Abstract
In a developing country like India, both availability and affordability of medical care are obstacles, leading to delay in seeking timely treatment. To reduce the cost incurred to the patients for strabismus surgery, we used half of a 6-0 polyglactin suture for performing common muscle weakening and strengthening procedures: a fixed and hang back recessions with plication and resection. We cut the 45-cm-long double-armed 6-0 polyglactin sutures in two halves, and with a modified approach, used one-half in each of two patients planned for monocular two horizontal muscles surgeries: fixed recession-plication and hang back recession-resection. By devising an intuitive manner of threading a single armed 22.5 cm suture we successfully carried out horizontal extraocular muscle surgeries on each of two patients of exotropia. We believe in the long run, this will reduce the cost to individual patients and sponsoring groups, and suggest that strabismus surgeons consider adopting this option.
Keywords: Half-suture strabismus surgery, modified suturing, reducing cost
In several studies, the global prevalence of strabismus is reportedly between 0.3% and 4.7%.[1] The psycho-social issues and associated risk of amblyopia need timely intervention.[2,3,4] In developing countries like India, economic constraints and lack of awareness are considered the major barriers to the delay in eye care services.[5] The estimated worldwide cost-utility analyses of strabismus surgery measure $1632/QALY compared favorably to other commonly performed ophthalmic interventions viz. cataract surgery with $2,093/QALY.[6,7] In our public university-affiliated medical college, the cost incurred to the patient for strabismus surgery ranges from INR 2500 to 3500 ($33 to 47), which despite appearing little is still burdensome to many. In an attempt to further mitigate this, we explored performing strabismus surgery using half a 6-0 polyglactin double-armed suture by splitting it and modifying the steps of suture passage. Sketch diagrams delineate our technique [Figs. 1-4].
Figure 1.
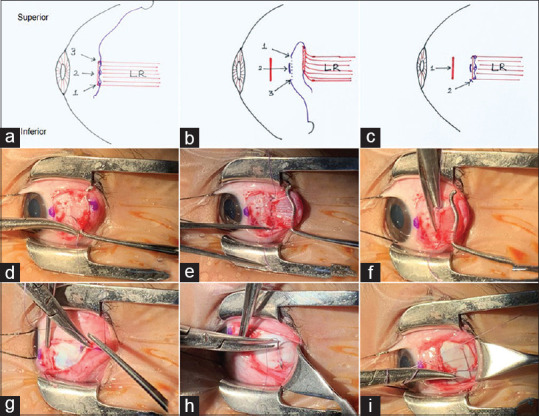
Sketch (a) illustrating steps for RCN showing anchoring bites to the muscles to be weakened (LR in this case) where arrows 1, 2, and 3 represent locking bite at the inferior edge, central belly, and superior edge, respectively, sketch (b) arrows 1 and 3 represent the intra-scleral course and arrow 2 represents the extra scleral course of the suture. Sketch (c) arrow 1 represents the remaining stump and arrow 2 represents locking knots affecting recession. Photographs (d-i) showing steps of half a suture recession
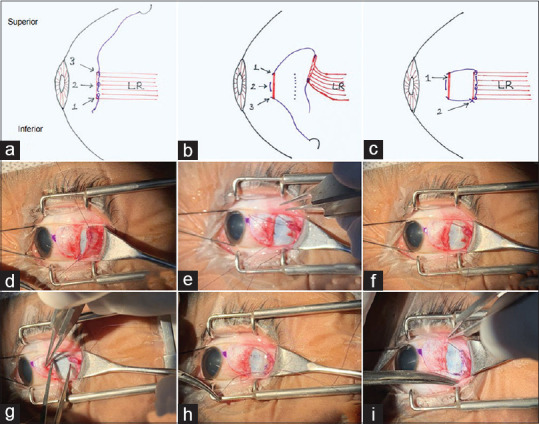
Figure 4.
