Abstract
Purpose:
Anophthalmic sockets cause disfigurement that may result in emotional and social distress. The choice of procedure and implant is based upon the surgeon’s experience. There remains no standardization of cosmetic result. We sought to identify quantifiable anatomical features and functional properties related to a successful cosmetic result in patients with ocular prosthesis and to determine correlations between self-reported and third-party assessment of cosmetic success.
Methods:
This was a prospective observational study, which included 107 adult patients (50.1% female; age 53.08 ± 18.64 years, range 18–89) with acquired anophthalmia following prosthesis fitting. Patients completed a self-assessment questionnaire on self-perception of body image and ocular properties. Three independent examiners assessed cosmetic score. Assessed variables included prosthesis movement, eyelid symmetry, prosthesis stability, and socket fullness.
Results:
The general cosmetic result was 8.1 ± 2.19 (on a predetermined scale of 1–10) as perceived by the patients and 7.2 ± 0.19 by the examiners. Interexaminer correlation was high for all variables (P < 0.05). A good cosmetic result was correlated with prosthesis movement (P = 0.02), eyelid symmetry (P = 0.001), and prosthesis stability (P = 0.01). Factors that correlated with a good cosmetic result on multivariate analysis were prosthesis movement (odds ratio [OR] 4.95, P = 0.004), eyelid symmetry (OR 4.51, P = 0.006), and socket fullness (OR 3.56, P = 0.005). No correlation was observed between patients’ perceptions of the overall cosmetic result and those of the examiners.
Conclusion:
The cosmetic result of prosthesis use among anophthalmic patients is generally good, as perceived by both patients and examiners. Good eyelid position and symmetry, orbital fullness, and prosthesis motility were associated with a better cosmetic result.
Keywords: Anophthalmic sockets, cosmetic result, prosthesis
Anophthalmia may occur due to congenital pathologies or following evisceration or enucleation.[1,2] Patients with an anophthalmic socket sustain profound disfigurement accompanied by emotional and social distress.[3,4,5,6] The aim of socket implantation surgery is to restore and preserve the orbital volume and contour, thus minimizing facial asymmetry and disfigurement due to volume deficit.[7] This objective is achieved by placing an adequately sized orbital implant and later by fitting a matching prosthesis. Many implantation procedures are employed, and various implant types and sizes are available to the surgeon.[8,9,10,11,12,13,14]
To date, the success of orbital implant procedures is generally estimated by the rate of complications, such as implant exposure and extrusion, eyelid malposition, post-implantation infection, conjunctival dehiscence, and socket contraction.[15,16,17,18,19,20,21,22] Although an acceptable cosmetic result is inarguably a major objective of these procedures, there is no objective standardization of cosmetic appearance following orbital implantation, and the choice of the most suitable procedure and implant is based solely upon the surgeon’s clinical impression and experience.
Many clinicians associate patients’ complaints following implantation to postenucleation socket syndrome.[23] This entity encompasses a myriad of clinical findings related to anatomical postsurgical changes, including loss of orbital volume, superior sulcus deformity, upper lid ptosis and lower lid laxity, and prosthesis movement.[24] However, the specific impact of each of them on the clinical presentation has never been delineated. Furthermore, many patients present with part of the clinical syndrome but still describe profound overall discontent.
We sought to identify quantifiable anatomical features and functional properties related to a successful cosmetic result of ocular prostheses surgery and define cosmetic success according to the patient and to independent examiners. This report presents the results of their impressions, and defines the relevant ocular and prosthetic cosmetic variables and their relation to the cosmetic result.
Methods
Patient selection
This prospective observational study on anophthalmic patients following prosthesis fitting was approved by the institutional ethics review board (#0023-09-BNZ). Participants were selected randomly, from anophthalmic patients attending an outpatient ocular prosthetic clinic for follow-up and prosthesis maintenance. The inclusion criteria of the study were age older than 18 years and unilateral anophthalmia for at least 12 months prior to enrolment. The exclusion criteria of the study were patients with residual ocular tissue (e.g., a phthisic eye), those who underwent orbital surgery during the past 12 months (including eyelid surgery, congenital anophthalmia patients), those with acute orbital complaints (including pain, conjunctival dehiscence, active inflammation of the orbit or surrounding soft tissues), and those unable to complete a questionnaire for any reason. Ethical Standards Board approval was obtained, or a waiver was granted.
