Abstract
Background:
Post-acute care rehabilitation is critically important to recover after trauma but many patients do not have access. A better understanding of the drivers behind inpatient rehabilitation facility (IRF) use has the potential for major cost-savings as well as higher quality, and more equitable patient care. We sought to quantify the variation in hospital rates of trauma patient discharge to inpatient rehabilitation and understand which factors (patient- vs injury- vs hospital-level) contribute the most.
Methods:
We performed a retrospective cohort study of 668,305 adult trauma patients admitted to 900 Level I-IV trauma centers between 2011 and 2015 using the National Trauma Data Bank (NTBD). Participants were included if they met the following criteria: age ≥18, injury severity score (ISS) ≥9, identifiable injury type, and who had one of the Centers for Medicare & Medicaid Services (CMS) preferred diagnoses for inpatient rehabilitation under the “60% rule”.
Results:
The overall risk- and reliability-adjusted hospital rates of discharge to IRF averaged 18.8% in the non-elderly adult cohort (18–64 years old) and 23.4% in the older adult cohort (65 years or older). Despite controlling for all patient, injury and hospital-level factors, hospital discharge of patients to IRF varied substantially between hospital quintiles and ranged from 9–30% in the non-elderly adult cohort and from 7–46% in the older adult cohort. Proportions of total variance ranged from 2.4% (patient insurance) to 12.1% (injury-level factors) in the non-elderly adult cohort and from 0.3% (patient-level factors) to 26.0% (unmeasured hospital-level factors) in the older adult cohort.
Conclusion:
Among a cohort of injured patients with diagnoses that are associated with significant rehabilitation needs, the hospital at which a patient receives their care may drive a patient’s likelihood of recovering at an IRF just as much, if not more, than their clinical attributes.
Keywords: Trauma, inpatient rehabilitation, post-acute care, hospital effect
Introduction
Recovery from illness or injury often extends well past a patient’s index hospitalization. Post-acute care (PAC) facilities have been shown to improve patient outcomes, mortality and functional status.1–3 Despite the known benefits, access to PAC facilities remains inconsistent among patients and there continues to be a sizeable, unmet need for rehabilitation services.4–7 Moreover, use of PAC facilities has become one of the most rapidly growing health care costs in the United States and has been identified as the primary cause of regional variation in Medicare per-beneficiary spending.8–11 A better understanding of the drivers behind PAC facility use has the potential for major cost-savings as well as higher quality, more cost-effective, and more equitable patient care.8,12
Unfortunately, hospital use of PAC facilities remains highly variable, despite controlling for several patient, clinical, and hospital-level factors.10,13–17 Equity in discharge to a PAC facility is of critical importance in the trauma population, where individuals are commonly affected during their most productive years of life, and where discharge to an inpatient rehabilitation facility (IRF) is associated with improved post-injury functional status, quality of life and 1-year survival.2,4,18 The importance of this benefit at the individual and population level is reflected in the Centers for Medicare & Medicaid Services (CMS) “60% rule” which stipulates that IRFs must have at least 60% of patients with one of thirteen primary diagnoses, of which five are injury-related (spinal cord injury, femur/hip fracture, brain injury, burns, and major multiple trauma).19 Patients with the above injuries have a high likelihood of needing PAC rehabilitation and thus represent an ideal population through which persistent, unexplained variation in hospital use of IRFs can be explored.
In this context, our study had three main objectives: 1) Identify the key patient and hospital-level factors that are associated with a trauma patient’s likelihood of discharge to an IRF, 2) Quantify the variation in hospital rates of discharge to IRF, and 3) Characterize the unexplained variation (patient vs injury vs hospital-level traits) that underlies this residual variation.
Methods
Data set and analytic cohort
To study the drivers behind trauma patients’ dispositions, we examined the National Trauma Data Bank® (NTDB) - the world’s largest trauma data repository with more than 7.5 million electronic records from more than 900 trauma centers from the United States.20 Our population of interest included adult patients admitted to Level I-IV trauma centers between 2011 and 2015 who met the following criteria: age ≥18, injury severity score (ISS) ≥9, identifiable injury type (blunt, penetrating, other), and who had one of the CMS preferred diagnoses for inpatient rehabilitation under the “60% rule”.19 These years were chosen because the definition of discharge disposition changed after 2015, which made it more difficult to isolate patients discharged to IRFs—the focus of this study. Patients who died before discharge or who did not have a valid discharge disposition code were not included in the analysis. For our patient age-stratified site variation analysis, we excluded hospitals with a volume of less than 100 patients per year in any of the study years (Supplementary eFigure 1).
Patient and hospital characteristics
The NTBD was abstracted for following patient demographics: age, gender, race (non-Hispanic White, non-Hispanic Black, Hispanic and Other), payer status (Medicare, Medicaid, Self-pay, Private, Other Government and Other), and frailty index. Based on the variables available in our database, we calculated a modified frailty index from the presence or absence of 10 patient comorbidities. The index ranges from 0.0 (least frail) to 1.0 (most frail). Using the inflection point observed in our data, we considered a modified frailty index of ≥0.4 to be “more frail” and included this as a binary variable in our analysis.21
The following injury traits were collected from the NTDB: injury type (blunt, penetrating, other), injury mechanism (cut, firearm, fall, motor vehicle collision (MVC), motorcycle, pedal cyclist, struck by22 and other), ISS, maximum abbreviated injury scale ≥3 (head/neck, face, chest, abdomen/pelvis, spine, upper extremity, lower extremity, external), Glasgow coma scale motor score, shock index23, and transfer status.
Hospital-level factors thought to be associated with discharge to IRF included trauma level (I–IV), region (categorized by four census regions: Midwest, Northeast, South, West), teaching status (university, community, non-teaching), number of beds dedicated to adult, number of intensive care unit (ICU) beds for burn and trauma patients, and number of core trauma surgeons. For analytic purposes, trauma level IV was grouped into trauma level III.
Outcomes
The primary outcome of interest was patient discharge to an IRF. Patients were categorized as discharged to an IRF if the discharge disposition was extracted as “discharged/transferred to inpatient rehab or designated unit” or “discharged/transferred to another type of rehabilitation or long term.” Of note, this does not include skilled nursing facilities or long-term acute care facilities. Sub-group analyses were performed after stratifying patients into two age cohorts: 18–64 years old and 65 years and older in order to account for the significant differences in payer mix as Medicare eligibility for most our study population begins at 65 years old.
Statistical analyses
Association of covariates and discharge to IRF:
We performed univariate analysis for each covariate and our primary outcome in both age cohorts. We used chi-square tests to evaluate the level of association between discharge to IRF and various patient, injury, and hospital-level traits. We then included all covariates in a multivariable logistic regression model with robust standard errors to further assess the statistical significance of the association between each covariate and discharge to IRF. Patients with incomplete data were not included in the regression.
Risk- and reliability-adjusted variation in hospital rates of discharge to IRF:
Using random effects logistic regression models, we generated empirical Bayes predictions of discharge to IRF for each hospital. These models were two-level hierarchical logistic regression models (patients nested within hospitals) and included patient, injury, and hospital-level traits as fixed effects. This technique shrinks the point estimate of rate of discharge to IRF back toward the mean rate, with the amount of shrinkage proportional to the reliability at each hospital. Reliability adjustment accounts for the chance-related variability that can occur when measured outcomes are infrequent.24 Finally, we ranked the hospitals according to their risk and reliability-adjusted discharge rates to IRF, and stratified the hospitals into quintiles.