Sketch (a) illustrating steps for resection showing anchoring bites to the muscles to be strengthened (MR in this case) at the desired point of resection where arrows 1, 2, and 3 represent locking bites at superior edge, central belly, and inferior edge, respectively; sketch (b) arrows 1 and 3 represent the intra-scleral course and arrow 2 represents the extra scleral course of suture. Sketch (c) arrow 1 represents final locking knots at muscle insertion after resection, arrow 2 represents the resected part of the redundant muscle. Photographs (d-i) showing steps of half a suture resection
Surgical Technique
After obtaining consent from the patient/parents, we performed elective horizontal strabismus surgery on two patients of exotropia (XT) using half of the double-armed, 6-0 polyglactin suture (Vicryl, Johnson & Johnson, 2670) which has a length of 45 cm. This left us with two single-armed suture fragments of 22.5 cm each, one to be used in each patient. The steps of weakening and strengthening procedures are described:
We performed recession (RCN) and plication surgery under GA on the left eye of a patient, age 3.5 years, with infantile alternate XT of 45 Prism Dioptre (PD). The 6-0 polyglactin suture was cut into two halves (each half = 22.5 cm) for each paired muscle procedure. We applied traction using 5-0 silk sutures, anchored at 12 and 6 0’clock. The lateral rectus (LR) muscle was first exposed and hooked.
Suturing steps for muscle RCN
In the usual manner, close to the insertion of LR, a small bite of full-thickness suture was first passed through the inferior edge of the tendon and secured by passing it through a twisted loop [Fig. 1d], ensuring that only about a centimeter of suture end was left free. This was followed by anchoring it to the mid tendon by forming a loop and ensnaring the second throw through it. Subsequently, at the superior edge of the LR the suture was anchored by a locking bite [Fig. 1e]. We then dis-inserted the LR from its insertion [Fig. 1f]. The point of recession was measured and marked, and the needle was first made to pass through the point on the sclera where the superior aspect of the tendon was desired to be positioned [Fig. 1g], and after 3-4 mm of intra-scleral passage it was brought out, re-inserted into the sclera, and after a second intra-scleral course exited at the desired point where the inferior aspect of the cut tendon was to be positioned [Fig. 1h]. Tying the free one-centimeter end of the suture, to the needle end of the suture allowed good proximation of the dis-inserted LR to the sclera [Fig. 1i]. After RCN ~ 11 cm of the suture was remaining.
Suturing steps for muscle plication
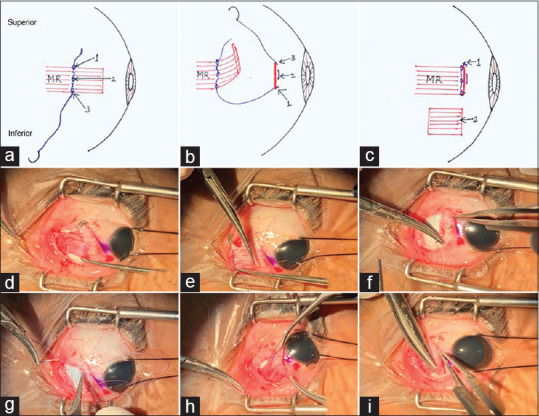
We anchored the remaining 6-0 polyglactin suture, first at the superior edge of MR using locking bites at the desired point of resection [Fig. 2d], leaving a centimeter of the free end, then a central anchorage was created by ensnaring the suture through a loop, and finally at the inferior edge through locking bites [Fig. 2e]. The muscle was drawn forward with locking forceps [Fig. 2f], while the suture needle was threaded through the sclera just anterior, and at the inferior end of the muscle stump, directing the suture towards the center of the stump [Fig. 2g]; thereafter the needle was re-inserted into the sclera and exited just anterior to the muscle stump, at the superior end [Fig. 2h]. Subsequently, tightening and tying of the suture ends affected the plication [Fig. 2i]: that still left two centimeters of suture to spare.
