Abstract
Purpose:
To assess the repeatability of ocular measurements, particularly astigmatism, taken using the latest version of an swept-source optical coherence tomography (SS-OCT) device, IOLMaster 700.
Methods:
This prospective observational study done in a private eye care centre. Study included 213 eyes of 152 patients diagnosed with cataract. Axial length (AL), Anterior corneal astigmatism (ΔK), Total corneal astigmatism (ΔTK), Aqueous depth (AD), Lens thickness (LT), Iris barycentre distance (IBD) and White to white distance (WTW) were analysed; three measurements were taken for each patient in the same sitting by the same examiner in an undilated state using the SS-OCT device. Repeatability was analysed using intraclass coefficient (ICC) and coefficient of variation (CV) measures, and astigmatism values were transformed into vector components (J0/J45) and categorised based on magnitude.
Results:
Astigmatism vector components (J0/J45) showed poor repeatability (ICC < 0.5 and CV > 0), while iris coordinates (IBD) and astigmatism magnitude had good correlation (ICC > 0.9) but more variations between the readings which was least for magnitude ≥ 1.5D; however, rest of the parameters demonstrated excellent repeatability (ICC > 0.9 with P value < 0.05).
Conclusion:
IOLMaster 700 demonstrated good reliability for the parameters measured, although, for astigmatism and iris barycentre distance, more number of readings and cross reference with other devices may be required to get clinically accurate results.
Keywords: Astigmatism, biometry, IOLMaster 700, repeatability, SS-OCT biometer
In the present age, accurate ocular biometry is essential for precise visual outcomes after refractive cataract surgery. In a span of a few decades, ocular biometry has advanced from the use of contact ultrasound probes to an era of noncontact imaging modalities.
The introduction of the partial coherence interferometry (PCI) based IOLMaster (Carl Zeiss Meditec AG) was a breakthrough in ocular biometry. In the initial PCI based devices, a low-coherence light source was used and optical A-scans were acquired using the reflections detected by a scanning mirror.[1] Later, the IOLMaster 500 (IOLM500) was launched which utilizes 780 nm laser diode infrared light to measure the axial length (AL), records keratometry (K) at 2.4 mm optical zone using 6 reference points on the corneal surface and uses lateral slit illumination technique to measure anterior chamber depth (ACD).[2] Despite this, AL measurements in few cases like subcapsular lens opacity, dense cataracts, poor fixation could not be achieved and an examination failure rate of as high as 35.47% has been reported with this device.[3]
To overcome some of these fallacies, and setting a new standard in ocular biometry, recently the IOLMaster®700 optical biometer (Carl Zeiss Meditec, Jena, Germany) was introduced. This utilizes new swept-source technology (SS-OCT) with a tunable laser of 1,055 nm as a light source providing optical B-scans, which enables us to measure full-length of the eye from the cornea to the retina on a longitudinal cut as well as cross-sectional visualization of the eye. It allows a 44 mm scan depth with 22 mm resolution in corneal tissue.[1,4] It also provides an improved signal-to-noise ratio as the narrow bandwidth light source reflections are projected to the eye one at a time.[1] The enhanced visualization with this device facilitates the detection of unusual eye geometries, such as a tilt or decentration of the crystalline lens, allows rapid data acquisition and measurement of the axial length along six different axes.[5,6] The deeper scans and good quality images give an advantage in eyes with posterior subcapsular cataracts and dense cataracts.[4] Furthermore, it provides a unique fixation check with the foveal image, so it reduces the risk of refractive surprises due to incorrect measurements caused by undetected poor fixation.[5,6]
The IOLMaster 700 is also known for its superior keratometry measurements as it utilizes telecentric keratometry, which combines a 950 nm light source and a unique optical configuration to ensure spot size remains constant irrespective of device-to-eye distance.[5] This technology makes patient movements less disruptive to image acquisition. Moreover, with the latest version, it is now possible to measure the posterior corneal curvature. Total keratometry (TK) combines telecentric keratometry and SS-OCT technology (assessment of anterior and posterior corneal curvatures respectively),[7] thereby giving us the astigmatism values which aids in the planning of Toric IOLs.
