Abstract
Objective:
To characterize national trends in urologist workforce, practice organization, and management of incident prostate cancer.
Methods:
Using Medicare claims data from 2010 to 2016, we identified all urologists billing Medicare and the practice with which they were affiliated. We characterized groups as solo, small single specialty, large single specialty, multispecialty, specialist, or hospital-owned practices. Using a 20% sample of national Medicare claims, we identified all patients with incident prostate cancer and identified their primary treatment.
Results:
The number of urologists increased from 9,305 in 2010 to 9,570 in 2016 (p = 0.03), while the number of practices decreased from 3,588 to 2,861 (p<0.001). The proportion of urologists in multispecialty groups increased from 17.1% in 2010 to 28.2% in 2016, while those within solo practices declined from 26.2% to only 15.8% over the same time period. A higher proportion of patients at hospital-owned practices were treated with observation (p<0.001) and surgery (p<0.001), while a higher proportion of patients at large single specialty practices were treated with radiation therapy (p<0.001).
Conclusions:
We characterized shifts in urologist membership from smaller, independent groups to larger, multispecialty or hospital-owned practices. This trend coincides with higher utilization of observation and surgical treatment for prostate cancer.
Keywords: heath services research, prostate cancer, practice organization, urology workforce
TWEET
Urology practices are consolidating quickly. The plurality of urologists moved to multispecialty groups by 2012.
INTRODUCTION
Physician practices are rapidly consolidating in the United States, as small independently owned groups merge or are acquired by larger hospital systems.1–9 Multiple factors motivate this shift, including the capital required for entrepreneurial activities,8 reimbursement patterns,2,10 administrative burdens,6,11 and the need for infrastructure to participate in quality measurements and population health management initiatives.12–14 While some published analyses demonstrate hospital integration in select specialty practices, such as cardiology and oncology,15 changes in urologist practice organization in recent years are not well understood.
Further, urologists’ practice context impacts treatment choice for and health care spending on men with prostate cancer.4,14,16–19 The structure of urology practices may even be associated with the quality of prostate cancer care.20 The implications of the ongoing shift in the organization of the urology workforce on the management of men with prostate cancer are poorly understood. Larger urology groups resulting from consolidation of smaller practices or assimilation into larger hospital-owned multispecialty settings may offer higher quality care at a lower cost, as a result of subspecialization within the group. Further, larger groups are better suited to invest in new and profitable technology, such as intensity-modulated radiation therapy vaults, which may impact utilization of specific treatment types.16 Lastly, hospital-owned groups may bill evaluation and management visits as taking place in a “hospital outpatient department” and receive higher total payments, thereby increasing the total spending associated with office urology care.3
Therefore, we use national Medicare data to build on prior work characterizing trends in the organization and practice context of urologists, as well as examine changes in the usage of observation, radiation, and surgery in the treatment of incident prostate cancer.
METHODS
Study Population
Using the Medicare Data on Provider Practice and Specialty file (MD-PPAS), we identified all urologists working as Medicare providers with a unique national provider identification (NPI) number.21 Using MD-PPAS, each provider’s individual NPI was associated with the tax identification number (TIN) of his or her practice annually between 2010 and 2016. We included all urologists filing any fee-for-service Part B non-institutional Medicare claims. MD-PPAS includes data on all Medicare providers, not a representative sample.
Next, we identified a cohort of men with newly diagnosed prostate cancer. Using a 20% sample of national Medicare beneficiaries, we retrospectively compiled this cohort of men diagnosed with prostate cancer from 2010 to 2015. We allowed for one year of treatment follow-up data through 2016. New cases of prostate cancer were identified using an algorithm validated with cancer registry data, that has a specificity of 99.8% and positive predictive value of 88.7%.22 Patients eligible for Parts A and B were included, while those patients with Medicare managed care plans were excluded to ensure the availability of complete claims.
