Abstract
Purpose of Review
Chronic thromboembolic pulmonary hypertension (CTEPH), included in group 4 PH, is an uncommon complication of acute pulmonary embolism (PE), in which emboli in the pulmonary vasculature do not resolve but rather form into an organized scar-like obstruction which can result in right ventricular (RV) failure. Here we provide an overview of current diagnosis and management of CTEPH.
Recent Findings
CTEPH management is complex with treatments that range from surgery, percutaneous interventions, to medical therapies. Current CTEPH medical therapies have largely been repurposed from pulmonary arterial hypertension (PAH).
Summary
The diagnosis of CTEPH can be challenging, requiring a multimodality approach to differentiate from disease mimics. While these treatments improve symptoms, they may not reverse the underlying pathology of CTEPH.
Keywords: Chronic thromboembolic pulmonary hypertension, Pulmonary embolism, Pulmonary hypertension, Pulmonary endarterectomy, Balloon pulmonary angioplasty
Introduction
The estimated prevalence of acute pulmonary embolism (PE) in the USA is about 112 cases per 100,000 [1]. With treatment, most cases of acute PE resolve with minimal abnormalities and normal hemodynamics [2, 3]. However, approximately 0.57–18.1% of patients develop “post-PE syndrome,” defined as persistent functional, exercise tolerance, and quality of life impairments [4–12]. These persistently symptomatic patients who have residual pulmonary vascular obstruction fall into two main groups: chronic thromboembolic disease (CTED) and chronic thromboembolic pulmonary hypertension (CTEPH). CTED is defined as having imaging evidence chronic pulmonary thromboembolism, exercise limitation, but normal resting cardiopulmonary hemodynamics [13]. CTEPH (0.79–3% of all PE survivors) is characterized by persistent obstruction of the pulmonary vasculature by organized fibrotic thrombi and associated pulmonary vascular remodeling, leading to pulmonary hypertension (PH) and increased right ventricular (RV) afterload, and ultimately to RV failure [14–16].
Risk Factors
Thrombophilia
CTEPH patients have higher frequency of elevated factor VIII and antiphospholipid antibodies, where beta-2 glycoprotein, lupus anticoagulant or anticardiolipin antibodies are reported to be 10 to 24% [17–20]. They also have decreased ADAMTS13 and increased von Willebrand factor levels, persisting even after pulmonary endarterectomy (PEA) [21]. However, there is no alteration in antithrombin, protein C or protein S, factor V Leiden levels, or activated protein C resistance [22].
Intravascular Device
Indwelling venous catheters, especially with recurrent placement, pacemaker and defibrillator leads, and ventriculoatrial shunts increase risk of CTEPH.
Acute PE Characteristics and Clinical Factors
CTEPH development is correlated with a systolic pulmonary artery (PA) pressure >50 mmHg at the time of acute PE diagnosis and hospital discharge, larger clot burden, recurrent PE, and diagnostic delay [5, 7, 23–27].
Miscellaneous Factors
These include non-O blood types [17, 23, 28], splenectomy [29], inflammatory conditions [30], hypothyroidism, thyroid replacement [23, 31], and malignancies [23, 31].
Clinical Presentation of CTEPH
Symptoms
CTEPH patients can present similarly to pulmonary arterial hypertension (PAH). Thus, it is incumbent to rule out CTEPH in all patients with PH. Typical symptoms include dyspnea on effort and impaired effort tolerance. Other symptoms include fatigue, exercise-induced chest discomfort, exercise-induced dizziness, or even syncope. Untreated, symptoms can progress. Delayed diagnosis is associated with advanced symptoms consistent with RV failure [32]. While there is often an antecedent history diagnostic or suggestive of a thromboembolic event, the absence of such a history should not rule out the possibility of CTEPH [33]. Indeed, at least 25% of patients with CTEPH had no prior history of venous thromboembolism [34].
Physical Examination
In early disease, the physical examination may be normal. More often, signs of PH on cardiac examination are present, including accentuated P2, right-sided 3rd and 4th heart sounds, tricuspid valve regurgitation (TR) (pansystolic, blowing, louder on inspiration), and pulmonic valve regurgitation (PR) (decrescendo diastolic murmur best heard over the pulmonic valve area), and RV lift. The presence of PR, and RV lift are suggestive of severe PH. With TR, the jugular venous pulse (JVP) exhibits prominent CV waves, and the liver may be pulsatile. An RV lift is suggestive of RV enlargement and can be appreciated by placing the heel of the hand over the left parasternal border. In advanced cases, signs of RV failure may be present (elevated JVP, dependent edema with or without ascites, and congestive hepatomegaly). Of note, a flow bruit over the lung fields due to turbulent flow through partially obstructed and/or recanalized pulmonary arteries may be heard in about 30% of cases, a finding that can be seen in other rare conditions such as pulmonary arteriovenous malformations and peripheral pulmonic stenosis [35].
Diagnosis and Workup
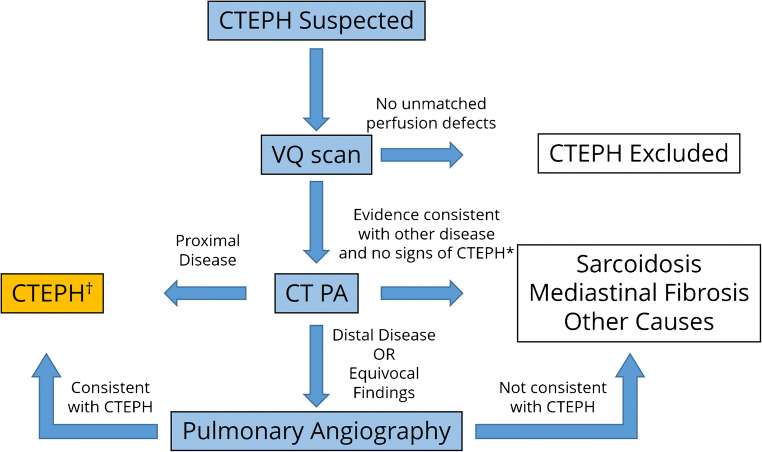
Similar to PAH, the diagnosis of CTEPH is often delayed and is commonly overlooked in the evaluation of patients with exertional dyspnea. In the case of CTEPH, further diagnostic testing is needed to determine whether patients fulfill criteria for surgical management or other treatment modalities [36, 37]. A general approach for the diagnosis of CTEPH is shown in Figure 1.
Figure 1.
Approach to CTEPH diagnosis. Patients with suspected CTEPH should first undergo a VQ scan, which can effectively rule out the disease due to its high sensitivity. Due to the low specificity of VQ scan, the next step is a CTPA, which confirms the diagnosis of CTEPH in patients with proximal disease. For patients with distal disease, pulmonary angiography aids in the planning of PTE or BPA at expert centers. *Some patients may have findings on CTPA consistent with alternative diagnoses, such as sarcoidosis or mediastinal fibrosis, in the absence of other typical CTEPH findings, such as mosaicism and bronchial collaterals.
Chest Radiograph
This can show enlarged main and central pulmonary arteries, which can exhibit regional differences in size, as well as RV enlargement. Hypolucent areas suggestive of diminished regional vascularity may be evident [38].
Ventilation/Perfusion (V/Q) Scan
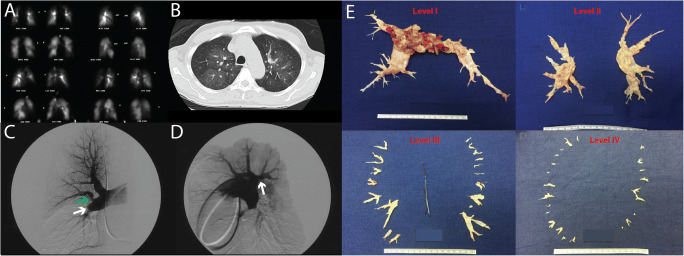
The V/Q scan is integral to the screening and workup of CTEPH [39]. A normal V/Q scan essentially rules out CTEPH with a negative predictive value of 100% [40]. In IPAH, the V/Q scan can be normal, have a “mottled” appearance, or subsegmental defects [41]. With CTEPH, the V/Q scan shows segmental or larger mismatched perfusion defects (Figure 2A). A positive V/Q scan is insufficient for diagnosis or estimation of the disease burden. Due to recanalization or remodeling of occluded vessels allowing for the penetration of radioisotope into the periphery with distal perfusion, the V/Q scan can underestimate the extent of disease [43]. Thus, a single segmental mismatch should raise suspicion for possible CTEPH. Additionally, other conditions can produce abnormal V/Q scans similar to that seen in CTEPH, including pulmonary venoocclusive disease, pulmonary artery sarcoma, pulmonary vasculitis, fibrosing mediastinitis, and sarcoidosis (see Conditions Simulating CTEPH below). Additional modalities are needed to confirm the diagnosis and evaluate the disease burden [44].
Figure 2.
Imaging and thrombus in CTEPH. A V/Q scan in the same patient showing multiple bilateral mismatched defects. B CT scan showing clear vascular mosaicism. C The white arrow highlights an angiographic “pouch” occlusion of the right interlobar vessel. The presence of organized thromboembolic disease is also evident by “web” narrowing of the proximal anterior upper lobe artery (green arrow). D The lateral right pulmonary arteriogram in the same patient shows another “web” narrowing (white arrow) of the proximal posterior upper lobe vessel not appreciated on the AP films. (The figure was published in Fedullo PF, Auger WR. “Medical Management of the Thoracic Surgery Patient”, 2010 pp: 477-482, copyright Elsevier [2010]) [37]. E University of California San Diego classification of PEA disease levels with illustrative figures for each level (Reprinted with permission of the American Thoracic Society. Copyright © 2021 American Thoracic Society. All rights reserved. Madani M, M. E. Ann Am Thorac Soc, 2016, 13 Suppl 3, S240-S247. Annuals of the American Thoracic Society is an official journal of the American Thoracic Society.) [42].
Computed Tomographic (CT) Pulmonary Angiography (CTPA)
CTPA is an important adjunct to the V/Q scan for evaluating disease burden and identifying parenchymal changes and potential disease mimics [45]. Compared to central defects noted in acute PE, CTPA findings of CTEPH include enlargement of central pulmonary arteries, as well as eccentric thrombus in the central, lobar, and segmental pulmonary arteries. Sensitivity and specificity for modern CT technology are 89–100% and 95–100% for main and lobar pulmonary arteries, respectively, and 84–100% and 92–99% for segmental pulmonary arteries, respectively [46–48]. The CTPA can reveal lesions such as webs, abrupt reduction in vessel diameter, pulmonary artery stenosis, bronchial artery collaterals, vascular mosaicism (Figure 2B), and linear scars suggestive of old pulmonary infarcts [49–52]. However, modern CTPA is limited in characterizing distal vessels and subsegmental disease. A normal CTPA does not exclude CTEPH. CTPA is sufficient for diagnosing proximal CTEPH, determining disease burden and operability. If distal disease is suspected, additional imaging modalities may be required.