Patient self-assessment
After providing informed consent, the recruited patients were asked to complete a self-assessment questionnaire. This included information on demographics and perception of their general body image and specific ocular features. The items were presented as statements concerning body image (“I am pleased with my general appearance”) or specific ocular properties (“I think my prosthesis moves well”). The results were expressed in numerical values.
Patient and prosthesis examinations
Following their completion of the self-assessment questionnaire, the patients were examined by three independent examiners (an orbital surgeon, an ophthalmology resident, and an ocularist). Each examiner completed a detailed checklist on anatomical features and functional properties of the patient’s features. The eyelid aperture, lagophthalmos, lower eyelid laxity, exophthalmometry, lower and upper fornix depth, socket and prosthesis movement, and conjunctival inflammatory signs were assessed [Fig. 1]. The prosthesis was then removed, and its dimensions, surface size, and volume were measured. Finally, the examiners queried the patient about general and specific cosmetic features, including prosthesis movement, eyelid symmetry, adequate conjunctiva surface, socket fullness, prosthesis stability, and general cosmetic appearance. The movement of the prosthesis was compared to the contralateral eye and ranked as percentage the movement of that eye. Results of the cosmetic result questions were scored on scales ranging from 1-10, in which 1 was always the worst score. For each feature, as well as for the general cosmetic results, a score was considered as being “good” if it was in the upper third of the scale.
Figure 1.
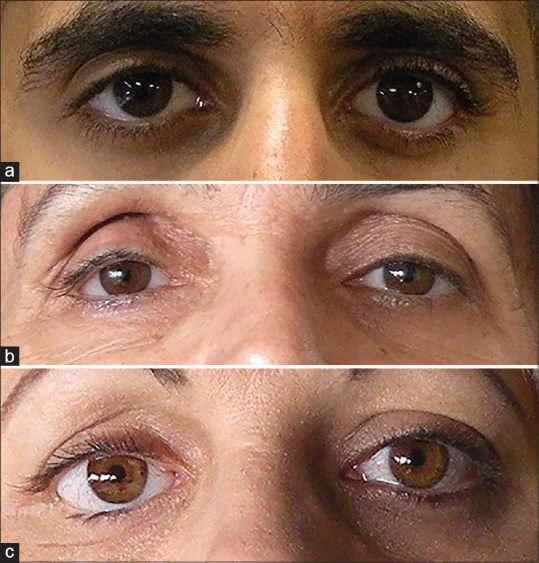
Clinical photos of three anophthalmic patients demonstrating variable cosmetic results. (a) A 32 year-old male with left ocular prosthesis and a good cosmetic result; symmetric eyelid opening and orbital volume. (b) A 61 year-old woman with a right deep superior eyelid sulcus deformity secondary to lack of orbital implant. (c) A 49 year-old woman post severe right orbital trauma and multiple reconstructions, demonstrating eyelid asymmetry secondary to lower eyelid retraction and relative enophthalmos
Statistical analysis
The statistical analysis was performed with SAS software (University edition, SAS Institute Inc.), using an alpha level of 0.05 for all measures. Inter-examiner agreement correlations were analyzed by the Fleiss–Kappa test. The Spearman correlation test was applied to analyze correlations between the variables used for the evaluations and for the scores given to the general cosmetic appearance, as well as the correlations between the examiners’ responses and those of the patients. The Kruskal–Wallis test was used to analyze correlations between anatomical variables and the general cosmetic appearance scores. An ordered logistic regression was performed to determine predictors of the general cosmetic appearance and to estimate univariate (crude) and multivariate (refined) odds ratios for the variables used for the evaluations. All of the results are presented as mean ± standard deviation.
Results
A total of 107 anophthalmic patients (50.1% females) completed the patient self-assessment questionnaire and were examined during the study. The average patient age was 53.08 ± 18.64 years (range 18–89) and time since anophthalmic surgery was 25.49 ± 2.06 years. Anophthalmia involved the right eye in 45.19% of the patients and an orbital implant was in place in 43.4% of them. The causes of anophthalmia included ocular trauma (49.5%), ocular disease (35.6%), ocular malignancy (9.9%), and ocular complications of a systemic disease (4.9%) [Table 1].
