Abstract
Background
In the United States (US), the incidence and severity of COVID-19 infections, hospitalizations, and deaths are higher in Black compared to White residents. Systemic inequities and differences in health behaviors may contribute to disparities in COVID-19 health outcomes. The aim of this study was to examine the impact of COVID-19 stay-at-home orders on changes in health behaviors and anxiety in Black and White adults residing in the US.
Methods
Beginning April 2020, the Pennington Biomedical Research Center COVID-19 Health Behaviors Study collected information on changes to employment, income, diet, physical activity, anxiety, and sleep patterns through a global online survey.
Results
Of 4542 survey respondents in the US, 7% identified as Black and 93% as White. Prior to the COVID-19 stay-at-home orders, a greater proportion of Blacks compared to Whites reported earning < US$50,000 per year (p < 0.0001). A greater proportion of Blacks reported being laid off, working fewer hours, and working from home following COVID-19 stay-at-home orders (p < 0.0001 for all). In the overall sample, eating behaviors improved, physical activity decreased, sleep time prolonged, and anxiety heightened following COVID-19 stay-at-home orders (p < 0.01 for all), which were universal between Black and White respondents (p ≥ 0.315 for all).
Conclusions
This study highlights the disproportionate changes to employment and income in Blacks, with no differential impact on health behaviors and anxiety compared to Whites due to COVID-19 stay-at-home orders. As the COVID-19 pandemic continues, disproportionate changes to employment and income status may widen among Blacks and Whites, which may influence health behaviors and anxiety.
Keywords: Anxiety, COVID-19, Employment, Health behaviors, Health disparities, Income
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by the severe acute respiratory syndrome coronavirus 2. In the United States (US), the incidence and severity of COVID-19 infections, hospitalizations, and deaths are higher in Black residents compared to White residents [1, 2]. Compared to Whites, Blacks have been almost three times, five times, and two times more likely, respectively, to contract, be hospitalized, or die from COVID-19 [1, 2].
Recent viewpoints and commentaries lack empirical data but have speculated that systemic inequities and differences in health behaviors may contribute to disparities in COVID-19 health outcomes [3–7]. Viewpoints have also highlighted the disproportionate economic and environmental impacts likely to occur among Blacks in the US due to COVID-19 [3–7]. For example, current evidence suggests that food insecurity has become exacerbated due to the COVID-19 pandemic in a low-income, predominantly African American cohort [8]. Food insecurity in this vulnerable population may be coupled with low-cost, energy-dense processed foods as well as a built environment characterized by living in more polluted and crime-prone neighborhoods, a lack of access to sidewalks, and limited transportation.
Further economic and environmental impacts, including not having the option to continue to work or the privilege to work from home, and access to COVID-19 vaccinations are likely to further affect COVID-19 infection rates, impede recovery from COVID-19, and challenge maintenance of health behaviors during the pandemic [6, 7, 9]. In order to identify health disparities in health behaviors and anxiety between Blacks and Whites, we tested the hypothesis that these metrics would be more negatively and disproportionately impacted by COVID-19 stay-at-home orders among Blacks compared to Whites in a cohort of 4542 US adults.
Methods
The Pennington Biomedical Research Center COVID-19 Health Behaviors Study assessed behavior change in response to COVID-19 stay-at-home orders [10]. From April 3, 2020 to May 3, 2020, this global survey collected anonymous information on individual and household demographics and changes to employment, income, diet (breakfast skipping and consumption of sugar-sweetened beverages, takeout, fast food, fried foods, desserts, fruits, and vegetables), physical activity (minutes/week adjusted for exercise intensity), anxiety, and sleep patterns. To assess health behaviors and anxiety prior to stay-at-home orders, participants were asked to recall using the phrase “before the COVID-19 outbreak in your country or region.” Health behaviors and anxiety during stay-at-home orders were assessed by asking the participants to recall using the phrase “since the COVID-19 outbreak in your country or region.” Diet was assessed using the Rapid Eating Assessment for Participants short version (REAP-s) [11]. Total intensity-adjusted physical activity, presented as metabolic equivalent (MET) minutes per week, was measured using a modified version of the Nurses’ Health Study Physical Activity Questionnaire [12] with METs for physical activity chosen from the Compendium of Physical Activities [13]. Sleep was determined by self-report sleep onset and wake times. Anxiety was evaluated using the generalized anxiety disorder 7-item (GAD-7) scale [14]. These measures were selected to provide a comprehensive representation of typically described lifestyle and mental health domains in participants before and after the pandemic. The specific survey domains are registered and available to the public at PhenX Toolkit (https://www.phenxtoolkit.org/covid19/) [15]. Herein, we report results of respondents residing in the US given that stay-at-home orders were not globally universal. Of note, while stay-at-home orders were variable within the US, 41 out of 50 states had implemented state-at-home mandates at the time of study start [16]. Recruitment occurred over 30 days via social media and word of mouth. Ethics approval and electronic consent were obtained [10].
