Abstract
Background:
The incidence of post-traumatic osteoarthritis (PTOA) using clinical radiographic grading criteria at 10 years after anterior cruciate ligament reconstruction (ACLR) has not been well-defined in a prospective cohort of young athletic patients.
Hypothesis:
Among young athletic patients, there is a high incidence of clinical radiographic PTOA at 10 years after ACLR. Additionally, there is a significant difference in clinical radiographic osteoarthritis changes (joint space narrowing [JSN] and osteophyte formation) between the ACL reconstructed and contralateral knees at 10 years.
Study Design:
Observational analysis of prospective multicenter cohort data; Level of evidence, 4.
Methods:
The first 146 patients in an ongoing nested cohort study within the Multicenter Orthopaedic Outcomes Network (MOON) prospective cohort presented for minimum 10-year follow-up. Included patients had a sports-related ACL injury, were age <33 years at time of ACLR, no prior history of ipsilateral or contralateral knee surgery, and no revision ACLR before follow-up. Bilateral knee metatarsophalangeal (MTP) view radiographs were obtained and graded by International Knee Documentation Committee (IKDC), Osteoarthritis Research Society International (OARSI), and modified Kellgren-Lawrence (KL) criteria by two blinded reviewers. The incidence and severity of ipsilateral and contralateral radiographic osteoarthritis were determined among patients without a contralateral ACL injury before 10-year follow-up (n=133).
Results:
Inter-rater reliability was substantial for IKDC (Gwet’s AC1 = 0.71), moderate for KL (0.48), and almost perfect for OARSI (0.84) grading systems. Among patients with a contralateral radiographically normal knee, the 10-year incidence of clinical radiographic PTOA after ACLR is 37% as defined by osteophytes and 23% as defined by JSN. The maximum side-to-side difference in medial or lateral compartment OARSI osteophyte grade was 0 in 65% of patients, 1 in 20%, and 2+ in 15%. The maximum difference in OARSI JSN grade was 0 in 77% of patients, 1 in 19%, and 2+ in 4%.
Conclusion:
In young active patients, the 10-year incidence of clinical radiographic PTOA after ACLR is 37% as defined by osteophytes and 23% as defined by JSN. The average difference in degree of osteophyte formation (≤1 grade in 85%) and JSN (≤1 grade in 96%) between the ACL reconstructed knee and contralateral knee is small.
Keywords: ACL reconstruction, joint space narrowing, post-traumatic osteoarthritis, radiographic osteoarthritis, weight bearing radiographs
Introduction
Anterior cruciate ligament (ACL) tears occur frequently in young athletic patients. These injuries often result in pathologically increased anterior and rotational laxity,2 with athletes frequently reporting knee instability during cutting and pivoting activities. A primary goal of ACL reconstruction (ACLR) is to reduce this increased anterior and rotational laxity of the knee. Unfortunately, patients are at increased risk for post-traumatic osteoarthritis (PTOA) after ACL injury regardless of surgical treatment or timing of surgery.31
Many studies have attempted to determine the risk of radiographic PTOA at long-term follow-up after ACLR with widely disparate results and often low methodological quality. A 2015 systematic review identified 64 studies with minimum 2-year follow-up that investigated risk factors for PTOA after ACL injury; only 2 of 64 studies were deemed low risk of bias and only 18 of 64 had a sample greater than 100 patients with follow-up data.31 In a 2009 systematic review of ACLR studies with minimum 10-year radiologic follow-up, 7 different radiologic grading systems were utilized in 31 studies with a prevalence of PTOA ranging from 0–48%.36 The same group performed an updated review in 2019 of studies published after August 2008 with minimum 10-year follow-up (n=41 studies identified) and found the prevalence of radiographic PTOA ranged from 0–100% in studies with a low methodologic quality rating and 1–80% in studies with a high methodologic quality rating.22 Common key shortcomings of prior studies of long-term risk of PTOA after ACLR are lack of a rigorous prospective cohort design, use of a non-standardized or non-reproducible protocol for obtaining radiographs, reliance on a radiographic assessment tool to define PTOA that has sub-optimal inter-rater reliability and fails to individually consider distinct pathologic changes in OA (osteophytes and joint space narrowing for example), and failure to consider the status of the contralateral un-injured knee.
It is difficult to counsel young athletic patients on the risk of clinical radiographic PTOA after ACLR as high-quality prospective evidence on the long-term incidence of PTOA in this specific patient population is scarce. Therefore, the goals of the current study were to determine the following in a young athletic cohort of patients following unilateral primary ACLR: 1) to determine the incidence of PTOA using clinical radiographic grading criteria, and 2) to determine the average side-to-side difference in radiographic osteoarthritic changes at 10 years after ACLR. In this cohort of young athletic patients, we hypothesized a high incidence of clinical radiographic PTOA at 10 years in the ACL reconstructed knee and a significant difference in the degree of osteoarthritic changes (joint space narrowing and osteophyte formation) between the reconstructed knee and contralateral knee.
Methods
Participants
During years 2005 through 2012, the Multicenter Orthopaedic Outcomes Network (MOON) consortium recruited a nested cohort of young athletic patients who underwent primary ACLR within 3 of the 7 consortium sites, with the primary interest of looking at PTOA. The inclusion criteria for this nested cohort included patients who were injured in sports with no history of concomitant ligament surgery, no previous ipsilateral knee surgery, no previous contralateral ACL injury or contralateral knee surgery, age less than 33 years at the time of primary ACLR, no contralateral ACL injury within 2 years after primary ACLR, and no revision ACL surgery before 10-year follow-up. An upper age limit was included in the study inclusion criteria as older patients are more likely to be less active and more likely to have degenerative OA changes unrelated to ACL injury. Among patients in the nested cohort study, reconstruction was performed by 1 of 5 experienced sports medicine fellowship-trained surgeons with acceptably low variability in femoral and tibial tunnel placement between cases and between surgeons.32 Rehabilitation following ACLR occurred following standardized guidelines.35 Each institution’s institutional review board approved the study. This nested cohort study is registered at ClinicalTrials.gov (identifier NCT02717559).