Nevertheless, the benefits of having numerous valuable parameters with IOL Master 700 can easily be lost if the measurements are not done accurately or the readings taken are inconsistent. In this study, we aimed to assess the repeatability of this device based on biometric measurements of patients having cataract, specifically astigmatism and iris barycentre values.
Methods
This prospective observational study included 213 eyes of 152 patients who underwent evaluation for cataract surgery at our centre with an age range of 40-87 years. Data was collected between October 2019 to February 2020. The study complied with the tenets of the Declaration of Helsinki and Good Clinical Practices. Informed consent was obtained from all patients after explaining the nature of the study.
Exclusion criteria: Evidence of corneal or retinal pathology; prior refractive surgery; abnormal structure such as phacodonesis, white cataract, or corneal scar; h/o use of soft contact lenses within 2 weeks or rigid contact lenses within 4 weeks; dry eye syndrome (with subjective dry eye symptoms, tear film break-up time shorter than 5 seconds) that would negatively impact the accuracy of biometry imaging; or unrecordable axial length.
Device specifications
The IOLMaster 700 is a SS-OCT device with telecentric keratometry. The wavelength for OCT varies from 1035 nm to 1080 nm and that of keratometer is 950 nm. The keratometer comprises of 18 points, arranged on three rings radially from the corneal centre. The optical axis of the SS-OCT and keratometer is identical, this ensures that the B-scan passes through the measuring points. It measures axial length (AL), anterior chamber depth (ACD), central cornea thickness (CCT), lens thickness (LT) and posterior corneal curvature (PK) using swept-source OCT technology; anterior corneal curvature (K) using reflected light spots on the surface of the cornea; and pupil diameter (PD), visual axis (line of sight), iris barycentre distance (IBD) and white-to-white (WTW) measurement based on a scleral and iris image. The measurement range for the AL is reported to be 14-38 mm, for ACD 0.7-8.0 mm, for corneal radii 5-11 mm, for LT 1-10 mm (phakic eye) and 0.13-2.5 mm (pseudophakic eye), for WTW 8-16 mm, and for CCT 200-1200 mm.
Patient examination and biometry
All patients underwent a complete ophthalmic examination by an ophthalmologist. After basic refraction, vision assessment and slit-lamp examination, ocular biometry with IOL Master 700 was done in an un-dilated state. After checking the calibration of the device, patients were asked to place their chin on the chin rest, forehead against the forehead support, and to look at the fixation point (blinking red light) of the device.
One measurement consists of 3 steps - 1. Coarse alignment: a green cross is centred on the pupillary axis along with 6 LED lights display.
2. Fine alignment: green cross centred on central corneal reflex along with 18 LEDs display for keratometry measurement, and OCT image is captured.
3. Fixation check scan: green cross centred on central corneal reflex with 6 LEDs display - to check correct fixation during measurement.
Patients were asked to blink and keep eyes wide open before each scan. A red, yellow and green light is provided with the live image, to check the alignment. Measurements can be done in Auto/Manual mode. We selected manual mode for our scans. For each patient, measurements were taken successively three times in a single session by the same examiner with the room lights switched off. In between each measurement, the participants were asked to move their heads away from the chin rest, and head position & alignment was checked each time to avoid head tilt errors. The measurements were considered acceptable if they satisfied the quality criteria for the device as defined by the manufacturer (green ticks, yellow exclamation marks, and red cross).
Data collection
In the present study, the following parameters were measured for each eye with the optical biometer: axial length (AL), aqueous depth (AD), lens thickness (LT), white-to-white distance (WTW), D keratometry (D K)/anterior corneal astigmatism, D total keratometry (Δ TK)/total corneal astigmatism, and iris barycentre distance (Ix, Iy) {Ix: x co-ordinate of iris centre relative to corneal apex, Iy: y co-ordinate of iris centre relative to corneal apex}.
Statistical analysis
Data were analysed using the statistical package SPSS (IBM SPSS Statistics for Windows, Version 20.0. IBM Corp). Descriptive was done for the continuous variables.
