Abstract
Purpose:
Previous research has indicated that patients with anorexia nervosa (AN) or atypical AN with premorbid history of overweight/obesity have greater weight loss and longer illness duration than patients with no such history. However, little is known about the association of premorbid overweight/obesity and receiving inpatient medical care during treatment for an eating disorder.
Methods:
Using logistic regression, we sought to determine if history of overweight/obesity was associated with receiving inpatient medical care in a sample of 522 patients (mean age 15.5 years, 88% female) with AN/atypical AN.
Results:
Binary results demonstrated greater percent weight loss (27.4% vs. 16.2%) and higher percent median body mass index (%mBMI, 99.8% vs. 85.2%) at presentation in those with a history of overweight/obesity (p < .001) but no difference in duration of illness (p = .09). In models adjusted for demographics and percent weight loss, history of overweight/obesity was associated with lower odds of receiving inpatient medical care (odds ratio .60 [95% confidence interval: .45–.80]) at 1-year follow-up. However, these associations were no longer significant after adjusting for %mBMI. Mediation results suggest that %mBMI fully mediates the relationship between history of overweight/obesity and inpatient medical care, in that those with a history of overweight/obesity are less likely to receive care due to presenting at a higher weight.
Conclusions:
Our findings suggest that, despite greater degree of weight loss and no difference in duration of illness, participants with a history of overweight/obesity are less likely to receive inpatient medical care.
Keywords: Anorexia nervosa, Atypical anorexia nervosa, Adolescents, Overweight, Obesity, Percent weight loss, Percent median body mass index, Inpatient medical care, Eating disorder
Although child/adolescent obesity and its comorbidities have been the focus of much public health scrutiny for the last decade, its overlap with eating disorder behaviors and diagnoses remains understudied. In fact, adolescents with overweight/obesity have an elevated risk for weight and shape concerns compared with their normal weight peers [1] and are equally at risk for engaging in extreme weight control practices and disordered eating, such as purging, binge eating, and laxative and diet pill use [2]. Given these risks, there is need for research to better understand how premorbid overweight/obesity status (i.e., a history of overweight or obesity) in adolescent patients with anorexia nervosa (AN) or atypical AN (AAN) may affect the course of illness and treatment. Studies show that 11%–36% of adolescent patients with AN or eating disorder not otherwise specified with dietary restriction (EDNOS-DR) have a history of overweight/obesity and that this rate is rising [3,4]. In addition, Lebow et al. [3] found that patients with AN or EDNOS-DR and a history of overweight/obesity had longer duration of illness, greater percent weight loss, and a higher body mass index (BMI) at intake compared with those who started in the normal weight range. These findings are particularly worrisome because longer duration of illness and higher percent weight loss have both been found to be predictive of poorer medical and psychological outcomes [5–7]. Thus, there is a critical need for studies that specifically examine the influence of premorbid overweight/obesity on the course and treatment of adolescents with AN/AAN.
To address this gap in knowledge, we used patient data from the National Eating Disorders Quality Improvement Collaborative (NEDQIC), a multisite collaborative of adolescent medicine programs that treat patients with eating disorders. Specifically, we set out to (1) examine differences in clinical markers of severity of illness (e.g., duration of illness and percent weight loss) in adolescent patients with AN and AAN by history of overweight/obesity and (2) investigate the association of premorbid overweight/obesity and likelihood of receiving inpatient medical care over 1-year follow-up. Based on prior studies, we hypothesized that patients with a history of overweight/obesity would have worse clinical markers of severity of illness than those with no history of overweight/obesity, including having had a longer duration of illness and greater weight loss at intake to an eating disorder program. We also hypothesized that despite having greater percent weight loss, patients with a history of overweight/obesity would present with a higher percent median BMI (%mBMI). Finally, we hypothesized that patients with AN/AAN and a history of overweight/obesity would be more likely to require intensive medical care during 1-year follow-up than those without a history of overweight/obesity.