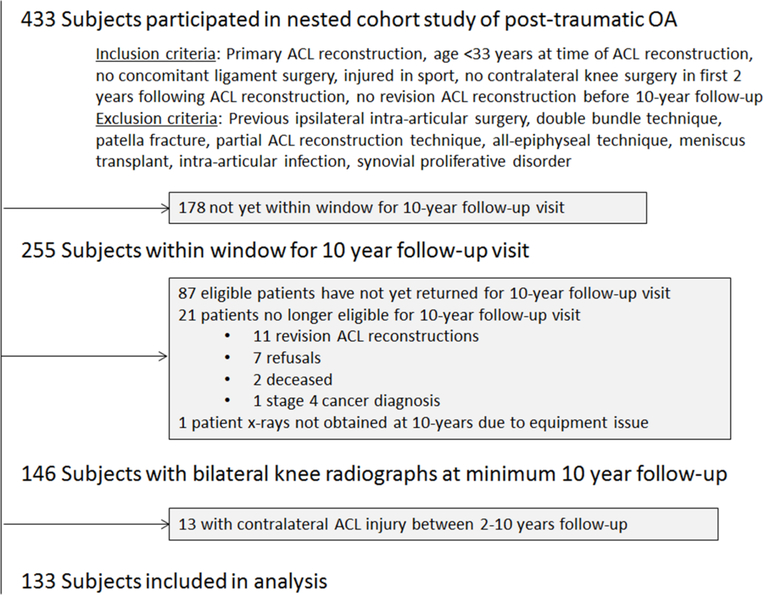
At the time of the current study, 147 of the total 255 patients within the window for a minimum 10-year follow-up visit had returned to their enrollment center to obtain bilateral knee radiographs (Figure 1); recruitment for minimum 10-year follow-up is still ongoing. One patient was unable to get radiographs at the visit due to an equipment issue (missing foot placement mat needed for correct positioning of the specialized x-ray view) and 13 of the 146 patients with radiographs had sustained a contralateral knee ACL injury with subsequent reconstruction between 2 and 10-years follow-up. This resulted in inclusion of 133 patients in the current study analysis.
Figure 1.
STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) diagram. ACL, anterior cruciate ligament. OA, osteoarthritis.
Baseline data collection
All participants completed questionnaires at enrollment to capture demographic information, injury history, patient-reported outcome measures, and the Marx activity level.24 Surgeon-completed questionnaires at the time of surgery documented physical examination, arthroscopic findings, and surgical technique that included graft type and meniscal and cartilage pathology and treatment. Meniscal status was classified as normal, stable meniscal tear without treatment, meniscal repair, or partial meniscectomy. Articular cartilage status grouped into two categories according to the modified Outerbridge scale: normal/grade 1 or grade 2, 3, or 4.23,27
Radiographic technique
Fixed flexion weight bearing radiographs using the metatarsophalangeal (MTP) radiographic technique4–6 were obtained at the 10-year follow-up visit. The MTP technique and measurement protocols are described in detail in related publications for risk factors of lateral16 and medial17 joint space narrowing after ACLR. This technique allows for high reproducibility of joint positioning6 and reliable assessment of joint space narrowing in the setting of knee OA.19 Fixed flexion radiographs were obtained with patients positioned with their feet in 15 degrees of external rotation and the first MTP point directly underneath the front of the x-ray detector. The patients bent their knees such that the patellae touched the detector. A free-standing calibration reference (Radiation Product Design, Albertville, MN) containing evenly spaced 5mm radio-opaque balls was positioned next to the fibular head, vertical to the ground. Identical positioning equipment was used at all sites. The images were felt to be adequate for radiographic grading in all cases; no cases were excluded due to image quality problems.
Radiographic grading
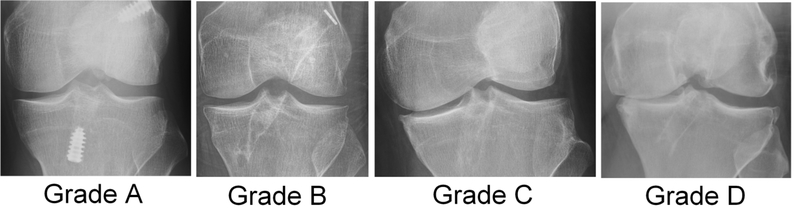
Quantitative assessments of joint space width can be performed on MTP radiographs, though this method is difficult to employ in a clinical setting as it requires computer-aided measurements with specialized software.9 Therefore, all radiographs were graded using three semi-qualitative radiographic grading scales in order to improve clinical interpretability of results. The International Knee Documentation Committee (IKDC) radiographic OA grading scale was selected as it has previously been shown to have high inter-rater reliability among surgeons grading radiographs of ACL reconstructed knees.34 Grade A is defined as no joint space narrowing (at least 4 mm of joint space), grade B defined as at least 4 mm joint space but small osteophytes, slight sclerosis, or femoral condyle flattening, grade C defined as 2–4 mm joint space, and grade D defined as <2 mm joint space (Figure 2).14
Figure 2.
Representative examples of IKDC osteoarthritis grades at 10 years after ACL reconstruction.
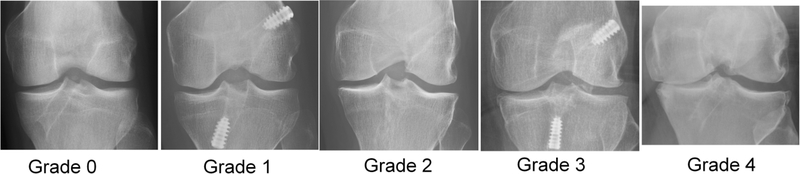
The modified Kellgren-Lawrence (KL) grading scale was selected as it is widely used in clinical settings. The KL grading system has fair to moderate reliability34, and due to its widespread use and inexact wording of the originally described scale18, several variations of the grading system have been utilized in epidemiological studies.30 For the purpose of the current study, KL grades were assigned as follows: grade 0, no radiographic evidence of osteoarthritis; grade 1, doubtful joint space narrowing and possible osteophytic lipping; grade 2, definite osteophytes and possible joint space narrowing; grade 3, definite but <50% joint space narrowing; and grade 4, >50% joint space narrowing (Figure 3).
