Abstract
This article describes a rationale and approach for modifying the traditional rural-urban commuting area (RUCA) coding scheme used to classify U.S. ZIP codes to enable suburban/rural vs. urban core comparisons in health outcomes research that better reflect current geographic differences in access to care in U.S. populations at risk for health disparities. The proposed method customization is being employed in the Patient-Centered Outcomes Research Institute-funded Management Of Diabetes in Everyday Life (MODEL) study to assess heterogeneity of treatment effect for patient-centered diabetes self-care interventions across the rural-urban spectrum. The proposed suburban/rural vs. urban core classification scheme modification is based on research showing that increasing suburban poverty and rapid conversion of many rural areas into suburban areas in the U.S. has resulted in similar health care access problems in areas designated as rural or suburban.
-
•
The RUCA coding scheme was developed when a much higher percentage of U.S. individuals resided in areas with very low population density.
-
•
Using the MODEL study example, this study demonstrates that the RUCA classification scheme using ZIP codes does not reflect real differences in health care access experienced by medically underserved study participants.
-
•
Both internal and external validation data suggest that the proposed suburban/rural vs. urban core customization of the RUCA geographic coding scheme better reflects real differences in healthcare access and is better able to assess the differential impact of clinical interventions designed to address geographic differences in access among vulnerable populations.
Keywords: Urban-rural classification, Diabetes, Medically underserved populations, Patient-centered outcomes research, Multiple chronic conditions, African American
Graphical abstract

Reclassification of Rural/Urban Classification Scheme from the Traditional Rural–urban Commuting Area (RUCA) ZIP code classification scheme to an Alternative Classification based on the research of Schanke-Mahl and colleagues.
Specifications table
| Subject Area: | Medicine and Dentistry |
| More specific subject area: | Public Health |
| Method name: | Multi-tiered Rural-Urban Commuting Area (RUCA)-ZIP code classification scheme |
| Name and reference of original method: | Hall SA, Kaufman JS, Ricketts TC. Defining urban and rural areas in U.S. epidemiologic studies. J Urban Health. 2006 Mar;83(2):162–75. doi: 10.1007/s11524–005–9016–3. |
| Resource availability: | Schnake-Mahl AS, Sommers BD. Health Care In The Suburbs: An Analysis Of Suburban Poverty And Health Care Access. Health Aff (Millwood) 2017;36:1777–85. |
Method details
Background
There are many alternative ways to categorize geographic areas to look at rural-urban differences in clinical, health services, and patient-centered outcomes research (PCOR), and the method chosen depends on the specific areas and conditions studied [1]. Historically, rural-urban classification schemes used in public health research have employed simple dichotomous classification approaches such as the Multi-tiered Rural-Urban Commuting Area (RUCA) ZIP code classification scheme [2,3]. This scheme classifies census tracts by using information on population density, urbanization, and daily commuting and by transferring tract-based RUCA classifications to ZIP code areas [4]. This classification method was developed when a much higher percentage of U.S. individuals resided in areas with very low population density. But for health outcomes research interventions designed to address geographic differences in access experienced by populations at risk for disparities in today's world, rural-urban classification schemes employed must reflect current geographic differences in access to care.
Rural areas are known to have higher proportions of uninsured, underinsured, and poor residents, and poor access to care, higher costs of health care services, and longer travel time when compared to urban residents [1]. However, studies have highlighted the difficulties low-income and minority suburban residents experience accessing health care [5]. Recent evidence documents (1): the growing difficulties low-income suburban residents face accessing health care [6]. (2) national trends of increasing suburban poverty [6,7], (3) rapid conversion of many rural areas into suburban areas [8], and (4) similar access to health care and transportation barriers in rural and suburban areas [5,7,9], As described by Van Dam, since the 1950s rural counties surrounding urban areas have rapidly converted into suburban areas by increasing in population, getting reclassified as urban, and joining major metropolitan statistical areas [8]. Suburban poverty is particularly increasing among communities of color through the negative effects of gentrification that has pushed minority populations out of cities to suburban locations to seek better housing opportunities [10], [11], [12], [13]. But even in suburban neighborhoods, historical racial residential segregation often continues, albeit in a new form. For instance in the Memphis Metropolitan Statistical Area, about 43% of suburban poor are living in high poverty or distressed neighborhoods [7].