Decomposition of variation source in hospital rates of discharge to IRF:
We generated a series of hierarchical generalized linear models to estimate patient, injury, and hospital-level contributions to observed variations in the discharge to IRF. Each model included a unique hospital identifier as a random-effects term. The initial model (known as the “unconditional model”) included only a hospital-level random effects term and from this model, we estimated the hospital-attributable residual intraclass correlation coefficient (RICC). The RICC ranges from 0 to 1 and is an estimation of the proportion of the “left-over” or unexplained variance in an outcome variable.25 For example, in our study, a hospital-level RICC of 0.25 would mean unexplained hospital effects make up 25% of the unexplained variation in rates of discharge to IRF.
We then estimated the variance partitioning coefficients (VPC) of patient demographics, patient injury traits, patient insurance and hospital factors. The VPC ranges from 0 to 1 and is a proportion measuring the contribution towards the total variance from each set of variables.25 For example, if a set of patient demographic variables had a VPC of 0.05, this would mean that these variables contribute to 5% of the total variation in rates of discharge to IRF. We calculated VPCs by fitting separate models that included both a hospital-level random effects term and only one of the following fixed effect covariate subsets: (1) patient demographics, (2) patient injury traits, (3) patient insurance, and (4) hospital factors.
Sensitivity analysis
In order to determine the degree to which our findings are based on the specific definition of IRF used by the NTDB, we performed a sensitivity analysis that looked at discharge to any post-acute care facility defined as: IRF, skilled nursing facility, intermediate care facilities, and long-term care hospital. We repeated the analyses described above using this broader definition of post-acute care facilities as our outcome of interest.
All analyses were performed using Stata/MP 15.1 StataCorp (College Station, TX) and carried out at the 5% significance level.
Results
Sample derivation
We identified 668,305 adult trauma patients admitted to 900 Level I-IV trauma centers participating in the NTDB. For our site variation analysis, we analyzed 518 hospitals for the non-elderly adult cohort (18–64 years old) and 548 hospitals in the older adult (≥65 years old) cohort. Complete demographics of our patient sample can be found in Table 1.
Table 1:
Patient Demographics and Discharge to Rehab
| Non-elderly adult cohort (Ages 18–64) | Older adult cohort (Ages ≥65) | |||||
|---|---|---|---|---|---|---|
| Yes (N=78,186) | No (N=343,177) | P-Value | Yes (N=57,067) | No (N=189,875) | P-Value | |
| Demographics | ||||||
| Gender (male) | 55015 (70.4%) | 248926 (72.6%) | <.001 | 24594 (43.1%) | 80557 (42.4%) | 0.004 |
| Race | ||||||
| NH-White | 55011 (70.4%) | 236347 (68.9%) | 48842 (85.6%) | 160401 (84.5%) | ||
| NH-Black | 10522 (13.5%) | 43046 (12.5%) | <.001 | 2467 (4.3%) | 8368 (4.4%) | <.001 |
| Hispanic | 6182 (7.9%) | 35978 (10.5%) | 2448 (4.3%) | 8573 (4.5%) | ||
| Other | 6471 (8.3%) | 27806 (8.1%) | 3310 (5.8%) | 12533 (6.6%) | ||
| Payer | ||||||
| Medicare | 5603 (7.2%) | 21065 (6.1%) | 41667 (73.0%) | 136102 (71.7%) | ||
| Medicaid | 10735 (13.7%) | 43255 (12.6%) | 804 (1.4%) | 2941 (1.5%) | ||
| Self-pay | 7319 (9.4%) | 62235 (18.1%) | <.001 | 489 (0.9%) | 2091 (1.1%) | <.001 |
| Private | 43686 (55.9%) | 163256 (47.6%) | 10372 (18.2%) | 33768 (17.8%) | ||
| Other government | 2465 (3.2%) | 11438 (3.3%) | 532 (0.9%) | 1638 (0.9%) | ||
| Other | 8378 (10.7%) | 41928 (12.2%) | 3203 (5.6%) | 13335 (7.0%) | ||
| Frailty (index≥0.4) | 294 (0.4%) | 1180 (0.3%) | 0.17 | 1403 (2.5%) | 6509 (3.4%) | <.001 |
| Injury traits | ||||||
| Type | ||||||
| Blunt | 73805 (94.4%) | 327706 (95.5%) | 56633 (99.2%) | 188458 (99.3%) | ||
| Penetrating | 3133 (4.0%) | 8881 (2.6%) | <.001 | 108 (0.2%) | 288 (0.2%) | 0.12 |
| Other | 1248 (1.6%) | 6590 (1.9%) | 326 (0.6%) | 1129 (0.6%) | ||
| Mechanism | ||||||
| Cut | 188 (0.2%) | 1067 (0.3%) | 23 (0.0%) | 102 (0.1%) | ||
| Firearm | 2941 (3.8%) | 7795 (2.3%) | 85 (0.1%) | 185 (0.1%) | ||
| Fall | 18739 (24.0%) | 80119 (23.3%) | 42948 (75.3%) | 144221 (76.0%) | ||
| MVC | 33086 (42.3%) | 128684 (37.5%) | <.001 | 9776 (17.1%) | 30071 (15.8%) | <.001 |
| Motorcycle | 11348 (14.5%) | 46284 (13.5%) | 1130 (2.0%) | 3746 (2.0%) | ||
| Pedal | 1055 (1.3%) | 8546 (2.5%) | 400 (0.7%) | 1572 (0.8%) | ||
| Struck | 2742 (3.5%) | 23064 (6.7%) | 583 (1.0%) | 2449 (1.3%) | ||
| Other | 8087 (10.3%) | 47618 (13.9%) | 2122 (3.7%) | 7529 (4.0%) | ||
| ISS | ||||||
| Moderate (9–15) | 24103 (30.8%) | 190310 (55.5%) | 38635 (67.7%) | 135803 (71.5%) | ||
| Severe (16–25) | 29374 (37.6%) | 110255 (32.1%) | <.001 | 14076 (24.7%) | 44318 (23.3%) | <.001 |
| Critical (≥26) | 24709 (31.6%) | 42612 (12.4%) | 4356 (7.6%) | 9754 (5.1%) | ||
| MAX AIS ≥3 | ||||||
| Max Head/Neck Injury AIS≥3 | 35349 (45.3%) | 143226 (41.8%) | <.001 | 17332 (30.4%) | 72210 (38.0%) | <.001 |
| Max Face Injury AIS≥3 | 1431 (1.8%) | 4264 (1.2%) | <.001 | 199 (0.3%) | 639 (0.3%) | 0.66 |
| Max Chest Injury AIS≥3 | 35033 (44.9%) | 135287 (39.5%) | <.001 | 10142 (17.8%) | 33343 (17.6%) | 0.24 |
