Abstract
Background
Health care workers are at a higher risk of getting infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) than the general population. Knowledge about medical students’ exposure to SARS-CoV-2 is lacking. Thus, we measured the prevalence of SARS-CoV-2 antibodies in a cohort of Danish medical students.
Methods
We invited all medical students at the University of Copenhagen (UCPH) to participate. Students underwent venous blood sampling and a questionnaire about work-life behaviors possibly associated with SARS-CoV-2 exposure and coronavirus disease 2019 (COVID-19) symptoms. Samples were analyzed for total immunoglobulin G (IgG) antibodies against SARS-CoV-2, and seropositive samples were screened for IgG, immunoglobulin M, and immunoglobulin A antibodies. We determined associations between seropositivity and clinical and social activities and self-reported symptoms.
Results
Between October 19 and 26, 1120 students participated in the questionnaire and 1096 were included. Of all included, 379 (34.58%) were seropositive. Seropositivity was associated with attendance at 2 parties at UCPH, on February 29 and March 6, 2020 (odds ratio [OR], 5.96; 95% CI, 4.34–8.24; P < .001). Four hundred sixty-one students (42.06%) worked with COVID-19 patients, which was significantly associated with seropositivity (OR, 1.38; 95% CI, 1.03–1.85; P = .033). The symptom most associated with seropositivity was loss of smell and/or taste (n = 183 of all, 31.35%; OR, 24.48; 95% CI, 15.49–40.60; P < .001). Bachelor’s students were significantly more likely to be seropositive than Master’s students (42.28% vs 16.87%; P < .001).
Conclusions
Medical students have the highest reported seropositivity in the Danish health care system. In this cohort of students at UCPH, seropositivity was associated with social behavior markers and, to a lesser extent, with self-reported contact with SARS-CoV-2-infected patients.
Keywords: anti-SARS-CoV-2 antibodies, coronavirus disease 2019, health care workers, medical students, seroprevalence
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was declared a pandemic by the World Health Organization on March 11, 2020 [1], and as of February 5, 2021, more than 136 million have been infected. Around 2.9 million have died because of COVID-19 [2].
The Danish medical school system has a Bachelor’s component and a Master’s component, each with a duration of 3 years. Both the Bachelor’s and Master’s are subdivided into 6 semesters, each of which equates to half a year of study. Every 6 months, a new group of medical students start at the University of Copenhagen (UCPH) [3]. Danish medical students are employed as health care workers in hospitals during their studies, especially during the pandemic [4]. Medical students assist the hospital departments in various functions such as acting as substitute health care workers in clinical departments, as viral testers (nasopharyngeal and throat swabs), and aiding in collecting blood samples for seroepidemiological studies from the very beginning of their studies [5]. Furthermore, a large part of the Master’s program at UCPH is based on clinical rotations at hospitals in the Capital Region of Denmark, including interacting with patients [3]. Consequently, medical students encounter asymptomatic individuals infected with SARS-CoV-2 as well as COVID-19 patients.
An early study showed that Danish medical students employed directly by the hospitals were a high-risk group, with a SARS-CoV-2 seroprevalence of 14.97% [6]. However, as most medical students are not employed at hospitals, the overall seroprevalence of medical students is unknown. They are also excluded them from the regional guidelines for systematic screening with nasopharyngeal and throat swabs for SARS-CoV-2 of health care workers. Therefore, a potential unreported number of SARS-CoV-2 outbreaks among medical students is possible.
Additionally, medical students are in the age group with the highest incidence of positive SARS-CoV-2 polymerase chain reaction tests in Denmark [7]. On March 6, 2020, there was a party at the Faculty of Health and Medical Sciences at UCPH, where it was later confirmed that at least 1 SARS-CoV-2-infected medical student had attended [8], and it has been suspected that said party was a superspreader event [9]. This also raises the possibility of the disease spreading rapidly [10].
We aimed to examine the prevalence of antibodies against SARS-CoV-2 in medical students at UCPH and investigate the seroprevalence in relation to their work and social life.
METHODS
Timeline
The first Danish COVID-19 patient was diagnosed on February 28, 2020. On March 11, 2020, there was a partial lockdown of Denmark, which included the UCPH. On April 15, 2020, restrictions were partially lifted [11]. Mask mandates were first announced during the summer of 2020. However, masks had been mandatory in all contact with patients suspected of having COVID-19 since the start of the pandemic [12]
Participants
All medical students enrolled at UCPH (n = 3673) [13] were offered the possibility to participate in this observational cohort study. Medical students were invited by email via their university email, sent out by the Union of Danish Medical Students (FADL).