These national trends of rapid conversion of many rural areas into suburban areas, increasing suburban minority populations, and increasing suburban poverty [5]. demand that traditional rural-urban classification methods be revised. This research suggests that suburban/rural vs. urban comparisons may be more appropriate for assessing differential geographic impact of interventions designed to help overcome transportation burdens associated with accessing health care. Suburban/rural vs. urban customizations of the RUCA geographic coding scheme may better reflect real differences in healthcare access and be better able to assess the differential impact of clinical interventions designed to address geographic differences in access.
Setting
The Patient-Centered Outcomes Research Institute (PCORI)-funded Management Of Diabetes in Everyday Life (MODEL) Study is pragmatic clinical trial that aims to examine the comparative effectiveness of text messaging, health coaching, and enhanced usual care in African American adults with uncontrolled diabetes and multiple chronic health conditions in medically underserved areas [1,2]. Data shows that the majority of African Americans (33.2 million or 79.6%) live in HRSA-designated primary care health professional shortage areas and in high-density African American communities [2]. These high-density African American communities are mostly entirely urban or suburban. In this paper we compare the RUCA ZIP code “Categorization C” approximation classification scheme [2,3]. with other customizations of this scheme based on alternative urban/rural classification methods in order to identify the best approach for assessing heterogeneity of treatment effect for alternative patient-centered diabetes self-care interventions across the rural-urban spectrum. We were particularly interested in identifying best classification schemes for the medically underserved African American population with diabetes and multiple chronic conditions targeted by the MODEL Study.
This method was prepared in January 2018, during the early recruitment phase of the MODEL Study. During this phase, we were recruiting patients from a total of eight practices. Initially, as part of the MODEL Study evaluation plan, we proposed using the RUCA ZIP code classification method to classify patient's residence as rural vs. urban [1]. We used this method because of the availability of ZIP code information for the study participants and this method is widely used in health services research and pragmatic clinical trials [1]. Our outlying MODEL core clinics located in Jackson, TN; Covington, TN; and Holly Springs, MS, all self-identified as rural, serving predominantly rural populations. In their preliminary estimates provided to our research team, these clinics estimated that between 50 and 85% of their patients resided in rural areas. We chose the core MODEL study sites to reflect the diversity of primary care practice sites in our area, as well as other medically underserved areas (MUA) nationwide. The characteristics of the diabetes patients served by these practices mirror those of the larger national target population of approximately 10 million African American adults of similar age, residing in MUA. Most recent estimates show that a substantial majority of African Americans live in urban or suburban areas—in metropolitan areas like Memphis, which has the 6th highest African American population of any city in the country [3]. Only 10% live in rural communities [5]. However, a year after we started recruiting patients for the MODEL study, we became aware that the RUCA ZIP code classification scheme was inappropriate for our geographic area and the population served by the study because a large majority of patients recruited from practices located in Jackson, TN; Covington, TN; and Holly Springs, MS were being classified as urban patients.
-
•
Inadequacy of multi-tiered rural–urban commuting area (RUCA) ZIP code classification scheme
As shown in Fig. 1, nearly all of the medically underserved geographic areas served by the MODEL program are classified as urban under the RUCA categorization scheme. Under the RUCA scheme eight of our participating core MODEL clinics are located in urban areas and well over 90% of the patients served by these core MODEL clinics reside in urban areas. Of note, many of the ZIP codes above which are now categorized as urban according to the RUCA methodology were categorized as rural as recently as 2004, attesting to the progressive urbanization of rural areas in the Mid-South over the last 20 years [14,15]. Even though most of our initially classified “rural” sites are located in and primarily serve “urban” ZIP codes according to the RUCA categorization, the people living in these areas report that they live in rural areas. This is consistent with recent research that demonstrates extremely poor concordance between rural-urban self-identification and RUCA designation [16]. Further, these areas associated with self-identified “rural” clinic sites have low population density, lack public bus service, are highly agricultural, and, with the exception of Jackson (population 67,005), they lack major urban nuclei with greater than 50,000 people [17].