| Max Abd/Pelvic Injury AIS≥3 | 9082 (11.6%) | 25123 (7.3%) | <.001 | 1297 (2.3%) | 2827 (1.5%) | <.001 |
| Max Spine Injury AIS≥3 | 18366 (23.5%) | 30274 (8.8%) | <.001 | 5080 (8.9%) | 9466 (5.0%) | <.001 |
| Max Upper Extremity Injury AIS≥3 | 5674 (7.3%) | 16224 (4.7%) | <.001 | 1351 (2.4%) | 3282 (1.7%) | <.001 |
| Max Lower Extremity Injury AIS≥3 | 30590 (39.2%) | 98642 (28.8%) | <.001 | 32609 (57.2%) | 90743 (47.8%) | <.001 |
| Max External AIS≥3 | 62 (0.1%) | 109 (0.0%) | <.001 | N/Aa | N/Aa | N/Aa |
| ED GCS Motor Score | ||||||
| 1 | 14150 (18.8%) | 23042 (7.0%) | 1515 (2.9%) | 3235 (1.9%) | ||
| 2–5 | 9751 (13.0%) | 20289 (6.1%) | <.001 | 1921 (3.6%) | 6150 (3.5%) | <.001 |
| 6 | 51316 (68.2%) | 287243 (86.9%) | 49467 (93.5%) | 165009 (94.6%) | ||
| Shock index (0–1) | ||||||
| <0.4 | 2680 (3.5%) | 9769 (2.9%) | 6415 (11.6%) | 21437 (11.6%) | ||
| 0.4–<0.5 | 7180 (9.4%) | 35832 (10.6%) | 13047 (23.6%) | 44889 (24.3%) | ||
| 0.5–<0.8 | 40315 (52.8%) | 209794 (62.3%) | <.001 | 30111 (54.4%) | 100584 (54.5%) | <.001 |
| ≥0.8 | 26166 (34.3%) | 81621 (24.2%) | 5803 (10.5%) | 17736 (9.6%) | ||
| Transfer (yes) | 18111 (23.2%) | 89593 (26.1%) | <.001 | 14248 (25.0%) | 55658 (29.3%) | <.001 |
| Hospital traits | ||||||
| Trauma Level | ||||||
| I | 52004 (68.0%) | 218573 (65.0%) | 27915 (50.4%) | 92579 (50.5%) | ||
| II | 22242 (29.1%) | 101970 (30.3%) | <.001 | 21063 (38.0%) | 70959 (38.7%) | <.001 |
| III | 2286 (3.0%) | 15614 (4.6%) | 6398 (11.6%) | 19668 (10.7%) | ||
| Region | ||||||
| Midwest | 19936 (25.8%) | 75222 (22.2%) | 14376 (25.3%) | 58707 (31.0%) | ||
| Northeast | 14697 (19.0%) | 50104 (14.8%) | <.001 | 16412 (28.9%) | 30782 (16.3%) | <.001 |
| South | 29917 (38.7%) | 142913 (42.2%) | 20288 (35.7%) | 65779 (34.8%) | ||
| West | 12678 (16.4%) | 70586 (20.8%) | 5756 (10.1%) | 33963 (17.9%) | ||
| Teaching | ||||||
| University | 44400 (56.8%) | 184962 (53.9%) | 24455 (42.9%) | 73143 (38.5%) | ||
| Community | 25995 (33.2%) | 116578 (34.0%) | <.001 | 23637 (41.4%) | 81011 (42.7%) | <.001 |
| Non-teaching | 7791 (10.0%) | 41637 (12.1%) | 8975 (15.7%) | 35721 (18.8%) | ||
| Beds Dedicated to Adult | ||||||
| 1–100 | 863 (1.1%) | 5836 (1.7%) | 1041 (1.8%) | 4225 (2.2%) | ||
| 101–250 | 8351 (10.7%) | 40792 (11.9%) | 8837 (15.5%) | 31654 (16.7%) | ||
| 251–350 | 13363 (17.1%) | 62010 (18.1%) | <.001 | 12653 (22.2%) | 38210 (20.2%) | <.001 |
| 351–500 | 20304 (26.0%) | 90228 (26.3%) | 12694 (22.3%) | 44775 (23.6%) | ||
| >500 | 35211 (45.1%) | 143702 (41.9%) | 21727 (38.1%) | 70663 (37.3%) | ||
| ICU Beds to Burn Patients | ||||||
| 0 | 50676 (65.9%) | 227053 (67.1%) | 43357 (78.0%) | 142851 (76.9%) | ||
| 1–5 | 7008 (9.1%) | 24256 (7.2%) | 3743 (6.7%) | 10188 (5.5%) | ||
| 6–8 | 9768 (12.7%) | 47157 (13.9%) | <.001 | 4150 (7.5%) | 17001 (9.2%) | <.001 |
| 9–10 | 3431 (4.5%) | 13621 (4.0%) | 1955 (3.5%) | 5540 (3.0%) | ||
| 11–12 | 1790 (2.3%) | 9084 (2.7%) | 487 (0.9%) | 3545 (1.9%) | ||
| >12 | 4209 (5.5%) | 17096 (5.1%) | 1887 (3.4%) | 6618 (3.6%) | ||
| ICU Beds to Trauma Patients | ||||||
| 0 | 995 (1.3%) | 4793 (1.4%) | 1482 (2.6%) | 5112 (2.7%) | ||
| 1–10 | 3221 (4.1%) | 15448 (4.5%) | 4053 (7.1%) | 13393 (7.1%) | ||
| 11–15 | 10457 (13.4%) | 43494 (12.7%) | 9282 (16.3%) | 24792 (13.1%) | ||
| 16–25 | 21102 (27.0%) | 100727 (29.4%) | <.001 | 19010 (33.4%) | 60787 (32.1%) | <.001 |
| 26–35 | 11464 (14.7%) | 58180 (17.0%) | 7770 (13.7%) | 30661 (16.2%) | ||
| >35 | 30774 (39.4%) | 120064 (35.0%) | 15253 (26.8%) | 54676 (28.9%) | ||
| Number of Core Trauma Surgeons | ||||||
| 0 | 64 (0.1%) | 531 (0.2%) | 215 (0.4%) | 874 (0.5%) | ||
| 1–3 | 3088 (3.9%) | 14343 (4.2%) | 3462 (6.1%) | 12142 (6.4%) | ||
| 4–6 | 36842 (47.1%) | 161170 (47.0%) | <.001 | 29905 (52.4%) | 95165 (50.1%) | <.001 |
| 7–8 | 19773 (25.3%) | 82703 (24.1%) | 12320 (21.6%) | 42926 (22.6%) | ||
| >8 | 18419 (23.6%) | 84430 (24.6%) | 11165 (19.6%) | 38768 (20.4%) |
Abbreviations: Non-Hispanic (NH), Motor vehicle collision (MVC), Injury severity score (ISS), Maximum abbreviated injury scale (MAX AIS), Emergency Department Glasgow Coma Scale (ED GCS), Intensive Care Unit (ICU)
No older adults with variable data available
Percentages were calculated based on patient cohort with available variable data. Percentages may not add up to 100% due to rounding error
Use of inpatient rehabilitation facilities
Among the 668,305 adult trauma patients, 135,253 (20.2%) were discharged to an IRF. Within the non-elderly adult cohort, 78,186 (18.6%) were discharged to an IRF and in the older adult cohort, 57,067 (23.1%). In the non-elderly adult cohort, patients discharged to an IRF tended to be male, non-Hispanic White, privately insured, had suffered blunt injuries, presented with a GCS motor score = 6, and had a shock index of greater than 0.5 (Table 1). In contrast, patients discharged to an IRF in the older adult cohort tended to be female and insured by Medicare but otherwise shared the same injury and presentation characteristics. In regard to hospital factors, in both cohorts, patients discharged to an IRF tended to be from Level I trauma centers, teaching hospitals, and hospitals with over 350 adult beds and greater than 16 dedicated trauma ICU beds (Table 1).