Urologist Practice Organization
Practices were categorized based upon previously described taxonomy, with the addition of the “hospital-owned” category.16,19 Practices were first sorted into hospital-owned versus non-hospital-owned groups. We defined hospital-owned practices empirically by examining the place-of-service code of submitted claims.23 Practices with 75% or more of their office visits billed with a “hospital outpatient department” place of service (as opposed to “office”) were designated “hospital-owned practices”. Most academic medical centers are likely categorized as hospital-owned practices. This group was included to analyze national trends among this type of practice within urology. We then stratified non-hospital-owned practices by size and diversity of providers.19 Any group with 1 or 2 physicians was considered a “solo practice”. For larger groups, those with more than 50% urologists were labeled “single specialty groups” and further characterized as “large” (10 or more physicians) or “small” (3–9 physicians). Groups that included fewer than 50% urologists and also had at least one primary care physician (i.e., specialty of general practice, internal medicine, family medicine, geriatrics, or pediatrics) were labeled “multispecialty groups.” Finally, groups with fewer than 50% urologists that did not include any primary care physicians were labeled “specialist groups.”
Urologist Group Assignment and Patient Urologist Assignment
Urologists were assigned to one primary practice for each calendar year from 2010 through 2016.21 Within the MD-PPAS dataset, 81.3% of included providers billed under one TIN alone. For those who submitted claims under more than one TIN in a given year, the TIN associated with the largest fraction of their claims was considered the primary group practice. Further, patients were assigned to one urologist through which they received treatment. If patients were treated by two or more urologists, the predominant urologist was determined based upon plurality of visits, duration of physician-patient relationship, and date of urology visits from the time of prostate cancer diagnosis.
Patient Treatment Modalities
For each man with an incident diagnosis of prostate cancer, we identified the primary treatment modality using Medicare claims data. We included patients managed with observation, radiation therapy, surgery, or other therapies, like ablative therapy or brachytherapy, using claims after prostate cancer diagnosis.24 A minority of men received hormone therapy and were not included in this analysis on treatment modality. We considered men who received no treatment for prostate cancer within 12 months of diagnosis as undergoing observation. In prior work we found an algorithm to correctly identify men on active surveillance with specificity 93.5% and sensitivity 88.2%.25 Thus, although the majority of the included men on “observation” were on active surveillance, the group will be referred to as undergoing observation for improved accuracy. Finally, we performed a sensitivity analysis by limiting urologists to those with only one TIN for the year.
Analysis
We assessed trends in provider distribution and patient treatment data using SAS statistical software (Cary, NC). Trends in number of urologists and number of unique practices over time were measured using Poisson regression with a linear term for year. Next, percent practice type for year 2010 versus year 2016 were assessed using chi-square tests. Finally, percent treatment type by practice type were also compared using chi-square tests. As a retrospective descriptive analysis of deidentified patient data, this study was deemed exempt from review by institutional IRB.
RESULTS
Distribution of Group Practice Types
We identified 9,305 urologists practicing within 3,588 practices participating in Medicare in 2010. Between 2010 and 2016, the number of urologists increased to 9,570 (p for trend = 0.03), while the number of unique practices decreased to 2,861 (p for trend < 0.001) (Figure 1). In 2010, the majority of the 3,588 practices were solo practices (n=2,184, 60.9%) (Figure 2). However, by 2016, this decreased to 1,371 solo practices, representing 47.9% of groups (p<0.001). In the same period, the number of multispecialty groups increased from 613 (17.1%) to 806 (28.2%) (p<0.001) and the number of hospital-owned practices increased from 165 (4.6%) to 226 (7.9%) (p<0.001).