Digital Subtraction Angiography (DSA)
DSA is the gold standard for CTEPH diagnosis and commonly used to determine operability for pulmonary thromboendarterectomy (PEA). Even in severe PH, risk of contrast-induced vasodilation and hemodynamic consequences are not increased [53]. Different angiographic patterns have been described: pouch defects, webs, bands or strictures, intimal irregularities, abrupt PA narrowing, and obstruction of lobar (proximal) and segmental (proximal/distal) vessels at their origin [54] (Figure 2 C and D). While CTPA studies are generally sufficient for determining operability, DSA can help determine surgical accessibility and suitability for balloon pulmonary angioplasty (BPA).
Echocardiography
Transthoracic echocardiography (TTE) is utilized to evaluate RV morphology and function and is a primary screening tool for PH [39]. RV hypertrophy with evidence of pressure-volume overload, leftward displacement of the interventricular septum, depressed tricuspid annular plane systolic excursion (TAPSE), and elevated PA systolic pressure are all common findings in PH [55], but do not differentiate CTEPH from other forms of PH.
Heart Catheterization
Right heart catheterization (RHC) is imperative for accurate assessment of cardiopulmonary hemodynamic and diagnosis of PH. CTEPH is defined as persistent organized thrombi after 3 months of anticoagulation and evidence of precapillary PH on RHC [13, 30, 32, 56, 57] with mPAP > 20 mmHg, pulmonary capillary wedge pressure (PCWP) ≤ 15 mmHg, and PVR > 3 wood units [58]. In patients with significant symptoms but normal resting hemodynamics, RHC can be accompanied by exercise to determine the presence of exercise PH (ePH) which may reflect early CTEPH [59–61]. In patients over the age of 50 years, coronary angiography or coronary CT angiography to exclude underlying coronary artery disease is often performed (as concomitant bypass surgery could be performed at the time of PEA). In patients younger than 50 undergoing PEA, significant coronary artery disease (CAD) was found only in those individuals with ≥ 3 risk factors of diabetes, hypertension, hyperlipidemia, obesity, tobacco use, or a family history of CAD [62].
CTED vs CTEPH
While patients with CTED may share similar symptoms and perfusion defects to patients with CTEPH, they do not demonstrate evidence of PH at rest on RHC [63, 64]. The reasons for effort dyspnea and exercise capacity limitation in CTED are not fully understood. ePH [60, 61] can account for limitations in some patients. On cardiopulmonary exercise tests, parameters suggesting increase in dead space fraction may be evident (e.g., increased slope of VE to VCO2). The natural history of CTED is not known or whether some patients with CTED progress to CTEPH. Selected reports suggest that PEA in highly symptomatic CTED patients leads to good outcomes [60, 63, 65]. Such treatment decisions need to be individualized.
Conditions Mimicking CTEPH
Pulmonary artery sarcoma is a very rare tumor that can simulate CTEPH [66, 67] and can be associated with hemoptysis, significant weight loss, fever, marked elevation in sedimentation rate, and anemia. Up to 75% arise from the pulmonary trunk and are mostly at the supravalvular level. Clues on imaging include hyperdense non-homogenous lesions that can distend the pulmonary vasculature, gadolinium enhancement on MRA, and fluorodeoxyglucose-avid on positron emission tomography (PET). Extravascular spread can also be seen in patients with advanced disease. Pulmonary artery in situ thrombosis has been well-described in Eisenmenger’s syndrome, in advanced parenchymal and airway disease with dilated pulmonary arteries, and even in severe PAH. In situ thrombosis is often nonobstructive, occurs in proximal and distal vessels, and appears as a smooth lining thrombus in a dilated vessel. In longstanding cases, calcification can be seen. In sarcoidosis, abnormal V/Q scans can be noted as well as some CT angiographic features associated with CTEPH (webs, intimal irregularities, abrupt vessel cut-off, and post-stenotic dilation) [68]. Fibrosing mediastinitis can cause compression and obstruction of the pulmonary vasculature (arteries and veins) [69] and with longstanding compression can result in pulmonary hypertension [70] resulting in large segmental mismatches on V/Q scan. Large vessel pulmonary vasculitis, such as Takayasu’s arteritis, giant cell arteritis, and Behçet's disease, can mimic CTEPH [71]. The presence of bruits over large systemic arteries and clinical features such as constitutional symptoms and evidence of other systemic vascular involvement can be seen. Some features on angiography which suggest vasculitis include a beaded appearance of the pulmonary arteries and circumferential concentric thickening with post-contrast enhancement [72].
Treatment Approaches
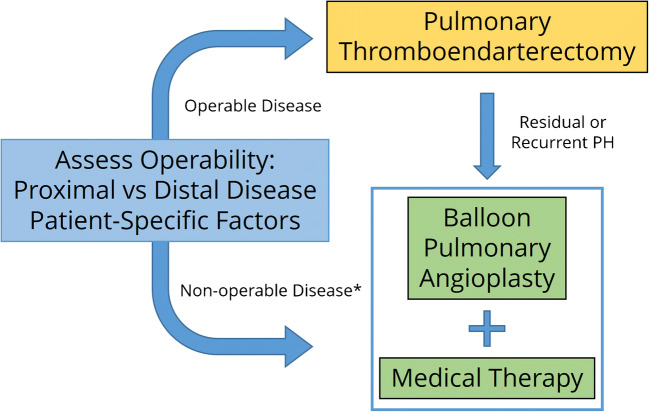
Patients with untreated CTEPH likely progress in severity due to the presence of small vessel disease both distal to but importantly away from the culprit sites of obstruction [73]. Progressive disease can culminate in worsening RV function and ultimately right heart failure. Before the advent of therapies, the 5-year survival was 30% when mPAP >40 mmHg and 10% when mPAP >50 mmHg [74]. This is in marked contrast to outcomes after PEA, with current in-hospital mortality rates <5%, and survival >90% at 1 year, and >70% at 10 years [75]. Thus, treatment should be carefully considered for all patients [76]. A general algorithm for CTEPH management is shown in Figure 3.
Figure 3.
Approach to CTEPH management. For patients with operable disease, PTE surgery is the gold standard treatment. For those with non-operable disease (*must be confirmed at CTEPH center), an approach of BPA and medical therapy can be used. Some patients who were not initially operable candidates due to medical illness may improve with BPA and medical therapy to the point where they can undergo PTE surgery.
Treatment of CTEPH
Anticoagulation
All patients with CTEPH should receive systemic anticoagulation, as this prevents recurrence of thromboembolic events and in situ PA thrombosis [3]. There are limited data comparing warfarin to DOACs in CTEPH. In one retrospective analysis, there was an equivalent rate of bleeding events and no statistical survival difference in patients receiving DOAC or warfarin [77•], but there was a higher rate of recurrent thrombosis in patients receiving DOAC. There are no data comparing indefinite anticoagulation compared to a shorter length of therapy compared to no therapy in CTEPH. Based on data extrapolated from acute PE literature, indefinite anticoagulation is recommended to prevent recurrent thromboembolic disease [13].
Inferior Vena Cava (IVC) Filters
There are no data supporting routine IVC filter use for management of CTEPH, and registry data show no differences in outcome for patient undergoing PEA with or without an IVC filter [78]. The current standard-of-care for most centers is to forego the insertion of an IVC filter prior to PEA unless there is a contraindication to anticoagulation [78].
Pulmonary Thromboendarterectomy (PEA)
PEA is the mainstay of treatment for CTEPH as it is the only potentially curative treatment modality. Assessment of operability should be directed by a multidisciplinary team at high-volume centers [79].
Determining Surgical Candidacy
This is based on severity of symptoms, surgical accessibility, severity of PH and RV dysfunction, correlation of severity of PH to the degree of obstruction, anticipated technical challenges, comorbidities, and patient preference [80]. Surgical accessibility is predominantly determined by level of obstruction as defined by pulmonary angiography or CTPA. Clot in the main, lobar, or proximal segmental PAs is generally more amenable to intervention, whereas distal segmental and subsegmental involvement presents more surgical challenges. In the latter, other approaches, such as BPA, may be more appropriate. In cases of vasculopathy with significant inaccessible distal disease burden, resection of proximal clot may not lead to a meaningful decrease in PVR. Surgical outcomes are closely linked to PVR reduction, and a persistently elevated postoperative PVR is associated with inability to wean from bypass, hemodynamic instability, early death, and poor long-term outcomes [42, 81]. Acceptable outcomes have been achieved in patients in their 70s and 80s deemed good surgical candidates [80]. While most patients who undergo PEA have a PVR in the range of 800–1200 C dynes/sec/cm5 (10–15 Wood units), there is no upper limit to the PVR or severity of RV dysfunction. In the case of CTED patients with significant dyspnea or ePH, PEA has had good results in selected patients [60, 65, 79].
Surgical Levels of Disease
Surgical levels of disease for CTEPH are classified according to those proposed by the University of California San Diego (UCSD) CTEPH group [80]. These are classified as follows (and depicted in Figure 2E):
Level 0: No evidence of thromboembolic disease in either lung
Level 1: Chronic thromboembolism (CTE) starting in the main pulmonary arteries (level C: complete occlusion of one main pulmonary artery with CTE)
Level 2: CTE starting at the level of lobar arteries or in the main descending pulmonary arteries
Level 3: CTE starting at the level of the segmental arteries
Level 4: CTE starting at the level of the subsegmental arteries
PEA Surgical Procedure
PEA is best performed at expert centers, defined by a volume of cases > 50/year, expertise to perform segmental PEA, operative mortality < 5%, and multi-specialty expertise with alternative treatment modalities. An approach via median steronotomy is superior to a thoracotomy as it avoids entering the pericardium and collateral vessels from the bronchials and other vessels. Cardiopulmonary bypass facilitates hemodynamic stability and assists with cooling the patient during periods of circulatory arrest. The PEA procedure is best carried out under a bloodless field to allow optimal definition of the endarterectomy plane and continue the dissection more distally. Thus, the patient is cooled to 20°C for periods of 20 min to facilitate optimal dissection. Identification of the correct endarterectomy plane is critical, as too superficial a plane results in an inadequate result and a plane that is too deep can risk tearing the artery with resultant uncontrollable bleeding and death. Once the correct plane is established, the specimen is then followed distally to the feathered tail end in each branch. Incomplete resection can result in minimal or no hemodynamic improvement in pulmonary pressures and PVR. In recent years, a major advance is the ability to perform distal endarterectomy in carefully selected cases [75, 80, 82].