Fig. 1.
Rural vs. urban designation of the geographic area served by the Management of Diabetes in Everyday Life (MODEL) Study according to the Multi-tiered Rural–urban Commuting Area (RUCA) ZIP code classification scheme.
As shown in Table 1, the high-density African American counties served by the MODEL program are predominantly urban according to the RUCA categorization scheme. Table 1 also shows evidence of another important differentiator with regard to access to health care for African American patients. Patients living in the central metro area of Shelby County have ready access to public transportation, while those outside of Shelby County central metro area do not. Table 2 shows that there are very few adult African American patients with diabetes living in RUCA-defined rural ZIP codes in the Mid-South. Thus, these data suggest that the RUCA rural-urban classification scheme does not differentiate medically underserved African American patients with diabetes in the Mid-South region on the basis of access to healthcare. Thus, the RUCA classification scheme is unlikely to be helpful in assessing heterogeneity of treatment effect across the rural-urban spectrum.
Table 1.
Comparison of alternative categorization schemes and rural–urban commuting area (RUCA) categorization for high-density african-american and medically underserved geographic areas served by MODEL program.
| State/County (City) | Core Model Clinics | Public Bus Service | NCHS Categorization | U.S Census Categorization | Categorization based on Schanke-Mahl and colleagues | RUCA Categorization* |
|---|---|---|---|---|---|---|
| Tennessee Shelby (Memphis) | Christ Community | Yes | 1—Large Central Metro | 1—Urbanized | 1—Center City | 38,104 (1.0, Urban) |
| Raleigh | Yes | 3,810,8 (,1.0,, U,rba,n) | ||||
| Third Street | Yes | 3,811,5 (,1.0,, U,rba,n) | ||||
| Eastmoreland | Yes | 3,812,6 (,1.0,, U,rba,n) | ||||
| Memphis Health Center | Yes | 3,813,0 (,1.0,, U,rba,n) | ||||
| Motley Intern. Medicine | Yes | 3,813,5 (,1.0,, U,rba,n) | ||||
| UTMP | Yes | 3,814,1 (,1.0,, U,rba,n) | ||||
| Madison (Jackson) | UT Family Medicine (Largest rural site) | Yes, but limited to Jackson urban core (ZIP codes 38,301–38,305) | 4—Small Metro | 1—Urbanized | 2—Suburban/Rural | 38,301 (1.0, Urban) |
| 3,830,5 (,1.0,, U,rba,n) | ||||||
| 3,831,3 (,2.0,, U,rba,n) | ||||||
| 3,835,6 (,2.0,, U,rba,n) | ||||||
| 3,836,6 (,2.0,, U,rba,n) | ||||||
| 3,839,1 (,2.0,, U,rba,n) | ||||||
| 3,839,2 (,2.0,, U,rba,n) | ||||||
| Tipton (Covington) | Tipton Family Med. Center (Rural site) | No | 2—Large Fringe Metro | 2—Urban Cluster/Rural | 2—Suburban/Rural | 38,004 (2.0, Urban) |
| 3,801,5 (,2.0,, U,rba,n) | ||||||
| 3,801,9 (,7.1,, U,rba,n) | ||||||
| 3,802,3 (,2.0,, U,rba,n) | ||||||
| 3,804,9 (,2.0,, U,rba,n) | ||||||
| 3,805,8 (,2.0,, U,rba,n) | ||||||
| Haywood | -Near Jackson- | No | 6—Non-Core | 1—Urbanized | 2—Suburban/Rural | 38,012 (7.1, Urban) |
| 3,806,9 (,3.0,, R,ura,l) | ||||||
