Abstract
Numerous studies have linked outdoor levels of PM2.5, PM10, NO2, O3, SO2, and other air pollutants to significantly higher rates of Covid 19 morbidity and mortality, although the rate in which specific concentrations of pollutants increase Covid 19 morbidity and mortality varies widely by specific country and study. As little as a 1-μg/m3 increase in outdoor PM2.5 is estimated to increase rates of Covid 19 by as much as 0.22 to 8%. Two California studies have strongly linked heavy wildfire burning periods with significantly higher outdoor levels of PM2.5 and CO as well as significantly higher rates of Covid 19 cases and deaths. Active smoking has also been strongly linked significantly increased risk of Covid 19 severity and death. Other exposures possibly related to greater risk of Covid 19 morbidity and mortality include incense, pesticides, heavy metals, dust/sand, toxic waste sites, and volcanic emissions. The exact mechanisms in which air pollutants increase Covid 19 infections are not fully understood, but are probably related to pollutant-related oxidation and inflammation of the lungs and other tissues and to the pollutant-driven alternation of the angiotensin-converting enzyme 2 in respiratory and other cells.
Keywords: PM2.5, PM10, Nitrogen dioxide (NO2), Ozone (O3), Wildfires, Smoking, Covid 19, SARS Cov 2
Introduction
Covid 19 (CoronaVIrus Disease 2019) is caused by SARS2 Cov 2 (severe acute respiratory syndrome coronavirus 2), which is a RNA respiratory virus which is believed to be transmitted mostly by droplet nuclei in the air (Brandt and Mersha 2021). Covid 19 is especially dangerous to older humans as death rates for those over 70 years of age is more than 10%, while less than 0.1% for children and young adults (Signorelli and Odone 2020). Covid 19 infection rates in the USA are also significantly higher in African Americans as compared to the population as a whole (Brandt et al. 2020; Phillips et al. 2020).
Many papers and reviews have reported that exposure to air pollutants such as PM2.5, NO2, and O3 are associated with higher rates of Covid 19 incidence, severity, or mortality (Brandt and Mersha 2021; Copat et al. 2020). In addition, other pollutant sources such as wildfires and smoking have also been associated with greater risks of Covid 19 infection and mortality (Meo et al. 2020; Salah et al. 2020). This review will attempt to review the published data on environmental factors and Covid 19 on papers published up to March 21, 2021. This review will also briefly discuss possible mechanisms in which environmental factors may affect Covid 19 morbidity and mortality.
Materials and methods
Databases such as PubMed, MEDLINE, Google Scholar, and Scopus were searched for articles. Search terms used included Covid 19, SARS Cov-2, influenza, PM2.5, PM10, ozone, nitrogen oxides, sulfur oxides, traffic, wildfires, wood burning, biomass burning, forest fires, traffic, pesticides, incense, solvents, sand, sandstorms, and volcanoes. Publications were searched up to March 21, 2021.
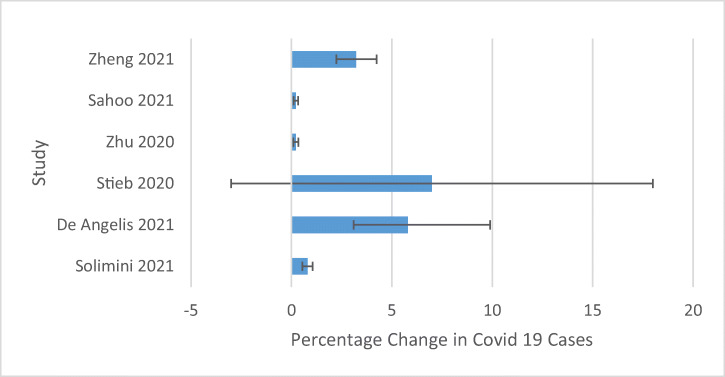
For papers relating outdoor air pollutants (“Introduction” section and Table), 31 papers were found that examined the following pollutants and their effects on Covid 19 morbidity and mortality: 29 papers for PM2.5, 14 papers for PM10, 2 that measured AQI (Air Quality Index), 13 papers for NO2, 8 papers which measured O3, 5 papers which measured SO2, 5 papers which measured CO, and 1 paper each for NH3, methane, lead, total volatile organics, and non-methane volatile organics. Table 1 is sorted first by various pollutants (PM2.5, PM10, NO2, etc.), then it is arranged with the papers which reported quantitative relationships between pollutant levels and rates of Covid 19 morbidity and mortality first, studies which calculated Ro (the basic reproduction ratio for Covid 19 values) are listed last, and other papers in the middle sections. Because many papers do not report social distancing measures, it was decided not to include social distancing measures in Table 1. Forest plots were also presented in Figs. 1, 2, and 3 to summarize the estimated relationships (in 4 or more studies cited—for the other pollutants, there were less than 4 studies and were presented in the text but not in the forest plots) between a 1 μg/m3 increases in ambient PM2.5, PM10, and NO2 and % increases in Covid 19 cases.
Table 1.
Air pollutants and their associations with Covid 19 morbidity and mortality
| Pollutant | Study reference | Location | Sample size and demographics | Time period of study | Covid 19 outcomes with increased pollutant |
|---|---|---|---|---|---|
| PM2.5 | (Solimini et al. 2021) |
63 nations 730 regions 5 continents |
237,749 Covid 19 cases | Begun when 10+ Covid 19 cases obtained in 1 region until 5/20/20 | A 10-μg/m3 PM2.5 increase is associated with a 8.1% increase cases (95% CI 5.4 to 10.5%) over 14-day lag |
| PM2.5 | (de Angelis et al. 2021) | Lombardy Italy, 1439 out of 1507 municipalities | 61,377 Covid 19 cases | 3/1/20 to 4/30/20 | A 10-μg/m3 PM2.5 increase is associated with a 58% increase cases (IRR 1.58, 95 % CI 1.31–19.90, p < 0.01) |
| PM2.5 | (Wu et al. 2020) |
USA 3087 counties |
3087 US counties representing 98% population. 1288 counties reporting Covid 19 deaths up to 4/22/20 | 1/2020 to 4/22/20 | A 1-μg/m3 PM2.5 increase is associated with a 8% increase in Covid 19 death rates (95% CI 2 to 15%). Death rates adjusted for 20 covariate factors including population size/density, age distribution, time of start and stay at home orders, weather, Covid 19 testing, smoking, obesity, and socioeconomic factors |
| PM2.5 | (Stieb et al. 2020) |
Canada 111 regions covering most of country |
73,390 cases average rate 208 cases/100,000—case rates highest in Quebec (489/100,000) and lowest in Nunavut (0/100,000) and NW Territories (12/100,00) | Up to 5/13/20 | A 1-μg/m3 increase is associated with 7% more Covid 19 cases (95% CI 0.97–1.18) adjusted for a number of factors including weather, % Black population, age distribution, and economic and medical factors |
| PM2.5 | (Zhu et al. 2020) | 120 cities all over China | Over 58,000 cases in 120 cities comprising about 70% China’s population | 1/23/20 to 2/29/20 | A 10-μg/m3 PM2.5 increase is associated with 2.24% increase cases (95% CI 1.02 to 3.46%), 0–14-day lag |
| PM2.5 | (Sahoo 2021) | 288 districts in India covering 65% India’s total Covid 19 cases | 21,700 cases India to 4/23/20 with about 65% in study region | 1/23/20 to 4/23/20 | A 10-μg/m3 increase is associated with a 2.21% more cases (95% CI 1.13 to 3.29) |
| PM2.5 | (Meo et al. 2021b) | London, England—not clear whether it means central London or metro area | Median 168 cases and 4 deaths per day over a 253 day period | 2/24/20 to 11/2/20 | A 1-μg/m3 PM2.5 increase is associated with 1.1% increase in Covid 19 cases and 2.3% increase in Covid 19 deaths (p < 0.001, both cases) |
| PM2.5 | (Zheng et al. 2021) | China |
81,132 Covid 19 cases 50,783 cases in Wuhan |
12/31/19 to 3/6/20 | A 10-μg/m3 PM2.5 increase is associated with 32.3% increase in Covid 19 cases (95% CI 22.4–42.4% ) adjusted for socioeconomic and social mobility factors |
| PM2.5 | (López-Feldman et al. 2021) |
Mexico City 14 out of 16 municipalities |
21,000+ Covid 19 deaths Mexico City up to 10/28/20 | Up till 10/28/20 | Increasing PM10 by 1 μg/m3 is associated with an 7.4% increase in Covid 19 deaths. Data adjusted for factors such as population density, health care factors, and smoking |
| PM2.5 | (Fiasca et al. 2020) |
Italy 62 out of 110 provinces |
Italy as a whole 239.410 Covid 19 cases by 5/24/20 and 743.419 cases by 11/30/20 | March to October 2020 | A 1-μg/m3 PM2.5 increase is associated with an increased Covid 19 incidence of 1.56 per 10,000 people (p < 0.001) |
| PM2.5 | (Sharma et al. 2021) | 10 nations with highest reported Covid 19 cases by 11/15/2020: the USA, India, Brazil, Russia, Spain, the UK, Italy, Peru, Iran, Chile | 10 nations with total of number of 34,526,346 Covid 19 cases and 813,442 Covid 19 deaths by 11/16/20 (note date different study period) | 2/1/2020 through 6/30/20 |
Higher PM2.5 is associated with more cases p < 0.01 and more mortality p < 0.05 Also higher ambient temperature is associated with significantly lower Covid 19 cases and mortality (p < 0.05 both cases) |
| PM2.5 | (Barnett-Itzhaki and Levi 2021) | 36 OECD nations | 36 OECD nations—population and Covid 19 cases not listed | 1/20/20 to 6/7/20 | 2017 levels of PM2.5 are associated with significantly more Covid 19 cases and mortality 40 days after the 1st confirmed case in each nation (p < 0.05) |
| PM2.5 | (Cascetta et al. 2021) |
Italy 107 provinces |
Up until 7/27/20—246,286 Covid 19 cases and 35,112 Covid 19 deaths | Up to 7/27/20 | If all Italy below 25 μg/m3 PM2.5, it was estimated that 7339 fewer cases up to July 2020. Covid 19 cases also significantly lower in seacoast areas |
| PM2.5 | (Bianconi et al. 2020) |
Italy 110 provinces |
105,792 deaths and 12,428 cases | 3/1/20 to 3/31/20 | Higher PM2.5/PM10 is associated significantly more Covid 19 cases p = 0.003 and mortality p = 0.004% |
| PM2.5 | (Fattorini and Regoli 2020) | Italy | Italy—total cases not reported | 2/24/20 to 4/27/20 | Long-term (2016–2020) PM2.5 exposure is associated with significantly increased Covid 19 cases |
| PM2.5 | (Dragone et al. 2021) |
Italy 12 provinces Lombardy |
42,823 Covid 19 cases | 2/24/20 to 3/31/20 for Covid 19 cases—for air pollution data 2/1/20 to 3/31/20 | Higher PM2.5 is associated with increased Covid 19 cases but no p values listed. This study also reported higher PM10, NO2, NH3, CO, and SO2 positively associated Covid 19 cases and O3 negatively associated Covid 19 cases, but no p values provided |
| PM2.5 | (Adhikari and Yin 2020) | Queens, New York City | 42,033 Covid 19 cases and 3221 Covid 19 deaths | 3/1/20 to 4/30/20 | Higher PM2.5 is associated with a significantly lower risk of Covid 19 cases (p < 0.001) and mortality (p < 0.044) |
| PM2.5 | (Bashir et al. 2020) | California, USA | 39,000 Covid 19 cases and 1800 deaths to 3/24/20 | 3/4/20- 4/24/20 | Increasing PM2.5 is associated fewer cases p < 0.01 and fewer deaths p < 0.01 |
