Abstract
Objectives
From the beginning of the COVID-19 pandemic, clinical practice and research globally have centred on the prevention of transmission and treatment of the disease. The pandemic has had a huge impact on the economy and stressed healthcare systems worldwide. The present study estimates disability-adjusted life years (DALYs), years of potential productive life lost (YPPLL) and cost of productivity lost (CPL) due to premature mortality and absenteeism secondary to COVID-19 in the state of Kerala, India.
Setting
Details on sociodemographics, incidence, death, quarantine, recovery time, etc were derived from public sources and the Collective for Open Data Distribution-Keralam. The working proportion for 5-year age–gender cohorts and the corresponding life expectancy were obtained from the 2011 Census of India.
Primary and secondary outcome measures
The impact of the disease was computed through model-based analysis on various age–gender cohorts. Sensitivity analysis was conducted by adjusting six variables across 21 scenarios. We present two estimates, one until 15 November 2020 and later updated to 10 June 2021.
Results
Severity of infection and mortality were higher among the older cohorts, with men being more susceptible than women in most subgroups. DALYs for males and females were 15 954.5 and 8638.4 until 15 November 2020, and 83 853.0 and 56 628.3 until 10 June 2021. The corresponding YPPLL were 1323.57 and 612.31 until 15 November 2020, and 6993.04 and 3811.57 until 10 June 2021, and the CPL (premature mortality) were 263 780 579.94 and 41 836 001.82 until 15 November 2020, and 1 419 557 903.76 and 278 275 495.29 until 10 June 2021.
Conclusions
Most of the COVID-19 burden was contributed by years of life lost. Losses due to YPPLL were reduced as the impact of COVID-19 infection was lesser among the productive cohorts. The CPL values for individuals aged 40–49 years old were the highest. These estimates provide the data necessary for policymakers to work on reducing the economic burden of COVID-19 in Kerala.
Keywords: COVID-19, health economics, health policy
Strengths and limitations of this study.
This is the first study to characterise the economic burden caused by COVID-19 in the state of Kerala using disability-adjusted life years, years of potential productive life lost and cost of productivity lost.
The study used publicly sourced data for analysis and presentation of results.
Exclusion of incidence of cases after 20 August 2020 due to data unavailability could lead to an underestimation of disability-adjusted life years.
Psychological impacts of mitigation strategies (eg, lockdown, travel restrictions, etc) that could increase mortality were not within the scope of the study.
Data on unpaid work and presenteeism and on postrecovery illness and the long-term effects of COVID-19 have not been considered.
Introduction
Since the first case of COVID-19 was reported in December 2019, COVID-19 has spread across all countries, infecting 176 705 044 people with 3 819 138 deaths and 160 737 654 recoveries worldwide as of 14 June 2021.1 Lower access to quality health facilities in low-income and middle-income countries has placed a sizeable proportion at higher risk.2 India ranks second with 29 507 438 cases and 28 148 977 recoveries as of 14 June 2021.1 Higher infection rates have increased the burden on healthcare systems and thus increased the fatality rate.3
Estimating mortality due to COVID-19 helps to understand the dynamics of the pandemic. The role of sociodemographics, social determinants, and geography is important to assess the differential risk levels to the disease with age, gender and geography.4 However, indirect effects due to morbidity and post-COVID-19 syndromes have highlighted the far-reaching consequences of the pandemic.5 Also, social determinants of health (SDH) often create inequalities between and within territories disproportionately, such as the losses incurred by the caregivers of the infected, front-line workers, food insecurity, work-life conditions, unemployment, etc, which have considerable impact on public and health systems.6 Governments have imposed strict measures to curtail the morbidity and mortality caused by COVID-19. Individual-level measures such as self-isolation and social distancing and population-level measures such as lockdowns are widely adopted to limit spread.2 7 8 SDH plays a vital role in strategising the interventions especially in Lower Middle Income Countries (LMIC), where there are differences in socioeconomic strata.6 Quantifying the health and economic impact of COVID-19 would be a reflection of the policy decisions taken.9 Economic impact assessment is highly important in countries/territories like India and states such as Kerala, where most of the infected people have recovered.
In India, the first case of COVID-19 was reported in Kerala on 30 January 2020. Timely interventions such as contact tracing, testing, quarantine, isolation and treatment had reduced the spread of the disease in Kerala.10 The number of cases in Kerala has now reached 2 728 239 with 11 181 deaths and 2 593 625 recoveries as of 13 June 2021. The resulting economic burden of COVID-19 in the state thus appears to be substantial. Therefore, the present study aimed to estimate the economic burden and productivity loss using disability-adjusted life years (DALYs), years of potential productive life lost (YPPLL) and cost of productivity lost (CPL) and their effects on age and gender in the state of Kerala.
Methods
Data collection
The present work is an age–gender cohort-based observational study designed to estimate DALYs and productivity losses due to COVID-19 in Kerala, India. The effect of multimorbidity was considered to estimate the burden of disease (BoD). The human capital approach was adopted to estimate productivity losses. Publicly available data from various sources were used to gather sociodemographic details, information on the incidence, death due to COVID-19, data on quarantine, per capita income, etc for the state of Kerala.11–13 The first reported case of COVID-19 in Kerala dates back to 30 January 2020, from when the estimates for the present study have been collected.12 13
The 5-year age–gender population of Kerala, the working population in each age–gender cohort and the corresponding life expectancies were obtained from the 2011 Census of India.11 Incidence data documented by Team Collective for Open Data Distribution-Keralam (CODD-K) until 20 August 2020 were used to classify the incidence of the age–gender cohorts (online supplemental table SI). Out of 52 199 reported cases until 20 August 2020, data on 7645 patients were excluded as they did not have information on age and gender.12 Recovery time documented by the team from CODD-K for 1012 patients in Kerala was used.12 Data on the number of deaths were extracted from the Government of Kerala dashboard and CODD-K.12 13 Infections were categorised as mild, moderate and severe/critical.13 14 Further, estimates updated until 2021 are also presented throughout, all of which will hereon be indicated using subscript ‘2021’. Table 1 presents the data on various parameters used in the study.