Method
Sample
The NEDQIC is a multisite quality improvement collaborative of adolescent medicine–based eating disorder programs, with past studies exploring predictors of weight outcomes in adolescent patients with eating disorders [8–10]. As part of the NEDQIC, 14 eating disorder programs took part in a retrospective chart review of patients presenting to their clinics in the calendar year 2010. Patients’ charts were reviewed at intake and at 1-year follow-up. One-year follow-up was defined as the visit between 9 and 15 months after the intake visit that was closest to 1 year. Participants meeting criteria for AN or AAN per DSM-5 criteria were included in the chart review. Chart review was performed by each site and combined into a database by the lead site (Boston Children’s Hospital). While geographically diverse, all sites had medical providers specializing in adolescent medicine working with a multidisciplinary team. However, levels of care available varied by site. Diagnoses were retroactively assigned by a local eating disorder expert based on DSM-5 criteria for AN and AAN [9]. The institutional review board approval was obtained at each site involved in data collection. A Health Insurance Portability and Accountability Act data sharing agreement was signed between each site and the lead site.
Measures
Chart review was performed and coded by each site using a 90-item data collection form previously published in the literature [9]. All programs provided information about participants at intake, including participants’ sex, age, race/ethnicity, eating disorder diagnosis, BMI (kg/m2), %mBMI, duration of illness, height, and highest self-reported weight. Sites also provided information at 1-year follow-up including height, weight, and type of eating disorder treatment received over the past year. Duration of illness was reported at intake by either the parent or patient and was defined as the amount of time eating disorder symptoms had been present. Percent weight loss was calculated by subtracting weight at intake from reported highest weight ever, dividing by highest weight ever, and multiplying by 100. Eating disorder–related treatment received during the last year was divided into two categories: medically specified care (inpatient medical and/or joint inpatient medical/psychiatric) and all other treatments including, inpatient psychiatric hospitalization, day treatment program/partial hospitalization, intensive outpatient program, psychotherapy, taking psycho-pharmacologic medications, family-based therapy, adolescent-focused individual therapy, nutritional therapy, and outpatient adolescent medical care [9]. Participants who received both inpatient medical care and other care were categorized as receiving inpatient medical care.
Data analysis
Participants’ intake BMI, age, and sex were used to calculate BMI percentile for age and sex according to Centers for Disease Control and Prevention growth charts [11]. Reported highest weight and intake height, age, and sex were used to calculate the highest BMI percentile that individual patients had ever reached. Two groups were created based on this highest BMI percentile. BMIs which were at or above the 85th percentile for age and sex [11] or ≥25 kg/m2 for participants aged 18 years or older were categorized as having a history of overweight/obesity, meaning that their highest weight was above the normal range [12]. Participants with BMI below the 85th and above the fifth percentile or those with BMI <25 and ≥18.5 kg/m2 if 18 years or older were categorized as having no history of overweight/obesity. A small number of participants (n = 18) had a highest weight in the underweight range (BMI percentile <5 or BMI <18.5 kg/m2 if over 18 years). Owing to the small sample size and aim of analyses, these participants were excluded. Participants were categorized as missing (n = 72) if they had missing or incomplete weight history data. The final sample consisted of 522 participants.
To address aim 1, participants with a history of overweight/obesity were compared to those with no history of overweight/obesity on duration of illness and %mBMI using Mann-Whitney U tests and on percent weight loss at intake using an independent t test. Participants were further compared on eating disorder diagnosis, sex, race/ethnicity, and treatment received at 1-year follow-up using chi-square tests. To address aim 2, we performed a series of logistic regression models with history of overweight/obesity as the primary predictor and inpatient medical care as the outcome. Given that data came from 14 outpatient sites that differed in availability of care as well as potential differences in criteria for referral to inpatient care, analyses were controlled for clustering in the data. In model 1, history of overweight/obesity was entered adjusting for age, sex, and race/ethnicity. Model 2 further adjusted for percent weight loss and model 3 for %mBMI at presentation. While diagnosis was also significantly correlated with history of overweight/obesity in bivariate correlations, it was not included as a predictor of care as it was significantly correlated with %mBMI (at r = .60) with potential for collinearity.