| PM2.5 | (Vasquez-Apestegui et al. 2020) | Lima, Peru | All of Peru until 6/12/20- 220,749 total Covid 19 cases and 2382 Covid 19 mortality | Until 6/12/20 | Previous PM2.5 levels (2010–2016) are associated with significantly higher cases and significantly higher case fatality rates (p > 0.05 both cases) |
| PM2.5 | (Liu et al. 2021) | 9 nations: China, Korea, Japan, Canada, the USA, Russia, England, Germany, France | Over 2.6 million Covid 19 cases from 9 nations to 5/20/20 | 1/21/20 to 5/20/20 | Increased PM2.5 is associated with higher Covid 19 cases especially in Russia, England, Germany, America, and Canada |
| PM2.5 | (Kolluru et al. 2021) | 5 Indian mega cities: New Delhi, Kolkata, Mumbai, Bangalore, Chennai | In May and June 2020—total Covid 19: 153,629 cases in 5 megacities and 6449 total Covid 19 deaths | February (pre-lockdown), May (lockdown), and June (unlock) 2020 | Increased PM2.5 is associated with significantly increased Covid 19 cases—May p < 0.01 June p = 0.04) and mortality (May p = 0.02 and June p = 0.37) |
| PM2.5 | (Jain et al. 2021) | 6 South Asian nations: Afghanistan, Bangladesh, India, Nepal, Pakistan, Sri Lanka | 11.2 million Covid 19 cases and 163,945 Covid 19 deaths | Up to 12/16/20 | Increased PM2.5 is associated with significantly increased Covid 19 cases and mortality. Temperature increases are associated with both increased and decreased Covid 19 patients depending upon the nation |
| PM2.5 | (Yao et al. 2020) | China | 82,214 cases up to 4/12/20 | Up till 4/12/20 | PM2.5 10 μg/m3 increase is associated with CFR (case fatality rate) increase 0.24% p = 0.0042 |
| PM2.5 | (Hou et al. 2021) | 14 major cities in China | 4294 cases up till 4/28/20 | Up to 4/28/20 | Long-term PM2.5 over 2015–2020 is associated significantly higher Covid 19 CFR |
| PM2.5 | (Travaglio et al. 2021) | England | 300,000 cases up to December 2020 | Till December 20 | Increased PM2.5 1 μg/m3 is associated with 12% increased Covid 19 mortality |
| PM2.5 | (Bilal et al. 2020) | Germany | About 180.000 cases by middle of June 2020 | 2/24/20 to 7/2/20 | Increased PM2.5 is associated with significantly less Covid 19 cases (p < 0.01) |
| PM2.5 | (Pei et al. 2021) |
China 325 cities |
Daily case rate during lockdown 2.26 per 100,000 | Up till 5/27/20 | Increased PM2.5 is associated with significantly increased Covid 19 cases p < 0.05 |
| PM2.5 | (Landoni et al. 2021) | 33 European nations | 1.48 million Covid 19 cases | 2/11/20 to 4/17/20 | Increased PM2.5 both cases p = 0.0001 and mortality p < 0.0001 increased |
| PM2.5 | Chakrabarty et al. 2021 | 50 US states | About 609,000 US Covid 19 cases by April 20/20 | 3/2/20 to 4/30/20 | Each 1 μg/m3 raised Ro by 0.25 (p = 0.006). Data adjusted for 43 factors including age, ethnic groups, health care, and many socioeconomic factors |
| PM10 | (Solimini et al. 2021) |
63 nations 730 regions 5 continents |
237,749 Covid 19 cases | Study begun after 10+ Covid 19 Cases obtained in region until 5/20/20 | Each 10 μg/m3 increase PM10 is associated with 11.5% increased (95% CI 7.8–14.9%) Covid 19 cases over 14-day lag |
| PM10 | (Zhu et al. 2020) | 120 cities all over China | Over 58,000 cases in 120 cities comprising about 70% China’s population | 1/23/20 to 2/29/20 | PM10—each 10 μg/m3 increase is associated with a 1.76% increased mortality (95% CI 0.89 to 2.23%) lag 0–14 days |
| PM10 | (Sahoo 2021) | 288 districts in India covering 65% India’s total Covid 19 cases | 21,700 cases India to 4/23/20 with about 65% in study region | 1/23/20 to 4/23/20 | PM10—each 10 μg/m3 increase is associated with a 2.67% increased cases (95% CI 0.33 to 5.01%) |
| PM10 | (Zheng et al. 2021) |
China 324 cities |
81,132 Covid 19 cases 50,783 cases in Wuhan | 12/31/19 to 3/6/20 | PM10 10 μg/m3 14.2% increased cases (95% CI 7.9 to 20.5%) |
| PM10 | (Bianconi et al. 2020) |
Italy 110 provinces |
105,672 Covid 19 cases and 12,428 Covid 19 deaths | 3/1/20 to 3/31/20 | Higher PM2.5/PM10 is associated with significantly more Covid 19 cases p = 0.003 and mortality p = 0.004% |
| PM10 | (Fiasca et al. 2020) |
Italy 67 provinces |
Italy as a whole 239.410 Covid 19 cases by 5/24/20 and 743.419 cases by 11/30/20 | March to October 2020 | PM10 each 1 μg/m3 cases increased 1.26 per 10,000 population (p < 0.001) |
| PM10 | (Bashir et al. 2020) | California | 39,000 Covid 19 cases and 1800 deaths to 3/24/20 | 3/2/20 to 4/24/20 | PM10 significantly fewer cases and deaths p < 0.05 both |
| PM10 | (Pei et al. 2021) | 325 Chinese cities | Daily case rate during lockdown 2.26 per 100,000 | Up to 5/27/20 | Higher PM10 is associated with higher Covid 19 cases |
| PM10 | (Hou et al. 2021) |
China 14 major cities |
4294 Covid 19 cases | Up till 4/28/20 | Higher PM10 over 5 year period (2015–2020) is associated with significantly higher Covid 19 case fatality rate |
| PM10 | (Liu et al. 2021) | 9 nations | Over 2.6 million Covid 19 cases from 9 nations to 5/20/20 | 1/21/20 to 5/20/20 | PM10 is associated with significantly higher PM10 incidence, especially in Russia, England, and Germany |
| PM10 | (Kolluru et al. 2021) | 5 Indian mega cities | In May and June 2020, total Covid 19 153,629 cases in 5 megacities and 6449 total Covid 19 deaths | March 2020 (pre-lockdown), May 2020 (lockdown), June 2020 (unlock) | PM10 is associated with higher rates Covid 19 cases (May 2020 p = 0.03, June 2020 p = 0.32), but not significantly associated Covid 19 mortality (May 2020 p = 0.30, June 2020 p = 0.25) |
| PM10 | (Bilal et al. 2020) | Germany | 180,000 Covid 19 cases in Germany up to June 2020 | 2/24/20 to 7/2/20 | PM10 not significantly related to Covid 19 cases (p > 0.20) |
| PM10 | (Fattorini and Regoli 2020) | Italy | Italy—total number of cases not reported | 2/24/20 to 4/27/20 | PM10 long-term (2016–2020) exposure is associated with significant higher Covid 19 cases |
| PM10 | (Landoni et al. 2021) | 33 European nations | 1.48 million cases Covid 19 by 5/17/20 | 2/11/20 to 5/17/20 | PM 10 increases cases p = 0.0035 but not mortality p = 0.44 |
| AQI = Air Quality Index consisting of PM2.5, PM10, SO2, NO2, and O3 | (Pei et al. 2021) | 325 Chinese cities | Daily case rate during lockdown 2.26 per 100,000 | Up to 5/27/20 | Higher AQI is associated with significantly higher Covid 19 cases |
| AQI (Air Quality Index) | (Hou et al. 2021) | 14 Chinese cities | 4294 Covid 19 cases | Up till 4/28/20 | Higher AQI over 2015–2020 is associated with significantly higher Covid 19 case fatality rate |
| NO2 | (Zhu et al. 2020) |
China 120 cities |
Over 58,000 cases in 120 cities comprising about 70% China’s population | 1/23/20 to 2/29/20 | A 10-μg/m3 increase is associated with 6.94% increase in Covid 19 cases (95% CI 2.38 to 11.51) 0 to 14-day lag |
| NO2 | (Zheng et al. 2021) | China 324 Cities |
81,132 cases overall 50,783 in Wuhan (62.6%) |
12/31/19 to 3/6/20 | Each 10 μg/m3 NO2 is associated with 37.8% increased Covid 19 cases (95% CI 23.8–52.0%) |
| NO2 | (Sahoo 2021) | 288 districts in India covering 65% India’s total Covid 19 cases | 21,700 cases India to 4/23/20 with about 65% cases in study region | 1/30/20 to 4/23/20 | A-10 μg/m3 increase in NO2 is associated with 4.56% increase in Covid 19 cases (95% CI 2.22 to 6.90) 0–14-day lag |
| NO2 | (de Angelis et al. 2021) |
Lombardy, Italy 1439 out of 1507 municipalities |
62,377 Covid 19 cases | 3/1/20 to 4/30/20 | A 10-μg/m3 NO2 increase is associated with a 7% decrease in Covid 19 cases (IRR 0.93, 95% VI 0.88–0.99, p = 0.03) |
| NO2 | (Ogen 2020) | Italy, Spain, France, Germany | 4443 fatal Covid 19 cases to 3/19/2020—of which 3487 in Northern Italy or Central Spain | 3/19/20 | 83% deaths in areas with NO2 above 100 μg/m2 NO2 |
| NO2 | (Bashir et al. 2020) | California | 39,000 Covid 19 cases and 1800 deaths to 3/24/20 | 3/2/20 to 4/24/20 | NO2 is associated with significantly reduced cases and deaths (p < 0.05 for both cases) |
| NO2 | (Liu et al. 2021) | 9 nations | Over 2.6 million Covid 19 cases from 9 nations to 5/20/20 | 1/21/20 to 5/20/20 | Increased NO2 is associated with significantly higher Covid 19 cases |
| NO2 | (Bilal et al. 2020) | Germany | 180,000 cases Germany up to mid-June 2020 | 2/24/20 to 7/2/20 | Increased NO2 is Associated with significantly more Covid 19 cases (p < 0.01) |
| NO2 | (Fiasca et al. 2020) | 67 out of 110 Italian provinces | Italy overall 239,410 cases by 5/24/20 and 743,141 cases by 11/3/2020 | March–October 2020 | Each 1 μm/m3 NO2 is associated with increased Covid 19 cases by 1.24 per 10,000 in population (p < 0.0.001) |
| NO2 | (Fattorini and Regoli 2020) | Italy | Italy—total cases not reported | 2/24/20 to 4/27/20 | Long-term NO2 exposure (2016-20) is associated with significantly higher Covid 19 cases |
| NO2 | (Landoni et al. 2021) | 33 European nations | 1.48 million Covid 19 Cases | 2/11/20 to 5/17/20 | Increased NO2 is associated with significantly greater cases (p < 0.0001) and mortality (p < 0.0001) |
| NO2 | (Barnett-Itzhaki and Levi 2021) | 36 OECD nations | 36 OECD nations—population and Covid 19 cases not listed | 1/20/20 to 6/7/20 | Higher NO2 is associated with significantly greater Covid 19 mortality (but not cases) by day 60 after first Covid 19 cases in various nations |
| NO2 | (Yao et al. 2021) | 63 Chinese cities, including Wuhan, other Hubei provinces, cities, and non-Hubei cities | Number of Covid 19 cases on 2/8/20 in study area not reported | 1/1/20 to 2/8/20 | Each increase of 10 μg/m3 NO2 is associated with Ro increase of 0.12 (95% CI 0.02–0.23) outside Hubei Province and 0.52 (95$ CI − 0.30 to 1.25) inside Hubei Province |
| O3 | (Zhu et al. 2020) | 120 cities in China | Over 58,000 Cases in 120 cities comprising about 70% China’s population | 1/23/20 to 2/29/20 | A 10-μg/m3 O3 increase is associated with 4.76% more cases (95% CI 1.99 to 7.52) 0 to 14-day lag |
| O3 | (Meo et al. 2021a) | London, England | Median 168 cases and 4 deaths per day over a 253 day period | 2/24/20 to 11/2/20 | 10 ppb O3 is associated with 0.8% increase in Covid 19 cases (p = < 0.001) and 4.4% increase in Covid 19 deaths (p < 0.001) |
| O3 | (Adhikari and Yin 2020) | Queens, New York—population 2,253,858 | 42.023 Covid 19 cases and 3221 deaths | 3/1/20 to 4/20/20 | O3 related to more cases (p < 0.001) but significantly lower Covid 19 mortality (p = 0.0038) |