For vector analysis, we converted astigmatism from the cylinder notation to power vector notation by applying a Fourier transformation using the following equations-

where C is negative cylindrical power and a is cylindrical axis. J0 refers to cylinder power set at orthogonally 90° and 180° meridians. Positive values of J0 indicate WTR astigmatism, and negative values of J0 indicate ATR astigmatism. J45 refers to a cross-cylinder set at 45° and 135°, representing oblique astigmatism. The participants were classified into three groups based upon the magnitude of astigmatism (ΔK): group 1: < 0.75 DC, group 2: 0.75- 1.49 DC and group 3: ≥ 1.50 DC.
The readings at three occasions were compared using Repeated measures (RM) ANOVA and demonstrated using a box plot. To establish repeatability, Intraclass correlation (ICC) and Coefficient of variation (CV) were calculated between the three readings for each parameter.
Results
Two hundred and thirteen eyes of 152 participants with a mean age of 62.5 ± 9.8 years were included in the study. Out of the 152 participants, 70 were females and 82 were males. Table 1 summarizes descriptive statistics calculated from the average values of all three readings for all the parameters. [Table 1].
Table 1.
Average values for all the parameters
| Parameters | Mean | Std. Deviation | Minimum | Maximum |
|---|---|---|---|---|
| Axial length (mm) | 23.53 | 1.37 | 19.62 | 31.50 |
| Anterior corneal astigmatism (D)(ΔK) | 0.87 | 0.66 | 0.00 | 4.50 |
| Anterior corneal astigmatism vector J0 | -0.003 | 0.377 | -1.26 | 2.10 |
| Anterior corneal astigmatism vector J45 | 0.037 | 0.393 | -1.30 | 1.98 |
| Total corneal astigmatism (D)(ΔTK) | 0.950 | 0.693 | 0.00 | 4.64 |
| Total corneal astigmatism vector J0 | 0.027 | 0.390 | -1.21 | 2.15 |
| Total corneal astigmatism vector J45 | 0.000 | 0.440 | -1.05 | 2.05 |
| Iris Coordinate (IBD) Ix | 0.357 | 0.267 | -0.80 | 0.90 |
| Iris Coordinate (IBD) Iy | 0.130 | 0.187 | -0.40 | 1.00 |
| Lens thickness (mm) | 4.413 | 0.420 | 3.00 | 5.77 |
| Aqueous depth (mm) | 2.607 | 0.360 | 1.75 | 4.84 |
| White to white (mm) | 11.95 | 0.42 | 10.80 | 12.90 |
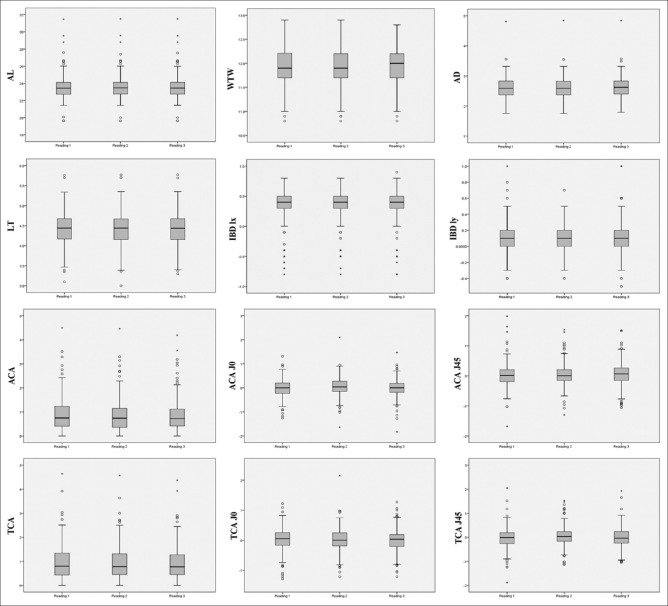
There was no significant difference (p > 0.05) noted among the three readings for any of the parameters calculated by repeated measures ANOVA. Fig. 1 depicts the box plot for three readings for each variable. [Fig. 1].
Figure 1.
