Abstract
Objectives
To systematically reivew the observational evidence of the effect of school closures and school reopenings on SARS-CoV-2 community transmission.
Setting
Schools (including early years settings, primary schools and secondary schools).
Intervention
School closures and reopenings.
Outcome measure
Community transmission of SARS-CoV-2 (including any measure of community infections rate, hospital admissions or mortality attributed to COVID-19).
Methods
On 7 January 2021, we searched PubMed, Web of Science, Scopus, CINAHL, the WHO Global COVID-19 Research Database, ERIC, the British Education Index, the Australian Education Index and Google, searching title and abstracts for terms related to SARS-CoV-2 AND terms related to schools or non-pharmaceutical interventions (NPIs). We used the Cochrane Risk of Bias In Non-randomised Studies of Interventions tool to evaluate bias.
Results
We identified 7474 articles, of which 40 were included, with data from 150 countries. Of these, 32 studies assessed school closures and 11 examined reopenings. There was substantial heterogeneity between school closure studies, with half of the studies at lower risk of bias reporting reduced community transmission by up to 60% and half reporting null findings. The majority (n=3 out of 4) of school reopening studies at lower risk of bias reported no associated increases in transmission.
Conclusions
School closure studies were at risk of confounding and collinearity from other non-pharmacological interventions implemented around the same time as school closures, and the effectiveness of closures remains uncertain. School reopenings, in areas of low transmission and with appropriate mitigation measures, were generally not accompanied by increasing community transmission. With such varied evidence on effectiveness, and the harmful effects, policymakers should take a measured approach before implementing school closures; and should look to reopen schools in times of low transmission, with appropriate mitigation measures.
Keywords: COVID-19, public health, epidemiology
Strengths and limitations of this study.
While the role of non-pharmaceutical interventions as a whole in limiting community spread of SARS-CoV-2 is beyond doubt, the specific role of school closures is less clear because of the smaller role that children play in transmission of the disease.
This is the first systematic review of the empirical evidence from the COVID-19 pandemic of the effectiveness of school closures and reopenings on community transmission of SARS-CoV-2.
We include data from 150 countries, investigating both school closures and school reopenings.
We were unable to meta-analyse due to data heterogeneity.
Introduction
School closures have been a common strategy to control the spread of SARS-CoV-2 during the COVID-19 pandemic. By 2 April 2020, 172 nations had enacted full closures or partial ‘dismissals’, affecting nearly 1·5 billion children.1 As cases of COVID-19 started to fall, many countries looked to reopen schools, often with significant mitigation measures in place.2 Over the northern hemisphere winter of 2020–21, many countries again closed schools with the aim of controlling a resurgence of cases. School closures have substantial negative consequences for children’s well-being and education, which will impact on life chances and long-term health.3 4 Closures exacerbate existing inequalities, with greater impacts on children from socioeconomically deprived backgrounds because those from higher income families have better opportunities for remote learning.
The role of non-pharmaceutical interventions (NPIs) collectively in limiting community spread is established. However, the specific contribution of school closures remains unclear. Observational studies suggest that school-aged children, particularly teenagers, play a role in transmission to peers and bringing infection into households,5 although the relative importance compared with adults remains unclear.6 Younger children appear less susceptible to infection and may play a smaller role in community transmission, compared with older children and adults.7 Although some modelling studies have suggested that school closures can reduce SARS-CoV-2 community transmission,8 others disagree.9 10
A rapid systematic review published in April 2020 found a small number of studies of the effectiveness of school closures in controlling the spread of COVID-19.11 However, this review was undertaken very early in the pandemic and included no observational data on SARS-CoV-2. Since then many studies on the effects of closing or reopening schools on SARS-CoV-2 community transmission have been published, but there has been no systematic review of these studies. A clearer understanding of the impact of school closures and reopenings on community transmission is essential to aid policymakers in deciding if and when to implement school closures in response to rising virus prevalence, and when it is prudent to reopen schools. Here, we synthesise the observational evidence of the impact of closing or reopening schools on community transmission of SARS-CoV-2.
Methods
The study protocol for this systematic review is registered on PROSPERO (ID: CRD42020213699).
Inclusion and exclusion criteria
We included any empirical study which reported a quantitative estimate of the effect of school closure or reopening on community transmission of SARS-CoV-2. We considered ‘school’ to include early years settings (eg, nurseries or kindergartens), primary schools and secondary schools, but excluded further or higher education (eg, universities). Community transmission was defined as any measure of community infection rate, hospital admissions or mortality attributed to COVID-19. We included studies published in 2020 or 2021 only. We included preprints, peer-reviewed and grey literature. We did not apply any restriction on language, but all searches were undertaken in English. We excluded prospective modelling studies and studies in which the assessed outcome was exclusively transmission within the school environment rather than the wider community.
Search strategy
We searched PubMed, Web of Science, Scopus, CINAHL, the WHO Global COVID-19 Research Database (including medRxiv and SSRN), ERIC, the British Education Index and the Australian Education Index, searching title and abstracts for terms related to SARS-CoV-2 AND terms related to schools or NPIs. To search the grey literature, we searched Google. We also included papers identified through professional networks. Full details of the search strategy are included in online supplemental appendix A. Searches were undertaken first on 12 October 2020 and updated on 7 January 2021.
bmjopen-2021-053371supp001.pdf (64.6KB, pdf)
Data extraction and risk of bias assessment
Article titles and abstracts were imported into the Rayyan QCRI webtool.12 Two reviewers independently screened titles and abstracts, retrieved full texts of potentially relevant articles and assessed eligibility for inclusion.
Two reviewers independently extracted data and assessed risk of bias. Data extraction was performed using a pre-agreed extraction template which collected information on publication type (peer-reviewed or preprint), country, study design, exposure type (school closure or reopening), setting type (primary or secondary), study period, unit of observation, confounders adjusted for, other NPIs in place, analysis method, outcome measure and findings. We used the Cochrane Risk of Bias In Non-randomised Studies of Interventions tool13 to evaluate bias.
Discrepancies were resolved by discussion in the first instance and by a third reviewer where necessary.
Data synthesis
Given the heterogeneous nature of the studies, prohibiting meta-analysis, a narrative synthesis was conducted. Schools often reopened with significant COVID-19 infection prevention and control measures in place, meaning that the effect of lifting restrictions may have been different from the effect of imposing them. We therefore considered the studies of school closures and school reopenings separately. We also aimed to evaluate differential effects for primary and secondary schools if data allowed.
Patient and public involvement
There was no patient or public involvement in this study.
Results
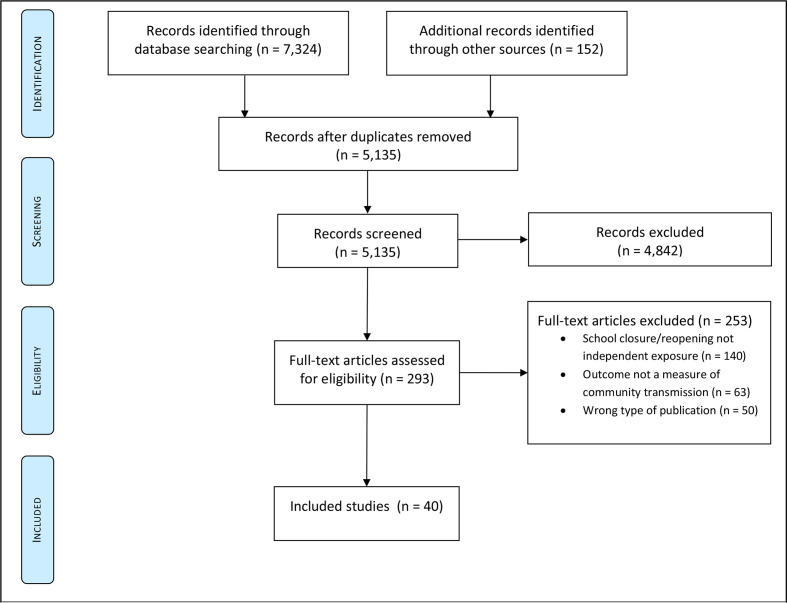
We identified 7474 studies (figure 1). After removing 2339 duplicates, 5135 unique records were screened for inclusion. We excluded 4842 records at the title or abstract stage, leaving 293 records for full-text review. Of these, 4014–53 met the inclusion criteria.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram.
Description of studies
Included studies are described in table 1, grouped by exposure type and study design. Of these, 32 studies14 15 18–21 23 24 26 29–40 42–44 46–53 reported the effect of school closures on community transmission of SARS-CoV-2, 1116 22–25 27 28 35 43–45 examined school reopening and 316 17 41 investigated the effect of school holidays. Some studies considered more than one exposure. All studies used data from national government sources or international data repositories. A total of 15 studies were from peer-reviewed journals, while 24 studies were from preprint servers and 1 study was a conference abstract.
Table 1.