| O3 | (Liu et al. 2021) | 9 nations | Over 2.6 million Covid cases from 9 nations to 5/20/20 | 1/21/20 to 5/20/20 | Higher O3 is associated with higher Covid 19 incidence, especially Canada and the USA |
| O3 | (Bilal et al. 2020) | Germany | 180 Covid 19 cases Germany to mid-June 20 | 2/24/20 to 7/2/20 | Higher O3 is associated with more cases (p < 0.05) |
| O3 | (Kolluru et al. 2021) | 5 megacities in India | In May and June 2020, total Covid 19: 153,629 cases in 5 megacities and 6449 total Covid 19 deaths | March 2020 (pre-lockdown), May 2020 (lockdown), and June 2020 (unlock.) | Higher O3 is associated with significantly lower number Covid 19 cases (May and June 2020, both p < 0.01) and mortality (May and June 2020, both p < 0.01) |
| O3 | Fattorini and Regoli 2020 | Italy | Italy—total Covid 19 cases not reported | 2/24/ to 4/27/20 | O3 long-term exposure (2016–2020) is associated with significantly more Covid 19 cases |
| O3 | (Tripepi et al. 2020) | Italy | 53,518 cases Italy up to 3/21/20 | Up to 3/21/20 | Covid 19 cases and mortality greater in areas near Lodi, Lombardy, and in areas with higher O3 (modification p = 0.001) |
| SO2 | (Zhu et al. 2020) | 120 cities in China | Over 58,000 cases in 120 cities comprising about 70% China’s population | 1/23/20 to 2/29/20 | A SO2 10-μg/m3 increase is associated with 7.79% decreases in cases (95% CI − 14.57 to − 1.01%) 0 to 14-day lag |
| SO2 | (Sahoo 2021) | 288 districts in India covering 65% India’s total Covid 19 cases | 21,700 cases India to 4/23/20 with about 65% in study region | 1/30/20 to 4/23/20 | A SO2 10-μg/m3 increase related to significantly less Covid 19 cases − 7.23% (95% − 10.99 to − 3.47%) 0–14-day lag |
| SO2 | (Bashir et al. 2020) | California | 39,000 Covid 19 cases and 1800 deaths to 3/24/20 | 3/4/20 to 3/24/20 | Increased SO2 is associated with significantly more cases and deaths (p < 0.001 both cases) |
| SO2 | (Liu et al. 2021) | 9 nations | Over 2.6 million Covid cases from 9 nations to 5/20/20 | 1/21/20 to 5/20/20 | Higher SO2 is associated with significantly more Covid 19 cases |
| SO2 | (Landoni et al. 2021) | 33 European nations | 1.48 million Covid 19 cases | 2/11/20 to 5/17/20 | Higher SO2 is not associated with Covid 19 cases or mortality (p = 0.44 and 0.99) |
| CO | (Zhu et al. 2020) | China | Over 58,000 cases in 120 cities comprising about 70% China’s population | 1/23/20 to 2/29/20 | Higher CO 10 μg/m3 is associated with 15.11% increase in cases (95% CI 0.44 to 29.77%) |
| CO | (Meo et al. 2021a) | London, England—not clear whether it means central London or metro area | Median 168 cases and 4 deaths per day over a 253 day period | 2/24/20 to 11/2/20 | CO—1 ppm increase is associated with 21.3% increase in Covid 19 cases (p = 0.057) and 21.8% Covid 19 deaths (p = 0.047) |
| CO | (Bashir et al. 2020) | California | 39,000 Covid 19 cases and 1800 deaths to 3/24/20 | 3/2/20 to 4/24/20 | Higher CO is associated with significantly more cases and deaths (p < 0.05 both cases) |
| CO | (Kolluru et al. 2021) | 5 Indian megacities | In May and June 2020—total Covid 19: 153,629 cases in 5 megacities and 6449 total Covid 19 deaths | March 2020 pre-lockdown, May 2020 (lockdown), June 2020 (unlock) | Higher CO not is associated with significantly more cases (May 2020 p = 0.47 and June 2020 p = 0.97) and mortality (May 2020 p = 0.28, June 2020 p = 0.70) |
| CO | (Liu et al. 2021) | 9 nations | Over 2.6 million Covid 19 cases from 9 nations to 5/20/20 | 1/21/20 to 5/20/20 | Higher CO is associated with more Covid 19 cases in China and Japan |
| NH3 (ammonia) | (Landoni et al. 2021) | 33 European nations | 1.48 million Covid 19 cases till 5/17/20 | 2/11/20 to 5/17/20 | Higher NH3 is associated with significantly more cases (p < 0.0001) and mortality (p < 0.0001) |
| Methane | (Landoni et al. 2021) | 33 European nations | 1.48 million Covid 19 cases till 5/17/20 | 2/11/20 to 5/17/20 | Higher methane is associated with significantly more cases (p < 0.0001) and mortality (p < 0.0001) |
| Non-methane volatile organics | (Landoni et al. 2021) | 33 European nations | 1.48 million Covid 19 cases till 5/17/20 | 2/11/20 to 5/17/20 | Higher volatile organics is associated with significantly more cases (p < 0.0001) and mortality (p = 0.0002) |
| Total volatile organics | (Bashir et al. 2020) | California, USA | 39,000 Covid 19 cases and 1800 deaths to 3/24/20 | 3/2/20 to 4/24/20 | No significant relationship between total volatile organics and Covid 19 cases and mortality (p > 0.10 both cases) |
| Airborne lead levels | (Bashir et al. 2020) | California, USA | 39,000 Covid 19 cases and 1800 deaths to 3/24/20 | 3/2/20 to 4/24/20 | No significant relationship between airborne lead and Covid 19 cases and mortality (p > 0.10 both cases) |
Fig. 1.
Relationships between 1 μg/m3 increase ambient PM2.5 and percentage change in Covid 19 cases
Fig. 2.
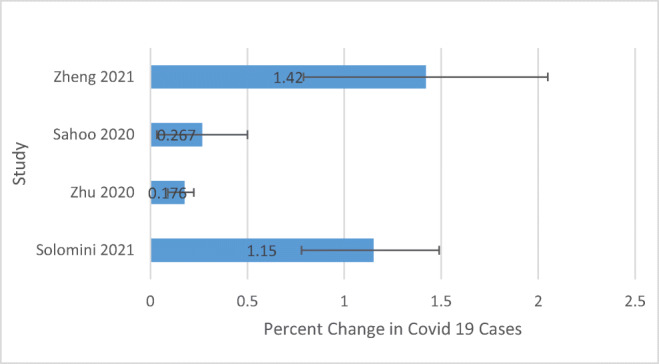
Relationships between 1 μg/m3 increase ambient PM10 and changes in Covid 19 cases
Fig. 3.
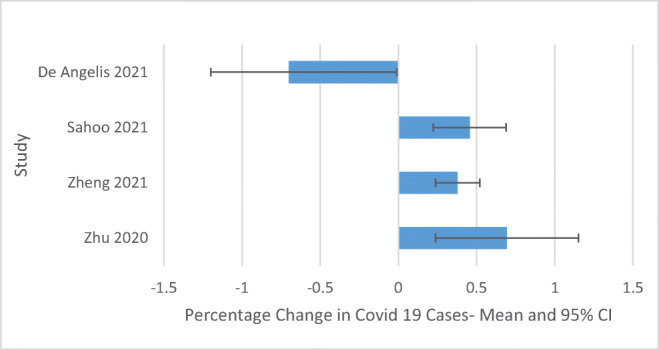
Relationships between 1 μg/m3 increase ambient NO2 and Covid 19 cases
In “Material and methods”section, a brief review was conducted of selected papers which measured changes in outdoor air quality as a result of the Covid 19 crises and lockdown. To save space, not all papers which measured changes in ambient air pollutants during the Covid 19 era were reported. Two papers measured the effects of wildfires on Covid 19 were reported (both from California, USA) (“Results” section). Four meta-analysis examining the effects of smoking on Covid 19 are reported in “Results” section, as well as some studies reporting the effects of smoking on other respiratory infections. To save space, not all individual smoking studies were reported. In “Results” section, some papers examining possible links with Covid 19 and environmental exposures such as pesticides, heavy metals, dust storms, incense, sewage, forested areas, and volcanoes. Section 6 examines possible links between airborne dust and respiratory infections. Section 7 summarizes possible physiological and biochemical mechanisms in which air pollutants may increase Covid 19 morbidity and mortality, including lung inflammation, oxidation, and altered expression of the ACE2 receptors.
Results
Outdoor PM2.5 and other air pollutants increase Covid 19 morbidity and mortality
Key points
Most studies have reported that higher outdoor levels of PM2.5, PM10, NO2, O3, SO2, and other pollutants are associated with significantly higher rates of Covid 19 Morbidity and Mortality.
Two studies have reported that increasing outdoor levels of PM2.5 and NO2 are associated with significantly higher Ro—reproduction rate for Covid 19.
Other studies have reported that higher levels of air pollutants are associated with significantly higher infection rates for influenza and other respiratory viruses.
A number of studies have reported that exposure to PM2.5, PM10, ozone, SO2, and NO2 are associated with higher rates of Covid 19 cases and mortality. Please see the following paragraphs and Table 1 for a summary of these studies. Some of these studies have estimated relationships between increased air pollution levels and increased (or decreased) rates of Covid 19 cases and mortality. For forest plots of the relationships between PM2.5, PM10, and NO2 and increases in Covid 19 cases,-please see Figs 1, 2, and 3 (data expressed as mean and 95% confidence intervals). Nine studies estimated that a 1-μg/m3 increase in outdoor PM2.5 increased case rates or death rates of Covid 19 by as much as 0.22 to 8%, with an unweighted average of a 2.74% increase per 1 μg/m3 PM2.5 (de Angelis et al. 2021, López-Feldman et al. 2021, Meo et al. 2021a, b, Sahoo 2021, Solimini et al. 2021, Stieb et al. 2020, Wu et al. 2020, Zheng et al. 2021, Zhu et al. 2020). Four published studies reported that a 10-μg/m3 increase in ambient NO2 was associated with a 4.56 to 37.8% increase in Covid 19 cases (Sahoo 2021; Zheng et al. 2021; Zhu et al. 2020) or a 7% decrease in Covid 19 cases (de Angelis et al. 2021). The average unweighted increase in Covid 19 cases per 10 μg/m3 NO2 was 10.57%.
Sharma’s study in 10 nations reported that temperature and pressure are negatively associated with Covid 19 cases, while ambient PM2.5 are significantly associated with more Covid 19 cases and deaths (Sharma et al. 2021). Solomini’s large study of 237,749 Covid-19 cases from 63 countries and 5 continents reported that a 10-μg/m3 increase in PM2.5 was associated with an 8.1% (95% CI 5.4 to 10.5%) increase in Covid 19 cases in a 14-day window (Solimini et al. 2021). Barnett reported that both ambient PM2.5 and nitrogen oxides were associated with significantly increased rates of both Covid 19 morbidity and mortality in 32 OECD countries (Barnett-Itzhaki and Levi 2021). De Angelis reported that a 10-μg/m3 increase in ambient PM2.5 was associated with a 58% increased risk of Covid 19 incidence in 1439 Lombardy Italian municipalities (95% CI 1.31–1.90, p < 0.01) (de Angelis et al. 2021).
A large US study of 3000 US counties (comprising 98% of the population) up to April 22, 2020 reported that only a 1-μg/m3 increase in PM2.5 was associated with an 8% increase in Covid 19 deaths (95% CI 2–15%) (Wu et al. 2020).
A study of 120 Chinese cities reported that an 10-μg/m3 increase in PM2.5 was associated with a 2.24% increase in Covid 19 mortality (95% CI 1.012 to 3.46) (Zhu et al. 2020). A 2021 study reported that an increase of 1 μg/m3 of PM2.5 was associated with a 7.4% increased risk of Covid 19 death in Mexico City (López-Feldman et al. 2021). Several Italian studies have also reported a significant association between ambient PM2.5 and significantly increased rates of Covid 19 cases, hospitalizations, and deaths (Bianconi et al. 2020; Cascetta et al. 2021; Fiasca et al. 2020). A study in all 107 Italian provinces reported that Covid 19 incidence and mortality were significantly higher in areas closest to Lodi, Lombardy and these effects were amplified by higher ozone levels (Tripepi et al. 2020). A study in Queens, New York, reported that increased ambient ozone were associated with increased Covid 19 cases (p < 0.001) but fewer Covid 19 deaths (p = 0.38), while increased PM2.5 were actually associated with lower risk of Covid 19 cases (p < 0.001) and mortality (p = 0.044) (Adhikari and Yin 2020).