Depicts the box plot for three readings for each variable. {The horizontal line within the box indicates the median, boundaries of the box indicate the 25th and 75th percentile. The mild outliers are marked with open circles (o) and extreme outliers with asterisks (*). AL: Axial Length; WTW: White-toWhite; AD: Aqueous Depth; LT: Lens Thickness; IBD Ix (Iris coordinate Ix); IBD Iy (Iris coordinate Iy);ACA (Anterior corneal astigmatism); ACA J0 & J45 (J0 & J45 vectors of anterior corneal astigmatism) ; TCA (Total corneal astigmatism); TCA J0 &J45 (J0 & J45 vectors of total corneal astigmatism).}
Repeatability and agreement of different parameters
Intraclass correlation (ICC)
Table 2 summarizes the values of ICC for all the parameters. Excellent correlation (ICC > 0.9) was noted for axial length, ΔK, Δ TK, IBD-Ix, lens thickness, aqueous depth and white to white; whereas IBD- Iy showed good correlation (ICC - 0.75-0.9) and all these were statistically significant (P < 0.001). However, poor ICC was noted for the vector components (J0, J45) of ΔK and ΔTK amongst the three readings which is discussed below based on astigmatism magnitude classification. [Table 2].
Table 2.
Value of Intraclass correlation for the parameters
| Parameters | ICC (95% CI) | P |
|---|---|---|
| Axial length | 1.000 (1.000-1.000) | <0.001 |
| Anterior corneal astigmatism (ΔK) | 0.977 (0.971-0.982) | <0.001 |
| Anterior corneal astigmatism ΔK- J0 | 0.222 (0.022-0.387) | 0.016 |
| Anterior corneal astigmatism ΔK- J45 | -0.183 (-0.488-0.068) | 0.917 |
| Total corneal astigmatism (ΔTK) | 0.947 (0.967-0.979) | <0.001 |
| Total corneal astigmatism ΔTK- J0 | 0.126 (-0.099-0.311) | 0.125 |
| Total corneal astigmatism ΔTK- J45 | 0.102 (-0.13-0.292) | 0.179 |
| Iris Coordinate (IBD) Ix | 0.979 (0.973-0.983) | <0.001 |
| Iris Coordinate (IBD) Iy | 0.841 (0.800-0.875) | <0.001 |
| Lens thickness | 0.999 (0.999-0.999) | <0.001 |
| Aqueous depth | 0.987 (0.983-0.990) | <0.001 |
| White to white | 0.964 (0.955-0.971) | <0.001 |
*ICC: Intraclass correlation
Coefficient of variation (CV)
The values of coefficient of variation is summarized in Table 3. Good CV (closer to zero) was noted for AL, LT, AD and WTW with AL showing least variation amongst the readings (CV = 0.054). However, ΔK and ΔTK; and their vector components (J0/J45) showed higher CV and to assess this in detail we divided the astigmatism analysis into 3 groups as discussed below. The CV was high for the Iris coordinates (Ix and Iy) also. [Table 3].
Table 3.
Value of coefficient of variation for the parameters
| Parameters | CV (%) | Sw |
|---|---|---|
| Axial length | 0.054 | 0.082 |
| Anterior corneal astigmatism (ΔK) | 22.803 | 25.475 |
| Anterior corneal astigmatism ΔK- J0 | 516.828 | 8894.28 |
| Anterior corneal astigmatism ΔK- J45 | -5411.61 | 81545.6 |
| Total corneal astigmatism (ΔTK) | 23.478 | 24.938 |
| Total corneal astigmatism ΔTK- J0 | -384.053 | 8581.25 |
| Total corneal astigmatism ΔTK- J45 | -218.611 | 1433.66 |
| Lens thickness | 0.210 | 0.403 |
| Aqueous depth | 1.193 | 3.003 |
| White to white | 0.711 | 0.979 |
| (IBD) Ix | 11.1 | 24.82 |
| (IBD) Iy | 15.13 | 122.66 |
*CV: coefficient of variation, Sw: Within Subject Variation
Reliability based on classification of astigmatism
We categorised the eyes based on the amount of astigmatism. Majority of eyes we analysed had value of <0.75D for both anterior and total corneal astigmatism (53.5 and 48.4% respectively); while 33.8% and 34.3% eyes had value between 0.75-1.49D, and 12.7% and 17.4% eyes had value ≥1.5D for anterior and total corneal astigmatism respectively.