We also performed a mediation analysis testing the hypothesis that weight at presentation (i.e., %mBMI) may mediate the relationship between history of overweight/obesity and receiving inpatient medical care given the focus on weight for admission [13,14]. To establish mediation, we followed the four steps proposed by Baron and Kenny [15]. We also calculated the indirect effect of history of overweight/obesity through %mBMI on inpatient medical care using the delta method in MPLUS 7.4 (Muthén & Muthén, Los Angeles, CA) [16,17].
Finally, as a sensitivity analysis, we performed tests to assess the difference between patients who had a highest weight ever and those who were missing weight history data. Patients with missing data did not differ from those with a reported highest weight by sex, diagnosis, %mBMI, or duration of illness; however, they were younger (p < .001) than those with a reported highest weight. Regression analyses were performed using Mplus version 7, and bivariate analyses were performed using IBM Statistical Package for Social Sciences, version 23 (IBM Corp., Armonk, NY).
Results
Table 1 shows clinical characteristics by the presence or absence of overweight/obesity history. Bivariate results reveal that at intake, participants with a history of overweight/obesity had significantly greater percent weight loss and higher %mBMI than those with no history of overweight/obesity (p < .001). Participants who were males (30.2% males vs. 17.9% females; p = .02) and nonwhite (26.8% nonwhite vs. 17.6% white; p = .04) were more likely to have a history of overweight/obesity. In addition, participants with a history of overweight/obesity were more likely to have an AAN diagnosis (66.3% AAN vs. 33% AN; p < .001). There was no statistically significant difference between weight history groups on duration of illness (p = .09); participants with a history of overweight/obesity were ill, on average, for 16.2 months, compared with 13.7 months for those without. Similarly, there were no statistical differences between weight groups on level of care received at 1-year follow-up, with 25.7% of those with a history of overweight/obesity receiving inpatient medical care compared to 26.6% of those without history of overweight/obesity (p = .86). Finally, of note, among the 101 participants with a history of overweight/obesity, 7.9% (n = 8) were still overweight/obese at intake.
Table 1.
Descriptive statistics for participants with AN or AAN at eating disorder treatment intake according to weight history
| Entire population (N = 522), n (%) | History of normal weight (n = 421) | History of overweight/obesity (n = 101) | p valuea | |
|---|---|---|---|---|
| Gender | ||||
| Female | 459 (87.9) | 377 (89.5) | 82 (81.2) | .03 |
| Male | 63 (12.1) | 44 (10.5) | 19 (18.8) | |
| Race/ethnicity | ||||
| White | 425 (81.4) | 350 (83.1) | 75 (74.3) | .04 |
| Nonwhite | 97 (18.6) | 71 (16.9) | 26 (25.7) | |
| Diagnosis | ||||
| AN | 316 (60.5) | 282 (67.0) | 34 (33.7) | <.001 |
| AAN | 206 (39.5) | 139 (33.0) | 67 (66.3) | |
| Mean (±SD) | ||||
| Age in years | 15.6 (2.3) | 15.7 (2.3) | 15.3 (2.3) | .07 |
| Duration of illness in months | 14.2 (16.9) | 13.7 (15.7) | 16.2 (21.0) | .09 |
| %mBMI | 88.1 (11.5) | 85.2 (9.2) | 99.8 (12.8) | <.001 |
| Percent weight loss | 18.4 (9.5) | 16.2 (7.9) | 27.4 (10.3) | <.001 |
| Comparison of care at 1-year follow-up; n (%) | ||||
| Inpatient medical care versus all other careb | ||||
| Inpatient medical care | 138 (26.4) | 112 (26.6) | 26 (25.7) | .86 |
| All other care | 384 (73.6) | 309 (73.4) | 75 (74.3) | |
AN = anorexia nervosa; AAN = atypical anorexia nervosa; %mBMI = percent median body mass index; SD = standard deviation.