Characteristics of included studies, stratified by study design
| Study | Country | Study period | Setting type | Unit of exposure | Confounders/Co-interventions adjusted for | Other NPI measures | Analysis type |
| School closures—pooled multiple-area before-after comparison studies (n=22) | |||||||
| Auger et al 14 |
USA | Study period: 13 March 2020 to 23 March 2020 Exposure period: 1 January 2020 to 29 April 2020 Lag period: 16 days (incidence), 26 days (mortality) |
Primary and secondary schools | US state |
Incidence: NPIs preschool closure (restaurant closure, stay-at-home orders). NPIs postschool closure (stay-at-home orders). Testing rate preschool and post school closure Mortality: NPIs preschool closure (restaurant closure, mass gathering ban, stay-at-home orders). NPIs postschool closure (restaurant closures, stay-at-home orders) Both: cumulative COVID-19 cases preschool closure. % of population under 15, % of population over 65, % of nursing home residents, social vulnerability index and population density |
Variable | Negative binomial regression to estimate effect of school closures on the changes in incidence and mortality rates, as calculated by interrupted time series analysis. |
| Banholzer et al 15 |
USA, Canada, Australia, Norway, Switzerland and EU-15 countries | Study period: n=100 cases until 15 April 2020 Exposure date: variable Lag period: 7 days |
Primary school closure data used to determine exposure date | Country | Border closure, event ban, gathering ban, venue closure, lockdown, work ban, day-of-the-week effects | Variable | Bayesian hierarchical model assuming negative binomial distribution of new cases. |
| Brauner et al 18 |
34 European and 7 non-European countries | Study period: 22 January 2020 to 30 May 2020 Exposure period: variable Incubation period: 6 days Infection to death: 22 days |
Primary and secondary schools | Regional data where available, otherwise country | Mass gathering bans, business closures, university closures, stay-at-home orders | Variable | Bayesian hierarchical model to estimate effectiveness of individual NPIs on the reproduction number |
| Chernozhukov et al 19 |
USA | Study period: 7 March 2020 to 3 June 2020 Exposure period: variable, but 80% of states closed within 2 days of 15 March 2020 Lag period: 14 days (incidence), 21 days (mortality) |
Primary and secondary schools | US state | Business closures, stay-at-home orders, hospitality closures, mask mandates, mobility data, national case/mortality trends | Variable | Regression model with autoregressive strucutres to allow for dynamic effects of other NPIs and mobility data. |
| Courtemanche et al 20 |
USA | Study period: 1 March 2020 to 27 April 2020 Exposure period: variable, generally mid-March Lag period: 10 and 20 days |
Not specified | US counties, or county equivalents | Other NPIs (stay-at-home orders, hospitality closure, limiting gathering size), total daily tests done in that state | Variable | Fixed effects regression to estimate the effect of school closure on the growth rate of cases (% change). |
| Dreher et al 21 |
USA | Study period: 500th case until 30 April 2020 Exposure period: variable |
Not specified | US state | Data collected on: demography (population density, population size, GDP, state-wide health and healthcare capacity) and on NPIs (stay-at-home orders, mass gathering bans and business closures). However, covariables with a p>0.1 in univariate analysis and collinear variables were excluded. Full details are not available of which covariables were included | Variable |
|
| Garchitorena et al 24 |
32 European countries | Study period: 1 February 2020 to 16 September 2020 Exposure period: variable Lag period: no lag applied |
Early years settings, primary schools and secondary schools | Country | Stay-at-home orders, university closures, mass gathering bans, mask mandates, work-from-home orders, public space closures, business and retail closures | Variable | Used incidence data, supplemented by a capture-recapture method using mortality data to infer undiagnosed cases. Compared this with a counterfactual age-structured Susceptible-Exposed-Infectious-Removed (SEIR) model coupled with Monte Carlo Markov Chain to estimate effectiveness of NPI combinations—then estimated their disentangled effects (considering each individual NPI over the duration of their implementation). |
| Hsiang et al 26 |
Italy, France, USA | Study period: 25 February 2020 to 6 April 2020 Exposure date: varied by country Lag period: no lag applied |
Not specified | Provincial/Regional level (Italy and France), state level (USA) | Other NPIs (travel ban and quarantine, work-from-home order, no social gatherings, social distancing rules, business and religious closures, home isolation), test regimes | Variable | Reduced-form econometric (regression) analysis to estimate the effect of school closures on the continuous growth rate (log scale). |
| Jamison et al 30 |
13 European countries | Study period: until 16 May 2020 Exposure period: variable Lag period: 18 days |
Not specified | Country | Workplace closures, public event cancellations, restricting gathering sizes, closing public transport, stay-at-home orders, internal movement restrictions and international travel, mobility data, population >65 years, population density, number of acute care beds per population, starting date of epidemic, day of the epidemic | Variable | Linear regression model reporting the percentage point reduction in the daily change of deaths measured as a 5-day rolling average. |
| Kilmek-Tulwin and Tulwin32 | 15 European countries; Argentina, Brazil and Japan | Study period: not specified Exposure period: variable |
Not specified | Country | None | Not specified | Wilcoxon signed rank test to determinethe significance of differences between pairs of incidence rates from different time points. Time points considered: 16th day, 30th day, 60th day since 100th case. Cases/million population compared following implementation of school closures. |
| Krishnamachari et al 33 |
USA | Study period: not specified Exposure period: variable |
Not specified | US state US city |
State analysis: days for preparation, population density, % urban, % black, % aged >65 years, % female City analysis: use of public transport for work, use of carpool for work, population density and % black Both analyses: days from state-level emergency declaration to gathering size restrictions, non-essential business closures, stay-at-home orders, gathering restrictions, restaurant closures |
Variable | Negative binomial regression comparing states/cities above and below median value for days to implement school closures, on rate ratio of cumulative incidence on days 14, 21, 28, 35 and 42 following the area’s 50th case. All variables in analysis classified a 1 if above median value for dataset, and 0 if below. |
| Li et al34 | Worldwide (167 geopolitical areas) | Study period: 1 January 2020 to 19 May 2020 Exposure period: variable |
Not specified | Country, province or state | None specified | School closures only considered in the context of travel and work restrictions, and mass gathering bans already being in place | Validate a novel SEIR model ('DELPHI') in the 167 countries between 28 April 2020 and 12 May 2020. Then elicit the effect of each day an NPI was in place on the DELPHI-derived changes to the infection rate at each time point. |
| Li et al3 | Worldwide (131 countries) | Study period: 1 January 2020 to 20 July 2020 Exposure period: variable |
Not specified | Country | Other NPIs (international travel bans, internal travel bans, stay-at-home requirements, public transport closures, mass gathering bans, public event bans, workplace closures) | Variable | Defined a time period as a period in which the NPIs in a given country were the same. Calculated the R ratio as the ratio between the daily R of each period and the R from the last day of the previous period. Pooled countries using log-linear regression with the introduction and relaxation of each NPI as independent variables for the first 28 days after introduction/relaxation of the NPI. |
| Liu et al 36 |
Worldwide (130 countries) | Study period: 1 January 2020 to 22 June 2020 Exposure period: variable Lag periods: 1, 5 and 10 days |
Not specified | Mostly country, although lags were examined at the World Region level | Various parsimonious models. Variables considered: workplace closure, cancellation of public events, gathering size restrictions, public transport closures, stay-at-home requirements, internal movement restrictions, international travel restrictions, income support for households, public information campaigns, testing policy and contact tracing policy | Variable | Parsimonious linear fixed effects panel regression, using stepwise backwards variable selection. Accounted for collinearity of interventions by conducting hierarchical cluster analysis with multiscale bootstrapping to test the statistical significance of identified clusters. |
| Papadopoulos et al 39 |
Worldwide (150 countries) | Study period: 1 January 2020 to 29 April 2020 Exposure period: variable Lag period: no lag applied |
Not specified | Country | NPIs (workplace closure, public event cancellations, gathering size restrictions, public transport closures, stay-at-home restrictions, internal travel restrictions, international travel restrictions, public information campaigns, testing systems and contact tracing systems), timing of each NPI in days since first case, overall stringency index and sociodemographics (population, life expectancy, purchasing power, longitude, date of first death, average household size) | Variable | Univariate regression model for effect of school closures on total log cases and total log deaths. Multivariate regression model for effect of timing of school closures (relative to first case) on log total cases and log total deaths. |
| Piovani et al,40 | 37 OECD Member Countries | Study period: 1 January 2020 to 30 June 2020 Exposure period: variable Lag period: 26 days |
Not specified | Country | Timing of mass gathering bans, time from first death to peak mortality, cumulative incidence at first death, log population size, hospital beds per population, % population aged 15–64 years, % urban, annual air passengers and population density | Variable | Multivariable negative binomial regression with panel data. |
| Rauscher 42 |
USA | Study period: until 27 April 2020 Exposure period: state’s 100th death until time of school closures Lag period: not specified |
Not specified | US state | Population density, number of schools, public school enrolment, stay-at-home order date, whether school closures were mandated or recommended | Variable | Regression analyses of time between the state’s 100th cases and day of school closures and the daily cumulative cases and deaths, measured on the log scale per 100 000 residents. |
| Stokes et al 46 |
Worldwide (130 countries) | Exposure: time before first death; and first 14 days after first death Lag period: up to 24 days |
Not specified | Country | An overall average strictness and timeliness of NPI measures (as a whole) derived from data on school closures, workplace closures, public event bans, gathering bans, public transport closures, stay-at-home orders, internal movement restrictions, international travel restrictions and public information campaigns. Also adjusted for days since NPI implementation, population density, % over 65, % male, life expectancy, hospital beds, GDP, health expenditure, international tourism, governance, region, testing policy, contact tracing policy | Variable | Multivariable linear regression to estimate the effect of NPIs (including school closures) as lagged variables on the daily mortality rate per 1 million 0–24 days after the first death, 14–38 days after the first death. |
| Wu et al 47 |
USA | Study period: until 28 May 2020 Exposure period: variable |
Not specified | US counties | Stay-at-home orders, mass gathering bans, restaurant closures, hospitality and gym closures, federal guidelines, foreign travel ban | Variable | Grouped together demographically and socioeconomically similar counties into five clusters, then developed a model of R for each cluster applying a Bayesian mechanistic model to excess mortality data. |
| Yang et al 48 |
USA | Study period: 21 January 2020 to 5 June 2020 Exposure period: variable |
Early years, and ‘schools’ (presumed primary and secondary) | US counties | County-level demographic characteristics, NPIs (school closures, leisure activity closure, stay-at-home orders, face mask mandates, daycare closures, nursing home visiting bans, medical service suspension) and previous week log R | Variable, but school closures generally implemented before other measures | Mechanistic transmission models fitted to lab-confirmed cases, applying lag times from the literature. Used generalised estimating equations with autoregression of confounders. |
| Yehya et al 49 |
USA | Study period: 21 January 2020 to 29 April 2020 Exposure measure: time (days) between 10th COVID-19 death and school closure Lag (exposure to mortality): up to 28 days |
Primary and secondary schools | US state | Population size, population density, % aged <18 years, % aged >65 years, % black, % Hispanic, % in poverty, geographical region | Variable | Multivariable negative binomial regression to estimate mortality rate ratios associated with each day of delaying school closure. |
| Zeilinger et al 50 |
Worldwide (176 countries) | Study period: until 17 August 2020 Exposure period: variable |
Not specified | Country | NPIs (mass gathering bans, social distancing rules, business closures, curfews, declaration of emergencies, border restrictions, lockdown); % population >65, % population urban, GDP, % exposed to high PM2.5 air pollution; day of the year, and days since 25th cumulative case | Variable | Non-parametric machine learning model applied to each country, before pooling the estimated NPI effects across countries. Including only the 90 days after the 25th cumulative case. |
| School closures—within-area before-after comparison studies (n=7) | |||||||
| Gandini et al23 2021 No evidence of association between schools and SARS-CoV-2 second wave in Italy |
Italy | Study period: 7 August 2020 to 2 December 2020 Exposure period: variable. School reopenings during September. Closures in October and Nobermber Lag: under investigation |
Early years, primary and secondary schools | Italian province | None specified | Variable | Created a model of R from data on new cases, parameters estimated using data from the first wave in Italy (serial interval 6.6) and Bayesian methodology to account for the epidemiological uncertainty. Reported as the median for the 7-day posterior moment. Compared neighbouring provinces that reopened or reclosed schools at different times. |
| Iwata et al 29 |
Japan | Study period: 27 January 2020 to 31 March 2020 Exposure date: 29 February 2020 Lag period: 9 days |
Primary and secondary schools | Country | None specified | Not specified | Time series analysis using Bayesian inference to estimate effect of school closures on the incidence rate of COVID-19. |
| Matzinger and Skinner 37 |