Statistical analyses were performed using SAS version 9.4 (Cary, NC), and p < 0.05 determined significance. Demographics were compared using unpaired t-tests (continuous variables) and chi-square analyses (categorical variables). General linear models compared change scores from pre- to post-stay-at-home orders between Blacks and Whites including pre-COVID-19 value (crude model) and age, body mass index (BMI), highest degree earned, household income, and household size as covariates (adjusted model). Sensitivity analysis using 1:1 random sampling (1000 iterations) of Blacks and Whites for health behaviors and anxiety was also performed. Post hoc power analysis (β = 0.8, α = 0.025 one-sided) estimated that with a sample of 319 Blacks, the minimal difference for change in eating behaviors is 3.8% when compared to Whites.
Results
Of the US respondents, a total of 125 (2.8%) reported being tested for COVID-19 with 16 (0.4%) reporting testing positive for COVID-19. Blacks accounted for 16.8% (n = 21) of those who tested for COVID-19, of whom 12.5% (n = 2) tested positive for COVID-19. As the timeline for completion of the COVID-19 Health Behaviors Study, COVID-19 testing, and potential positive COVID-19 test were not accounted for, the few respondents who also reported testing positive for COVID-19 were included in the present analyses.
Of 4542 respondents in the US, 319 (7%) identified as Black and 4223 (93%) as White. Compared to Whites, Blacks were younger (49.5 ± 14.6 versus 52.1 ± 15.6 years), had a higher BMI (31.9 ± 7.5 versus 28.7 ± 6.8 kg/m2), completed fewer years of education (30.4% versus 37.4% completing bachelor’s degree), lived in a household with more dependents (1.0 ± 1.1 versus 0.8 ± 1.1 dependents), and lower household income (40.2% versus 25.2% earning < US$50,000 per year) (p ≤ 0.03 for all).
Following stay-at-home orders, most respondents in the overall sample reported being laid off (60.6%), working fewer hours (51.5%), and working from home (35.5%), with no significant correlations expressed between household income and any change in employment status (0.09 ≤ r ≤ 0.10; p ≥ 0.22 for all). Analysis in the overall sample also provided evidence that eating behaviors improved (+ 4.9%, p < 0.01) due to less breakfast skipping and consumption of takeout, fast food, and fried foods and greater fruit consumption, while sleep time prolonged (+ 3.2%) (p < 0.01 for both). Additionally, physical activity decreased (− 4.4%) and anxiety heightened (+ 95.8%) (p < 0.01 for both).
