Abstract
Metabolic syndrome is currently considered to be a global epidemic, causing a significant increase in the cost of health care, apart from deteriorating the quality of life. Skin serves as a mirror of underlying metabolic sinister. Various dermatological conditions like psoriasis, acanthosis nigricans, lichen planus, acne vulgaris, acrochordons, atopic dermatitis, etc. have been reported to be associated with metabolic syndrome. We hereby present an evidence-based review of the various dermatological conditions and their association with the development of metabolic syndrome.
Key Words: Evidence-based review, metabolic syndrome, skin
Introduction
Metabolic syndrome (MetS) also known as syndrome X or “insulin resistance syndrome” is a combination of multiple clinical parameters including abdominal obesity, hypertension, insulin resistance and dyslipidemia. One-fourth to one-third of world population is estimated to suffer from MetS and it is associated with significant morbidity and mortality.[1] Obesity acts as the primary trigger in the pathogenesis of MetS that finally contributes to insulin resistance and the final pathway of inflammation leading to Type 2 diabetes and cardiovascular disease. MetS has increasingly become relevant in recent times due to exponential increase in obesity worldwide. Although it is not a dermatological diagnosis, several cutaneous conditions have shown to have an association with MetS and thus they can serve as a clinical indicator for impending MetS and help in early diagnosis and appropriate management
Metabolic Syndrome[2]
MetS was first described as syndrome X in 1988. Over time, definition of MetS has been changed to be more refined and easy to diagnose, though the basic components remain the same. Abdominal obesity is represented by an increased waist circumference (different for males and females) and dyslipidemia by increased triglycerides and/or decreased high-density lipoprotein (HDL). Hypertension is diagnosed according to current definition and insulin resistance/hyperglycemia is identified by increased fasting glucose or type 2 diabetes mellitus. Table 1 shows the change in definition of MetS over time and the harmonized criteria.
Table 1.
Definition of metabolic syndrome, as per various crieria
| WHO | EGIR 1999 | NCEP ATPIII | IDF 2005 | Harmonized criteria | |
|---|---|---|---|---|---|
| Criteria | Insulin resistance IGF, OFG, TDM 2, evidence of IR plus two of the five | Hyperinsulinemia plus two of four | None absolute three of five | Central obesity obligatory | Three or more |
| Obesity | Waist/hip ratio >0.90 M >0.85 F or BMI >30 kg/m2 | Waist circumference >94 cm M >80 cm F | Waist circumference >40 in. M >35 in. F | Waist circumference >94 cm M >80 cm F | Waist circumference >90 cm M >80 cm F |
| Hyperglycaemia | Insulin resistance | Insulin resistance | Fasting glucose >100 mg | Fasting glucose >100 mg | Fasting glucose >5.6 mmol/l or T2DM |
| Dyslipidemia | Triglycerides >150 mg/dl | TG >177 mg/dl | TG >150 mg/dl | TG >150 mg/dl | TG >1.69 mmol/l or on previous antilipidemic treatment |
| HDL <35 mg/dl M <39 mg/dl F | HDL <39 mg/dl | ||||
| Dyslipidemia separate | HDL <40 mg/dl M <50 mg/dl | HDL <40 mg/dl M <50 mg/dl | HDL <1.03 mmol/l M <1.29 mmol/l F | ||
| Hypertension | >140/90 mmHg | >140/90 mmHg | >130/85 mmHg | >130/85 mmHg | >130/85 mmHg or known hypertension |
Pathogenesis
The pathogenesis of MetS is complex and remains to be fully elucidated. It is still debated whether the individual components represent distinct pathologies or manifestations of a common pathogenesis. The most widely accepted theory for the pathogenesis of MetS is visceral obesity acting as the primary trigger which leads to insulin resistance and chronic inflammation, the main players in the initiation and progress of the disease process [Figure 1].
Figure 1.