Blood sampling took place between October 19 and 26 at 5 test locations. In relation to the sampling, participants were asked to complete a questionnaire regarding symptomatology, information about demographics, type of work, history of contact with COVID-19-infected patients, social life, and general habits during the pandemic. A translated version of the questionnaire is presented in the Supplementary Methods. The participants did not know their enzyme-linked immunosorbent assay (ELISA) results from our study before filling out our questionnaire. The questionnaire was made in Research Electronic Data Capture (RedCap), and all the data collected were also managed by REDCap. REDCap is a secure, web-based tool hosted on servers owned by the Capital Region [14, 15].
Blood Samples
A venous blood sample of 6 mL was drawn from the antecubital region from all participants. Serum was stored at –80ºC until analysis and only thawed once.
A commercial immunoglobulin (Ig) ELISA method (Beijing Wantai Biological Pharmacy Enterprise, Beijing, China) was used for determining seropositivity by measuring total antibodies to SARS-CoV-2 as previously described [16, 17]. The assay has a sensitivity of around 97% with a specificity of 99.5% in COVID-19 convalescent individuals. The samples that tested positive for total antibodies to SARS-CoV-2 went on to be analyzed using a direct ELISA method to detect IgG, IgA, and IgM levels, as previously described [18]. Both ELISA assays used in this study use the RBD of recombinant SARS-CoV-2 spike protein to target antibodies [16, 18]. The IgG, IgA, and IgM direct ELISAs have a sensitivity and specificity of 94.3% and 99.5%, 63.4% and 99.3%, and 61.4% and 99.1%, respectively. The performance of the IgG, IgA, and IgM assays was tested in samples from convalescent individuals obtained within 11 weeks of disease onset [18].
Patient Consent
The study complied with the Declaration of Helsinki II and was approved by the regional ethics committee of the Capital Region (H-20055767) and by the Danish Data Protection Authorities (P-2020–92). Following the guidelines for providing oral and written information, all patients gave written informed consent to participate in the study.
Statistics
The primary outcome was the proportion of the study population with a positive antibody test for SARS-CoV-2. Calculations were done using R, version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria). Baseline characteristics and exposures were presented as number (%) for factors and mean (SD) or median (interquartile range [IQR]) for numeric variables, as appropriate.
To account for the expected clustering effect of medical students socializing within the semester, potential exposure variables (eg, working with COVID-19 patients) were explored using multiple logistic regression models adjusted for the semester at the medical school as well as age and sex. The results of these regressions are reported as odds ratios (ORs) of seropositivity and presented with 95% CIs. A P value of <.05 was considered significant.
Similarly, we tested the association between symptoms and seropositivity in univariate logistic regression models. Further, as COVID-19-like symptoms were expected to be common (eg, runny nose) in the background population, we wished to estimate the prevalence of patients with SARS-CoV-2 antibodies without symptoms attributable to COVID-19. We calculated the probability of having symptoms of COVID-19 adjusted for the probability of seronegative participants having symptoms. This was done as previously described [19], and details can be seen in the Supplementary Data.
Further, to look at exposures independent of the 2 parties, we chose to perform repeat analyses on the subgroup of participants who did not participate in any of the parties.