Comparison between those with a history of overweight/obesity and those with a history of normal weight.
All other care = inpatient psychiatric hospitalization, day treatment program/partial hospitalization, intensive outpatient care, and outpatient care.
Table 2 contains results from regression models testing the association of overweight/obesity with receiving inpatient medical care at 1-year follow-up. In the initial logistic regression (model 1) adjusting for age, sex, and race/ethnicity, history of overweight/obesity did not predict inpatient medical care (p = .70, odds ratio [OR]: .95 [95% confidence interval {CI}: .56–1.52]). However, in model 2, after further adjustment for percent weight loss, history of overweight/obesity was associated with lower odds of receiving inpatient medical care (p < .001, OR: .60 [95% CI: .45–.80]). In model 3, adjusting for sex, age, race, percent weight loss, and %mBMI, history of overweight was no longer significantly associated with inpatient medical care; however, percent weight loss (p < .001, OR: 1.02 [95% CI: 1.01–1.03]) and %mBMI (p = .01, OR: .97 [95% CI: .95–.99]) were significantly associated with inpatient medical care. That is, in the final model, higher %mBMI was associated with lower odds of receiving inpatient medical care and greater percent weight loss was associated with higher odds of receiving care.
Table 2.
Logistic regression analysis predicting receiving inpatient medical care at 1-year follow-up: ORs (95% CI)
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Variables | |||
| Age | 1.00 (.94–1.06) | .96 (.93–1.04) | .98 (.93–1.04) |
| Sex | .96 (.94–1.43) | 1.02 (.73–1.57) | 1.10 (.74–1.60) |
| Race | 1.47 (.94–1.86) | 1.11 (.94–1.84) | 1.33 (.94–1.87) |
| History of overweight/obesity | .95 (.56–1.52) | .60** (.45–.80) | 1.06 (.67–1.68) |
| Percent weight loss | 1.04*** (1.02–1.06) | 1.02*** (1.01–1.03) | |
| %mBMI | .97* (.95–.99) |
p < .05;
p < .01;
p < .001.
CI = confidence interval; %mBMI = percent median body mass index; ORs = odds ratios.
We tested the hypothesis that %mBMI at intake may mediate the relationship between history of overweight/obesity and receiving inpatient medical care by 1-year follow-up (Figure 1). Our mediation hypothesis was supported. When adjusting for covariates, history of overweight/obesity was significantly related to both inpatient medical care (OR: .60, standard error [SE] = .15, p < .01, step 1) and %mBMI (β: .49, SE = .03, p < .001, step 2). In addition, %mBMI was significantly related to inpatient medical care (OR: .97, SE = .01, p < .01, step 3). To test for mediation, we entered history of overweight/obesity and %mBMI as predictors of inpatient medical care. The association between %mBMI and inpatient medical care remained significant, whereas the relationship between history of overweight/obesity and inpatient medical care was not significant (OR: 1.07, SE = .193, p = .71, step 4). Furthermore, the indirect effect of history of overweight/obesity through %mBMI on inpatient medical care was significant (OR: .65, SE = .21, p < .05), indicating full mediation.
Figure 1.