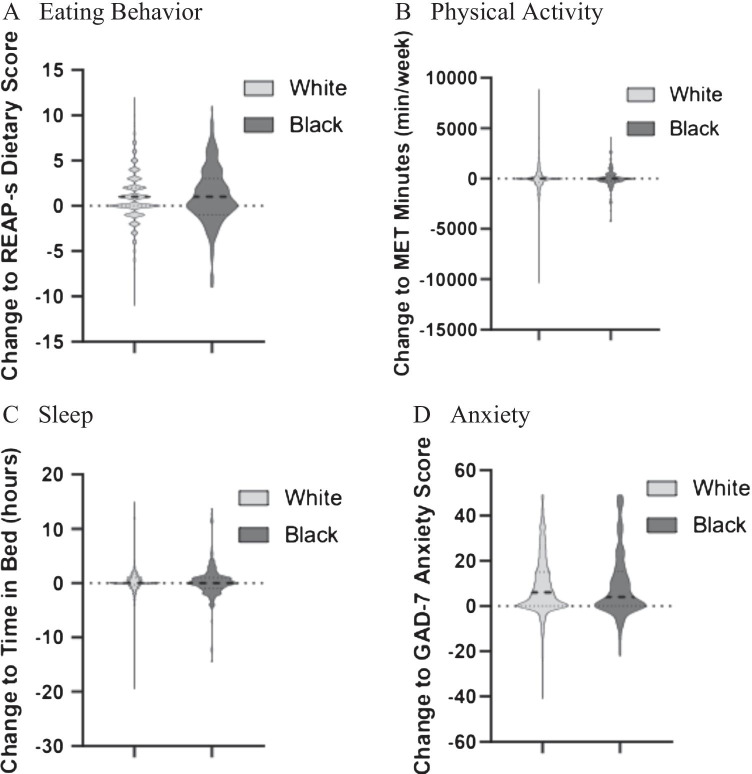
In our crude models, changes (Δ) to eating behaviors (Blacks ΔREAP-S = 1.07 ± 3.16; Whites ΔREAP-S = 0.88 ± 2.7; p = 0.388), physical activity (Blacks ΔMET-minutes per week = − 152.9 ± 2,062.1; Whites ΔREAP-S = − 55.8 ± 1210.2; p = 0.315), sleep time (Blacks Δhours per day = 0.29 ± 3.02; Whites Δhours per day = 0.26 ± 2.31; p = 0.853), and anxiety (Blacks ΔGAD-7 = 9.0 ± 14.4; Whites ΔGAD-7 = 8.6 ± 13.0; p = 0.388) were similar between Blacks and Whites (Fig. 1), which persisted in adjusted models (p ≥ 0.106 for adjusted models). As sample size differences existed between Blacks and Whites, we performed a sensitivity analysis utilizing a random sampling approach of Blacks and Whites, which yielded similar findings for changes in health behaviors and anxiety.
Fig. 1.
A–D Change in health behaviors and anxiety in response to COVID-19 stay-at-home orders in Black and White respondents. Reports mean change and variance (crude model) in total number of White and Black respondents for change in A eating behavior measured with the Rapid Eating Assessment for Participants (REAPs) survey, B intensity-adjusted physical activity in metabolic (MET) minutes, C sleep time assessed by self-reported time into and out of bed, and D anxiety measured with the General Anxiety Disorder 7-Item (GAD-7) scale
Discussion
In April 2020, COVID-19 stay-at-home orders mandated for approximately 60 days in most regions led to drastic universal changes in health behaviors and anxiety among Blacks and Whites. These results, while contrary to our hypothesis and prior viewpoints and commentaries [3–7], are plausible because stay-at-home orders were abrupt, and the entire population was forced to adapt simultaneously. Blacks, however, reported a disproportionate reduction in household income and employment loss during the initial COVID-19 stay-at-home orders. These findings were interesting as the presented health behaviors are perceived to be under personal control [17], while employment and income status are factors considered outside of personal control [18]. These startling data further expose systemic inequities among Black Americans at the start of the pandemic.
Although adults across the US were sampled, Blacks may have been underrepresented in our sample (7%) compared to 13% of the US population [19], thereby affecting the generalizability of our interpretations. Additionally, a greater proportion of Whites (10.4–12.1% greater prevalence) reported not working prior to COVID-19 compared to Blacks (p < 0.0001 for all). This was unexpected but may be due to greater financial security prior to COVID-19 in Whites and potentially explains the higher proportion of Blacks working from home in response to stay-at-home orders. While random sampling of Whites and Blacks in sensitivity analyses yielded similar findings for heath behaviors and anxiety, follow-up of these health behaviors is warranted to examine the long-term implications of COVID-19 in Blacks.