RESULTS
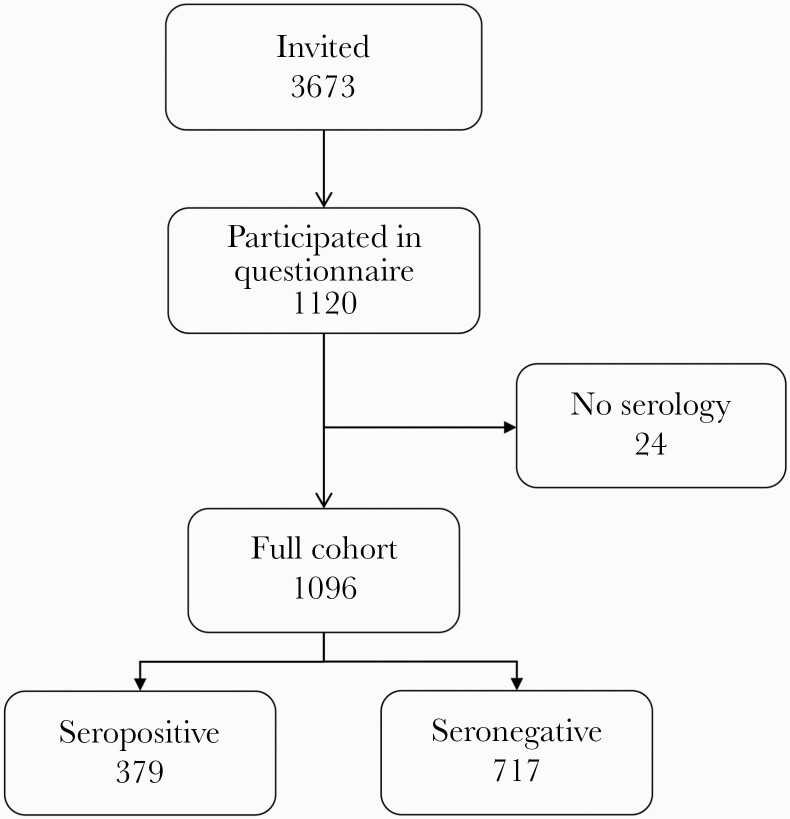
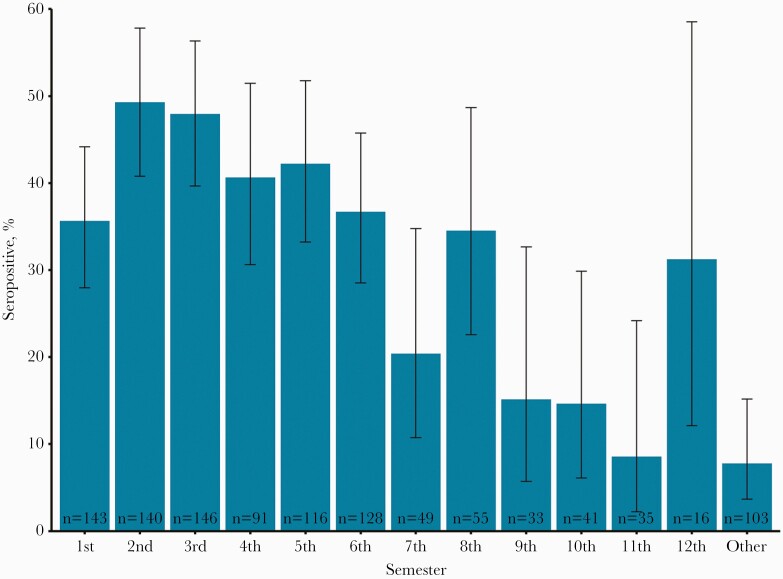
From October 19 to 26, a total of 1120 out of 3673 medical students (30.5%) filled out the questionnaire, and of these 1096 had full serology performed and were included in the study (Figure 1 shows a CONSORT diagram of the study population). The median age (IQR) was 23.5 (22.1–25.3) years, and 782 (71.35%) were female. The medical students at UCPH have the following distribution: 1313 women and 595 men at the Bachelor’s level, and 1130 women and 635 men at the Master’s level. We have a slight but significant increase compared to the overall student population, of whom 2443 of 3673 (67%) were female (P = .003). Of the included medical students, 379 (34.58%; 95% CI, 31.82%–37.45%) had anti-SARS-CoV-2 antibodies, based on the SARS-CoV-2 ELISA test from Wantai. Among the seropositive, 288 (76.0%; 95% CI, 71.4%–80.0%) had detectable IgG antibodies, 10 (2.6%; 95% CI, 1.4%–4.8%) had IgM antibodies, 58 (15.3%; 95% CI, 12.0%–19.3%) had IgA antibodies, and 88 (23.2%; 95% CI, 19.3%–27.7%) were seronegative on the direct test (Supplementary Figure 1 shows the distribution of antibodies on the direct test). Table 1 shows baseline characteristics of the cohort divided according to seropositivity. The seropositive participants were significantly younger (23.48 vs 24.3; P < .001), more likely to be male (41.08% for men vs 31.97% for women; P = .01), and had a significantly higher BMI (22.7 vs 22.2; P = .014). Figure 2 shows the percent seropositive for each semester of medical school. Bachelor’s students (1st–6th-semester students) were significantly more likely to be seropositive than Master’s students (42.28% vs 16.87%; P < .001).
Figure 1.
CONSORT diagram.
Table 1.