Figure 1:
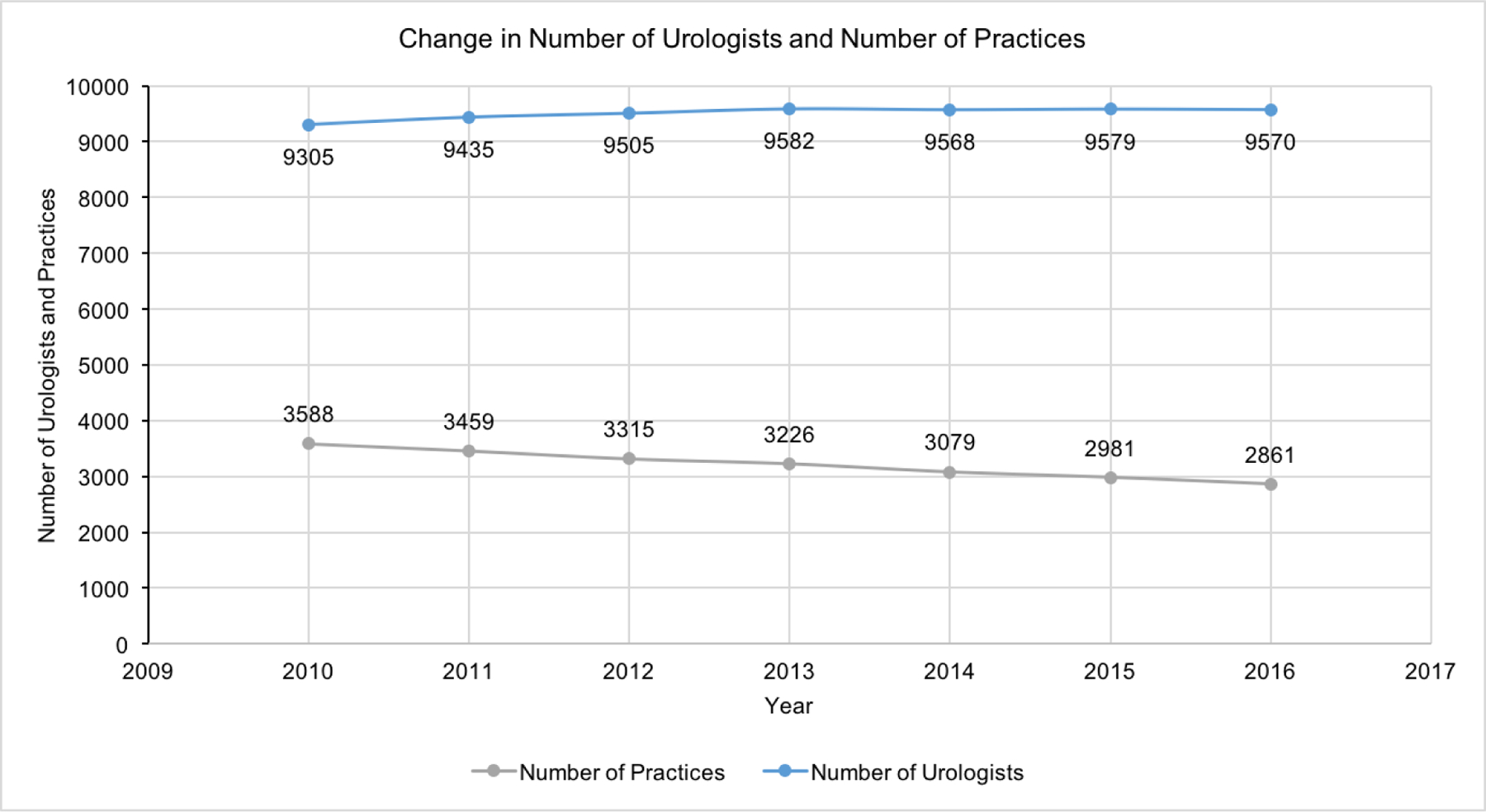
The change in number of urologists and number of practices from 2010 to 2016.
Figure 2:
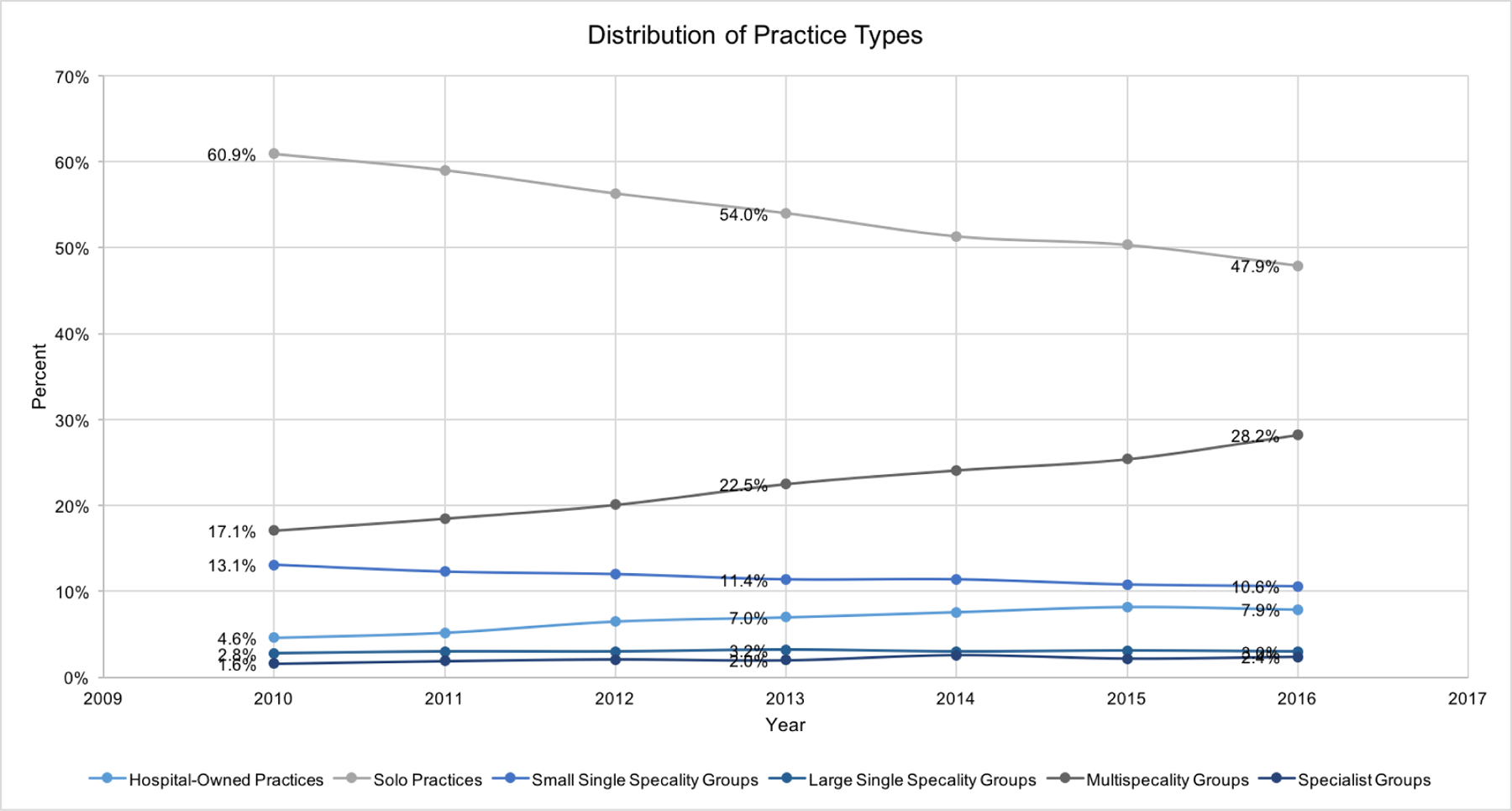
The change in the distribution of practice types from 2010 to 2016.
Distribution of Urologists
Of the 9,305 urologists in 2010, the plurality was practicing within solo practices (n=2,435, 26.2%) (Figure 3). However, by 2016, only 15.8% of urologists were part of a solo practice (p<0.001). By 2016, the number of urologists increased to 9,570 with the plurality (n=3,737, 39.0%) practicing within a multispecialty group (p<0.001). Urologists practicing within a hospital-owned practice also increased from 7.0% in 2010 to 9.3% of urologists in 2016 (p<0.001). Around 81.6% of urologists practices at only one TIN, which is similar to the rates for all physicians of 81.1%.
