Abstract
Background: Our aim in this study was to compare the results of video-assisted thoracoscopic surgery with those of open surgery regarding efficacy, morbidity, and long-term recurrence of bronchogenic cysts in light of the literature.
Methods: This study comprises the data of 51 patients whose pathological diagnosis revealed bronchogenic cyst after surgical excision between January 2010 and December 2016. There were two groups according to the type of resection: video-assisted thoracoscopic surgery (VATS) and thoracotomy.
Results: Of the patients included in the study, 25 (49%) were male and 26 (51%) were female. Their average age was 41.7 ± 14.1 years. While 14 patients (27.5%) were asymptomatic in the preoperative period, 37 patients (72.5%) had symptoms. The Charlson Comorbidity Index was 0 in 35 patients (68.6%) and 1 and above in 16 patients (31.4%). While 22 (43.1%) patients underwent cyst excision via VATS, 29 (56.9%) patients underwent thoracotomy. The average length of hospital stay was 1.77 ± 0.68 days for patients who had VATS, whereas it was 3.82 ± 3.3 days for patients who had thoracotomy (p <0.001).
Conclusion: VATS procedure is a safe method in the surgical treatment of bronchogenic cysts, with less hospitalization and similar recurrence rates.
Keywords: bronchogenic cyst, mediastinal lesions, VATS
Introduction
Bronchogenic cysts are the most common congenital anomaly of the mediastinum that develops due to the abnormal development of the tracheobronchial system in the embryonic period. Although it is more often seen in childhood, it can also be seen in adult patients. Bronchogenic cysts can be asymptomatic or can present with varied symptoms such as cough, dyspnea, hemoptysis, and difficulty in swallowing. Although there may be no symptoms in patients diagnosed with mediastinal bronchogenic cyst (MBC), symptoms due to compression of adjacent organs (mass effect), infection, hemoptysism, and rarely malignant transformation can be seen due to cyst growth. Therefore, surgical excision is accepted as the gold standard treatment method regardless of the symptoms in patients diagnosed with MBC.1) Videothoracoscopic surgery has been routinely used since the 90s. There are many different publications in the literature regarding complete excision and long-term results of VATS surgery.
Our aim in this study was to compare the results of video-assisted thoracoscopic surgery (VATS) with those of open surgery regarding efficacy, morbidity, and long-term recurrence of bronchogenic cysts in light of the literature.
Methods
This study comprises the data of 54 patients whose pathological diagnosis revealed bronchogenic cyst after surgical excision between January 2010 and December 2016. The data were retrospectively analyzed. Three patients who did not show up on follow-up examinations and whose data were not available were excluded from the study.
Preoperative evaluation
Physical examinations and detailed anamnesis of the patients were evaluated. Electrocardiography and standard laboratory tests were examined. A standard chest radiograph and computed tomography (CT) of the thorax were performed in all patients prior to surgery. Magnetic resonance imaging (MRI) was requested for those patients for whom additional radiological evaluation was considered for the diagnosis. The patients included in the study were divided into two groups according to the type of resection: VATS and thoracotomy.
Thoracotomy was preferred more frequently in patients with lesions 5 cm or more or in patients who had previous sequelae of lung parenchymal lesions or surgeons preferences. The comorbidities of the patients were classified according to the Charlson Comorbidity Index (CCI). The Maier Classification was used for the localization of the MBC.