Baseline Characteristics
| Seronegative | Seropositive | P | |
|---|---|---|---|
| No. | 717 | 379 | |
| Age, median [IQR], y | 23.8 [22.2–25.6] | 23.1 [21.9–24.5] | <.001 |
| Female, No. (%) | 532 (74.2) | 250 (66.0) | .005 |
| Body mass index, mean (SD), kg/m2 | 22.2 (2.6) | 22.7 (2.9) | .011 |
| Tobacco use, No. (%) | 64 (8.9) | 38 (10.0) | .585 |
| Asthma, No. (%) | 76 (10.6) | 38 (10.0) | .835 |
| Diabetes, No. (%) | 8 (1.1) | 3 (0.8) | .757 |
| Other chronic lung disease, No. (%) | 2 (0.3) | 1 (0.3) | 1.000 |
| Heart disease, No. (%) | 3 (0.4) | 1 (0.3) | 1.000 |
| Kidney disease, No. (%) | 0 (0.0) | 2 (0.5) | .119 |
| Weakened immune system, No. (%) | 5 (0.7) | 5 (1.3) | .328 |
| Hypertension, No. (%) | 5 (0.7) | 0 (0.0) | .171 |
| Allergies, No. (%) | 224 (31.2) | 96 (25.3) | .043 |
Seropositive was defined using the Wantai total Ig assay; tobacco use was defined as active smoker or user of snuff.
Abbreviations: Ig, immunoglobulin; IQR, interquartile range.
Figure 2.
Risk of seropositivity according to semester. Error bars indicate the 95% CIs.
Exposures
Table 2 shows potential exposures divided according to seropositivity. Similarly, Supplementary Tables 1 and 2 show potential exposures for Master’s and Bachelor’s students. To correct for the expected clustering effect associated with socializing with other medical students during the semester, a multivariate logistic model was used to determine the significance of the exposures. The results of this logistic regression are shown in Table 3. Overall, the association of seropositivity was greatly increased for participants of the 2 parties held on February 29, 2020, and March 6, 2020, at the Faculty of Health and Medical Sciences, UCPH. At the party on February 29, 272 (24.84%) individuals from the cohort participated, and of these, 161 (59.19%) were seropositive, resulting in an OR of 2.45 (95% CI, 1.74–3.45; P < .001). Similarly, for the party on March 6, 290 (26.48%) individuals from the cohort participated, and of these, 181 (62.41%) were seropositive, resulting in an OR of 3.62 (95% CI, 2.64–5.00; P < .001). Attending either party was associated with an OR of 5.84 (95% CI, 4.26–8.06; P < .001), while attending both parties was associated with an OR of 6.41 (95% CI, 4.11–10.13; P < .001). Working with COVID-19 patients was common in the cohort (n = 461, 42.06%) and was associated with a significantly increased risk of seropositivity, with medical students who reported working with COVID-19 patients having an OR of 1.40 (95% CI, 1.05–1.88; P = .024). Age and sex were not significant predictors of seropositivity.
Table 2.
Exposures and Risk
| Seronegative | Seropositive | P | |
|---|---|---|---|
| No. | 717 | 379 | |
| Participated in party on 3/6, No. (%) | 109 (15.2) | 181 (47.9) | <.001 |
| Participated in party on 2/29, No. (%) | 111 (15.5) | 161 (42.6) | <.001 |
| Participated in either of the 2 parties, No. (%) | 170 (23.7) | 257 (67.8) | <.001 |
| Hours at institute, median [IQR] | 8.00 [0–25] | 24.00 [6–30] | <.001 |
| Any work, No. (%) | 588 (82.0) | 335 (88.4) | .007 |
| Any work with COVID-19 patients, No. (%) | 269 (37.5) | 192 (50.7) | <.001 |
| Had work testing for COVID-19 (swab), No. (%) | 48 (49.0) | 42 (57.5) | .283 |
| No. of contacts/d, No. (%) | .303 | ||
| 1–2 | 199 (27.8) | 119 (31.5) | |
| 3–5 | 276 (38.5) | 142 (37.6) | |
| 6–10 | 146 (20.4) | 60 (15.9) | |
| 11–15 | 52 (7.3) | 27 (7.1) | |
| 16–20 | 24 (3.3) | 13 (3.4) | |
| >20 | 20 (2.8) | 17 (4.5) | |
| >10 contacts/d, No. (%) | 96 (13.4) | 57 (15.1) | .464 |
| Bachelor’s student, No. (%) | 441 (61.5) | 323 (85.2) | <.001 |
| Travel to area of risk, No. (%) | 67 (9.3) | 44 (11.6) | .248 |
| Austria, No. (%) | 14 (2.0) | 7 (1.8) | 1.000 |
| Italy, No. (%) | 12 (1.7) | 4 (1.1) | .598 |
Seropositive was defined using the Wantai total Ig assay; travel risk areas were defined as travel to Italy, France, Austria, or China during the period January 1 to April 1 (no one traveled to China).