Table 1.
Demographics of 107 Anophthalmic Patients (107 Eyes) Evaluated for Ocular Prosthesis Outcome
| Variable | n |
|---|---|
| Side | |
| Right | 47 (44%) |
| Left | 60 (56%) |
| Gender | |
| Male | 53 (49%) |
| Female | 54 (51%) |
| Age (year±SD) | 53.08±18.64 |
| Mechanism of injury | |
| Ocular malignancy | 50/102 (49%) |
| Ocular trauma | 11 (9.9%) |
| Ocular disease | 38 (35.6%) |
| Systemic disease | 5 (4.9%) |
| Orbital implant present | 46 (43%) |
SD=standard deviation
The inter-examiner correlation was good for all variables (K > 0.27, P = 0.001); therefore, the average value of all three examiners was used for further analysis. The examiners estimated specific ocular cosmetic variables by focusing on those related to prosthesis function, prosthesis appearance in the socket, as well as facial symmetry. The average score was 2.86 ± 0.9 (median 3, range 1–5) for prosthesis movement, 3.6 ± 1.03 (median 4, range 1-5) for eyelid symmetry, 2.8 ± 0.55 (median 3, range 1–3) for adequate conjunctiva surface, 3.77 ± 0.48 (median 3, range 1–4) for prosthesis stability, and 3.5 ± 1.2 (median 4, range 1–5) for socket fullness. The examiners rated the general cosmetic appearance of all patients as 7.2 ± 0.19 (range 1–10). This was based on the overall impression of the cosmetic result of the subject and not on any specific factors.
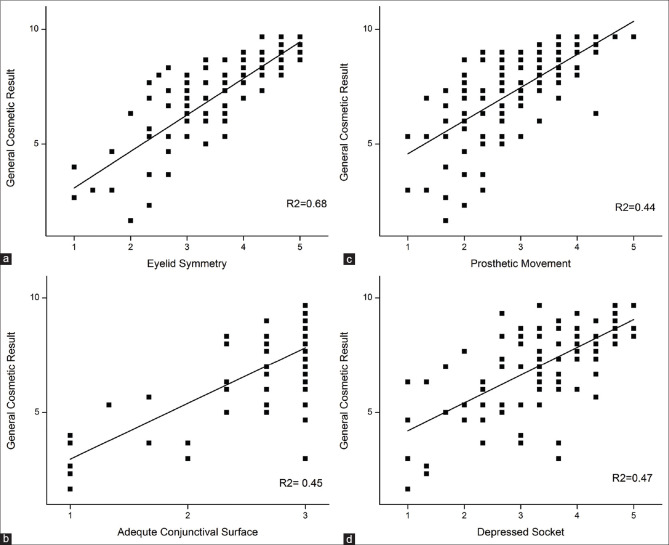
Examinations of the correlations between specific cosmetic features and the general cosmetic result revealed that prosthesis movement had an odds ratio (OR) of 6.81 (95% confidence interval [CI] 3.21 14.42, P < 0.0001, Table 2); eyelid symmetry had an OR of 7.77 (95% CI 3.58 16.87, P < 0.0001); an adequate conjunctiva surface had an OR of 5.12 (95% CI 1.6 16.32, P = 0.006), and socket fullness had an OR of 5.24 (95% CI 2.67 10.29, P < 0.0001) [Fig. 2]. The factors found on multivariate analysis to be significantly related to a good cosmetic result were prosthesis movement (OR 4.95, 95% CI 1.69 14.53, P = 0.004), eyelid symmetry (OR 4.51, 95% CI 1.55 13.09, P = 0.006), and socket fullness (OR 3.56, 95% CI 1.46 8.69, P = 0.005). Among patients who received an upper third score on all 3 of these features (a score of 4 or 5, n = 17), the predictive value of a good general cosmetic result (upper third, range 8–10) was 100%.
Table 2.