A study of 49 Chinese cities reported that for every 10 μg/m3 increase in PM2.5, the case fatality rate (CFR) of Covid 19 increased by 0.24% (95% CI of 0.01–0.48%) (Yao et al. 2020). A nitrogen dioxide mapping study in Italy, Spain, France, and Germany reported that nitrogen dioxide levels above 100 μm/m3 were associated with 83% of the Covid 19 deaths (Ogen 2020). A study in Lima, Peru, reported that higher PM2.5 levels were associated with significantly higher Covid 19 incidence and case mortality rates (Vasquez-Apestegui et al. 2020). A study of 111 regions in all Canadian provinces reported that each 1 μg/m3 increase in PM2.5 was associated with a 7% increased incidence of Covid 19 (OR 1.07, 95% CI 0.97–1.18) (Stieb et al. 2020).
A large study in 9 nations (China, Japan, Korea, Canada, the USA, Russia, England, Germany, and France) reported that higher levels of PM2.5, PM10, SO2, NO2, and O3 generally were associated with significantly higher rates of Covid 19 infection (Liu et al. 2021). This study also concluded that the effects of PM2.5 and PM10 on Covid 19 incidence are more sensitive in Russia, England, Germany, and France, while O3 and PM2.5 effects are more sensitive to Covid 19 incidence in the USA and Canada (Liu et al. 2021).
A study of about 1.48 million Covid 19 cases in 33 European Nations from 2/11/20 to 5/17/20 reported that increasing outdoor concentrations of PM2.5, NO2, NH3, methane, and non-methane volatile organic compounds were all independently associated with significantly increased risk of both Covid 19 incidence and deaths (Landoni et al. 2021). Increasing PM10 was associated with significantly greater Covid 19 cases but not significantly Covid 19 mortality. Increasing SO2 was not associated with significantly greater Covid 19 cases and mortality (Landoni et al. 2021).
A large study of more than 58,000 Covid 19 cases in 120 Chinese cities reported that 10 μg/m3 increases (lag 0–14) in the following pollutants were associated with the following increases in Covid 19 cases: PM2.5 2.24% (95% CI 1.02 to 3.46), PM10 1.76%(95% CI 0.89 to 2.63), NO2 6.94% (2.38 to 11.51), O3 4.76% increase (95% CI 1.99 to 7.52), and CO 15.11% increase (0.44 to 29.77%) (Zhu et al. 2020). A 10-μg/ m3 increase in SO2 was associated with a 7.79% decrease in Covid 19 cases (95% CI − 14.57 to − 1.01) (Zhu et al. 2020). A German study involving 123,248 Covid 19 cases reported that higher levels of NO2 and O3 were all associated with significantly higher rates of Covid 19 cases and deaths, while higher levels of PM2.5 were associated with significantly lower levels of Covid 19 cases and deaths (Bilal et al. 2020). A geographically weighted regression model in China reported that both higher outdoor levels of PM2.5 and higher AQI (Air Quality Index) (consisting of PM2.5, PM10, SO2, NO2, CO, and ozone) were associated with significantly higher Covid 19 incidences (Pei et al. 2021).
Hou reported that long-term (1, 3, or 5 years), worse (higher) AQI in 14 Chinese cities was associated significantly higher Covid 19 case fatality rate (Hou et al. 2021). A study in 12 Lombardy, Italy, provinces reported that ambient PM2.5 exposure was associated with significantly greater rates of Covid 19 infection with lag rates as high as 10 days (Dragone et al. 2021). An Indian study reported that 10 μg/m3 increase during (Lag 0-14 days) of the following outdoor air pollutants were associated with significantly increased risk of Covid 19 infections PM2.5 2.21% increase (95% CI 1.13 to 3.29%), PM10 2.67% increase (95% CI 0.33 to 5.01%), and NO2 4.56% increase (95% CI 2.22 to 6.90%) (Sahoo 2021). A study in 5 Indian megacities (Bangalore, Chennai, Delhi, Kolkata, and Mumbai) reported that higher outdoor levels of PM2.5, PM10, CO, and O3 were associated with significantly higher levels of both Covid 19 cases and deaths (Kolluru et al. 2021).
A study in 324 Chinese cities reported that each increase of 10 μg/m3 of the following pollutants was associated with a significant increase in Covid 19 rates: NO2 37.8% increase (95% CI 23.8–53.0%), PM2.5 32.3% increase (95% CI 22.5–42.4%), and PM10 14.2% increase (7.9–20.5%) (Zheng et al. 2021). A study of more than 11 million Covid 19 cases in 6 South Asian nations (Afghanistan, Bangladesh, India, Nepal, Pakistan, and Sri Lanka) reported that higher outdoor PM2.5 was associated with significantly higher rates of both Covid 19 infection and death (Jain et al. 2021).
A study in London, England, reported that the following increases in outdoor air pollutants were associated with the following increases in Covid 19 cases and Covid 19 deaths respectively: for each 1 μg/m3 increase in PM2.5 1.1 and 2.3% increases in cases and mortality, for each 1 ppm increase in CO 21.3 and 21.8% increases in cases and mortality, and for each 10 ppb 03 0.8 and 4.4% increases in cases and mortality (Meo et al. 2021b).
An English study of over 300,000 Covid 19 cases reported that each 1 μg/m3 increase in outdoor PM2.5 was associated with a 12% increase in Covid 19 cases (Travaglio et al. 2021). An Italian study reported that relatively high levels of long-term exposure to outdoor pollutants (NO2, O3, PM2.5, PM10) during the period 2016–2020 were associated with significantly higher levels of Covid 19 cases (Fattorini and Regoli 2020).
Ambient PM 2.5 and NO2 increases Ro rate of Covid 19
Ro is described as the basic reproduction ratio for Covid 19. The Ro rates for Covid 19 are generally between 1.0 and 3.0, with higher values representing higher Covid 19 reproduction rates. A study in all 50 US states compared Covid 19 Ro rates and their relationships between ambient PM2.5 from the period March 2 to April 30, 2020 (Chakrabarty et al. 2021). Each increment in ambient 1 μg/m3 PM2.5 was associated with a significant 0.25 increase in Ro (95% CI 0.048–0.447) (Chakrabarty et al. 2021). During this time, Ro was the highest in New Jersey at 3.41 and New York at 3.30 and lowest in Alaska at 1.60 and Wyoming at 1.76 (Chakrabarty et al. 2021). During this time period, Ro values generally dropped from early March to late April 2020 with the institution of social distancing and school/workplace closures (Chakrabarty et al. 2021).
A study of 63 Chinese cities also reported that higher outdoor NO2 levels were associated with significantly higher Ro basic reproduction rate (Yao et al. 2021). Each 10 μg/m3 increase in NO2 was associated with a Ro increase of 0.12 outside Hubei Province and 0.52 inside Hubei Province (Yao et al. 2021).
Air pollution increases risk of respiratory infection in general
Other studies have reported that higher air pollution levels can significantly increase risk of respiratory infections in general. A study of 6814 multi-ethnic adults aged 44 to 84 years in 6 US cities reported that an increase of estimated PM2.5 and NOx from 25 to 75% percentile increased the risk of respiratory infections by 1.04 (OR 1.04, 95% CI 1.00 to 1.09) and 1.15 (OR 1.15, 95% CI 1.10 to 1.20), respectively (Kirwa et al. 2021). A Chinese study reported that increased outdoor levels of PM2.5, PM10, CO, and SO2 were associated with significantly higher levels of influenza-like illness in both children and adults (Su et al. 2019). A Utah study involving 112,467 subjects with lower respiratory infection (77% of which were 2 years or less) reported that higher PM2.5 levels were associated with significantly higher rates of lower respiratory illness (Horne et al. 2018).
A 2002–2003 Chinese study reported that higher levels of API (air pollution index consisting of airborne outdoor levels of particulate matter, sulfur and nitrogen dioxides, carbon monoxide, and ground level ozone) were associated with significantly higher mortality rates due to SARS (severe acute respiratory syndrome) (Cui et al. 2003). A 2019 Korean study linked higher ambient levels of PM10 with significantly higher rates of adenovirus (HAdV), metapneumovirus (HMPV), human coronavirus (HCoV), human bocavirus (HBov), human parainfluenza virus (HPIV), and influenza virus (IV) (Cheon et al. 2019).
Covid 19 restrictions and lowered outdoor air pollutants
Key points
Most, but not all, studies have reported that airborne levels of many pollutants have fallen significantly during the Covid 19 lockdowns.
On the positive side, a number of studies have noted that Covid 19 lockdowns and reduced industrial/traffic activity have been associated with drops in ambient levels of PM2.5 and other pollutants (Srivastava 2021).
An analysis of 10,000+ sampling sites in 380 World Cities reported that during the 2020 lockdown periods PM2.5 and NO2 fell by an average of 16.1 and 45.8%, while ozone levels rose by an average of 5.4% (He et al. 2021). A study of 50 more polluted capital cities reported a mean drop in PM2.5 of 11% (Rodríguez-Urrego and Rodríguez-Urrego 2020). A study of more than 1500 air monitoring sites in 377 Chinese cities reported a mean 16 and 20% reduction of PM2.5 and PM10 when comparing January 20 to April 8, 2020, with the same period in 2019 (Fan et al. 2020). A study in Baghdad, Iran, reported mean pollution drops of 6% for NO2, and 8% for PM2.5 during the March 1 to July 24, 2020, as compared to 2019 (Hashim et al. 2021). Another study noted significant drops in outdoor PM2.5 during the Covid 19 crisis in 9 world cities including New York City, Los Angeles, Zaragoza, Rome, Dubai, Delhi, Mumbai, Beijing, and Shanghai (Chauhan and Singh 2020). Studies in 4 large Pakistani cities (Lahore, Islamabad, Karachi, and Pewshawar) reported that during the Covid 19 period, average PM2.5 levels fell 13 to 33% in satellite observations and 23 to 58% in ground based observations (Ali et al. 2021). A Chinese study reported that comparing outdoor pollutant levels from January 21 to March 23 during the both 2020 and 2019, reported that average PM2.5 levels fell by an average of 35%, 29%, and 19% respectively in Wuhan, Hubei (Wuhan excluded), and China (Hubei excluded) and NO2 levels fell by an average of 53%, 50%, and 30% respectively in Wuhan, Hubei, and China respectively (Chu et al. 2021). During the lockdown period between March 1 to May 31, 2020, mean outdoor levels of PM10, PM2.5, NO, NO2, and CO levels fell by an average of 58%, 47%, 76%, 68 and 58% respectively in Delhi, India, as compared to the 2019 values (Srivastava et al. 2021). A study in 7 Korean cities reported that mean PM2.5 levels fell by an average of 7.5 to 24.9% during the 2020 lockdown as compared to 2019 (Kwak et al. 2021). An Italian study reported reductions in outdoor PM2.5 as high as 53% and reductions in NO2 as high as 67% (Donzelli et al. 2021).
At least two studies have reported significant declines in average ambient volatile organic compounds (VOCs) during the lockdown period—including a 37–57% reduction of total VOCs in China (Li et al. 2020) and a 48–68% reduction in benzene in Italy (Collivignarelli et al. 2020).
Wildfires are associated with increased Covid 19 rates
Key points
Two California studies have reported significant increases in both ambient PM2.5 and Covid 19 cases and/or deaths during heavy wildfire burning periods.
Wildfires and extensive wood burning both produce large quantities of carbon monoxide, fine particulates, and other toxic chemicals (such as carcinogenic polycyclic aromatic hydrocarbons or PAHs) which have been documented to be associated with significantly higher rates of respiratory and cardiovascular problems (Larson and Koenig 1994; Naeher et al. 2007; Reid et al. 2016; Youssouf et al. 2014). A study of 10 California counties affected by the severe 2020 wildfires reported that during the heavy burning period between August 15, 2020, and September 22, 2020, mean PM2.5 levels increased by 221% (92.91 vs 28.97 μg/m3, p < 0.001), mean carbon monoxide levels increased by 151% (4.77 vs 1.90 ppm, p < 0.001), and during this same wildfire period, Covid 19 cases jumped by 57% (p < 0.001), and the number of Covid 19-related deaths rose by 148% (p < 0.001) (Meo et al. 2021a). A study conducted by same authors reported significantly higher rates of Covid 19 cases and significantly higher PM2.5 outdoor levels in San Francisco during this same 2020 wildfire period (Meo et al. 2020).
Other studies and reviews have reported that exposure to wildfire smoke in firefighters are associated with significantly greater risk of respiratory infections such as pneumonia and acute bronchitis (Navarro et al. 2021).
Smoking increases Covid 19 risk
Key points
Most studies have reported that Covid 19 morbidity and mortality rates are significantly higher in smokers.