USA | Study period: 6 March 2020 to 1 May 2020 Exposure date: 14 March 2020 (Georgia, Tennessee), 6 March 2020 (Mississippi) Lag period: under investigation |
Primary and secondary schools | US state | None specified | Not specified | Calculated changes to the doubling time of new cases, hospitalisations and deaths by plotting log2 of cases, hospitalisations and deaths against time, and using segmented regression to analyse changes in the trends in response to NPI implementation. |
| Neidhofer and Neidhofer 38 |
Argentina, Italy, South Korea | Study period: not specified Exposure date: Italy 4 March 2020 Argentina 16 March 2020 South Korea not specified Lag period: analysis up to 18 days postschool closure |
Not specified | Country | Indirectly adjusted for in derivation of counterfactual, based on most comparable countries for: population size and density, median age, % aged >65 years, GDP per capita, hospital beds per 100 000 inhabitants, public health expenditures, average number of reported COVID-19 deaths before day zero, growth rate of reported COVID-19 cases with respect to the day before and mobility patterns retrieved from Google Mobility Reports | All three countries: banning of public events, restriction of international flights, contact tracing, public information campaign. Other unspecified interventions in place in each country | Difference-in-differences comparison to a synthetic control unit (derived from the weighted average of the epidemic curves from comparable countries that closed schools later), to estimate the % reduction in deaths in the 18 days postschool closure. |
| Shah et al 53 |
Australia, Belgium, Italy, UK, USA | Study period: 1 February 2020 to 30 June 2020 Exposure period: variable Lag period: 6 weeks |
Not specified | Country | Other NPIs (workplace closures, public event cancellations, restrictions on mass gatherings, public transport closure, stay-at-home orders, internal movement restrictions) and mobility data from Apple | Not specified | Poisson regression to estimate the effect of NPIs on mortality (outcome measure not fully explained). |
| Sruthi et al 43 |
Switzerland | Study period: 9 March 2020 to 13 September 2020 | Secondary schools used as exposure date | Swiss Canton (region) | Closures of hairdressers, bars, nightclubs, restaurants and retail. Travel restrictions. Mask mandates. Number of hotel rooms within the Canton. Results stratified by Cantons with and without mask mandates in place within secondary schools | Variable | Artificial intelligence model to disentangle the effect of individual NPIs on Rt. R estimated exclusively from incidence data. |
| Stage et al 44 |
Denmark, Germany, Norway | Study period: March–June 2020 Closure dates: Around 16 March 2020 Reopening dates: staggered, from late April to mid-May Lag period: under study |
Early years, primary and secondary schools | Country | None specified but timing of other NPIs, and changes to testing capacity outlined within analysis | Variable | Closures: observed data compared against counterfactual unmitigated simulation using an epidemic model fitted by Approximate Bayesian Computation, with a Poisson Gaussian process regression model. Response dates measured as a change in growth rate occurring at least 5 days after the intervention, exceeding the 75th centile of the modelled data, and where the deviation persists for at least 5 days. Reopening: growth rate change for each loosening of restrictions, estimating an instantaneous growth rate via a General Additive Model using a quasi-Poisson family with canonical link and default thin plate regression splines. |
| School closures—pooled multiple-area comparisons of interventions in place at a fixed time point (n=3) | |||||||
| Juni et al 31 |
Worldwide (144 countries) | Study period: Until 28 March 2020 Exposure date: 11 March 2020 Lag period: 10 days |
Not specified | Country | Country-specific factors (GDP per capita, health expenditure as % of GDP, life expectancy, % aged ≥65 years, Infectious Disease Vulnerability Index, urban population density), geography factors (flight passengers per capita, closest distance to a geopolitical area with an already established epidemic, geogrpahical region) and climatic factors (temperature, humidity) | Variable | Weighted random-effects regression analysis to estimate the effect of school closures on the changes to the incidence rate (measured as the ratio of rate ratios, dividing cumulative cases up to 28 March 2020, by cumulative cases until 21 March 2020, for each area). |
| Walach and Hockertz 52 |
34 European countries, Brazil, Canada, China, India, Iran, Japan and USA | Study period: until 15 May 2020 Exposure period: cut-off 15 May 2020 Lag period: no lag applied |
Not specified | Country | Days of pandemic, life expectancy, smoking prevalence | Variable | First examined correlations between multiple individual variables and cases/deaths in non-parametric analysis. Then incorporated those with an r>0.3 into generalised linear models, starting with the best correlated variables and adding in only those that improved model fit. |
| Wong et al 51 |
Worldwide (139 countries) | Analysis period: 15 April 2020 to 30 April 2020 Exposure cut-off date: 31 March 2020 Lag period: 14 days |
Not specified | Country | Stringency index (workplace closure, public event cancellation, restrictions on gathering size, public transport closure, stay-at-home orders, restrictions on internal movement and international travel, public information campaigns), GDP, population density | Variable | Multivariable linear regression to estimate the effect of school closures on the rate of increase in cumulative incidence of COVID-19. |
| School reopening studies (n=11) | |||||||
| Beesley 16 |
Worldwide (24 countries) | Study period: until 1 September 2020 Exposure date: variable Lag period: under investigation |
Mostly all schools, but in the Netherlands noted that primary schools were reopened first | Country | None | Not specified | Naked eye analysis of 7-day rolling average of new cases. |
| Ehrhardt et al 22 |
Germany | Study period: 25 February 2020 to 4 August 20202 Exposure period: school closures 17 March 2020 Staggered school reopening 4 May 2020 to 29 June 2020 |
Early years settings, primary and secondary schools | Baden-Wurttemberg (region of Germany) | None specified | Not specified | Presentation of an epidemic curve showing daily new cases in Baden-Wurttemberg from 25 February 2020 to 7 August 2020 with key school dates labelled. |
| Gandini et al23 | See description in school closure section above | ||||||
| Garchitorena et al24 | See description in school closure section above | ||||||
| Harris et al25 | USA | Study period: January–October 2020 Exposure period: variable Lag period: 1–2 weeks |
Not specified | US counties | Adjusted for NPIs (stay-at-home orders, non-essential business closures, non-essential business reopening, restaurant closures, restaurant reopenings, mask mandates and resumption of religious gatherings), with state, county and calendar week fixed effects | Variable | Difference-in-differences event study model with propensity score matching comparing exposure data (codified as: virtual only 0, hybrid model 0.5, in-person teaching only 1) with inpatient hospitalisations with diagnoses of COVID-19 or COVID-19-related symptoms from insurance data. |
| Ingelbeen et al 27 |
Belgium | Study period: 1 August 2020 to 30 November 2020 Exposure date: 1 September 2020 Lag period: no lag applied |
Primary and secondary schools | Brussels, Belgium | None specified | Cafes, restaurants and sports facilities had already been reopened in a limited way from June, and five close contacts were permitted from July | Plotted R using data from the national contact tracing system. Also used the contact tracing data to examine age-specific trends in cases/contacts following school reopenings. |
| Isphording et al 28 |
Germany | Study period: 1 July 2020 to 5 October 2020 Exposure period: variable |
Not specified | German counties | Adjusted for mobility data from a private company which have data on one-third of German mobile phone users, and Google mobility reports. Fixed effects used to control for demographic differences | Not specified | Regression model comparing changes in new cases between counties that reopen schools after the summer holidays, with counties that have not yet reopened schools. Considered data from 2 weeks before reopening to 3 weeks after. |
| Li et al35 | See description in school closure section above | ||||||
| Sruthi et al43 | See description in school closure section above | ||||||
| Stein-Zamir et al 45 |
Germany | Study period: 1 July 2020 to 5 October 2020 Exposure period: variable |
Not specified | German counties | Adjusted for mobility data from a private company which have data on one-third of German mobile phone users, and Google mobility reports. Fixed effects used to control for demographic differences | Not specified | Regression model comparing changes in new cases between counties that reopen schools after the summer holidays, with counties that have not yet reopened schools. Considered data from 2 weeks before reopening to 3 weeks after. |
| Stage et al44 | See description in school closure section above | ||||||
| School holiday studies (n=3) | |||||||
| Beesley16 | See description in school reopening section above | ||||||
| Bjork et al 17 |
11 European countries | Study period: 30 March 2020 to 7 June 2020 Exposure period: 10 February 2020 to 8 March 2020 Lag period: n/a |
Not specified | Region | Population density, age distribution, country | Variable | Variance-weighted least squares linear regression comparing timing of February/March half-term with excess mortality (compared with 2015–2019 data for each region). |
| Pluemper and Neumayer 41 |
Germany | Study period: 10 June 2020 to 23 September 2020 Exposure period: variable |
Not specified | School holiday timing: state (n=16) Outcome data: district (n=401) |
Average taxable income and proportion of residents who are foreigners | Not specified | Multivariable regression model comparing incident growth rate 2 weeks before summer holidays up to 2 weeks afterwards, with fixed effects to account for for interdistrict differences, and a lagged dependent variable to account for background natioinal trends in the data. |
n/a, not available; NPI, non-pharmaceutical intervention; OECD, Organisation for Economic Co-operation and Development.
All studies were ecological in nature, that is, the unit of analysis was national or regional. Of the school closure studies, 13 reported data from a single country or region (the USA (n=10),14 19–21 33 37 42 47–49 Italy (n=1),23 Japan (n=1)29 and Switzerland (n=1)43); 4 reported discrete estimates for several countries26 38 44 53 and 15 studies pooled data from multiple countries (globally (n=8),31 34–36 39 46 50 51 Europe only (n=2),24 30 Europe and other high-income countries (n=5)15 18 32 40 52). The studies on school reopening generally reported on single countries (Germany (n=2),22 28 USA (n=1),25 Switzerland (n=1),43 Belgium (n=1),27 Israel (n=1),45 Italy (n=1)23), but one reported discrete estimates for three countries (Denmark, Germany and Norway),44 two pooled data from multiple countries globally16 35 and one pooled data from multiple European countries.24 Of the three school holiday studies, one reported on Germany,41 one pooled data from 24 countries globally16 and one pooled data from multiple European countries.17
The majority of studies (n=24) did not specify the type of school setting being studied. However, eight studies specified that they were reporting on primary and secondary schools only,14 16 18 19 27 29 37 49 and six additionally include early years settings.22–24 44 45 48 The two remaining studies used the date of primary school (n=1)15 or secondary school (n=1)43 closure as their exposure date, but did not indicate this was temporally distinct from closure of the other setting. Very few studies reported independent effect sizes for different setting types: two closure studies24 48 and four reopening studies.16 22 24 44
Studies that specifically sought to estimate an effect of school closure policy on SARS-CoV-2 transmission included eight school closure studies,14 23 29 32 37 38 42 44 six school reopening studies22 23 25 28 44 45 and three school holiday studies. The remaining studies primarily sought to estimate the effect of NPIs (but reported an independent estimate for schools, alongside estimates for other NPIs within their analysis).
The studies used different analytic approaches: regression models (n=24),14 17 19–21 25 26 28 30 31 33 35 36 39–42 44 46 48 49 51–53 Bayesian modelling (n=3),15 18 47 comparison to a synthetic control group (n=4),24 34 38 44 machine learning approaches (n=2),43 50 time series analysis (n=1)29 and visual representation of changes in transmission over time compared against the timing of school policy interventions, with or without formal statistical analysis (n=4).16 22 37 45 We identified three study designs used to estimate the effect of school closures: pooled multiple-area before-after comparisons (n=22),14 15 18–21 24 26 30 32–36 39 40 42 46–50 within-area before-after comparisons (n=7)23 29 37 38 43 44 53 and pooled multiple-area comparisons of interventions in place at a fixed time point (n=3).31 51 52
In most instances of school closures, particularly in European countries, other NPIs were introduced at or around the same time. Some studies dealt with this at the design stage, choosing to study places where school closures were done in (relative) isolation37 and some at the analytical stage (typically by undertaking regression and having multiple comparator countries). Some studies did not appear to have a mechanism in place to deal with this potential confounding.32 40 44 52 Studies which pooled data from multiple areas also adjusted for other potential confounders, such as population factors (eg, proportion of population aged ≥65 years, population density) and SARS-CoV-2 testing regimes.
Among school closure studies, 1814 15 19 20 24 26 29 31–34 37 39 42–44 50 51 reported effects on incidence, 1114 19 21 30 38–40 42 46 52 53 on mortality, 137 on hospital admissions and mortality and 818 21 23 35 36 43 47 48 on an estimate of the effective Reproductive number (R) (derived from incidence and/or mortality data). Of the school reopening studies, six reported effects on incidence,16 22 24 28 44 45 two on hospitalisations25 44 and four on R.23 27 35 43 Two school holiday studies reported an effect on incidence,16 41 while the other reported on mortality.17 The assumed lag period from school policy changes to changes in incidence rate varied between 7 and 20 days, with longer time periods of 26–28 days generally assumed for mortality.
Risk of bias is summarised in table 2. Of the school closure studies, 14 were found to be at moderate risk of bias,14 15 18–20 24 26 30 35–37 46–48 14 at serious risk21 23 29 31 33 34 38 39 42 43 49–51 53 and 4 at critical risk of bias.32 40 44 52 Of the school reopening studies, four were found to be at moderate risk,24 25 28 35 four at serious risk23 27 43 44 and three at critical risk of bias.16 22 45 The school holiday studies were found to be at moderate (n=1),41 serious (n=1)17 or critical (n=1)16 risk of bias.
Table 2.