Examiner-Scored Factors Related to a Good Cosmetic Result (Upper Third of Range)
| Variable | OR (95% CI, P) | |
|---|---|---|
|
| ||
| Crude | Refined | |
| Prosthesis movement | 6.81 (3.21 14.42, <0.0001) | 2.1 (1.01 4.4, 0.045) |
| Eyelid symmetry | 7.77 (3.58 16.87, <0.0001) | 5.6 (2.4 13.5, 0.0001) |
| Orbit fullness | 5.24 (2.67 10.29, <0.0001) | 3.1 (1.6 5.9, 0.0008) |
| Sufficient conjunctiva area | 5.12 (1.6 16.32, <0.0001) | 4.1 (0.9 18.2, 0.07) |
| Prosthesis stability | 2 (0.87 4.63, 0.1) | 1.1 (0.4 3.3, 0.81) |
OR=odds ratio; CI=confidence interval
Figure 2.
Correlation between specific cosmetic features and the general cosmetic result. (a) eyelid symmetry. (b) Adequate conjunctival surface. (c) Prosthetic movement. (d) Depressed socket
The patients were asked to complete a similar questionnaire in which they were able to judge their own cosmetic result, as well as score specific features related to their appearance and prosthesis function. The average general cosmetic result the patients gave themselves was 8.1 ± 2.19 (range 1–10). The average score was 3.13 ± 1.51 (range 1–5) for prosthesis movement, was 3.41 ± 1.49 (range 1–5) for eyelid symmetry, 2.24 ± 0.86 (range 1–3) for adequate conjunctiva surface, 3.62 ± 0.85 (range 1–4) for prosthesis stability, and 3.2 ± 1.55 (range 1–5) for socket fullness. A good general cosmetic result (scale range 4–5) correlated with prosthesis movement (OR = 1.4, 95% CI 1.04 1.86, P = 0.02, Table 3), eyelid symmetry (OR = 1.66, 95% CI 1.22 2.24, P = 0.001), and prosthesis stability (OR = 1.96, 95% CI 1.17 3.27, P = 0.01). Multivariate analysis confirmed that eyelid symmetry (OR = 1.66, 95% CI 1.18 2.33, P = 0.003) and prosthesis stability (OR = 2.17, 95% CI 1.18 4.01, P = 0.01) remained significantly correlated to a good cosmetic result [Table 3].
Table 3.
Patient Self-report Factors Related to a Good Cosmetic Result (Upper Third of Range)
| Variable | OR (95% CI, P) | |
|---|---|---|
|
| ||
| Crude | Refined | |
| Prosthesis movement | 1.4 (1.04 1.86, 0.02) | 1.25 (0.88 1.78, 0.22) |
| Eyelid symmetry | 1.66 (1.22 2.24, 0.001) | 1.66 (1.18 2.33, 0.003) |
| Orbit fullness | 0.8 (0.6 1.06, 0.12) | |
| Sufficient conjunctiva area | 1.28 (0.72 2.27, 0.41) | |
| Prosthesis stability | 1.96 (1.17 3.27, 0.01) | 2.17 (1.18 4.01, 0.01) |
OR=odds ratio; CI=confidence interval.
There was a moderate correlation between patient self-report and that of the examiners regarding adequate conjunctiva surface (Spearman correlation 0.33, P = 0.001). The patients’ perceptions of general cosmetic result did not correlate with those of the examiners.
Discussion
In this study, we sought to identify quantifiable anatomical features and functional properties related to a successful cosmetic result of prostheses in patients with ocular prosthesis, and to identify the parameters that define cosmetic success. The findings demonstrated that the cosmetic results of anophthalmic patients wearing a prosthesis according to professional examiners is good in most patients. They associated a good result with the ability of the prosthesis to move in comparison to the contralateral eye, eyelid symmetry, and socket fullness. In contrast, the patients mostly rated their own cosmetic result as good according to eyelid symmetry and prosthesis stability. The only parameter that correlated well between the patients and the examiners was sufficient conjunctiva surface.