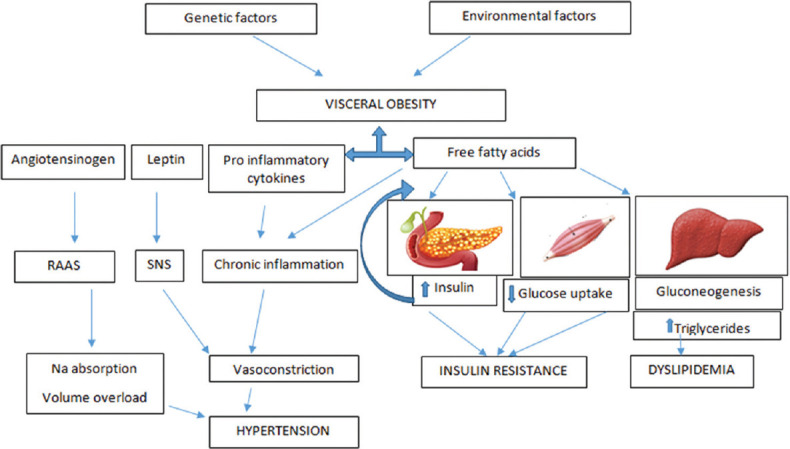
Pathophysiology of metabolic syndrome
Adipose tissue acts as an endocrine organ and produces biologically active proteins called adipokines which can be pro-inflammatory or anti-inflammatory.[3] In obesity, there is unbalanced production of the adipokines leading to a chronic low grade inflammatory state.[4] The chronic inflammation associated with visceral adiposity contributes to the activation of the renin-angiotensin-aldosterone system (RAAS), sympathetic nervous system (SNS) and vasoconstrictive effects which ultimately leads to hypertension.
Visceral obesity increases the amount of free fatty acids (FFA) in the body and that in turn causes decreased uptake of glucose in the muscles. In the liver, FFA increases the production of glucose by gluconeogenesis. This increased blood glucose level, in turn induces greater insulin secretion from the pancreas. Insulin itself has a lipolytic effect which increases FFA levels. This leads to a vicious cycle.
FFA increases production of triglycerides and VLDL in the liver. In addition to that, there is a decrease in HDL.
All these changes cumulatively lead to the development of type 2 diabetes (T2DM) and coronary artery disease (CAD).
Dermatoses associated with metabolic syndrome
The cascade of inflammatory changes associated with MetS is also shared by certain dermatoses. Thus, any pathophysiological dysfunction in metabolic parameters in the body may contribute to skin diseases and vice versa. Certain dermatoses have very strong association with MetS and hence, they can act as cutaneous marker of the latter. For example, psoriasis seems to have similar genetic propensities and risk factors to MetS, and the presence of latter may increase Psoriasis Area Severity Index (PASI). The connection to atopic dermatitis is less clear but present in significant number of patients. Acanthosis nigricans and insulin resistance have an intimate relation with MetS due to obvious pathophysiological similarities, while acne and androgenetic alopecia may have similar susceptibilities. Hence dermatologists examining these disorders at their clinic should keep an eye out for the markers of MetS in susceptible patients.[5]
Let us look at the different disorders in details:
Psoriasis
Psoriasis is a chronic inflammatory disease affecting the skin, nails and joints.
Psoriasis and MetS have a common immunpathogenesis that involves chronic inflammation by pro-inflammatory cytokines such as IFN-gamma, IL-17, IL-23 and TNF-alpha.[6,7] Chronic Th-1 and Th-17 mediated inflammatory cytokines and insulin-like growth factor 1 (IGF-1) stimulates keratinocyte proliferation in psoriasis and have a role in the pathogenesis of diabetes and hyperlipidemia.[8,9] Various studies have demonstrated an association between psoriasis and MetS. A study with 6,868 patients found a significantly higher risk of developing MetS in psoriatic patients compared to the general population (P < 0.001).[10] In a study conducted in South-East Asian population in 2014, the prevalence of MetS was found to be significantly higher in patients with psoriasis compared to healthy subjects (49.25% vs. 30.65%, P < 0.0001).[11] While a study in India found the difference to be statistically insignificant (P = 0.12).[12] Increased severity of psoriasis is also associated with higher odds of MetS.[13] Furthermore patients with psoriasis have a more difficult to control hypertension and have more vascular complications in diabetes compared to nonpsoriatic patients.[6]
Management of psoriasis with MetS is challenging since, on one hand, the syndrome affects the treatment outcome of psoriasis and on the other hand, the systemic treatments of psoriasis may lead to negative consequences of metabolic parameters. Cyclosporine may cause nephrotoxicity in obese and hypertensive patients while acitretin has a known adverse effect of dyslipidemia. Methotrexate is associated with liver fibrosis in obese, diabetic and alcoholic patients. Significant PASI improvement was observed by NBUVB in patients without MetS compared to MetS patients (P = <0.05).[14] Similar results were observed with etanercept where a BMI of >30 kg/m2 showed a decreasing effect on its efficacy.[15] Better response to secukinumab was observed in patients who weighed <90 kg compared to those who weighed above it.[16] However, ustekinumab demonstrated better results in obese individuals.[16] On the other hand, pioglitazone and metformin have demonstrated improvement in PASI along with metabolic parameters.[17] Simvastatin demonstrated a faster decrease in PASI scores compared to patients not on it.[18] This shows that treating comorbidities along with psoriasis is the best way to control disease severity. The comorbidities and adverse effects associated with the use of drugs is outlined in Table 2.