Table 4 depicts ICC values of magnitude of anterior and total corneal astigmatism based on the classification. Correlation between values was higher for high astigmatism (≥1.5D) for both ΔK and ΔTK (0.988 and 0.962 respectively). Similarly, although the vector components J0 and J45 showed poor ICC (<0.5) but the values for astigmatism ≥1.5D had better correlation compared to lower astigmatism values. [Table 4].
Table 4.
Intraclass correlation values of anterior and total corneal astigmatism and vector components in the subgroups
| Parameters | ICC | 95% CI | P | ||
|---|---|---|---|---|---|
|
| |||||
| LL | UL | ||||
| Anterior corneal astigmatism (ΔK) (D) | < 0.75 | 0.819 | 0.749 | 0.872 | <0.001 |
| 0.75-1.49 | 0.805 | 0.707 | 0.874 | <0.001 | |
| ≥1.50 | 0.988 | 0.980 | 0.993 | <0.001 | |
| Total corneal astigmatism (ΔTK) (D) | < 0.75 | 0.686 | 0.564 | 0.778 | <0.001 |
| 0.75-1.49 | 0.691 | 0.544 | 0.796 | <0.001 | |
| ≥1.50 | 0.962 | 0.935 | 0.979 | <0.001 | |
| Anterior corneal astigmatism ΔK- J0 | < 0.75 | 0.002 | -0.369 | 0.279 | 0.499 |
| 0.75-1.49 | 0.157 | -0.247 | 0.446 | 0.195 | |
| ≥1.50 | 0.26 | -0.402 | 0.639 | 0.176 | |
| Anterior corneal astigmatism ΔK- J45 | < 0.75 | 0.08 | -0.257 | 0.338 | 0.298 |
| 0.75-1.49 | -0.044 | -0.544 | 0.314 | 0.573 | |
| ≥1.50 | -0.504 | -1.850 | 0.265 | 0.870 | |
| Total corneal astigmatism ΔTK- J0 | < 0.75 | -0.519 | -1.109 | -0.074 | 0.991 |
| 0.75-1.49 | 0.091 | -0.342 | 0.400 | 0.312 | |
| ≥1.50 | 0.194 | -0.391 | 0.558 | 0.217 | |
| Total corneal astigmatism ΔTK- J45 | < 0.75 | 0.139 | -0.196 | 0.391 | 0.185 |
| 0.75-1.49 | -0.216 | -0.794 | 0.198 | 0.821 | |
| ≥1.50 | 0.266 | -0.266 | 0.598 | 0.132 | |
Coefficient of variation was high for both ΔK and ΔTK, although on analysing the CV in subgroups based on magnitude values; for both anterior and total corneal astigmatism, least variation was seen for astigmatism magnitude ≥1.5D (7.44 and 8.08) compared to values of 0.75-1.49 D (14.66 and 16.01) and astigmatism < 0.75D showed very high variation in between the readings (31.66 and 34.31) [Table 3a].
Table 3a.
Value of coefficient of variation for anterior and total corneal astigmatism in the subgroups
| Parameters | CV (%) | SW | |
|---|---|---|---|
| Anterior corneal astigmatism ΔK | <0.75 | 31.66 | 30.82 |
| 0.75-1.50 | 14.66 | 11.16 | |
| ≥1.50 | 7.44 | 7.96 | |
| Total corneal astigmatism ΔTK | <0.75 | 34.31 | 29.88 |
| 0.75-1.50 | 16.01 | 13.76 | |
| ≥1.50 | 8.08 | 7.86 | |
Correlation between parameters
Axial length showed positive significant correlation with anterior and total corneal astigmatism (r = 0.187 and 0.143 respectively), white to white (r = 0.177), and aqueous depth (r = 0.272). Lens thickness showed positive significant correlation with anterior and total corneal astigmatism (r = 0.226 and 0.240 respectively), and aqueous depth (r = 0.571). White to white also showed positive correlation with aqueous depth (r = 0.255). Anterior and total corneal astigmatism were also significantly positively correlated (r = 0.959).