Multivariable analysis adjusting for all patient, injury, and hospital factors highlighted differences in covariates between age cohorts (Table 2). In the non-elderly adult cohort, a frailty index of ≥0.4 was associated with a higher odds of discharge to IRF (adjusted odds ratio [aOR], 1.18; 95% confidence interval [CI] 1.02–1.37; p = 0.025), but in the older adult cohort, a frailty index of ≥0.4 was associated with a lower odds of discharge to IRF (aOR, 0.73, 95% CI, 0.68 – 0.78, p < 0.001). Regarding insurance status, in the non-elderly adult cohort, having Medicare yielded a higher odds of discharge to IRF (aOR, 1.11; 95% CI 1.07 – 1.15; p < 0.001) compared to those privately insured, whereas in the older adult cohort, being privately insured yielded a lower odds of discharge to IRF (aOR, 0.91; 95% CI; 0.88 – 0.84, p < 0.001) compared to those insured by Medicare. When compared to non-Hispanic White patients, non-Hispanic Black patients had a similar odds of discharge to IRF (aOR, 1.01; 95% CI, 0.98 – 1.04; p = 0.484) in the non-elderly adult cohort, whereas they had a lower odds in the older adult cohort (aOR, 0.85; 95% CI 0.80 – 0.090; p < 0.001).
Table 2:
Multivariable logistic regression model adjusting for all patient-, injury-, and hospital-level covariates to determine associate with discharge to an inpatient rehabilitation facility
| Non-elderly adult cohort (Ages 18–64) | Older adult cohort (Ages ≥65) | ||||
|---|---|---|---|---|---|
| Characteristic (reference group) | aOR (95% CI) | P-Value | Characteristic (reference group) | aOR (95% CI) | P-Value |
| Demographics | |||||
| Female gender (Male) | 0.89 (0.87 – 0.91) | <.001 | 1.12 (1.09 – 1.15) | <.001 | |
| Race (NH-White) | |||||
| NH-Black | 1.01(0.98 – 1.04) | 0.48 | 0.85 (0.80 – 0.90) | <.001 | |
| Hispanic | 0.82 (0.79 – 0.85) | <0.001 | 0.80 (0.75 – 0.85) | <.001 | |
| Other | 0.99 (0.95 – 1.03) | 0.70 | 0.95 (0.90 – 1.01) | 0.11 | |
| Payer (Private) | Payer (Medicare) | ||||
| Medicare | 1.11 (1.07 – 1.15) | <0.001 | Medicaid | 0.83 (0.75 – 0.91) | <.001 |
| Medicaid | 0.80 (0.78 – 0.83) | <0.001 | Self-pay | 0.58 (0.51 – 0.65) | <.001 |
| Self-pay | 0.41 (0.40 – 0.42) | <0.001 | Private | 0.92 (0.88 – 0.94) | <.001 |
| Other government | 0.74 (0.70 – 0.79) | <0.001 | Other government | 0.99 (0.85 – 1.14) | 0.86 |
| Other | 0.71 (0.69 – 0.74)) | <0.001 | Other | 0.79 (0.74 – 0.84) | <.001 |
| Frailty (index≥0.4) | 1.18 (1.02 – 1.37) | 0.03 | 0.73 (0.68 – 0.78) | <.001 | |
| Injury traits | |||||
| Type (Blunt) | |||||
| Penetrating | 0.47 (0.05 – 4.40) | 0.51 | N/Aa | N/Aa | |
| Other | 1.19 (1.10 – 1.29) | <.001 | 1.02 (0.87 – 1.20) | 0.81 | |
| Mechanism (MVC) | Mechanism (Fall) | ||||
| Cut | 1.77 (0.19 – 16.73) | 0.62 | Cut | N/Aa | N/Aa |
| Firearm | 2.91 (0.31 – 27.30) | 0.35 | Firearm | N/Aa | N/Aa |
| Fall | 1.12 (1.09 – 1.15) | <.001 | MVC | 1.21 (1.17 – 1.26) | <.001 |
| Motorcycle | 1.08 (1.05 – 1.11) | <.001 | Motorcycle | 1.14 (1.05 – 1.24) | 0.001 |
| Pedal | 0.73 (0.68 – 0.78) | <.001 | Pedal | 1.05 (0.92 – 1.19) | 0.49 |
| Struck | 0.75 (0.71 – 0.79) | <.001 | Struck | 0.92 (0.82 – 1.02) | 0.10 |
| Other | 0.84 (0.82 – 0.87) | <.001 | Other | 1.07 (1.00 – 1.14) | 0.03 |
| ISS (Moderate 9–15) | |||||
| Severe (16–25) | 2.15 (2.10 – 2.20) | <.001 | 1.55 (1.50 – 1.60) | <.001 | |
| Critical (≥26) | 3.70 (3.58 – 3.82) | <.001 | 2.04 (1.93 – 2.16) | <.001 | |
| MAX AIS ≥3 | |||||
| Max Head/Neck Injury AIS≥3 | 0.91 (0.88 – 0.93) | <.001 | 0.78 (0.75 – 0.81) | <.001 | |
| Max Face Injury AIS≥3 | 0.87 (0.81 – 0.93) | <.001 | 0.83 (0.68 – 1.00) | 0.05 | |
| Max Chest Injury AIS≥3 | 0.82 (0.80 – 0.84) | <.001 | 0.94 (0.90 – 0.98) | 0.001 | |
| Max Abd/Pelvic Injury AIS≥3 | 0.79 (0.77 – 0.82) | <.001 | 1.13 (1.04 – 1.22) | 0.005 | |
| Max Spine Injury AIS≥3 | 3.14 (3.06 – 3.22) | <.001 | 2.18 (2.08 – 2.29) | <.001 | |
| Max Upper Extremity Injury AIS≥3 | 1.19 (1.14 – 1.23) | <.001 | 1.13 (1.05 – 1.23) | 0.001 | |
| Max Lower Extremity Injury AIS≥3 | 2.00 (1.95 – 2.04) | <.001 | 1.76 (1.70 – 1.82) | <.001 | |
| Max External AIS≥3 | 1.00 (0.68 – 1.45) | 0.97 | N/A | N/A | |
| ED GCS Motor Score (GCS = 6) | |||||
| 1 | 2.93 (2.84 – 3.01) | <.001 | 1.75 (1.63 – 1.89) | <.001 | |
| 2–5 | 2.59 (2.50 – 2.66) | <0.001 | 1.18 (1.11 – 1.26) | <.001 | |