Postoperative Management Principles
Postoperative management principles are employed similar to post-bypass cardiac surgery patients. With mechanical ventilation, the aim is to keep plateau pressures below 30 cm of water pressure. With prolonged periods of cardiopulmonary bypass, hypothermia and circulatory arrest-induced metabolic acidosis may be present in the early postoperative period. Fluid administration is minimized as patients commonly have a significantly positive postoperative fluid balance. DVT prophylaxis is begun on the evening of surgery and is typically replaced by therapeutic anticoagulation with heparin when the chest tube output is < 50 ml/h for 2 consecutive hours. Atrial arrhythmias occur in about 20–30% of patients postoperatively [83, 84].
Postoperative Complications and Management
Some of these are common to other cardiac surgery procedures such as pleural effusion, bleeding, arrhythmias, and wound infection. There are a number of potential PEA-specific complications. A steal phenomenon can occur because of loss of hypoxic vasoconstriction and diversion of blood to regions of low vascular resistance that results in low V/Q regions that contribute to hypoxemia. This generally resolves over weeks to months which can facilitate weaning patients off supplemental oxygen following hospital discharge [85, 86]. Reperfusion pulmonary edema (RPE) is a form of high permeability edema that results from increased perfusion to endarterectomized vessels, perioperative ischemia, inflammation, and ventilator-associated lung injury. This can range in severity from mild to profound alveolar hemorrhage. Initial rates of reperfusion pulmonary edema for PEA were approximately 30–40%. With improved techniques and experience, the rate of reperfusion pulmonary edema has reduced to approximately 9.6% [79]. Most cases (60%) occur immediately following surgery, with 30% of cases presenting within 48 h and 10% after 48 h [85]. The management of RPE is generally supportive as in other forms of permeability edema. Rescue therapies such as inhaled nitric oxide, inhaled epoprostenol, prone positioning, paralytics, and, if necessary, venovenous extracorporeal membrane oxygenation (ECMO) may be used [87–89]. Re-thrombosis can be seen in patients with unilateral disease, especially in the setting of surgery for complete occlusion [80]. Pericardial effusion occurs more frequently than following other cardiac surgery surgeries due to the presence of anticoagulation, possible lymphatic disruption, and diminution in cardiac size. Placement of a posterior pericardial drain or window may prevent pericardial morbidity [37]. Residual postoperative PH is an important contributor to perioperative mortality [90]. In these cases, a wide pulmonary pulse pressure is commonly observed [37]. This often resolves within 72 h [91, 92], and use of inhaled nitric oxide or inhaled epoprostenol may be of value. By contrast, irreversible PH likely reflects persistent distal disease not adequately attended to and/or small vessel remodeling away from areas of obstruction, i.e., small vessel vasculopathy of non-occluded vessels.
Outcomes Following PEA
The in-hospital mortality has steadily improved with rates down to 2.2% reported in 2012 [14]. The 3-year survival for CTEPH patients undergoing PEA is 90% compared to 70% in those not having surgery [13, 78]. Functional class after 1 year was class I or II in 90% of patients [93]. The 5-year and 10-year survival following PEA is 82% and 75%, respectively [79] and is paralleled by improvements in hemodynamics, 6MWD, functional class (FC), and RV and left ventricle (LV) ejection fractions [94, 95]. Among operable patients who did not undergo surgery, 5-year survival is 53%, and among inoperable patients, it is 59% [96]. Residual PH (despite good macroscopic endarterectomy results) following PEA is approximately 11–35%. Depending on the definition used, residual PH is more often due to underlying small vessel vasculopathy or remodeling and not a direct consequence of residual or recurrent large vessel obstruction [97].
Balloon Pulmonary Angioplasty (BPA)
Introduction
Although BPA in patients with CTEPH was first described in 2001 [98], its use became more widespread after several encouraging Japanese reports in 2012 [48, 99, 100]. With refinement of techniques, improved outcomes, and reduced complications, BPA has become an established procedure in major centers.
Identification and Workup for Appropriate Cases
BPA can be considered in CTEPH patients deemed technically inoperable or high risk for PEA [39] or in those with persistent or recurrent PH post-PEA. Segmental pulmonary angiography is generally used to identify lesions amendable to BPA, such as webs and slit-like lesions in the distal vasculature [101]. In the case of obstructed lesions, BPA may still be feasible provided there is antegrade or collateral flow past the lesion [79, 101]. Intravascular ultrasound or optical coherence tomography may have a role in reducing the frequency and severity of complications while allowing for intervention of more complex lesions [102, 103]. Generally, a staged procedure is preferred, often requiring 3–10 sessions per patient. Some centers prefer the use of smaller balloons for initial sessions followed by sequential dilations with subsequent sessions [99, 104]. Webs and ring-like stenoses tend to be easier to dilate, total occlusions have a low success rate but a low complication rate (likely because the wire cannot be passed), while subtotal occlusions have an intermediate success rate but a higher incidence of complications [105]. It is rare for a stenosis to recur at a site of successfully treated lesion; thus, stents are not employed.
Complications of BPA
Initially the incidence of RPE was significantly higher than with PEA in the range of 56–61%. With more experience, the incidence has decreased to 10–30% [99, 100, 106, 107]. In experienced centers, reperfusion edema is now a rare occurrence. Lung injury is now the most common complication due to wire injury, balloon overdilation, or high-pressure injection of contrast medium [108], with an incidence of 5.9–17.8% [109–111]. Minor hemoptysis likely reflects minor vascular injury and generally resolves spontaneously and has an incidence of 7–14% [110, 111]. Pulmonary artery perforation, dissection, and rupture are rare but serious complications. Immediate intervention with balloon tamponade, covered stent deployment, coil embolization, or gel foam instillation may be required to achieve hemostasis. In the Japanese and French series, the incidence was of perforation was 2.8–2.9%, dissection 0.4–1.9%, and rupture 0.1% [110, 111].
Outcomes of BPA
BPA has been reported to improve short- and long-term outcomes in multiple domains [13, 79, 106, 108, 110–113] (selected studies listed in Table 1). BPA has been associated with improvements in hemodynamics [110], 6MWD [112], cardiopulmonary exercise testing [114], RV systolic function [99, 100, 106, 107, 115, 116], and quality of life [106]. In the Japanese and French series, the 3-year survival following BPA was 94.5 and 95.1%, respectively [110, 111].
Table 1.
Selected studies of BPA with hemodynamic and other outcomes (since 2017)
| Study | N, population | mPAP, mmHg | PVR, WU | CI, L/min/m2 | 6MWD, m | WHO FC |
|---|---|---|---|---|---|---|
| Aoki (2017) (Japan) | N=424, before and 6 months after BPA | 38 ± 10 to 25 ± 6 | 7.3 ± 3.2 to 3.8 ± 1 | 2.7 ± 0.1 to 2.5 ± 0.5 | 380 ± 138 to 486 ± 112 | Pre-BPA 28%; not reported post-BPA |
| Ogawa (2017) (Japan) | N=308, before and immediately after BPA. | 43.2 ± 11 to 24.3 ± 6.4 | 10.6 ± 5.6 to 4.5 ± 2.8 | 2.6 ± 0.8 to 2.9 ± 0.7 | 318.1 ± 122.1 to 401.3 ± 104.8 | Median FC: 3 to 2 |
| Olsson (2017) (Germany) | N=56, before and 24 weeks after BPA | 40 ± 12 to 33 ± 11 | 7.4 ± 3.6 to 5.5 ± 3.5 | 2.4 ± 0.6 to 2.5 ± 0.6 | 358 ± 108 to 391 ± 108 | % of pts in WHO III/IV: 84% to 29% |
| Darocha (2017) (Poland) | N=22, before and immediately after BPA | 51.7 ± 10.6 to 35 ± 9.1 | 10.4 ± 3.9 to 5.5 ± 2.2 | 2.2 ± 0.5 to 2.5 ± 0.4 | 323 ± 135 to 410 ± 109 | % of pts in WHO III/IV: 96% to 20% |
| Kriechbaum (2018) (Germany) | N=51, before and 6 months after BPA | 39.5 ± 12.1 to 32.6 ± 12.6 | 6.4 ± 2.7 to 5 ± 2.3 | 2.5 ± 0.6 to 2.5 ± 0.5* | 375 to 308.5 | % of pts in WHO III/IV: 96% to 12% |
| Brenot (2019) (France) | N=79 from more recent period; before and 3-6 months after BPA | 43.6 ± 9.1 to 29.5 ± 7.7 | 7.5 ± 3 to 3.6 ± 2 | 2.73 ± 0.62 to 3.18 ± 0.68 | 407 ± 103 to 449 ± 86 | % of pts in WHO III/IV: 55.1% to 8% |
| Hoole (2020) (UK) | N=30, before and 3 months after BPA | 44.7 ± 11 to 34.4 ± 8.3 | 8.3 ± 3.5 to 5.5 ± 2.5 | CO: 4.4 ± 1.1 to 4.8 ± 1.1 | 366 ± 107 to 440 ± 94 | % of pts in WHO III/IV: 80% to 13% |
*Not statistically significant. Abbreviations: mPAP mean pulmonary artery pressure, PVR pulmonary vascular resistance, WU Wood units, CI cardiac index, 6MWD 6-min walk distance, WHO World Health Organization, FC functional class, CO cardiac output
Medical Management
Currently, those patients deemed non-operable would be considered for PH-targeted therapy with or without BPA [13]. Giving PH-directed medical therapies pre-PEA in patients who are surgical candidates is highly controversial and generally thought to merely delay the surgery with no postoperative benefits [117]. The medications that have been used to treat CTEPH are the same as those used for WHO group 1 PH (selected randomized controlled trials (RCTs) listed in Table 2).
Table 2.