Figure 3:
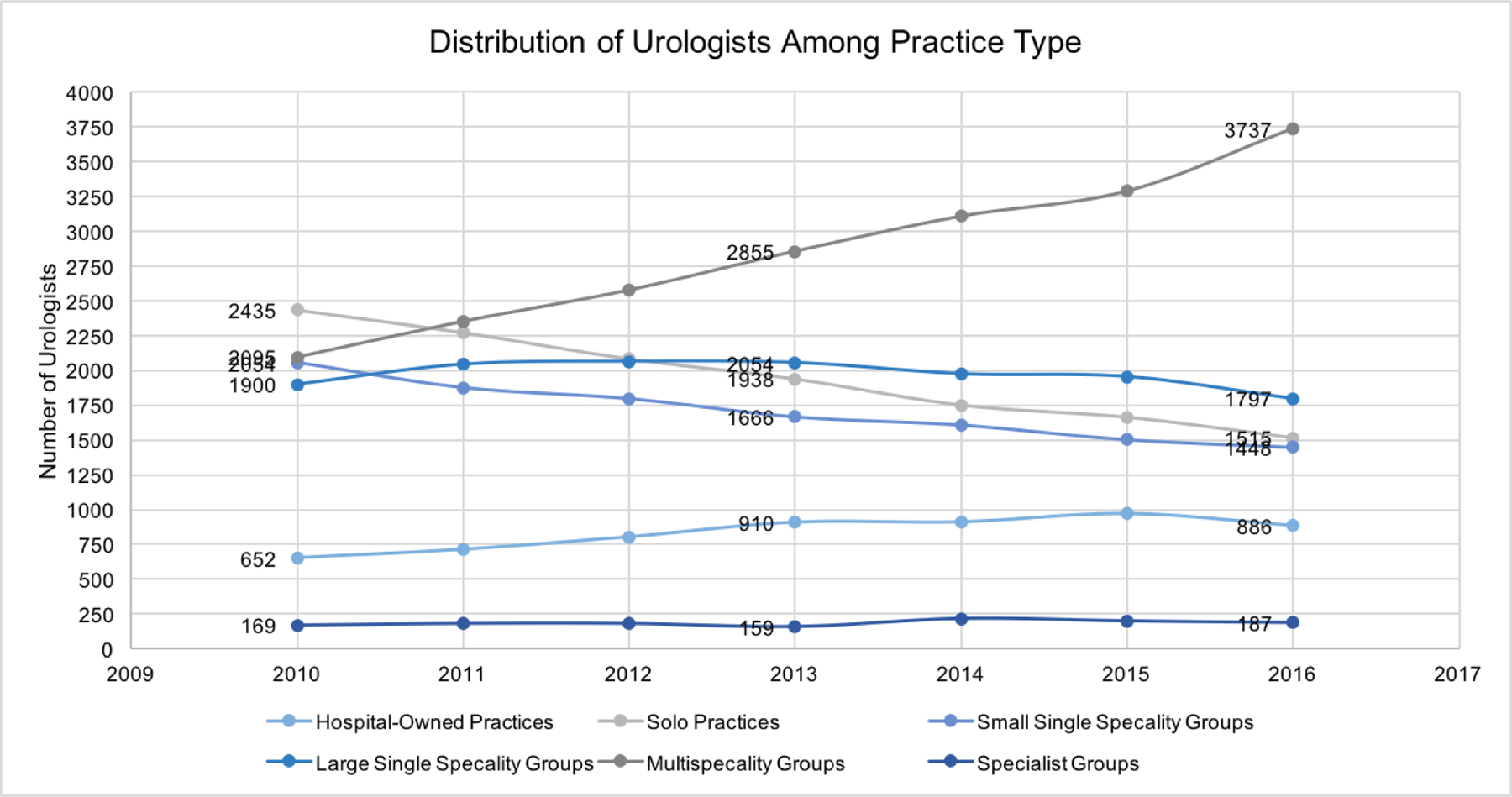
The change in the distribution of urologists among practice types from 2010 to 2016.
Men with Incident Prostate Cancer
The distribution of prostate cancer patients mirrored that of urologists in this time period. In 2010, a plurality of men with a new diagnosis of prostate cancer were cared for by a urologist in either a solo practice (23.1%) or a small single specialty group (28.5%). However, by 2015, the majority of men with incident prostate cancer were cared for by urologists in a multispecialty group (27.8%) or large single specialty group (26.8%). A growing proportion of men with prostate cancer are being managed by urologists in hospital-owned practices, from 3.8% in 2010 to 6.5% of men diagnosed in 2015.
Utilization of Treatment Type Across Practice Types
We noted a difference in the distribution of treatment types across practice types. In 2015, between 20.8% of patients at large single specialty groups to 24.0% of patients at specialist groups were managed with observation (Figure 4). Observation increased with time across all practice types aside from hospital-owned practices, by up to 7.9%. Radiation therapy was utilized for 24.7% of patients at hospital-owned practices to 44.2% of patients at large single specialty groups. Radiation therapy use was the highest for patients managed in large single specialty (p<0.001) and specialist groups (p = 0.10). Hospital-owned practices had the lowest utilization of this modality (p<0.001). Surgery, instead, was most frequently utilized by hospital-owned practices with 33.5% (p<0.001) of patients treated using this approach. Hospital-owned practices increased surgical utilization by 5.7% during the study period. Solo practices treated patients with surgery least frequently (15.3%) (p<0.001). Of note, between 21.4% and 29.1% of men with incident diagnoses of prostate cancer were treated with other therapies, like ablative therapy and brachytherapy, as well as hormonal therapies. The percentage decreased across the study period. Men treated with other therapies comprised 8.0% of patients at specialist groups and 14.7% of patients at solo practices. Finally, the sensitivity analysis on treatment type for urologists who practice in only one TIN was qualitatively similar to that for all urologists (Supplementary Figure 1).