Surgical technique
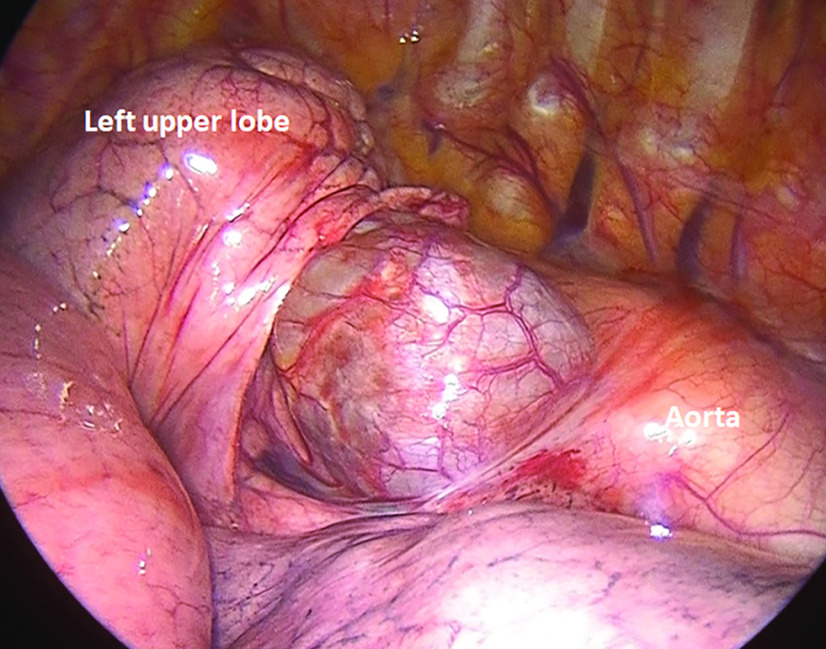
The patients in both groups were intubated under general anesthesia with a double-lumen endotracheal tube, providing selective lung ventilation. After positioning the patients in the lateral decubitus position, the thorax was entered through a 1 cm incision usually through the 7th or 8th intercostal space anterior axillary line for VATS, using a 30-degree telescopic camera (Karl Storz, Tuttlingen, Germany). Depending on the location of the lesion, 1 or 2 3-4 cm auxiliary port incisions were used. In patients who underwent thoracotomy, standard thoracotomy incisions were used according to the location of the lesion. In principle, complete excision was targeted in all patients without perforating the cyst (Fig. 1). In perforated cysts, the cyst wall was completely removed along with the surrounding tissue. In 1 patient undergoing VATS, thoracotomy was performed suspecting that the cyst could not be removed completely due to the diameter of the cyst. In our study, this patient was included in the thoracotomy group. After surgery, 1 chest tube was placed in the thoracic cavity. Histological examinations confirmed the diagnosis of MBC based on the existence of ciliated columnar epithelial lining.
Fig. 1. Intraoperative view of the posterior mediastinal cyst.
Postoperative follow-up
In all patients, the operation was terminated by placing 1 chest tube. The chest tubes of the patients were removed when the daily fluid drainage was below 100 cc/day. Complications were defined as undesired events that developed during hospitalization and in the first 30 days after discharge. Persistent air leak, atelectasis, and empyema were defined as complications.
Total excision (R0) was performed in all patients. All the patients had long-term follow-ups. During the study, all patients were contacted and called to the hospital for investigation of any recurrences.
Statistical analysis
Statistical analysis was performed using SPSS Windows 22.0 (IBM, Armonk, NY, USA). Numerical variables were evaluated as mean ± standard deviation and median (min–max), and categorical variables were evaluated by number and percentage. Parametric test assumptions (normality and homogeneity of variances) were checked before the groups were compared in terms of numerical variables. Whether there was a difference between the groups was examined by the t-test in dependent groups. Categorical values were analyzed by the Fisher’s exact test. Mann–Whitney U test was used to compare continuous variables. The significance level was taken as p <0.05 in the study.
Results
Of the patients included in the study, 25 (49%) were male and 26 (51%) were female. The average age was 41.7 ± 14.1 years (min–max: 16–68 years). While 14 patients (27.5%) were asymptomatic in the preoperative period, 37 patients (72.5%) had symptoms. A total of 16 patients (31.4%) had comorbidities. The CCI was 0 in 35 patients (68.6%) and 1 and above in 16 patients (31.4%). While 22 (43.1%) patients underwent cyst excision via VATS, 29 (56.9%) patients underwent thoracotomy. The average length of hospital stay was 1.77 ± 0.68 days for patients who had VATS, whereas it was 3.82 ± 3.3 days for patients who had thoracotomy (p <0.001). Table 1 shows the comparison of the demographic characteristics of the patients.