A number of studies have reported that tobacco smoking is related to increased Covid 19 risk. Salah’s meta-analysis reported smoking about doubled Covid 19 mortality risk (OR 2.07, 95% CI 1.59–2.69, 10 studies of 11,189 patients) (Salah et al. 2020). A July 2020 meta-analysis of 47 studies of 32,849 hospitalized Covid 19 patients reported that current smokers had much greater risks of severe Covid 19 disease versus former smokers/non-smokers, including greater risk of severe Covid 19 (OR 1.31, 1,12–1.54) and Covid 19 mortality (OR 1.26, 95% CI 1.20–1.32) (Reddy et al. 2021). A meta-analysis of 22 published studies on 5689 Covid 19 patients reported that severe disease risk was significantly greater in smokers (OR 1.34, 95% CI 1.07–1.67) (Karanasos et al. 2020). A 2021 meta-analysis of 19 studies reported that smoking was associated with an almost doubled risk of worse Covid 19 progression (OR 1.96, 95% CI 1.36–2.82) (Jiménez-Ruiz et al. 2021). A 2021 analysis of 109 articles involving 517,020 Covid 19 patients reported that a smoking history was associated with a significantly increased risk of ICU admission (OR 1.73, 95% CI 1.36–2.19) and significantly increased risk of death (OR 1.58, 95% CI 1.38–1.81) (Zhang et al. 2021). A 2021 review reported that there have not been any studies so far on the associations between secondhand tobacco smoke and Covid 19 (Brandt and Mersha 2021).
Smoking increases risk of other respiratory infections
Smoking can also increase the risk of other respiratory infections such as influenza and tuberculosis. A 2019 meta-analysis of 9 studies with 40,685 participants reported that current smokers are more than 5 times more likely to develop laboratory confirmed influenza than never smokers (OR 5.69, 95% CI 2.79–11.60, 3 studies). Meta-analyses of the relationships between smoking and tuberculosis (TB) have reported that active smoking is associated with a 2.284-fold increased risk of developing pulmonary TB (OR 2284, 95% CI 1765–2.954, 14 studies) and a 2.236-fold increased risk of dying from TB (OR 2.236, 95% CI 1.340–3.732, 6 studies) (Slama et al. 2007). Secondhand tobacco exposure as compared to no first- or secondhand exposure was associated with a 3.353-fold increased risk of TB (OR 3.353, 95% CI 2.028–5.543, 3 studies) (Slama et al. 2007).
Other possible environmental risk factors for Covid 19 transmission—incense, pesticides, metals, desert dust/sand, toxic waste sites, volcanic emissions
Key points
Other possible risk factors for Covid 19 incidence and/or mortality include incense, pesticides, metals, sand, toxic waste sites, and volcanic emissions.
Some researchers have postulated that exposure to incense sticks (Amoatey et al. 2020), pesticides (Rajak et al. 2021), and heavy metals (Skalny et al. 2020) may increase risk of Covid 19 morbidity and mortality. It has been hypothesized that pesticides exposure may increase risk of Covid 19 by damaging the respiratory, immune, cardiovascular, hepatic, and nervous systems (Rajak et al. 2021). Many toxic heavy metals can damage the immune system, and human and animal studies have reported that toxic heavy metal exposure can increase risk of respiratory infections like respiratory syncytial virus (RSV) and influenza (Skalny et al. 2020). Some researchers have suggested that indoor incense exposure may increase Covid 19 risks (Amoatey et al. 2020). A US study of 3143 counties up to May 31, 2020, reported that diesel particulate concentrations and proximity to Risk Management Plan (RMP) and toxic waste sites were associated with significantly higher Covid 19 mortality rates (Hendryx and Luo 2020).
Some have postulated that dust storms may also be associated with greater Covid 19 risk (Middelton 2020). Every year, about half a billion tons of desert dust become airborne and can travel for thousands of miles (Middelton 2020). Dust storms may also spread influenza (both Covid 19/SARS Cov2 and influenza are RNA respiratory viruses). A Taiwan study reported that mean outdoor airborne influenza concentrations were 21 to 31 times higher during 24 days of dust storms as compared to 10 control days (mean concentrations of influenza per cubic meter of outdoor air at Wan-Li station 268 vs. 13, p = 0.02, at Shin-Jhaung station 276 vs. 9, p = 0.01) (Chen et al. 2010).
Other researchers have noted that viable Covid 19 is found in human sewage, which may potentially be a major source of Covid 19 infection (Rooney et al. 2021; Senatore et al. 2021).
An Italian study reported significantly lower Covid 19 mortality rates in heavily forested areas (more than 1 hectare forest per person) (Roviello and Roviello 2020). The authors hypothesized that the lower Covid 19 death rates in the forested Italian regions could be due to the PM2.5 filtering ability of forests and/or the production of anti-viral volatile organics (which are both volatilized in the atmosphere and present in foodstuffs like Bay leaves) by common Italian trees/shrubs such as Laurus nobilis or bay laurel (Roviello and Roviello 2020).
Italian researchers reported relatively high Covid 19 infection rates on Sicily east of volcanic Mt. Etna (which have been active for much of 2020 and early 2021) and hypothesized that toxic gases and trace metals may play some role in promoting Covid 19 (Raciti and Calabrò 2020).
Is SARS Cov 2/Covid 19 spread by airborne dust?
Key points
SARS Cov 2 and other respiratory viruses like virus may possibly be spread by airborne dust as well as by droplet nuclei.
Viability of SARS Cov 2 has been estimated to be perhaps about 1.2 h in air and from several hours to several days on living and inanimate surfaces.
PM2.5 may possibly serve as a direct vector for transmission of Covid 19/SARS Cov2 and other viruses. SARS Cov 2 has been found to bind to particulate matter surrounded by water (Borisova and Komisarenko 2020). In addition, PM2.5 and SARS Cov 2 can enter the nose to brain olfactory nerve delivery system and cause neurological symptoms (Borisova and Komisarenko 2020). Several studies have reported viable SARS Cov2 can be detected in PM2.5 or PM10 fractions of air (Tung et al. 2021). Viable SARS Cov 2 has been detected on PM10 fractions on 2020 outdoor air in Italy (Chirizzi et al. 2021; Setti et al. 2020) and on PM2.5 and smaller airborne fractions from 2 Chinese hospitals (Liu et al. 2020). A Malaysian study reported that RNA from SARS Cov 2 was collected from the PM2.5 from the air of hospital wards housing SARS Cov 2 patients (Nor et al. 2021). On the other hand, a study in Leipzig, Germany, found no evidence of SARS Cov 2 RNA in either 8 weekly outdoor air particulate samples collected during the pandemic or in purified extracts from 9 species of pollen (Dunker et al. 2021).
To spread Covid 19, the virus would have to survive its travel on droplets or air particulates. Information on SARS Cov2 virus survival time in air droplets or particulates is sparse. Von Dormelan reported that SARS Cov2 has a median half-life of about 1.1–1.2 h on airborne aerosols (van Doremalen et al. 2020). SARS Cov 2/Covid 19 survival on inanimate surfaces vary considerable from study to study—they had been reported as long as 3 to 9 days on plastic surfaces, 2 days on stainless steel, 1 day on cardboard, and 4 h on copper (Marquès and Domingo 2020). SARS Cov2 viability is generally longer under conditions of lower temperature and humidity (Marquès and Domingo 2020). Viability/survival of SARS Cov2/Covid 19 has been estimated at 9 h for hands as compared to influenza (another RNA respiratory virus) of 1.8 h (Hirose et al. 2020). Some studies have suggested that particulate pollution may increase airborne survival of many types of viruses times by binding to bacteria and providing protection from UV light and by reducing dehydration (Navarro et al. 2021; Reche et al. 2018).
Other possible mechanisms in which air pollutants may increase risk of Covid 19 infection/death, lung damage, oxidation/inflammation, and overexpression of angiotensin-converting enzyme 2
Key points
Air pollution may possibly increase Covid 19 morbidity and mortality by promoting oxidation and inflation.
PM2.5, NO2, and other air pollutants may increase Covid 19 susceptibility by altering the ACE2 or angiotension 2 receptor which is a binding site for SAR Cov2.
Besides direct transmission on particulates, air pollutants may also help spread Covid 19 infection by other mechanisms including promoting lung damage, or binding to and overexpression of angiotensin-converting enzyme 2 (Comunian et al. 2020). Various human, animal, and cell studies have reported that exposure to particulate pollution can increase lung inflammation and oxidation (Comunian et al. 2020).
Exposure to PM2.5 and NO2 may increase incidence and severity of Covid 19 by altering expression of angiotensin-converting enzyme 2 (ACE2) in respiratory cells (Alifano et al. 2020; Paital and Agrawal 2020; Samavati and Uhal 2020). ACE2 is a membrane enzyme found in the lungs, nasal epithelium, arteries, kidney, heart, and intestines and regulates blood pressure by modifying angiotensin 2 into angiotensin 1–7, which is a vasodilator and anti-inflammatory agent (Comunian et al. 2020). ACE2 receptors are a receptor for coronavirus binding including SARS Cov 2/Covid 19 (Alifano et al. 2020; Paital and Agrawal 2020). SARS Cov2 binding to these ACE2 receptors can alter expression causing increased inflammation and cardiac damage (Comunian et al. 2020; Samavati and Uhal 2020). Exposure to airborne PM2.5 has been shown to increase ACE2 receptors in mice (Lin et al. 2018). ACE2 receptors tend to both more common in older humans, and the greater number of ACE2 receptors in elders may partially explain the significantly higher Covid 19 morbidity and mortality seen in older patients (Comunian et al. 2020; Wong et al. 2020). The significantly higher rates of Covid 19 cases and death seen in African Americans in the USA may be due to a number of factors including ACE2 genetic polymorphisms, higher average exposures to PM2.5 and other pollutants, more crowded housing, and socioeconomic factors (Brandt et al. 2020; Phillips et al. 2020).
Italian researchers have proposed a “double-hit” hypothesis in which combined exposure to PM2.5 and NO2 can increase susceptibility to Covid 19 (Frontera et al. 2020). In the first step, chronic exposure to PM2.5 causes lung damage, inflammation, increased susceptibility to viral infection, and alveolar ACE-2 overexpression (Frontera et al. 2020). This may increase viral load by depleting ACE-2 receptors and impairing host defenses. Exposure to NO2 can then cause additional lung damage including inflammation and edema, and increased susceptibility to infections including Covid 19 (Frontera et al. 2020). After the lungs have experienced a PM2.5 and NO2 “double hit,” they are much more susceptible to SARS Cov 2 binding the ACE-2 sites and causing serious infection (Frontera et al. 2020) .
Much more study on the relationships on the ACE2 receptors, SARS Cov 2/Covid-19, and air pollutants are needed (Samavati and Uhal 2020). For a good 2020 discussion on ACE2 receptors, please see Samavati and Uhal (2020)
Mechanisms in which air pollution increases influenza infection rates
Particulate pollution may also increase the risk of many other infections. A mouse study reported that long-term exposure to PM2.5 enhanced survival of the influenza virus by downregulating pulmonary macrophage Kdm6a and altering histone modification in IL-6 and IFNβ promoter regions (Ma et al. 2017). Another murine study reported that intratracheal PM2.5 exposure reduces influenza immunity by inhibiting activation of NLRP3 inflammasome and expression of interferon-β (Tao et al. 2020).
Discussion
Many environmental exposures have been strongly linked to higher Covid 19 morbidity and mortality including PM2.5, PM10, NO2, O3, wildfires, and smoking. Other exposures which may possibly be related to higher Covid 19 morbidity and mortality include sulfur oxides, carbon monoxide, volatile organic chemicals, incense, pesticides, heavy metals, dust/sandstorms, toxic waste sites, and volcanic emissions.
Outdoor exposure to PM2.5 and other particulate fractions have been consistently associated with higher levels of Covid 19 incidence, severity, and mortality, although the degree in which a given amount of PM2.5 increases Covid 19 factors varies considerable from study to study (Table 1). Table 1 notes that significantly higher rates of Covid 19 morbidity and/or mortality were associated with higher outdoor levels of the following pollutants: PM2.5 in 27 out of 29 studies, PM10 in 12 out of 14 studies, NO2 in 11 out of 13 cases, O3 in 7 out of 8 cases, SO2 in 2 out of 5 cases, and CO in 4 out of 5 cases.
One limitation of this review is that most of these studies published to date have involved air pollution and Covid 19 morbidity and mortality only during the early pandemic period up until sometime between January and October 2021 (please see Table 1). Additional studies examining the effects of air pollutants on Covid 19 cases/deaths during the late pandemic period in late 2020 or 2021 might yield interesting information.