Table 1.
Parameters used in the study
| Parameters | Value | Sensitivity analysis* | Reference | End date | |
| Number of cases | 10% (S12), 20% (S13) and 30% (S14) increase in infected cases | 3 12 | 20 August 2020 | ||
| Actual | 52 199 | ||||
| Valid records | 44 554 | ||||
| Number of deaths | 10% (S18), 20% (S19) and 30% (S20) increase in deaths | 3 12 13 | 10 June 2021 | ||
| Actual | 1869 | ||||
| Valid records | 1841 | ||||
| Quarantine | 10% (S15), 20% (S16) and 30% (S17) increase in mild cases | 12 13 | 29 August 2020 | ||
| Home (mild cases) | 158 543 | ||||
| Hospital | 14 646 | – | |||
| Severity (%) | 14 | NA | |||
| Moderate | 80 | ||||
| Severe/critical | 20 | ||||
| Disability weights (average: S3, S4, S5) (lower: S6, S7, S8; upper: S9, S10, S11): three methods of disability weight calculation in each case (online supplemental table SII) | 3 29–31 | NA | |||
| Whooping cough | 0.051 | (0.032, 0.074) | |||
| Severe paratyphoid fever | 0.133 | (0.088, 0.19) | |||
| Asthma | 0.043 | (0.036, 0.05) | |||
| Moderate iron deficiency anaemia | 0.052 | (0.034, 0.076) | |||
| Mild diarrhoeal diseases | 0.074 | (0.049, 0.104) | |||
| Mild symptomatic peptic ulcer disease without anaemia | 0.011 | (0.005, 0.021) | |||
| Pharyngitis | 0.070 | (0.07, 0.07) | |||
| Symptomatic tension-type headache | 0.037 | (0.022, 0.057) | |||
| Moderate angina due to ischaemic heart disease | 0.080 | (0.052, 0.113) | |||
| Moderate symptomatic peptic ulcer disease with mild anaemia | 0.118 | (0.081, 0.163) | |||
| Other moderate mental disorders | 0.133 | (0.091, 0.186) | |||
| Life expectancy for age–gender cohort | 25% (S1) and 50% (S2) decrease | 3 11 | NA | ||
| Burden of isolation after discharge/recovery | 0 | 2-week isolation (S21) | 3 | NA | |
| Recovery time for age–gender cohort (duration of disability) | 12 | Available for 1012 patients | |||
| Age group | Time to recovery (days) | Age group | Time to recovery (days) | ||
| 0–1 | 13.00 | 45 to 50 | 13.49 | ||
| 1–5 | 17.55 | 50 to 55 | 15.55 | ||
| 5–10 | 14.40 | 55 to 60 | 13.57 | ||
| 10–15 | 15.59 | 60 to 65 | 13.61 | ||
| 15–20 | 13.94 | 65 to 70 | 18.94 | ||
| 20–25 | 13.82 | 70 to 75 | 15.00 | ||
| 25–30 | 13.16 | 75 to 80 | 11.57 | ||
| 30–35 | 14.07 | 80 to 85 | 15.00 | ||
| 35–40 | 13.54 | 85+ | 17.33 | ||
| 40–45 | 15.26 | ||||
| Life expectancy at age of death (L) | 11 | NA | |||
| Age | Male | Female | |||
| 0–1 | 72.5 | 77.9 | |||
| 1–5 | 72.3 | 77.8 | |||
| 5–10 | 68.4 | 73.9 | |||
| 10–15 | 63.4 | 69.0 | |||
| 15–20 | 58.6 | 64.1 | |||
| 20–25 | 53.7 | 59.2 | |||
| 25–30 | 48.9 | 54.4 | |||
| 30–35 | 44.2 | 49.5 | |||
| 35–40 | 39.5 | 44.7 | |||
| 40–45 | 34.8 | 39.9 | |||
| 45–50 | 30.3 | 35.1 | |||
| 50–55 | 25.9 | 30.5 | |||
| 55–60 | 21.8 | 26.2 | |||
| 60–65 | 17.9 | 21.9 | |||
| 65–70 | 14.3 | 17.9 | |||
| 70–75 | 11.4 | 14.3 | |||
| 75–80 | 8.6 | 11.0 | |||
| 80–85 | 6.2 | 7.9 | |||
| 85+ | 4.5 | 5.6 | |||
| Discount rate for value of life (%) | 2.90 | – | 17 | NA | |
| Age–gender population | Online supplemental table SIII | – | 11 | NA | |
| Age–gender working population | |||||
| Discount rate (financial benchmark) (%) | 4.25 | – | 24 | 6 November 2020 | |
| Stay in intensive care unit (days) | 8 | – | 26 27 | NA | |
| Retirement age in Kerala (years) | 56 | – | 22 | NA | |
| Number of working days in a week | 6 | – | 45 | NA | |
| Per capita gross domestic product in Kerala | 221 904 rupees/year | – | 46 | 2020 | |
*Scenarios for the sensitivity analysis have been denoted by S1–S21. A detailed description is provided in online supplemental table SIV.
NA, not applicable.
bmjopen-2021-049619supp001.pdf (90.4KB, pdf)
Estimation of the distribution of cases until 10 June 2021
The distribution of cases for age–gender cohorts in Kerala in 2020 and in India in 2020 and 2021 was used to estimate the distribution of cases in Kerala until 10 June 2021 (online supplemental table SI). The rationale behind the method is that the percentage deviations in the distribution of cases for each age–gender cohort in India then (2020) and now (2021) and those of Kerala are assumed to be the same. In this way, the distribution of cases for age–gender cohorts was computed until 10 June 2021 (online supplemental table SV). The actual number of cases in Kerala as of 10 June 2021 is 2 688 590, while our estimates cumulate to 2 688 516, with an error of 0.0028%.