Table 1. Comparison of the groups according to the demographic characteristics of the patients.
| Variables | Thoracotomy (n = 29) | VATS (n = 22) | p-Value | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Gender | Male | 13 | 44.8 | 12 | 54.5 | 0.492 |
| Female | 16 | 55.2 | 10 | 45.5 | ||
| Age (years) (mean ± SD) | 41.1 ± 16.1 | 42.5 ± 11.3 | 0.710 | |||
| Side | Right | 21 | 72.4 | 21 | 95.5 | 0.033 |
| Left | 8 | 27.6 | 1 | 4.5 | ||
| Symptom | No | 7 | 24.1 | 7 | 31.8 | 0.543 |
| Yes | 22 | 75.9 | 15 | 68.2 | ||
| Symptom | Cough | 11 | 27.9 | 6 | 27.3 | |
| Pain | 8 | 27.6 | 4 | 18.2 | ||
| Dyspnea | 1 | 3.4 | 3 | 13.6 | ||
| Dysphagia | 2 | 6.9 | 2 | 9.1 | ||
| Comorbidity | 10 | 34.5 | 6 | 27.3 | 0.583 | |
| CCI | 0 | 19 | 65.5 | 16 | 72.7 | 0.583 |
| >1 | 10 | 34.5 | 6 | 27.3 | ||
| Cyst diameter (cm) | <5 | 12 | 41.4 | 14 | 63.6 | 0.115 |
| >5 | 17 | 58.6 | 8 | 36.4 | ||
| Adhesions between cyst and mediastinum | No | 20 | 69 | 16 | 72.7 | 0.770 |
| Yes | 9 | 31 | 6 | 27.3 | ||
| Maier classification | Type I | 5 | 20.8 | 12 | 57.1 | |
| Type II | 8 | 33.3 | 4 | 19 | ||
| Type III | 1 | 4.2 | 2 | 9.5 | ||
| Type IV | 6 | 25 | 2 | 9.5 | ||
| Type V | 4 | 16.4 | 1 | 4.8 | ||
| Cyst diameter (cm) (mean ± SD) | 5.05 ± 2.11 | 4.18 ± 2.03 | 0.144 | |||
| Operation time (minutes) | 90.51 ± 22.65 | 48.90 ± 20.32 | <0.001 | |||
| Hospitalization time (days) (mean ± SD) | 3.82 ± 3.3 | 1.77 ± 0.68 | <0.001 | |||
| Drainage time (days) | 3.41 ± 2.94 | 1.72 ± 0.63 | <0.001 | |||
VATS: video-assisted thoracoscopic surgery; CCI: Charlson Comorbidity Index; SD: standard deviation
Complications occurred in 4 patients (7.8%). In 2 patients, atelectasis developed due to secretion retention; in 1 patient, persistent air leakage occurred due to lung laceration during the procedure; and in 1 patient, pyothorax developed on postoperative day 10. Drainage and medical treatment were applied to the patient who developed pyothorax. Factors affecting complications are evaluated in Table 2. All the patients who developed complications were in the thoracotomy group. Recurrence appeared in 1 patient in the thoracotomy group at 46 months after the operation.
Table 2. Evaluation of prognostic factors affecting complications.