Figure 3.
Representative examples of modified Kellgren-Lawrence knee osteoarthritis grades at 10 years after ACL reconstruction.
The Osteoarthritis Research Society International (OARSI) grading scale for knee OA was also utilized. The medial and lateral tibiofemoral compartments are graded separately, with grades 0–3 assigned for joint space narrowing, tibial osteophytes, and femoral osteophytes. For the purpose of the current study, grading of joint space narrowing and osteophyte formation was based upon comparison with representative images from the standardized, publicly available OARSI radiologic atlas.1
Clinical radiographic osteoarthritis grading scales rely on individual interpretation of radiographs and have varying degrees of inter-rater reliability34. To determine the inter-rater reliability of the IKDC, modified KL, and OARSI grading scales in the specific patient population and radiographic protocol used in the current study, bilateral knee radiographs were graded by two independent reviewers blinded to patient and surgical information, with the exception of ACLR status. Anterior cruciate ligament reconstruction status was not blinded due to multiple radiographic signs of ACLR (including bone tunnels and implants utilized for graft fixation). After determining inter-rater reliability of the three grading scales based on the initial review, all radiographs with discrepant scores were then reviewed by both reviewers simultaneously and with continued blinding to all patient and surgical data. If agreement could not be met by secondary review, a mechanism was in place for adjudication by a third reviewer, though no cases required this step. The purpose of the secondary review was to obtain agreement on a final grade rather than averaging two grades; averaging grades would result in creation of half-grades (as an example, KL grade 2.5 as the average of grade 2 and grade 3) that do not exist on the original scales and are therefore difficult to interpret.
Definition of osteoarthritis
Multiple definitions have been utilized in previous literature to define OA using clinical radiographic grading criteria.8,10 For the purposes of the current study, we utilized two definitions of OA to improve the interpretability of results. The first definition of OA is the presence of definite osteophytes, which is represented on the clinical grading scales as IKDC grade B or higher, KL grade 2 or higher, and an OARSI osteophyte grade of 1 or more on either the femur or tibia of either compartment. The second definition of OA is the presence of joint space narrowing of OARSI grade 1 or greater in either the medial or lateral compartment. All high KL grade (3 and 4) and IKDC grade (C and D) knees meet the joint spaced narrowing-based definition of OA, and no normal (IKDC A) or normal/near normal (KL 0 and 1) knees meet this definition. However, due to the language used in the definition of KL grade 2 (possible joint space narrowing) and use of a specific joint space width cutoff (≥4 mm) for IKDC grade B, some but not all KL 2 or IKDC B knees may have mild narrowing as reported on the OARSI grading scale.
Statistical analysis
All statistical analyses were performed with standard statistical software packages (JMP Pro 15.0; SAS Institute, Cary NC) (STATA 15.1; StataCorp, College Station, TX). It is our belief that an estimation of the incidence of PTOA must be within 15% of the true population value in order to facilitate a meaningful discussion of PTOA risk to a young active patient with an ACL injury who is considering ACLR surgery. An a-priori power analysis determined that interim analysis of the initial 100 patients with 10-year follow-up in the ongoing nested cohort would be adequate to determine the incidence of post-traumatic osteoarthritis with a 95% confidence interval of ±14% at 80% power. A total of 133 patients in the current study analysis and a-priori determined sample size of 100 patients was therefore exceeded. Inter-rater reliability between blinded reviewers for OA grading scales was determined by Gwet’s AC1 statistic as this is provides a more stable estimate and is less affected by prevalence and marginal probability than Cohen’s Kappa.12,13,33 Values for Gwet’s AC1 statistic vary from 0 to 1.0, and Landis and Koch20 suggest the following benchmark scale for interpreting inter-rater agreement: <0.00 poor; 0.00–0.20 slight; 0.21–0.40 fair; 0.41–0.60 moderate; 0.61–0.80 substantial; 0.81–1.00 almost perfect. The percentages of ACLR and contralateral knees with OA according to osteophyte and joint space narrowing definitions were estimated for the entire sample; the percentages of PTOA in the ACLR knee (per both OA definitions) were also determined in the subset of patients without evidence of OA in the contralateral knee. The percentage of ACLR and contralateral knees within each IKDC grade, modified KL grade, and OARSI joint space narrowing and osteophyte grades (both compartment specific grades as well as maximum grade in either compartment) were determined. Finally, side-to-side differences in OA severity were reported as the percentage of patients with 0 through 3 grades difference between knees in IKDC grade, 0 through 4 grades difference in KL grade, 0 through 3 grades difference in OARSI joint space narrowing grade, and 0, 1, 2, or 3+ grades difference in OARSI osteophyte grade (femoral + tibial grade in same compartment). Differences in OARSI joint space narrowing and osteophyte grades were determined for the entire knee (maximum grade either compartment in the ACL reconstructed knee versus contralateral knee) as well as medial and lateral compartment-specific differences in OARSI grades.