Disability-adjusted life years
DALYs are standard measures to estimate the BoD in public health and are calculated as the sum of years lived with disability (YLD) and years of life lost (YLL).3 9 15 DALYs take into account the disability caused by the disease (YLD) and the premature mortality (YLL).9 Determining YLLs, YLDs and DALYs would allow us to measure the shortfall of the deceased and life years lost. YLLs explain the loss incurred as a result of death due to an event by comparing it with the years that they would have lived otherwise. YLLs become high in case of either higher mortality or mortality of younger people or both.4 YPPLL and CPL are widely adopted measures that mainly explain the economic burden due to an event.16
DALYs were calculated using an incidence-based approach.3 17 DALY estimates were obtained for the age–gender split to identify the more vulnerable groups.9 Although incidence-based approaches do not consider the severity of diseases, due to the diverse impact of COVID-19, severity was considered to assign the disability weight (DW).3 Initial estimates of YLDs are presented only until 20 August 2020, and the DALY estimates in this study are certainly an underestimation. However, YLDs contribute only a minor share to the DALY estimates.3 9 18 Discounting for the value of life (discount rate of 2.9%) was used in the calculation of DALYs.17 DALYs with no discounting are also presented in table 2. DWs were chosen based on the symptoms experienced by patients and varied based on the severity of infection. The proportion of home quarantine cases was considered to be mild, while the proportion of hospitalised cases was further split into moderate and critical (table 1). The symptoms, the proportion of people experiencing each symptom and the corresponding DWs are presented in online supplemental table SII.19
Table 2.
DALY estimates for the baseline scenario (scenario 3)
| Age | DALYs until 15 November 2020 | DALYs until 10 June 2021 | ||||||
| Discounted | Undiscounted | Discounted | Undiscounted | |||||
| Male | Female | Male | Female | Male | Female | Male | Female | |
| 0–1 | 30.3 | 61.8 | 72.6 | 155.9 | 63.7 | 64.8 | 145.1 | 155.9 |
| 1–5 | 0.4 | 0.4 | 0.4 | 0.4 | 50.7 | 19.7 | 72.7 | 0.4 |
| 5–10 | 0.3 | 0.3 | 0.3 | 0.3 | 47.4 | 15.5 | 68.7 | 0.3 |
| 10–15 | 58.4 | 30.1 | 127.2 | 69.3 | 114.1 | 80.5 | 190.6 | 138.3 |
| 15–20 | 57.0 | 58.6 | 117.8 | 128.6 | 265.0 | 200.8 | 469.4 | 385.0 |
| 20–25 | 137.3 | 113.8 | 269.7 | 237.5 | 590.7 | 465.0 | 1021.5 | 888.7 |
| 25–30 | 262.7 | 192.2 | 490.4 | 381.4 | 893.3 | 639.8 | 1517.3 | 1197.4 |
| 30–35 | 126.0 | 132.0 | 222.4 | 248.1 | 1583.7 | 1168.2 | 2653.4 | 2129.1 |
| 35–40 | 636.2 | 351.3 | 1067.8 | 626.3 | 3581.9 | 1862.3 | 5886.8 | 3263.6 |
| 40–45 | 899.7 | 189.7 | 1428.1 | 319.8 | 5050.7 | 2306.4 | 7900.9 | 3831.0 |
| 45–50 | 1150.2 | 507.0 | 1728.1 | 807.8 | 6874.1 | 4193.9 | 10 242.4 | 6634.4 |
| 50–55 | 1603.7 | 952.0 | 2280.2 | 1434.0 | 9240.0 | 5943.5 | 13 054.6 | 8906.5 |
| 55–60 | 2343.5 | 1413.5 | 3161.6 | 2017.8 | 11 231.3 | 8078.1 | 15 108.0 | 11 502.2 |
| 60–65 | 2639.5 | 1426.8 | 3383.5 | 1927.5 | 13 502.1 | 8690.6 | 17 273.9 | 11 716.8 |
| 65–70 | 2610.8 | 1089.5 | 3189.4 | 1396.5 | 11 711.3 | 7826.5 | 14 271.9 | 10 006.4 |
| 70–75 | 1669.8 | 983.4 | 1961.0 | 1201.3 | 9513.7 | 6775.0 | 11 160.8 | 8265.5 |
| 75–80 | 898.2 | 508.6 | 1014.8 | 594.0 | 5201.8 | 4080.8 | 5873.8 | 4763.0 |
| 80–85 | 556.2 | 430.7 | 607.6 | 482.0 | 2908.8 | 2637.2 | 3174.4 | 2946.8 |
| 85+ | 274.3 | 196.5 | 292.5 | 212.8 | 1428.5 | 1579.8 | 1521.0 | 1708.0 |
| Total | 15 954.5 | 8638.4 | 21 415.5 | 12 241.5 | 83 853.0 | 56 628.3 | 111 607.3 | 78 439.5 |
DALYs, disability-adjusted life years.
| (1) |
where r=discount rate; D=disability duration (years); and I=number of incident cases.
| (2) |
where L=life expectancy at age of death (years) and n=number of deaths.
| (3) |
Most of the BoD studies do not consider multimorbidity, which might yield inaccurate estimates.15 Three methods for calculation of combined disability weights (CDW) for multimorbidity as reported by Hilderink et al,15 viz additive, multiplicative and maximum limit methods, were employed in this study.
| (4) |
| (5) |
| (6) |
where ‘i’ and ‘j’ indicate the DWs of ‘i’th and ‘j’th disabilities.
