clinical characteristics such as age and comorbidity. Simultaneously, this study reports slight decreases in resource utilization in the year following surgery, suggesting that there may be some benefits to surgery for bladder and bowel dysfunction among even the most old and frail surgical populations. Future studies are needed in order to explore these findings further to help with improved surgical decision-making in older and frail older adults.
Supplementary Material
Supplemental Table 1. Procedure codes
Supplemental Table 2: Characteristics of all nursing home residents and community-dwelling residents undergoing surgery for bladder and bowel dysfunction
Supplemental Table 3: Frequency of 30-day complications among nursing home residents and community-dwelling older adults.
Supplemental Table 4: Outcomes based on procedure group and stratified by whether the subject resides in a nursing home or in the community.
Impact Statement:
We certify that this work is novel and adds to the literature by addressing surgical outcomes for bladder and bowel dysfunction in older adults.
Key Points:
Nursing home residents demonstrated increased relative risk of 30-day complications and 1-year mortality compared to community-dwelling older adults, despite matching on key characteristics such as procedure type, age, sex, race, comorbidity, and year.
Nursing home residents demonstrated slight decreases in resource utilization (measured by greater decreases in hospitalizations, emergency room visits, and office visits) in the year following surgery for bladder and bowel dysfunction, compared to community-dwelling older adults.
Why does this paper matter?
This study demonstrates worse outcomes, as measured by 30-day complications and 1-year mortality, among nursing home residents compared to propensity score matched community-dwelling older adults, suggesting that non-measurable factors such as frailty contribute to poorer surgical outcomes.
Acknowledgements
Funding: NIH-NIA R01AG058616-01
Footnotes
None of the authors have any conflicts of interest related to this project.
References
- 1.Morgan C, Endozoa N, Paradiso C, McNamara M, McGuire M. Enhanced toileting program decreases incontinence in long term care. Joint Commission journal on quality and patient safety / Joint Commission Resources. 2008;34(4):206–208. [DOI] [PubMed] [Google Scholar]
- 2.Rubin EB, Buehler AE, Halpern SD,. States worse than death among hospitalized patients with serious illnesses. JAMA internal medicine. 2016;176(10):1557–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suskind AM, Zhao S, Boscardin WJ, Covinsky K, Finlayson E. Comparative Outcomes for Pelvic Organ Prolapse Surgery Among Nursing Home Residents and Matched Community-Dwelling Older Adults. The Journal of urology. 2020:101097JU0000000000001331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Massarweh NN, Legner VJ, Symons RG, McCormick WC, Flum DR. Impact of advancing age on abdominal surgical outcomes. Arch Surg 2009;144(12):1108–1114. [DOI] [PubMed] [Google Scholar]
- 5.Hendren S, Birkmeyer JD, Yin H, Banerjee M, Sonnenday C, Morris AM. Surgical complications are associated with omission of chemotherapy for stage III colorectal cancer. Diseases of the colon and rectum 2010;53(12):1587–1593. [DOI] [PubMed] [Google Scholar]
- 6.Venkatesh AK, Mei H, Kocher KE, et al. Identification of Emergency Department Visits in Medicare Administrative Claims: Approaches and Implications. Acad Emerg Med 2017;24(4):422–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of clinical epidemiology. 1992;45(6):613–619. [DOI] [PubMed] [Google Scholar]
- 8.Austin PC. A comparison of 12 algorithms for matching on the propensity score. Statistics in medicine. 2014;33(6):1057–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schafer JL, Kang J. Average causal effects from nonrandomized studies: a practical guide and simulated example. Psychol Methods. 2008;13(4):279–313. [DOI] [PubMed] [Google Scholar]
- 10.Rockwood K, Stolee P, McDowell I. Factors associated with institutionalization of older people in Canada: testing a multifactorial definition of frailty. Journal of the American Geriatrics Society. 1996;44(5):578–582. [DOI] [PubMed] [Google Scholar]
- 11.Suskind AM, Walter LC, Zhao S, Finlayson E. Functional Outcomes After Transurethral Resection of the Prostate in Nursing Home Residents. Journal of the American Geriatrics Society. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang V, Zhao S, Boscardin J, et al. Functional Status and Survival After Breast Cancer Surgery in Nursing Home Residents. JAMA surgery. 2018;153(12):1090–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Suskind AM, Walter LC, Jin C, et al. Impact of frailty on complications in patients undergoing common urological procedures: a study from the American College of Surgeons National Surgical Quality Improvement database. BJU international. 2016;117(5):836–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Finlayson E, Wang L, Landefeld CS, Dudley RA. Major abdominal surgery in nursing home residents: a national study. Annals of surgery. 2011;254(6):921–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1. Procedure codes
Supplemental Table 2: Characteristics of all nursing home residents and community-dwelling residents undergoing surgery for bladder and bowel dysfunction
Supplemental Table 3: Frequency of 30-day complications among nursing home residents and community-dwelling older adults.
Supplemental Table 4: Outcomes based on procedure group and stratified by whether the subject resides in a nursing home or in the community.