Abbreviations: COVID-19, coronavirus disease 2019; IQR, interquartile range.
Table 3.
Results of a Multivariate Logistic Model of Exposures and Baseline Characteristics
| OR | 95% CI | P | |
|---|---|---|---|
| Age | 0.99 | 0.94–1.04 | .787 |
| Female | 0.77 | 0.56–1.05 | .099 |
| Working with COVID-19 | 1.4 | 1.05–1.88 | .024 |
| Participated in party on 2/29 | 2.45 | 1.74–3.45 | <.001 |
| Participated in party on 3/6 | 3.62 | 2.64–5 | <.001 |
| Hours at institute (0–2 h, ref) | 1 | 1.00–1.00 | |
| Hours at institute (2–25 h) | 1.14 | 0.74–1.75 | .543 |
| Hours at institute (>25 h) | 1.4 | 0.87–2.25 | .163 |
In addition to the abovementioned variables, the model was adjusted for the semester of the student (data not shown).
Abbreviations: COVID-19, coronavirus disease 2019; OR, odds ratio.
The number of hours spent at the institute (the Faculty of Health and Medical Sciences, UCPH) and the number of social contacts per day were not significant predictors of seropositivity. Likewise, there was no increased risk for medical students who had traveled to either of the countries where the SARS-CoV-2 virus was most prevalent in the early spring (France, Italy, Austria, and China). However, there were relatively few instances of travel to these countries. No medical students traveled to China during the study period.
The subanalysis results looking at participants who did not participate in either of the 2 parties can be seen in Supplementary Table 3. Overall, the risks were similar. However, in this group, travel to an area of risk was significantly associated with seropositivity (OR, 2.37; 95% CI, 1.15–4.72; P = .016).
Symptoms
Having any illness during the period was significantly associated with seropositivity (596 of all, 54.48%), with an OR of 4.80 (95% CI, 3.62–6.40; P < .001). Still, 22.22% of seropositive participants reported no illness during the period. The symptom most strongly associated with seropositivity was loss of smell and/or taste (n = 182 of all, 16.61%), with an OR of 24.48 (95% CI, 15.49–40.60; P < .001). Table 4 shows the association of seropositivity for participants who reported any illness, fever, or loss of smell and/or taste and those who reported at least 3 symptoms. All reported symptoms and associated risk are shown in Supplementary Table 4.
Table 4.
Selected Symptoms and Seropositivity
| All | % | Seropositive | % | OR | 95% CI | P | |
|---|---|---|---|---|---|---|---|
| Any illness | 596 | 54.48 | 294 | 77.78 | 4.8 | 3.62–6.4 | <.001 |
| Fever | 345 | 31.48 | 193 | 50.92 | 3.86 | 2.95–5.06 | <.001 |
| Loss of taste/smell | 182 | 16.61 | 161 | 42.48 | 24.48 | 15.49–40.6 | <.001 |
| At least 3 symptoms | 526 | 47.99 | 264 | 69.66 | 3.99 | 3.06–5.22 | <.001 |
Abbreviation: OR, odds ratio.
When adjusting for the prevalence of symptoms among seronegative participants, 61.7% of seropositive participants had symptoms attributable to their infection.
DISCUSSION
Our study showed that medical students at UCPH had a high seroprevalence of antibodies against SARS-CoV-2 in October 2020 compared with earlier studies of the general Danish population or other health care workers [6, 20]. In August 2020, the seroprevalence of SARS-CoV-2 antibodies in Denmark was 4.6% in the age group 20–29 years [21]. A review from November 2020 showed an overall average seroprevalence of SARS-CoV-2 antibodies among health care workers on a global scale of 8.7% [22]. However, it is difficult to directly compare medical students and other health care workers because of the possible difference in social behaviors and working environments. Danish medical students often work in multiple hospitals and hospital wards. We found that the risk of seropositivity was greatly increased for individuals who attended 2 parties held on February 29, 2020, and March 6, 2020, at the Faculty of Health and Medical Sciences, UCPH, before the lockdown of Denmark on March 11. This could potentially have been a superspreader event [9], much like the ones seen in the United States [23], Thailand [24], etc. These superspreader events can be very problematic, especially as one-fifth of the participants at the social gatherings for medical students did not have any disease symptoms. Therefore, these students were able to work at various hospitals all over the Capital Region of Denmark.