Selected randomized controlled trials using PH-directed medical therapy in CTEPH
| Study | Medication | N, design; evaluation interval | 6MWD change, meters | mPAP change, mmHg | PVR change, dynes/sec/cm5 | CO change, L/min | NT-proBNP change, pg/mL | WHO FC change | Borg dyspnea score change |
|---|---|---|---|---|---|---|---|---|---|
| Ghofrani (2013) (CHEST-1) | Riociguat vs placebo in CTEPH | N=261, RCT; week 12 | 39 vs −6 | −4 vs 0.8 | -226 vs 23 | 0.8 vs −0.03 | −291 vs 76 | 33% vs 15% improved | −0.8 vs 0.2 |
| Simonneau (2015) (CHEST-2) | Riociguat vs placebo in CTEPH | N=211, 1 year follow-up of CHEST-1 | 59 vs 37 | Not reported | Not reported | Not reported | −375 vs −505 | 50% vs 39% improved | −0.8 vs −0.57 |
| Jais (2008) (BENEFiT) | Bosentan vs placebo in CTEPH | N=157, RCT; week 16 | 2.9 vs 0.8 | Placebo corrected −2.5* | −146 vs +30 | Placebo corrected CI +0.3 | Treatment effect −622 ng/L in favor of bosentan | 14.5% vs 11.3% improved* | −0.4 vs 0.2 |
| Ghofrani (2017) (MERIT-1) | Macitentan vs placebo in CTEPH | N=80, RCT, week 16 (hemodynamics) and week 24 (NT-proBNP, 6MWD) | 35 vs 1 | −3.5 vs −1.7 | −206 vs −86 | 0.76 vs −0.02 | −651 vs −360 | 0% worsened vs 8% worsened* | −0.1 vs −.3* |
| Escribano-Subias (2018) (AMBER-1) | Ambrisentan vs placebo in CTEPH | N=33, RCT; week 16 | 28.3 vs 6.8 | Not reported | −212.5 vs −108.5 | Not reported | Geometric mean −29.4% of baseline vs +14.1% of baseline | Not reported | Not reported |
| Suntharalingam (2008) | Sildenafil vs placebo in CTEPH | N=19, RCT; week 12 | 17.9 vs 0.4* | −5.8 vs 0.4* | −179 vs 18 | CI −0.1 vs −0.1* | −355 vs −77* | 100% vs 0% improved | −0.7 vs 0.2* |
| Sadushi-Kolici (2019) | High-dose vs low-dose subcutaneous treprostinil | N=105, RCT; week 24 | 45.4 vs 3.8 | −3.4 vs −0.4 | −214 vs 73 | 0.6 vs −0.2 | −157.5 vs 330.6 | 51% vs 17% improved | −0.4 vs −0.1* |
Soluble Guanylate Cyclase Stimulator
Riociguat, a guanylate cyclase stimulator, is currently the only FDA-approved therapy for CTEPH. Riociguat was evaluated in the CHEST-1 study, a randomized controlled trial of 261 patients with inoperable CTEPH or persistent pulmonary hypertension following PEA; the riociguat group demonstrated an increased 6MWD (+39 m vs −6 m in controls) and reduction in PVR. There were no significant adverse events [118]. This data was confirmed in the CHEST-2 long-term follow-up [119]. The subsequent RIVER trial, which evaluated hemodynamic benefits of riociguat in patients with PAH and CTEPH, found that after 1 year of treatment, there was a significant reduction in RA size, RV area, and RV thickness; an increase in TAPSE; and an increase in RV fractional area change [120].
Endothelin Receptor Antagonists (ERA)
The BENEFiT randomized controlled trial showed that bosentan improved PVR and CI but with no improvement in exercise capacity [121]. However, subsequent meta-analysis that included BENEFiT data suggested that there may be an increase in 6MWD and a decrease in mPAP [122]. The MERIT-1 randomized controlled trial evaluated of macitentan in NYHA FC III/IV patients with inoperable CTEPH demonstrated a significant 27% reduction of PVR with macitentan vs 12.8% in placebo along with an improvement of 6MWD (35 m vs 1 m with placebo) [123]. The AMBER-1 study was an RCT to evaluate ambrisentan for inoperable CTEPH. It also showed an improvement in 6WMD in the treatment arm (28 m vs 7 m), a marked decrease in NT-proBNP (−29.4% vs +14.1%), and a reduction in PVR. However, the trial was stopped early for futility of enrollment [124].
Phosphodiesterase-5 Inhibitors (PDE5i)
A small RCT examined sildenafil vs placebo for inoperable CTEPH and showed improved FC and PVR reduction with no change in exercise capacity [125]. Data for PDE5i are lacking in CTEPH and such patients should be treated with riociguat, as concomitant use of riociguat and PDE5i can cause profound hypotension and is contraindicated.
Prostanoids
In an RCT of treprostinil in 105 patients with inoperable or persistent/recurrent CTEPH following PEA and NYHA FC III/IV, patients were given high-dose vs low-dose subcutaneous treprostinil; the 6MWD improved by 45 m in the high-dose group and 4.3 m in the low-dose group, with similar rates of adverse events [126•]. Other smaller cohort and uncontrolled studies have shown hemodynamic benefit and improvement in exercise capacity for epoprostenol [127], survival (as compared to historical controls) and hemodynamic benefit for treprostinil [128], and improvement in exercise capacity, FC, symptoms, and quality of life in an RCT for iloprost for PH (of which CTEPH patients comprised 28% of the population) [129].
Combination Therapy
A retrospective study of dual upfront combination therapy (ERA + PDE5i vs riociguat) for inoperable CTEPH demonstrated an improvement in FC and 6MWD and reduction in mPAP and PVR. The effect was more pronounced with the combination of ERA + riociguat and ERA + tadalafil than ERA + sildenafil [130].
Medical Therapy Versus BPA
There have been two meta-analyses of BPA vs CTEPH medical therapies. Compared to placebo, both medical therapy and BPA showed a significant improvement in 6MWD, mPAP, and PVR; but, BPA showed more significant effects [131, 132]. The ongoing RACE trial is evaluating riociguat vs BPA for inoperable CTEPH (NCT02634203).
Combined Medical Therapy and BPA
The strategy of riociguat before BPA was evaluated in 36 patients in which riociguat was administered for 3 months before BPA. There was a significant initial improvement in FC and reduction in mPAP and PVR on riociguat, which improved further after BPA [133]. In a recently published study, BPA improved hemodynamics with an additional improvement in CO and reduction in PVR after 6 months of treatment with riociguat [134].
Conclusions
CTEPH remains a challenging and highly morbid condition. All patients who are surgical candidates should undergo PEA. Advances for non-operable patients, including the use of BPA alone or with medical therapies, have expanded with improved evaluation, techniques, and outcomes with decreased complications. However, many of these options have only been shown to improve short-term endpoints with little data on long-term outcomes. New approaches to prevent the development of CTEPH after acute PE and novel therapies for CTEPH are sorely needed.
Abbreviations
- 6MWD
6-min walk distance
- BNP
Brain natriuretic peptide
- BPA
Balloon pulmonary angioplasty
- CAD
Coronary artery disease
- CEC
Circulating endothelial cells
- CI
Cardiac index
- CO
Cardiac output
- CRP
C-reactive protein
- CT
Computed tomography
- CTED
Chronic thromboembolic disease
- CTEPH
Chronic thromboembolic pulmonary hypertension
- CTPA
Computed tomographic pulmonary angiography
- DECT
Dual energy computed tomography
- DOAC
Direct oral Anticoagulant
- DSA
Digital subtraction angiography
- DVT
Deep venous thrombosis
- ECG
Electrocardiogram
- ECMO
Extracorporeal membrane oxygenation
- ERA
Endothelin receptor antagonist
- ETT
Endotracheal tube
- FC
Functional class
- GLS
Global longitudinal strain
- ICU
Intensive care unit
- IPAH
Idiopathic pulmonary arterial hypertension
- IVC
Inferior vena cava
- JVP
Jugular venous pressure
- LV
Left ventricle
- mPAP
Mean pulmonary arterial pressure
- MMP-9
Matrix metalloproteinase-9
- MRI
Magnetic resonance imaging
- MRA
Magnetic resonance angiography
- NT-proBNP
N-terminal pro-brain natriuretic peptide
- PA
Pulmonary artery
- PAH
Pulmonary arterial hypertension
- PDE5i
Phosphodiesterase 5 inhibitor
- PE
Pulmonary embolism
- PEA
Pulmonary endarterectomy
- PFG
Pulmonary flow grade
- PH
Pulmonary hypertension
- PVR
Pulmonary vascular resistance
- RA
Right atrium
- RCT
Randomized controlled trial
- RHC
Right heart catheterization
- RPE
Reperfusion pulmonary edema
- RV
Right ventricle
- TAPSE
Tricuspid annular plane systolic excursion
- TR
Tricuspid regurgitation
- UCSD
University of California, San Diego
- V/Q
Ventilation/perfusion
- VO2
Peak oxygen consumption
- VE
Minute ventilation
- WHO
World Health Organization
Compliance with Ethical Standards
Conflict of Interest
Dr. Maron reports personal fees from Actelion, outside the submitted work. In addition, Dr. Maron has a patent US patent 9,605,047 issued, a patent US pending patent PCT/US2019/059890 pending, and a patent applications 62475955 and 029672 pending.
Dr. Tapson reports grants from Bayer and grants and personal fees from Janssen and Actelion, outside the submitted work.
Dr. Rajagopal reports grants and personal fees from Janssen and United Therapeutics and personal fees from Altavant, Apie Therapeutics, Bayer, Insmed, and Liquidia Technologies, outside the submitted work. In addition, Dr. Rajagopal has a patent US patent 62/673,175. “Dynamic 129Xe Gas Exchange Spectroscopy” licensed to Polarean Corporation.