Figure 2.
Sketch (a) illustrating steps for plication showing anchoring bites to the muscles to be strengthened (MR in this case) at a desired point of resection where arrows 1,2 and 3 represent locking bites at superior edge, central belly, and inferior edge, respectively; sketch (b) arrows 1 and 3 represent the intra-scleral course and arrow 2 represents the extra scleral course of suture just anterior to the muscle insertion; sketch (c) arrow 1 represents final locking knots at muscle insertion effecting plication. Photographs (d-i) showing steps of half a suture plication
On another patient, age 17 years, planned for residual alternate XT of 30 PD, we performed hang back RCN and resection (RXN) surgery with the remaining half of 6-0 polyglactin suture. The steps are detailed as follows:
Suturing steps for hang back technique of muscle RCN
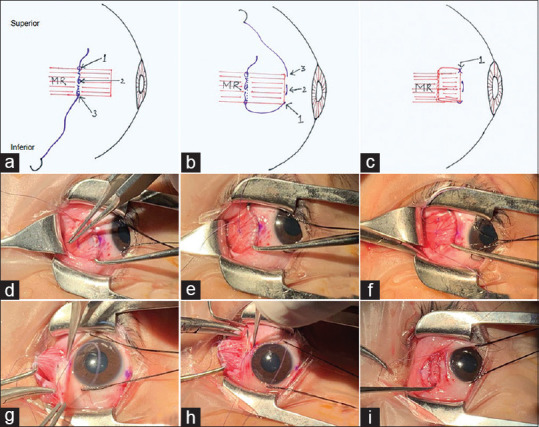
In an identical fashion as in the first case, we anchored the suture near the insertion of the LR. We then dis-inserted the LR from its insertion [Fig. 3d]. The suture needle was threaded through the sclera just anterior, and at the upper end of the muscle stump, directing the suture towards the center of the stump [Fig. 3e]; thereafter the needle was re-inserted into the sclera and exited just anterior to the muscle stump, at the inferior end [Fig. 3f]. The point of recession was measured and marked [Fig. 3g]. Subsequently, we pulled the suture needle towards the free end of the suture at the point of desired recession and the two ends were tied [Fig. 3h] resulting in the muscle to hang back to the desired recession position [Fig. 3i].
Figure 3.
Sketch (a) illustrating steps for hang back recession showing anchoring bites to the muscles to be weakened (LR in this case) where arrows 1, 2, and 3 represent locking bite at inferior edge, central belly and superior edge, respectively, sketch (b) arrows 1 and 3 represent the intra-scleral course and arrow 2 represents the extra scleral course of the suture. Sketch (c) arrow 1 represents the remaining stump and arrow 2 represents locking knots affecting hang back recession. Photographs (d-i) showing steps of half a suture hang back recession
Suturing steps for muscle RXN
In an identical manner to the plication just described, we anchored the remaining suture at the desired point of resection [Fig. 4d]. After dis-inserting the tendon [Fig. 4e], the suture needle was threaded through the sclera just anterior, and at the inferior end of the muscle stump, directing the suture towards the center of the stump [Fig. 4f; thereafter the needle was re-inserted into the sclera and exited just anterior to the muscle stump, at the superior end [Fig. 4g]. Subsequent tying of the suture ends, brought about the resection [Fig. 4h], and the redundant muscle-tendon portion was excised [Fig. 4i].
In each case, we used 8-0 polyglactin suture (Vicryl, Jhonson & Jhonson 2348) for conjunctival closure.
We took 6.36 minutes for RCN, 7.42 for plication, 6.49 for RXN and 6.58 for hang back. After 6 weeks follow up both the patients were orthotropic.
