Abstract
Umbilicoplasty is a key component of any abdominoplasty as the umbilicus has been described as the central aesthetic subunit to the abdomen. Here, we describe our preferred technique for umbilicoplasty which involves a half-moon design with periumbilical defatting which in our hands produces consistent, aesthetically pleasing results.
The umbilicus forms the central aesthetic subunit of the abdomen, and examples of an aesthetically pleasing umbilicus have been previously described in detail.1,2 The critical components of the aesthetically pleasing umbilicus as described by Craig et al include small size, T-shape or vertical orientation, and superior hooding.3 A widened, everted, or horizontally oriented umbilicus is readily perceived as displeasing and can be a source of much discontent for abdominal contouring patients both preoperatively and postoperatively. These factors need to be taken into consideration when planning for umbilicoplasty.
Umbilicoplasty in abdominal contouring procedures involves repositioning and insetting of the umbilicus following excision of excess skin and subcutaneous tissue with or without plication of the abdominal wall.4 A number of techniques have been described for insetting the umbilicus at the time of abdominoplasty, and each seeks to address the components of an aesthetically pleasing umbilicus.5,6 Despite the current body of literature regarding umbilicoplasty, there has yet to be written a reliable technique with a simple learning curve that achieves consistent and reproducible results in a wide variety of patients with different body habitus.
Here, we describe our technique for half-moon umbilicoplasty, which is a simple, easily reproducible, stepwise procedure with results that we have found to be consistently pleasing with a stable appearance over time (Video). Our technique achieves all goals of umbilicoplasty: carefully controlled size, superior hooding and vertical orientation through asymmetric flap design, and inversion through careful tethering of the stalk to the abdominal wall and can be applied to a range of different abdominal contours with consistent results.
SURGICAL TECHNIQUE
Marking and Local Anesthesia
Once the patient has been appropriately sedated/intubated and properly positioned on the operating table, we begin by marking the midline of the abdomen from the anterior commissure of the labia majora up to the xiphoid. We additionally mark a semi-lunate incision around the umbilicus with a diameter and height measuring approximately 1.5 cm; this can vary slightly depending on the patient’s body habitus (Figure 1A, B). It is the senior author’s preference to then tattoo the markings with methylene blue to maintain the integrity of markings during prepping and throughout the operation. Maintaining anatomic orientation of the umbilicus throughout the procedure is critical to avoid accidental twisting of the umbilical stalk and potential devitalization of the umbilicus. The patient is then prepped and draped in the usual sterile fashion.
Figure 1.
Preoperative axis and umbilical markings. (A) Representative image of preoperative markings showing the midline, upper horizontal incision, and periumbilical markings with and semi-lunate incision. (B) Diagram demonstrating the preoperative semi-lunate incision. Note the inferior inverted V, which is important for the future inset of the neo-umbilicus.
Initial Dissection of Umbilical Stalk
The operation begins with an incision made along the semi-lunate umbilical marking using a #11 blade scalpel while the umbilicus is lifted with 2 single hooks. Dissection of the umbilical stalk is then carried out using Metzenbaum scissors in a “pushing manner.” This maneuver should be continued circumferentially around the native umbilicus to free it from the abdominal tissue. It is imperative during this time to avoid blindly transecting the umbilical stalk and to avoid accidentally entering an unsuspected periumbilical hernia.
Once dissection of the umbilical stalk is complete, it is critical to mark the umbilicus to maintain its orientation throughout the remainder of the case. The senior author’s preferred technique is to suture a 1.5-cm cut end of suction tubing to the umbilicus with the flange facing superiorly (Figure 2). This maneuver makes it easier to palpate and identify the position of the umbilicus beneath the abdominal flap toward the end of the case when the umbilical transposition takes place.
Figure 2.

Umbilical marker using the distal end of suction tubing. Representative photograph demonstrating tagging of the umbilicus with the distal end of the suction tubing. This is sutured into place using 3-0 Nylon suture.
Following this step, the surgeon should proceed to perform the abdominoplasty in his/her preferred manner. If rectus plication is being performed, it should be done with great care to avoid strangulation of the umbilical stalk. After trimming excess skin from the superior abdominoplasty skin flap, closure of the abdomen is begun in the midline. While the lateral aspects of the incision are still open, palpate the location of the umbilical stalk and transpose this onto the abdominoplasty skin flap by marking it with a transverse line perpendicular to the midline marking.
Creation of Umbilicus
Once the abdominoplasty incision is closed, an inferiorly based flap is designed by marking an inverted U-shaped incision that is 1.5 cm in diameter and is drawn with the 2 ends beginning and ending on the recently transposed transverse line at the level of the new umbilicus. This flap will become the inferior aspect of the neo-umbilicus.