The other authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Heart Failure
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Wiener RS, Schwartz LM, Woloshin S. Time trends in pulmonary embolism in the United States: Evidence of overdiagnosis. Arch Intern Med. 2011;171(9):831–837. doi: 10.1001/archinternmed.2011.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fedullo P, Kerr KM, Kim NH, Auger WR. Chronic thromboembolic pulmonary hypertension. Am J Respir Crit Care Med. 2011;183(12):1605–1613. doi: 10.1164/rccm.201011-1854CI. [DOI] [PubMed] [Google Scholar]
- 3.Piazza G, Goldhaber SZ. Chronic thromboembolic pulmonary hypertension. N Engl J Med. 2011;364(4):351–360. doi: 10.1056/NEJMra0910203. [DOI] [PubMed] [Google Scholar]
- 4.Sista AK, Miller LE, Kahn SR, Kline JA. Persistent right ventricular dysfunction, functional capacity limitation, exercise intolerance, and quality of life impairment following pulmonary embolism: Systematic review with meta-analysis. Vasc Med. 2017;22(1):37–43. doi: 10.1177/1358863X16670250. [DOI] [PubMed] [Google Scholar]
- 5.Klok FA, van Kralingen KW, van Dijk AP, Heyning FH, Vliegen HW, Huisman MV. Prospective cardiopulmonary screening program to detect chronic thromboembolic pulmonary hypertension in patients after acute pulmonary embolism. Haematologica. 2010;95(6):970–975. doi: 10.3324/haematol.2009.018960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guerin L, Couturaud F, Parent F, Revel MP, Gillaizeau F, Planquette B, et al. Prevalence of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism. Prevalence of CTEPH after pulmonary embolism. Thromb Haemost. 2014;112(3):598–605. doi: 10.1160/TH13-07-0538. [DOI] [PubMed] [Google Scholar]
- 7.Pengo V, Lensing AW, Prins MH, Marchiori A, Davidson BL, Tiozzo F, et al. Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. N Engl J Med. 2004;350(22):2257–2264. doi: 10.1056/NEJMoa032274. [DOI] [PubMed] [Google Scholar]
- 8.Klok FA, Dzikowska-Diduch O, Kostrubiec M, Vliegen HW, Pruszczyk P, Hasenfuss G, et al. Derivation of a clinical prediction score for chronic thromboembolic pulmonary hypertension after acute pulmonary embolism. J Thromb Haemost. 2016;14(1):121–128. doi: 10.1111/jth.13175. [DOI] [PubMed] [Google Scholar]
- 9.Ende-Verhaar YM, Cannegieter SC, Vonk Noordegraaf A, Delcroix M, Pruszczyk P, Mairuhu AT, et al. Incidence of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism: a contemporary view of the published literature. Eur Respir J. 2017;49(2). [DOI] [PubMed]
- 10.Konstantinides SV, Vicaut E, Danays T, Becattini C, Bertoletti L, Beyer-Westendorf J, et al. Impact of thrombolytic therapy on the long-term outcome of intermediate-risk pulmonary embolism. J Am Coll Cardiol. 2017;69(12):1536–1544. doi: 10.1016/j.jacc.2016.12.039. [DOI] [PubMed] [Google Scholar]
- 11.Ribeiro A, Lindmarker P, Johnsson H, Juhlin-Dannfelt A, Jorfeldt L. Pulmonary embolism: one-year follow-up with echocardiography doppler and five-year survival analysis. Circulation. 1999;99(10):1325–1330. doi: 10.1161/01.CIR.99.10.1325. [DOI] [PubMed] [Google Scholar]
- 12.Klok FA, van der Hulle T, den Exter PL, Lankeit M, Huisman MV, Konstantinides S. The post-PE syndrome: a new concept for chronic complications of pulmonary embolism. Blood Rev. 2014;28(6):221–226. doi: 10.1016/j.blre.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 13.Kim NH, Delcroix M, Jais X, Madani MM, Matsubara H, Mayer E, et al. Chronic thromboembolic pulmonary hypertension. Eur Respir J. 2019;53(1). [DOI] [PMC free article] [PubMed]
- 14.Madani MM, Auger WR, Pretorius V, Sakakibara N, Kerr KM, Kim NH, et al. Pulmonary endarterectomy: recent changes in a single institution's experience of more than 2,700 patients. Annals of Thoracic Surgery. 2012;94(1):97–103. doi: 10.1016/j.athoracsur.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 15.Klok FA, Couturaud F, Delcroix M, Humbert M. Diagnosis of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism. Eur Respir J. 2020;55(6). [DOI] [PubMed]
- 16.Coquoz N, Weilenmann D, Stolz D, Popov V, Azzola A, Fellrath JM, et al. Multicentre observational screening survey for the detection of CTEPH following pulmonary embolism. Eur Respir J. 2018;51(4):1702505. doi: 10.1183/13993003.02505-2017. [DOI] [PubMed] [Google Scholar]
- 17.Bonderman D, Turecek PL, Jakowitsch J, Weltermann A, Adlbrecht C, Schneider B, et al. High prevalence of elevated clotting factor VIII in chronic thromboembolic pulmonary hypertension. Thromb Haemost. 2003;90(3):372–376. doi: 10.1160/TH03-02-0067. [DOI] [PubMed] [Google Scholar]
- 18.Kyrle PA, Minar E, Hirschl M, Bialonczyk C, Stain M, Schneider B, et al. High plasma levels of factor VIII and the risk of recurrent venous thromboembolism. N Engl J Med. 2000;343(7):457–462. doi: 10.1056/NEJM200008173430702. [DOI] [PubMed] [Google Scholar]
- 19.Wolf M, Boyer-Neumann C, Parent F, Eschwege V, Jaillet H, Meyer D, et al. Thrombotic risk factors in pulmonary hypertension. Eur Respir J. 2000;15(2):395–399. doi: 10.1034/j.1399-3003.2000.15b28.x. [DOI] [PubMed] [Google Scholar]
- 20.Auger WR, Permpikul P, Moser KM. Lupus anticoagulant, heparin use, and thrombocytopenia in patients with chronic thromboembolic pulmonary-hypertension - a preliminary-report. American Journal of Medicine. 1995;99(4):392–396. doi: 10.1016/S0002-9343(99)80187-9. [DOI] [PubMed] [Google Scholar]
- 21.Newnham M, South K, Bleda M, Auger WR, Barbera JA, Bogaard H, et al. The ADAMTS13-VWF axis is dysregulated in chronic thromboembolic pulmonary hypertension. Eur Respir J. 2019;53(3). [DOI] [PMC free article] [PubMed]
- 22.Sompradeekul S, Fedullo P, Le D, editors. Congenital and acquired thrombophilias in patients with chronic thromboembolic pulmonary hypertension. Am J Resp Crit Care; 1999: Amer Lung Assoc 1740 Broadway, New York, NY 10019 USA.
- 23.Bonderman D, Wilkens H, Wakounig S, Schafers HJ, Jansa P, Lindner J, et al. Risk factors for chronic thromboembolic pulmonary hypertension. Eur Respir J. 2009;33(2):325–331. doi: 10.1183/09031936.00087608. [DOI] [PubMed] [Google Scholar]
- 24.Becattini C, Agnelli G, Pesavento R, Silingardi M, Poggio R, Taliani MR, et al. Incidence of chronic thromboembolic pulmonary hypertension after a first episode of pulmonary embolism. Chest. 2006;130(1):172–175. doi: 10.1378/chest.130.1.172. [DOI] [PubMed] [Google Scholar]
- 25.de Perrot M, Fadel E, McRae K, Tan K, Slinger P, Paul N, et al. Evaluation of persistent pulmonary hypertension after acute pulmonary embolism. Chest. 2007;132(3):780–785. doi: 10.1378/chest.06-2493. [DOI] [PubMed] [Google Scholar]
- 26.Lang I, Kerr K. Risk factors for chronic thromboembolic pulmonary hypertension. Proc Am Thorac Soc. 2006;3(7):568–570. doi: 10.1513/pats.200605-108LR. [DOI] [PubMed] [Google Scholar]
- 27.Berghaus TM, Barac M, von Scheidt W, Schwaiblmair M. Echocardiographic evaluation for pulmonary hypertension after recurrent pulmonary embolism. Thromb Res. 2011;128(6):e144–e147. doi: 10.1016/j.thromres.2011.07.045. [DOI] [PubMed] [Google Scholar]
- 28.Delcroix M, Kerr K, Fedullo P. Chronic thromboembolic pulmonary hypertension. epidemiology and risk factors. Ann Am Thorac Soc. 2016;13 Suppl 3(Suppl 3):S201–S206. doi: 10.1513/AnnalsATS.201509-621AS. [DOI] [PubMed] [Google Scholar]
- 29.Jais X, Ioos V, Jardim C, Sitbon O, Parent F, Hamid A, et al. Splenectomy and chronic thromboembolic pulmonary hypertension. Thorax. 2005;60(12):1031–1034. doi: 10.1136/thx.2004.038083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilkens H, Konstantinides S, Lang IM, Bunck AC, Gerges M, Gerhardt F, et al. Chronic thromboembolic pulmonary hypertension (CTEPH): Updated Recommendations from the Cologne Consensus Conference 2018. Int J Cardiol. 2018;272S:69–78. doi: 10.1016/j.ijcard.2018.08.079. [DOI] [PubMed] [Google Scholar]
- 31.Lang IM, Simonneau G, Pepke-Zaba JW, Mayer E, Ambroz D, Blanco I, et al. Factors associated with diagnosis and operability of chronic thromboembolic pulmonary hypertension. A case-control study. Thromb Haemost. 2013;110(1):83–91. doi: 10.1160/TH13-02-0097. [DOI] [PubMed] [Google Scholar]
- 32.Kim NH, Delcroix M, Jenkins DP, Channick R, Dartevelle P, Jansa P, et al. Chronic thromboembolic pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D92–D99. doi: 10.1016/j.jacc.2013.10.024. [DOI] [PubMed] [Google Scholar]
- 33.Swan D, Hitchen S, Klok FA, Thachil J. The problem of under-diagnosis and over-diagnosis of pulmonary embolism. Thromb Res. 2019;177:122–129. doi: 10.1016/j.thromres.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 34.Pepke-Zaba J, Delcroix M, Lang I, Mayer E, Jansa P, Ambroz D, et al. Chronic thromboembolic pulmonary hypertension (CTEPH): results from an international prospective registry. Circulation. 2011;124(18):1973–1981. doi: 10.1161/CIRCULATIONAHA.110.015008. [DOI] [PubMed] [Google Scholar]
- 35.Auger W, Moser K. Pulmonary flow murmurs - A distinctive physical sign found in chronic pulmonary thromboembolic disease. Slack Inc 6900 Grove Rd, Thorofare, NJ 08086: Clinical Research; 1989. [Google Scholar]
- 36.Fedullo PF, Auger WR. Clinical features and evaluation of chronic thromboembolic pulmonary hypertension. Medical Management of the Thoracic Surgery Patient: Saunders/Elsevier. 2010:477–82.
- 37.Madani M, Jamieson SW. Chronic thromboembolic pulmonary hypertension and pulmonary thromboendarterectomy. Medical management of the thoracic surgery patient: Saunders/Elsevier. 2010:483–90.