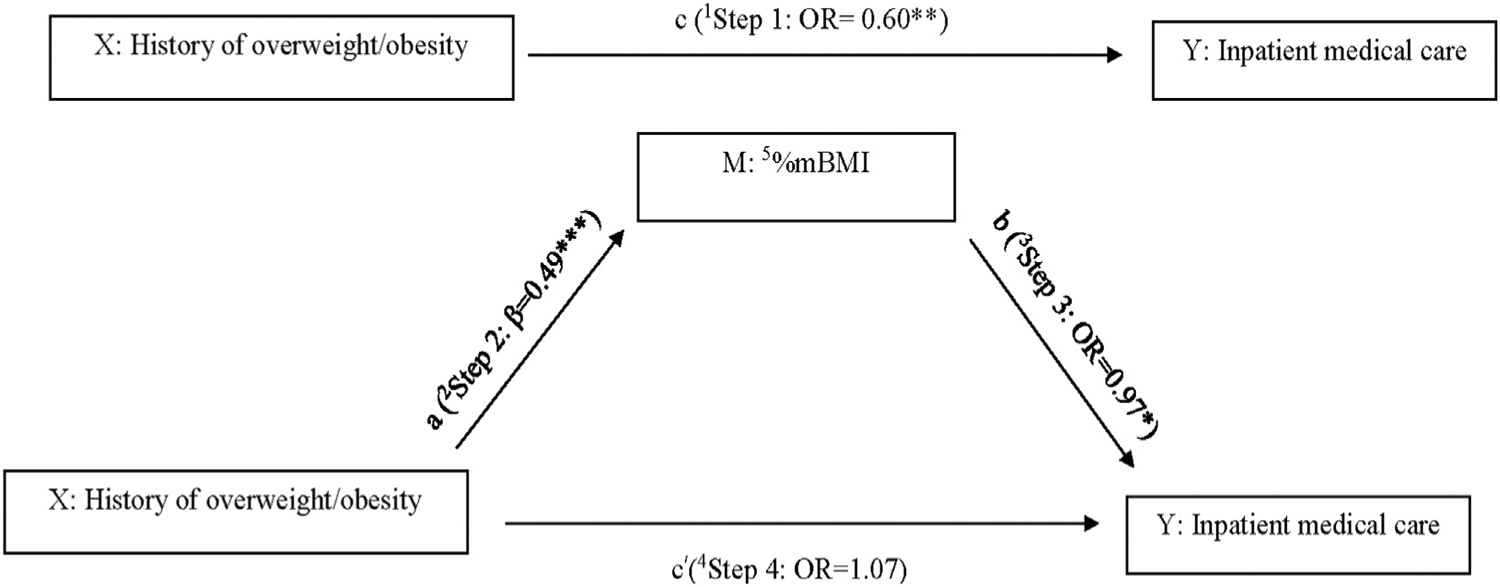
Mediation of association between history of overweight/obesity and inpatient medical care by %mBMI. 1Step 1: Significant association between history of overweight/obesity (predictor) and inpatient medical care (outcome). 2Step 2: Significant association between history of overweight/obesity (predictor) and %mBMI (mediator). 3Step 3: Significant association between %mBMI (mediator) and inpatient medical care (outcome). 4Step 4: Association between history of overweight/obesity (predictor) and inpatient medical care (outcome) no longer significant after adjusting for mediating variable, %mBMI indicating full mediation. 5%mBMI = percent median body mass index. *p < .05, **p < .01, ***p < .001.
Discussion
To our knowledge, this is the first study to investigate the association of premorbid history of overweight/obesity and intensity of eating disorder treatment received over 1-year follow-up in a cohort of patients with AN or AAN. Contrary to our hypotheses, we found that patients with a history of overweight/obesity were less than half as likely to receive inpatient medical care once we accounted for the percent of body weight they had lost. However, when we accounted for %mBMI, history of overweight/obesity was no longer associated with receiving inpatient medical care. Mediation analyses revealed that %mBMI fully mediated the relationship between history of overweight/obesity and inpatient medical care, meaning that those with a history of overweight/obesity were less likely to receive inpatient medical care due to presenting at a higher weight. Our findings highlight the persistent focus on weight status at presentation, rather than degree of weight loss, in clinical decision-making in eating disorder care.