Most of the studies to date have compared Covid 19 rates while measuring only one outdoor air pollutant and have not considered multiple outdoor air pollutants at the same time. Of course, interactions and correlations between pollutants could have played a major role in influencing Covid 19 morbidity and mortality rates. In the future, large epidemiological studies with good statistical power of Covid 19 and multiple air pollutants might be able to yield useful data on the interactions between pollutants. In addition to epidemiological studies, more studies are needed to study the effects on air pollution and infection at the molecular and cellular levels.
A complication with comparing outdoor pollution levels with Covid 19 morbidity and mortality is that many other factors can also play a role in determining Covid 19 morbidity and mortality: including weather, social distancing measures, Covid 19 vaccines, population density, age structure, socioeconomic factors, the quality and affordability of health care systems, mask wearing, handwashing, nasal disinfection, surface cleaning, HEPA air filters, quarantine, and nutrition (Aggarwal et al. 2020; Ayenigbara et al. 2020; Calzetta et al. 2021; Chiesa et al. 2021; Chu et al. 2020; Curtis 2021; Ferrer and Sanchez-Gonzalez 2021; Fouladi Dehaghi et al. 2020; Hradsky and Komarek 2021; Matrajt and Leung 2020; Mechanick et al. 2021; Nussbaumer-Streit et al. 2020; Pradhan et al. 2020; Rodríguez et al. 2021; Romano Spica et al. 2020; Thu et al. 2020). A meta-analysis of 29 unadjusted and 9 adjusted studies has reported that social distancing measures can play a major role in reducing Covid 19 spread (Chu et al. 2020). On the other hand, lack of social distancing, mask wearing, and other protective behaviors can increase risk of Covid 19 spread. For example, the Sturgis, South Dakota, USA Motorcycle Rally which was held from August 7 to 16, 2020, had about 500,000 attendees from all over the USA, had relatively little social distancing and mask usage, and was estimated to cause an additional 115,208 to 266,790 cases of Covid 19 throughout the USA (Dave and Sabia 2020). Social distancing may play a major role in modifying the effects of air pollution on Covid 19 morbidity and mortality. However, a limitation of this review is the fact that many of the studies cited in Table 1 did not describe social distancing methods in detail. Therefore, social distancing methods was not reported in Table 1, although they might have been very interesting. Further study is needed to determine how various factors like air pollution, social distancing, mask usage, handwashing, surface cleaning, HEPA, quarantine, medical care, Covid 9 vaccinations, social-economic factors, and nutrition interact with each other.
Another limitation of this review is that it reviewed papers published only up to March 21, 2021. Certainly, more useful papers and insights on air pollution effects on Covid 19 will be produced after 3/21/21. Hopefully, this review will encourage other clinicians, researchers, and public health experts to further examine the complex relationships between air pollution and infection with Covid 19 and other pathogens.
These studies linking higher Covid 19 morbidity and mortality offer additional arguments for reducing air pollution levels in both the developed and developing worlds. In 2015, it was estimated that outdoor PM2.5 pollution alone caused 4.2 million annual deaths (95% CI 3.7 to 4.8 million) and 103.1 million (95% CI 90.8 to 115.1 million) disability-adjusted life-years (Cohen et al. 2017). Cutting back on air pollution by using cleaner transportation, heating, and industrial methods and by reducing biomass (wood/leaves/straw/forest/wildfire) burning can reduce risk of many health problems including Covid 19 and other respiratory infections. Use of face masks can also reduce risk from both PM2.5 and Covid 19 exposure (Xu et al. 2020).
Conclusions
Airborne pollutants play an important role in Covid 19 infection and severity. Limiting environmental exposures offer great potential for reducing both morbidity and mortality from Covid 19 and other respiratory infections like influenza. Much more research on the interplay between Covid 19/other infections, air pollutants, and other factors such as handwashing/vaccination/nutrition are needed.
Acknowledgements
The author thanks all of the good researchers he cites in the review. The author also thanks Tamara Tuuminen, MD of Helsinki, Finland, and David Brown, DrPH of North Westport, CT, USA, for reading the manuscript and making helpful suggestions.
Author contribution
Luke Curtis researched and wrote the entire review.
Availability of data and materials
All data were based on already published articles.
Declarations
Ethics approval
No human subjects—just cited published literature.
Consent for publication
Yes—no human data used.
Competing interests
The author declares no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Adhikari A, Yin J (2020) Short-term effects of ambient ozone, PM(2.5,) and meteorological factors on COVID-19 confirmed cases and deaths in Queens, New York. Int J Environ Res Public Health 17(11):4047 [DOI] [PMC free article] [PubMed]
- Aggarwal N, Dwarakanathan V, Gautam N, Ray A. Facemasks for prevention of viral respiratory infections in community settings: a systematic review and meta-analysis. Indian J Public Health. 2020;64:S192–s200. doi: 10.4103/ijph.IJPH_470_20. [DOI] [PubMed] [Google Scholar]
- Ali SM, Malik F, Anjum MS, Siddiqui GF, Anwar MN, Lam SS, Nizami AS, Khokhar MF. Exploring the linkage between PM(2.5) levels and Covid-19 spread and its implications for socio-economic circles. Environ Res. 2021;193:110421. doi: 10.1016/j.envres.2020.110421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alifano M, Alifano P, Forgez P, Iannelli A. Renin-angiotensin system at the heart of Covid-19 pandemic. Biochimie. 2020;174:30–33. doi: 10.1016/j.biochi.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amoatey P, Omidvarborna H, Baawain MS, Al-Mamun A. Impact of building ventilation systems and habitual indoor incense burning on SARS-CoV-2 virus transmissions in Middle Eastern countries. Sci Total Environ. 2020;733:139356. doi: 10.1016/j.scitotenv.2020.139356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Angelis E, Renzetti S, Volta M, Donato F, Calza S, Placidi D, Lucchini RG, Rota M. Covid-19 incidence and mortality in Lombardy, Italy: an ecological study on the role of air pollution, meteorological factors, demographic and socioeconomic variables. Environ Res. 2021;195:110777. doi: 10.1016/j.envres.2021.110777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayenigbara IO, Adeleke OR, Ayenigbara GO, Adegboro JS, Olofintuyi OO. Covid-19 (SARS-CoV-2) pandemic: fears, facts and preventive measures. Germs. 2020;10:218–228. doi: 10.18683/germs.2020.1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett-Itzhaki Z, Levi A (2021) Effects of chronic exposure to ambient air pollutants on COVID-19 morbidity and mortality - a lesson from OECD countries. Environ Res 195:110723 [DOI] [PMC free article] [PubMed]
- Bashir MF, Ma BJ, Bilal KB, Bashir MA, Farooq TH, Iqbal N, Bashir M (2020) Correlation between environmental pollution indicators and COVID-19 pandemic: a brief study in Californian context. Environ Res 187:109652 [DOI] [PMC free article] [PubMed]
- Bianconi V, Bronzo P, Banach M, Sahebkar A, Mannarino MR, Pirro M. Particulate matter pollution and the Covid-19 outbreak: results from Italian regions and provinces. Arch Med Sci. 2020;16:985–992. doi: 10.5114/aoms.2020.95336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilal BMF, Benghoul M, Numan U, Shakoor A, Komal B, Bashir MA, Bashir M, Tan D (2020) Environmental pollution and COVID-19 outbreak: insights from Germany. Air Qual Atmos Health 3:1–10 [DOI] [PMC free article] [PubMed]
- Borisova T, Komisarenko S (2020) Air pollution particulate matter as a potential carrier of SARS-CoV-2 to the nervous system and/or neurological symptom enhancer: arguments in favor. Environ Sci Pollut Res Int:1–7 [DOI] [PMC free article] [PubMed]
- Brandt EB, Mersha TB. Environmental determinants of coronavirus disease 2019 (Covid-19) Curr Allergy Asthma Rep. 2021;21:15. doi: 10.1007/s11882-021-00993-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt EB, Beck AF, Mersha TB. Air pollution, racial disparities, and Covid-19 mortality. J Allergy Clin Immunol. 2020;146:61–63. doi: 10.1016/j.jaci.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calzetta L, Ritondo BL, Coppola A, Matera MG, Di Daniele N, Rogliani P (2021) Factors influencing the efficacy of COVID-19 vaccines: a quantitative synthesis of phase III trials. Vaccines 9(4):341 [DOI] [PMC free article] [PubMed]
- Cascetta E, Henke I, Di Francesco L (2021) The effects of air pollution, sea exposure and altitude on Covid-19 hospitalization rates in Italy. Int J Environ Res Public Health 18 [DOI] [PMC free article] [PubMed]
- Chakrabarty RK, Beeler P, Liu P, Goswami S, Harvey RD, Pervez S, van Donkelaar A, Martin RV. Ambient PM(2.5) exposure and rapid spread of Covid-19 in the United States. Sci Total Environ. 2021;760:143391. doi: 10.1016/j.scitotenv.2020.143391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan A, Singh RP. Decline in PM(2.5) concentrations over major cities around the world associated with Covid-19. Environ Res. 2020;187:109634. doi: 10.1016/j.envres.2020.109634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen PS, Tsai FT, Lin CK, Yang CY, Chan CC, Young CY, Lee CH. Ambient influenza and avian influenza virus during dust storm days and background days. Environ Health Perspect. 2010;118:1211–1216. doi: 10.1289/ehp.0901782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheon JMYY, Yoon YS, Lee ES, Lee JH, Hjuh Y, Mun JW, Jhung WM, Hyun BR. Influence of fine particulate matter 10 on respiratory virus infection in the Republic of Korea. Korean J Fam Med. 2019;9:454–459. doi: 10.21215/kjfp.2019.9.5.454. [DOI] [Google Scholar]
- Chiesa V, Antony G, Wismar M, Rechel B (2021) COVID-19 pandemic: health impact of staying at home, social distancing and 'lockdown' measures-a systematic review of systematic reviews. J Public Health (Oxf) [DOI] [PMC free article] [PubMed]
- Chirizzi D, Conte M, Feltracco M, Dinoi A, Gregoris E, Barbaro E, La Bella G, Ciccarese G, La Salandra G, Gambaro A, Contini D. SARS-CoV-2 concentrations and virus-laden aerosol size distributions in outdoor air in north and south of Italy. Environ Int. 2021;146:106255. doi: 10.1016/j.envint.2020.106255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and Covid-19: a systematic review and meta-analysis. Lancet. 2020;395:1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu B, Zhang S, Liu J, Ma Q, He H. Significant concurrent decrease in PM(2.5) and NO(2) concentrations in China during Covid-19 epidemic. J Environ Sci (China) 2021;99:346–353. doi: 10.1016/j.jes.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, Balakrishnan K, Brunekreef B, Dandona L, Dandona R, Feigin V, Freedman G, Hubbell B, Jobling A, Kan H, Knibbs L, Liu Y, Martin R, Morawska L, Pope CA, III, Shin H, Straif K, Shaddick G, Thomas M, van Dingenen R, van Donkelaar A, Vos T, Murray CJL, Forouzanfar MH. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389:1907–1918. doi: 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collivignarelli MC, Abba A, Bertanza G, Pedrazzani R, Ricciardi P, Carnevale Miino M. Lockdown for CoViD-2019 in Milan: what are the effects on air quality? Sci Total Environ. 2020;732:139280. doi: 10.1016/j.scitotenv.2020.139280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comunian S, Dongo D, Milani C, Palestini P (2020) Air pollution and Covid-19: the role of particulate matter in the spread and increase of Covid-19's morbidity and mortality. Int J Environ Res Public Health 17(12):4487 [DOI] [PMC free article] [PubMed]