We detect that the overall association of seropositivity was increased by the number of hours spent at UCPH. The seropositive group spent a median of 24 hours at the institute, while the seronegative group only spent a median of 8 hours. At the UCPH, there are shared study halls and a shared canteen area. Furthermore, a notable amount of medical education consists of shared class lectures. These locations can potentially have been places with increased risk of getting infected with SARS-CoV-2. The Master’s program in medicine at UCPH is mainly clinically based education at hospitals and the Bachelor’s program mainly occurs at the UCPH, which could also have influenced the difference in seropositivity between the groups. The difference in where the education takes place can also be seen by the number of hours the Master’s students and Bachelor’s students spent at UCPH. However, attendance at the 2 parties was higher among the Bachelor’s students than the Master’s students. There was no significant correlation between social interaction in either the Bachelor’s or Master’s group.
From the first semester, medical students can work in the Danish health care system in various functions at different hospitals via the Union of Danish Medical Students’ employment agency (FADL’s vagtbureau). This gives great flexibility but carries a risk as the medical students move around.
Loss of taste and/or smell was a common symptom of COVID-19 infection in our study, and it was highly associated with seropositivity, with an OR of 24.48 (95% CI, 15.49–40.60; P < .001). The percentage of medical students who lost their taste and/or smell during the study period was considerably higher than what has previously been reported in other studies of specific symptoms and seropositivity (20.9% vs 16% vs 15%) [25–27]. A considerable number of medical students with antibodies did not exhibit any symptoms, which raises the risk of asymptomatic disease transmission.
Among those positive, in the total Ig ELISA, only around 76% were seropositive using the direct ELISA. This discrepancy in seropositivity may be due to the total Ig assay’s greater sensitivity (by including all antibody isotypes) than the direct IgG ELISA format [28]. Furthermore, it is important to note that the Wantai Ig assay is intended for the qualitative detection of total antibodies to SARS-CoV-2, whereas the direct ELISAs are quantitative. Therefore, due to, for example, antibody waning, low IgG titers would possibly be under the limit of detection by the direct ELISA, as the blood sampling took place up to 7 months after a suspected COVID-19 infection [28, 29].
In this study, we found a relatively high association of seropositivity among participants who recalled having had a runny and/or stuffed nose (OR, 1.98; 95% CI, 1.51–2.58). This is similar to a Swedish study of health care workers that reported an OR of seropositivity of runny nose of 1.68 (95% CI, 1.33–2.10) [30]. We think there are several reasons for the relatively strong correlation to this otherwise unspecific symptom. First, the cohorts investigated here are relatively young and healthy and report fewer everyday episodes of illness. Second, the period from the outbreak of the pandemic to the study was mainly during the summer. Thus, there were fewer episodes of seasonal rhinitis. Third, there could be an element of recall bias, as participants could have been more likely to recall having had symptoms if they also tested positive for COVID-19 during their illness.
The strengths of this study include the large sample size and a high percentage of participants who completed the questionnaire. Despite this, participation was low relative to the number of medical students we invited (30.5% of the medical students at UCPH participated). Some medical students were aware of their antibody status before participating in the study, which could have promoted a selection bias. However, it is difficult to know which way this has affected our study. Those who knew they were positive for SARS-CoV-2 antibodies might not want to participate, since they already knew their result.
In contrast, medical students who had suspected infection might be more eager to participate. All medical students were invited to participate regardless of previous antibody status or presence of symptoms. The study was limited by relying on participants’ retrospectively self-reported symptoms, social behavior, contact with COVID-19 patients, etc., which allows for an unknown amount of misclassification. Another limitation is the possibility that many of the medical students had SARS-CoV-2 7 months earlier than the samples were collected, which creates a risk of an uncertain seroprevalence estimate due to the possibility of antibody waning. Furthermore, some of the medical students had had their antibodies tested before the study [6], which means that recall bias could have influenced their answers relating to symptoms, number of contacts, social behavior, etc., on our questionnaire.