The objective of an ocular prosthesis is to achieve a cosmetic result that will allow the patient to feel that it provides an acceptable cosmetic appearance. An ocularist strives for a prosthetic cosmetic result that is as symmetrical as possible to the contralateral side [Fig. 3]. Our results confirm this, indicating that symmetry was a major deciding factor in what patients considered as being a good result. They also judged eyelid position, orbital fullness and ocular function, in the form of ocular movement, as related to a better cosmetic result.[25,26] There was no correlation between patients scoring and those of the examiners except for adequate conjunctiva surface. The factor with the greatest correlation to the patients’ definition of surgical success was prosthesis stability. This may reflect more the feeling of the prosthesis in the socket and less its appearance and explains why it was not a significant factor for the examiners. Dave et al.[27] checked anophthalmic patients’ satisfaction and objective examination by a single observer and found correlations in movement, fullness, color, and eye size. They also found that young anophthalmic patients were more concerned with their appearance, prosthesis retention, color matching, and prosthesis comfort than older patients. Our own results did not demonstrate correlations with these factors, matching more closely the results they found among older patients and reflecting the older population in our study (average age in our study was 53 with a 25 average interval between surgery and operation, compared to an average age of 28 years in their study). Our older study population was as satisfied with the prosthetic result, but less occupied with their appearance and did not appreciate the reason for asymmetry of the anophthalmic side. These results may be of decisive interest to the treating ocularist and indicate that while the ultimate goal is to provide a patient with the best possible cosmetic result, factors that observers perceive as important may not necessarily be the ones that result in patient satisfaction.
Figure 3.

Clinical photograph of a 35-YO patient before (a) and after (b) secondary orbital sphere ceramic 22 mm implant. Note the post enucleation socket syndrom (PESS) apearence before surgery with enophthalmos, ptosis and deep superior eyelid sulcus. Post operatively (b), there is symmetric fulness of both upper eyelids and improved left upper eyelid position
Patients self-impression is based not only on appearance but also on many psychological variables that influence their acceptance to wearing an ocular prosthesis, and may even be more important than clinical or demographic factors.[5] Feelings of shame, shyness, sadness, preoccupation with hiding the prosthesis, social insecurity and fear were all found to significantly affect patients self-awareness of their cosmetic image, psychosocial perceptions and behavior.[28] Conversely, observers are not impacted by these psychological factors and are more likely to base their impression on appearance. This creates a disparity between patient satisfaction and observer views. To optimize the surgical and prosthesis results, it is important to also address the more objective observation factors. This will help improve patient’s self-esteem, as well as the way they are perceived by their friends and family.
While this study includes a relatively large cohort of patients and the data were gathered in an independent manner by all the observers, the subjectivity of the responses raises several limitations to this study. The observer’s perception of cosmetic success will inevitably influence their judgment and, therefore, these results may not reflect the views of other observers, particularly with regard to cultural influences on the definitions of cosmetic beauty. However, the inclusion of three independent observers and the strong correlation between them suggest that the significant factors may indeed be related to a better overall cosmetic result. A further limitation relates to patient selection. While all patients who attended the clinic were asked to participate in the study, it is possible that those with a better cosmetic result were more likely to agree, thus resulting in the high overall favorable cosmetic result. It would be interesting to note whether future studies from other clinics in other countries reproduce results similar to these, or offer other factors that are related to success.
In this study, we focused on the main anatomical features and functional properties that are related to a favorable cosmetic result. These properties originate from the socket anatomy, surgical procedures and healing process. Specific decisions during the early stages of management and surgery affect these properties, whether the surgeon decides to insert an implant of a specific size, reattach the extraocular muscles and spare as much conjunctiva as possible, can all affect the prosthesis physical characteristics and the final cosmetic result. In larger sockets, or when an implant is not inserted, bulkier prostheses may be needed, which would affect their motility, stability and eyelid closure. Further studies are needed to explore the impact of these factors on the specific anatomical features and functional properties, as well as on the general cosmetic result. Any correlations between clinical findings and the final cosmetic outcome would be of great importance to treating physicians when choosing treatment strategies in such patients.