- Copat C, Cristaldi A, Fiore M, Grasso A, Zuccarello P, Signorelli SS, Conti GO, Ferrante M. The role of air pollution (PM and NO(2)) in Covid-19 spread and lethality: a systematic review. Environ Res. 2020;191:110129. doi: 10.1016/j.envres.2020.110129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui Y, Zhang ZF, Froines J, Zhao J, Wang H, Yu SZ, Detels R. Air pollution and case fatality of SARS in the People’s Republic of China: an ecologic study. Environ Health. 2003;2:15. doi: 10.1186/1476-069X-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis L (2021) Nutrition is associated with Covid 19 incidence, severity, and mortality. J Infect Dis Ther 9:10000458 ISSN: 2332-0877
- Dave DMD, Sabia J. The contagion externality of a superspreading event: the Sturgis Motorcycle Rally and Covid 19. South Econ J. 2020;10:1–39. doi: 10.1002/soej.12475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donzelli G, Cioni L, Cancellieri M, Llopis-Morales A, Morales-Suarez-Varela M (2021) Relations between air quality and Covid-19 lockdown measures in Valencia, Spain. Int J Environ Res Public Health 18(5):2296 [DOI] [PMC free article] [PubMed]
- van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, de Wit E, Munster VJ. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragone R, Licciardi G, Grasso G, Del Gaudio C, Chanussot J (2021) Analysis of the chemical and physical environmental aspects that promoted the spread of SARS-CoV-2 in the Lombard area. Int J Environ Res Public Health 18(3):1326 [DOI] [PMC free article] [PubMed]
- Dunker S, Hornick T, Szczepankiewicz G, Maier M, Bastl M, Bumberger J, Treudler R, Liebert UG, Simon JC. No SARS-CoV-2 detected in air samples (pollen and particulate matter) in Leipzig during the first spread. Sci Total Environ. 2021;755:142881. doi: 10.1016/j.scitotenv.2020.142881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan Z, Zhan Q, Yang C, Liu H, Zhan M (2020) How did distribution patterns of particulate matter air pollution (PM(2.5) and PM(10)) change in China during the COVID-19 outbreak: a spatiotemporal investigation at Chinese City-level. Int J Environ Res Public Health 17:6724 [DOI] [PMC free article] [PubMed]
- Fattorini D, Regoli F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environ Pollut (Barking, Essex : 1987) 2020;264:114732. doi: 10.1016/j.envpol.2020.114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer G, Sanchez-Gonzalez MA (2021) Effective nasal disinfection as an overlooked strategy in our fight against COVID-19. Ear Nose Throat J 26:1455613211002929 [DOI] [PubMed]
- Fiasca F, Minelli M, Maio D, Minelli M, Vergallo I, Necozione S, Mattei A (2020) Associations between COVID-19 incidence rates and the exposure to PM2.5 and NO(2): a Nationwide observational study in Italy. Int J Environ Res Public Health 17(24):9318 [DOI] [PMC free article] [PubMed]
- Fouladi Dehaghi B, Ghodrati-Torbati A, Teimori G, Ibrahimi Ghavamabadi L, Jamshidnezhad A (2020) Face masks vs. COVID-19: a systematic review. Investigacion y Educacion en Enfermeria 38(2, e13) [DOI] [PMC free article] [PubMed]
- Frontera A, Cianfanelli L, Vlachos K, Landoni G, Cremona G. Severe air pollution links to higher mortality in Covid-19 patients: The “double-hit” hypothesis. J Infect. 2020;81:255–259. doi: 10.1016/j.jinf.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashim BM, Al-Naseri SK, Al-Maliki A, Al-Ansari N. Impact of Covid-19 lockdown on NO(2), O(3), PM(2.5) and PM(10) concentrations and assessing air quality changes in Baghdad, Iraq. Sci Total Environ. 2021;754:141978. doi: 10.1016/j.scitotenv.2020.141978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He C, Hong S, Zhang L, Mu H, Xin A, Zhou Y, Liu J, Liu N, Su Y, Tian Y, Ke B, Wang Y, Yang L. Global, continental, and national variation in PM(2.5), O(3), and NO(2) concentrations during the early 2020 Covid-19 lockdown. Atmos Pollut Res. 2021;12:136–145. doi: 10.1016/j.apr.2021.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendryx M, Luo J. Covid-19 prevalence and fatality rates in association with air pollution emission concentrations and emission sources. Environ Pollut (Barking, Essex : 1987) 2020;265:115126. doi: 10.1016/j.envpol.2020.115126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirose R, Ikegaya H, Naito Y, Watanabe N, Yoshida T, Bandou R, Daidoji T, Itoh Y, Nakaya T (2020) Survival of SARS-CoV-2 and influenza virus on the human skin: importance of hand hygiene in COVID-19. Clin Infect Dis ciaa 1517 [DOI] [PMC free article] [PubMed]
- Horne BD, Joy EA, Hofmann MG, Gesteland PH, Cannon JB, Lefler JS, Blagev DP, Korgenski EK, Torosyan N, Hansen GI, Kartchner D, Pope CA., 3rd Short-term elevation of fine particulate matter air pollution and acute lower respiratory infection. Am J Respir Crit Care Med. 2018;198:759–766. doi: 10.1164/rccm.201709-1883OC. [DOI] [PubMed] [Google Scholar]
- Hou CK, Qin YF, Wang G, Liu QL, Yang XY, Wang H. Impact of a long-term air pollution exposure on the case fatality rate of Covid-19 patients - a multi-city study. J Med Virol. 2021;93:2938–2946. doi: 10.1002/jmv.26807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hradsky O, Komarek A. Demographic and public health characteristics explain large part of variability in Covid-19 mortality across countries. Eur J Pub Health. 2021;31:12–16. doi: 10.1093/eurpub/ckaa226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain M, Sharma GD, Goyal M, Kaushal R, Sethi M (2021) Econometric analysis of COVID-19 cases, deaths, and meteorological factors in South Asia. Environ Sci Pollut Res Int 28(22):28518–28534 [DOI] [PMC free article] [PubMed]
- Jiménez-Ruiz CA, López-Padilla D, Alonso-Arroyo A, Aleixandre-Benavent R, Solano-Reina S, de Granda-Orive JI. Covid-19 and smoking: a systematic review and meta-analysis of the evidence. Arch Bronconeumol. 2021;57(Suppl 1):21–34. doi: 10.1016/j.arbres.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karanasos A, Aznaouridis K, Latsios G, Synetos A, Plitaria S, Tousoulis D, Toutouzas K. Impact of smoking status on disease severity and mortality of hospitalized patients with Covid-19 infection: a systematic review and meta-analysis. Nicotine Tob Res. 2020;22:1657–1659. doi: 10.1093/ntr/ntaa107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirwa K, Eckert CM, Vedal S, Hajat A, Kaufman JD. Ambient air pollution and risk of respiratory infection among adults: evidence from the multiethnic study of atherosclerosis (MESA) BMJ Open Respir Res. 2021;8:e000866. doi: 10.1136/bmjresp-2020-000866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolluru SSR, Patra AK, Nazneen, Shiva Nagendra SM. Association of air pollution and meteorological variables with Covid-19 incidence: evidence from five megacities in India. Environ Res. 2021;195:110854. doi: 10.1016/j.envres.2021.110854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwak KH, Han BS, Park K, Moon S, Jin HG, Park SB, Baik JJ (2021) Inter- and intra-city comparisons of PM(2.5) concentration changes under COVID-19 social distancing in seven major cities of South Korea. Air Qual Atmos Health 11:1–14 [DOI] [PMC free article] [PubMed]
- Landoni G, Lembo R, Cianfanelli L, Frontera A. Air pollutants and SARS-CoV-2 in 33 European countries. Acta Biomed Ateneo Parmense. 2021;92:e2021166. doi: 10.23750/abm.v92i1.11155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson TV, Koenig JQ. Wood smoke: emissions and noncancer respiratory effects. Annu Rev Public Health. 1994;15:133–156. doi: 10.1146/annurev.pu.15.050194.001025. [DOI] [PubMed] [Google Scholar]
- Li L, Li Q, Huang L, Wang Q, Zhu A, Xu J, Liu Z, Li H, Shi L, Li R, Azari M, Wang Y, Zhang X, Liu Z, Zhu Y, Zhang K, Xue S, Ooi MCG, Zhang D, Chan A. Air quality changes during the Covid-19 lockdown over the Yangtze River Delta Region: an insight into the impact of human activity pattern changes on air pollution variation. Sci Total Environ. 2020;732:139282. doi: 10.1016/j.scitotenv.2020.139282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin CI, Tsai CH, Sun YL, Hsieh WY, Lin YC, Chen CY, Lin CS. Instillation of particulate matter 2.5 induced acute lung injury and attenuated the injury recovery in ACE2 knockout mice. Int J Biol Sci. 2018;14:253–265. doi: 10.7150/ijbs.23489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu YNZ, Chen Y, Guo M, Liu L, Gali NM, Sun L, Duan Y, Cai J, Westerdahl D, Liu X, Xu K, Ho K, Kan H, Fu Q, Lan K. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020;582:557–561. doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- Liu Q, Xu S, Lu X (2021) Association between air pollution and COVID-19 infection: evidence from data at national and municipal levels. Environ Sci Pollut Res Int 727:138704 [DOI] [PMC free article] [PubMed]
- López-Feldman A, Heres D, Marquez-Padilla F. Air pollution exposure and Covid-19: a look at mortality in Mexico City using individual-level data. Sci Total Environ. 2021;756:143929. doi: 10.1016/j.scitotenv.2020.143929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma JH, Song SH, Guo M, Zhou J, Liu F, Peng L, Fu ZR. Long-term exposure to PM2.5 lowers influenza virus resistance via down-regulating pulmonary macrophage Kdm6a and mediates histones modification in IL-6 and IFN-β promoter regions. Biochem Biophys Res Commun. 2017;493:1122–1128. doi: 10.1016/j.bbrc.2017.09.013. [DOI] [PubMed] [Google Scholar]
- Marquès M, Domingo JL. Contamination of inert surfaces by SARS-CoV-2: persistence, stability and infectivity. A review. Environ Res. 2020;193:110559. doi: 10.1016/j.envres.2020.110559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matrajt L, Leung T. Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerg Infect Dis. 2020;26:1740–1748. doi: 10.3201/eid2608.201093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechanick JI, Carbone S, Dickerson RN, Hernandez BJD, Hurt RT, Irving SY, Li DY, McCarthy MS, Mogensen KM, Gautier JBO, Patel JJ, Prewitt TE, Rosenthal M, Warren M, Winkler MF, McKeever L. Clinical nutrition research and the Covid-19 Pandemic: a scoping review of the ASPEN COVID-19 Task Force on Nutrition Research. JPEN J Parenter Enteral Nutr. 2021;45:13–31. doi: 10.1002/jpen.2036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meo SA, Abukhalaf AA, Alomar AA, Alessa OM. Wildfire and Covid-19 pandemic: effect of environmental pollution PM-2.5 and carbon monoxide on the dynamics of daily cases and deaths due to SARS-COV-2 infection in San-Francisco USA. Eur Rev Med Pharmacol Sci. 2020;24:10286–10292. doi: 10.26355/eurrev_202010_23253. [DOI] [PubMed] [Google Scholar]
- Meo SA, Abukhalaf AA, Alomar AA, Alessa OM, Sami W, Klonoff DC. Effect of environmental pollutants PM-2.5, carbon monoxide, and ozone on the incidence and mortality of SARS-COV-2 infection in ten wildfire affected counties in California. Sci Total Environ. 2021;757:143948. doi: 10.1016/j.scitotenv.2020.143948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meo SA, Adnan Abukhalaf A, Sami W, Hoang TD (2021b) Effect of environmental pollution PM2.5, carbon monoxide, and ozone on the incidence and mortality due to SARS-CoV-2 infection in London, United Kingdom. J King Saud Univ Sci 33:101373 [DOI] [PMC free article] [PubMed]
- Middleton N (2020): UN program-impacts of sand and dust stors on oceans: a scientoific environmental assessment for policy makers. Available at https://www.unep.org/resources/report/impacts-sand-and-dust-storms-oceans. Accessed 30 July 2021
- Naeher LP, Brauer M, Lipsett M, Zelikoff JT, Simpson CD, Koenig JQ, Smith KR. Woodsmoke health effects: a review. Inhal Toxicol. 2007;19:67–106. doi: 10.1080/08958370600985875. [DOI] [PubMed] [Google Scholar]