- 38.Woodruff W, 3rd, Hoeck BE, Chitwood W, Jr, Lyerly H, Sabiston D, Jr, Chen J. Radiographic findings in pulmonary hypertension from unresolved embolism. Am J Roentgenol. 1985;144(4):681–686. doi: 10.2214/ajr.144.4.681. [DOI] [PubMed] [Google Scholar]
- 39.Galie N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT) Eur Heart J. 2016;37(1):67–119. doi: 10.1093/eurheartj/ehv317. [DOI] [PubMed] [Google Scholar]
- 40.Tunariu N, Gibbs SJR, Win Z, Gin-Sing W, Graham A, Gishen P, et al. Ventilation-perfusion scintigraphy is more sensitive than multidetector CTPA in detecting chronic thromboembolic pulmonary disease as a treatable cause of pulmonary hypertension. J Nucl Med. 2007;48(5):680–684. doi: 10.2967/jnumed.106.039438. [DOI] [PubMed] [Google Scholar]
- 41.Moradi F, Morris TA, Hoh CK. Perfusion scintigraphy in diagnosis and management of thromboembolic pulmonary hypertension. Radiographics. 2019;39(1):169–185. doi: 10.1148/rg.2019180074. [DOI] [PubMed] [Google Scholar]
- 42.Ryan KL, Fedullo PF, Davis GB, Vasquez TE, Moser KM. Perfusion scan findings understate the severity of angiographic and hemodynamic compromise in chronic thromboembolic pulmonary hypertension. Chest. 1988;93(6):1180–1185. doi: 10.1378/chest.93.6.1180. [DOI] [PubMed] [Google Scholar]
- 43.Narechania S, Renapurkar R, Heresi GA. Mimickers of chronic thromboembolic pulmonary hypertension on imaging tests: a review. Pulm Circ. 2020;10(1):2045894019882620. doi: 10.1177/2045894019882620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gopalan D, Delcroix M, Held M. Diagnosis of chronic thromboembolic pulmonary hypertension. Eur Respir Rev. 2017;26(143):160108. doi: 10.1183/16000617.0108-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ley S, Ley-Zaporozhan J, Pitton MB, Schneider J, Wirth GM, Mayer E, et al. Diagnostic performance of state-of-the-art imaging techniques for morphological assessment of vascular abnormalities in patients with chronic thromboembolic pulmonary hypertension (CTEPH) Eur Radiol. 2012;22(3):607–616. doi: 10.1007/s00330-011-2290-4. [DOI] [PubMed] [Google Scholar]
- 46.Reichelt A, Hoeper MM, Galanski M, Keberle M. Chronic thromboembolic pulmonary hypertension: evaluation with 64-detector row CT versus digital substraction angiography. Eur J Radiol. 2009;71(1):49–54. doi: 10.1016/j.ejrad.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 47.Sugimura K, Fukumoto Y, Satoh K, Nochioka K, Miura Y, Aoki T, et al. Percutaneous transluminal pulmonary angioplasty markedly improves pulmonary hemodynamics and long-term prognosis in patients with chronic thromboembolic pulmonary hypertension. Circ J. 2012;76(2):485–488. doi: 10.1253/circj.CJ-11-1217. [DOI] [PubMed] [Google Scholar]
- 48.Hasegawa I, Boiselle PM, Hatabu H. Bronchial artery dilatation on MDCT scans of patients with acute pulmonary embolism: comparison with chronic or recurrent pulmonary embolism. AJR Am J Roentgenol. 2004;182(1):67–72. doi: 10.2214/ajr.182.1.1820067. [DOI] [PubMed] [Google Scholar]
- 49.King MA, Ysrael M, Bergin CJ. Chronic thromboembolic pulmonary hypertension: CT findings. AJR Am J Roentgenol. 1998;170(4):955–960. doi: 10.2214/ajr.170.4.9530043. [DOI] [PubMed] [Google Scholar]
- 50.Giannouli E, Maycher B. Imaging techniques in chronic thromboembolic pulmonary hypertension. Curr Opin Pulm Med. 2013;19(5):562–574. doi: 10.1097/MCP.0b013e3283645a00. [DOI] [PubMed] [Google Scholar]
- 51.Pena E, Dennie C. Acute and chronic pulmonary embolism: an in-depth review for radiologists through the use of frequently asked questions. Seminars in Ultrasound, CT and MRI. Elsevier; 2012. [DOI] [PubMed] [Google Scholar]
- 52.Pitton MB, Duber C, Mayer E, Thelen M. Hemodynamic effects of nonionic contrast bolus injection and oxygen inhalation during pulmonary angiography in patients with chronic major-vessel thromboembolic pulmonary hypertension. Circulation. 1996;94(10):2485–2491. doi: 10.1161/01.CIR.94.10.2485. [DOI] [PubMed] [Google Scholar]
- 53.Auger WR, Fedullo PF, Moser KM, Buchbinder M, Peterson KL. Chronic major-vessel thromboembolic pulmonary artery obstruction: appearance at angiography. Radiology. 1992;182(2):393–398. doi: 10.1148/radiology.182.2.1732955. [DOI] [PubMed] [Google Scholar]
- 54.Ghio S, Raineri C, Scelsi L, Recusani F, D'Armini AM, Piovella F, et al. Usefulness and limits of transthoracic echocardiography in the evaluation of patients with primary and chronic thromboembolic pulmonary hypertension. J Am Soc Echocardiogr. 2002;15(11):1374–1380. doi: 10.1067/mje.2002.124938. [DOI] [PubMed] [Google Scholar]
- 55.Jenkins D, Mayer E, Screaton N, Madani M. State-of-the-art chronic thromboembolic pulmonary hypertension diagnosis and management. Eur Respir Rev. 2012;21(123):32–39. doi: 10.1183/09059180.00009211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Coulden R. State-of-the-art imaging techniques in chronic thromboembolic pulmonary hypertension. Proc Am Thorac Soc. 2006;3(7):577–583. doi: 10.1513/pats.200605-119LR. [DOI] [PubMed] [Google Scholar]
- 57.Simonneau G, Montani D, Celermajer DS, Denton CP, Gatzoulis MA, Krowka M, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J. 2019;53(1). [DOI] [PMC free article] [PubMed]
- 58.Kovacs G, Berghold A, Scheidl S, Olschewski H. Pulmonary arterial pressure during rest and exercise in healthy subjects: a systematic review. Eur Respir J. 2009;34(4):888–894. doi: 10.1183/09031936.00145608. [DOI] [PubMed] [Google Scholar]
- 59.Guth S, Wiedenroth CB, Rieth A, Richter MJ, Gruenig E, Ghofrani HA, et al. Exercise right heart catheterisation before and after pulmonary endarterectomy in patients with chronic thromboembolic disease. Eur Respir J. 2018;52(3). [DOI] [PubMed]
- 60.Held M, Grun M, Holl R, Hubner G, Kaiser R, Karl S, et al. Cardiopulmonary exercise testing to detect chronic thromboembolic pulmonary hypertension in patients with normal echocardiography. Respiration. 2014;87(5):379–387. doi: 10.1159/000358565. [DOI] [PubMed] [Google Scholar]
- 61.Pandey AK, Lee NS, Marsal J, Knowlton KU, McDivit AM, Blanchard DG, et al. Evaluation of routine coronary angiography before pulmonary thromboendarterectomy. Ann Thorac Surg. 2021;111(5):1703–1709. doi: 10.1016/j.athoracsur.2020.06.107. [DOI] [PubMed] [Google Scholar]
- 62.van Kan C, van der Plas MN, Reesink HJ, van Steenwijk RP, Kloek JJ, Tepaske R, et al. Hemodynamic and ventilatory responses during exercise in chronic thromboembolic disease. J Thorac Cardiovasc Surg. 2016;152(3):763–771. doi: 10.1016/j.jtcvs.2016.05.058. [DOI] [PubMed] [Google Scholar]
- 63.Held M, Kolb P, Grun M, Jany B, Hubner G, Grgic A, et al. Functional characterization of patients with chronic thromboembolic disease. Respiration. 2016;91(6):503–509. doi: 10.1159/000447247. [DOI] [PubMed] [Google Scholar]
- 64.Taboada D, Pepke-Zaba J, Jenkins DP, Berman M, Treacy CM, Cannon JE, et al. Outcome of pulmonary endarterectomy in symptomatic chronic thromboembolic disease. Eur Respir J. 2014;44(6):1635–1645. doi: 10.1183/09031936.00050114. [DOI] [PubMed] [Google Scholar]
- 65.Yin K, Zhang Z, Luo R, Ji Y, Zheng D, Lin Y, et al. Clinical features and surgical outcomes of pulmonary artery sarcoma. J Thorac Cardiovasc Surg. 2018;155(3):1109–1115. doi: 10.1016/j.jtcvs.2017.10.101. [DOI] [PubMed] [Google Scholar]
- 66.Wyler von Ballmoos MC, Chan EY, Reardon MJ. Imaging and surgical treatment of primary pulmonary artery sarcoma. Int J Cardiovasc Imaging. 2019;35(8):1429–1433. doi: 10.1007/s10554-018-1489-8. [DOI] [PubMed] [Google Scholar]
- 67.Tandon R, Baughman RP, Stanley J, Khan AA. The link between chronic thromboembolic pulmonary hypertension and sarcoidosis: association or visual masquerade? Sarcoidosis Vasc Diffuse Lung Dis. 2017;34(4):352–355. doi: 10.36141/svdld.v34i4.5852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Limsukon A, Fuller C, Lewis MI. Mediastinitis, fibrosing mediastinitis, and mediastinal hemorrhage. Medical Management of the Thoracic Surgery Patient: Saunders/Elsevier. 2010:405–14.