Productivity losses (YPPLL and CPL)
YPPLL is defined as the number of productive years an average person would have lived otherwise. The working population proportion of each cohort was multiplied with the YPPLL to estimate the CPL lost due to morbidity and absenteeism. Recovery days for the severe cases were extended by 8 days to account for intensive care unit (ICU) stay. Productivity losses were estimated using the human capital approach considering absenteeism and premature mortality for temporary and permanent losses, respectively.9 20 For calculation of productivity losses, people from the age group 15–60 were chosen considering the employment age21 and retirement age in Kerala.22 17 23
| (7) |
where ‘i’ represents ‘n’ age–gender cohorts; Di=deaths at age; wi=productive years remaining at age of death (years); and d=discount rate for the value of life as proposed by the Reserve Bank of India.24 These are applicable for every year excluding the first year.25 CPL for premature mortality and absenteeism was computed as shown in Eqn. (8) and (9).
| (8) |
| (9) |
where S=average salary per day considering the number of paid working days per week as six; Lj=average recovery time; n=number of incident cases; and P=proportion of the working population, in cohort ‘j’. For the computation of productivity losses, the proportion of the working population was considered along with an extended disability period for severe cases to account for ICU stay.26 27
Sensitivity analysis
A spectrum of scenarios (online supplemental table SIV) were considered to analyse the effect of each parameter on the DALY estimates. The key idea of performing sensitivity analysis is to assist policymakers in anticipating the effects brought in by each of the driving variables. As most of the deceased cases had underlying health conditions that reduce the life expectancy, scenario 1 and scenario 2 have been developed.4 28 Increasing the number of mild cases, overall cases and deaths is a conservative analysis to help the healthcare fraternity and policymakers.3
Validation
To ensure credibility, data related to COVID-19 (table 1) were collected from various official sources, reports and published works.3 11–14 26 27 29–31 Discount rates for the financial benchmark and the value of life were taken into account based on the values defined by the Reserve Bank of India24 and Shanmugam,17 respectively. For the computation of DALY, three different approaches to calculate the CDW as mentioned by Hilderink et al15 were used. The DALY estimates and productivity losses were computed as done by Wyper et al32 and Rumisha et al.33
Patient and public involvement
The data used for inputs and analysis were derived from public sources (such as websites) and published literature. Our research question for estimating the economic burden and productivity losses in Kerala was based on the increase in the number of cases in Kerala from July to November 2020. The increase in the number of cases would also mean increased productivity losses due to COVID-19 for patients and their family members, especially those who died or were hospitalised. However, as our model-based analysis used data from published sources such as publications, websites and modelling methods, patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of the research.
Cohort description
From July 2020 to June 2021 there was a significant increase in the number of COVID-19 cases in Kerala. The increase in the number of cases would also mean increased economic loss due to COVID-19 for patients and their family members, mainly due to the increase in hospitalisations and deaths. We did not involve any patients in the design of this study as we used publicly available sources. However, we aim to disseminate the findings of this paper through various media channels postpublication to reach out to policymakers and the general public in the state of Kerala.
Results
From the distribution of cases and deaths (online supplemental figure S1, until 15 November 2020; online supplemental figure S2, until 10 June 2021), it is clear that older adults are disproportionately vulnerable to being severely affected by the disease. Although the 25–30 age group of men and women accounts for 13.45% and 11.06% of the total number of cases, their proportionate mortality remains as low as 0.80% and 1.17%, respectively (online supplemental figure S1). Contrastingly, while the male and female proportion of cases for the age group 65–70 is only 2.11% and 2.75% of the overall cases, their proportionate mortality remains as high as 17.88% and 13.13%, respectively (online supplemental figure S1). The 2021 estimates confirm that the elderly people from the age group 55–70 (online supplemental figure S2) are greatly affected as their proportionate mortality is 39.99%, although their proportionate incidence is as low as 12.34%.
bmjopen-2021-049619supp002.pdf (612.2KB, pdf)
DALY estimates calculated using the average DW scores using the additive method were considered as the baseline scenario for sensitivity analysis. From online supplemental table SVI, it is clear that the YLL accounts for the major proportion of DALYs (discounted), with male and female YLL and YLL2021 in the age group 60–65 cumulating to 16.58%–16.46% and 16.21%–15.43%, respectively. Since the cohort does not fall into the productive population (considering the employment age), these might not impact productivity losses. Considering the YLLs and DALYs in the productive population, the YLLs and DALYs of men and women are the highest for the age group 55–60. Comparing the discounted and undiscounted DALYs, we see that the undiscounted DALY and DALY2021 of males and females are 36.02% and 44.15% and 33.1% and 38.52% higher than those of the discounted ones. The discount rate for the value of life was considered as 2.90% for all the scenarios in the study.17 Also, DALYs per million and DALY2021 per million were estimated to be 709.2 and 4050.99 based on the projected population of Kerala for the year 2020, which is 34 678 294.34
Online supplemental figure S3A–I and online supplemental figure S4A–I show that overall the DALYs for males are higher than those for females, except for the age groups 30–35, 15–20 and those less than 10. About 47.69% and 45.34% of overall DALYs and 43.46% and 43.43% of the overall DALY2021 for males and females, respectively, are from the age group 55–70. It is highly disproportionate as the number of cases from this age group piles up to only 11.13% and 13.11% (2020) and 11.32% and 13.37% (2021) of cases for men and women, respectively. Online supplemental figures S3 and S4 present the DALYs calculated for the nine different scenarios (refer to online supplemental table SII) that involve altering the DW calculation methods and values.
To measure the impact of the disease on the productivity of the state, YPPLL and CPL were calculated among the productive age group of 15–60 years. The age group 25–49 being the majority is the prime contributor to productivity. Fortunately, the infection has a relatively lesser impact in terms of duration of illness and mortality on this age group, which has reduced the losses to some extent (table 3). Recovery days mentioned in online supplemental table SIII are exclusive of the ICU stay of severe cases.
Table 3.
YPPLL and CPL (mortality and absenteeism) until 15 November 2020
| Age group | YPPLL | CPL: death | CPL: morbidity | |||
| Male | Female | Male | Female | Male | Female | |
| 15–19 | 8.02 | 16.04 | 200 004.28 | 144 074.81 | 1 308 538.75 | 325 006.38 |
| 20–24 | 43.05 | 25.83 | 5 009 096.46 | 849 735.38 | 13 824 381.71 | 2 252 069.57 |
| 25–29 | 81.38 | 54.25 | 15 385 047.11 | 2 675 078.71 | 28 999 248.30 | 3 130 470.52 |
| 30–34 | 46.07 | 46.07 | 9 543 101.81 | 2 934 692.41 | 32 044 805.25 | 4 055 127.61 |
| 35–39 | 197.61 | 107.79 | 41 717 765.16 | 8 623 040.56 | 28 976 931.25 | 4 149 430.14 |
| 40–49 | 646.28 | 215.43 | 135 448 141.17 | 17 470 735.95 | 48 999 357.83 | 9 131 773.54 |
| 50–59 | 301.17 | 146.91 | 56 477 423.96 | 9 138 644.00 | 30 872 800.27 | 6 134 611.07 |
| Total | 263 780 579.94 | 41 836 001.82 | 185 026 063.37 | 29 178 488.82 | ||
CPL, cost of productivity lost; YPPLL, years of potential productive life lost.