The finding that percent weight loss is a unique indicator of inpatient medical care is in line with a recent position paper by the Society for Adolescent Health and Medicine, which highlighted the need to take into consideration not only %mBMI but also degree and rate of weight loss, when establishing level of malnutrition resulting from a restrictive eating disorder [13,14]. In our study, those patients with a history of overweight/obesity lost, on average, 27.5% of their body weight, which further supports this position. According to Peebles et al. [6], adolescent patients who lost more than 25% of their body weight through food restriction, but were not underweight at intake, presented to eating disorder care with more severe medical sequelae, such as bradycardia and orthostasis, than other patients with AN, bulimia nervosa (BN), or other subthreshold AN and BN diagnoses [6]. Furthermore, a study of adolescents and adults with AN found that patients who presented to treatment with greater weight loss relative to their highest weight and at a higher BMI had more severe psychological AN symptomatology at treatment discharge [5]. The authors posited that these patients were more likely to have been overweight or near-overweight before their eating disorder. Therefore, relying on % mBMI as the defining indicator for medical treatment of eating disorder care has the potential to miss those who may have severe psychological symptomatology and potentially significant medical sequelae.
While it is recommended that percent and rate of weight loss are considered when establishing malnutrition [13], approvals from insurance companies for more intensive treatments are often based on degree of malnutrition at intake; this is one potential explanation for those with a history of overweight/obesity being less likely to receive inpatient medical care [13,14] compared to those with no history of overweight/obesity. Furthermore, there was a greater proportion of males and nonwhite participants in those with a history of overweight/obesity than in those without. AN has historically been under-recognized in men and in racial/ethnic minorities [18], which has contributed to documented treatment disparities, with most treatment facilities being geared toward women [19] and individuals from minority groups being underdiagnosed and/or undertreated [20]. Given these disparities, it is possible that a history of overweight/obesity was associated with lower odds of inpatient medical care not only because of a high intake weight but also because of gender and race/ethnicity. Finally, an alternative explanation of the findings may be that participants who enter into care at a higher weight are able to be treated in outpatient care without needing to go into inpatient medical care. Indeed, in an article previously published by the NEDQIC, % mBMI was the only predictor of weight recovery regardless of the level of treatment received [9], thus indicating that for weight restoration, outpatient care may be appropriate for those with a higher intake weight. However, given that recovery from an eating disorder encompasses more than weight restoration, future research is needed to elucidate the medical and psychiatric outcomes of patients by weight history and level of care received.
Of note, our results were somewhat divergent from a similar study by Lebow et al. [3] who had found that participants with a history of overweight/obesity with AN or EDNOS-DR had a longer duration of illness [3] than those with a normal weight history at eating disorder treatment intake. In the present study, participants with a history of overweight/obesity also had a longer duration of illness; however, this difference was not statistically significant. This inconsistency requires further research, as length of illness is a marker for recovery, with early detection and treatment indicating a better outcome [7].
Strengths and limitations
Our findings contribute to the emerging body of literature on the intersection of overweight/obesity and restrictive eating disorders. Given the low prevalence rate of AN and AAN [19–21], the present study provides a large sample size to detect differences by weight history. In addition, while previous literature has focused on the intersection of overweight/obesity and binge eating disorder and BN [22–25], few studies have examined the association of overweight/obesity and AN or AAN. This study represents a critical step in understanding this understudied phenomenon of restrictive eating disorders in individuals with overweight or obesity.
There are a number of limitations in this retrospective study, most notably the way in which a history of overweight/obesity was established. In the present study, history of overweight/obesity was calculated using participants’ self-reported highest weight and current height and age; we used current height and age as participants were not asked timing of their highest ever weight nor their height at that time. While this is a limitation, it likely contributed to an underestimation of participants with a history of overweight/obesity. Indeed, the prevalence of a history of overweight/obesity was much higher (36% compared with 16.5% in the present study) in a similar sample in a study by Lebow et al. [3] which used growth charts to establish historical weight. Furthermore, we did not have information on other medical or psychological indicators of illness severity, such as electrolyte disturbances, cardiac dysrhythmia, or overevaluation of weight and shape concerns [13,26], thus limiting our ability to determine which patients met medical criteria for hospitalization. In addition, not all sites were able to offer the same types of care; however, we controlled for clustering in our data to account for these differences by site [9]. Finally, we used DSM-5 diagnoses in bivariate analyses; however, DSM-4 was in use when the data were collected. Thus, while our findings suggest that participants with a history of overweight/obesity are more likely to receive an AAN diagnosis, our findings should be interpreted with some caution. Given these limitations, future research should examine the ways in which other medical and psychological indicators may differ by weight history and how those may contribute to level of care received once in treatment. Finally, while the sample is representative of patients presenting to adolescent medicine–based eating disorder clinics, it is an entirely clinically based sample. This sample cannot be generalized to the community where adolescents may struggle simultaneously with concerns of overweight/obesity and restrictive eating disorders but have not yet or may never enter treatment.