Findings from the risk of bias assessment using the ROBINS-I tool, stratified by study design
| Study | Confounding or co-intervention bias |
Selection bias |
Misclassification bias |
Deviation bias | Missing data bias | Outcome measurement bias | Outcome reporting bias | Overall judgement | Likely direction |
| School closures—pooled multiple-area before-after comparison studies | |||||||||
| Auger et al14 | Moderate | Low | Low | Low | Low | Low | Low | Moderate | Favours experimental |
| Banholzer et al15 | Moderate | Low | Low | Low | Low | Moderate | Low | Moderate | Unpredictable |
| Brauner et al18 | Moderate | Low | Low | Low | Low | Low | Low | Moderate | Unpredictable |
| Chernozhukov et al19 | Moderate | Low | Moderate | Low | Low | Low | Low | Moderate | Unpredictable |
| Courtemanche et al20 | Moderate | Low | Low | Low | Low | Low | Low | Moderate | Unpredictable |
| Garchitorena et al24 | Moderate | Low | Low | Low | Low | Low | Low | Moderate | Unpredictable |
| Hsiang et al26 | Moderate | Low | Low | Low | Low | Low | Low | Moderate | Unpredictable |
| Jamison et al30 | Moderate | Low | Low | Low | Low | Low | Low | Moderate | Unpredictable |
| Li et al35 | Moderate | Low | Low | Low | Low | Low | Low | Moderate | Unpredictable |
| Liu et al36 | Moderate | Low | Low | Low | Low | Low | Moderate | Moderate | Unpredictable |
| Stokes et al46 | Moderate | Low | Low | Low | Low | Low | Moderate | Moderate | Unpredictable |
| Wu et al47 | Moderate | Low | Low | Low | Low | Low | Low | Moderate | Unpredictable |
| Yang et al48 | Moderate | Low | Low | Low | Low | Low | Low | Moderate | Unpredictable |
| Krishnamachari et al33 | Moderate | Low | Serious | Low | Low | Low | Low | Serious | Unpredictable |
| Dreher et al21 | Serious | Low | Moderate | Low | Low | Moderate | Low | Serious | Favours experimental |
| Li et al34 | Moderate | Low | Serious | Low | Low | Low | Low | Serious | Unpredictable |
| Papadopoulos et al39 | Moderate | Low | Moderate | Low | Low | Serious | Low | Serious | Unpredictable |
| Rauscher42 | Serious | Low | Low | Low | Low | Low | Low | Serious | Favours experimental |
| Yehya et al49 | Serious | Low | Low | Low | Low | Moderate | Low | Serious | Favours experimental |
| Zeilinger et al50 | Moderate | Low | Low | Low | Low | Serious | Low | Serious | Favours experimental |
| Kilmek-Tulwin and Tulwin32 | Critical | Moderate | Low | Low | Low | Moderate | Low | Critical | Favours experimental |
| Piovani et al40 | Critical | Low | Low | Low | Low | Serious | Low | Critical | Favours experimental |
| School closures—within-area before-after comparison studies | |||||||||
| Matzinger and Skinner37 | Moderate | Low | Low | Low | Low | Moderate | Low | Moderate | Unpredictable |
| Gandini et al23 | Serious | Moderate | Low | Moderate | Low | Moderate | Low | Serious | Unpredictable |
| Iwata et al29 | Serious | Low | Low | Low | Low | Moderate | Low | Serious | Unpredictable |
| Neidhofer and Neidhofer38 | Serious | Serious | Low | Low | Low | Low | Moderate | Serious | Favours experimental |
| Shah et al53 | Serious | Low | Moderate | Low | Low | Moderate | Low | Serious | Unpredictable |
| Sruthi et al43 | Serious | Low | Low | Low | Low | Moderate | Low | Serious | Unpredictable |
| Stage—closures | Critical | Low | Low | Low | Low | Moderate | Low | Critical | Favours experimental |
| School closures—pooled multiple-area comparisons of interventions in place at a fixed time point | |||||||||
| Juni et al31 | Serious | Low | Low | Low | Low | Low | Low | Serious | Favours experimental |
| Wong et al51 | Serious | Low | Low | Low | Low | Low | Low | Serious | Unpredictable |
| Walach and Hockertz52 | Critical | Low | Serious | Low | Low | Serious | Low | Critical | Unpredictable |
| School reopening studies | |||||||||
| Garchitorena et al24 | Moderate | Low | Low | Low | Low | Low | Low | Moderate | Unpredictable |
| Harris et al25 | Moderate | Moderate | Low | Moderate | Low | Low | Moderate | Moderate | Unpredictable |
| Isphording et al28 | Moderate | Low | Low | Low | Low | Moderate | Low | Moderate | Unpredictable |
| Li et al35 | Moderate | Low | Low | Low | Low | Low | Low | Moderate | Unpredictable |
| Gandini et al23 | Serious | Moderate | Low | Moderate | Low | Moderate | Low | Serious | Unpredictable |
| Ingelbeen et al27 | Serious | Low | Low | Low | Low | Moderate | Low | Serious | Unpredictable |
| Sruthi et al43 | Serious | Low | Low | Low | Low | Moderate | Low | Serious | Unpredictable |
| Stage—opening | Serious | Low | Low | Low | Low | Moderate | Low | Serious | Unpredictable |
| Beesley16 | Critical | Low | Moderate | Moderate | Low | Serious | Low | Critical | Favours experimental |
| Ehrhardt et al22 | Critical | Low | Low | Moderate | Low | Low | Low | Critical | Favours experimental |
| Stein-Zamir et al45 | Critical | Low | Low | Low | Low | Serious | Low | Critical | Unpredictable |
| School holiday studies | |||||||||
| Pluemper and Neumayer41 | Moderate | Low | Low | Low | Low | Low | Low | Moderate | Unpredictable |
| Bjork et al17 | Low | Low | Low | Serious | Low | Low | Low | Serious | Favours comparator |
| Beesley16 | Critical | Low | Moderate | Moderate | Low | Serious | Low | Critical | Favours experimental |
Scale applied: low, moderate, serious or critical.
‘Favours experimental’ indicates that the bias likely resulted in an exaggeration of the reduction in community transmission associated with school closures.
ROBINS-I, Cochrane Risk of Bias In Non-randomised Studies of Interventions.
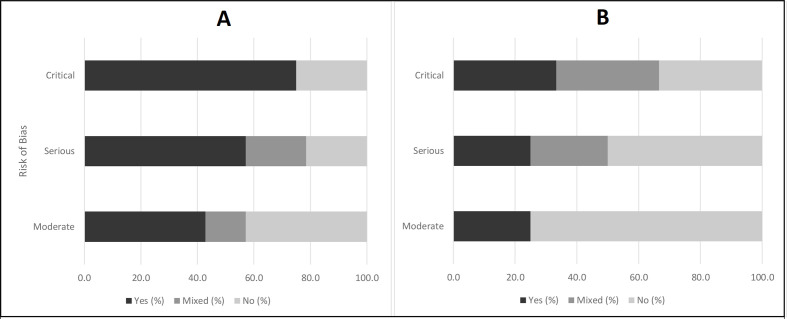
There was significant heterogeneity in the study findings (table 3): 17 studies14 24 31 32 34–38 40 42–44 48–51 reported that closing schools was associated with a reduction in transmission rates; 915 18 20 23 26 29 30 39 47 found no association between school closures and transmission; 519 21 33 46 53 reported mixed findings with evidence of a reduction in transmission in some analyses but not others and 1 study52 reported that school closures were associated with an increase in mortality. The reported effect size of closing schools ranged from precise estimates of no effect26 to approximately halving the incidence14; and from approximately doubling mortality52 to approximately halving mortality.14 The studies at the highest risk of bias generally reported large reductions in transmission associated with school closures, while studies at lower levels of bias reported more variable findings (figure 2). Of the school reopening studies, six22–25 28 44 reported no increase in transmission associated with reopening of schools, while two16 43 reported mixed findings and three27 35 45 reported increases in transmission. Of the four school reopening studies at lowest risk of bias,24 25 28 35 three24 25 28 reported no association between school reopenings and transmission.
Table 3.
Findings from included studies, stratified by study design
| Study | Main finding | Outcome measure | Detailed results | Other comments |
| School closures—pooled multiple-area before-after comparison studies (n=22) | ||||
| Auger et al 14 |
School closures associated with reduced transmission: school closures were associated with decreases in the rate of growth of COVID-19 incidence and mortality |
Regression coefficient estimating effect of school closures on changes to weekly incidence and mortality rates | Adjusted model: incidence: 62% (95% CI 49% to 71%) relative reduction Mortality: 58% (95% CI 46% to 67%) relative reduction |
Sensitivity analysis of shorter and longer lag periods did not significantly alter the findings. Early school closure associated with greater relative reduction in COVID-19 incidence and mortality. |
| Banholzer et al, 15 |
School closures not associated with a change in transmission: school closures not statistically significantly associated with a reduction in the incidence rate |
Relative reduction in new cases compared with cumulative incidence rate prior to NPI implementation | 8% (95% CrI 0% to 23%) | Sensitivity analyses for altering n=100 cases start point, and 7-day lag, did not significantly change the findings. Concede that close temporal proximity of interventions precludes precise estimates, but that NPIs were sufficiently staggered within countries, and sufficiently heterogeneous across countries to have confidence that school closures were less effective than other NPIs. |
| Brauner et al 18 |
School closures not associated with a change in transmission: school closures not statistically significantly associated with a reduction in Rt |
% reduction in Rt with 95% Bayesian CrI | 8.6% (95% CrI −13.3% to 30.5%) | Authors report close collinearity with university closures making independent estimates difficult. Findings robust to variety of sensitivity analyses. |
| Chernozhukov et al 19 |
School closures associated with a mixed effect on transmission: school closures not associated with a change in incidence rate, but statistically significantly associated with a reduction in mortality rate |
Regression coefficient estimating the change in weekly incidence rate and weekly mortality rate, measured on the log scale | Incidence rate: 0.019 (SE 0.101) Mortality rate: −0.234 (SE 0.112) |
The authors report more precise estimates for other NPIs due to considerable variation in their timing between states, whereas there was very little variation in the timing of school closures across the country, with 80% of states closing schools within a couple of days of 15 March 2020. School closures significantly associated with reductions in mobility. |
| Courtemanche et al 20 |
School closures not associated with a change in transmission: school closures not statistically associated with the growth rate of confirmed cases |
Regression coefficient estimating effect of school closures on the growth rate of cases (% change) | Applying a 10-day lag: 1.71% (95% CI −0.38% to 3.79%) Applying a 20-day lag: 0.17% (95% CI −1.60% to 1.94%) |
|
| Dreher et al 21 |
School closures associated with a mixed effect on transmission: school closures associated with a statistically significant reduction in Rt, but no association with doubling time of cases or deaths |
Regression coefficients from the linear and cox proportional hazards regressions. The first analysis is stratified into the first 7 days after iimplementation, and the second 7 days |
|
In adjusted models using Google mobility data, a 10% increase in time spent at home was reported in the week following school closures. |
| Garchitorena et al 24 |
School closures associated with reduced transmission: school closures statistically significantly associated with a reduction in COVID-19 transmission |
Ratio of transmission rates with and without implementation of the NPI (assessed over the duration of the NPI being in place) Presented as a forest plot so the reported results here are estimated | EY settings: 9% reduction (95% CI 1% to 16%) Primary schools: 10% reduction (95% CI 2% to 18%) Secondary schools: 11% reduction (95% CI 3% to 19%) |
|
| Hsiang et al 26 |
School closures not associated with a change in transmission: school closures not statistically associated with the growth rate of confirmed cases |
Regression coefficient estimating effect of school closures on the continuous growth rate (log scale) | Italy: −0.11 (95% CI −0.25 to 0.03) France: −0.01 (95% CI −0.09 to 0.07) USA: 0.03 (95% CI −0.03 to 0.09) |
Sensitivity analysis applying a lag to NPI measures on data from China did not significantly alter the findings. |
| Jamison et al 30 |
School closures not associated with transmission: school closures not statistically significantly associated with relative changes in the 5-day rolling average of COVID-19 mortality |
Percentage point change to the 5-day rolling average of COVID-19 mortality | −2.8 (95% CI −6.7 to 1.0), p=0.150 | |
| Kilmek-Tulwin and Tulwin32 |
School closures associated with reduced transmission: earlier school closures associated with lower incidence rates in the follow-up period |
Change in incidence rate on the 16th, 30th and 60th day post 100th cases between countries ranked by the cases/million population at school closure | 16th day: r=0.647, p=0.004 30th day: r=0.657, p=0.002 60th day: r=0.510, p=0.031 |
|
| Krishnamachari et al 33 |
School closures associated with a mixed effect on transmission: school closures not statistically significantly associated with cumulative incidence rate in most analyses, but associated with a significant reduction in some analyses |
Rate ratio of cumulative incidence between areas that below the median time from state-of-emergency declaration to closure and those above the median time, at days 14, 21, 28, 35 and 42 following the area’s 50th case | US states: 14 days: 2.27 (95% CI 0.80, 1.70) p=0.42 21 days: 1.38 (95% CI 0.91, 2.10) p=0.13 28 days: 1.52 (95% CI 0.98 to 2.33), p=0.06 35 days: 1.59 (95% CI 1.03 to 2.44), p=0.04 42 days: 1.64 (95% CI 1.07 to 2.52), p=0.02 US 25 most populous cities: 14 days: 1.08 (95% CI 0.75 to 1.55), p=0.68 21 days: 1.22 (95% CI 0.81 to 1.83), p=0.34 28 days: 1.24 (95% CI 0.78 to 1.98), p=0.35 35 days: 1.24 (95% CI 0.75 to 2.05), p=0.40 42 days: 1.16 (95% CI 0.67 to 2.02), p=0.59 |
Secondary analysis comparing results in cities of low and high population density at 35 days post-50th case in the state. In low-density cities, they report a non-significant trend towards early school closures reducing cumulative incidence rate, in high-density cities they report the opposite—a non-significant trend towards late school closures reducing cumulative incidence rate. |
| Li et al34 |
School closures associated with reduced transmission: school closures were associated with a reduction in the COVID-19 incidence rate |
Reported the additional benefit of every day that school closures were added to travel and work restrictions, and mass gathering bans | 17.3 (SD 6.6) percentage point reduction in infection rate Travel and work restriction and mass gathering bans alone: 59.0 (SD 5.2) residual infection rate ovserved compared with DELPHI predicted no intervention Travel and work restriction and mass gatherings bans with school closures: 41.7 (SD 4.3) |