Results
Demographics and inter-rater reliability of radiographic osteoarthritis scoring systems
Among the 133 patients included in the analysis who did not have repeat ipsilateral ACL surgery or primary contralateral ACL surgery, the median age at the time of ACLR was 21 years (interquartile range: 19–25 years) and 51% of patients were female (Table 1). The median Marx activity score24 at the time of ACLR was16 (interquartile range: 12–16) and body mass index (BMI) was 22.9 kg/m2 (interquartile range: 21.0, 25.1). The graft utilized for ACLR was patella tendon autograft in 62%, hamstring autograft in 35%, and allograft in 3%. Outerbridge grade 2+ articular cartilage damage was encountered intraoperatively in the medial compartment in 9% of patients, in the lateral compartment in 17%, and in the patellofemoral compartment in 7%. The medial meniscus was normal in 63% of patients, had a stable tear left in situ or abraded & trephinated in 10.5%, had a tear treated with repair in 16.5%, and had a tear treated with partial meniscectomy in 10%. The lateral meniscus was normal in 44% of patients, had a stable tear left in situ or abraded & trephinated in 19.5%, had a tear treated with repair in 7.5%, and had a tear treated with partial meniscectomy in 29%.Subsequent ipsilateral arthroscopic knee surgery (non-ACL surgery) occurred in 19% at median 2.5 years after ACLR (interquartile range 0.72–5.27 years), and none of the 133 patients included the analysis had contralateral knee surgery (ACL-surgery or non-ACL surgery) by 10 years follow-up (Table 1).
Table 1.
Demographics at time of ACL reconstruction, intraoperative findings, and repeat non-ACL surgerya
| Variable | Level | Median (interquartile range) or Number (percentage) |
|---|---|---|
| Age, years | 21 (19, 25) | |
|
| ||
| Sex | Male Female |
65 (49%) 68 (51%) |
|
| ||
| Body Mass Index (BMI), kilograms/meters2 | 22.9 (21.0, 25.1) | |
|
| ||
| Smoking status | Current Quit Never smoked |
4 (3%) 8 (6%) 121 (91%) |
|
| ||
| ACL graft type | BTB autograft Hamstring autograft Allograft |
82 (62%) 47 (35%) 4 (3%) |
|
| ||
| Marx activity score | 16 (12, 16) | |
|
| ||
| Medial meniscus status | Normal Stable untreated tear Stable tear, trephination Repaired tear Partial meniscectomy |
84 (63%) 12 (9%) 2 (1.5%) 22 (16.5%) 13 (10%) |
|
| ||
| Lateral meniscus status | Normal Stable untreated tear Stable tear, trephination Repaired tear Partial meniscectomy |
58 (44%) 24 (18%) 2 (1.5%) 10 (7.5%) 39 (29%) |
|
| ||
| Medial compartment articular cartilage status | Grade 0–1 Grade 2+ |
121 (91%) 12 (9%) |
|
| ||
| Lateral compartment articular cartilage status | Grade 0–1 Grade 2+ |
111 (83%) 22 (17%) |
|
| ||
| Patellofemoral compartment articular cartilage status | Grade 0–1 Grade 2+ |
124 (93%) 9 (7%) |
|
| ||
| Additional ipsilateral surgery (non-ACL surgery) | No | 108 (81%) |
| Yes | 25 (19%) | |
| Surgery for arthrofibrosisb | 14/25 (56%)c | |
| Partial meniscectomy | 11/25 (44%)c | |
| Removal tibial hardware | 2/25 (8%)c | |
| Chondroplasty | 2/25 (8%)c | |
| Microfracture | 1/25 (4%)c | |
| Removal loose body | 1/25 (4%)c | |
|
| ||
| Additional contralateral surgery (non-ACL surgery) | No Yes |
133 (100%) 0 (0%) |
Key: ACL= anterior cruciate ligament; BTB=bone-patellar tendon-bone; Grade = modified Outerbridge articular cartilage grade
Reported values are for the 133/146 subjects with bilateral radiographs at 10 years follow-up who did not undergo revision ipsilateral ACL surgery or contralateral primary ACL surgery.
Surgery for arthrofibrosis included arthroscopic anterior debridement, synovectomy, and/or manipulation under anesthesia.
Percentages equal greater than 100% as one or more procedures couple be performed at time of repeat non-ACL surgery
Among blinded reviewers, inter-rater reliability varied among scoring systems. The inter-rater reliability of the IKDC scoring system was substantial (Gwet’s AC1 = 0.71), the modified KL scoring system was moderate (AC1 = 0.48), and the OARSI scoring system was almost perfect (AC1 = 0.83) (Table 2).
Table 2.
Inter-rater reliabilty of knee osteoarthritis scoring systems
| Scoring System | Gwet’s AC1 (95% confidence interval)* |
|---|---|
| IKDC grade | 0.71 (0.65–0.77) |
| Modified Kellgren Lawrence (KL) grade | 0.48 (0.41–0.55) |
| OARSI grade (all criteria) | 0.84 (0.82–0.86) |
| Medial joint space narrowing | 0.78 (0.72–0.83) |
| Lateral joint space narrowing | 0.91 (0.88–0.95) |
| Medial femoral osteophyte | 0.94 (0.91–0.97) |
| Lateral femoral osteophyte | 0.77 (0.73–0.84) |
| Medial tibial osteophyte | 0.77 (0.72–0.83) |
| Lateral tibial osteophyte | 0.84 (0.79–0.88) |
Landis and Koch20 suggest the following benchmark scale for interpreting inter-rater agreement: <0.00 poor; 0.00–0.20 slight; 0.21–0.40 fair; 0.41–0.60 moderate; 0.61–0.80 substantial; 0.81–1.00 almost perfect.
Incidence of radiographic osteoarthritis
The 10-year incidence of PTOA in the ACLR knee with no radiographic evidence of OA in the contralateral ACL-intact knee is 37% as defined by osteophytes and 23% as defined by joint space narrowing (Table 3). In the ACLR knee the incidence of PTOA at 10 years following surgery was 43% for OA defined by definite osteophytes and 27% for OA defined by joint space narrowing. In the contralateral, non-ACL injured knee, the incidence of OA was 10% as defined by osteophytes and 5% as defined by joint space narrowing.
Table 3.
Incidence of radiographic osteoarthritis
| OA definition | ACL reconstructed knee | Contralateral knee | Present in ACL reconstructed knee and absent in contralateral knee |
|---|---|---|---|
| Definite osteophytes* | 43% (57/133) | 10% (13/133) | 37% (44/120) |
| Joint space narrowing** | 27% (35/133) | 5% (7/133) | 23% (29/126) |
Definite osteophytes defined as KL grade 2 or higher, IKDC grade B or higher, and OARSI osteophyte grade 1 or higher (any compartment)
Joint space narrowing defined as OARSI grade 1 narrowing or higher in any compartment.
