Abstract
Background
Racial and ethnic minority groups are disproportionally represented among U.S. coronavirus disease (COVID-19) cases, owing to long-standing systemic inequities in the social determinants of health. Among Hispanic populations, a lack of access to testing sites has resulted in delayed time to diagnosis, risking increased spread within high-risk communities. The accessibility and expertise of community pharmacists support expanded pharmacist roles in public health and pandemic response, including point-of-care (POC) diagnostic testing.
Objective
To determine the local impact of community pharmacist-provided COVID-19 testing among a majority-Hispanic, lower income population during the early COVID-19 pandemic, as assessed by a patient satisfaction survey.
Methods
A 10-question Likert-type questionnaire was administered in English and Spanish to patients who received a pharmacist-provided POC COVID-19 test at a large-chain community pharmacy in Arizona between May 1, 2020 and June 14, 2020. Questions surrounded patient perceptions of the testing process and subsequent pharmacist counseling on their test results.
Results
A total of 622 patients completed the survey (94.1% participation rate among successful contacts, representing 28.3% of all eligible patients). The mean age was 42 years, 51% were female, and 64% of patients identified as Hispanic. More than 97% of surveyed patients either agreed or strongly agreed that receiving a pharmacist-provided COVID-19 test at a community pharmacy was a comfortable experience, expanded their access to care, and allowed them to receive their test results in a timely manner. In addition, more than half of surveyed patients “did not know” where they would have alternatively sought testing if the community testing site was not available. Overall, the results of this study demonstrated highly favorable patient perceptions of pharmacist-provided POC testing for COVID-19, with more than 99% of surveyed patients satisfied with their testing experience.
Conclusion
Among patients in a lower income majority-Hispanic community, pharmacist-provided POC testing services for COVID-19 were well received and expanded patient access to testing during the early pandemic.
Key Points.
Background
-
•
Hispanic populations are among the racial and ethnic minority groups at highest risk for health disparities. During the coronavirus disease (COVID-19) pandemic, this has resulted in increased rates of infection and hospitalization, compounded by a lack of access to testing sites.
-
•
Community pharmacists are among the most accessible health care providers and the first touchpoint of patient engagement within the health care system. Pharmacists are thus well positioned for early detection and triage assessment in the early COVID-19 period.
Findings
-
•
A majority-Hispanic population reported highly favorable perceptions of pharmacist-provided point-of-care testing and counseling for COVID-19, with 98%-99% satisfied with their testing experience and viewing these services as beneficial for their community.
-
•
Most patients did not know where they would have alternatively gone to receive COVID-19 testing if the community pharmacy site was not available, highlighting the essential role of community pharmacies in expanding access to health care services.
-
•
Patients primarily found out about the COVID-19 testing site through referrals from family and friends, emphasizing the importance of community outreach and interpersonal relationship building to maximize awareness of community pharmacy services within Hispanic communities.
Background
The coronavirus disease (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has dealt unprecedented challenges to U.S. health care systems and communities, with more than 35 million cases and more than 600,000 deaths as of August 2021.1 Although all populations have been affected by the pandemic, racial and ethnic minority groups are disproportionally represented among U.S. COVID-19 cases, owing to long-standing systemic inequities in the social determinants of health, including crowded housing conditions, increased representation in essential frontline occupations, and decreased use and access to health care services.2 In particular, persons identifying as Hispanic or Latinx have been found to have significantly higher rates of COVID-19 test positivity across several distinct geographic regions, with evidence for a sustained elevated incidence of COVID-19 over time.3, 4, 5, 6, 7, 8 These disparities are most evident among patients who are Hispanic and between the ages of 18 and 49 years, as they are 4.5 times more likely to be hospitalized for COVID-19 than patients within the same age group who are non-Hispanic and white.9 Patients who are Hispanic may additionally be at increased risk for in-hospital mortality.10 , 11 During public health emergencies, when allocation of resources is often limited, diagnostic testing is needed for triage assessment to prevent the spread of illness within high-risk communities. Delayed diagnosis of COVID-19 is associated with increased hospital visits, poor health outcomes, and increased viral transmission.12 Thus, outreach to highly affected minority communities is essential for detecting cases quickly and controlling virus spread. Among a low-income Latinx community in San Francisco, the median time from COVID-19 symptom onset to time of testing was 4 days, with 25% of patients having a delay of 9 days or longer.13 Lack of access to a testing site was identified as the most common barrier to obtaining testing, as well as not knowing where or how to make an appointment and lacking insurance or a primary care provider.13