Conclusion
In conclusion, patients mostly considered the parameters of eyelid symmetry and prosthesis stability when grading the success of anophthalmic prostheses placement for whatever cause. Orbital surgeons, ophthalmologists, and ocularists looked at aspects concerning prosthesis motility in comparison to the contralateral eye, eyelid symmetry, and socket fullness for determining the success of the procedure. According to the findings of the current study, we propose that the oculoplastic surgeons and ocularists should rethink their priorities when planning surgery and fitting prostheses in order to accommodate the patients’ definitions of a good cosmetic result.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Revere KE, Katowitz JA, Nazemzadeh M, Katowitz WR. Management of the microphthalmic orbit. In: Katowitz, James A, William R, editors. Pediatric Oculoplastic Surgery. 2nd ed. Vol. 1. Springer; 2018. pp. 831–74. [Google Scholar]
- 2.Handler LF, Heher KL, Katowitz JA. Congenital and acquired anophthalmia. Curr Opin Ophthalmol. 1994;5:84–90. [PubMed] [Google Scholar]
- 3.Ye J, Lou L, Jin K, Xu Y, Ye X, Moss T, et al. Vision-related quality of life and appearance concerns are associated with anxiety and depression after eye enucleation:A cross-sectional study. PLoS One. 2015;10 doi: 10.1371/journal.pone.0136460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahn JM, Lee SY, Yoon JS. Health-related quality of life and emotional status of anophthalmic patients in Korea. Am J Ophthalmol. 2010;149:1005–11. e1. doi: 10.1016/j.ajo.2009.12.036. [DOI] [PubMed] [Google Scholar]
- 5.McBain HB, Ezra DG, Rose GE, Newman SP. Appearance Research Collaboration (ARC) The psychosocial impact of living with an ocular prosthesis. Orbit. 2014;33:39–44. doi: 10.3109/01676830.2013.851251. [DOI] [PubMed] [Google Scholar]
- 6.Saxby E, Davies R, Kerr J. Living with an artificial eye-the emotional and psychosocial impact. Eye (Lond) 2019;33:1349–51. doi: 10.1038/s41433-019-0398-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Borrelli M, Geerling G. Current concepts of ocular adnexal surgery. GMS Interdiscip Plast Reconstr Surg DGPW. 2013;2:Doc06. doi: 10.3205/iprs000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jovanovic N, Carniciu AL, Russell WW, Jarocki A, Kahana A. Reconstruction of the orbit and anophthalmic socket using the dermis fat graft:A major review. Ophthalmic Plast Reconstr Surg. 2020;36:529–39. doi: 10.1097/IOP.0000000000001610. [DOI] [PubMed] [Google Scholar]
- 9.Shah CT, Hughes MO, Kirzhner M. Anophthalmic syndrome:A review of management. Ophthalmic Plast Reconstr Surg. 2014;30:361–5. doi: 10.1097/IOP.0000000000000217. [DOI] [PubMed] [Google Scholar]
- 10.Son J, Kim C, Yang J. Comparison of experimental porous silicone implants and porous silicone implants. Graefes Arch Clin Exp Ophthalmol. 2012;250:879–85. doi: 10.1007/s00417-011-1902-7. [DOI] [PubMed] [Google Scholar]
- 11.Schellini S, El Dib R, Silva LR, Farat JG, Zhang Y, Jorge EC. Integrated versus non-integrated orbital implants for treating anophthalmic sockets. Cochrane Database Syst Rev. 2016;11:CD010293. doi: 10.1002/14651858.CD010293.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Custer PL, Kennedy RH, Woog JJ, Kaltreider SA, Meyer DR. Orbital implants in enucleation surgery:A report by the American Academy of Ophthalmology. Ophthalmology. 2003;110:2054–61. doi: 10.1016/S0161-6420(03)00857-1. [DOI] [PubMed] [Google Scholar]