Radiographic osteoarthritis severity
According to IKDC grading criteria, 57% of ACLR knees were normal (IKDC A) and 35% had mild changes (IKDC B) with few (8%) having higher grade changes (IKDC C or D) (Table 4). In the contralateral knee, 90% were normal (IKDC A) with mild changes in 8% (IKDC B) and moderate in 2% (IKDC C). The ACLR knee was normal or near normal according to modified KL criteria in 57% (grades 0 or 1), had mild OA changes in 35% (grade 2), and moderate changes in 6% (grade 3) and severe in 2% (grade 4). The contralateral knee was modified KL grade 0–1 in 87%, grade 2 in 8%, grade 3 in 2% and grade 4 in 0% of cases. According to OARSI criteria, there was grade 1 or less joint space narrowing in 85% in either compartment of ACLR knees, grade 2 narrowing in 3% and grade 2 narrowing in 2%; the contralateral knee had OARSI grade 0–1 narrowing in 99% of cases and grade 2 narrowing in 1%. For the OARSI osteophyte grade, 83% of ACLR knees had a maximum grade (tibial grade plus femoral grade) of 0–1 in either compartment, 13% had a maximum grade of 2, and 4% had a grade of 3 or higher. In the contralateral knee, 94% had a maximum OARSI osteophyte grade 0–1, and 6% had a grade of 2 or higher. Similar distributions were observed for the medial and lateral compartment-specific OARSI joint space narrowing and osteophyte grades (Supplement 1).
Table 4.
Radiographic osteoarthritis severity
| ACL reconstructed knee | Contralateral knee | |
|---|---|---|
| IKDC grade A B C D |
76 (57%) 47 (35%) 8 (6%) 2 (2%) |
120 (90%) 11 (8%) 2 (2%) 0 (0%) |
| Modified KL grade 0 1 2 3 4 |
47 (36%) 29 (21%) 47 (35%) 8 (6%) 2 (2%) |
102 (77%) 18 (14%) 11 (8%) 2 (2%) 0 (0%) |
| OARSI maximum JSN grade, medial and lateral compartments 0 1 2 3 |
98 (73%) 29 (22%) 4 (3%) 2 (2%) |
126 (94%) 6 (5%) 1 (1%) 0 (0%) |
| OARSI maximum osteophyte grade (tibial + femoral osteophyte grade), medial and lateral compartments 0 1 2 3+ |
76 (57%) 34 (26%) 17 (13%) 6 (4%) |
120 (90%) 5 (4%) 6 (5%) 2 (1%) |
Key: Reported as number (percentage)
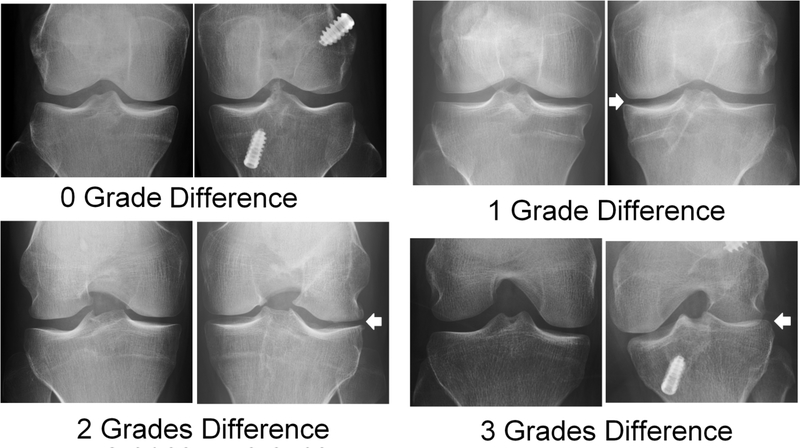
Side-to-side difference in osteoarthritis severity
When comparing the ACLR knee to the contralateral knee, 94% of patients had 1 grade or less difference in IKDC radiographic OA grade, 5% had 2 grades difference, and 1% had 3 grades difference (Table 5). When utilizing the modified KL grading system, 73% had 1 grade or less difference, 23% had 2 grades difference, and 4% had 3–4 grades difference. The maximum difference in OARSI joint space narrowing grade (medial or lateral compartment) between knees was 1 grade or less in 96% of patients, 2 grades in 3%, and 3 grades in 1% (Figure 4). The maximum difference in osteophyte grade (femoral + tibial grade) for either medial or lateral compartment was 1 grade or less in 85% of patients, 2 grades in 12% and 3 or more grades in 3% of patients (Figure 5). Similar distributions were observed when comparing medial and lateral compartment-specific OARSI joint space narrowing and osteophyte grades between knees (Supplement 2).
Table 5.