In the face of public health emergencies, community pharmacists are the most accessible health care providers and the first touchpoint of patient engagement within the health care system. Pharmacists are well positioned in the community to expand access to care and resources amid a public health crisis, as pharmacies are a highly accessible resource for patients, particularly in underserved and rural communities where patients may not have their own physician. During the pandemic, the Department of Health and Human Services (DHHS), under the Public Readiness and Emergency Preparedness Act, expanded pharmacists’ scope of practice by authorizing the ordering and administration of COVID-19 diagnostic tests across various communities.14 To increase the accessibility of timely testing for at-risk communities, Walgreens partnered with DHHS and initiated no-cost COVID-19 testing to patients by late April 2020, during the time a stay-at-home order was active across Arizona.15 During this period of early first-wave pandemic activity, routine health services were restricted as facilities worked to transition from traditional care delivery models to limited occupancy appointments and telemedicine, with patients potentially experiencing increased barriers to care during this time, particularly among lower income communities. Local pharmacies have the opportunity to mitigate some of these barriers with services such as point-of-care (POC) testing for COVID-19 and pharmacist counseling, which may expand health care access to underserved communities and help alleviate the increased burden on the health care system. Previous literature has supported the public health role of community pharmacists, including during national emergencies, through services such as immunization, disease-state management, and POC testing, with more patients successfully linked to care.16, 17, 18 However, whether patients would perceive these pharmacy services favorably is underexplored within the literature, particularly given the mistrust of government and health care systems among some Hispanic groups owing to factors such as perceived discrimination.19
Objective
The objective of this study was to determine the local impact of community pharmacist-provided COVID-19 testing among a majority-Hispanic, lower income population during the early COVID-19 pandemic, as assessed by a patient satisfaction survey.
Methods
Testing site and patient population
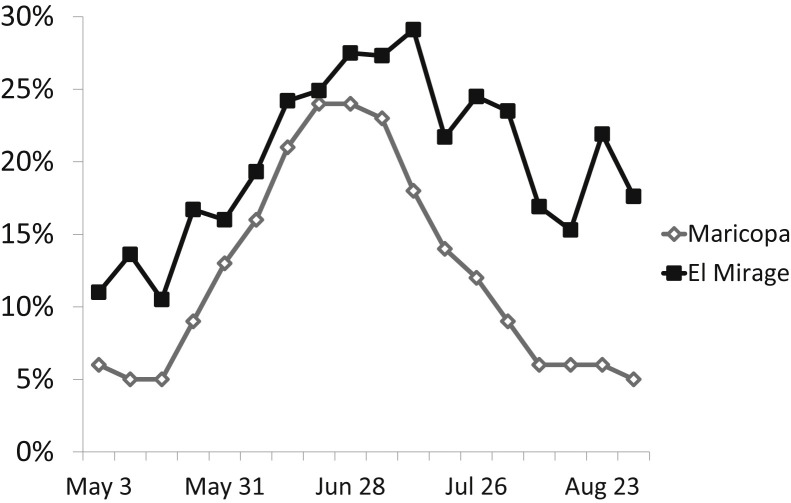
The collaboration between Walgreens and DHHS to provide rapid POC COVID-19 testing at no cost to eligible patients led to the opening of the first Walgreens testing site in Arizona in the city of El Mirage, part of the Greater Phoenix area, on May 1, 2020. Selection of this location was based on criteria set forth by the Center for Disease Control and Prevention’s social vulnerability index (SVI), which uses U.S. census data to rank communities on 15 social factors including socioeconomic status, household composition, minority status, housing type, and transportation.20 These factors help public officials map vulnerable communities in need of support before, during, and after a public health crisis. Possible scores range from 0 (lowest vulnerability) to 1 (highest vulnerability), with an SVI of 0.9057 for El Mirage. Based on 2019 U.S. census data, the population of El Mirage consists of approximately 36,000 people, with 60% identifying as Hispanic or non-white.21 A total of 13% of residents are foreign-born, and more than one-third speak a language other than English at home.21 The median household income is 10% lower than that for Maricopa County, whereas the median per capita income is 36% lower, reflective of a higher average household size.21 During the first wave of COVID-19 activity in Arizona (May 1, 2020-September 1, 2020), a total of 7850 COVID-19 tests were administered to nonappointment patients at the El Mirage location. COVID-19 positivity rates were consistently higher at the El Mirage location than for Maricopa County,22 peaking at 29% in July (Figure 1 ). Consistent with a previous report of Hispanic communities in Massachusetts,8 these higher positivity rates persisted into the late first-wave period, remaining elevated (15%-25%) despite the county’s rates dropping down to early May levels (5%-6%) by mid-August.
Figure 1.