- 69.McNeeley MF, Chung JH, Bhalla S, Godwin JD. Imaging of granulomatous fibrosing mediastinitis. AJR Am J Roentgenol. 2012;199(2):319–327. doi: 10.2214/AJR.11.7319. [DOI] [PubMed] [Google Scholar]
- 70.Dion J, Terrier B, Jais X, Mehdaoui A, Sattler C, Amar D, et al. Atypical vasculitis mimicking chronic thromboembolic pulmonary hypertension. Am J Med. 2015;128(10):e47–e49. doi: 10.1016/j.amjmed.2015.05.028. [DOI] [PubMed] [Google Scholar]
- 71.Zhu FP, Luo S, Wang ZJ, Jin ZY, Zhang LJ, Lu GM. Takayasu arteritis: imaging spectrum at multidetector CT angiography. Br J Radiol. 2012;85(1020):E1282–E1E92. doi: 10.1259/bjr/25536451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Galie N, Kim NH. Pulmonary microvascular disease in chronic thromboembolic pulmonary hypertension. Proc Am Thorac Soc. 2006;3(7):571–576. doi: 10.1513/pats.200605-113LR. [DOI] [PubMed] [Google Scholar]
- 73.Riedel M, Stanek V, Widimsky J, Prerovsky I. Longterm follow-up of patients with pulmonary thromboembolism. Late prognosis and evolution of hemodynamic and respiratory data. Chest. 1982;81(2):151–158. doi: 10.1378/chest.81.2.151. [DOI] [PubMed] [Google Scholar]
- 74.Jenkins D, Madani M, Fadel E, D'Armini AM, Mayer E. Pulmonary endarterectomy in the management of chronic thromboembolic pulmonary hypertension. Eur Respir Rev. 2017;26(143):160111. doi: 10.1183/16000617.0111-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hoeper MM, Mayer E, Simonneau G, Rubin LJ. Chronic thromboembolic pulmonary hypertension. Circulation. 2006;113(16):2011–2020. doi: 10.1161/CIRCULATIONAHA.105.602565. [DOI] [PubMed] [Google Scholar]
- 76.Bunclark K, Newnham M, Chiu YD, Ruggiero A, Villar SS, Cannon JE, et al. A multicenter study of anticoagulation in operable chronic thromboembolic pulmonary hypertension. J Thromb Haemost. 2020;18(1):114–122. doi: 10.1111/jth.14649. [DOI] [PubMed] [Google Scholar]
- 77.Delcroix M, Lang I, Pepke-Zaba J, Jansa P, D'Armini AM, Snijder R, et al. Long-term outcome of patients with chronic thromboembolic pulmonary hypertension: results from an international prospective registry. Circulation. 2016;133(9):859–871. doi: 10.1161/CIRCULATIONAHA.115.016522. [DOI] [PubMed] [Google Scholar]
- 78.Mahmud E, Madani MM, Kim NH, Poch D, Ang L, Behnamfar O, et al. Chronic thromboembolic pulmonary hypertension: evolving therapeutic approaches for operable and inoperable disease. J Am Coll Cardiol. 2018;71(21):2468–2486. doi: 10.1016/j.jacc.2018.04.009. [DOI] [PubMed] [Google Scholar]
- 79.Madani M, Mayer E, Fadel E, Jenkins DP. Pulmonary endarterectomy. patient selection, technical challenges, and outcomes. Ann Am Thorac Soc. 2016;13 Suppl 3:S240–S247. doi: 10.1513/AnnalsATS.201601-014AS. [DOI] [PubMed] [Google Scholar]
- 80.Archibald CJ, Auger WR, Fedullo PF, Channick RN, Kerr KM, Jamieson SW, et al. Long-term outcome after pulmonary thromboendarterectomy. Am J Resp Crit Care. 1999;160(2):523–528. doi: 10.1164/ajrccm.160.2.9808109. [DOI] [PubMed] [Google Scholar]
- 81.Thistlethwaite PA, Kaneko K, Madani MM, Jamieson SW. Technique and outcomes of pulmonary endarterectomy surgery. Ann Thorac Cardiovasc Surg. 2008;14(5):274–282. [PubMed] [Google Scholar]
- 82.D'Armini AM, Morsolini M, Mattiucci G, Grazioli V, Pin M, Valentini A, et al. Pulmonary endarterectomy for distal chronic thromboembolic pulmonary hypertension. J Thorac Cardiovasc Surg. 2014;148(3):1005-11–12 e1-2. doi: 10.1016/j.jtcvs.2014.06.052. [DOI] [PubMed] [Google Scholar]
- 83.Farasat S, Papamatheakis DG, Poch DS, Higgins J, Pretorius VG, Madani MM, et al. Atrial arrhythmias after pulmonary thromboendarterectomy. J Card Surg. 2019;34(5):312–317. doi: 10.1111/jocs.14028. [DOI] [PubMed] [Google Scholar]
- 84.Havranek S, Fingrova Z, Ambroz D, Jansa P, Kuchar J, Dusik M, et al. Atrial fibrillation and atrial tachycardia in patients with chronic thromboembolic pulmonary hypertension treated with pulmonary endarterectomy. Eur Heart J Suppl. 2020;22(Suppl F):F30–FF7. doi: 10.1093/eurheartj/suaa096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Jenkins DP, Madani M, Mayer E, Kerr K, Kim N, Klepetko W, et al. Surgical treatment of chronic thromboembolic pulmonary hypertension. Eur Respir J. 2013;41(3):735–742. doi: 10.1183/09031936.00058112. [DOI] [PubMed] [Google Scholar]
- 86.Moser KM, Metersky ML, Auger WR, Fedullo PF. Resolution of vascular steal after pulmonary thromboendarterectomy. Chest. 1993;104(5):1441–1444. doi: 10.1378/chest.104.5.1441. [DOI] [PubMed] [Google Scholar]
- 87.Lee KC, Cho YL, Lee SY. Reperfusion pulmonary edema after pulmonary endarterectomy. Acta Anaesthesiol Sin. 2001;39(2):97–101. [PubMed] [Google Scholar]
- 88.Thistlethwaite PA, Madani MM, Kemp AD, Hartley M, Auger WR, Jamieson SW. Venovenous extracorporeal life support after pulmonary endarterectomy: indications, techniques, and outcomes. Ann Thorac Surg. 2006;82(6):2139–2145. doi: 10.1016/j.athoracsur.2006.07.020. [DOI] [PubMed] [Google Scholar]
- 89.Berman M, Tsui S, Vuylsteke A, Snell A, Colah S, Latimer R, et al. Successful extracorporeal membrane oxygenation support after pulmonary thromboendarterectomy. Ann Thorac Surg. 2008;86(4):1261–1267. doi: 10.1016/j.athoracsur.2008.06.037. [DOI] [PubMed] [Google Scholar]
- 90.Mayer E, Jenkins D, Lindner J, D'Armini A, Kloek J, Meyns B, et al. Surgical management and outcome of patients with chronic thromboembolic pulmonary hypertension: results from an international prospective registry. J Thorac Cardiovasc Surg. 2011;141(3):702–710. doi: 10.1016/j.jtcvs.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 91.Kramm T, Eberle B, Guth S, Mayer E. Inhaled iloprost to control residual pulmonary hypertension following pulmonary endarterectomy. Eur J Cardiothorac Surg. 2005;28(6):882–888. doi: 10.1016/j.ejcts.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 92.Riedel B. The pathophysiology and management of perioperative pulmonary hypertension with specific emphasis on the period following cardiac surgery. Int Anesthesiol Clin. 1999;37(2):55–79. doi: 10.1097/00004311-199903720-00005. [DOI] [PubMed] [Google Scholar]
- 93.Condliffe R, Kiely DG, Gibbs JS, Corris PA, Peacock AJ, Jenkins DP, et al. Improved outcomes in medically and surgically treated chronic thromboembolic pulmonary hypertension. Am J Respir Crit Care Med. 2008;177(10):1122–1127. doi: 10.1164/rccm.200712-1841OC. [DOI] [PubMed] [Google Scholar]
- 94.Cannon JE, Su L, Kiely DG, Page K, Toshner M, Swietlik E, et al. Dynamic risk stratification of patient long-term outcome after pulmonary endarterectomy: results from the United Kingdom National Cohort. Circulation. 2016;133(18):1761–1771. doi: 10.1161/CIRCULATIONAHA.115.019470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.D'Armini AM, Zanotti G, Ghio S, Magrini G, Pozzi M, Scelsi L, et al. Reverse right ventricular remodeling after pulmonary endarterectomy. J Thorac Cardiovasc Surg. 2007;133(1):162–168. doi: 10.1016/j.jtcvs.2006.08.059. [DOI] [PubMed] [Google Scholar]
- 96.Quadery SR, Swift AJ, Billings CG, Thompson AAR, Elliot CA, Hurdman J, et al. The impact of patient choice on survival in chronic thromboembolic pulmonary hypertension. Eur Respir J. 2018;52(3):52:1800589. doi: 10.1183/13993003.00589-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lang IM, Dorfmuller P, Vonk NA. The pathobiology of chronic thromboembolic pulmonary hypertension. Ann Am Thorac Soc. 2016;13(Suppl 3):S215–S221. doi: 10.1513/AnnalsATS.201509-620AS. [DOI] [PubMed] [Google Scholar]
- 98.Feinstein JA, Goldhaber SZ, Lock JE, Ferndandes SM, Landzberg MJ. Balloon pulmonary angioplasty for treatment of chronic thromboembolic pulmonary hypertension. Circulation. 2001;103(1):10–13. doi: 10.1161/01.CIR.103.1.10. [DOI] [PubMed] [Google Scholar]
- 99.Mizoguchi H, Ogawa A, Munemasa M, Mikouchi H, Ito H, Matsubara H. Refined balloon pulmonary angioplasty for inoperable patients with chronic thromboembolic pulmonary hypertension. Circ Cardiovasc Interv. 2012;5(6):748–755. doi: 10.1161/CIRCINTERVENTIONS.112.971077. [DOI] [PubMed] [Google Scholar]
- 100.Kataoka M, Inami T, Hayashida K, Shimura N, Ishiguro H, Abe T, et al. Percutaneous transluminal pulmonary angioplasty for the treatment of chronic thromboembolic pulmonary hypertension. Circ Cardiovasc Interv. 2012;5(6):756–762. doi: 10.1161/CIRCINTERVENTIONS.112.971390. [DOI] [PubMed] [Google Scholar]
- 101.Ogo T. Balloon pulmonary angioplasty for inoperable chronic thromboembolic pulmonary hypertension. Curr Opin Pulm Med. 2015;21(5):425–431. doi: 10.1097/MCP.0000000000000188. [DOI] [PubMed] [Google Scholar]
- 102.Nagayoshi S, Fujii S, Nakajima T, Muto M. Intravenous ultrasound-guided balloon pulmonary angioplasty in the treatment of totally occluded chronic thromboembolic pulmonary hypertension. EuroIntervention. 2018;14(2):234–235. doi: 10.4244/EIJ-D-17-00770. [DOI] [PubMed] [Google Scholar]
- 103.Tatebe S, Fukumoto Y, Sugimura K, Miura Y, Nochioka K, Aoki T, et al. Optical coherence tomography is superior to intravascular ultrasound for diagnosis of distal-type chronic thromboembolic pulmonary hypertension. Circulation Journal. 2013;77(4):1081–1083. doi: 10.1253/circj.CJ-12-1493. [DOI] [PubMed] [Google Scholar]
- 104.Ikeda N. Balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension. Cardiovasc Interv Ther. 2020;35(2):130–141. doi: 10.1007/s12928-019-00637-2. [DOI] [PubMed] [Google Scholar]
- 105.Kawakami T, Ogawa A, Miyaji K, Mizoguchi H, Shimokawahara H, Naito T, et al. Novel angiographic classification of each vascular lesion in chronic thromboembolic pulmonary hypertension based on selective angiogram and results of balloon pulmonary angioplasty. Circ Cardiovasc Interv. 2016;9(10):e003318. doi: 10.1161/CIRCINTERVENTIONS.115.003318. [DOI] [PubMed] [Google Scholar]
- 106.Hoole SP, Coghlan JG, Cannon JE, Taboada D, Toshner M, Sheares K, et al. Balloon pulmonary angioplasty for inoperable chronic thromboembolic pulmonary hypertension: the UK experience. Open Heart. 2020;7(1):e001144. doi: 10.1136/openhrt-2019-001144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Brenot P, Jais X, Taniguchi Y, Garcia Alonso C, Humbert M, Fadel E, et al. Balloon pulmonary angioplasty for inoperable chronic thromboembolic pulmonary hypertension: the initial experience at Paris-Sud University. D26 with friends like these: inside the spectrum of PE and CTEPH. Am Thorac Soc. 2018:A7788-A.