Implications and contribution
AN and AAN are debilitating disorders, which are both mentally and medically harmful. It is imperative that these disorders are ideally prevented, but at least caught early, given their high mortality rate and effect on quality of life [26,27]. While historically a relationship between overweight/obesity and restrictive eating disorders has been minimally investigated, our study highlights the need for further research and awareness of this intersection. This is especially true for adolescents with overweight/obesity as these young people are often subjected to weight stigma and are encouraged by friends, family, and society to lose weight, often at any cost [28]. Our findings suggest the potential suboptimal treatment of individuals with a history of higher weights who develop restrictive eating disorders, thereby putting them at risk of poorer prognosis.
IMPLICATIONS AND CONTRIBUTION.
The present study found that the history of overweight/obesity in adolescent patients with anorexia nervosa or atypical anorexia nervosa was associated with lower odds of receiving inpatient medical care despite greater percentage weight lost and no difference in illness duration.
Acknowledgments
The authors thank Carly Milliren, M.P.H., for her guidance on data analysis.
Funding Sources
The study was supported in part by MCH/HRSA Leadership Education in Adolescent Health grants, T71MC0009 and T71MC00008, and the Program for Patient Safety and Quality at Boston Children’s Hospital.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to disclose.
References
- [1].Calzo JP, Sonneville KR, Haines J, et al. The development of associations among body mass index, body dissatisfaction, and weight and shape concern in adolescent boys and girls. J Adolesc Health 2012;51:517–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Neumark-Sztainer D, Wall M, Story M, Sherwood NE. Five-year longitudinal predictive factors for disordered eating in a population-based sample of overweight adolescents: Implications for prevention and treatment. Int J Eat Disord 2009;42:664–72. [DOI] [PubMed] [Google Scholar]
- [3].Lebow J, Sim LA, Kransdorf LN. Prevalence of a history of overweight and obesity in adolescents with restrictive eating disorders. J Adolesc Health 2015;56:19–24. [DOI] [PubMed] [Google Scholar]
- [4].Whitelaw M, Gilbertson H, Lee KJ, Sawyer SM. Restrictive eating disorders among adolescent inpatients. Pediatrics 2014;134:e758–64. [DOI] [PubMed] [Google Scholar]
- [5].Berner LA, Shaw JA, Witt AA, Lowe MR. The relation of weight suppression and body mass index to symptomatology and treatment response in anorexia nervosa. J Abnorm Psychol 2013;122:694–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Peebles R, Hardy KK, Wilson JL, Lock JD. Medical compromise in eating disorders not otherwise specified: Are diagnostic criteria for eating disorders markers of severity? Pediatrics 2010;125:e1193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Steinhausen HC. Outcome of eating disorders. Child Adolescent Psychiatric Clinics North Am 2009;18:225–42. [DOI] [PubMed] [Google Scholar]
- [8].Forman SF, Grodin LF, Graham DA, et al. An eleven site national quality improvement evaluation of adolescent medicine-based eating disorder programs: Predictors of weight outcomes at one year and risk adjustment analyses. J Adolesc Health 2011;49:594–600. [DOI] [PubMed] [Google Scholar]
- [9].Forman SF, McKenzie N, Hehn R, et al. Predictors of outcome at 1 year in adolescents with DSM-5 restrictive eating disorders: Report of the national eating disorders quality improvement collaborative. J Adolesc Health 2014; 55:750–6. [DOI] [PubMed] [Google Scholar]
- [10].Kapphahn CJ, Hehn R, Woods ER, et al. Effect of hospitalization on weight restoration in adolescents with restrictive eating disorders. Los Angeles, CA: Society for Adolescent Health and Medicine; 2015. [Google Scholar]
- [11].Centers for Disease Control and Prevention, National Center for Health Statistics. CDC growth charts: United States. 2000. Available at: https://www.cdc.gov/growthcharts/.AccessedOctober 17, 2016.