Percent positive COVID-19 diagnostic tests for Maricopa County and El Mirage testing center (May 1, 2020-September 1, 2020). Maricopa County data are per the Arizona Department of Health Services.22 Abbreviation used: COVID-19, coronavirus disease.
The COVID-19 testing site was located in the parking lot of a closed Walgreens retail space in addition to drive-thru COVID-19 testing services. Advertising for this location consisted of posted signage. Bilingual team members were available at the site to assist patients who were primarily Spanish-speaking. Pharmacists were trained to operate the COVID-19 testing site and facilitate the ordering and administration of COVID-19 diagnostic tests to patients after attending a live training workshop provided by Walgreens personnel. POC testing was available with or without a previous appointment and was offered at no cost to the patient. Patients were not required to list insurance information but were required to provide identification for team members to verify the age criteria and laboratory test order matched the patient being tested. At each testing site, patients performed a pharmacist-guided nasal self-swab collection, and specimen samples were processed onsite within 30 minutes by Abbott Diagnostic’s ID NOW rapid molecular device (Abbott Laboratories, Abbott Park, IL).23 The ID NOW device by Abbott Diagnostics obtained Emergency Use Authorization approval by the Food and Drug Administration on March 27, 2020, and COVID-19 testing in El Mirage began on April 1, 2020. In compliance with city ordinances issued to avoid crowding and maximize testing capacity, patients were instructed to exit the testing site directly after test administration. Patients received their results within 24 hours from a trained pharmacist by a follow-up phone call, as well as a printed copy of test results to be mailed within 3-5 days. During these follow-up calls, pharmacists provided counseling to testing participants for both positive and negative test results, including patient education and awareness on signs and symptoms of COVID-19, infection prevention practices, and the appropriate time to seek medical attention for severe or life-threatening symptoms.
Study design and survey instrument
This study was approved by the Midwestern University Institutional Review Board in January 2021. Adult patients without an appointment who received COVID-19 testing at the Walgreens El Mirage testing location between May 1, 2020 and June 14, 2020 were contacted by telephone from January 11, 2021 to February 15, 2021 and invited to complete a survey on their testing experience. The period of early first-wave COVID-19 was selected as the testing time frame for the survey given the need to increase testing accessibility during this time period to quickly track and prevent further spread of the disease, particularly as many primary care physician offices were anticipated to be closing down or limiting capacity. Patients who received COVID-19 testing by appointment were not included as these patients received their test results electronically through a third-party platform (non-Walgreens data) and were not contacted by a pharmacist. Survey participation was voluntary, and verbal informed consent was obtained from all participants.
The survey was conducted by the first author and other Walgreens personnel, including pharmacy interns who volunteered their time to assist with outreach. The authors recruited both English- and Spanish-speaking personnel to accommodate patients’ preferred language. The survey consisted of 10 questions and took approximately 10-15 minutes to administer. Questions 1-8 of the survey used a 4-point Likert-type scale asking the participant to rate their level of agreement with a series of statements related to their experience at the testing site. Topics addressed included health care access, patient knowledge of COVID-19 symptoms, timeliness of the test results, and overall satisfaction. Question 9 asked participants how they heard about the testing site, and question 10 asked where they would have sought COVID-19 testing if the El Mirage site was unavailable. Finally, as an open-ended question, the participants were invited to share any additional feedback on their experience. The survey was developed by the study authors and revised following peer review by outside faculty with expertise in public health. The demographics of the survey participants were additionally recorded to compare with those of all eligible patients and assess the representativeness of the surveyed sample.
Descriptive statistics were used to summarize survey results. Inferential statistics (chi-square for nominal data) were used to compare responses between patient subgroups. Statistical analyses were performed using Microsoft Excel 2010 (Microsoft Corporation, Redmond, WA).
Results
A total of 2200 patients without an appointment received COVID-19 testing during the time period of May 1, 2020-June 14, 2020. Of those patients, 661 were able to be reached (answered the phone initially or made a return call), and 622 consented to participate in the survey for a 94.1% participation rate among successful contacts, representing 28.3% of all eligible patients. Of the surveyed patients, the mean age was 42 years, 51% were female, and 64% of the patients identified as Hispanic. Survey participants appeared demographically similar to the overall population during this time period (Table 1 ). A positive test for COVID-19 infection was seen in 15.9% of total patients and 17.4% of surveyed patients. Most surveyed patients (58%) were referred to the testing site by friends or family, 17% saw posted advertising, 7% were referred by a Walgreens staff member, and 19% found out about the site through other means. Most of the patients (55%) “did not know” where they would have gone to obtain a COVID-19 test if the El Mirage Walgreens site was not available, and 2% would not have sought testing at all. The remaining patients would have gone to an urgent care facility or the emergency department (25%), an alternative retail or community-based clinic (9%), or a primary care physician (8%).