Figure 4:

The percent of patients treated with observation, radiation therapy, surgery, and other therapies among practice types from 2010 to 2015.
DISCUSSION
Our findings suggest urologists are shifting their practice context from smaller, privately owned organizations to larger, multispecialty and hospital-owned groups. The number of hospital-owned practices and multispecialty groups as well as number of urologists within these groups has expanded rapidly, yet the plurality of practices continues to be solo practices. These changes are accompanied by practice specific trends in the management of prostate cancer with members of hospital-owned practices more frequently utilizing surgery, and members of large single specialty groups more frequently utilizing radiation therapy. Collectively, these findings suggest urologist and urology practices are susceptible to national trends of consolidation, and adds to a growing body of literature suggesting the treatment of prostate cancer is related to practice organization.
Prior studies characterize the shift in practice organization occurring nationally across many specialties.2,3,7,11,15 One study found that only one third of practices were comprised of ten providers or fewer by 2015.11 Another study identified an increase in the market share of hospital-owned practices, with surgical and medical subspecialties witnessing the greatest changes, compared to primary care.15 Our results are consistent with these trends, as the proportion of solo practices has decreased while that of hospital-owned practices and multispecialty groups has increased. Although subspecialty groups are thought to be resistant to national trends,11 our data confirms that in this domain, urology practices mirror primary care groups with a shift of urology groups toward larger and more consolidated practices.15 Perhaps the tradeoffs associated with consolidation (e.g., established referral networks, reduced administrative burden) are increasingly attractive regardless of specialization. Furthermore, we identified a slight increase in the total number of urologists serving the United States growing Medicare population. This finding is reassuring given a growing Medicare population and an aging urologist workforce.26
Beyond the economic and policy considerations of these trends, practice organization is important for physicians and patients. A variety of studies have linked urologists’ practice organization to treatment choice and costs of care for prostate cancer.14,16,17 For example, up to 90% of unexplained variability in observation has been attributed to characteristics of the treatment facility, including patient volume and its status as an academic center.27 While 12% of patients were managed with observation, rates were significantly higher among patients treated at academic programs and high volume centers. Our study also reveals variability in utilization of observation with rates between 20.8% and 24.0%, with multi-specialty groups and hospital-owned practices most likely to use observation. Further work to understand geographic variation in urologist workforce and practice distribution, and implications for cancer care access and outcomes, appears warranted particularly within a paradigm shift towards population health management.26,28
The study findings should be considered in the context of several limitations. First, the present study is a descriptive analysis only, and thus no causation is implied. Additionally, the study data was limited to patients who are Medicare beneficiaries, as well as physicians and practices submitting Medicare claims. Nonetheless, the majority of patients with diagnosed with prostate cancer are Medicare enrollees.29 Second, the data set did not include information on disease characteristics, thus some of the observed differences may be secondary to differences in disease severity. While variation in disease stage is possible in small samples of patients or practices, this is unlikely in the national cohort described here. Further, previous work using SEER-Medicare data demonstrated no meaningful differences in cancer stage and grade among men managed by different types of urology practices.16 Further, the group type labels we used are established and consistent with other studies in the growing body of literature on this topic.16,19,30 The identification of hospital-owned practices, for example, is derived from prior work.23 The algorithm we used to identify these groups relies on billing place of service codes. These codes strongly influence the degree of reimbursement received for evaluation and management services. Thus, practices are incentivized to bill office visits with a “hospital-outpatient department” place of service when they have the opportunity to do so. We thus anticipate these estimations of hospital-owned practices to be accurate.