Table 3 shows that the CPL values for people aged 40–49 years were the highest and constituted about 51.34% and 41.76% of the total CPL values (for premature mortality) for men and women, respectively. CPL values for absenteeism are also highest for the same age cohort for both men and women, accounting for up to 26.53% and 31.35%, respectively. CPL2021 (for premature mortality) gets the highest shares of 58.98% and 58.73% from the male and female cohorts of the 41–50 age group (table 4). Similarly, CPL2021 has a maximum of 25.89% and 30.96% from the same cohorts, respectively.
Table 4.
YPPLL and CPL (mortality and absenteeism) until 10 June 2021
| Age group | YPPLL | CPL: death | CPL: morbidity | |||
| Male | Female | Male | Female | Male | Female | |
| 16–20 | 65.17 | 48.88 | 1 625 265.52 | 439 040.27 | 102 297 314.03 | 23 652 339.15 |
| 21–25 | 165.51 | 130.67 | 19 259 902.22 | 4 298 973.72 | 886 623 358.12 | 140 085 916.15 |
| 26–30 | 282.14 | 200.23 | 53 340 135.18 | 9 872 885.34 | 1 831 188 038.59 | 187 207 907.26 |
| 31–35 | 552.34 | 395.84 | 114 409 861.84 | 25 214 693.78 | 1 875 906 232.92 | 243 394 778.33 |
| 36–40 | 1321.80 | 647.59 | 279 048 434.48 | 51 808 021.93 | 1 788 669 340.39 | 262 987 085.64 |
| 41–50 | 3994.98 | 2015.17 | 837 278 167.58 | 163 427 668.31 | 2 860 063 434.24 | 541 756 862.03 |
| 51–59 | 611.09 | 373.19 | 114 596 136.95 | 23 214 211.95 | 1 703 001 999.97 | 350 660 556.84 |
| Total | 1 419 557 903.76 | 278 275 495.29 | 11 047 749 718.26 | 1 749 745 445.40 | ||
Refer to online supplemental table SVII for incidence and deaths.
CPL, cost of productivity lost; YPPLL, years of potential productive life lost.
Sensitivity analysis
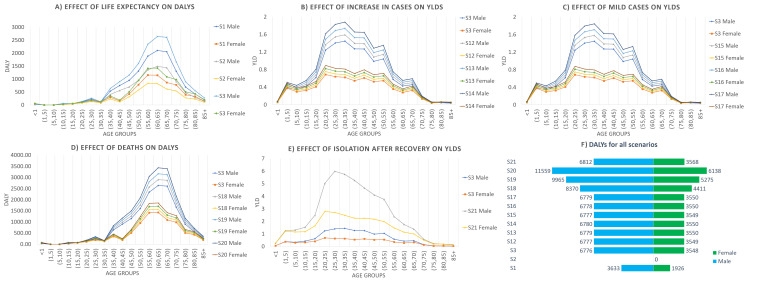
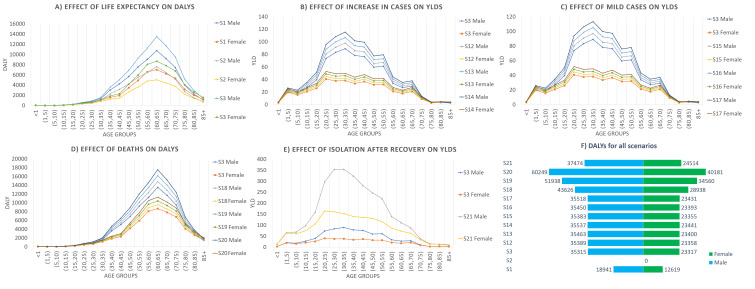
Figure 1A–F presents the sensitivity analysis explaining the role of each variable in economic burden to provide a better interpretation of the changes and comparison of the DALY estimates across all the scenarios for 2020. Figure 2A–F presents similar results for 2021 estimates. In figure 1A it is evident that the reduction in life expectancy by 25% and 50% reduced the DALYs by 19.7% and 42.47% for males and by 18.78% and 41.08% for females, respectively. Likewise, DALY2021 reduced by 19.53% and 42.11% for males and by 18.89% and 41.17% for females, respectively (figure 2A). In figure 1B, C, E and figure 2B, C, E, only YLD values were compared as the variables adjusted in these scenarios do not alter the YLLs. Comparing the DALY estimates might not explain the effect of the variables clearly. In figure 1A, D and figure 2A, D, the DALY estimates were directly compared. Increasing the overall cases by 10%, 20% and 30% increased the YLDs proportionately equal to the percentage increase in the number of cases. An increase in the mild cases by 10%, 20% and 30% increased the YLDs by 9.15%, 18.31% and 27.46%, respectively, for both the male and female cohorts. An increase in deaths by 10%, 20% and 30% increased the DALYs by 9.91%, 19.91% and 29.9%, respectively, for both the male and female cohorts. The increase in the burden of isolation of 2 weeks increased the YLDs from 12.24 to 48.01 for males and from 6.88 to 26.74 for females, and YLD2021 from 738.82 to 2897.92 for males and from 414.90 to 1612.10 for females.
Figure 1.
Sensitivity analysis (15 November 2020): (A) effect of life expectancy on DALYs; (B) effect of increase in cases on YLDs; (C) effect of mild cases on YLDs; (D) effect of deaths on DALYs; (E) effect of isolation after recovery on YLDs; and (F) DALYs for all scenarios. DALYs, disability-adjusted life years; YLDs, years lived with disability.