- [12].Centers for Disease Control and Prevention, National Center for Health Statistics. Defining childhood obesity. 2015. Available at: http://www.cdc.gov/obesity/childhood/defining.html.AccessedOctober 17, 2016.
- [13].Society for Adolescent Health and Medicine, Golden NH, Katzman DK, Sawyer SM, et al. Position paper of the society for adolescent health and medicine: Medical management of restrictive eating disorders in adolescents and young adults. J Adolesc Health 2015;56: 121–5. [DOI] [PubMed] [Google Scholar]
- [14].Golden NH, Katzman DK, Kreipe RE, et al. Eating disorders in adolescents: Position paper of the Society for Adolescent Medicine. J Adolesc Health 2003;33:496–503. [DOI] [PubMed] [Google Scholar]
- [15].Baron RM, Kenny DA. The moderatoremediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Personal Soc Psychol 1986;51:1173. [DOI] [PubMed] [Google Scholar]
- [16].MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol 2007;58:593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Muthén LK, Muthén BO. Mplus user’s guide. 6th edition. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- [18].Austin SB, Spadano-Gasbarro J, Greaney ML, et al. Disordered weight control behaviors in early adolescent boys and girls of color: An under-recognized factor in the epidemic of childhood overweight. J Adolesc Health 2011;48:109–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Robinson KJ, Moutnford VA, Sperlinger DJ. Being men with eating disorders: Perspective of male eating disorder service-users. J Health Psychol 2013;18:176–86. [DOI] [PubMed] [Google Scholar]
- [20].Cachelin FM, Rebeck R, Veisel C, Striegel-Moore RH. Barriers to treatment for eating disorders among ethnically diverse women. Int J Eat Disord 2001;30:269–78. [DOI] [PubMed] [Google Scholar]
- [21].American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, D.C.: American Psychiatric Association; 2013. [Google Scholar]
- [22].Eddy KT, Tanofsky-Kraff M, Thompson-Brenner H, et al. Eating disorder pathology among overweight treatment-seeking youth: Clinical correlates and cross-sectional risk modeling. Behav Res Ther 2007;45: 2360–71. [DOI] [PubMed] [Google Scholar]
- [23].Masheb RM, White MA, Grilo CM. Substantial weight gains are common prior to treatment-seeking in obese patients with binge eating disorder. Compr Psychiatry 2013;54:880–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Blomquist KK, Barnes RD, White MA, et al. Exploring weight gain in year before treatment for binge eating disorder: A different context for interpreting limited weight losses in treatment studies. Int J Eat Disord 2011; 44:435–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Masheb R, White MA. Bulimia nervosa in overweight and normal-weight women. Compr Psychiatry 2012;53:181–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-anlaysis of 36 studies. Arch Gen Psychiatry 2011;68:724–31. [DOI] [PubMed] [Google Scholar]
- [27].Winkler LA, Christiansen E, Lichtenstein MB, et al. Quality of life in eating disorders: A meta-analysis. Psychiatry Res 2014;219:1–9. [DOI] [PubMed] [Google Scholar]
- [28].Greenhalgh S Fat-talk nation: The human cost of America’s war on fat. Ithaca, NY: Cornell University Press; 2015. [Google Scholar]