| Hardeman | -Near Jackson- | No | 6—Non-Core | 2—Urban Cluster/Rural | 2—Suburban/Rural | 38,008 (7.1, Urban) |
| 3,803,9 (,2.0,, U,rba,n) | ||||||
| 3,804,2 (,7.1,, U,rba,n) | ||||||
| 3,804,4 (,8.1,, U,rba,n) | ||||||
| ,380,52 ,(3.,0,U,rba,n) | ||||||
| ,380,61 ,(3.,0,U,rba,n) | ||||||
| 3,806,7 (,2.0,, U,rba,n) | ||||||
| 38,075, (1,0.3,, R,ura,l) | ||||||
| 3,837,7 (,7.1,, U,rba,n) | ||||||
| 3,838,1 (,8.1,, U,rba,n) | ||||||
| McNairy | -Near Jackson- | No | 6—Non-Core | 2—Urban Cluster/Rural | 2—Suburban/Rural | 38,310 (10.3, Rural) |
| 3,833,4 (,9.0,, R,ura,l) | ||||||
| 38,359, (1,0.3,, R,ura,l) | ||||||
| 3,837,5 (,7.0,, R,ura,l) | ||||||
| 3,837,9 (,9.0,, R,ura,l) | ||||||
| Mississippi | Hawkins Family Practice (Rural site) | No | 2 – Large Fringe Metro | 2—Urban cluster/Rural | 2—Suburban/Rural | 38,635 (2.0, Urban) |
| Marshall (Holly | 38,642, (2,.0,, Ur,ban,) | |||||
| Springs) | 3,866,1 (,2.0,, U,rba,n) | |||||
| 3,868,5 (,2.0,, U,rba,n) | ||||||
| Lafayette | -Near Holly Springs- | No | 5—Micropolitan | 1—Urbanized | 2—Suburban/Rural | 38,601 (5.0, Rural) |
| 3,865,5 (,4.0,, R,ura,l) | ||||||
| 3,867,3 (,4.0,, R,ura,l) | ||||||
| 3,894,9 (,5.0,, R,ura,l) | ||||||
| Tate | -Near Holly Springs- | No | 2 – Large Fringe Metro | 2—Urban cluster/Rural | 2—Suburban/Rural | 38,618 (2.0, Urban) |
| 3,863,8 (,2.0,, U,rba,n) | ||||||
| 3,866,8 (,2.0,, U,rba,n) |
* Representative ZIP codes categorized according to the multi-tiered Rural–Urban Commuting Area (RUCA)–ZIP code “Categorization C” approximation.
Table 2.
Number and characteristics of african-american adults living with diabetes in RUCA-defined rural ZIP codes in the mid-south.
| County | RUCA rural ZIP codes | Total Population in rural ZIP codes* | Total Adults (≥ 18) N (%)* | African- American Adults N (%)* | African- American (AA) Adults with Diabetes N (%)+ | No. Rural AA Adults with Diabetes adults# | |
|---|---|---|---|---|---|---|---|
| Counties with MODEL clinics | Shelby, TN | N/A | N/A | N/A | N/A | 927,644 (12) | N/A |
| Madison, TN | N/A | N/A | N/A | N/A | 98,294 (13) | N/A | |
| Marshall, MS | N/A | N/A | N/A | N/A | 37,144 (14) | N/A | |
| Tipton, TN | N/A | N/A | N/A | N/A | 61,081 (12.5) | N/A | |
| Counties adjacent to MODEL clinics | Fayette, TN | N/A | N/A | N/A | N/A | 38,413 (14.8) | N/A |
| Lauderdale, TN | 38,037 | 1773 | 1352 (76.3) | 485 (27.4%) | 27,815 (14.6) | 54 | |
| 38,040 | 5193 | 3863 (74.4) | 837 (16.1%) | 91 | |||
| 38,041 | 5085 | 4480 (88.1) | 2515 (49.5%) | 324 | |||
| 38,063 | 17,043 | 12,373 (72.6) | 6092 (35%) | 632 | |||
| Haywood, TN | N/A | N/A | N/A | N/A | 18,787 (13.2) | N/A | |
| Crockett, TN | N/A | N/A | N/A | N/A | 14,586 (11.9) | N/A | |
| Gibson, TN | 38,233 | 2852 | 2213 (77.6) | 216 (7.6%) | 49,683 (11.3) | 19 | |
| 38,316 | 2917 | 2269 (77.8) | 104 (3.6%) | 9 | |||
| 38,330 | 4404 | 3329 (75.6) | 514 (11.7%) | 44 | |||
| 38,369 | 1887 | 1441 (76.4) | 228 (12.1%) | 20 | |||