- 13.Kim EL, Bernardino CR, Levin F. Orbital volume augmentation using expandable hydrogel implants in acquired anophthalmia and phthisis bulbi. Orbit. 2016;35:91–6. doi: 10.3109/01676830.2016.1139593. [DOI] [PubMed] [Google Scholar]
- 14.Schmitzer S, Simionescu C, Alexandrescu C, Burcea M. The anophthalmic socket-reconstruction options. J Med Life. 2014;(Spec No. 4):23–9. 7. [PMC free article] [PubMed] [Google Scholar]
- 15.Shoamanesh A, Pang NK, Oestreicher JH. Complications of orbital implants:A review of 542 patients who have undergone orbital implantation and 275 subsequent PEG placements. Orbit. 2007;26:173–82. doi: 10.1080/01676830701555204. [DOI] [PubMed] [Google Scholar]
- 16.Custer PL, Trinkaus KM. Porous implant exposure:Incidence, management, and morbidity. Ophthalmic Plast Reconstr Surg. 2007;23:1–7. doi: 10.1097/01.iop.0000249432.18688.ee. [DOI] [PubMed] [Google Scholar]
- 17.Wang J-K, Liao S-L, Lai P-C, Lin LLK. Prevention of exposure of porous orbital implants following enucleation. Am J Ophthalmol. 2007;143:61–7. doi: 10.1016/j.ajo.2006.09.037. [DOI] [PubMed] [Google Scholar]
- 18.Sagoo MS, Rose GE. Mechanisms and treatment of extruding intraconal implants:Socket aging and tissue restitution (the “Cactus Syndrome“) Arch Ophthalmol. 2007;125:1616–20. doi: 10.1001/archopht.125.12.1616. [DOI] [PubMed] [Google Scholar]
- 19.Nunery WR, Cepela MA, Heinz GW, Zale D, Martin RT. Extrusion rate of silicone spherical anophthalmic socket implants. Ophthalmic Plast Reconstr Surg. 1993;9:90–5. doi: 10.1097/00002341-199306000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Shore JW, McCord CD, Jr, Bergin DJ, Bergin DJ, Dittmar SJ, Maiorca JP, et al. Management of complications following dermis-fat grafting for anophthalmic socket reconstruction. Ophthalmology. 1985;92:1342–50. doi: 10.1016/s0161-6420(85)33865-4. [DOI] [PubMed] [Google Scholar]
- 21.Tawfik HA, Raslan AO, Talib N. Surgical management of acquired socket contracture. Curr Opin Ophthalmol. 2009;20:406–11. doi: 10.1097/ICU.0b013e32832ed85b. [DOI] [PubMed] [Google Scholar]
- 22.Smerdon DL, Sutton GA. Analysis of the factors involved in cosmetic failure following excision of the eye. Br J Ophthalmol. 1988;72:768–73. doi: 10.1136/bjo.72.10.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tyers AG, Collin JR. Orbital implants and post enucleation socket syndrome. Trans Ophthalmol Soc U K. 1982;102(Pt 1):90–2. [PubMed] [Google Scholar]
- 24.Smit TJ, Koornneef L, Zonneveld FW, Groet E, Otto AJ. Computed tomography in the assessment of the postenucleation socket syndrome. Ophthalmology. 1990;97:1347–51. doi: 10.1016/s0161-6420(90)32411-9. [DOI] [PubMed] [Google Scholar]
- 25.Raizada K, Shome D, Honavar SG. New measurement device and technique for assessing implant and prosthetic motility. Ophthalmic Plast Reconstr Surg. 2007;23:59–60. doi: 10.1097/IOP.0b013e31802dd428. [DOI] [PubMed] [Google Scholar]
- 26.Johnson WJ. Fitting the anophthalmic socket:Achieving cosmesis with comfort. Adv Ophthalmic Plast Reconstr Surg. 1990;8:126–35. [PubMed] [Google Scholar]
- 27.Dave TV, Nayak A, Palo M, Goud Y, Tripuraneni D, Gupta S. Custom ocular prosthesis-related concerns:Patient feedback survey-based report vis-à-vis objective clinical grading scales. Orbit. 2020:1–7. doi: 10.1080/01676830.2020.1797826. doi:10.1080/01676830.2020.1797826. [DOI] [PubMed] [Google Scholar]
- 28.Goiato MC, dos Santos DM, Bannwart LC, Moreno A, Pesqueira AA, Haddad MF, et al. Psychosocial impact on anophthalmic patients wearing ocular prosthesis. Int J Oral Maxillofac Surg. 2013;42:113–9. doi: 10.1016/j.ijom.2012.05.028. [DOI] [PubMed] [Google Scholar]