| Shock index (Index ≥0.8) | |||||
| <0.4 | 1.07 (1.02 – 1.13) | 0.007 | 1.02 (0.97 – 1.07) | 0.47 | |
| 0.4–<0.5 | 0.90 (0.87 – 0.93) | <.001 | 0.99 (0.95 – 1.03) | 0.65 | |
| 0.5–<0.8 | 0.85 (0.83 – 0.87) | <.001 | 1.02 (0.98 – 1.06) | 0.43 | |
| Transfer (Yes) | 0.81 (0.79 – 0.83) | <.001 | 0.90 (0.87 – 0.92) | <.001 | |
| Hospital traits | |||||
| Trauma Level (Level I) | |||||
| II | 0.84 (0.70 – 1.01) | 0.07 | 0.89 (0.73 – 1.08) | 0.23 | |
| III | 1.07 (0.84 – 1.37) | 0.57 | 1.01 (0.78 – 1.31) | 0.93 | |
| Region (Midwest) | |||||
| Northeast | 2.89 (1.26 – 6.61) | 0.012 | 6.05 (3.15 – 11.61) | <.001 | |
| South | 2.19 (0.53 – 9.07) | 0.28 | 1.15 (0.12 – 10.83) | 0.91 | |
| West | 1.40 (0.57 – 3.46) | 0.47 | 0.40 (0.11 – 1.50) | 0.18 | |
| Teaching (University) | |||||
| Community | 1.02 (0.89 – 1.17) | 0.79 | 1.08 (0.91 – 1.29) | 0.37 | |
| Non-teaching | 0.66 (0.54 – 0.80) | <.001 | 0.85 (0.69 – 1.06) | 0.15 | |
| Beds Dedicated to Adult (>500) | |||||
| 1–100 | 0.77 (0.64 – 0.92) | 0.004 | 0.79 (0.59 – 1.07) | 0.12 | |
| 101–250 | 0.65 (0.55 – 0.76) | <.001 | 0.77 (0.62 – 0.95) | 0.02 | |
| 251–350 | 0.85 (0.75 – 0.95) | 0.004 | 0.81 (0.69 – 0.95) | 0.008 | |
| 351–500 | 0.84 (0.76 – 0.92) | <.001 | 0.95 (0.83 – 1.10) | 0.51 | |
| ICU Beds to Burn Patients (Beds = 0) | |||||
| 1–5 | 2.02 (1.72 – 2.35) | <.001 | 1.87 (1.53 – 2.28) | <.001 | |
| 6–8 | 0.62 (0.51 – 0.75) | <.001 | 0.45 (0.36 – 0.56) | <.001 | |
| 9–10 | 6.44 (3.99 – 10.41) | <.001 | 0.81 (0.45 – 1.44) | 0.47 | |
| 11–12 | 4.13 (2.48 – 6.89) | <.001 | 1.30 (0.80 – 2.14) | 0.29 | |
| >12 | 4.92 (2.95 – 8.21) | <.001 | 1.36 (0.89 – 2.09) | 0.16 | |
| ICU Beds to Trauma Patients (Beds = 0) | |||||
| 0 | 0.60 (0.29 – 1.23) | 0.16 | 0.48 (0.27 – 0.84) | 0.01 | |
| 1–10 | 0.70 (0.34 – 1.42) | 0.32 | 0.45 (0.26 – 0.80) | 0.006 | |
| 11–15 | 0.68 (0.33 – 1.38) | 0.29 | 0.63 (0.36 – 1.10) | 0.10 | |
| 16–25 | 0.51 (0.25 – 1.04) | 0.06 | 0.45 (0.25 – 0.79) | 0.006 | |
| 26–35 | 0.47 (0.23 – 0.95) | 0.04 | 0.46 (0.26 – 0.81) | 0.007 | |
| Number of Core Trauma Surgeons (N>8) | |||||
| 0 | 1.14 (0.33 – 3.90) | 0.84 | 0.62 (0.24 – 1.59) | 0.32 | |
| 1–3 | 1.01 (0.90 – 1.13) | 0.92 | 0.77 (0.68 – 0.88) | <.001 | |
| 4–6 | 1.00 (0.94 – 1.07) | 0.99 | 1.06 (0.97 – 1.15) | 0.21 | |
| 7–8 | 1.03 (0.97 – 1.08) | 0.36 | 1.06 (0.98 – 1.14) | 0.14 |
Abbreviations: Non-Hispanic (NH), Motor vehicle collision (MVC), Injury severity score (ISS), Maximum abbreviated injury scale (MAX AIS), Emergency Department Glasgow Coma Scale (ED GCS), Intensive Care Unit (ICU)
Calculation of odds ratio and 95% confidence interval limited by very small sample size
Risk- and reliability-adjusted hospital variation
At the hospital-level, the mean risk- and reliability-adjusted rate of discharge to IRF was 18.8% in the non-elderly adult cohort and 23.4% in the older adult cohort. However, hospital discharge of patients to IRF varied substantially between hospital quintiles and ranged from 9–30% in the non-elderly adult cohort and from 7–46% in the older adult cohort (Figure 1). These values show that despite controlling for all patient, injury, and hospital-level factors, there was a 3-fold difference in the discharge rates of non-elderly adults to IRF between hospitals in the top and bottom quintiles and an over 6-fold difference in the older adult cohort.
Figure 1. Risk- and reliability-adjusted hospital rates of discharge to inpatient rehabilitation.
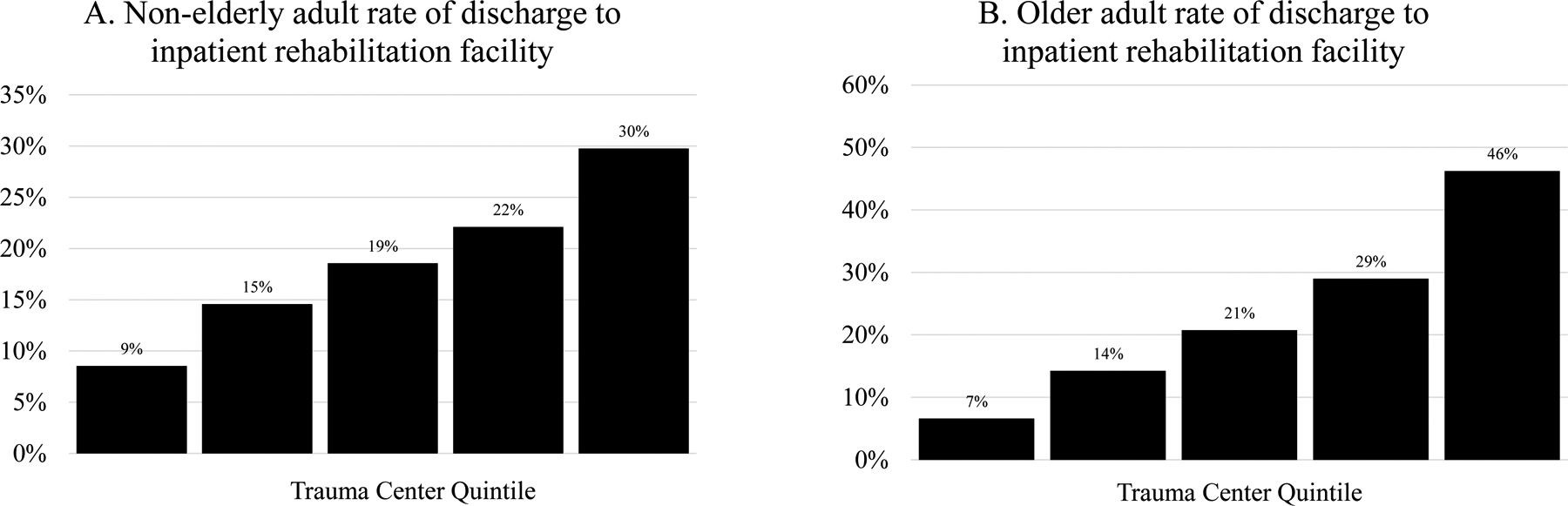
Risk- and reliability-adjusted hospital rates of discharge to inpatient rehabilitation in A) non-elderly adults and B) older adults
Multilevel analysis
In both age cohorts, we calculated the RICC to evaluate the proportion of unexplained variance attributable to unmeasured hospital-level factors. In the non-elderly adult cohort, 12.7% of the unexplained variance is attributable to unmeasured hospital-level factors and in the older adult patients, 24.5%. We then examined proportions of total variance attributable to different groups of variables (Figure 2). We found that proportions ranged from 2.4% (patient insurance) to 12.1% (injury-level factors) in the non-elderly adult cohort and from 0.3% (patient-level factors) to 26.0% (unmeasured hospital-level factors) in the older adult cohort.