Table 1.
Demographics of patients without an appointment receiving COVID-19 testing from May 1, 2020 to June 14, 2020
| Characteristic | Surveyed patients (n = 622) | All patients (n = 2200) | P value |
|---|---|---|---|
| Age, y, mean (SD) | 42 (16.6) | 42 (16.1) | 0.192 |
| Female sex, n (%) | 319 (51.3) | 1164 (52.9) | 0.474 |
| Race/Ethnicity, n (%) | |||
| Hispanic | 398 (64.0) | 1373 (62.4) | 0.472 |
| White, non-Hispanic | 159 (25.6) | 572 (26.0) | 0.826 |
| Black or African American | 30 (4.8) | 129 (5.9) | 0.320 |
| Other | 35 (5.6) | 126 (5.7) | 0.924 |
| Positive COVID-19 test result, n (%) | 108 (17.4) | 350 (15.9) | 0.385 |
Abbreviation used: COVID-19, coronavirus disease.
Results obtained from the patient satisfaction survey are displayed in Table 2 . In addition, 55% of surveyed patients (n = 342) responded to the open-ended question at the end of the survey soliciting any additional feedback on the testing experience, with 88% of comments being exclusively positive, 8% mixed positive and negative, and 4% negative. More than 99% of surveyed patients felt comfortable receiving COVID-19 testing at a community pharmacy setting, and more than 97% reported that having the community testing site available expanded their access to health care services, including 62% of patients who “strongly agreed” with this statement. This was reflected in the patient comments as well, which stated that the testing site was easy to access and that they liked having the site available in the community. Some patients noted living 30-45 minutes away from the pharmacy but making the drive as it was their nearest available testing site, such as a patient who said that it was “located far from my house but I was glad to have found a place to get tested since there were no available locations near me.” Several also expressed appreciation for having a nonappointment testing option, including a patient who stated, “I am elderly and do not know how to make an appointment online, so it was nice that the testing site took me in without an appointment.” Although a few patients did comment that their testing results were delayed, more than 98% of the patients agreed that they received their COVID-19 test result quickly, with 66% of patients strongly agreeing. Nearly 100 patients specifically praised the fast turnaround time of the testing site in their comments, with many results received within hours, including a patient who said she was “shocked the test results were given so quickly” and a first-responder who “appreciated being able to get back to my job so quick.”
Table 2.
Responses to patient perception survey of pharmacist-guided point-of-care COVID-19 testing and counseling (n = 622)
| Parameter |
Response, n (%) |
||||
|---|---|---|---|---|---|
| Survey question | Strongly agree | Agree | Disagree | Strongly disagree | Declined to answer |
| Q1. I felt comfortable going to a community pharmacy to receive testing for COVID-19 infection. | 399 (64.2) | 219 (35.2) | 4 (0.6) | 0 | 0 |
| Q2. Having a testing center at a community pharmacy improved my access to health care services. | 385 (61.9) | 222 (35.7) | 13 (2.1) | 2 (0.3) | 0 |
| Q3. After my conversation with the pharmacist, I felt more knowledgeable about managing coronavirus signs and symptoms. | 288 (46.3) | 272 (43.7) | 55 (8.8) | 7 (1.1) | 0 |
| Q4. After my conversation with the pharmacist, I felt more knowledgeable about knowing when to seek medical attention for potential COVID-19 symptoms. | 289 (46.5) | 259 (41.6) | 67 (10.8) | 7 (1.1) | 0 |
| Q5. My test results were reported to me in a timely manner. | 412 (66.2) | 194 (31.2) | 10 (1.6) | 5 (0.8) | 1 (0.2) |
| Q6. Pharmacist-provided testing services benefit my community. | 385 (61.9) | 226 (36.3) | 8 (1.3) | 0 | 2 (0.3) |
| Q7. Overall, I am satisfied with the testing services I received. | 420 (67.5) | 197 (31.7) | 3 (0.4) | 2 (0.3) | 0 |
| Q8. I would be willing to receive a pharmacist-provided test for COVID-19 infection at a community pharmacy again. | 406 (65.3) | 203 (32.6) | 7 (1.1) | 0 | 6 (1.0) |
Abbreviations used: COVID-19, coronavirus disease; Q, question.