|
| Li et al35 |
School closures associated with reduced transmission: school closures associated with a reduction in Rt across the 28 days following closures |
Ratio between R while NPI in place, and R on the last day of the previous time period. Reported at 7, 14 and 28 days (as well as visual representation of each individual day to demonstrate trend) | Day 7: 0.89 (95% CI 0.82 to 0.97) Day 14: 0.86 (95% CI 0.72 to 1.02) Day 28: 0.85 (95% CI 0.66 to 1.10) |
|
| Liu et al 36 |
School closures associated with reduced transmission: school closures associated with a statistically significant reduction in Rt across analyses |
‘Strong’ evidence for NPI effectiveness if statistically significant across multiple parsimonious models varying the follow-up period, the lag time and the classification of the NPI. 'Moderate' evidence if significant in some models; ‘weak' if not Effect sizes from individual models are a regression coefficient on change in R |
‘Strong' evidence of effectiveness for school closures. Effect sizes in individual models between 0.0 and −0.1 | |
| Papadopoulos et al 39 |
School closures not associated with a change in transmission: school closures not statistically significantly associated with a reduction in the total number of log cases or deaths |
Regression coefficient estimating the effect of school closures, and timing of school closures relative to first death, on log total cases and log total deaths | Univariate analysis of school closure policy showed no statistically significant association with log total cases (−0.03 (95% CI −0.256 to 0.218) or log total deaths (−0.025 (95% CI −0.246 to 0.211), p=0.776) Univariate analysis of timing of school closure was significantly associated with reductions in outcomes, so was considered in multivariate analysis. Multivariate analysis showed found no statistically significant association with log total cases (coefficient −0.006, CIs not reported) or deaths (−0.012 (95% CI −0.024 to 0.00), p=0.050) |
|
| Piovani et al 40 |
School closures associated with reduced transmission: earlier school closures associated with lower cumulative COVID-19 mortality |
Regression coefficient estimating % change in cumulative mortality for every day school closures delayed | Every 1 day delay in school closures was associated with an increase of 4.37% (95% CI 1.58 to 7.17), p=0.002 in cumulative COVID-19 mortality over the study period | |
| Rauscher 42 |
School closures associated with reduced transmission: school closures were associated with fewer cases and fewer deaths |
Percentage point increase in the number of new cases and deaths for every day school closures were delayed (not clear over what period the outcome measure represents, assumed until end of study period on 27 April 2020 | Each day a state delayed school closures was associated with 0.3% higher cases (p<0.01) and 1.3% higher mortality (p<0.01) | Sensitivity analysis removing the seven states that only recommended school closures, but did not mandate them, did not significantly alter the findings. |
| Stokes et al 46 |
School closures associated with mixed effect on transmission: school closures not statistically significantly associated with a reduction in mortality from 0 to 24 days after the first death, but associated with a reduction in the 14–38 days after |
Regression coefficient estimating effect of school closure timeliness and stringency on the daily mortality rate per 1 000 000 population | 0–24 days: −0.119 (95% CI −1.744 to 0.398) 14–38 days: −1.238 (95% CI −2.203 to –0.273) No observable trend by stringency of school closure measure (recommended vs partial closure vs full closure) |
Sensitivity analyses for lab-confirmed COVID-19 versus clinical diagnosis; and for using negative binomial regression analayses did not alter the findings. |
| Wu et al 47 |
School closures not associated with transmission: school closures not statistically significantly associated with R |
Output from Bayesian mechanistic model in the format: learnt weight (95% CI) Estimating effect of school closures on R | School closures not statistically significantly associated with Rt in any of the clusters, or when data are aggregated without clustering No clusters: 0.047 (95% CI –0.118 to 0.212) Cluster 1: 0.081 (95% CI –0.246 to 0.408) Cluster 2: 0.060 (95% CI –0.209 to 0.329) Cluster 3: 0.112 (95% CI –0.292 to 0.516) Cluster 4: 0.098 (95% CI –0.194 to 0.390) Cluster 5: 0.038 (95% CI –0.134 to 0.210) |
|
| Yang et al 48 |
School closures associated with reduced transmission: school closures and early years settings closures statistically significantly associated with reductions in R |
% reduction in R | School closure associated with 37% reduction in R (95% CI 33% to 40%) Daycare closures associated with 31% reduction (26%–35%) |
Sensitivity analysis using mortality data to derive Reff did not significantly alter findings Secondary analysis using data from google found that 32% (95% CI 28% to 34%) of the effect of school closures was explained by changes in workplace mobility. |
| Yehya et al 49 |
School closures associated with reduced transmission: earlier school closures were associated with reductions in COVID-19 mortality at 28 days |
Regression coefficient estimating increase in mortality at 28 days associated with each day school closures were delayed | 5% (Mortality Rate Ratio 1.05, 95% CI 1.01 to 1.09) | Sensitivity analyses for starting exposure from first COVID-19 death, or for excluding New York/New Jersey from analysis, did not significantly change the findings. |
| Zeilinger et al 50 |
School closures associated with reduced transmission: school closures associated with a reduction in growth rate of COVID-19 cases |
Growth rate calculated as the ratio of cumulative cases from 1 day to the next, applying a 7-day moving mean to smooth out weekday effects | School closures associated with drop in predicted growth rate between 10 and 40 days after implementation, median drop 0.010 (not clear what this value equates to but relatively large compared with other NPIs) | |
| School closures—within-area before-after comparison studies (n=7) | ||||
| Gandini et al 23 |
School (re-)closures not associated with a change in transmission: reclosing schools not associated with a change in the rate of decline of R |
Plotting Rt over time with school reclosure timings noted Analysed the effect of reclosing schools on Rt, which was done proactively before national lockdown in two large provinces | Lombardy and Campania closed schools before the national school closures in November. In both cases, they find that Rt started to decline around 2 weeks before school closures, and the rate of decline did not change after school closures | Mitigation measures in place in reopened schools included: temperature checks, hand hygiene, increased cleaning and ventilation, one-way systems, mask mandates, social distancing and bans on school sports/music. |
| Iwata et al 29 |
School closures not associated with a change in transmission: school closures not statistically associated with the incidence rate of new cases |
Time series analysis coefficient estimating effect of school closures on the change in daily incidence rate | 0.08 (95% CI −0.36 to 0.65) | Sensitivity analysis for different lag times did not change the general finding of null effect. |
| Matzinger and Skinner 37 |
School closures associated with reduced transmission: school closures were associated with reductions in the doubling time of new COVID-19 cases, hospitalisations and deaths |
Changes to the doubling time of the epidemic in each state, following school closures | Georgia: 7 days after school closures the doubling time slowed from 2.1 to 3.4 days Tennessee: 8 days after school closures the doubling time slowed from 2 to 4.2 days Mississippi: 10–14 days after school closures the doubling time slowed from 1.4 to 3.5 days |
Only included Georgia, Tennessee and Mississippi in their explicit analysis of school closure effect because these were the only states where the authors felt there was a long enough gap between implementation of school closures and other NPI measures. However, they show several figures of other states that initiated school closures at the same time as other lockdown measures. In these states (Arizona, Florida, Ilinois, Maryland, Massachussetts, New Jersey, New York and Texas), a similar pattern is observed for doubling time of cases, with time lags varying between 1 and 2 weeks. Patterns appeared to be similar for hospitalisations and deaths, although these data were not always reported, and more difficult to interpret. |
| Neidhofer and Neidhofer 38 |
School closures associated with reduced transmission: school closures were associated with reductions in COVID-19 mortality |
% Reduction in deaths in the 18 days postschool closure, compared with synthetic control unit | Argentina: 63%–90% reduction, Italy: 21%–35% reduction, South Korea: 72%–96% reduction in daily average COVID-19 deaths over the 18 days following school closures, compared with the counterfactual | Sensitivity analysis using only excess mortality in Italy reached similar conclusion Selected Argentina, Italy and South Korea because they closed schools at a different time to enacting national lockdown. Supplementary analysis of: Switzerland, Germany, the Netherlands, Indonesia, Canada, Brazil, France, UK, Spain, where school closure was implemented relatively later, and alongside other NPIs:
|
| Shah et al 53 |
School closures associated with mixed effect on transmission: in Italy, school closures were associate with a reduction in mortality. In the other four countries no aassociation was found between school closures and mortality |
Regression coefficient for effect of school closures on mortality (not explained in any greater detail) | Italy 0.81 (95% CI 0.68 to 0.97) Reported only as ‘no association’ for other countries |
|
| Sruthi et al 43 |
School closures associated with reduced transmission: secondary school closure was associated with a reduction in Rt |
Changes to time-varying reproductive number R, estimated from data on new cases. Assumed to be in an infectious state for 14 days from diagnosis | Secondary school closures associated with an average reduction of Rt around 1.0 | |
| Stage et al 44 |
School closures associated with reduced transmission: school closures associated with reductions in the growth rate of new cases |
% reduction in growth rate of new cases (Germany only—in Denmark and Norway the graph is drawn without formal statistical analysis) | 26%–65% reduction in growth rate of cases across the different states of Germany. No quantitative estimate for Norway or Denmark but authors report a ‘clear drop’ in new cases after school closures | |
| School closures—pooled multiple-area comparisons of interventions in place at a fixed time point (n=3) | ||||
| Juni et al 31 |
School closures associated with reduced transmission: school closures were statistically significantly associated with a relative reduction in the incidence rate of COVID-19 |
Regression coefficient estimating effect of school closures on changes to the incidence rate | Adjusted model: 0.77 (95% CI 0.63 to 0.93), p=0.009 |
Sensitivity analyses of seperating out high income countries did not significantly effect the results. |
| Walach and Hockertz 52 |
School closures associated with increased transmission: school closures associated with an increase in COVID-19 mortality |
Regression coefficient estimating effect of school closures on the COVID-19 mortality rate | Cases: school closures not associated with cases in univariate analysis so not considered for modelling Mortality: 2.54 (95% 1.24 to 3.85), p<0.0001 |
|
| Wong et al 51 |
School closures associated with reduced transmission: school closures were associated with a smaller rate of increase in cumulative incidence of COVID-19 |
Regression coefficient estimating effect of school closures on the rate of increase in cumulative incidence | −0.53 (95% CI −1.00 to –0.06), p=0.027 | Report no collinearity or interactions between different covariables in the model. |
| School reopening studies (n=11) | ||||
| Beesley 16 |
School reopenings associated with a mixed effect on transmission: school reopening was associated with increases in the 7-day rolling average of new cases in most countries, but not all |
Change in 7-day rolling average of new cases | China saw no change. Austria, Canada, France, Germany, Israel, Japan, the Netherlands, Singapore, Spain, Switzerland and the UK saw increases after 24–47 days; with longer lag times attributed to these countries opening schools in a limited to staggered way | Primary versus secondary: in the Netherlands, it was noted that the rise in cases 24 days after primary schools opened was much smaller than the rise 40 days after secondary schools reopened. |
| Ehrhardt et al 22 |
School reopenings not associated with a change in transmission: school reopenings not associated with any change in the rate of new cases |
Presentation of an epidemic curve showing daily confirmed new cases, with school reopening date labelled | Daily new cases peaked at 1400/day and dropped to around 100/day at the time of staggered school reopening. Daily new cases remained at, or generally below, this level throughout the following 3 months until after schools broke up for summer holidays | Range of comprehensive infection prevention and control measures were in place in schools at the time of school reopening. |
| Gandini et al 23 |
School reopenings not associated with a change in transmission: timing of school reopenings not consistently associated with onset of increases in R |
Plotting R over time with school reopening timings noted. Pairing geographically neighbouring and socioeconomically similar provinces who reopened schools at different times. Comparing time between school reopening and subsequent increases in R—measured as the start of 3 consecutive weeks of increasing R | Bolzano opened schools a week earlier than Trento, but Trento saw a sustained rise in R 1 week ealier than Bolzano. In Abruzzo and Marche; Sicily and Calabria; and Veneto and Apulia; one province reopened schools a week before the other, but Rt increases occured at the same time | Mitigation measures in place in reopened schools included: temperature checks, hand hygiene, increased cleaning and ventilation, one-way systems, mask mandates, social distancing and bans on school sports/music. |