Figure 2.
Sensitivity analysis (10 June 2021): (A) effect of life expectancy on DALYs; (B) effect of increase in cases on YLDs; (C) effect of mild cases on YLDs; (D) effect of deaths on DALYs; (E) effect of isolation after recovery on YLDs; and (F) DALYs for all scenarios. DALYs, disability-adjusted life years; YLDs, years lived with disability.
Three different approaches for the average, lower and upper limit values of DW were used to arrive at YLDs. DALYs are seen to be the highest when the number of deaths is altered. DALYs increase by 29.9% from that of scenario 3 for both cohorts when the number of deaths increases by 30%. These values would still be higher if mortality among the younger cohorts is high due to their longer life expectancy during the age of death.
Discussion
Main findings of this study
In this study, for the baseline scenario, the YLLs were 15 942.3 and 8631.6 and the YLDs were 12.2 and 6.9 for males and females. Also, YLL2021 were 83 114.1 and 56 213.4 and YLD2021 were 738.8 and 414.9 for males and females. DALYs and DALY2021 were estimated as 709.2 per million and 4050.99 per million population based on the year 2020 population projections.34 However, the DALY estimates will be impacted by the quality of the data reported. Based on an article published by the British Broadcasting Corporation (BBC), the number of deaths due to COVID-19 as estimated by the volunteers is 3356, which is 70.44% higher than the officially reported count of 1969 as of 19 November 2020.13 35 Considering the effect of asymptomatic cases that act as latent spreaders, DWs due to presenteeism and unpaid work could increase the losses.36 These facts are concerning as the actual DALYs might be way higher than those estimated using official figures.
The DALY2021 estimates sum up to 83 853 and 56 628.3 for males and females, respectively, indicating a very high impact of the pandemic. YLL2021 were computed at 83 114.1 and 56 213.4 for males and females, while YLD2021 were only 738.8 and 414.9 for males and females. Reports state that the second wave has affected the younger population significantly, unlike the first. The distribution of cases among the age groups 21–30, 31–40 and 41–50 until 31 May 2021 was 261 232, 252 935 and 233 126 people, respectively. Also, 18% of the people who died in April and May 2021 in the state were not comorbid.37
In addition, the productivity losses in terms of YPPLL and CPL for mortality and absenteeism for the productive population (15–60 years of age) were estimated. Multimorbidity was taken into account in the calculation of CDW. CPL values (for premature mortality) for the younger population less than 25 years of age were just 1.97% and 2.37% for the male and female cohorts, respectively. Likewise, CPL2021 (premature mortality) for the same cohorts constitutes 1.47% and 1.70%, respectively. This is because of the lesser proportion of people working in this age group and also the lesser impact of the disease in terms of mortality. Considering the CPL due to absenteeism, the values for younger people less than 25 years of age were 8.16% and 8.83% for the male and female cohorts, respectively. A similar trend is observed in CPL2021 due to absenteeism, with 8.95% and 9.36% contribution from the male and female cohorts less than 25 years of age. This is higher compared with that of deaths due to a relatively lower proportion of people dying due to infection.
What is already known on this topic
Several researchers have been conducting research to estimate the economic burden and productivity losses of various diseases around the globe, such as the estimation of YLLs due to COVID-19 in the USA,4 India18 and Switzerland,7 DALYs due to COVID-19 in Korea3 and Italy,9 YPPLL due to cancer in Brazil, Russia, India, China and South Africa,38 YPPLL due to the five leading causes of deaths in Iran,16 productivity loss due to cardiovascular disease and mental illness in India,36 etc. COVID-19 has created a significant impact across the globe, some of which include 1.2 million YLLs in the USA from 1 February 2020 to 11 July 20204; 2 million YLL in India as of 17 October 202018; 1.75 million YLLs due to mass confinement of 3 months in Switzerland7; 2531 DALYs in Korea between 20 January 2020 and 24 April 2020, with YLLs and YLDs constituting 89.7% and 10.3%, respectively3; and 121 449 DALYs and productivity losses of €300 million and €100 million due to premature mortality and absenteeism, respectively, in Italy.9
What this study adds
As is evident from this study, the disease has impacted the older population to a greater extent. The proportion of cases for the age group 65–70 in Kerala is only 2.11% and 2.75% of the overall cases, while their deaths remain as high as 17.88% and 13.13%. Other studies reveal a similar trend of the disease, which provides strong insights into providing more care to the elderly. Indrayan and Mishra18 found that the relative incidence of the younger age group (<20) was only 1/3 (12:36)%, whereas those of adults aged more than 60 and between 50 and 59 were 1.5 (8:12)% and 1.88 (14.5:7.7)%, respectively.18 This trend prevails even outside the country, as Garg et al19 concluded that out of 1482 hospitalised patients from 1 March to 28 March 2020 across 14 states of the USA, 3/4 were aged 50 or more.