Side-to-side difference in OA findings
| Number (percentage) | |
|---|---|
| IKDC grade difference 0 grades 1 grade 2 grades 3 grades |
87 (65%) 38 (29%) 7 (5%) 1 (1%) |
| Kellgren-Lawrence grade difference 0 grades 1 grade 2 grades 3 grades 4 grades |
64 (48%) 33 (25%) 31 (23%) 4 (3%) 1 (1%) |
| OARSI maximum difference JSN grade, medial and lateral compartments 0 grades 1 grade 2 grades 3 grades |
102 (77%) 26 (19%) 4 (3%) 1 (1%) |
| OARSI maximum difference osteophyte grade (femoral + tibial osteophyte grade), medial and lateral compartments 0 grades 1 grade 2 grades 3+ grades |
86 (65%) 27 (20%) 16 (12%) 4 (3%) |
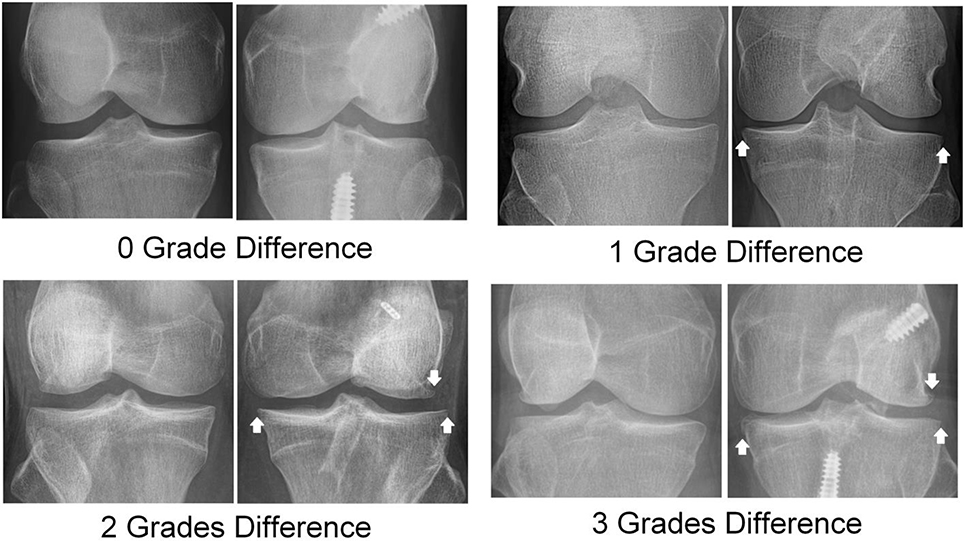
Figure 4.
Representative examples of maximum side to side differences in OARSI joint space narrowing (JSN) grade in either the medial or lateral tibiofemoral compartment at 10 years after unilateral ACL reconstruction. Joint space narrowing is indicated by the white arrows.
Figure 5.
Representative examples of maximum side to side differences in OARSI osteophyte grade (tibial grade plus femoral grade) in either the medial or lateral tibiofemoral compartment at 10 years after unilateral ACL reconstruction. Tibial and femoral marginal osteophytes are indicated by the white arrows. Femoral notch and tibial intercondylar eminence osteophytes are not considered in OARSI osteophyte grading.
Discussion
The estimated risk of PTOA after ACL injury varies dramatically in the literature22, which has limited the ability of clinicians to effectively counsel young ACL injured athletes on the long term risk of clinical radiographic PTOA after ACLR. The purpose of this prospective multicenter study was therefore to estimate the incidence of PTOA within a clinically acceptable degree of certainty at 10 years after ACLR in a carefully selected cohort of young, athletic patient population with a highly reproducible radiographic protocol. The incidence of PTOA depends on the preferred definition of OA, which varies among clinicians and researchers. Therefore, we have reported estimates of the 10-year incidence of clinical radiographic PTOA following ACLR using an osteophyte-based definition of OA (37%) and a joint space narrowing-based definition of OA (23%) among patients with a contralateral ACL-intact and radiographically normal knee. Finally, the current study demonstrates that side-to-side differences in radiographic OA changes are small in the majority of patients, with 96% having 1 grade or less difference in OARSI joint space narrowing grade and 85% having 1 grade or less difference in OARSI osteophyte grade (Table 5).
Multiple clinical radiographic grading scales and definitions of OA were utilized in the current study, as one of the challenges in interpreting the existing literature on radiographic PTOA at long term follow-up after ACLR is use of varying definitions of OA and differing radiographic OA grading scales. An advantage of the OARSI scale is that it allows for separate grading of individual pathologic OA features, which resulted in excellent inter-rater reliability in the current study. Though both the IKDC and KL grading scales mix several pathologic changes in a single scale (a potential source of ambiguity when assigning a grade), the IKDC scale had superior inter-rater reliability than KL which is consistent with a prior reliability study of ACLR knees.34 A meta-analysis by Claes et al. reported a 28% prevalence of PTOA at 10 years after ACLR as defined by IKDC C or D radiographic changes.7 In contrast, 8% of ACLR knees in the current study had IKDC C or D changes. The greater OA proportion reported in the meta-analysis may be secondary to inclusion of cases performed between 1978–1997 (with potential inclusion of outdated surgical techniques and rehabilitation protocols), inclusion of older patients, and inclusion of retrospective studies with the inherent bias of a retrospective design.7
The current study demonstrates a lower incidence of radiographic OA in the contralateral knee which is consistent with prior long-term follow-up studies with bilateral knee radiographic assessments.3,21,25 In a mean 14-year follow-up study of patients randomized to hamstring or bone-patellar tendon-bone (BTB) autograft ACLR, the incidence of OA was 57% (as defined by KL grade 2+) in the reconstructed knee and 18% in the contralateral knee with no difference between graft types.3 Murray found a 33% prevalence of PTOA (as defined by IKDC grades C or D) in the ACLR knee and a 7% prevalence in the contralateral knee at mean 13 years following ACLR with BTB autograft in a series of 114 patients.25 In a retrospective study of 249 patients with mean 7.9 years follow-up, Li et al. report 39% of ACLR knees had a higher KL grade than the contralateral uninjured knee.21 However, the current study expands upon the existing literature as our results indicate the magnitude difference in osteophyte formation and joint space narrowing between the ACLR and contralateral knee is often small; risk factors for high grade side-to-side differences are unclear as a larger sample will be required to perform an appropriate analysis.