Table 2.
Therapy for psoriasis causing adverse effects in comorbidities
| Therapy | Comorbidities | Adverse effects |
|---|---|---|
| Cyclosporine | Obesity, hypertension | Nephrotoxicity |
| Acitretin | Obesity | Dyslipidemia |
| Methotrexate | Obesity, diabetes | Liver fibrosis |
Acanthosis nigricans
Acanthosis Nigricans is a common, easily identifiable marker of underlying MetS. It is characterized by hyperpigmented, leathery patches most commonly over nape of neck, axillae and groin. Hyperinsulinemia stimulates keratinocytes and fibroblasts leading to these characteristic leathery patches. Patients with facial AN need a thorough evaluation for detection of MetS.[19] Increased waist to hip ratio (WHR) (P < 0.001), hyperglycemia (P = 0.001), and dyslipidemia (P = 0.228) were found in patients with facial AN. Another study found a higher prevalence of MetS in obese women with AN (60%) compared to controls (37.6%) (P = 0.0001).[20] Significant positive correlation was also found between AN and BMI, fasting insulin and HOMA-IR. So AN can be a useful clinical tool to identify patients at risk of developing MetS.
Acne
Acne vulgaris is an inflammatory disorder involving the sebaceous glands influenced by excess sebum production, altered follicular keratinization, Propionibacterium acnes colonization and inflammation. The common pathogenesis in acne and MetS is enhanced activity of mechanistic target of rapamycin complex 1 (mTORC1). The activity of mTORC1 was found to be elevated in both involved and noninvolved skin of patients of acne vulgaris.[21] Enhanced mTORC1 signaling is also a known characteristic of insulin resistance, obesity, and T2DM.[22] A study in adult men with acne found the prevalence of MetS to be comparable between cases (17%) and controls (9%) (P = .09).[23] However prevalence of insulin resistance was significantly higher in cases (22%) compared to controls (11%) (P = 0.03). Acne in women has been linked with insulin resistance and dyslipidemia.[24] Metformin, an oral antidiabetic drug and an mTORC1 inhibitor caused a reduction of acne in young males who adopted a hypoglycemic diet in conjunction with the drug.[25] Since patients with acne have a higher tendency to develop insulin resistance; close observation is significant for controlling disease progression to T2DM.
Rosacea
Rosacea is a complex chronic disorder of the face with a number of overlapping features like persistent erythema, telangiectasia, papules, pustules, phymatous changes and sometimes ocular manifestations. The current idea about pathophysiology of rosacea is that it involves a disordered and hyperactive immune system (mainly innate, but sometimes adaptive immunity as well), that can cause inflammation and vasodilatation, coupled with neurogenic dysregulation and other external trigger factors.[26]
A 2013 study had shown rosacea patients to have more incidence of dyslipidemia and cardiovascular diseases.[27] while a 2015 study has noted association of moderate-to-severe rosacea with metabolic disorders, hypertension and hyperlipidemia.[28]
Following this, a study by Akin Belli et al.[29] found MetS (P = 0.186) and insulin resistance (P < 0.009) to be higher in rosacea group compared to healthy controls. They hypothesized that insulin resistance and rosacea have similar pathophysiological factors like raised cathelicidin LL-37, oxidative stress and pro-inflammatory cytokines; hence they can occur together in a patient. Therefore they recommended testing for insulin resistance by HOMA-IR in rosacea patients.