Figure 2: Partitioned variance.
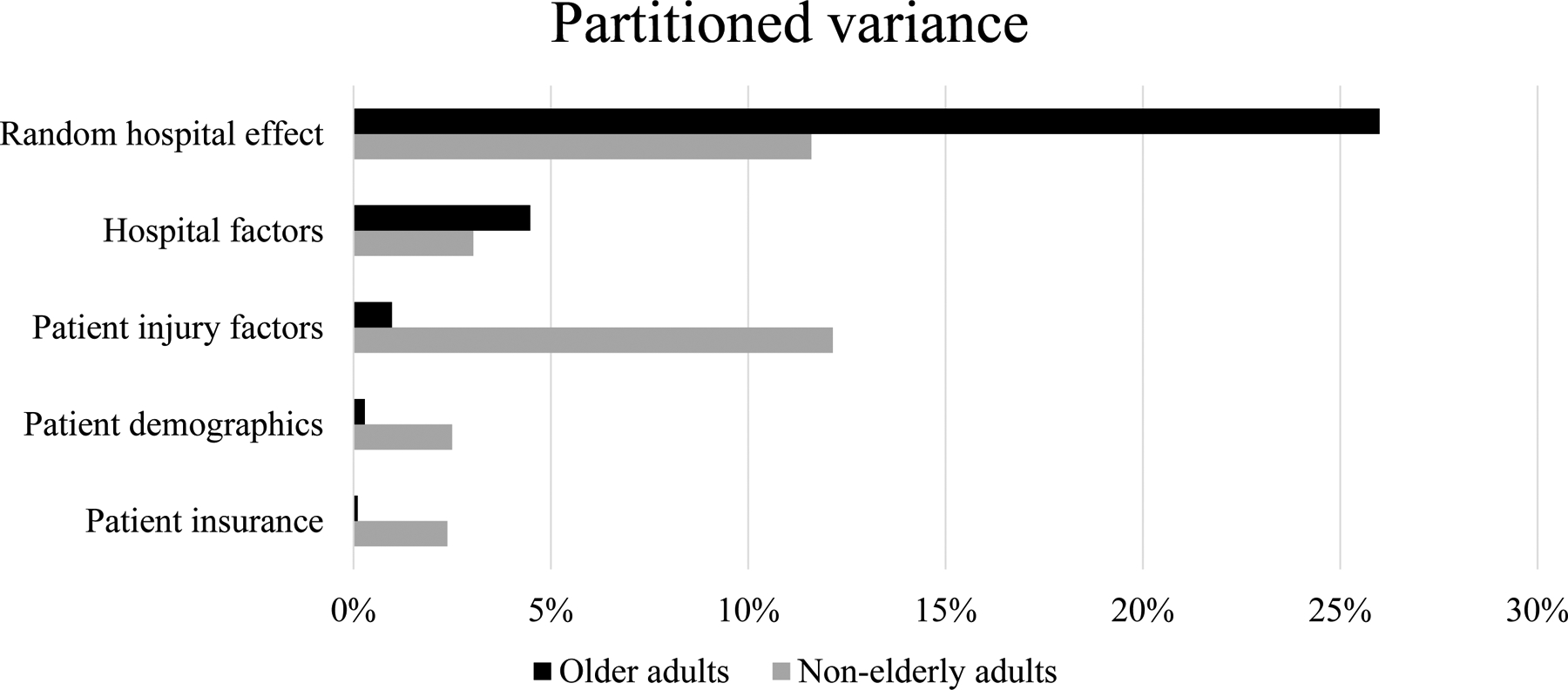
Variance partitioning coefficients (VPC) of random hospital effect, hospital factors, patient insurance, patient demographics, patient injury traits, and patient insurance. The VPC ranges from 0 to 1 and is a proportion measuring the contribution towards the total variation in discharge to inpatient rehabilitation facility from each set of variables.
Sensitivity analysis
When using discharge to any PAC facility as our outcome variable, the risk- and reliability-adjusted hospital rates varied between quintiles from 21–38% in the non-elderly adult cohort and from 54–72% in the older adult cohort. Proportions of total variances attributable to various patient and hospital-level factors did not change substantively in either age cohort. As expected with this more inclusive sensitivity analysis, we found a slight reduction in the effect size of unmeasured hospital-level factors, but it remained among the two most influential drivers of disposition (Supplementary eFigure 2 and 3).
Discussion
The results of this study reveal substantial variation in hospital rates of discharge to IRF. We found that, overall, one in five trauma patients are discharged to an IRF, but after controlling for patient, clinical, and hospital-level factors, hospital discharge rates differed between top and bottom quintiles by 3-fold in the non-elderly adult cohort (9–30%) and over 6-fold in the older adult cohort (7–46%). Breaking down this variation, we found that unexplained hospital-effect accounted for 11% of the total variation in the non-elderly adult cohort and 26% in the older adult cohort. This contribution to total unexplained variation was matched in the non-elderly adult cohort only by patient injury-factors but in the older adult population, it far outweighed any other patient-level contributions. These findings suggest that the hospital at which a patient receives their care may drive a patient’s likelihood of being discharged to an IRF as much, if not more, than their clinical attributes.