The age–gender cohort-based study aims to help policymaking in terms of protecting the most vulnerable population from infection. The positive relationship between the Case Fatality Rate (CFR) and the elderly population shows the importance to be accorded for strategies of distribution for both health infrastructure and vaccines, based on population distribution.39 There has been a steady drop in CFR in Kerala since the emergence of the disease,13 and although multiple variants of the virus have emerged improvements in health infrastructure and therapeutic efforts have been able to keep the CFR abated. This would also decrease the relative contribution of YLLs to the DALYs eventually. Strategies of governance have a vital role to play in curtailing the CFR, and are not limited to political stability, government effectiveness, regulatory quality and control of corruption, with rule of law and voice and accountability having a negative association with the latter.39
Sensitivity analysis has been vastly adopted by researchers to depict the influence of one or more variables on the outcome(s).3 4 A total of 21 scenarios by adjusting six variables were analysed in the study for the 2020 and 2021 estimates. The increase in the number of deaths greatly increased the DALYs, whereas the reduction in life expectancy reduced the DALYs. Reducing life expectancy could be related to the practical findings of the researchers. The majority of older patients have had underlying medical conditions such as pneumonia (68.8%), hypertension (34.4%), diabetes mellitus (50%) and chronic obstructive airway disease (15.6%),40 and 89.3% of older adults (65 or more) had comorbidities.19
Limitations of this study
Exclusion of incidence of cases post 20 August 2020 in the estimation of DALYs due to unavailability of open data has led to a certain underestimation. Also, the psychological impacts of the mitigation strategies are a potential risk that could increase mortality and are not within the scope of the present study.7 Most of the policies have not considered mental illness and allied problems.7 41 42 Although YLDs contribute a minor proportion to DALYs, including factors such as unpaid work and presenteeism might improve the accuracy. In Kerala, about 30% and 10% of recovered patients have experienced postrecovery illness and long-term effects, which have not been considered in the study, resulting in an underestimation of YLDs.43 Data on the number of deaths from Madhya Pradesh (MP), Andhra Pradesh (AP) and part of Tamilnadu indicate that these estimates could be possible under-reporting, and this might be the case for Kerala as well.44 The ‘excess deaths’ approach shows a clear spike in deaths. In May 2020, MP and AP reported 34 320 and 27 100 deaths, whereas deaths in May 2021 have reached 164 838 and 120 845. Not all of these could be directly attributed to COVID-19 as some relate to deaths due to shortage of oxygen and burden on hospitals.44
Conclusion
In conclusion, this is the first study to characterise the economic burden caused by COVID-19 in Kerala using DALYs, YPPLL and CPL. YLL contributed most to the disease burden due to COVID-19. Losses due to YPPLL were reduced as the impact of COVID-19 infection was relatively lesser among the productive age groups. People aged 40–49 years reported the highest CPL values. Decision-makers could use these estimates in order to focus and make efforts on reducing the economic burden and the longer impact of COVID-19 in Kerala.
The methodological framework used in this study can be applied to other states in India and other developing countries where disease notification data are collected by the government and are available in the public domain. Estimation of economic burden using DALYs, YPPLL and CPL attributable to COVID-19 in other states in India and other developing countries could provide the basis for interstate comparison and prioritisation of healthcare resources in resource-limited settings. Subgroup analysis would give deeper insights into the most vulnerable cohorts that require special attention in order to minimise the losses.
Supplementary Material
Acknowledgments
We like to sincerely thank Dr Geetha R Menon, Scientist E, ICMR-National Institute of Medical Statistics, New Delhi, for her comments towards improving this manuscript.
Footnotes
Twitter: @amibanerjee1
Contributors: Conception and design of the study, acquisition of data, or analysis and interpretation of data: DJ, NMS, JM. Drafting the article or revising it critically for important intellectual content: NMS, DJ, JM, JGR, AB. Final approval of the version to be submitted: JM, DJ, JGR, AB.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. All data are incorporated into the article and are openly available from the references mentioned.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study was conducted using publicly available data. No ethical approvals were sought for this study.
References
- 1.Worldometer . COVID-19 coronavirus pandemic, 2020. [Google Scholar]
- 2.Laxminarayan R, Wahl B, Dudala SR, et al. Epidemiology and transmission dynamics of COVID-19 in two Indian states. Science 2020;370:691–7. 10.1126/science.abd7672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jo MW, Go DS, Kim R, et al. The burden of disease due to COVID-19 in Korea using disability-adjusted life years. J Korean Med Sci 2020;35:1–10. 10.3346/jkms.2020.35.e199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Quast T, Andel R, Gregory S, et al. Years of life lost associated with COVID-19 deaths in the United States. J Public Health 2020;42:717–22. 10.1093/pubmed/fdaa159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Horton R. Offline: COVID-19 is not a pandemic. Lancet 2020;396:874. 10.1016/S0140-6736(20)32000-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO . WHO Coronavirus disease 2019 (COVID-19) Situation Report - 73, 2020: 1–13. [Google Scholar]
- 7.Moser DA, Glaus J, Frangou S, et al. Years of life lost due to the psychosocial consequences of COVID-19 mitigation strategies based on Swiss data. Eur Psychiatry 2020;63:e58. 10.1192/j.eurpsy.2020.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eubank S, Eckstrand I, Lewis B, et al. Commentary on Ferguson, et al., "Impact of Non-pharmaceutical Interventions (NPIs) to Reduce COVID-19 Mortality and Healthcare Demand". Bull Math Biol 2020;82:52. 10.1007/s11538-020-00726-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nurchis MC, Pascucci D, Sapienza M, et al. Impact of the burden of COVID-19 in Italy: results of disability-adjusted life years (dalys) and productivity loss. Int J Environ Res Public Health 2020;17:4233–12. 10.3390/ijerph17124233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Menon JC, Rakesh PS, John D, et al. What was right about Kerala's response to the COVID-19 pandemic? BMJ Glob Health 2020;5:e003212. 10.1136/bmjgh-2020-003212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Office of the Registrar General & Census Commissioner . Ministry of home Affairs, government of India, 2020. [Google Scholar]
- 12.Team CODD-K, 2020. Available: covid19kerala.info
- 13.C-DIT . GoK Dashboard | official Kerala COVID-19 statistics, 2020. [Google Scholar]
- 14.Aylward, Bruce (WHO); Liang W (PRC) . Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19, 2020. [Google Scholar]
- 15.Hilderink HBM, Plasmans MHD, Snijders BEP, et al. Accounting for multimorbidity can affect the estimation of the burden of disease: a comparison of approaches. Arch Public Health 2016;74:37. 10.1186/s13690-016-0147-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Najafi F, Karami-Matin B, Rezaei S, et al. Productivity costs and years of potential life lost associated with five leading causes of death: evidence from Iran (2006-2010). Med J Islam Repub Iran 2016;30:412. [PMC free article] [PubMed] [Google Scholar]
- 17.Shanmugam KR. Discount rate for health benefits and the value of life in India. Economics Research International 2011;2011:1–5. 10.1155/2011/191425 [DOI] [Google Scholar]
- 18.Indrayan A, Mishra A. Preliminary estimates of years of life lost (YLL) due to COVID-19 in India. medRxiv 2020:1–10. [Google Scholar]
- 19.Garg S, Kim L, Whitaker M, et al. Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 - COVID-NET, 14 States, March 1-30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:458–64. 10.15585/mmwr.mm6915e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kirch W, ed. Human Capital Approach, Encyclopedia of Public Health. Springer, Dordrecht, 2008. [Google Scholar]
- 21.India Development Gateway (InDG) . Child labour — Vikaspedia, 2020. [Google Scholar]
- 22.Kerala Kaumudi Online . Govt mulls extension of retirement age as it considers deferring salary cut plan - Kerala - General, 2020. [Google Scholar]
- 23.SISA Research paper. Quantitative Skills - Consultancy for Research and Statistics. Calculating the discounted YPLL - annotated.