| Variables | No complication (n = 47) | Complication (n = 4) | p-Value | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Gender | Male | 24 | 51.1 | 1 | 25 | 0.317 |
| Female | 23 | 48.9 | 3 | 75 | ||
| Age (years) (mean ± SD) | 41.4 ± 14.5 | 45.5 ± 7.04 | 0.648 | |||
| Side | Right | 38 | 80.9 | 4 | 100 | 0.335 |
| Left | 9 | 19.1 | 0 | 0 | ||
| Symptom | No | 14 | 29.8 | 0 | 0 | 0.565 |
| Yes | 33 | 70.2 | 4 | 100 | ||
| Comorbidity | 14 | 29.8 | 2 | 50 | 0.581 | |
| CCI | 0 | 33 | 70.2 | 2 | 50 | 0.581 |
| >1 | 14 | 29.8 | 2 | 50 | ||
| Surgical approach | VATS | 22 | 46.8 | 0 | 0 | 0.124 |
| Thoracotomy | 25 | 53.2 | 4 | 100 | ||
| Cyst diameter (cm) | <5 | 26 | 55.3 | 0 | 0 | 0.034 |
| >5 | 21 | 44.7 | 4 | 100 | ||
| Adhesions between cyst and mediastinum | No | 36 | 76.6 | 0 | 0 | 0.0605 |
| Yes | 11 | 23.4 | 4 | 100 | ||
CCI: Charlson Comorbidity Index; SD: standard deviation; VATS: video-assisted thoracoscopic surgery
Discussion
Bronchogenic cyst is a rare congenital pathology and is thought to originate from the primitive ventral foregut in the early stages of the embryological period.2) Bronchogenic cysts comprise approximately 40%–50% of cystic lesions located in the mediastinum. CT and MRI are the most important imaging methods for the detection of a mediastinal cystic lesion and its relationship with the vital organs around it. It is believed that the reason for the increase in the incidence of cysts in recent years is the developments in radiological examination techniques.3,4) More than half of the cases apply to the clinic with symptoms. In our study, 37 (72.5%) patients had various symptoms at the time of admission. There are studies stating that asymptomatic cases will also become symptomatic over time.5) Chest pain, shortness of breath, difficulty swallowing, and cough are the main symptoms, but various symptoms can be seen in a wide spectrum. Symptoms usually occur as a result of compression of neighboring structures (mass effect) due to the growth of the cyst.1,4,6) Growing cysts pose serious risks of mass effect on mediastinal structures, infection, and rupture.7)
VATS is the increasingly preferred method in mediastinal surgery. The preferred curative treatment method in patients presenting with symptoms is generally thoracoscopic or conventional surgical resection. Alternative treatment methods such as robotic assisted thoracic surgery and endobronchial ultrasound-guided needle aspiration have controversial long-term results since they are still under development.8,9) In asymptomatic patients, controversy about surgical treatment and timing continues, but studies in previous years have shown that even if patients are asymptomatic, symptoms may develop during follow-up, or asymptomatic patients may present with serious complications such as infection, pneumothorax, pleural effusion, and superior vena cava obstruction.6,10,11) In addition, it has been reported that bronchogenic cysts have the potential to become malignant over time.12,13) Since controversy continues in asymptomatic patients in terms of the need and timing of surgical treatment, CCI of all patients were evaluated to assess the effect of factors related to comorbidity in the decision-making process. The CCI of 16 patients (31.4%) was 1 point and above. There was no significant difference in terms of the effect of CCI on complications. Although the traditional method for bronchogenic cyst resection is thoracotomy, in recent years, VATS has become the more preferred method, and studies on the applicability and validity of this method have been conducted.6,14–17)
In Guo et al.’s series of 99 patients, reported in 2016, 65 patients underwent thoracoscopic resection. The patient group who underwent thoracoscopy had a shorter length of hospital stay, and there was no difference in terms of complications and recurrence. Thoracoscopic surgery is recommended as the first choice due to its advantages.4) Similarly, in our study, while the length of hospital stay was significantly shorter in the VATS group, no difference was found in terms of complication development and recurrence in the long term. The most important factor affecting complication was found to be the cyst diameter being 5 cm and above. R0 resection was performed in all patients. However, despite R0 resection, recurrence occurred in a case; this is possibly due to remaining mucous residue from rupture of the cyst. Electrocautery should be applied to the mucosa in cases where complete resection is unlikely. Recurrent cases have been reported in the literature, usually in the form of case reports.18)
Limitation
Potential sources of bias in the present study include its retrospective design, the inclusion of operations performed by different surgeons, the small number of women in the patient sample, and nonevaluation (not assessing) postoperative pain scores of the patients.
Conclusion
VATS procedure is a safe method in the surgical treatment of bronchogenic cysts, with less hospitalization and similar recurrence rates. There is no difference in the development of recurrence using the different surgical approaches. In order to prevent recurrence, we think that in the surgical treatment of cystic lesions in the posterior location, cyst rupture should be avoided, irrigated in cases where rupture occurs, and it should be made sure that there is no residual mucosa. However, further studies are required regarding the recurrence rates of cystic lesions.
Disclosure Statement
The authors declare that there is no conflict of interest.