| Garchitorena et al 24 |
School reopenings not associated with a change in transmission: partial relaxations of school closure measures associated with a null effect on COVID-19 transmission |
Ratio of transmission rates with and without implementation of the NPI (assessed over the duration of the NPI being in place) Presented as a forest plot so the reported results here are estimated | EY settings: 0% (95% CI −8% to 8%) Primary schools: 2% (95% CI −7% to 10%) Secondary schools: 1% (95% CI −7% to 9%) |
|
| Harris et al 25 |
School reopenings not associated with a change in transmission: school reopenings not statistically significantly associated with an increase in COVID-19 hospitalisation rate |
Regression coefficient reported for both hospitalisations per 100 000 population, and log total hospitalisations | Hospitalisations per 100 000 population: 0.295 (95% CI −0.072 to 0.662) Log total hospitalisations: −0.019 (95% CI −0.074 to 0.036) |
Post hoc stratified analysis showed a statistically significant increase in hospitalisations for those counties in the top 25% of hospitalisation preschool reopenings, but no effects for those <75th centile. |
| Ingelbeen et al 27 |
School reopenings associated with increased transmission: R increased after schools were reopened |
Plotted R compared against the changes to the NPIs in place during the study period | R started to increase from approximately 1 week before schools reopened (from 0.9 to 1 at reopening), and then increase more sharply to 1.5 over the next fortnight | Also used the national contact tracing data to examine age-specific trends in number of contacts per case, and number of transmission events between age groups. The increase in Rt after school reopening did not appear to be driven by school-aged children, but by general increases in social mixing across all age groups. |
| Isphording et al 28 |
School reopenings not associated with a change in transmission: school reopenings not statistically significantly associated with a change in rate of new COVID-19 cases |
Regression coefficient estimating change in number of new cases per 100 000 in the 3 weeks postschool reopenings | Reduction of 0.55 cases per 100 000 associated with first 3 weeks of reopening schools. CIs reported only graphically, but upper estimate just crosses 0 (ie, reopening schools led to non-sginificant reduction in transmission of COVID-19) | Sensitivity analysis showed this to be true for all age groups. West German counties drove the non-significant reduction in transmission associated with reopening of schools, while in East Germany the rate of new cases remained constant. |
| Li et al 35 |
School reopenings associated with increased transmission: school reopenings associated with an increase in Rt across the 28 days following reopening |
Ratio between R while NPI in place, and R on the last day of the previous time period. Reported at 7, 14 and 28 days (as well as visual representation of each individual day to demonstrate trend) | Day 7: 1.05 (95% CI 0.96 to 1.14) Day 14: 1.18 (95% CI 1.02 to 1.36) Day 28: 1.24 (95% CI 1.00 to 1.52) |
|
| Sruthi et al 43 |
School reopenings associated with mixed effect on transmission: secondary school reopening not associated with increase in Rt if mask mandates in place within schools |
Changes to time-varying reproductive number R, estimated from data on new cases. Assumed to be in an infectious state for 14 days from diagnosis | Secondary schools reopened with mask mandates in place associated with no change in the R, compared with secondary schools being closed Secondary schools reopened without mask mandates in place associated with an approximate 1.0 increase in R |
|
| Stein-Zamir et al 45 |
School reopenings associated with increased transmission: school reopenings were associated with an increase in new cases of COVID-19 |
Presentation of an age-stratified epidemic curve showing confirmed cases of COVID-19 in Jerusalem, by date, and comparing to dates of school closure/reopening | Difficult to elicit exact effect sizes from the epidemic curve, but approximately 2 weeks after schools started to reopen, the number of new cases started to increase | Increases in cases after school reopening was more pronounced in younger age groups,10–19 but were also seen across all ages to a lesser extent. |
| Stage et al 44 |
School reopenings not associated with transmission: school reopening not associated with increases in the growth rate of hospitalisations or cases |
Changes to the incidence rate and changes to instantaneous growth rate in hospitalisations (Denmark) and cases (Denmark, Germany and Norway) | In Germany, the growth rate of cases remained stable throughout and after the staggered reopening of schools. In Denmark and Norway, the growth rate of cases (and hospitalisations for Denmark) remained stable and negative, meaning that incidence continued to reduce despite school reopening | |
| School holiday studies (n=3) | ||||
| Beesley 16 |
School holidays associated with a mixed effect on transmission: school holidays were associated with increases in the 7-day rolling average of new cases in most countries, but not all |
Change in 7-day rolling average of new cases | In Austria, France, Germany and Switzerland, it was noted that school holidays ‘exacerbated’ the resurgence in incidence rate (not commented on for other countries) Sweden saw a reduction in the rolling average 23 days after they closed for summer holidays (the rolling average peaked within that 23-day period) |
|
| Bjork et al 17 |
School holidays associated with increased transmission: timing of a school winter holiday during the exposure period was positively associated with all-cause excess mortality |
All-cause weekly excess mortality per million residents, between 30 March 2020 and 7 June 2020 compared with 2015–2019 mortality rates, compared with regions with no winter holiday or a holiday in the week before the exposure period | Winter holiday in weeks 7, 8, 9 and 10 associated with weekly excess mortality of 13.4 (95% CI 9.7 to 17.0), 5.9 (95% CI 2.3 to 9.5), 13.1 (95% CI 9.7 to 16.5) and 6.2 (95% CI 1.0 to 11.4) per million residents, respectively | The comparator group included those holidaying in week 6 or not at all, and was itself associated with excess mortality of 8.6 (95% CI 6.9 to 10.3). |
| Pluemper and Neumayer 41 |
School holidays associated with increased transmission: school holidays associated with increases in the incident growth rate |
Percentage point increase in the incident growth rate associated with each week of the summer holiday | Each week of summer school holidays increased the incident growth rate by an average of 0.72 percentage points (95% 0.41 to 1.03). The effect of individual weeks increased during the holidays, such that the first 3 weeks were not indpendently statistically significant, but the sixth week of holidays was associated with an average 1.91 (95% CI 1.47 to 2.42) percentage points increase, which accounts for 49% of the national average growth rate that week | Larger effect sizes for richer regions, and regions with more foreigners, suggesting these regions had a higher proportion of travellers going abroad (the baseline rate in Germany was low at the start of the summer holidays). |
CrI, credible interval; NPI, non-pharmaceutical intervention.
Figure 2.
Main findings, stratified by risk of bias. (A) The studies’ response to the question: Did school closures reduced community transmission? (Yes, No, Mixed). (B) The studies’ response to the question: Did school reopenings increase community transmission? (Yes, No, Mixed).
Narrative synthesis of findings
School closures
Pooled multiple-area before-after comparisons
We identified 22 studies14 15 18–21 24 26 30 32–36 39 40 42 46–50 that analysed before-after data on multiple geographical units, and then pooled the results into one unified estimate of effect (generally by using regression analysis). These studies relied on different timings of NPI implementation in different areas to establish their independent effects, and were therefore at risk of collinearity if compared areas implemented the same NPIs at similar times. These studies were also at risk of bias from sociocultural differences between compared areas.
Of these studies, 1114 24 32 34–36 40 42 48–50 reported that school closures were associated with significantly reduced community transmission of SARS-CoV-2, 715 18 20 26 30 39 47 reported no association and 419 21 33 46 reported mixed findings. Those studies found to be at higher risk of bias, generally because they were judged not to have adjusted appropriately for NPIs, testing or sociodemographic data, tended to report reductions in transmission; whereas those studies at lower risk of bias were as likely to report null effects as they were reductions (see figure 2).
Of the three studies20 using this approach which were considered to be at the lowest risk of confounding, two reported no association and one reported that school closures reduced transmission. Courtemanche et al20 used a fixed effects model (to account for interarea sociodemographic differences) in an event study design to estimate the effect of NPIs (including school closures) on SARS-CoV-2 incidence in US counties between March and April 2020. They adjusted for relevant NPIs, testing regime confounders and underlying trends in each counties’ growth rates, and reported a null effect of school closures on growth rate, applying a lag of either 10 or 20 days. Hsiang et al26 used a reduced form of econometric regression to compare changes in incidence in French regions, Italian regions and US states (in three separate analyses) before and after NPI implementation (including school closures) until early April 2020. Other key NPIs and testing regimes were adjusted for. The authors report a null effect of school closures on growth rate of SARS-CoV-2 incidence, with narrow CIs for France and the USA, but a regression coefficient suggestive of a non-significant preventative effect in Italy (−0.11 (95% CI −0.25 to 0.03)). Li et al54 used the’EpiForecast’ model of R54 to estimate the effectiveness of different NPIs (including school closures) over time in 131 countries between January and June 2020. They identified time periods in which the NPIs in a given country were static, and calculated the ‘R ratio’ by dividing the average daily R of each period by the R from the last day of the previous period. They reported pooled estimates, regressed across all countries, for the first 28 days after introduction/relaxation of each NPI. Although the CIs for each daily effect size included 1, the trend was clearly towards a reduction in transmission following school closure implementation.
Within-area before-after comparisons
We identified seven studies23 29 37 38 43 44 53 that compared community transmission of SARS-CoV-2 before and after school closure for single geographical units, and did not pool the results with those of other areas. This approach controls for confounding from population sociodemographic factors, but remains vulnerable to confounding from other NPIs and temporal changes to testing regimes. As with the pooled before-after comparison studies, those studies at higher risk of bias from confounding were more likely to report reductions in transmission associated with school closures.
One study using this approach was found to be at moderate risk of bias. Matzinger et al37 identified the three US states which introduced school closures first, and with a sufficient lag before implementing other measures to assess their specific impact. They plotted incidence rates on a log2 scale and identified points of inflexion in the period after school closure. This assumes exponential growth in the absence of interventions, which may not have occurred given changes to testing regimes. The doubling time of new cases in Georgia slowed from 2.1 to 3.4 days 1 week after closing schools. Similar results were observed in Tennessee (2.0 to 4.2 days after 1 week) and Mississippi (1.4 to 3.4 days after 2 weeks). The authors also noted inflexion points for hospitalisations and mortality at later time points, although numerical changes were not reported. Tennessee showed a slowing in hospitalisations 1 week after cases, and mortality 1 week after hospitalisation. Mississippi showed a slowing in hospitalisations and mortality at the same time, 1 week after cases—the authors do not comment on this discrepancy. Georgia lacked early hospitalisation data to make such a comparison.
Pooled multiple-area comparisons of interventions in place at a fixed time point
Three studies31 51 52 considered countries from around the world using a design in which NPIs were considered as binary variables on a specific date (ie, in place or not in place), and the cumulative incidence or mortality to that point was compared with the number of new cases of COVID-19 over a subsequent follow-up period; countries were then compared using regression analysis to elicit independent effect sizes for individual policies including school closures. This approach reduces bias from different testing regimes over time and between countries. However, the use of a single cut-off date for whether school closure was in place means that the effects of long-standing and recent school closures were pooled, introducing misclassification bias. Two of these studies31 51 were at serious risk of bias and reported that school closures were associated with lower incidence; and one study52 was at critical risk of bias and reported that closing schools was not associated with incidence but was associated with increased mortality. Each of these studies was at high risk of confounding from other NPIs, in addition to the risk of misclassification bias described above.