| 38,382 | 9515 | 3425 (36.0) | 1685 (17.7%) | 68 | |||
| Carroll, TN | 38,201 | 10,093 | 7943 (78.7) | 959 (9.5%) | 28,522 (12.3) | 93 | |
| 38,220 | 1849 | 1449 (78.4) | 257 (13.9%) | 25 | |||
| 38,235 | 441 | 325 (73.7) | 51 (11.6%) | 5 | |||
| 38,258 | 1500 | 1174 (78.3) | 222 (14.8%) | 21 | |||
| 38,317 | 2537 | 1963 (77.4) | 150 (5.9%) | 14 | |||
| 38,318 | 476 | 368 (77.3) | 9 (1.9%) | 1 | |||
| 38,342 | 1438 | 1107 (77.0) | 62 (4.3%) | 6 | |||
| 38,387 | 375 | 306 (81.6) | 13 (3.5%) | 1 | |||
| 38,390 | 907 | 703 (77.5) | 39 (4.3%) | 4 | |||
| Henderson, TN | 38,328 | 730 | 562 (77.1) | 8 (1.1%) | 27,769 (13.9) | 1 | |
| 38,368 | 1985 | 1504 (75.8) | 15 (0.8%) | 2 | |||
| 38,371 | 1235 | 974 (78.9) | 3 (0.2%) | 0 | |||
| 38,388 | 1840 | 1407 (76.5) | 378 (20.5%) | 40 | |||
| Chester, TN | N/A | N/A | N/A | N/A | 17,131 (13.4) | N/A | |
| Hardeman, TN | 38,075 | 6936 | 6060 (87.3) | 3692 (53.2) | 27,253 (13.3) | 429 | |
| DeSoto, MS | N/A | N/A | N/A | N/A | 161,252 (13) | N/A | |
| Tate, MS | N/A | N/A | N/A | N/A | 28,886 (15.1) | N/A | |
| Lafayette, MS | 38,601 | 2371 | 1764 (74.4) | 1171 (49.4%) | 47,351 (11.4) | 99 | |
| 38,655 | 36,699 | 29,542(80.5) | 8731 (23.8%) | 801 | |||
| 38,673 | 746 | 549 (73.7) | 492 (66%) | 41 | |||
| 38,677 | 4198 | 4168 (99.3) | 635 (15.1%) | 72 | |||
| 38,949 | 297 | 218 (73.7) | 11 (3.7%) | 1 | |||
| Benton, MS | N/A | N/A | N/A | N/A | 8729 (13.8) | N/A | |
| Union, MS | 38,627 | 1120 | 837 (74.8) | 27 (2.4%) | 27,134 (10.1) | 2 | |
| 38,650 | 3881 | 2883 (74.3) | 270 (7%) | 20 | |||
| 38,652 | 16,600 | 12,317 (74.2) | 3305 (19.9%) | 247 | |||
| 38,828 | 3970 | 2961 (74.6) | 254 (6.4%) | 19 | |||
| Total: | 3205 |
U.S. Census, 2010.
BRFSS, 2013.
**Estimate based on the product number of adults in column (iv) and percentage of African Americans in column (v).
Estimate based on the product of percentage diabetics in county in column (vi) and estimated number of African American adults in column (vii).
Technical steps
Our method for customizing the RUCA ZIP code “Categorization C” approximation classification scheme simply involves reassigning ZIP Codes to alternative categories based on alternative theoretical models or classification schemes. The alternative classification schemes include the NCHS classification scheme, the U.S. Census classification scheme, and a scheme developed based on the work of Schnake-Mahl and colleagues. We used different categorization schemes and compared them with RUCA for medically underserved geographic areas served by the MODEL Program (Table 1). Additionally, we created a patient-level dataset with a list of ZIP Codes for the MODEL participants. We created variables for each classification scheme and assigned ZIP Codes to categories based on the classification scheme. As shown in Table 3, we examined the number and proportion of patients assigned to suburban/rural and urban categories based on RUCA and alternative classification schemes.