CONCLUSIONS
In summary, our study suggests that urologists are shifting from smaller, independent groups to larger, multispecialty or hospital-owned practices. This work characterizes the impact of systemic pressures and national trends within the field. Practice organization has been shown to impact treatment type for patients with prostate cancer. Improving our understanding of urologist practice organization provides insight into factors impacting treatment utilization. These trends, within the larger context of ongoing changes in the organization and delivery of health care, can inform further study and policy interventions to control the spending on care.
Supplementary Material
HIGHLIGHTS.
The number of urologists increased from 9,305 to 9,570, while the number of urology practices decreased from 3,588 to 2,861 between 2010 and 2016.
The proportion of urologists in a multispecialty groups increased from 17.1% in 2010 to 28.2%% in 2016, while those within solo practices declined from 26.2% in 2010 to 15.8% in 2016.
A higher proportion of patients at hospital-owned practices were treated with observation and surgery, while those at large single specialty practices were treated with radiation therapy.
Support/Financial Disclosures:
This study was supported by Agency for Healthcare Research and Quality R01HS025707. Dr. Skolarus is supported by National Cancer Institute R37CA222885 and R01CA242559.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest:
The authors report no conflicts of interest associated with the publication of this work.
REFERENCES
- 1.Muhlestein BDB, Smith NJ. Physician Consolidation : Rapid 2016;9(9):1638–1642. [DOI] [PubMed] [Google Scholar]
- 2.O’Malley AS, Bond AM, Berenson RA. Rising Hospital Employment of Physicians: Better Quality, Higher Cost? Issue Brief Cent Stud Health Syst Change 2011;(136):1–4. [PubMed] [Google Scholar]
- 3.Burns LR, Goldsmith JC, Sen A. Horizontal and Vertical Integration of Physicians: A Tale of Two Tails Vol 15. Emerald Group Publishing Limited; 2013. doi: 10.1108/S1474-8231(2013)0000015009 [DOI] [PubMed] [Google Scholar]
- 4.Casalino LP, Ramsay P, Baker LC, Pesko MF, Shortell SM. Medical Group Characteristics and the Cost and Quality of Care for Medicare Beneficiaries. Health Serv Res 2018;53(6):4970–4996. doi: 10.1111/1475-6773.13010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liebhaber A, Grossman JM. Physicians moving to mid-sized, single-specialty practices. Track Rep 2007;(18):1–5. [PubMed] [Google Scholar]
- 6.Kocher R, Sahni NR. Hospitals’ Race to Employ Physicians — The Logic behind a Money-Losing Proposition. N Engl J Med 2011;364(19):1790–1794. [DOI] [PubMed] [Google Scholar]
- 7.Casalino LP, Pham H, Bazzoli G. Growth of single-specialty medical groups. Health Aff 2004;23(2):82–90. doi: 10.1377/hlthaff.23.2.82 [DOI] [PubMed] [Google Scholar]
- 8.Pham HH, Devers KJ, May JH, Berenson R. Financial pressures spur physician entrepreneurialism. Health Aff 2004;23(2):70–81. doi: 10.1377/hlthaff.23.2.70 [DOI] [PubMed] [Google Scholar]
- 9.Machta RM, Maurer KA, Jones DJ, Furukawa MF, Rich EC. A systematic review of vertical integration and quality of care, efficiency, and patient-centered outcomes. Health Care Manage Rev 2019;44(2):159–173. doi: 10.1097/HMR.0000000000000197 [DOI] [PubMed] [Google Scholar]
- 10.Burns LR, McCullough JS, Wholey DR, Kruse G, Kralovec P, Muller R. Is the System Really the Solution? Operating Costs in Hospital Systems. Med Care Res Rev 2015;72(3):247–272. doi: 10.1177/1077558715583789 [DOI] [PubMed] [Google Scholar]
- 11.Muhlestein DB, Smith NJ. Physician consolidation: Rapid movement from small to large group practices, 2013–15. Health Aff 2016;35(9):1638–1642. doi: 10.1377/hlthaff.2016.0130 [DOI] [PubMed] [Google Scholar]
- 12.Gaynor M, Mostashari F, Ginsburg PB. Making health care marketswork competition policy for health care. JAMA - J Am Med Assoc 2017;317(13):1313–1314. doi: 10.1001/jama.2017.1173 [DOI] [PubMed] [Google Scholar]