Many of the patients in the current study with PTOA had only mild radiographic changes. The patients in the current study had no history of prior knee injury and sustained an ACL injury during sporting activity; the higher degree of radiologic OA changes reported in some other long-term follow-up studies may in part be due to inclusion of patients with previous knee injuries and potentially higher energy injuries.22,31 It is unclear whether patients with early radiographic changes at 10 years are at risk for clinically significant PTOA at 20 years. Progression is likely to occur in the second decade after ACLR; a prospective study comparing 15 and 20 year follow-up radiographs demonstrated a 42% prevalence of tibiofemoral OA (per KL criteria) at 20 years and a 13% increase in prevalence from years 15 to 20.28 Repeat assessment of our enrolled patients may be warranted at 20 years follow-up, particularly as the radiographic technique utilized has high demonstrated reproducibility6,19 and sensitivity to change in joint space narrowing with longitudinal assessment.26
The current study has several limitations. This is a large ongoing nested cohort study, and though the current interim analysis was adequately powered to determine the incidence of PTOA within a clinically acceptable margin of error, not all patients within the window for a minimum 10-year visit have followed up, which potentially introduces selection bias. The study only included primary ACL reconstructions and do not apply to revision ACL reconstructions. Patients were not enrolled into the nested cohort until 2 years after ACLR, and the standardized bilateral MTP radiographic views obtained at 10 years in the nested cohort were not obtained pre-operatively. Potential risk factors for PTOA at 10 years after ACLR, including graft choice, BMI, post-operative sports participation, and meniscus and cartilage status and treatment, cannot be determined in this interim analysis; this will require follow-up of the majority of the nested cohort study to have adequate power for a multivariable analysis. Specifically, the larger cohort will be needed to determine the effect of meniscus or cartilage status at the time of ACLR or the effect of subsequent meniscus or cartilage-related surgery on risk of PTOA at 10 years. Similarly, follow-up of the majority of the nested cohort will be required to effectively assess the strength of association between radiographic findings of PTOA and knee symptom severity in young patients after ACLR. The side-to-side differences in joint space narrowing and osteophyte formation between the ACLR and contralateral knees at 10 years are small, and it is apparent that repeat imaging at 20 years follow-up will be necessary to determine whether these initial radiographic changes are a precursor for more severe and clinically significant changes at 20 years. The inter-rater reliability of the KL grading system in the current study was relatively low; this is a known issue with the KL grading system and is likely due to qualitative assessment of joint space narrowing and inclusion of multiple pathologic changes on a single scale.15 Finally, though standardized weight bearing radiographs were used in the current analysis, the current study could not assess for OA-related changes detectable on magnetic resonance imaging such as cartilage degeneration or bone marrow edema that may precede radiographic evidence of OA.11,29
Conclusion
The 10 year incidence of clinical radiographic PTOA after ACL reconstruction in a young athlete with a radiographically normal contralateral knee is 37% as defined by osteophytes and 23% as defined by joint space narrowing. The contralateral ACL-uninjured knee has a 10-year incidence of osteophyte-defined OA of 10% and joint space narrowing-defined OA of 6%. The difference in degree of osteophyte formation and joint space narrowing between the ACLR knee and contralateral knee was small in the majority of these patients, as 85% had ≤1 point side-to side difference in medial and lateral compartment osteophyte grades, while 96% had ≤1 point difference in medial and lateral joint space narrowing grades.
Supplementary Material
What is known about the subject:
Post-traumatic osteoarthritis occurs after ACL reconstruction, though estimates of the incidence and severity of PTOA at 10 years vary widely and often fail to consider the status of the contralateral knee.
What this study adds to existing knowledge:
The 10 year incidence of clinical radiographic PTOA after ACL reconstruction in a young athlete with a radiographically normal contralateral knee is 37% as defined by osteophytes and 23% as defined by joint space narrowing. The average difference in degree of osteophyte formation and joint space narrowing between the ACL reconstructed knee and contralateral ACL-intact knee is small.
Contributor Information
MOON Knee Group:
Josh S. Everhart, Morgan H. Jones, Sercan Yalcin, Emily K. Reinke, Laura J. Huston, Jack T. Andrish, Charles L. Cox, David C. Flanigan, Christopher C. Kaeding, Nancy Obuchowski, Richard D. Parker, Angela D. Pedroza, Rosemary A. Sanders, Carl S. Winalski, and Kurt P. Spindler
References
- 1.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007;15Suppl A:A1–56. [DOI] [PubMed] [Google Scholar]
- 2.Amis AA. The functions of the fibre bundles of the anterior cruciate ligament in anterior drawer, rotational laxity and the pivot shift. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):613–620. [DOI] [PubMed] [Google Scholar]
- 3.Barenius B, Ponzer S, Shalabi A, et al. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. The American journal of sports medicine. 2014;42(5):1049–1057. [DOI] [PubMed] [Google Scholar]
- 4.Buckland-Wright JC, Lynch JA, Dave B. Early radiographic features in patients with anterior cruciate ligament rupture. Ann Rheum Dis. 2000;59(8):641–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buckland-Wright JC, Ward RJ, Peterfy C, Mojcik CF, Leff RL. Reproducibility of the semiflexed (metatarsophalangeal) radiographic knee position and automated measurements of medial tibiofemoral joint space width in a multicenter clinical trial of knee osteoarthritis. J Rheumatol. 2004;31(8):1588–1597. [PubMed] [Google Scholar]
- 6.Buckland-Wright JC, Wolfe F, Ward RJ, Flowers N, Hayne C. Substantial superiority of semiflexed (MTP) views in knee osteoarthritis: a comparative radiographic study, without fluoroscopy, of standing extended, semiflexed (MTP), and schuss views. J Rheumatol. 1999;26(12):2664–2674. [PubMed] [Google Scholar]