Table 3.
Reclassification of MODEL study participants based on urban-rural classification schemes*.
| Urban-Rural Classification Scheme |
||||
|---|---|---|---|---|
| RUCA | Option 1 (Schnake-Mahl) | Option 2 (NCHS) | Option 3 (U.S. Census) | |
| Urban, No. (%) | 133 | 106 | 110 | 119 |
| Suburban/Rural, No. (%) | 6 | 33 | 29 | 19 |
| Reclassified, No. (%) | 0 (0) | 27 (19.4) | 23 (16.5) | 13 (11.5) |
MODEL study participants were reclassified using their residence ZIP codes.
Method validation for alternative rural-urban classification schemes
Given the issues above, there are several alternative urban/rural categorization schemes that are more appropriate and informative for our region. We conducted a systematic review of different approaches used to classify urban rural areas in the U.S. In the following sections, we outline three major alternative rural-urban classification schemes and their respective advantages and disadvantages:
-
•
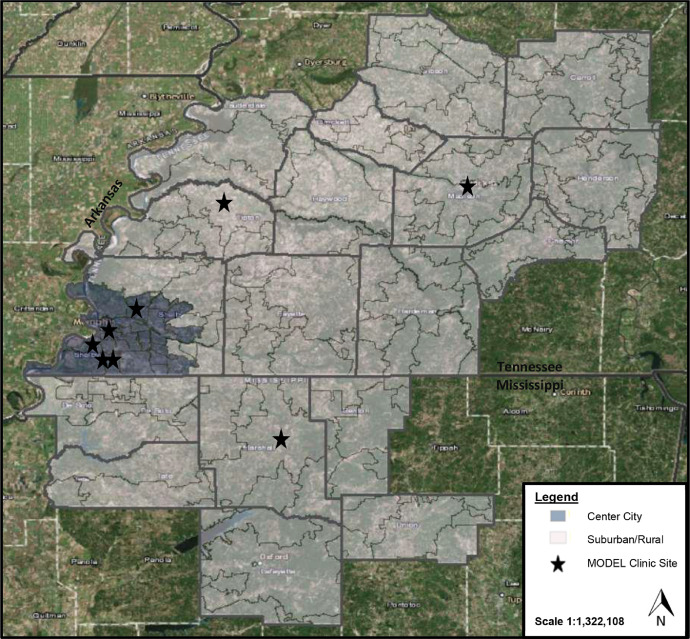
Option 1: Suburban/rural vs. urban core classification scheme.
This customization of the RUCA ZIP code classification is based on the work of Schnake-Mahl and colleagues and this classification scheme is illustrated in Fig. 2. This scheme contrasts suburban/rural areas and metropolitan statistical area center city areas (urban core) served by the MODEL Program. The study by Schnake-Mahl and colleagues highlighted the need to consider suburban populations and not just focus on urban and rural areas, particularly when suburban poor population continues to increase [5]. The conceptual definition of urban, suburban, and rural areas is based on the census definition, defining urban as center city only, suburban as areas outside of center city but inside the county that includes the center city and the areas inside the suburban county of the MSA. Rural areas are outside of MSA. Although, Schnake-Mahl and colleagues considered urban, suburban, and rural areas separately, the decision to combine rural with suburban areas is supported by evidence showing similar access to care and transportation barriers for patients living in rural and suburban areas (Table 1) [5,7,9].
-
•
Option 2: Suburban/rural vs. large central metropolitan classification scheme
Fig. 2.
Suburban/rural vs. urban core designation of the geographic area served by the Management of Diabetes in Everyday Life (MODEL) Study based on the research of Schanke-Mahl and colleagues.