Age showed significant positive correlation with anterior and total corneal astigmatism, and lens thickness; and negative correlation with aqueous depth.
Discussion
With the advent of biometers giving better keratometry and visual axis centration values, precise measurements are crucial for getting satisfactory refractive cataract surgery outcomes. In this study, we aimed to assess the repeatability of our SS-OCT biometer IOLMaster 700, in terms of AL, ΔK, ΔTK, Iris barycentre distance (Ix & Iy), WTW, AD and LT, all of these play a key role in IOL calculations for toric and other premium IOLs. To the best of our knowledge, there have been few studies on the repeatability of this device but none has reported repeatability of corneal astigmatism based on magnitude, total astigmatism (ΔTK) and Iris barycentre distance (Ix & Iy).
In our study, there was no statistically significant difference noted among the three readings of any of the parameters. There was an excellent correlation (ICC > 0.9) for all the parameters and this was statistically significant. Axial length showed the highest correlation values (ICC = 1) and the least coefficient of variation i.e., best repeatability amongst all the parameters.
Precise astigmatism measurement becomes vital in series and axis determination of Toric IOLs. For anterior and total corneal astigmatism analysis, we transformed cylindrical values in J0/J45 vector components and divided the eyes into 3 groups based on astigmatism magnitude values. For both anterior and total corneal astigmatism, ICC and CV values were better for cylindrical magnitude ≥1.5D as compared to the lower magnitude groups, which signifies excellent repeatability for higher astigmatism values and more variations in lower magnitude values. The repeatability measures were poor for the J0/J45 vector components of astigmatism, though the P value was not statistically significant. There are very few studies for repeatability of astigmatism; Kiraly et al. in their study using IOLMaster 700, analysed 55 eyes for CCT, mean K and, vector components J0/J45 and, demonstrated that intra operator repeatability of J0, J45 and, K mean was high- 0.989, 0.974 and 0.999 respectively.[8] Some studies using other devices have demonstrated similar results. A recent study done by Schiano et al. on 96 eyes using ANTERION device (AS-OCT biometer) concluded that astigmatism measurements (both magnitude and axis of keratometric and total corneal power astigmatism) showed slightly worse repeatability compared to the other parameters and, the repeatability significantly improved when eyes with keratometric astigmatism more than 1.0 D were analysed.[9] In another study using SS-OCT biometer (Argos) done by Nemeth et al., they found an excellent Intraclass correlation coefficient (ICC) for all measured parameters except for the dioptre values and the vector values of astigmatism (J0/J45).[10] It is also stated that when the mean value of a parameter is near zero, the CV is sensitive to small changes in the mean, limiting its usefulness.[11,12] Therefore we did not consider the CV for both vector J0 and J45, whose mean values were close to zero, as the results were not reliable. So for astigmatism, the consistency between readings was more for higher cylinder (≥1.5D), both for magnitude as well as axis. And it can be suggested that for toric IOL calculations, specially for low to moderate astigmatism, more number of readings and axis reference from other devices, needs to be taken to increase the accuracy in results.
Iris barycentre distance becomes crucial for centration of IOLs on visual axis, especially when using markerless devices; and IOL centration is of supreme importance for getting good outcomes with premium IOLs. As it is known that decentration relative to visual axis can result in decrease postoperative visual function of diffractive multifocal IOLs and residual astigmatism in Toric IOLs.[13] Many studies have demonstrated the importance of angle alpha in IOL centration. Mahr et al. in their study, have shown that angle alpha is a predominantly horizontal phenomenon i.e., the horizontal coordinate is more important.[14] We found an excellent repeatability with Ix (ICC-0.979) and good repeatability with Iy (ICC-0.841), although CV was poor. As stated earlier, the mean of both these values was closer to zero, so their CV was not very reliable. Hence for Ix and Iy, the readings correlated well but had a variation between them, however, Ix correlated better than Iy. WTW, AD, and LT showed a high ICC and less CV suggesting good repeatability between the readings.