With respect to their interactions with the pharmacy staff, many patients praised the staff’s professionalism and friendliness: “Everyone was wonderful and very professional in how they took care of the patients,”/“They were very nice, kind, and professional; everyone explained everything very clearly which allowed me to tell my family members more about COVID”/“I felt very safe going there. They were taking precautions and the service was very professional.” Of the surveyed patients, 90% agreed or strongly agreed that they felt more knowledgeable about COVID-19 symptom management after speaking with the pharmacist, and 88% agreed or strongly agreed that they then knew when to seek further medical attention. Multiple patients shared how the pharmacist counseling helped them and their family feel “very well informed” about COVID-19, including a patient who said that the pharmacist “provided very great information” that “saved his life” at a time when he could not find any other help or support in Phoenix. Another shared, “My wife and I had a fantastic experience with the pharmacist! The pharmacist that was there was amazing! She told us exactly what to do and what to look out for and how to cope with everything,” and a grandmother testing positive for COVID-19 said that “the pharmacist was great as she explained everything I needed to do after testing positive to make my grandkids safe.” One patient shared that she “was hospitalized two days after receiving my COVID test and was thankful that I knew when to call 911.” Of the approximately 10% of patients who disagreed that they felt more knowledgeable after speaking with the pharmacist, most stated that they had never received a post-visit phone call and, therefore, did not have a conversation with the pharmacist or said that they did not remember the counseling given the months that had passed from their initial testing date.
Overall, 98%-99% of the surveyed patients reported being satisfied with their testing experience and willing to receive pharmacist-provided POC testing services again. Many patients summed up their experience as “amazing,” “awesome,” or “perfect,” and several shared that they had already visited the testing site multiple times, including a patient who stated that since testing she had referred more than 20 friends and family members. Similarly, 98% of patients agreed or strongly agreed that pharmacist-provided testing services benefit the community, stating that “this is a necessary resource that needs to be in the communities for people .” Multiple patients noted the pervasive fear and anxiety that was present during the early pandemic and that “a testing site was really needed in the community at the start of the pandemic” and provided substantial benefit and comfort, and that the counseling and support of the pharmacists and the staff “made it not scary.” Some patients stated that they “wish there were more locations open since there is a great need for them,” particularly expansion into rural areas.
Hispanic, older adult (aged ≥65 years), female, and COVID-positive patient subgroups were additionally assessed (Table 3 ). Older adults were less likely to have a positive COVID-19 test result than younger patients (6.1% vs. 18.7%, P = 0.008), whereas patients who were Hispanic were more likely to have a positive test result than patients who were non-Hispanic (22.9% vs. 7.6%, P < 0.001). Across all subgroups, perceptions of the pharmacist-guided POC COVID-19 testing experiences were broadly similar with respect to the percent of strongly agree/agree responses, with the exception that older adults were less likely to report feeling more knowledgeable after receiving pharmacist counseling on potential signs and symptoms of COVID-19 infection (82% vs. 91%, P = 0.018) and when to seek medical attention (77% vs. 89%, P = 0.004). A significantly higher proportion of patients who were Hispanic, by contrast, reported feeling more knowledgeable (>92% agreement, Table 3).
Table 3.
Subgroup comparisons among surveyed patients receiving pharmacist-guided point-of-care COVID-19 testing and counseling
| Parameter | All surveyed patients, n = 622 | COVID(+) n = 108 (17.4) | Age ≥ 65 y n = 66 (10.6) | Female n = 319 (51.2) | Hispanic n = 398 (64.0) |
|---|---|---|---|---|---|
| COVID(+) | 108 (17.4) | 108 (100)a | 4 (6.1)a | 63 (19.7) | 91 (22.9)a |
| Q1. I felt comfortable going to a community pharmacy to receive testing for COVID-19 infection. – SA/A | 618 (99.4) | 107 (99.1) | 65 (98.5) | 317 (99.4) | 397 (99.7) |
| Q2. Having a testing center at a community pharmacy improved my access to health care services. – SA/A | 607 (97.6) | 105 (97.2) | 63 (95.5) | 310 (97.2) | 388 (97.5) |
| Q3. After my conversation with the pharmacist, I felt more knowledgeable about managing coronavirus signs and symptoms. – SA/A | 560 (90.0) | 100 (92.6) | 54 (81.8)a | 283 (88.7) | 375 (94.2)a |
| Q4. After my conversation with the pharmacist, I felt more knowledgeable about knowing when to seek medical attention for potential COVID-19 symptoms. – SA/A | 548 (88.1) | 100 (92.6) | 51 (77.3)a | 278 (87.1) | 368 (92.5)a |
| Q5. My test results were reported to me in a timely manner. – SA/A | 606 (97.4) | 104 (96.3) | 62 (93.9) | 310 (97.2) | 388 (97.5) |
| Q6. Pharmacist-provided testing services benefit my community. – SA/A | 611 (98.2) | 108 (100) | 63 (95.5) | 311 (97.5) | 393 (98.7) |
| Q7. Overall, I am satisfied with the testing services I received. – SA/A | 617 (99.2) | 107 (99.1) | 64 (97.0) | 316 (99.1) | 396 (99.5) |
| Q8. I would be willing to receive a pharmacist-provided test for COVID-19 infection at a community pharmacy again. – SA/A | 609 (97.9) | 103 (95.4) | 64 (97.0) | 311 (97.5) | 391 (98.2) |
Abbreviations used: A, agree; COVID-19, coronavirus disease; Q, question; SA, strongly agree.