The outlined flap is incised through the epidermis and dermis down to the subcutaneous tissue. When performing this maneuver, it is important to leave a small amount of subcutaneous tissue on your inferiorly based flap. With a fine-tipped needle cautery (eg, Colorado tip) on a medium setting, a generous amount of subcutaneous fat is resected circumferentially around the position of the new umbilicus. It is especially important to resect enough fat superior and inferior to the neo-umbilicus to create a pleasant umbilical sulcus (Figure 3A, B). The dissection is carried down to the abdominal fascia.
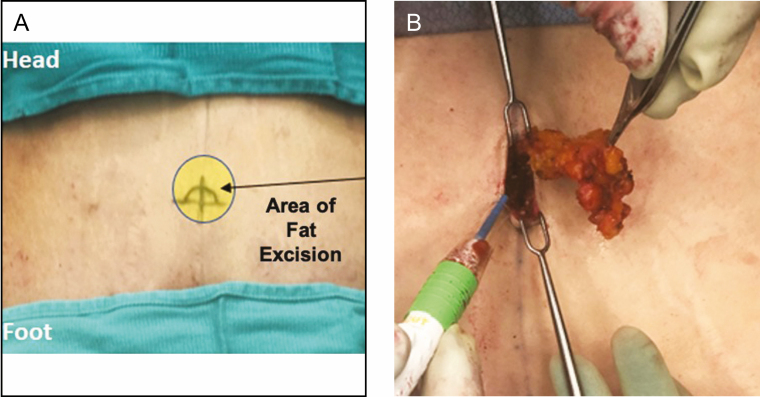
Figure 3.
Circumferential adipose tissue debulking. (A) Overlay depiction of the periumbilical area that undergoes defatting. (B) Image depicting typical periumbilical fat excision, which is performed using an insulated fine needle cautery tip.
Following fat resection, the umbilicus is located using the previously placed umbilical marker. At this point, it is important to ensure that the umbilical stalk is not twisted by identifying the superiorly positioned flange and the methylene blue tattooing. A clear 3-0 polydioxanone suture is placed on the superior aspect (12 o′clock) of the umbilicus from the abdominal wall fascia to the midline dermis of the abdominal skin to the midline dermis of the superior border of the umbilicus but not tied yet to allow for the placement of a second suture. This second similar suture is placed including the dermis of the midline of the inferior border (6 o′clock) of the umbilicus and the apex of the U-flap. This is performed to better define the umbilical sulcus and draw the scars into the sulcus making them less visible.
The final maneuver is to tie both of the polydioxanone sutures down with the goal of pulling the superior edge of the umbilicus down toward the abdominal wall and into the previously defatted space. Additional sutures at the 3′ and 9 o′clock positions can be used if desired to improve the aesthetic result and can be specifically helpful in thin abdominal flaps. If performing a Fleur-de-lis abdominoplasty, a vertically rather than horizontally oriented lenticular incision should be used, and all 4 quadrants of the above-described sutures should always be used to inset the umbilicus. If the preoperative umbilicus is considerably stretched out, shortened of the umbilicus can be performed by trimming the distal end. The final closure is completed by using 4-0 clear Monocryl deep dermal sutures around the entirety of the umbilicus followed by a running 5-0 fast-absorbing plain gut suture followed by cyano-acrylate skin glue (Figure 4A-E).
Figure 4.
The end result of umbilicoplasty following epidermal closure and gluing. (A) Preoperative image of a 53-year-old female before abdominoplasty. (B) Acute postoperative image of this patient depicting the degree of periumbilical depression relative to the surface plane in oblique view of the periumbilical depression. (C) 1-year postoperative image of the patient from Figure 4A. (D) 1-year postoperative image of a 53-year-old female following abdominoplasty. (E) 1-year postoperative image of a 51-year-old female following abdominoplasty.
DISCUSSION
In this manuscript, we describe our preferred surgical technique for umbilicoplasty in the setting of abdominoplasty. Given the importance of the umbilicus as the central aesthetic unit of the abdomen, being able to achieve reproducible, cosmetically acceptable results is of upmost important. In our experience, our technique meets these standards and incorporates all the keys of an aesthetically pleasing umbilicus: small, vertically orientated with superior hooding.3
There are several reports in the literature describing different variations in umbilicoplasty.2,4,7-13 In a recent systematic review by Joseph et al, the authors elegantly describe the various differences in approaches described by these reports. Specifically, the components of umbilicoplasty can be broken down into umbilical incision, abdominal incision, suturing of the umbilicus to the rectus, stalk plication, periumbilical defatting, and skin suture.6 The variations of umbilical incision include round, round with superior excision, round with inferior excision, vertical ellipse, and inverted-U. Variations of abdominal incision include similarly round, vertical ellipse and inverted-U along with vertical line, Y-shaped, inverted-V chevron, double-opposing Y, inverted-V, and vertical oval.