For other parameters also, our results were consistent with many other studies. Blasco et al. studied repeatability of the parameters axial length (AL), anterior chamber depth (ACD), central corneal thickness (CCT), lens thickness (LT), white-to-white (WTW), and K1 and K2 keratometric readings in 30 phakic eyes using IOLMaster 700, and found a high repeatability performance with AL showing lowest coefficient of variation, and the LT had the highest one.[15] A study by Ozgun et al. in 93 healthy eyes showed the ICC of AL was best (ICC = 1.000), followed by ACD (ICC = 0.999), LT (ICC = 0.994), K (ICC = 0.988) and WTW (ICC = 0.725).[16] Srivannaboon et al. in their study including 100 cataract eyes, found that using IOLMaster 700, all parameters (CCT, ACD, LT, and AL) measured by the SS-OCT technology, showed very high ICCs (0.99 to 1.00) while the keratometry and WTW measurements, which were determined using an LED light source, showed slightly lower ICCs (0.93 to 0.99).[1]
We found a significant positive correlation of axial length with- anterior and total astigmatism, WTW, and aqueous depth; as it is known that as eyes get larger, AC depth and corneal diameter increases. The study by Ozgun et al. also demonstrated a positive correlation of AL with ACD and WTW.[16] We also found that age had a positive correlation with astigmatism values & lens thickness and negative correlation with aqueous depth. Kim et al. in their study showed that age had an inverse correlation with AL and ACD, and had a positive correlation with Keratometry.[17]
Most of the parameters in our study demonstrated excellent repeatability, although, for astigmatism and iris barycentre distance, the repeatability was less. The reason for these findings could be- 1. Corneal measurements are known to be affected by tear film instabilities. Though we took the measurements on an untouched cornea, but this component could be a contributing factor for the variation in the astigmatism values. Moreover, even after perfect alignment the head tilt errors cannot be eliminated completely, which can result in variation in the cylindrical axis. 2. As we know that in this device, different parameters are measured using different technologies, this might be the reason for the difference in the repeatability of these parameters, as variables measured using OCT technology showed better repeatability. 3. Moreover, the iris barycentre distance values are derived from iris image which is captured in the first scan, so there could be patient fixation error which could have caused such variation in these values.
The detailed analysis of astigmatism and iris coordinate values in our study provided a good insight on the importance of repeating biometry for precise IOL calculations. One limitation of our study was that we did not evaluate the post-operative results, as it can validate whether the variation in astigmatism values can result in a clinically significant alteration in results.
Conclusion
In summary, this SS-OCT device provides good reliability for all the parameters measured. Although for astigmatism and IBD values, in view of higher variation between the readings, it is advised to take multiple readings and cross-check with other devices to increase the accuracy of desired postoperative outcomes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Srivannaboon S, Chirapapaisan C, Chonpimai P, Loket S. Clinical comparison of a new swept-source optical coherence tomography-based optical biometer and a time-domain optical coherence tomography-based optical biometer. J Cataract Refract Surg. 2015;41:2224–32. doi: 10.1016/j.jcrs.2015.03.019. [DOI] [PubMed] [Google Scholar]
- 2.Bhatt AB, Schefler AC, Feuer WJ, Yoo SH, Murray TG. Comparison of predictions made by the intraocular lens master and ultrasound biometry. Arch Ophthalmol. 2008;126:929–33. doi: 10.1001/archopht.126.7.929. [DOI] [PubMed] [Google Scholar]