Note: Values are given as n (%).
Statistically significant difference (P < 0.05) compared with all surveyed patients.
Discussion
This study aimed to determine the local impact of pharmacist-provided POC testing in a low-income primarily Hispanic community in the early pandemic period. Overall, the results of the survey demonstrated highly favorable patient perceptions of pharmacist-provided POC testing for COVID-19, with 99% of surveyed patients satisfied with their testing experience. Most of the surveyed patients identified having no alternative testing site available to them, supporting the local impact of testing availability in community pharmacy settings and expanding health care access to vulnerable populations. Based on the most recent Medical Expenditure Panel Survey in 2018,24 patients who were Hispanic were twice as likely as any other racial or ethnic group to be uninsured, and less than half identified having an office-based health care provider for routine care, highlighting the importance of using alternative care delivery models to provide effective outreach, particularly during public health emergencies. The availability of nonappointment testing options was also highlighted by the surveyed patients as a positive feature of the site, which may expand access to care. Many Hispanic persons work frontline jobs such as within grocery stores, construction, food delivery, and cleaning and sanitation services, which in addition to increasing COVID-19 exposure risk may have inconsistent schedules or lack paid time off, limiting the ability of these workers to schedule appointments.25 Nonappointment options also increase access for patients without reliable Internet or technology to schedule the appointment or those who may hesitate to call to make an appointment owing to language barriers.
The high observed COVID-19 positivity rate at the El Mirage site is consistent with existing data demonstrating the disproportionate impact of the pandemic on Hispanic communities in the United States. The pandemic has created fear and anxiety among Hispanic families as many of them face language barriers and limited access to health information in their communities. A national survey conducted by the Pew Research Center revealed Hispanic adults were more likely to view COVID-19 as a major threat to the health of the U.S. population (65% vs. 47%) as well as a major threat to their personal health (39% vs. 27%).26 In addition to work-related exposures, approximately 25% of Hispanic persons live in multigenerational households compared with only 15% of non-Hispanic whites, which can make it difficult for families to take precautions, maintain social distancing, and care for sick loved ones without risking exposure.25 This supports the need to reach vulnerable populations quickly, and efficiently use preventative services such as POC testing, patient education, and other useful resources in the community during future health crises.
Many patients praised the friendliness, professionalism, and knowledge of the pharmacists at the testing site. Respect for the normative cultural values of personalismo (formal friendliness/relationship building), simpatía (kindness), respeto (respect), and familismo (family loyalty) can help pharmacists provide culturally competent health care to patients who are Hispanic and support community outreach.27 Several patients noted referring friends and family to the testing site after their positive personal experience and more than half of all surveyed patients learned of the site from such referrals, highlighting the expansive impact and importance of developing interpersonal relationships and earning patient trust. The patients who did not report feeling more knowledgeable after their conversation with the pharmacist largely were those who did not receive the intended follow-up counseling phone call, for example because they did not answer their phone or their provided contact number was not in service. Pharmacist counseling was delivered during the follow-up call to streamline the testing process and to allow the counseling to be tailored on the basis of the patient’s test result. However, providing general counseling during the testing visit itself may have allowed for better capture of the 10% of patients who missed out on this information. The lower proportion of older adults who reported feeling more knowledgeable after receiving pharmacist counseling is also worthy of consideration for future health outreach efforts.
Previous studies have recognized the benefits of including community pharmacists in the detection of infectious diseases and prevention of spread among low-resource settings where access to traditional health services is limited. Most published studies evaluating POC testing have focused on known diseases in the community, such as influenza and streptococcus. However, a recent article on community pharmacists’ contributions to disease management during the COVID-19 pandemic highlighted the significant structural health disparities that challenge the current U.S. health care system, stressing the importance of interfacing public health with other sectors of the health care system, including community pharmacies, to better prepare a quick response to a public health crisis.28 , 29 Ultimately, the positive patient perceptions of pharmacist-provided health care services revealed in the present study has broad implications beyond the current pandemic. Virtually all patients agreed that community pharmacy testing benefits their community, with calls for additional sites and expansion into rural areas. This supports increased pharmacist roles in providing preventative services in the community including POC testing, primary care services, and select prescription authority to not only strengthen the U.S. health care system but to make it more inclusive, accessible, and effective for the most vulnerable.