References
- 1).De Giacomo T, Diso D, Anile M, et al. Thoracoscopic resection of mediastinal bronchogenic cysts in adults. Eur J Cardio-Thoracic Surg 2009; 36: 357– 9. [DOI] [PubMed] [Google Scholar]
- 2).Maier HC. Bronchiogenic cysts of the mediastinum. Ann Surg 1948; 127: 476– 502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Ribet ME, Copin MC, Gosselin B. Bronchogenic cysts of the mediastinum. J Thorac Cardiovasc Surg 1995; 109: 1003– 10. [DOI] [PubMed] [Google Scholar]
- 4).Guo C, Mei J, Liu C, et al. Video-assisted thoracic surgery compared with posterolateral thoracotomy for mediastinal bronchogenic cysts in adult patients. J Thorac Dis 2016; 8: 2504– 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5).Limaïem F, Ayadi-Kaddour A, Djilani H, et al. Pulmonary and mediastinal bronchogenic cysts: a clinicopathologic study of 33 cases. Lung 2008; 186: 55– 61. [DOI] [PubMed] [Google Scholar]
- 6).Weber T, Roth TC, Beshay M, et al. Video-assisted thoracoscopic surgery of mediastinal bronchogenic cysts in adults: a single-center experience. Ann Thorac Surg 2004; 78: 987– 91. [DOI] [PubMed] [Google Scholar]
- 7).Wang X, Chen K, Li Y, et al. The video-assisted thoracic surgery for mediastinal bronchogenic cysts: a single-center experience. World J Surg 2018; 42: 3638– 45. [DOI] [PubMed] [Google Scholar]
- 8).Xu S, Liu B, Wang X, et al. Robotic thoracic surgery of the anterior superior mediastinal bronchogenic cyst. Ann Transl Med 2015; 3: 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9).Maturu VN, Dhooria S, Agarwal R. Efficacy and safety of transbronchial needle aspiration in diagnosis and treatment of mediastinal bronchogenic cysts: systematic review of case reports. J Bronchology Interv Pulmonol 2015; 22: 195– 203. [DOI] [PubMed] [Google Scholar]
- 10).Fievet L, D'Journo XB, Guys JM, et al. Bronchogenic cyst: best time for surgery? Ann Thorac Surg 2012; 94: 1695– 9. [DOI] [PubMed] [Google Scholar]
- 11).Patel SR, Meeker DP, Biscotti CV, et al. Presentation and management of bronchogenic cysts in the adult. Chest 1994; 106: 79– 85. [DOI] [PubMed] [Google Scholar]
- 12).Granato F, Voltolini L, Ghiribelli C, et al. Surgery for bronchogenic cysts: always easy? Asian Cardiovasc Thorac Ann 2009; 17: 467– 71. [DOI] [PubMed] [Google Scholar]
- 13).Miralles Lozano F, Gonzalez-Martínez B, Luna More S, et al. Carcinoma arising in a calcified bronchogenic cyst. Respiration 1981; 42: 135– 7. [DOI] [PubMed] [Google Scholar]
- 14).Martinod E, Pons F, Azorin J, et al. Thoracoscopic excision of mediastinal bronchogenic cysts: results in 20 cases. Ann Thorac Surg 2000; 69: 1525– 8. [DOI] [PubMed] [Google Scholar]
- 15).Muramatsu T, Shimamura M, Furuichi M, et al. Thoracoscopic resection of mediastinal bronchogenic cysts in adults. Asian J Surg 2011; 34: 11– 4. [DOI] [PubMed] [Google Scholar]
- 16).Jung HS, Kim DK, Lee GD, et al. Video-assisted thoracic surgery for bronchogenic cysts: is this the surgical approach of choice? Interact Cardiovasc Thorac Surg 2014; 19: 824– 9. [DOI] [PubMed] [Google Scholar]
- 17).Jain P, Sanghvi B, Shah H, et al. Thoracoscopic excision of mediastinal cysts in children. J Minim Access Surg 2007; 3: 123– 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Hasegawa T, Murayama F, Endo S, et al. Recurrent bronchogenic cyst 15 years after incomplete excision. Interact Cardiovasc Thorac Surg 2003; 2: 685– 7. [DOI] [PubMed] [Google Scholar]