Previous studies have already identified several patient and clinical factors that contribute to variation in trauma patient discharge to IRF.26–29 There is a large body of evidence showing that older age and increased injury severity score are associated with discharge to IRF, while being uninsured or of Hispanic ethnicity is associated with a lower odds of discharge to IRF; all of which are concordant with the findings from our study.4,5,26 Prior work has also shown that like Hispanics, non-Hispanic Black patients also have lower odds of discharge to IRF.5,26,27 However, we did not observe this difference in discharge to IRF between non-Hispanic Black patients and non-Hispanic White patients in our non-elderly adult cohort. Given known racial differences in mechanism of injury, this may potentially be a result of limiting our population to the five injury patterns (spinal cord injury, femur/hip fracture, brain injury, burns and major multiple trauma) that fall under the “60% rule” and are therefore more homogenous from a discharge disposition standpoint.30
At the hospital-level, there unfortunately exists a paucity of studies evaluating factors that drive variation in trauma patient discharge to IRF. In our study, we found that patients discharged to IRF tended to be from Level-I trauma centers, teaching hospitals, and hospitals with higher numbers of adult beds and beds dedicated to trauma ICU. However, after multivariable analysis, none of these variables remained statistically and clinically significant in both age cohorts. This poses a challenge for interventional targets and highlights the need for novel hospital metrics to better explain hospital variation in discharge to IRF. Prior work has suggested that hospital ownership of a PAC facility is a factor in their use.13 However, another recent study showed that hospital ownership of an IRF was associated with higher episode payments.31 Although this factor was not available for analysis in our study, given the higher cost associated with use of IRF, it is unlikely to be a major hospital-level driver of disposition in our cohort.
Despite controlling for these patient and hospital-level covariates, persistent variation in hospital use of PAC facilities has been demonstrated among a variety of medical and surgical populations.14,15,32 Our study further emphasizes the need to better understand the drivers of this unexplained variation as the repercussions of unexplained variation are multifold. Our study showed that overall, 20% of trauma patients are discharge to IRF, but this likely represents a mix of both under- and overutilization of this important resource. In our risk- and reliability-adjusted models, we showed the lowest-utilizer hospital quintile had a discharge rate of 9% in the non-elderly adult cohort and 7% in the older adult cohort implying not all patients who needed intensive post-injury rehabilitation were granted access. Reasons for this low utilization remain unclear but may be related to current fee-for-service models that disincentivize the use of this expensive resource. Conversely, the highest-utilizer hospital quintile had a discharge rate of 30% in the non-elderly adult cohort and 46% in the older adult cohort. This raises the concern that there may be hospitals that overuse IRFs resulting in unnecessary financial expenditures and inappropriate allocation of resources. Behaviors at both extremes have important implications for health care reform and quality of patient care.
Our results must be interpreted in light of the study’s limitations. First, although we show that unexplained hospital factors are key drivers in the disposition of the trauma patient, we cannot prove a causal relationship with observational data. Second, because we applied the “60% rule” as inclusion criteria for our study population, our results may not be completely generalizable to the whole trauma population. However, this population was purposefully chosen as it represents a cohort with an above average likelihood of needing post-discharge rehabilitation. Third, given the confines of the NTDB, we were not able determine IRF referral appropriateness or control for all patient and hospital-level factors such as variables for social support and hospital ownership of a PAC facility, but the current exploratory analysis can be used to help identify targets for subsequent in-depth inquiry. Finally, use of registry data may generate discrepancy related to coding of the severity of clinical characteristics as well as discharge destination. However, our sensitivity analysis showed that regardless of the definition of PAC facility type, hospital factors still explain a large portion of variation.
In summary, our data suggest discharge to IRF is substantially driven by the hospital at which a trauma patient receives their care. Further studies are needed to identify these unexplained hospital factors in order to optimize equity of access, value, and quality of care. Post-injury rehabilitation at an IRF is an expensive and scarce resource and every effort must be made to make sure the proper patients have access.
Supplementary Material
eFigure 1. Participant flow diagram
Abbreviations: National Trauma Data Bank (NTDB), Injury severity score (ISS), Centers for Medicare & Medicaid Services (CMS)
eFigure 2. Risk- and reliability-adjusted hospital rates of discharge to inpatient rehabilitation. Risk- and reliability-adjusted rates of discharge to any PAC facility including inpatient rehabilitation facility, skilled nursing facility, intermediate care facilities, and long-term care hospital in A) non-elderly adults and B) older adults
eFigure 3: Partitioned Variance. Variance partitioning coefficients (VPC) of random hospital effect, hospital factors, patient insurance, patient demographics, patient injury traits, and patient insurance. The VPC ranges from 0 to 1 and is a proportion measuring the contribution towards the total variation in discharge to any PAC facility (inpatient rehabilitation facility, skilled nursing facility, intermediate care facilities, and long-term care hospital) from each set of variables.
Funding:
Alisha Lussiez is supported by the Surgical Oncology Scientist Fellowship Award administered from the National Cancer Institute T32CA009672. John R. Montgomery is supported by the Obesity Surgery Scientist Fellowship Award administered from the National Institute of Diabetes and Digestive and Kidney Diseases T32-DK108740. Mark R. Hemmila receives salary support from Blue Cross Blue Shield of Michigan/Blue Care Network (a nonprofit mutual company) and the Michigan Department of Health and Human Services through grant funding of the Michigan Trauma Quality Improvement Program.
Footnotes
Disclosures statement: Dr. Justin Dimick reported receiving personal fees from ArborMetrix, Inc outside the submitted work.
Conference presentations: This work was presented at the 2020 American College of Surgeon’s clinical congress
References
- 1.Sultana I, Erraguntla M, Kum HC, Delen D, Lawley M. Post-acute care referral in United States of America: a multiregional study of factors associated with referral destination in a cohort of patients with coronary artery bypass graft or valve replacement. BMC Med Inform Decis Mak. 2019;19(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nehra D, Nixon ZA, Lengenfelder C, Bulger EM, Cuschieri J, Maier RV, Arbabi S. Acute Rehabilitation after Trauma: Does it Really Matter? J Am Coll Surg. 2016;223(6):755–763. [DOI] [PubMed] [Google Scholar]