- 13.Schneider EC, Hall CJ. Can the Merit-Based Incentive Payment System Deliver? 2017:708–710. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell JM. Urologists’ use of intensity-modulated radiation therapy for prostate cancer. N Engl J Med 2013;369(17):1629–1637. doi: 10.1056/NEJMsa1201141 [DOI] [PubMed] [Google Scholar]
- 15.Nikpay S, Richards M, Penson D. Hospital-Physician Consolidation Accelerated in the Past Decade in Cardiology, Oncology. Health Aff 2018;37(7):1123–1127. doi: 10.1097/01.JU.0000553049.21054.37 [DOI] [PubMed] [Google Scholar]
- 16.Hollenbeck BK, Kaufman SR, Yan P, et al. Urologist Practice Affiliation and Intensity-modulated Radiation Therapy for Prostate Cancer in the Elderly. Eur Urol 2018;73(4):491–498. doi: 10.1016/j.eururo.2017.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bekelman JE, Suneja G, Guzzo T, Pollack CE, Armstrong K, Epstein AJ. Effect of practice integration between urologists and radiation oncologists on prostate cancer treatment patterns. J Urol 2013;190(1):97–101. doi: 10.1016/j.juro.2013.01.103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Modi PK, Herrel LA, Kaufman SR, et al. Urologist Practice Structure and Spending for Prostate Cancer Care. Urology 2019;130:65–71. doi: 10.1016/j.urology.2019.03.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Modi PK, Kaufman SR, Herrel LA, et al. Practice-Level Adoption of Conservative Management for Prostate Cancer. J Oncol Pract 2019;15(10):e863–e869. doi: 10.1200/jop.19.00088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Modi PK, Yan P, Hollenbeck BK, et al. Urologist Practice Structure and Quality of Prostate Cancer Care. Urol Pract 2019:in press. doi: 10.1097/upj.0000000000000123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Medicare Data on Provider Practice and Specialty (MD-PPAS) Centers for Medicare & Medicaid Services. https://www.resdac.org/cms-data/files/md-ppas. Published2017.
- 22.Hollenbeck BK, Bierlein MJ, Kaufman SR, et al. Implications of Evolving Delivery System Reforms for Prostate Cancer Care. Am J Manag Care 2016;22(9):569–575. [PMC free article] [PubMed] [Google Scholar]
- 23.Neprash HT, Chernew ME, Hicks AL, Gibson T, Michael McWilliams J. Association of financial integration between physicians and hospitals with commercial health care prices. JAMA Intern Med 2015;175(12):1932–1939. doi: 10.1001/jamainternmed.2015.4610 [DOI] [PubMed] [Google Scholar]
- 24.Sammon JD, Trinh QD, Menon M. Use of advanced treatment technologies among men at low risk of dying from prostate cancer. BJU Int 2014;114(2):166–167. doi: 10.1111/bju.12547 [DOI] [PubMed] [Google Scholar]
- 25.Modi PK, Kaufman SR, Qi J, et al. National Trends in Active Surveillance for Prostate Cancer: Validation of Medicare Claims-based Algorithms. Urology 2018;120:96–102. doi: 10.1016/j.urology.2018.06.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Skolarus TA, Hofer TP, Montgomery JS, et al. Urologist Workforce Variation Across the VHA. Fed Pract 2015;32(3):18–22. [PMC free article] [PubMed] [Google Scholar]
- 27.Löppenberg B, Friedlander DF, Krasnova A, et al. Variation in the use of active surveillance for low-risk prostate cancer. Cancer 2018;124(1):55–64. doi: 10.1002/cncr.30983 [DOI] [PubMed] [Google Scholar]
- 28.Odisho AY, Cooperberg MR, Fradet V, Ahmad AE, Carroll PR. Urologist density and county-level urologic cancer mortality. J Clin Oncol 2010;28(15):2499–2504. doi: 10.1200/JCO.2009.26.9597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Herget KA, Patel DP, Hanson HA, Sweeney C, Lowrance W t. Recent decline in prostate cancer incidence in the United States, by age, stage, and Gleason score. Cancer Med 2016;5(1):136–141. doi: 10.1002/cam4.549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Welch WP, Cuellar AE, Stearns SC, Bindman AB. Proportion of physicians in large group practices continued to grow in 2009–11. Health Aff 2013;32(9):1659–1666. doi: 10.1377/hlthaff.2012.1256 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