The COVID-19 Health Behaviors Study was among the first global surveys that collected and published diverse responses from adults at the onset of COVID-19 stay-at-home orders. This survey allowed for examination of health behavior changes and factors protecting against a decline in physical activity in adults during the initial COVID-19 stay-at-home orders in the US [10, 20]. Our survey might not be the only or largest survey to assess varying responses to COVID-19 stay-at-home orders but was the first to collect information on employment and income, while simultaneously collecting information on a variety of health behaviors and anxiety at the onset of COVID-19 stay-at-home orders. Previous studies have since reported negative impacts of COVID-19 stay-at-home orders on college student’s mental health [21], weight-related behaviors in individuals with obesity [22], and found race/ethnicity-based factors as an inequity on well-being [23]. Although in-line with previous findings, our results expand upon the aforementioned studies by presenting a collective group of results overall and by race in the same sampled population.
Of note, the present findings are increasingly important as COVID-19 still has a stronghold over our pre-2020 way of life and has persisted for over 1 year [24]. As new variants are being discovered [25], Black Americans being less likely to receive the COVID-19 vaccination [26], as well as new closures to countries outside of the US [27], long-term impacts on health behaviors will likely emerge in those with greater vulnerability to income instability. Additionally, our present study did not aim to examine low-income Whites, which may also be a critically susceptible population as the COVID-19 pandemic persists. However, previous evidence suggests that Black individuals are more vulnerable during the COVID-19 pandemic compared to Whites, especially low-income Blacks [23]. Therefore, it remains prudent to prioritize mental and physical healthcare for our Black communities to halt the perpetual disparity of COVID-19 infection and impaired recovery.
Acknowledgements
The authors would like to thank Corby K. Martin, PhD, and Christoph Hoechsmann, PhD (Ingestive Behavior Laboratory, Pennington Biomedical Research Center, Baton Rouge, LA, US), for their involvement in the development of the Global Health Behaviors Study. No compensation was received for their role.
Author Contribution
LMR had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. JRS, MK, and EWF contributed equally to this work. EWF and LMR conceptualized and designed the study. All authors acquired, analyzed, and interpreted presented data and critically reviewed the manuscript for important intellectual content.
Funding
This research was funded in part by P30 DK072476; U54 GM104940.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code Availability
The SAS version 9.4 codes used for analysis of data presented in this study are available from the corresponding author upon reasonable request.
Declarations
Ethics Approval
This study was approved and overseen by the Institutional Review Board at Pennington Biomedical Research Center.
Consent to Participate
Upon following the link provided and entering the survey, interested individuals received instructions that detailed the purpose of the study, and after it was verified that they were adults, provided consent to participate.
Competing Interests
The authors declare no competing interests.
Disclaimer
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Joshua R. Sparks, Maryam Kebbe and Emily W. Flanagan contributed equally to this work.
References
- 1.Centers for Disease Control and Prevention. Coronavirus diseases 2019 (COVID-19): health equity considerations and racial and ethnic minority groups. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html. Accessed October 22, 2020.
- 2.The New York Times. The fullest look yet at the racial inequity of coronavirus. https://www.nytimes.com/interactive/2020/07/05/us/coronavirus-latinos-african-americans-cdc-data.html. Accessed October 28, 2020.
- 3.Kirby T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respir Med. 2020;8(6):547–548. doi: 10.1016/S2213-2600(20)30228-30229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Dorn A, Cooney RE, Sabin ML. COVID-19 exacerbating inequalities in the US. THE LANCET. 2020;395(10232):1243. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yancy CW. COVID-19 and African Americans. JAMA. 2020;323(19):1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 6.Hooper MW, Nápoles AM, Pérex-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abbasi J. Taking a closer look at COVID-19, health inequities, and racism. JAMA. 2020;324(5):427–429. doi: 10.1001/jama.2020.11672. [DOI] [PubMed] [Google Scholar]