- Navarro KM, Clark KA, Hardt DJ, Reid CE, Lahm PW, Domitrovich JW, Butler CR, Balmes JR. Wildland firefighter exposure to smoke and Covid-19: a new risk on the fire line. Sci Total Environ. 2021;760:144296. doi: 10.1016/j.scitotenv.2020.144296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nor NSM, Yip CW, Ibrahim N, Jaafar MH, Rashid ZZ, Mustafa N, Hamid HHA, Chandru K, Latif MT, Saw PE, Lin CY, Alhasa KM, Hashim JH, Nadzir MSM. Particulate matter (PM(2.5)) as a potential SARS-CoV-2 carrier. Sci Rep. 2021;11:2508. doi: 10.1038/s41598-021-81935-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nussbaumer-Streit B, Mayr V, Dobrescu AI, Chapman A, Persad E, Klerings I, Wagner G, Siebert U, Christof C, Zachariah C, Gartlehner G. Quarantine alone or in combination with other public health measures to control Covid-19: a rapid review. Cochrane Database Syst Rev. 2020;4:Cd013574. doi: 10.1002/14651858.CD013574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogen Y. Assessing nitrogen dioxide (NO(2)) levels as a contributing factor to coronavirus (Covid-19) fatality. Sci Total Environ. 2020;726:138605. doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paital B, Agrawal PK (2020) Air pollution by NO2 and PM2.5 explains COVID-19 infection severity by overexpression of angiotensin-converting enzyme 2 in respiratory cells: a review. Environ Chem Lett 18:1–18 [DOI] [PMC free article] [PubMed]
- Pei L, Wang X, Guo B, Guo H, Yu Y (2021) Do air pollutants as well as meteorological factors impact Corona virus disease 2019 (COVID-19)? Evidence from China based on the geographical perspective. Environ Sci Pollut Res Int 28(27):35584–35596 [DOI] [PMC free article] [PubMed]
- Phillips N, Park IW, Robinson JR, Jones HP (2020) The perfect storm: COVID-19 health disparities in US blacks. J Racial Ethn Health Disparities 23:1–8 [DOI] [PMC free article] [PubMed]
- Pradhan D, Biswasroy P, Kumar Naik P, Ghosh G, Rath G. A review of current interventions for Covid-19 prevention. Arch Med Res. 2020;51:363–374. doi: 10.1016/j.arcmed.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raciti L, Calabrò RS. Can volcanic trace elements facilitate Covid-19 diffusion? A hypothesis stemming from the Mount Etna area, Sicily. Med Hypotheses. 2020;144:110058. doi: 10.1016/j.mehy.2020.110058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajak P, Ganguly A, Sarkar S, Mandi M, Dutta M, Podder S, Khatun S, Roy S (2021) Immunotoxic role of organophosphates: an unseen risk escalating SARS-CoV-2 pathogenicity. Food Chem Toxicol 149:112007 [DOI] [PMC free article] [PubMed]
- Reche I, D'Orta G, Mladenov N, Winget DM, Suttle CA. Deposition rates of viruses and bacteria above the atmospheric boundary layer. ISME J. 2018;12:1154–1162. doi: 10.1038/s41396-017-0042-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy RK, Charles WN, Sklavounos A, Dutt A, Seed PT, Khajuria A. The effect of smoking on Covid-19 severity: a systematic review and meta-analysis. J Med Virol. 2021;93:1045–1056. doi: 10.1002/jmv.26389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid CE, Brauer M, Johnston FH, Jerrett M, Balmes JR, Elliott CT. Critical review of health impacts of wildfire smoke exposure. Environ Health Perspect. 2016;124:1334–1343. doi: 10.1289/ehp.1409277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez M, Palop ML, Seseña S, Rodríguez A. Are the portable air cleaners (PAC) really effective to terminate airborne SARS-CoV-2? Sci Total Environ. 2021;785:147300. doi: 10.1016/j.scitotenv.2021.147300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Urrego D, Rodríguez-Urrego L. Air quality during the Covid-19: PM(2.5) analysis in the 50 most polluted capital cities in the world. Environ Pollut (Barking, Essex : 1987) 2020;266:115042. doi: 10.1016/j.envpol.2020.115042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romano Spica V, Gallè F, Baldelli G, Valeriani F, Di Rosa E, Liguori G, Brandi G. Swimming pool safety and prevention at the time of Covid-19: a consensus document from GSMS-SItI. Ann Ig. 2020;32:439–448. doi: 10.7416/ai.2020.2368. [DOI] [PubMed] [Google Scholar]
- Rooney CM, Moura IB, Wilcox MH. Tracking Covid-19 via sewage. Curr Opin Gastroenterol. 2021;37:4–8. doi: 10.1097/MOG.0000000000000692. [DOI] [PubMed] [Google Scholar]
- Roviello V, Roviello GN (2020) Lower COVID-19 mortality in Italian forested areas suggests immunoprotection by Mediterranean plants. Environ Chem Lett 14:1–12 [DOI] [PMC free article] [PubMed]
- Sahoo MM (2021) Significance between air pollutants, meteorological factors, and Covid-19 infections: probable evidences in India. Environ Sci Pollut Res Int 28(30):40474–40495 [DOI] [PMC free article] [PubMed]
- Salah HM, Sharma T, Mehta J. Smoking doubles the mortality risk in Covid-19: a meta-analysis of recent reports and potential mechanisms. Cureus. 2020;12:e10837. doi: 10.7759/cureus.10837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samavati L, Uhal BD. ACE2, much more than just a receptor for SARS-COV-2. Front Cell Infect Microbiol. 2020;10:317. doi: 10.3389/fcimb.2020.00317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senatore V, Zarra T, Buonerba A, Choo KH, Hasan SW, Korshin G, Li CW, Ksibi M, Belgiorno V, Naddeo V. Indoor versus outdoor transmission of SARS-COV-2: environmental factors in virus spread and underestimated sources of risk. Euro-Mediterr J Environ Integr. 2021;6:30. doi: 10.1007/s41207-021-00243-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setti L, Passarini F, De Gennaro G, Barbieri P, Perrone MG, Borelli M, Palmisani J, Di Gilio A, Torboli V, Fontana F, Clemente L, Pallavicini A, Ruscio M, Piscitelli P, Miani A. SARS-Cov-2RNA found on particulate matter of Bergamo in Northern Italy: first evidence. Environ Res. 2020;188:109754. doi: 10.1016/j.envres.2020.109754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma GD, Bansal S, Yadav A, Jain M, Garg I. Meteorological factors, Covid-19 cases, and deaths in top 10 most affected countries: an econometric investigation. Environ Sci Pollut Res Int. 2021;28:28624–28639. doi: 10.1007/s11356-021-12668-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Signorelli C, Odone A. Age-specific Covid-19 case-fatality rate: no evidence of changes over time. Int J Public Health. 2020;65:1435–1436. doi: 10.1007/s00038-020-01486-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skalny AV, Lima TRR, Ke T, Zhou JC, Bornhorst J, Alekseenko SI, Aaseth J, Anesti O, Sarigiannis DA, Tsatsakis A, Aschner M, Tinkov AA. Toxic metal exposure as a possible risk factor for Covid-19 and other respiratory infectious diseases. Food Chem Toxicol. 2020;146:111809. doi: 10.1016/j.fct.2020.111809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slama K, Chiang CY, Enarson DA, Hassmiller K, Fanning A, Gupta P, Ray C. Tobacco and tuberculosis: a qualitative systematic review and meta-analysis. Int J Tuber Lung Dis. 2007;11:1049–1061. [PubMed] [Google Scholar]
- Solimini A, Filipponi F, Fegatelli DA, Caputo B, De Marco CM, Spagnoli A, Vestri AR. A global association between Covid-19 cases and airborne particulate matter at regional level. Sci Rep. 2021;11:6256. doi: 10.1038/s41598-021-85751-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastava A. Covid-19 and air pollution and meteorology-an intricate relationship: a review. Chemosphere. 2021;263:128297. doi: 10.1016/j.chemosphere.2020.128297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastava AK, Bhoyar PD, Kanawade VP, Devara PCS, Thomas A, Soni VK. Improved air quality during Covid-19 at an urban megacity over the Indo-Gangetic Basin: from stringent to relaxed lockdown phases. Urban Clim. 2021;36:100791. doi: 10.1016/j.uclim.2021.100791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stieb DM, Evans GJ, To TM. Brook JR, Burnett RT. An ecological analysis of long-term exposure to PM(2.5) and incidence of Covid-19 in Canadian health regions. Environ Res. 2020;191:110052. doi: 10.1016/j.envres.2020.110052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su W, Wu X, Geng X, Zhao X, Liu Q, Liu T. The short-term effects of air pollutants on influenza-like illness in Jinan, China. BMC Public Health. 2019;19:1319. doi: 10.1186/s12889-019-7607-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao RJ, Cao WJ, Li MH, Yang L, Dai RX, Luo XL, Liu Y, Ge BX, Su X, Xu JF. PM2.5 compromises antiviral immunity in influenza infection by inhibiting activation of NLRP3 inflammasome and expression of interferon-β. Mol Immunol. 2020;125:178–186. doi: 10.1016/j.molimm.2020.07.001. [DOI] [PubMed] [Google Scholar]
- Thu TPB, Ngoc PNH, Hai NM, Tuan LA. Effect of the social distancing measures on the spread of Covid-19 in 10 highly infected countries. Sci Total Environ. 2020;742:140430. doi: 10.1016/j.scitotenv.2020.140430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travaglio M, Yu Y, Popovic R, Selley L, Leal NS, Martins LM. Links between air pollution and Covid-19 in England. Environ Pollut (Barking, Essex : 1987) 2021;268:115859. doi: 10.1016/j.envpol.2020.115859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripepi G, Plebani M, Iervasi G, Gori M, Leonardis D, D'Arrigo G, Fusaro M (2021) Distance from the outbreak of infection, ozone pollution and public health consequences of SARS-CoV-2 epidemic: the HOPE method. Eur J Pub Health 31(1):7–12 [DOI] [PMC free article] [PubMed]
- Tung NT, Cheng PC, Chi KH, Hsiao TC, Jones T, BeruBe K, Ho KF, Chuang HC. Particulate matter and SARS-CoV-2: a possible model of Covid-19 transmission. Sci Total Environ. 2021;750:141532. doi: 10.1016/j.scitotenv.2020.141532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasquez-Apestegui V, Parras-Garrido E, Tapia V, Paz-Aparicio VM, Rojas JP, Sanchez-Ccoyllo OR, Gonzales GF (2020) Association between air pollution in Lima and the high incidence of COVID-19: findings from a post hoc analysis. Research Square. 10.21203/rs.3.rs-39404/v1 [DOI] [PMC free article] [PubMed]
- Wong LSY, Loo EXL, Kang AYH, Lau HX, Tambyah PA, Tham EH. Age-related differences in immunological responses to SARS-CoV-2. J Allergy Clin Immunol Pract. 2020;8:3251–3258. doi: 10.1016/j.jaip.2020.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X, Nethery RC, Sabath BM, Braun D, Dominici F (2020) Exposure to air pollution and COVID-19 mortality in the United States: a nationwide cross-sectional study. MedRxiv. 10.1101/2020.04.05.20054502
- Xu J, Xiao X, Zhang W, Xu R, Kim SC, Cui Y, Howard TT, Wu E, Cui Y. Air-filtering masks for respiratory protection from PM(2.5) and pandemic pathogens. One Earth (Cambridge, Mass) 2020;3:574–589. doi: 10.1016/j.oneear.2020.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y, Pan J, Wang W, Liu Z, Kan H, Qiu Y, Meng X, Wang W. Association of particulate matter pollution and case fatality rate of Covid-19 in 49 Chinese cities. Sci Total Environ. 2020;741:140396. doi: 10.1016/j.scitotenv.2020.140396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y, Pan J, Liu Z, Meng X, Wang W, Kan H, Wang W. Ambient nitrogen dioxide pollution and spreadability of Covid-19 in Chinese cities. Ecotoxicol Environ Saf. 2021;208:111421. doi: 10.1016/j.ecoenv.2020.111421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youssouf H, Liousse C, Roblou L, Assamoi EM, Salonen RO, Maesano C, Banerjee S, Annesi-Maesano I. Non-accidental health impacts of wildfire smoke. Int J Environ Res Public Health. 2014;11:11772–11804. doi: 10.3390/ijerph111111772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H, Ma S, Han T, Qu G, Cheng C, Uy JP, Shaikh MB, Zhou Q, Song EJ, Sun C (2021) Association of smoking history with severe and critical outcome in Covid-19 patients: a systemic review and meta-analysis. Eur J Integr Med 101313 [DOI] [PMC free article] [PubMed]
- Zheng P, Chen Z, Liu Y, Song H, Wu CH, Li B, Kraemer MUG, Tian H, Yan X, Zheng Y, Stenseth NC, Jia G (2021) Association between coronavirus disease 2019 (COVID-19) and long-term exposure to air pollution: evidence from the first epidemic wave in China. Environmental Pollution (Barking, Essex: 1987) 276:116682 [DOI] [PMC free article] [PubMed]
- Zhu Y, Xie J, Huang F, Cao L. Association between short-term exposure to air pollution and Covid-19 infection: evidence from China. Sci Total Environ. 2020;727:138704. doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data were based on already published articles.