In conclusion, we found that medical students at UCPH have an overall high seroprevalence of SARS-CoV-2 antibodies compared with other groups of health care workers and the general Danish population. The risk of infection among medical students appears to be partly related to working with COVID-19-infected patients, but to a greater extent related to their social behavior. This study shows a strong correlation between seropositivity and attending the suspected superspreader events at UCPH. However, due to the inherent limitations of the study, we can only speculate that a substantial number of the medical students included in this work were infected with SARS-CoV-2 at said parties. The parties could also signify proxies for increased risk behavior for contracting COVID-19 in the study population. A large proportion of the medical students showed no symptoms related to COVID-19 and therefore posed a risk of being asymptomatic carriers of the infection. This study highlights the importance of knowing the risks associated with both social and work-related transfer of SARS-CoV-2 among medical students at UCPH and the value in limiting large social gatherings during this pandemic.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments
The authors would like to thank Camilla Xenia Holtermann Jahn, Sif Kaas Nielsen, and Jytte Bryde Clausen, from the Laboratory of Molecular Medicine at Rigshospitalet, for their excellent technical assistance. The authors want to thank all the volunteer medical students from UCPH who participated in the study. The authors would also like to thank FADL’s vagtbureau for putting their highly trained staff at our disposal to help take the blood samples.
Financial support. This work was supported by grants from the Carlsberg Foundation (CF20-476 0045), and the Novo Nordisk Foundation (NFF205A0063505 and NNF20SA0064201). The funders did not influence the study design, conduct, or reporting.
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Author contributions. J.R.M., J.P.S.N., K.F., C.B.H., P.B.N., T.L., and R.B.H. organized sample collection and analyzed the data; J.R.M., J.P.S.N., P.G., and K.I. wrote the paper with input from all co-authors. All authors approved the final version of the manuscript.
References
- 1.World Health Organization. Rolling updates on coronavirus disease (COVID-19).2020. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Accessed 2 December 2020.
- 2.World Health Organization. WHO coronavirus disease (COVID-19) dashboard.2021. Available at: https://covid19.who.int/. Accessed 14 April 2021.
- 3.University of Copenhagen. Undervisning og opbygning. Available at: https://studier.ku.dk/kandidat/medicin/undervisning-og-opbygning/. Accessed 21 December 2020.
- 4.Rasmussen S, Sperling P, Poulsen MS, et al. . Medical students for health-care staff shortages during the COVID-19 pandemic. Lancet 2020; 395:e79–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Union of Danish Medicial Students employment agency (FADL’s vagtbureau). vagtbureau Fs. Om vagtbureauet. 2020. Available at: https://fadlvagt.dk/om-vagtbureauet/. Accessed 2 December 2020.
- 6.Iversen K, Bundgaard H, Hasselbalch RB, et al. . Risk of COVID-19 in health-care workers in Denmark: an observational cohort study. Lancet Infect Dis 2020; 20:1401–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Statens Serum Institut. COVID-19 - Danmark.2020. Available at: https://experience.arcgis.com/experience/aa41b29149f24e20a4007a0c4e13db1d. Accessed 2 December 2020.
- 8.Danish Patient Safety Authority. COVID-19-smittet var til fredagsbar på Panum Instituttet i København fredag 6. marts.2020. Available at: https://stps.dk/da/nyheder/2020/covid-19-smittet-var-til-fredagsbar-paa-panum-instituttet-i-koebenhavn-fredag-6-marts/?fbclid=IwAR0FFElUCtLHSMtPh3jg-mOWN-yO7HQciv_hg8Z5GH1DrIR2Hb5L7CMLAYw#. Accessed 2 December 2020.
- 9.Statens Serum Institut. Opdateret notat vedrørende kvalitativ risikovurdering af diskoteker, spillesteder og nattelivsamt større forsamlinger.2021. Available at: https://www.ssi.dk/-/media/ssi-files/kvalitativ-risikovurdering-af-diskoteker-spillesteder-og-natteliv-og-storre-forsamlinger_06082020.pdf?la=da. Accessed 2 March 2021.
- 10.Kochańczyk M, Grabowski F, Lipniacki T. Super-spreading events initiated the exponential growth phase of COVID-19 with ℛ0 higher than initially estimated. R Soc Open Sci 2020; 7:200786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jespersen S, Mikkelsen S, Greve T, et al. . Severe acute respiratory syndrome coronavirus 2 seroprevalence survey among 17 971 healthcare and administrative personnel at hospitals, prehospital services, and specialist practitioners in the central Denmark region. Clin Infect Dis. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sundhedsstyrelsen. Krav om mundbind i den kollektive trafik og særlige anbefalinger til personer i øget risiko. 2020. Available at: https://www.sst.dk/da/nyheder/2020/krav-om-mundbind-i-den-kollektive-trafik-og-saerlige-anbefalinger-til-personer-i-oeget-risiko?fbclid=IwAR2Px3uKKZj_7ia6XbWOJ4ExkCAM2DC__jhMF6oh6JTiWsz1wR1pZidKQ6Y. Accessed 5 March 2020.