This customization of the RUCA ZIP code classification is based on the National Center for Health Statistics (NCHS) classification scheme and is illustrated in Fig. 3. This scheme contrasts suburban/rural and large central metropolitan areas served by the MODEL Program. This classification is based on 2010 Office of Management and Budget's (OMB) standards [18]. The NCHS has developed a six-level urban-rural classification scheme for U.S. counties, including the following categories: 1–large central metro, 2–large fringe metro, 3–medium metro, 4–small metro, 5–micropolitan, and 6–non-core. Compared with RUCA, this classification scheme better reflects the geographic differences in access to transportation that could impact the effectiveness of primary care-based self-care interventions designed to help overcome transportation burdens associated with accessing primary care services for diabetes. However, this classification scheme categorizes MODEL practices located in areas such as Marshall and Tate counties in MS and Tipton in TN as large fringe metro sites that self-identify as rural sites (Table 1).
-
•
Option 3: Urban cluster/rural vs. urbanized area classification scheme
Fig. 3.
Designation of the geographic area served by the Management of Diabetes in Everyday Life (MODEL) Study using the NCHS Classification.
This customization of the RUCA ZIP code classification is based on the U.S. Census classification scheme and is illustrated in Fig. 4. This scheme contrasts urban cluster/rural areas vs. urbanized areas served by the MODEL Program. The conceptual definition of urban clusters and urbanized areas is based on population density [19]. This classification scheme also better reflects true geographic differences in access to transportation, however, this classification scheme overstates the urban character of the Jackson, TN/Madison County area and that this area's low geographic density and transportation characteristics have more in common with the other suburban areas than they do with the urban core of Memphis (Table 1).
Fig. 4.
Designation of the geographic area served by the Management of Diabetes in Everyday Life (MODEL) Study using the Census Classification.
Selection of suburban/rural vs. urban core classification scheme
Based on the comparison of the RUCA classification system with other urban/rural classification systems, we changed our urban/rural classification scheme and adopted option 1—a classification scheme based on the work of Schnake-Mahl and colleagues [5]. Given that a large proportion of poor Americans live in the suburbs, many of whom lack health insurance and regular access to care, and have similar transportation barriers as those living in rural areas, combining suburban with rural was the most appropriate approach for our underserved population. Thus, we changed our approach by categorizing center city as urban and other areas as suburban/rural for our analysis. Using this approach, 19.4% of MODEL participants were reclassified as suburban/rural (Table 3). Our new definition of rural is more closely linked to the true level geographic access to health services experienced by low-income people in suburban areas and is more consistent with the Goldsmith Modification definition of rural proposed by Goldsmith et al. [20]. Although suburban areas have grown in population and joined metro areas, our data shows (Table 1) that these areas still lack public transportation services that are available in metro areas. Furthermore, population density of suburban areas of Mid-South region is still too low to support more dense location of key health services.
We redefined traditional urban/rural classification approach for the purposes of this study on basis of functional healthcare seeking characteristics of the communities the MODEL program is seeking to serve. Since our study is designed to track and explain economic and social differences, we think that adopting the new classification scheme proposed by Schnake-Mahl and colleagues will highlight major differences in demographics and socioeconomic characteristics between urban and suburban in the Mid-South. According to this classification scheme, the MODEL practices located in Jackson, TN; Covington, TN; and Holly Springs, MS that self-identified as rural practices were classified as suburban/rural sites, whereas all other classification schemes classified either one or more of these practices as large fringe metro or urbanized sites. The classification method proposed by Schnake-Mahl and colleagues that we adopted is appropriate for studying disparities in underserved minority populations in Mid-South and may not be applicable to other regions of the country. Therefore, future studies should consider multiple urban rural classification schemes when classifying medically underserved populations.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors would like to acknowledge the contributions of Carrie Jo. Riordan, MPH and Patti Smith, MPH for their assistance.
References
- 1.Hart L.G., Larson E.H., Lishner D.M. Rural definitions for health policy and research. Am J. Public Health. 2005;95:1149–1155. doi: 10.2105/AJPH.2004.042432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hall S.A., Kaufman J.S., Ricketts T.C. Defining urban and rural areas in U.S. epidemiologic studies. J. Urban Health. 2006;83:162–175. doi: 10.1007/s11524-005-9016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruca Data. ZIP Code RUCA approximation. Available at https://depts.washington.edu/uwruca/ruca-approx.php. Accessed on February 23, 2021.