Our technique is unique to all other described methods although is most similar to Malic et al.10 Both techniques employ an inverted-U umbilical and abdominal incision and periumbilical defatting. Our technique differs in that the umbilical incision is more of an inverted-V than an inverted-U, though the abdominal flap is an inverted-U. We also prefer to keep this inferior flap thicker leaving some subcutaneous tissue rather than incising at the level of the deep dermis. This helps to ensure the viability of this small flap and makes the transition from the inferior abdominal skin to the umbilical sulcus smoother. We perform more extensive circumferential defatting, approximately 1.5 cm superior and inferior and 0.5 cm lateral to the umbilical incisions. The amount of fat removed will depend on the actual thickness of the abdominal flap. Finally, when securing the umbilicus to the rectus fascia, we like to secure at both the 6 and 12 o′clock positions rather than just at the 6 o′clock position. This allows for a better definition of the umbilical sulcus and helps hide the lower scar making it less visible.
The senior author feels that natural scar contraction of the superior border incision over time can result in an umbilical hood, which is aesthetically desirable. This technique of umbilicoplasty can also be coupled with midline superior liposculpting from the umbilicus to the xiphoid to accentuate the linea alba. Finally, in patients with thin abdominal flaps, additional sutures can be placed at 3 and 9 o′clock positions to increase the umbilical setback to accentuate the umbilical contour (Figure 5A, B). In conclusion, our surgical technique for umbilicoplasty is unique and allows for an aesthetically pleasing umbilicus that is easily reproducible.
Figure 5.
Umbilicoplasty in fleur-de-lis abdominoplasty. (A) Preoperative image of a 41-year-old female before fleur-de-lis abdominoplasty. (B) Postoperative image 2 years following fleur-de-lis abdominoplasty.
Supplementary Material
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
- 1.Matarasso A, Wallach SG. Abdominal contour surgery: treating all aesthetic units, including the mons pubis. Aesthet Surg J. 2001;21(2):111-119. [DOI] [PubMed] [Google Scholar]
- 2.Pallua N, Markowicz MP, Grosse F, Walter S. Aesthetically pleasant umbilicoplasty. Ann Plast Surg. 2010;64(6):722-725. [DOI] [PubMed] [Google Scholar]
- 3.Craig SB, Faller MS, Puckett CL. In search of the ideal female umbilicus. Plast Reconstr Surg. 2000;105(1):389-392. [DOI] [PubMed] [Google Scholar]
- 4.Castillo PF, Sepulveda CA, Prado AC, Troncoso AL, Villaman JJ. Umbilical reinsertion in abdominoplasty: technique using deepithelialized skin flaps. Aesthetic Plast Surg. 2007;31(5):519-520. [DOI] [PubMed] [Google Scholar]
- 5.Clo TC, Nogueira DS. A new umbilical reconstruction technique used for 306 consecutive abdominoplasties. Aesthetic Plast Surg. 2012;36(5):1009-1014. [DOI] [PubMed] [Google Scholar]
- 6.Joseph WJ, Sinno S, Brownstone ND, Mirrer J, Thanik VD. Creating the perfect umbilicus: a systematic review of recent literature. Aesthetic Plast Surg. 2016;40(3):372-379. [DOI] [PubMed] [Google Scholar]
- 7.Bruekers SE, van der Lei B, Tan TL, Luijendijk RW, Stevens HP. “Scarless” umbilicoplasty: a new umbilicoplasty technique and a review of the English language literature. Ann Plast Surg. 2009;63(1):15-20. [DOI] [PubMed] [Google Scholar]
- 8.Dogan T. Umbilicoplasty in abdominoplasty: a new approach. Ann Plast Surg. 2010;64(6):718-721. [DOI] [PubMed] [Google Scholar]
- 9.Lesavoy MA, Fan K, Guenther DA, Herrera F, Little JW. The inverted-v chevron umbilicoplasty for breast reconstruction and abdominoplasty. Aesthet Surg J. 2012;32(1):110-116. [DOI] [PubMed] [Google Scholar]
- 10.Malic CC, Spyrou GE, Hough M, Fourie L. Patient satisfaction with two different methods of umbilicoplasty. Plast Reconstr Surg. 2007;119(1):357-361. [DOI] [PubMed] [Google Scholar]
- 11.Mazzocchi M, Trignano E, Armenti AF, Figus A, Dessy LA. Long-term results of a versatile technique for umbilicoplasty in abdominoplasty. Aesthetic Plast Surg. 2011;35(4):456-462. [DOI] [PubMed] [Google Scholar]
- 12.Rodriguez-Feliz JR, Makhijani S, Przybyla A, Hill D, Chao J. Intraoperative assessment of the umbilicopubic distance: a reliable anatomic landmark for transposition of the umbilicus. Aesthetic Plast Surg. 2012;36(1):8-17. [DOI] [PubMed] [Google Scholar]
- 13.Rozen SM, Redett R. The two-dermal-flap umbilical transposition: a natural and aesthetic umbilicus after abdominoplasty. Plast Reconstr Surg. 2007;119(et al. ):2255-2262. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.