- 7.Claes S, Hermie L, Verdonk R, Bellemans J, Verdonk P. Is osteoarthritis an inevitable consequence of anterior cruciate ligament reconstruction? A meta-analysis. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2013;21(9):1967–1976. [DOI] [PubMed] [Google Scholar]
- 8.Culvenor AG, Engen CN, Øiestad BE, Engebretsen L, Risberg MA. Defining the presence of radiographic knee osteoarthritis: a comparison between the Kellgren and Lawrence system and OARSI atlas criteria. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3532–3539. [DOI] [PubMed] [Google Scholar]
- 9.Duryea J, Li J, Peterfy CG, Gordon C, Genant HK. Trainable rule-based algorithm for the measurement of joint space width in digital radiographic images of the knee. Med Phys. 2000;27(3):580–591. [DOI] [PubMed] [Google Scholar]
- 10.Felson DT, McAlindon TE, Anderson JJ, et al. Defining radiographic osteoarthritis for the whole knee. Osteoarthritis Cartilage. 1997;5(4):241–250. [DOI] [PubMed] [Google Scholar]
- 11.Guermazi A, Eckstein F, Hayashi D, et al. Baseline radiographic osteoarthritis and semi-quantitatively assessed meniscal damage and extrusion and cartilage damage on MRI is related to quantitatively defined cartilage thickness loss in knee osteoarthritis: the Multicenter Osteoarthritis Study. Osteoarthritis Cartilage. 2015;23(12):2191–2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gwet KL. Computing inter-rater reliability and its variance in the presence of high agreement. Br J Math Stat Psychol. 2008;61(Pt 1):29–48. [DOI] [PubMed] [Google Scholar]
- 13.Gwet KL. Handbook of inter-rater reliability: The definitive guide to measuring the extent of agreement among raters. Advanced Analytics, LLC; 2014. [Google Scholar]
- 14.Hefti F, Müller W, Jakob RP, Stäubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3–4):226–234. [DOI] [PubMed] [Google Scholar]
- 15.Hunter DJ, Le Graverand MP, Eckstein F. Radiologic markers of osteoarthritis progression. Curr Opin Rheumatol. 2009;21(2):110–117. [DOI] [PubMed] [Google Scholar]
- 16.Jones MH, Spindler KP, Andrish JT, et al. Differences in the Lateral Compartment Joint Space Width After Anterior Cruciate Ligament Reconstruction: Data From the MOON Onsite Cohort. Am J Sports Med. 2018;46(4):876–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jones MH, Spindler KP, Fleming BC, et al. Meniscus treatment and age associated with narrower radiographic joint space width 2–3 years after ACL reconstruction: data from the MOON onsite cohort. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2015;23(4):581–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kothari M, Guermazi A, von Ingersleben G, et al. Fixed-flexion radiography of the knee provides reproducible joint space width measurements in osteoarthritis. Eur Radiol. 2004;14(9):1568–1573. [DOI] [PubMed] [Google Scholar]
- 20.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 21.Li RT, Lorenz S, Xu Y, et al. Predictors of radiographic knee osteoarthritis after anterior cruciate ligament reconstruction. The American journal of sports medicine. 2011;39(12):2595–2603. [DOI] [PubMed] [Google Scholar]
- 22.Lie MM, Risberg MA, Storheim K, Engebretsen L, Øiestad BE. What’s the rate of knee osteoarthritis 10 years after anterior cruciate ligament injury? An updated systematic review. Br J Sports Med. 2019;53(18):1162–1167. [DOI] [PubMed] [Google Scholar]
- 23.Marx RG, Connor J, Lyman S, et al. Multirater agreement of arthroscopic grading of knee articular cartilage. Am J Sports Med. 2005;33(11):1654–1657. [DOI] [PubMed] [Google Scholar]
- 24.Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. The American journal of sports medicine. 2001;29(2):213–218. [DOI] [PubMed] [Google Scholar]
- 25.Murray JR, Lindh AM, Hogan NA, et al. Does anterior cruciate ligament reconstruction lead to degenerative disease?: Thirteen-year results after bone-patellar tendon-bone autograft. Am J Sports Med. 2012;40(2):404–413. [DOI] [PubMed] [Google Scholar]
- 26.Nevitt MC, Peterfy C, Guermazi A, et al. Longitudinal performance evaluation and validation of fixed-flexion radiography of the knee for detection of joint space loss. Arthritis Rheum. 2007;56(5):1512–1520. [DOI] [PubMed] [Google Scholar]
- 27.Outerbridge RE. The etiology of chondromalacia patellae. The Journal of bone and joint surgery British volume. 1961;43-b:752–757. [DOI] [PubMed] [Google Scholar]
- 28.Risberg MA, Oiestad BE, Gunderson R, et al. Changes in Knee Osteoarthritis, Symptoms, and Function After Anterior Cruciate Ligament Reconstruction: A 20-Year Prospective Follow-up Study. The American journal of sports medicine. 2016;44(5):1215–1224. [DOI] [PubMed] [Google Scholar]
- 29.Roemer FW, Kwoh CK, Hannon MJ, et al. What comes first? Multitissue involvement leading to radiographic osteoarthritis: magnetic resonance imaging-based trajectory analysis over four years in the osteoarthritis initiative. Arthritis Rheumatol. 2015;67(8):2085–2096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schiphof D, Boers M, Bierma-Zeinstra SM. Differences in descriptions of Kellgren and Lawrence grades of knee osteoarthritis. Ann Rheum Dis. 2008;67(7):1034–1036. [DOI] [PubMed] [Google Scholar]
- 31.van Meer BL, Meuffels DE, van Eijsden WA, et al. Which determinants predict tibiofemoral and patellofemoral osteoarthritis after anterior cruciate ligament injury? A systematic review. British journal of sports medicine. 2015;49(15):975–983. [DOI] [PubMed] [Google Scholar]
- 32.Wolf BR, Ramme AJ, Wright RW, et al. Variability in ACL tunnel placement: observational clinical study of surgeon ACL tunnel variability. Am J Sports Med. 2013;41(6):1265–1273. [DOI] [PubMed] [Google Scholar]
- 33.Wongpakaran N, Wongpakaran T, Wedding D, Gwet KL. A comparison of Cohen’s Kappa and Gwet’s AC1 when calculating inter-rater reliability coefficients: a study conducted with personality disorder samples. BMC Med Res Methodol. 2013;13:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wright RW, Group M. Osteoarthritis Classification Scales: Interobserver Reliability and Arthroscopic Correlation. J Bone Joint Surg Am. 2014;96(14):1145–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wright RW, Haas AK, Anderson J, et al. Anterior Cruciate Ligament Reconstruction Rehabilitation: MOON Guidelines. Sports health. 2015;7(3):239–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Øiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37(7):1434–1443. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.