Limitations of this study included potential poor patient recollection of experiences owing to the long follow-up period and that the telephonic survey methods may have limited inclusion of homeless, high-poverty patients without access to a phone. The older adult patients surveyed were less likely to report feeling more knowledgeable after receiving pharmacist counseling on potential signs and symptoms of COVID-19 infection and when to seek medical attention, which could be partially attributable to recall bias, since this group was also less likely to test positive for COVID-19. Other limitations included the survey being conducted by pharmacy personnel, whereby participants may have felt inclined to answer positively, and the inability to reach all eligible patients; however, the surveyed patients were demographically similar to the full sample. Patient perceptions during the late pandemic period were also unknown. Further studies would be beneficial to confirm these findings in other cities with differing patient demographics.
Conclusion
The study results support the local impact of community pharmacy testing sites on expanding health care access to underserved and vulnerable populations who are most affected by health care disparities. Community pharmacists may provide added benefit in alleviating the burden on the health care system during public health emergencies, including through the provision of pharmacist counseling and patient education.
Acknowledgments
The authors thank the following students from Midwestern University College of Pharmacy Glendale campus for their assistance in administering the survey: Denisse Garcia Zavala, Delmi Juarez Zelaya, Claudia Kopec, Leidy Wynne Perez, and Melika Peyvandi.
Biographies
Janelle Patel, PharmD, PGY-1 Community Pharmacy Resident, Walgreens Specialty Pharmacy, Phoenix, AZ
Nikki Christofferson, PharmD, Specialty Pharmacy Site Manager, Walgreens Specialty Pharmacy, Phoenix, AZ
Kellie J. Goodlet, PharmD, BCPS, BCIDP, Assistant Professor, Department of Pharmacy Practice, College of Pharmacy, Midwestern University, Glendale, AZ
Footnotes
Disclosure: The authors declare no relevant conflicts of interest or financial relationships.
Previous presentation: A poster of the study findings was previously presented at the virtual 2021 APhA Annual Meeting and Exposition (March 11-15, 2021).
ORCID Kellie J. Goodlet: http://orcid.org/0000-0002-9736-0891
References
- 1.World Health Organization Coronavirus disease (COVID-19) dashboard: United States of America. https://covid19.who.int/region/amro/country/us/ Available at:
- 2.Centers for Disease Control and Prevention Health equity considerations and racial and ethnic minority groups. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html Available at:
- 3.Khanna N., Klyushnenkova E.N., Kaysin A. Association of COVID-19 with race and socioeconomic factors in family medicine. J Am Board Fam Med. 2021;34(Suppl):S40–S47. doi: 10.3122/jabfm.2021.S1.200338. [DOI] [PubMed] [Google Scholar]
- 4.Turner N.A., Pan W., Martinez-Bianchi V.S., et al. Racial, ethnic, and geographic disparities in novel coronavirus (severe acute respiratory syndrome coronavirus 2) test positivity in North Carolina. Open Forum Infect Dis. 2020;8(1):ofaa413. doi: 10.1093/ofid/ofaa413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Escobar G.J., Adams A.S., Liu V.X., et al. Racial disparities in covid-19 testing and outcomes: retrospective cohort study in an integrated health system. Ann Intern Med. 2021;174(6):786–793. doi: 10.7326/M20-6979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Podewils L.J., Burket T.L., Mettenbrink C., et al. Disproportionate incidence of covid-19 infection, hospitalizations, and deaths among persons identifying as Hispanic or Latino - Denver, Colorado March-October 2020. MMWR Morb Mortal Wkly Rep. 2020;69(48):1812–1816. doi: 10.15585/mmwr.mm6948a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mackey K., Ayers C.K., Kondo K.K., et al. Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: a systematic review. Ann Intern Med. 2021;174(3):362–373. doi: 10.7326/M20-6306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tieskens K.F., Patil P., Levy J.I., et al. Time-varying associations between COVID-19 case incidence and community-level sociodemographic, occupational, environmental, and mobility risk factors in Massachusetts. BMC Infect Dis. 2021;21(1):686. doi: 10.1186/s12879-021-06389-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention COVID-19 racial and ethnic health disparities. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/disparities-hospitalization.html Available at:
- 10.Wiley Z., Ross-Driscoll K., Wang Z., Smothers L., Mehta A.K., Patzer R.E. Racial and ethnic differences and clinical outcomes of COVID-19 patients presenting to the emergency department. Clin Infect Dis. 2021 doi: 10.1093/cid/ciab290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dai C.L., Kornilov S.A., Roper R.T., et al. Characteristics and factors associated with COVID-19 infection, hospitalization, and mortality across race and ethnicity. Clin Infect Dis. 2021 doi: 10.1093/cid/ciab154. accessed April 6, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rong X.M., Yang L., Chu H.D., Fan M. Effect of delay in diagnosis on transmission of COVID-19. Math Biosci Eng. 2020;17(3):2725–2740. doi: 10.3934/mbe.2020149. [DOI] [PubMed] [Google Scholar]
- 13.Rubio L.A., Peng J., Rojas S., et al. The COVID-19 symptom to isolation cascade in a Latinx community: a call to action. Open Forum Infect Dis. 2021;8(2):ofab023. doi: 10.1093/ofid/ofab023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.United States Department of Health and Human Services HHS statements on authorizing licensed pharmacists to order and administer covid-19 tests. https://www.hiv.gov/blog/hhs-statements-authorizing-licensed-pharmacists-order-and-administer-covid-19 Available at:
- 15.Office of the Governor Doug Ducey Stay home, stay healthy, stay connected. https://azgovernor.gov/governor/news/2020/03/stay-home-stay-healthy-stay-connected Available at:
- 16.Gubbins P.O., Klepser M.E., Dering-Anderson A.M., et al. Point-of-care testing for infectious diseases: opportunities, barriers, and considerations in community pharmacy. J Am Pharm Assoc (2003) 2014;54(2):163–171. doi: 10.1331/JAPhA.2014.13167. [DOI] [PubMed] [Google Scholar]
- 17.Saldarriaga E.M., Vodicka E., La Rosa S., Valderrama M., Garcia P.J. Point-of-care testing for anemia, diabetes, and hypertension: a pharmacy-based model in Lima, Peru. Ann Glob Health. 2017;83(2):394–404. doi: 10.1016/j.aogh.2017.03.514. [DOI] [PubMed] [Google Scholar]
- 18.Strand M.A., Bratberg J., Eukel H., Hardy M., Williams C. Community pharmacists’ contributions to disease management during the COVID-19 pandemic [published correction appears in Prev Chronic Dis. 2020;17:E98] Prev Chronic Dis. 2020;17:E69. doi: 10.5888/pcd17.200317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perez D., Sribney W.M., Rodríguez M.A. Perceived discrimination and self-reported quality of care among Latinos in the United States. J Gen Intern Med. 2009;24(Suppl 3):548–554. doi: 10.1007/s11606-009-1097-3. Suppl 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agency for Toxic Substances and Disease Registry CDC/ATSDR SVI fact sheet. https://www.atsdr.cdc.gov/placeandhealth/svi/fact_sheet/fact_sheet.html Available at:
- 21.United States Census Bureau Quickfacts. https://www.census.gov/quickfacts/fact/table/elmiragecityarizona/INC110219 Available at:
- 22.Arizona Department of Health Services COVID-19 data. https://www.azdhs.gov/covid19/data/index.php Available at:
- 23.ID NOW COVID-19 [package insert] Abbott Diagnostics Scarborough, Inc; Scarborough, ME: 2020. [Google Scholar]
- 24.Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey. https://meps.ahrq.gov/mepsweb/ Available at:
- 25.Bucknor C. Hispanic workers in the United States. Center for Economic and Policy Research. https://cepr.net/images/stories/reports/hispanic-workers-2016-11.pdf Available at:
- 26.Krogstad J.M., Gonzalez-Barrera A., Lopez M.H. Hispanics more likely than Americans overall to see coronavirus as a major threat to health and finances. Pew Research Center. 2020. https://www.pewresearch.org/fact-tank/2020/03/24/hispanics-more-likely-than-americans-overall-to-see-coronavirus-as-a-major-threat-to-health-and-finances/ Available at:
- 27.Flores G. Culture and the patient-physician relationship: achieving cultural competency in health care. J Pediatr. 2000;136(1):14–23. doi: 10.1016/s0022-3476(00)90043-x. [DOI] [PubMed] [Google Scholar]
- 28.Lurie N., Fremont A. Building bridges between medical care and public health. JAMA. 2009;302(1):84–86. doi: 10.1001/jama.2009.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maani N., Galea S. COVID-19 and underinvestment in the public health infrastructure of the United States. Milbank Q. 2020;98(2):250–259. doi: 10.1111/1468-0009.12463. [DOI] [PMC free article] [PubMed] [Google Scholar]