- 3.Zogg CK, Scott JW, Metcalfe D, Gluck AR, Curfman GD, Davis KA, Dimick JB, Haider AH. Association of Medicaid Expansion with Access to Rehabilitative Care in Adult Trauma Patients. JAMA Surg. 2019;154(5):402–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scott JW, Neiman PU, Uribe-Leitz T, Scott KW, Zogg CK, Salim A, Haider AH. Impact of Affordable Care Act-related insurance expansion policies on mortality and access to post-discharge care for trauma patients: An analysis of the National Trauma Data Bank. J Trauma Acute Care Surg. 2019;86(2):196–205. [DOI] [PubMed] [Google Scholar]
- 5.Sacks GD, Hill C, Rogers SO. Insurance status and hospital discharge disposition after trauma: Inequities in access to postacute care. J Trauma - Inj Infect Crit Care. 2011;71(4):1011–1015. [DOI] [PubMed] [Google Scholar]
- 6.Pack QR, Squires RW, Lopez-Jimenez F, Lichtman SW, Rodriguez-Escudero JP, Zysek VN, Thomas RJ. The current and potential capacity for cardiac rehabilitation utilization in the united states. J Cardiopulm Rehabil Prev. 2014;34(5):318–326. [DOI] [PubMed] [Google Scholar]
- 7.Kamenov K, Mills JA, Chatterji S, Cieza A. Needs and unmet needs for rehabilitation services: a scoping review. Disabil Rehabil. 2019;41(10):1227–1237. [DOI] [PubMed] [Google Scholar]
- 8.Mechanic R Post-acute care - The next frontier for controlling medicare spending. N Engl J Med. 2014;370(8):692–694. [DOI] [PubMed] [Google Scholar]
- 9.Werner RM, Coe NB, Qi M, Konetzka RT. Patient Outcomes after Hospital Discharge to Home with Home Health Care vs to a Skilled Nursing Facility. JAMA Intern Med. 2019;179(5):617–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sacks GD, Lawson EH, Dawes AJ, Weiss RE, Russell MM, Brook RH, Zingmond DS, Ko CY. Variation in hospital use of postacute care after surgery and the association with care quality. Med Care. 2016;54(2):172–179. [DOI] [PubMed] [Google Scholar]
- 11.Montgomery JR, Cain-Nielsen AH, Jenkins PC, Regenbogen SE, Hemmila MR. Prevalence and Payments for Traumatic Injury Compared with Common Acute Diseases by Episode of Care in Medicare Beneficiaries, 2008–2014. JAMA - J Am Med Assoc. 2019;321(21):2129–2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chandra A, Dalton M, Holmes J Large Increases In Spending On Postacute Care In Medicare Point To The Potential For Cost Savings In These Settings. Heal Aff. 2013;32(5):864–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abdelsattar ZM, Gonzalez AA, Hendren S, Regenbogen SE, Wong SL. Hospital Ownership of a Postacute Care Facility Influences Discharge Destinations after Emergent Surgery. Ann Surg. 2016;264(2):291–296. [DOI] [PubMed] [Google Scholar]
- 14.Kanters AE, Nikolian VC, Kamdar NS, Regenbogen SE, Hendren SK, Suwanabol PA. Academic hospitals discharge fewer patients to postacute care facilities after colorectal resection. Dis Colon Rectum. 2019;62(4):483–490. [DOI] [PubMed] [Google Scholar]
- 15.Balentine CJ, Mason MC, Richardson PJ, Kougias P, Bakaeen F, Naik AD, Berger DH, Anaya DA. Variation in postacute care utilization after complex surgery. J Surg Res. 2018;230:61–70. [DOI] [PubMed] [Google Scholar]
- 16.Balentine CJ, Naik AD, Robinson CN, Petersen NJ, Chen GJ, Berger DH, Anaya DA. Association of high-volume hospitals with greater likelihood of discharge to home following colorectal surgery. JAMA Surg. 2014;149(3):244–251. [DOI] [PubMed] [Google Scholar]
- 17.Buntin MB, Garten AD, Paddock S, Saliba D, Totten M, Escarce JJ. How much is postacute care use affected by its availability? Health Serv Res. 2005;40(2):413–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davidson GH, Hamlat CA, Rivara FP, Koepsell TD, Jurkovich GJ, Arbabi S. Long-term survival of adult trauma patients. JAMA - J Am Med Assoc. 2011;305(10):1001–1007. [DOI] [PubMed] [Google Scholar]
- 19.Medicare Payment Advisory Commission (MEDPAC). Inpatient rehabilitation facility services. 2012;(March):Chapter 9. [Google Scholar]
- 20.Hashmi ZG, Kaji AH, Nathens AB. Practical guide to surgical data sets: National Trauma Data Bank (NTDB). JAMA Surg. 2018;153(9):852–853. [DOI] [PubMed] [Google Scholar]
- 21.Hamidi M, Zeeshan M, Leon-Risemberg V, Nikolich-Zugich J, Hanna K, Kulvatunyou N, Saljuqi AT, Fain M, Joseph B. Frailty as a prognostic factor for the critically ill older adult trauma patients. Am J Surg. 2019;218(3):484–489. [DOI] [PubMed] [Google Scholar]
- 22.Fingerhut L External Cause of Injury Mortality Matrix for ICD-10. Published online2002.
- 23.Montoya KF, Charry JD, Calle-Toro JS, Núñez LR, Poveda G. Shock index as a mortality predictor in patients with acute polytrauma. J Acute Dis. 2015;4(3):202–204. [Google Scholar]
- 24.Dimick JB, Staiger DO, Birkmeyer JD. Ranking hospitals on surgical mortality: The importance of reliability adjustment. Health Serv Res. 2010;45(6 PART 1):1614–1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wynants L, Timmerman D, Bourne T, Van Huffel S, Van Calster B. Screening for data clustering in multicenter studies: The residual intraclass correlation. BMC Med Res Methodol. 2013;13(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Englum BR, Villegas C, Bolorunduro O, Haut ER, Cornwell III EE, Efron DT, Haider AH. Racial, ethnic, and insurance status disparities in use of posthospitalization care after trauma. J Am Coll Surg. 2011;213(6):699–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chun Fat S, Herrera-Escobar JP, Seshadri AJ, Al Rafai SS, Hashmi ZG, de Jager E, Velmahos C, Kasotakis G, Velmahos G, Salim A, et al. Racial disparities in post-discharge healthcare utilization after trauma. Am J Surg. 2019;218(5):842–846. [DOI] [PubMed] [Google Scholar]
- 28.Khorgami Z, Ewing KL, Mushtaq N, Chow GS, Howard CA. Predictors of discharge destination in patients with major traumatic injury: Analysis of Oklahoma Trauma Registry. Am J Surg. 2019;218(3):496–500. [DOI] [PubMed] [Google Scholar]
- 29.Chan L, Doctor J, Temkin N, MacLehose RF, Esselman P, Bell K, Dikmen S. Discharge disposition from acute care after traumatic brain injury: The effect of insurance type. Arch Phys Med Rehabil. 2001;82(9):1151–1154. [DOI] [PubMed] [Google Scholar]
- 30.Loberg JA, Hayward RD, Fessler M, Edhayan E. Associations of race, mechanism of injury, and neighborhood poverty with in-hospital mortality from trauma. Medicine (Baltimore). 2018;97(39):e12606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carroll NW, Hearld LR, Joseph R. Hospital ownership of postacute care providers and the cost of care. Health Care Manage Rev. 2020;45(4):E35–E44. [DOI] [PubMed] [Google Scholar]
- 32.Makam AN, Nguyen OK, Xuan L, Miller ME, Goodwin JS, Halm EA. Factors associated with variation in long-term acute care hospital vs skilled nursing facility use among hospitalized older adults. JAMA Intern Med. 2018;178(3):399–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Participant flow diagram
Abbreviations: National Trauma Data Bank (NTDB), Injury severity score (ISS), Centers for Medicare & Medicaid Services (CMS)
eFigure 2. Risk- and reliability-adjusted hospital rates of discharge to inpatient rehabilitation. Risk- and reliability-adjusted rates of discharge to any PAC facility including inpatient rehabilitation facility, skilled nursing facility, intermediate care facilities, and long-term care hospital in A) non-elderly adults and B) older adults
eFigure 3: Partitioned Variance. Variance partitioning coefficients (VPC) of random hospital effect, hospital factors, patient insurance, patient demographics, patient injury traits, and patient insurance. The VPC ranges from 0 to 1 and is a proportion measuring the contribution towards the total variation in discharge to any PAC facility (inpatient rehabilitation facility, skilled nursing facility, intermediate care facilities, and long-term care hospital) from each set of variables.