- 4.Rural-Urban Commuting Area Codes . U.S. Department of Agriculture; 2021. Economic Research Service.https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx Available at. Accessed on February 23. [Google Scholar]
- 5.Schnake-Mahl A.S., Sommers B.D. Health care in the suburbs: an analysis of suburban poverty and health care access. Health Aff. (Millwood) 2017;36:1777–1785. doi: 10.1377/hlthaff.2017.0545. [DOI] [PubMed] [Google Scholar]
- 6.Allard S.W. Russell Sage Foundation; New YorkNY: 2017. Places in Need: The Changing Geography of Poverty. [Google Scholar]
- 7.Kneebone E. Brookings Institution; WashingtonDC: 2014. The Growth and Spread of Concentrated Poverty, 2000 to 2008–2012. [Google Scholar]
- 8.Dam A.V. The real (surprisingly comforting) reason rural America is doomed to decline. Wash. Post. 2019;24 https://www.washingtonpost.com/business/2019/05/24/real-surprisingly-comforting-reason-rural-america-is-doomed-decline/ [Google Scholar]
- 9.Felland L.E., Lauer J.R., Cunningham P.J. Suburban poverty and the health care safety net. Res Brief. 2009;13:1–12. [PubMed] [Google Scholar]
- 10.McDougall G.S. Urban services and the suburbanization of blacks. Soc. Sci. Q. 1986;67:596. [Google Scholar]
- 11.Erickson R.A., Miller T.K. Race and resources in large American cities: an examination of intraurban and interregional variations. Urban Aff. Rev. 1978;13:401–420. [Google Scholar]
- 12.P* Farley JE. Segregation indices: what can they tell us about housing segregation in 1980? Urban Stud. 1984;21:331–336. [Google Scholar]
- 13.Bloomberg CityLab; 2019. The Changing Demographics of America's Suburbs.https://www.bloomberg.com/news/articles/2019-11-07/the-changing-demographics-of-america-s-suburbs Available at. Accessed on February 23, 2021. [Google Scholar]
- 14.McDonald J.F. Urban Studies Research; 2013. Urban Areas in the Transformation of the South: A Review of Modern History. [Google Scholar]
- 15.Tennessee Advisory Commission on Intergovernmental Relations; 2021. Just How Rural or Urban are Tennessee's 95 Counties? Finding a Measure for Policy Makers.https://www.tn.gov/content/dam/tn/tacir/documents/2016JustHowRuralOrUrban.pdf Available at. Accessed on February 23. [Google Scholar]
- 16.Onega T., Weiss J.E., Alford-Teaster J., Goodrich M., Eliassen M.S., Kim S.J. Concordance of rural-urban self-identity and zip code-derived rural-urban commuting area (RUCA) designation. J. Rural Health. 2020;36:274–280. doi: 10.1111/jrh.12364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ricketts T.C., Johnson-Webb K.D., Taylor P. Office of Rural Health Policy; 1998. Definitions of rural: A handbook For Health Policy Makers and Researchers.https://www.shepscenter.unc.edu/wp-content/uploads/2014/10/ruralit.pdf Available at. Accessed on February 23, 2021. [Google Scholar]
- 18.NCHS Urban-Rural Classification Scheme For Counties. Centers for Disease Control and Prevention. Available at https://www.cdc.gov/nchs/data_access/urban_rural.htm. Accessed on February 23, 2021.
- 19.Urban and Rural. United States Census Bureau. Available at https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural.html. Accessed on February 23, 2021.
- 20.Goldsmith H., Puskin D.S., Stiles D.J. 1993. Improving the Operational Definition of "Rural Areas" For Federal Programs.https://www.ruralhealthinfo.org/pdf/improving-the-operational-definition-of-rural-areas.pdf Available at. Accessed on February 23, 2021. [Google Scholar]