- 8.Persad G, Emanuel EJ, Sangenito S. Public perspectives on COVID-19 vaccine prioritization. JAMA. 2021;4(4):e217943. doi: 10.1001/jamanetworkopen.2021.7943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dubowitz T, Dastidar MG, Troxel WM, Beckman R, Nugroho A, Siddiqi S, Cantor J, Baird M, Richardson AS, Hunter GP, Mendoza-Graff A, Collins RL. Food insecurity in a low-income, predominantly African American cohort following the COVID-19 pandemic. AJPH. 2021;111(3):494–497. doi: 10.2105/AJPH.2020.306041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flanagan EW, Beyl RA, Fearnbach SN, Altazan AD, Martin CK, Redman LM. The impact of COVID-19 stay-at-home orders on health behaviors in adults. Obesity (Silver Spring). 2020;published ahead of print. 10.1002/oby.23066 [DOI] [PMC free article] [PubMed]
- 11.Segal-Isaacson CJ, Wylie-Rosett J, Gans KM. Validation of a short dietary assessment questionnaire: the Rapid Eating and Activity Assessment for Participants short version (REAP-S). Diabetes Educ. 2004;30:774, 776, 778 passim. 10.1177/014572170403000512 [DOI] [PubMed]
- 12.Wolf AM, Hunter DJ, Colditz GA, Manson JE, Stampfer MJ, Corsano KA, Rosner B, Kriska A, Willett WC. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol. 1994;23(5):991–999. doi: 10.1093/ije/23.5.991. [DOI] [PubMed] [Google Scholar]
- 13.Ainsworth BE, Haskell WL, Herrmann D, Meckes N, Bassett DR, Jr, Tudor-Locke C, Greer JL, Vezina J, Whitt-Glover MC, Leon AS. 2011 Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 14.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing general-ized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 15.Hamilton CM, Strader LC, Pratt JG, Maiese D, Hendershot T, Kwok RK, Hammond JA, Huggins W, Jackman D, Pan H, Nettles DS, Beaty TH, Farrer LA, Kraft P, Marazita ML, Ordovas JM, Pato CN, Spitz MR, Wagener D, Williams M, Junkins HA, Harlan WR, Ramos EM, Haines J. The PhenX Toolkit: get the most from your measures. Am J Epidemiol. 2011;174(3):253–260. doi: 10.1093/aje/kwr193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The New York Times. See which states and cities have told residents to stay at home. https://www.nytimes.com/interactive/2020/us/coronavirus-stay-at-home-order.html. Accessed June 8, 2021.
- 17.Ziff MA, Conrad P, Lachman ME. The relative effects of perceived personal control and responsibility on health and health-related behaviors in young and middle-aged adults. Health Educ Behav. 1995;22(1):127–142. doi: 10.1177/109019819502200111. [DOI] [PubMed] [Google Scholar]
- 18.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(Supplement 2):19–31. doi: 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.United States Census Bureau. Race. https://www.census.gov/topics/population/race.html. Accessed December 8, 2020.
- 20.Fearnbach SN, Flanagan EW, Höchsmann C, Beyl RA, Altazan AD, Martin CK, Redman LM. Factors protecting against a decline in physical activity during the COVID-19 pandemic. Medicine & Science in Sports & Exercise. 2020;published ahead of print. doi:10.1249/MSS.0000000000002602. [DOI] [PMC free article] [PubMed]
- 21.Son C, Hegde S, Smith A, Wang X, Sasangohar F. Effects of COVID-19 on college students’ mental health in the United States: interview survey study. J Med Internet Res. 2020;22(9):e21279. doi: 10.2196/21279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Almandoz JP, Xie L, Schellinger JN, Mathew MS, Gazda C, Ofori A, Kukreja S, Messiah SE. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clinical Obesity. 2020;10(5):e12386. doi: 10.1111/cob.12386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chakrabarti S, Hamlet LC, Kaminsky J, Subramanian SV. Association of human mobility restrictions and race/ethnicity-based, sex-based, and income-based factors with inequities in well-being during the COVID-19 pandemic in the United States. JAMA Netw Open. 2021;4(4):e217373. doi: 10.1001/jamanetworkopen.2021.7373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The New York Times. A timeline of the coronavirus pandemic. https://www.nytimes.com/article/coronavirus-timeline.html. Accessed January 21, 2021.
- 25.Centers for Disease Control and Prevention. About variants of the virus that causes COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant.html. Accessed June 7, 2021.
- 26.Centers for Disease Control and Prevention. Demographic characteristics of people receiving COVID-19 vaccinations in the United States. https://covid.cdc.gov/covid-data-tracker/#vaccination-demographic. Accessed June 7, 2021.
- 27.World Health Organization. Situation Reports. Coronavirus disease (COVID-19) weekly epidemiological update and weekly operational update. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed June 7, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
The SAS version 9.4 codes used for analysis of data presented in this study are available from the corresponding author upon reasonable request.