- 24.Reserve bank of India. ratios and rates. © Reserv. bank India. all rights Reserv.
- 25.Michael FD, Mark JS, Karl C. Methods for the economic evaluation of health care programmes. Fourth Edi. Oxford, United Kingdom: Oxford University Press, 2015. [Google Scholar]
- 26.Phua J, Weng L, Ling L, et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med 2020;8:506–17. 10.1016/S2213-2600(20)30161-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rees EM, Nightingale ES, Jafari Y, et al. COVID-19 length of hospital stay: a systematic review and data synthesis. BMC Med 2020;18:270. 10.1186/s12916-020-01726-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hanlon P, Chadwick F, Shah A, et al. COVID-19 - exploring the implications of long-term condition type and extent of multimorbidity on years of life lost: a modelling study. Wellcome Open Res : 2020;5:75. 10.12688/wellcomeopenres.15849.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.GBD 2015 Mortality and Causes of Death Collaborators . Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the global burden of disease study 2015. Lancet 2016;388:1459–544. 10.1016/S0140-6736(16)31012-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Salomon JA, Haagsma JA, Davis A, et al. Disability weights for the global burden of disease 2013 study. Lancet Glob Health 2015;3:e712–23. 10.1016/S2214-109X(15)00069-8 [DOI] [PubMed] [Google Scholar]
- 31.Ock M, Lee JY, Oh IH, et al. Disability weights measurement for 228 causes of disease in the Korean burden of disease study 2012. J Korean Med Sci 2016;31 Suppl 2:S129–38. 10.3346/jkms.2016.31.S2.S129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wyper GMA, Assunção RMA, Colzani E, et al. Burden of disease methods: a guide to calculate COVID-19 Disability-Adjusted life years. Int J Public Health 2021;66:1–7. 10.3389/ijph.2021.619011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rumisha SF, George J, Bwana VM, et al. Years of potential life lost and productivity costs due to premature mortality from six priority diseases in Tanzania, 2006-2015. PLoS One 2020;15:e0234300. 10.1371/journal.pone.0234300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Census2011 . Kerala population sex ratio in Kerala literacy rate data, 2011-2020. [Google Scholar]
- 35.Biswas S. India coronavirus: How a group of volunteers ‘exposed’ hidden Covid-19 deaths - BBC News. BBC News Serv, 2020. [Google Scholar]
- 36.Fathima FN, Kahn JG, Krishnamachari S, et al. Productivity losses among individuals with common mental illness and comorbid cardiovascular disease in rural Karnataka, India. Int J Noncommun Dis 2019;4:86–92. 10.4103/jncd.jncd_17_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.The Hindu . Second wave impacted youth more: Minister - The Hindu, 2021. Available: https://www.thehindu.com/news/national/kerala/second-wave-impacted-youth-more-minister/article34754237.ece [Accessed 14 Jun 2021].
- 38.Pearce A, Sharp L, Hanly P, et al. Productivity losses due to premature mortality from cancer in Brazil, Russia, India, China, and South Africa (BRICS): a population-based comparison. Cancer Epidemiol 2018;53:27–34. 10.1016/j.canep.2017.12.013 [DOI] [PubMed] [Google Scholar]
- 39.Farzanegan MR, Feizi M, Gholipour HF. Globalization and the outbreak of COVID-19: an empirical analysis. JRFM 2021;14:105. 10.3390/jrfm14030105 [DOI] [Google Scholar]
- 40.Aggarwal A, Shrivastava A, Kumar A, et al. Clinical and epidemiological features of SARS-CoV-2 patients in SARI ward of a tertiary care centre in New Delhi. J Assoc Physicians India 2020;68:19–26. [PubMed] [Google Scholar]
- 41.Stark L, Ager A. A systematic review of prevalence studies of gender-based violence in complex emergencies. Trauma Violence Abuse 2011;12:127–34. 10.1177/1524838011404252 [DOI] [PubMed] [Google Scholar]
- 42.Rendall MS, Weden MM, Favreault MM, et al. The protective effect of marriage for survival: a review and update. Demography 2011;48:481–506. 10.1007/s13524-011-0032-5 [DOI] [PubMed] [Google Scholar]
- 43.The Hindu . COVID-19 | Kerala cm calls for more effective measures for containment, 2020. [Google Scholar]
- 44.Yadav Y. What shocking data on Covid second wave deaths really reveals: Yogendra Yadav, 2021. Available: https://theprint.in/opinion/what-shocking-data-on-covid-second-wave-deaths-really-reveals-yogendra-yadav/678890/?fbclid=IwAR3lCQ9pYGunAmztxOtv2VUNESewRcrVckaCuH3cvYIM5keEcdEOtO0k3LE [Accessed 17 Jun 2021].
- 45.ExcelNotes . Working days in Kerala, India, 2020. [Google Scholar]
- 46.MOSPI . Ministry of statistics and program implementation. Gov. India, 2021. Available: http://mospi.nic.in/ [Accessed 13 Mar 2021].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-049619supp001.pdf (90.4KB, pdf)
bmjopen-2021-049619supp002.pdf (612.2KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. All data are incorporated into the article and are openly available from the references mentioned.