- 3.McAlinden C, Wang Q, Pesudovs K, Yang X, Bao F, Yu A, et al. Axial length measurement failure rates with the IOLMaster and Lenstar LS 900 in eyes with cataract. PLoS One. 2015;10:e0128929. doi: 10.1371/journal.pone.0128929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Passi SF, Thompson AC, Gupta PK. Comparison of agreement and efficiency of a swept source-optical coherence tomography device and an optical low-coherence reflectometry device for biometry measurements during cataract evaluation. Clin Ophthalmol. 2018;12:2245–51. doi: 10.2147/OPTH.S182898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurian M, Negalur N, Das S, Puttaiah NK, Haria D, J TS, et al. Biometry with a new swept-source optical coherence tomography biometer:Repeatability and agreement with an optical low-coherence reflectometry device. J Cataract Refract Surg. 2016;42:577–81. doi: 10.1016/j.jcrs.2016.01.038. [DOI] [PubMed] [Google Scholar]
- 6.Drexler W, Liu M, Kumar A, Kamali T, Unterhuber A, Leitgeb RA. Optical coherence tomography today:Speed, contrast, and multimodality. J Biomed Opt. 2014;19:071412. doi: 10.1117/1.JBO.19.7.071412. [DOI] [PubMed] [Google Scholar]
- 7.Wang L, Spektor T, de Souza RG, Koch DD. Evaluation of total keratometry and its accuracy for intraocular lens power calculation in eyes after corneal refractive surgery. J Cataract Refract Surg. 2019;45:1416–21. doi: 10.1016/j.jcrs.2019.05.020. [DOI] [PubMed] [Google Scholar]
- 8.Kiraly L, Stange J, Kunert KS, Sel S. Repeatability and agreement of central corneal thickness and keratometry measurements between four different devices. J Ophthalmol. 2017;2017:6181405. doi: 10.1155/2017/6181405. doi:10.1155/2017/6181405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schiano-Lomoriello D, Hoffer KJ, Abicca I, Savini G. Repeatability of automated measurements by a new anterior segment optical coherence tomographer and biometer and agreement with standard devices. Sci Rep. 2021;11:983. doi: 10.1038/s41598-020-79674-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nemeth G, Modis L., Jr Ocular measurements of a swept-source biometer:Repeatability data and comparison with an optical low-coherence interferometry biometer. J Cataract Refract Surg. 2019;45:789–97. doi: 10.1016/j.jcrs.2018.12.018. [DOI] [PubMed] [Google Scholar]
- 11.Wang L, Shirayama M, Koch DD. Repeatability of corneal power and wavefront aberration measurements with a dual-Scheimpflug Placido corneal topographer. J Cataract Refract Surg. 2010;36:425–30. doi: 10.1016/j.jcrs.2009.09.034. [DOI] [PubMed] [Google Scholar]
- 12.Chen D, Lam AK. Reliability and repeatability of the Pentacam on corneal curvatures. Clin Exp Optom. 2009;92:110–8. doi: 10.1111/j.1444-0938.2008.00336.x. [DOI] [PubMed] [Google Scholar]
- 13.Piracha A. Using angle alpha in premium IOL screening. Cataract and refractive surgery today. 2016. [Last accessed on 2020 Jun 07]. Available from: https://crstoday.com/articles/2016-mar/using-angle-alpha-in-premium-iol-screening/
- 14.Mahr MA, Simpson MJ, Erie JC. Angle alpha orientation and magnitude distribution in a cataract surgery population. J Cataract Refract Surg. 2020;46:372–7. doi: 10.1097/j.jcrs.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 15.Ferrer-Blasco T, Domínguez-Vicent A, Esteve-Taboada JJ, Aloy MA, Adsuara JE, Montés-Micó R. Evaluation of the repeatability of a swept-source ocular biometer for measuring ocular biometric parameters. Graefes Arch Clin Exp Ophthalmol. 2017;255:343–9. doi: 10.1007/s00417-016-3555-z. [DOI] [PubMed] [Google Scholar]
- 16.Totuk OM, Aykan U. Repeatability of the new swept source optical biometer IOLMaster®700 measurements. EC Ophthalmol? 2017;7(3):78–85. [Google Scholar]
- 17.Kim JH, Kim M, Lee SJ, Han SB, Kong YT, Yang HK, et al. Age-related differences in ocular biometry in adult Korean population. BMC Ophthalmol. 2016;16:146. doi: 10.1186/s12886-016-0328-8. [DOI] [PMC free article] [PubMed] [Google Scholar]