- 108.Jin Q, Zhao ZH, Luo Q, Zhao Q, Yan L, Zhang Y, et al. Balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension: State of the art. World J Clin Cases. 2020;8(13):2679–2702. doi: 10.12998/wjcc.v8.i13.2679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ejiri K, Ogawa A, Fujii S, Ito H, Matsubara H. Vascular injury is a major cause of lung injury after balloon pulmonary angioplasty in patients with chronic thromboembolic pulmonary hypertension. Circ Cardiovasc Interv. 2018;11(12):e005884. doi: 10.1161/CIRCINTERVENTIONS.117.005884. [DOI] [PubMed] [Google Scholar]
- 110.Ogawa A, Satoh T, Fukuda T, Sugimura K, Fukumoto Y, Emoto N, et al. Balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension: results of a multicenter registry. Circ Cardiovasc Qual Outcomes. 2017;10(11):e004029. doi: 10.1161/CIRCOUTCOMES.117.004029. [DOI] [PubMed] [Google Scholar]
- 111.Brenot P, Jais X, Taniguchi Y, Garcia Alonso C, Gerardin B, Mussot S, et al. French experience of balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension. Eur Respir J. 2019;53(5):1802095. doi: 10.1183/13993003.02095-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zoppellaro G, Badawy MR, Squizzato A, Denas G, Tarantini G, Pengo V. Balloon pulmonary angioplasty in patients with chronic thromboembolic pulmonary hypertension- a systematic review and meta-analysis. Circ J. 2019;83(8):1660–1667. doi: 10.1253/circj.CJ-19-0161. [DOI] [PubMed] [Google Scholar]
- 113.Tanabe N, Kawakami T, Satoh T, Matsubara H, Nakanishi N, Ogino H, et al. Balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension: A systematic review. Respir Investig. 2018;56(4):332–341. doi: 10.1016/j.resinv.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 114.Andreassen AK, Ragnarsson A, Gude E, Geiran O, Andersen R. Balloon pulmonary angioplasty in patients with inoperable chronic thromboembolic pulmonary hypertension. Heart. 2013;99(19):1415–1420. doi: 10.1136/heartjnl-2012-303549. [DOI] [PubMed] [Google Scholar]
- 115.Darocha S, Banaszkiewicz M, Pietrasik A, Siennicka A, Piorunek M, Grochowska E, et al. Changes in estimated glomerular filtration after balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension. Cardiorenal Med. 2020;10(1):22–31. doi: 10.1159/000502254. [DOI] [PubMed] [Google Scholar]
- 116.Kriechbaum SD, Wiedenroth CB, Wolter JS, Hutz R, Haas M, Breithecker A, et al. N-terminal pro-B-type natriuretic peptide for monitoring after balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension. J Heart Lung Transplant. 2018;37(5):639–646. doi: 10.1016/j.healun.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 117.Castro MA, Piloto B, Fernandes CJCD, Jardim C, Salibe W, Oleas FG, et al. Use of medical therapies before pulmonary endarterectomy in chronic thromboembolic pulmonary hypertension patients with severe hemodynamic impairment. Plos One. 2020;15(5):e0233063. doi: 10.1371/journal.pone.0233063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ghofrani HA, D'Armini AM, Grimminger F, Hoeper MM, Jansa P, Kim NH, et al. Riociguat for the treatment of chronic thromboembolic pulmonary hypertension. N Engl J Med. 2013;369(4):319–329. doi: 10.1056/NEJMoa1209657. [DOI] [PubMed] [Google Scholar]
- 119.Simonneau G, D'Armini AM, Ghofrani HA, Grimminger F, Hoeper MM, Jansa P, et al. Riociguat for the treatment of chronic thromboembolic pulmonary hypertension: a long-term extension study (CHEST-2) Eur Respir J. 2015;45(5):1293–1302. doi: 10.1183/09031936.00087114. [DOI] [PubMed] [Google Scholar]
- 120.Marra AM, Halank M, Benjamin N, Bossone E, Cittadini A, Eichstaedt CA, et al. Right ventricular size and function under riociguat in pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension (the RIVER study) Respir Res. 2018;19(1):258. doi: 10.1186/s12931-018-0957-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jais X, D'Armini AM, Jansa P, Torbicki A, Delcroix M, Ghofrani HA, et al. Bosentan for treatment of inoperable chronic thromboembolic pulmonary hypertension: BENEFiT (Bosentan Effects in iNopErable Forms of chronIc Thromboembolic pulmonary hypertension), a randomized, placebo-controlled trial. J Am Coll Cardiol. 2008;52(25):2127–2134. doi: 10.1016/j.jacc.2008.08.059. [DOI] [PubMed] [Google Scholar]
- 122.Becattini C, Manina G, Busti C, Gennarini S, Agnelli G. Bosentan for chronic thromboembolic pulmonary hypertension: findings from a systematic review and meta-analysis. Thromb Res. 2010;126(1):e51–e56. doi: 10.1016/j.thromres.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 123.Ghofrani HA, Simonneau G, D'Armini AM, Fedullo P, Howard LS, Jais X, et al. Macitentan for the treatment of inoperable chronic thromboembolic pulmonary hypertension (MERIT-1): results from the multicentre, phase 2, randomised, double-blind, placebo-controlled study. Lancet Respir Med. 2017;5(10):785–794. doi: 10.1016/S2213-2600(17)30305-3. [DOI] [PubMed] [Google Scholar]
- 124.Escribano-Subias P, Bendjenana H, Curtis PS, Lang I, Vonk NA. Ambrisentan for treatment of inoperable chronic thromboembolic pulmonary hypertension (CTEPH) Pulm Circ. 2019;9(2):2045894019846433. doi: 10.1177/2045894019846433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Suntharalingam J, Treacy CM, Doughty NJ, Goldsmith K, Soon E, Toshner MR, et al. Long-term use of sildenafil in inoperable chronic thromboembolic pulmonary hypertension. Chest. 2008;134(2):229–236. doi: 10.1378/chest.07-2681. [DOI] [PubMed] [Google Scholar]
- 126.Sadushi-Kolici R, Jansa P, Kopec G, Torbicki A, Skoro-Sajer N, Campean IA, et al. Subcutaneous treprostinil for the treatment of severe non-operable chronic thromboembolic pulmonary hypertension (CTREPH): a double-blind, phase 3, randomised controlled trial. Lancet Respir Med. 2019;7(3):239–248. doi: 10.1016/S2213-2600(18)30367-9. [DOI] [PubMed] [Google Scholar]
- 127.Cabrol S, Souza R, Jais X, Fadel E, Ali RH, Humbert M, et al. Intravenous epoprostenol in inoperable chronic thromboembolic pulmonary hypertension. J Heart Lung Transplant. 2007;26(4):357–362. doi: 10.1016/j.healun.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 128.Skoro-Sajer N, Bonderman D, Wiesbauer F, Harja E, Jakowitsch J, Klepetko W, et al. Treprostinil for severe inoperable chronic thromboembolic pulmonary hypertension. J Thromb Haemost. 2007;5(3):483–489. doi: 10.1111/j.1538-7836.2007.02394.x. [DOI] [PubMed] [Google Scholar]
- 129.Olschewski H, Simonneau G, Galie N, Higenbottam T, Naeije R, Rubin LJ, et al. Inhaled iloprost for severe pulmonary hypertension. N Engl J Med. 2002;347(5):322–329. doi: 10.1056/NEJMoa020204. [DOI] [PubMed] [Google Scholar]
- 130.Gabrielly M, Bourlier D, Taniguchi Y, Jevnikar M, Sekine A, Boucly A, et al. Initial dual oral combination therapy in inoperable chronic thromboembolic pulmonary hypertension (CTEPH) 2018. [Google Scholar]
- 131.Kalra R, Duval S, Thenappan T, Raveendran G, Pritzker M, Prisco SZ, et al. Comparison of balloon pulmonary angioplasty and pulmonary vasodilators for inoperable chronic thromboembolic pulmonary hypertension: a systematic review and meta-analysis. Sci Rep. 2020;10(1):8870. doi: 10.1038/s41598-020-65697-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Phan K, Jo HE, Xu J, Lau EM. Medical therapy versus balloon angioplasty for CTEPH: a systematic review and meta-analysis. Heart Lung Circ. 2018;27(1):89–98. doi: 10.1016/j.hlc.2017.01.016. [DOI] [PubMed] [Google Scholar]
- 133.Wiedenroth CB, Ghofrani HA, Adameit MSD, Breithecker A, Haas M, Kriechbaum S, et al. Sequential treatment with riociguat and balloon pulmonary angioplasty for patients with inoperable chronic thromboembolic pulmonary hypertension. Pulm Circ. 2018;8(3):2045894018783996. doi: 10.1177/2045894018783996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Aoki T, Sugimura K, Terui Y, Tatebe S, Fukui S, Miura M, et al. Beneficial effects of riociguat on hemodynamic responses to exercise in CTEPH patients after balloon pulmonary angioplasty - A randomized controlled study. Int J Cardiol Heart Vasc. 2020;29:100579. doi: 10.1016/j.ijcha.2020.100579. [DOI] [PMC free article] [PubMed] [Google Scholar]