Discussion
There are many studies that have explored the idea of economizing ophthalmic surgeries, though often they deal with cataracts.[8] Similarly, efforts have been made to economies strabismus surgery without compromising the effectiveness and safety. In 2011, Nihalani and Hunter reviewed the idea of adjustable sutures that can reduce the cost for repeat surgery and also the risk associated with repeat general anesthesia. Similar to our technique, Zucca et al., in 2014, performed horizontal muscle surgeries using single-armed 6-0 polyglactin suture in 20 patients and reported a comparable result as with the use of double-armed sutures.[9] He found this technique easier and quicker. In a study from AIIMS, New Delhi, the average reported cost per strabismus patient was INR 3545, close to our estimate, and in which the sutures contributed INR 564.[10] While in ours, the cost of a 6-0 polyglactin suture was INR 760.
We have demonstrated that a single 6-0 polyglactin suture can be used in two patients, each of whom was undergoing two muscle surgeries. However, it does of course require patients to be scheduled in pairs. Also, we do have an opinion that the plication surgeries may be performed more comfortably by using the usual double-armed sutures than our half a suture technique.
Conclusion
We have successfully demonstrated that with a little ingenuity the four common extra-ocular muscle surgeries employed in strabismus viz. RCN-RXN, hang back RCN and plication can be performed using half a 6-0 polyglactin suture in one patient. This can substantially reduce costs both to patients and sponsoring institutions. We encourage strabismus surgeons to seriously consider this option.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Coats DK, Stager DR, Beauchamp GR, Stager DR, Mazow ML, Paysse EA, et al. Reasons for delay of surgical intervention in adult strabismus. Arch Ophthalmol. 2005;123:497–9. doi: 10.1001/archopht.123.4.497. [DOI] [PubMed] [Google Scholar]
- 2.Jackson S, Harrad RA, Morris M, Rumsey N. The psychosocial benefits of corrective surgery for adults with strabismus. Br J Ophthalmol. 2006;90:883–8. doi: 10.1136/bjo.2005.089516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kothari M, Balankhe S, Gawade R, Toshnival S. Comparison of psychosocial and emotional consequences of childhood strabismus on the families from rural and urban India. Indian J Ophthalmol. 2009;57:285–8. doi: 10.4103/0301-4738.53053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hatt SR, Leske DA, Holmes JM. Responsiveness of health-related quality-of-life questionnaires in adults undergoing strabismus surgery. Ophthalmology. 2010;117:2322–8. doi: 10.1016/j.ophtha.2010.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kovai V, Krishnaiah S, Shamanna BR, Thomas R, Rao GN. Barriers to accessing eye care services among visually impaired populations in rural Andhra Pradesh, South India. Indian J Ophthalmol. 2007;55:365–71. doi: 10.4103/0301-4738.33823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beauchamp CL, Beauchamp GR, Stager DR, Brown MM, Sr, Brown GC, Felius J. The cost utility of strabismus surgery in adults. J AAPOS. 2006;10:394–9. doi: 10.1016/j.jaapos.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 7.Brown GC, Brown MM, Sharma S, Brown H, Smithen L, Leeser DB, et al. Value-based medicine and ophthalmology: An appraisal of cost-utility analyses. Trans Am Ophthalmol Soc. 2004;102:177–88. [PMC free article] [PubMed] [Google Scholar]
- 8.Khan A, Amitava AK, Rizvi SAR, Siddiqui Z, Kumari N, Grover S. Cost-effectiveness analysis should continually assess competing health care options especially in high volume environments like cataract surgery. Indian J Ophthalmol. 2015;63:496–500. doi: 10.4103/0301-4738.162600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zucca I, Cuccu A, Piludu SI, Galantuomo MS, Borman A, Fossarello M. Innovative single-armed suture technique for Strabismus surgery. Invest Ophthalmol Vis Sci. 2014;55:2595. [Google Scholar]
- 10.Singh S, Sinha RA. Cost analysis study of squint surgery in a tertiary care ophthalmic hospital for development of users charges. DJO. 2013;23:299–303. [Google Scholar]