School reopening studies
Eleven studies16 22–25 27 28 35 43–45 considered the effect of school reopening on subsequent SARS-CoV-2 community transmission.24 Of these, five were pooled multiple-area before-after comparison studies,24 25 28 35 43 and six were within-area multiple-area before-after comparison studies.16 22 23 27 44 45 These studies benefited from more staggered lifting of restrictions (compared with their implementation), and more stable testing regimes.
Of the four studies at a lower risk of bias,24 25 28 35 three24 25 28 reported that schools were reopened without associated increases in transmission, while one35 reported increased transmission. Garchitorena et al24 compared incidence data, with adjustment for underdetection, from 32 European countries, using multivariate linear regression models with adjustment for other NPIs and fixed effects to account for intercountry sociodemographic differences. They reported no association with incidence rates up to 16 September 2020 of reopening early years settings (0% mean change in incidence rate (95% CI −8% to 8%)), primary schools (2% (95% CI −7% to 10%)), or secondary schools (−1% (95% CI −7% to 9%)). Harris et al25 estimated the effect of school reopenings on COVID-19 hospitalisation in the USA using an event study model, with analysis at the county-level. They adjusted for other NPIs, and used fixed effects to account for calendar week effects and intercounty differences. They applied a 1-week lag period, and compared data from 10 weeks before to 6 weeks after school reopenings. They initially report null effects when pooling the effects across all counties, however, post hoc sensitivity analyses suggested that there were increases in hospitalisations for counties that were in the top 25% of baseline hospitalisation rate at school reopening (compared with null effects for the bottom 75%). Isphording et al28 compared changes to the COVID-19 incidence rate in German counties that were first to reopen schools after the summer holidays, with those yet to reopen (noting that the timing of such decisions was set years in advance, and not changed due to the pandemic). They considered data from 2 weeks before to 3 weeks after school reopenings, and adjusted for mobility data, and used fixed effects to account for intercounty sociodemographic differences. They reported no association between school reopenings and incidence. One study Li et al,35 is described above as it reports on the effect of both school closures and school reopenings around the world. As for school closures, their effect sizes for each individual day in the 28-day period postschool reopenings were not always statistically significant, but the data trend is clearly that of an increase in transmission associated with school reopenings.
The seven studies16 22 23 27 43–45 at serious and critical risk of confounding are more difficult to interpret, again predominantly due to the high risk of confounding. Three16 23 44 reported no association between school reopening and transmission, two22 43 reported mixed findings and two27 45 reported increased transmission following reopening of schools.
School holiday studies
Three studies16 17 41 reported changes in SARS-CoV-2 community transmission associated with school holidays. These holidays occurred according to predetermined timetables and are therefore unlikely to be influenced by background trends in infections. Two studies examined associations between timing of summer holidays on incidence rates in Germany41 and in multiple European countries,16 respectively. The other study17 reported on the timing of the February/March 2020 half-term break timing in countries that neighbour the Alps. Of these, one reported mixed findings on the effect of summer holidays,16 and two reported that school holidays were associated with increased transmission.17 41 The authors of these studies considered the primary exposure to be increased social contact from international travel, rather than decreases from the temporary closure or schools.
Different school setting types
One school closure study,48 three school reopening studies16 22 44 and one study looking at closures and reopenings24 considered evidence of independent effects for different types of school closures.
Two studies reported independent effect sizes for different settings, but found considerable overlap between the effect sizes, and noted high temporal correlation between the policy timings meaning that collinearity limits the interpretability of the findings. Garchitorena et al24 (moderate risk of bias) reported the effect of both school closures and school reopenings on changes to R in 32 European countries, with almost completely overlapping estimates of transmission reductions associated with closures in early years settings, primary schools and secondary schools; and equally null effects for each setting associated with reopenings. Yang et al48 (moderate risk of bias) reported that school closures in US counties (presumed primary and secondary combined) were associated with 37% (95% CI 33% to 40%) reductions in R, compared with 31% reductions for early years settings (95% CI 26% to 35%).
Two studies reported staggered reopenings of different school settings, generally with younger children students returning first, and a week or two between each reopenings. Both studies found null effects on transmission overall, and therefore did not report any differential effect by setting type. Stage et al44 (serious risk of bias) noted staggered reopenings in Norway, Denmark and Germany. Ehrhardt et al22 (critical risk of bias) noted staggered reopenings of schools in Baden-Wuttemberg (a region of Germany).
Beesley16 (critical risk of bias) noted that increases in the 7-day rolling average of new cases were greater in the 40 days after secondary school reopening than they were in the 24 days following primary schools reopening. However, this study is at high risk of confounding from other NPIs, and it is not clear why the chosen (and different) lag periods were applied.
Discussion
We identified 40 studies that provided a quantitative estimate of the impact of school closures or reopening on community transmission of SARS-CoV-2. The studies included a range of countries and were heterogenous in design. Among higher quality, less confounded studies of school closures, 6 out of 14 reported that school closures had no effect on transmission, 6 reported that school closures were associated with reductions in transmission, and 2 reported mixed findings (figure 2); with findings ranging from no association to a 60% relative reduction in incidence and mortality rate.14 Most studies of school reopening reported that school reopening, with extensive infection prevention and control measures in place and when the community infection levels were low, did not increase community transmission of SARS-CoV-2.
The strength of this study is that it draws on empirical data from actual school closures and reopenings during the COVID-19 pandemic and includes data from 150 countries. By necessity, we include observational rather than randomised controlled studies, as understandably no jurisdictions have undertaken such trials. We were unable to meta-analyse due to study heterogeneity. We were unable to meaningfully examine differences between primary and secondary schools as very few studies distinguished between them, despite the different transmission patterns for younger and older children. Data are also lacking from low-income countries, where sociocultural factors may produce different effects of school closures on transmission to high-income settings, leaving a substantial gap in the evidence base. Data in these studies come exclusively from 2020, and many studies report only up to the summer months, it is therefore unclear whether our findings are robust to the effects of new SARS-CoV-2 variants and vaccines.
A major challenge with estimating the ‘independent’ effect of school closures, acknowledged by many of the studies, is disentangling their effect from other NPIs occurring at the same time. While most studies tried to account for this, it is unclear how effective these methods were. Even where adjustment occurred there is a risk of residual confounding, which likely overestimated preventative associations; and collinearity (highly correlated independent variables meaning that is impossible to estimate specific effects for each) which could bias results towards or away from the null. One exception was a paper by Matzinger and Skinner,37 which focused on three US states that implemented school closures first and without co-interventions, and reported a twofold increase in the time for cases to double 1 week after school closures. However, it is possible that the benefits observed here may be attributable, at least in part, to a ‘signalling effect’ with other changes to social mobility (eg, working from home) being prompted by school closures. Another approach, although ineligible for inclusion in our study, is to examine transmission data for breakpoints, and then work backwards to see what NPIs were in place at the time. Two studies that did this found that transmission started to drop following other NPIs, before school closures were implemented, and found no change in the gradient of decline after school closures in Switzerland55 and Germany.56 This may suggest school closures have different effects when implemented first, or on top of other restrictions, perhaps due to a broader signalling effect that the first implemented NPI has on societal mobility patterns. The true independent effect of school closures from the first wave around the world may simply be unknowable.
In contrast, lifting of NPIs in the summer of 2020 (including school reopenings) generally occurred in a more staggered way, and on a background of stable testing regimes and outcome ascertainment. Good-quality observational studies considering data from across 32 European countries,24 Germany alone28 and the USA25 all demonstrated that school reopenings can be successfully implemented without increasing community transmission of SARS-CoV-2, where baseline incidence is low and robust infection prevention and control measures are in place. This finding is in keeping with several studies showing little or no effect of school reopening on intraschool transmission rates.6 57 58 However, the US-based study did comment that those counties with the highest 25% of baseline hospitalisations at the time of reopenings (above 40 admissions per 100 000 population per week) did see an increase in transmission following school reopenings, although the bottom 75% of counties did not see any effect. This may explain why the other school reopening study at lower risk of bias35 reported a clear, although non-significant, trend towards school reopenings being associated with increases in transmission rates across 131 countries worldwide, with the authors noting “we were unable to account for different precautions regarding school reopening that were adopted by some countries” before citing Israel as an example where an uptick in transmission occurred following reopening, and where ‘students were in crowded classrooms and were not instructed to wear face masks’.
The variability in findings from our included studies are likely to reflect issues with study design. However, this may also suggest that there is no single effect of school closures and reopenings on community transmission and that contextual factors modify the impact of closures in different countries and over time. If the purpose of school closures is reduction in social contacts among children, the level of social mixing between children that occurs outside school once schools are closed is likely to be a key determinant of their effect at reducing community transmission. This will be influenced by other NPIs, and other key contextual factors including background prevalence of infection, use of preventive measures in schools prior to closures, age of children affected as well as sociodemographic and cultural factors.
Different countries have adopted different approaches to controlling COVID-19. Early in the pandemic school closures were common, and in some places were one of the first major social distancing measures introduced. The effectiveness of the overall bundle of lockdown measures implemented is proven, but the incremental benefit of school closures remains unclear. In contrast, only one of the four studies of school reopenings assessed at a lower risk of bias reported an increase in community transmission. Collectively, the evidence around school reopenings, while more limited in size, tends to suggest that school reopenings, when implemented during periods of low incidence and accompanied by robust preventive measures, are unlikely to have a measurable impact on community transmission. Further research is needed to validate these findings and their generalisability, including with respect to new variants. These findings are highly important given the harmful effects of school closures.3 4 Policymakers and governments need to take a measured approach before implementing school closures in response to rising infection rates, and look to reopen schools, with appropriate mitigation measures in place, where other lockdown measures have successfully brought community transmission of SARS-CoV-2 under control.
Supplementary Material
Footnotes
Twitter: @seb_walsh, @jackmbirch
Contributors: SW, CW, CBo, RMV and OTM designed the review protocol. SW, AC, VB, SR and JMB screened articles for inclusion, assessed risk of bias and performed data extraction. SW and OTM drafted the manuscript. All authors commented on the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplemental information. All included data in this systematic review are already in the public domain.
Ethics statements
Patient consent for publication
Not required.
References
- 1.UNESCO . Global monitring of school closures caused by COVID-19 [Internet]. Education:From disruption to recovery, 2020. Available: https://en.unesco.org/covid19/educationresponse [Accessed 18 Dec 2020].
- 2.Unicef . Framework for reopening schools, 2020. [Google Scholar]
- 3.UNESCO . Adverse consequences of school closures [Internet], 2020. Available: https://en.unesco.org/covid19/educationresponse/consequences [Accessed 18 Dec 2020].