- 13.University of Copenhagen. Bestand. 2021. Available at: https://us.ku.dk/studiestatistik/studiestatistikker/bestand/?fbclid=IwAR11VkxjefOzUFQhrekNzrms2U5KBsN7TM4PJdHrCO_CP39Y4z_BJsOa4lY. Accessed 13 January 2021.
- 14.Harris PA, Taylor R, Minor BL, et al. ; REDCap Consortium . The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019; 95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, et al. . Research Electronic Data Capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harritshoej LH, Gybel-Brask M, Afzal S, et al. . Comparison of sixteen serological SARS-CoV-2 immunoassays in sixteen clinical laboratories. J Clin Microbiol. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weidner L, Gänsdorfer S, Unterweger S, et al. . Quantification of SARS-CoV-2 antibodies with eight commercially available immunoassays. J Clin Virol 2020; 129:104540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hansen CB, Jarlhelt I, Perez-Alos L, et al. . SARS-CoV-2 antibody responses are correlated to disease severity in COVID-19 convalescent individuals. J Immunol. In press. [DOI] [PubMed] [Google Scholar]
- 19.D’Souza M, Nielsen D, Svane IM, et al. . The risk of cardiac events in patients receiving immune checkpoint inhibitors: a nationwide Danish study. Eur Heart J. In press. [DOI] [PubMed] [Google Scholar]
- 20.Statens Serum Institut. Næsten en halv million danskere deltog i “Vi Tester Danmark”. Nu går fase 2 af projektet i gang.2020. Available at: https://www.ssi.dk/aktuelt/nyheder/2020/nasten-en-halv-million-danskere-deltog-i-vi-tester-danmark-nu-gar-fase-2-af-projektet-gar-i-gang. Accessed 21 December 2020.
- 21.Statens Serum Institut. Covid-19: den nationale prævalensundersøgelse.2020. Available at: https://covid19.ssi.dk/-/media/arkiv/dk/aktuelt/nyheder/2020/notat---covid-19-prvalensundersgelsen.pdf?la=da&fbclid=IwAR0YkCdkM-fRDv4Sc_JI9DLP2mMdONwq2HXmV-uqH_O8AxmCeWFjAebZOqU. Accessed 7 October 2020.
- 22.Galanis P, Vraka I, Fragkou D, et al. . Seroprevalence of SARS-CoV-2 antibodies and associated factors in health care workers: a systematic review and meta-analysis. J Hosp Infect. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lemieux JE, Siddle KJ, Shaw BM, et al. . Phylogenetic analysis of SARS-CoV-2 in Boston highlights the impact of superspreading events. Science. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chau NVV, Hong NTT, Ngoc NM, et al. . Superspreading event of SARS-CoV-2 infection at a bar, Ho Chi Minh City, Vietnam. Emerg Infect Dis. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foster KJ, Jauregui E, Tajudeen B, et al. . Smell loss is a prognostic factor for lower severity of coronavirus disease 2019. Ann Allergy Asthma Immunol 2020; 125:481–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lan FY, Filler R, Mathew S, et al. . COVID-19 symptoms predictive of healthcare workers’ SARS-CoV-2 PCR results. PLoS One 2020; 15:e0235460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee Y, Min P, Lee S, Kim SW. Prevalence and duration of acute loss of smell or taste in COVID-19 patients. J Korean Med Sci 2020; 35:e174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bal A, Pozzetto B, Trabaud MA, et al. . Evaluation of high-throughput SARS-CoV-2 serological assays in a longitudinal cohort of patients with mild COVID-19: clinical sensitivity, specificity and association with virus neutralization test. Clin Chem. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seow J, Graham C, Merrick B, et al. . Longitudinal observation and decline of neutralizing antibody responses in the three months following SARS-CoV-2 infection in humans. Nat Microbiol 2020; 5:1598–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rudberg AS, Havervall S, Månberg A, et al. . SARS-CoV-2 exposure, symptoms and seroprevalence in healthcare workers in Sweden. Nat Commun 2020; 11:5064. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.