- 4.Viner R, Russell S, Saulle R. Impacts of school closures on physical and mental health of children and young people: a systematic review. medRxiv 2021:1;2021.02.10.21251526http://medrxiv.org/content/early/2021/02/12/2021.02.10.21251526.abstract [Google Scholar]
- 5.ECDC . COVID-19 in children and the role of school settings in COVID-19 transmission. Stockholm, 2020. [Google Scholar]
- 6.Ismail SA, Saliba V, Lopez Bernal J, et al. SARS-CoV-2 infection and transmission in educational settings: a prospective, cross-sectional analysis of infection clusters and outbreaks in England. Lancet Infect Dis 2021;21:344–53. 10.1016/S1473-3099(20)30882-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Viner RM, Mytton OT, Bonell C, et al. Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: a systematic review and meta-analysis. JAMA Pediatr 2021;175:143–56. 10.1001/jamapediatrics.2020.4573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Panovska-Griffiths J, Kerr CC, Stuart RM, et al. Determining the optimal strategy for reopening schools, the impact of test and trace interventions, and the risk of occurrence of a second COVID-19 epidemic wave in the UK: a modelling study. Lancet Child Adolesc Health 2020;4:817–27. 10.1016/S2352-4642(20)30250-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang SL, Harding N, Zachreson C, et al. Modelling transmission and control of the COVID-19 pandemic in Australia. Nat Commun 2020;11:5710. 10.1038/s41467-020-19393-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davies NG, Kucharski AJ, Eggo RM, et al. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. Lancet Public Health 2020;5:e375–85. 10.1016/S2468-2667(20)30133-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Viner RM, Russell SJ, Croker H, et al. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health 2020;4:397–404. 10.1016/S2352-4642(20)30095-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile APP for systematic reviews. Syst Rev 2016;5:210. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Auger KA, Shah SS, Richardson T, et al. Association between statewide school closure and COVID-19 incidence and mortality in the US. JAMA 2020;324:859–70. 10.1001/jama.2020.14348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Banholzer N, van WE, Kratzwald B, et al. Estimating the impact of non-pharmaceutical interventions on documented infections with COVID-19: A cross-country analysis [Internet]., 2020. Available: https://medrxiv.org/cgi/content/short/2020.04.16.20062141
- 16.Beesley R. The role of school reopening in the spread of COVID-19 [Internet], 2020. Available: https://medrxiv.org/cgi/content/short/2020.09.03.20187757
- 17.Bjork J, Mattisson K, Ahlbom A. Excess mortality across regions of Europe during the first wave of the COVID-19 pandemic - impact of the winter holiday travelling and government responses [Internet]., 2020. Available: https://medrxiv.org/cgi/content/short/2020.11.24.20237644 [DOI] [PMC free article] [PubMed]
- 18.Brauner JM, Mindermann S, Sharma M, et al. The effectiveness and perceived burden of nonpharmaceutical interventions against COVID-19 transmission: a modelling study with 41 countries [Internet], 2020. Available: https://medrxiv.org/cgi/content/short/2020.05.28.20116129
- 19.Chernozhukov V, Kasahara H, Schrimpf P. Causal impact of masks, policies, behavior on early covid-19 pandemic in the U.S. J Econom 2021;220:23–62. 10.1016/j.jeconom.2020.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Courtemanche C, Garuccio J, Le A, et al. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff 2020;39:1237–46. 10.1377/hlthaff.2020.00608 [DOI] [PubMed] [Google Scholar]
- 21.Dreher N, Spiera Z, McAuley FM, et al. Impact of policy interventions and social distancing on SARS-CoV-2 transmission in the United States [Internet]., 2020. Available: https://medrxiv.org/cgi/content/short/2020.05.01.20088179 [DOI] [PMC free article] [PubMed]
- 22.Ehrhardt J, Ekinci A, Krehl H, et al. Transmission of SARS-CoV-2 in children aged 0 to 19 years in childcare facilities and schools after their reopening in may 2020, Baden-Württemberg, Germany. Eurosurveillance 2020;25. 10.2807/1560-7917.ES.2020.25.36.2001587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gandini S, Rainisio M, Iannuzzo ML. No evidence of association between schools and SARS-CoV-2 second wave in Italy. [Internet], 2020. Available: https://medrxiv.org/cgi/content/short/2020.12.16.20248134
- 24.Garchitorena A, Gruson H, Cazelles B, et al. Quantifying the efficiency of non-pharmaceutical interventions against SARS-COV-2 transmission in Europe [Internet], 2020. Available: https://medrxiv.org/cgi/content/short/2020.08.17.20174821
- 25.Harris D, Ziedan E, Hassig S. The effects of school Reopenings on COVID-19 hospitalizations, 2021. [Google Scholar]
- 26.Hsiang S, Allen D, Annan-Phan S, et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 2020;584:262–7. 10.1038/s41586-020-2404-8 [DOI] [PubMed] [Google Scholar]
- 27.Ingelbeen B, Peckeu L, Laga M. Reducing contacts to stop SARS-CoV-2 transmission during the second pandemic wave in Brussels. Belgium, 2020. https://medrxiv.org/cgi/content/short/2020.12.23.20248795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Isphording I, Lipfert M, Pestel N. School Re-Openings after summer breaks in Germany did not increase SARS-CoV-2 cases, 2020. [Google Scholar]
- 29.Iwata K, Doi A, Miyakoshi C. Was school closure effective in mitigating coronavirus disease 2019 (COVID-19)? time series analysis using Bayesian inference. International Journal of Infectious Diseases 2020;99:57–61. 10.1016/j.ijid.2020.07.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jamison J, Bundy D, Jamison D, et al. Comparing the impact on COVID-19 mortality of self-imposed behavior change and of government regulations across 13 countries [Internet]., 2020. Available: https://medrxiv.org/cgi/content/short/2020.08.02.20166793 [DOI] [PMC free article] [PubMed]
- 31.Jüni P, Rothenbühler M, Bobos P, et al. Impact of climate and public health interventions on the COVID-19 pandemic: a prospective cohort study. Can Med Assoc J 2020;192:E566–73. 10.1503/cmaj.200920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Klimek-Tulwin M, Tulwin T. Early school closures can reduce the first-wave of the COVID-19 pandemic development. Z Gesundh Wiss 2020:1–7. 10.1007/s10389-020-01391-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Krishnamachari B, Dsida A, Zastrow D, et al. Effects of Government Mandated Social Distancing Measures on Cumulative Incidence of COVID-19 in the United States and its Most Populated Cities [Internet], 2020. Available: https://medrxiv.org/cgi/content/short/2020.05.22.20110460
- 34.ML L, Bouardi HT, Lami OS, et al. Forecasting COVID-19 and Analyzing the Effect of Government Interventions [Internet], 2020. Available: https://medrxiv.org/cgi/content/short/2020.06.23.20138693
- 35.Li Y, Campbell H, Kulkarni D, et al. The temporal association of introducing and lifting non-pharmaceutical interventions with the time-varying reproduction number (R) of SARS-CoV-2: a modelling study across 131 countries. Lancet Infect Dis 2021;21:193–202. 10.1016/S1473-3099(20)30785-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu Y, Morgenstern C, Kelly J, et al. The impact of non-pharmaceutical interventions on SARS-CoV-2 transmission across 130 countries and territories. BMC Med 2021;19:40. 10.1186/s12916-020-01872-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Matzinger P, Skinner J. Strong impact of closing schools, closing bars and wearing masks during the Covid-19 pandemic: results from a simple and revealing analysis. medRxiv : the preprint server for health sciences 2020. [Google Scholar]
- 38.Neidhofer C, Neidhofer G. The effectiveness of school closures and other pre-lockdown COVID-19 mitigation strategies in Argentina, Italy, and South Korea. ZEW Discussion Paper [Internet]., 2020. Available: https://pesquisa.bvsalud.org/portal/resource/en/mdl-20203403367
- 39.Papadopoulos DI, Donkov I, Charitopoulos K, et al. The impact of lockdown measures on COVID-19: a worldwide comparison [Internet], 2020. Available: https://medrxiv.org/cgi/content/short/2020.05.22.20106476
- 40.Piovani D, Christodoulou MN, Hadjidemetriou A, et al. Effect of early application of social distancing interventions on COVID-19 mortality over the first pandemic wave: an analysis of longitudinal data from 37 countries. J Infect 2021;82:133–42. 10.1016/j.jinf.2020.11.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pluemper T, Neumayer E. Summer School Holidays and the Growth Rate in Sars-CoV-2 Infections Across German Districts [Internet]., 2020. Available: https://medrxiv.org/cgi/content/short/2020.10.11.20210773
- 42.Rauscher E. Lower State COVID-19 Deaths and Cases with Earlier School Closure in the U.S. [Internet]., 2020. Available: https://medrxiv.org/cgi/content/short/2020.05.09.20096594
- 43.Sruthi CK, Biswal MR, Joshi H, et al. How Policies on Restaurants, Bars, Nightclubs, Masks, Schools, and Travel Influenced Swiss COVID-19 Reproduction Ratios [Internet]., 2020. Available: https://medrxiv.org/cgi/content/short/2020.10.11.20210641
- 44.Stage HB, Shingleton J, Ghosh S, et al. Shut and re-open: the role of schools in the spread of COVID-19 in Europe [Internet], 2020. Available: https://medrxiv.org/cgi/content/short/2020.06.24.20139634 [DOI] [PMC free article] [PubMed]
- 45.Stein-Zamir C, Abramson N, Shoob H, et al. A large COVID-19 outbreak in a high school 10 days after schools’ reopening, Israel, May 2020. Eurosurveillance 2020;25:2001352. 10.2807/1560-7917.ES.2020.25.29.2001352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stokes J, Turner AJ, Anselmi L, et al. The relative effects of non-pharmaceutical interventions on early Covid-19 mortality: natural experiment in 130 countries [Internet]., 2020. Available: https://medrxiv.org/cgi/content/short/2020.10.05.20206888 [DOI] [PMC free article] [PubMed]
- 47. Wu JY, Killeen BD, Nikutta P, et al. Changes in Reproductive Rate of SARS-CoV-2 Due to Non-pharmaceutical Interventions in 1,417 U.S. Counties [Internet]., 2020. Available: https://medrxiv.org/cgi/content/short/2020.05.31.20118687
- 48.Yang B, Huang AT, Garcia-Carreras B, et al. Effect of specific non-pharmaceutical intervention policies on SARS-CoV-2 transmission in the counties of the United States [Internet]., 2020. Available: https://medrxiv.org/cgi/content/short/2020.10.29.20221036 [DOI] [PMC free article] [PubMed]
- 49.Yehya N, Venkataramani A, Harhay MO. Statewide interventions and Covid-19 mortality in the United States: an observational study. Clin Infect Dis 2020. 10.1093/cid/ciaa923. [Epub ahead of print: 08 Jul 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zeilinger EL, Nader IW, Jomar D, et al. Onset of effects of non-pharmaceutical interventions on COVID-19 worldwide [Internet], 2020. Available: https://medrxiv.org/cgi/content/short/2020.09.02.20185660 [DOI] [PMC free article] [PubMed]
- 51.Wong MC, Huang J, Teoh J, et al. Evaluation on different non-pharmaceutical interventions during COVID-19 pandemic: an analysis of 139 countries. J Infect 2020;81:e70–1. 10.1016/j.jinf.2020.06.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Walach H, Hockertz S. What association do political interventions, environmental and health variables have with the number of Covid-19 cases and deaths? A linear modeling approach [Internet], 2020. Available: https://medrxiv.org/cgi/content/short/2020.06.18.20135012
- 53.Shah S, Ray B, Holy C, et al. Co3 effectiveness of government measures to reduce COVID-19 mortality across 5 different countries. Value in Health 2020;23:S400–1. 10.1016/j.jval.2020.08.018 [DOI] [Google Scholar]
- 54.Abbott S, Hellewell J, Thompson RN. Estimating the time-varying reproduction number of SARS-CoV-2 using national and subnational case counts [version 2; peer review: 1 approved with reservations].. Wellcome Open Research [Internet] 2020;5https://wellcomeopenresearch.org/articles/5-112/v2 [Google Scholar]
- 55.Lemaitre JC, Perez-Saez J, Azman AS, et al. Assessing the impact of non-pharmaceutical interventions on SARS-CoV-2 transmission in Switzerland. Swiss Med Wkly 2020;150:w20295. 10.4414/smw.2020.20295 [DOI] [PubMed] [Google Scholar]
- 56.Wieland T. Change points in the spread of COVID-19 question the effectiveness of nonpharmaceutical interventions in Germany [Internet], 2020. Available: https://medrxiv.org/cgi/content/short/2020.07.05.20146837
- 57.Varma JK, Thamkittikasem J, Whittemore K, et al. COVID-19 infections among students and staff in New York City public schools. Pediatrics 2021;147:e2021050605. 10.1542/peds.2021-050605 [DOI] [PubMed] [Google Scholar]
- 58.Zimmerman KO, Akinboyo IC, Brookhart MA, et al. Incidence and secondary transmission of SARS-CoV-2 infections in schools. Pediatrics 2021;147:e2020048090. 10.1542/peds.2020-048090 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-053371supp001.pdf (64.6KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplemental information. All included data in this systematic review are already in the public domain.