Hidradenitis suppurativa
Hidradenitis suppurativa is a chronic, recurrent disease involving hair follicles in intertriginous areas like axillary, inframammary and inguinal regions. It presents with painful recurrent nodules, pustules, sinuses and abscesses which cause scarring and deformity and significantly degrades the quality of life of the patient. The pathophysiology is not clearly known, but postulated to be perifollicular inflammation which causes occlusion and bursting of hair follicles leading to sustained inflammation and the subsequent clinical features. Contributing factors include dysregulated immune system, genetics, smoking and obesity.[30]
A meta-analysis found a significant association between HS and smoking, dyslipidemia, obesity, MetS; and also mentioned that the severity of HS increases with increase in these risk factors.[31] Obesity is said to provide a low-grade pro-inflammatory environment and increase friction in intertriginous areas (leading to follicular occlusion).[30] The meta-analysis also noted that reduction in weight can lead to spontaneous resolution of mild disease, while treatment response rate of severe disease improves with weight loss as well. Diabetes mellitus and increased insulin levels can cause hypersensitivity of follicular androgen receptors and contribute to HS.[31]
A study demonstrated that patients with high BMI may have a more severe disease along with joint pain and respond less to treatment.[32] Another study noted post bariatric surgery patients with significant weight loss reporting a reduction in the severity of HS.[33] Metformin, a drug for insulin resistance and hyperglycemia, has been effective in controlling symptoms of HS, thereby demonstrating the role of insulin and glucose in the pathogenesis of HS.[34]
Androgenetic alopecia
Androgenetic alopecia is a common hair loss disorder in males and females which is genetic and androgen dependent and presents with age related thinning.[35] Elevated insulin levels favors vasoconstriction and nutritional deficiency in the follicles of the scalp and it enhances the effect of DHT on follicular miniaturization.[36] AGA, diabetes and hypertension often have familial connection. A case-control study with patients of AGA in India showed higher prevalence of MetS (P = 0.001) and higher levels of triglycerides and blood pressure (P < 0.05).[35] Another study with female patients found a significant correlation between female pattern hair loss and hypertension and central obesity. They postulated the role of testosterone in increasing insulin resistance which can contribute to female pattern hair loss, and androgens and aldosterone behind the common occurrence of hair loss and hypertension.[37] Another population based survey also noted connection between male AGA and components of MetS, notably HDL-C.[38]
All the studies recommend investigating for components of MetS in patients with AGA, as early treatment of MetS can prevent future complications. Lowering of insulin resistance and losing weight might help improve hair growth.
Lichen planus
Lichen planus is a chronic disease affecting the skin, mucous membranes and appendages. Patients with lichen planus were found to have significantly higher markers of metabolic and cardiovascular risk factors compared to controls (P < 0.001).[39,40] Among the various parameters of MetS, dyslipidemia were found to be significantly higher in patients of lichen planus. This has been attributed to the high levels of ESR, CRP and fibrinogen in lichen planus. Screening for lipid levels may be useful in patients of lichen planus to detect individuals at risk and start preventive treatment against MetS.
Atopic dermatitis
Atopic dermatitis is a chronic pruritic relapsing inflammatory skin condition. A cross sectional study in Korean adult women with atopic dermatitis found an association with MetS (P = 0.02) and increased triglyceride level (P = 0.05).[41] One possible explanation is that both diseases have altered expression of T cell cytokines.
Others
Multiple skin tags can be a sign of insulin resistance, while xanthoma and xanthelasma can be signs of dyslipidemia, which are linked to MetS.[42]
Seborrheic dermatitis has also recently been suggested as a predictive factor for MetS.[43]
A Brazilian study has noted correlation between pemphigus (vulgaris and foliaceous) and MetS, but suggested steroid use to be a confounding factor.[44]
A study on animal model by Nagase T et al.[45] noted accelerated skin aging in MetS, believed to be mediated by molecular pathways like oxidative stress.
A case series has reported failure of skin grafting in patients with high waist-hip ratio, which is a marker of MetS.[46]
Conclusion
Hence we see that MetS; a systemic disease has an intimate relationship with multiple cutaneous diseases. Patients presenting with these diseases, the markers of MetS, should be asked about and, if required, investigated for the presence of MetS. This can help an early diagnosis of a systemic disease with numerous complications. The dermatoses also respond better to treatment if underlying metabolic problems are corrected.
Further investigations are needed to detect all the connections between the skin and MetS, and dermatologists should have a better understanding of the same, to help patients with dermatoses as well as metabolic complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hu Y, Zhu Y, Lian N, Chen M, Bartke A, Yuan R. Metabolic syndrome and skin diseases. Front Endocrinol (Lausanne) 2019;10:788. doi: 10.3389/fendo.2019.00788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stefanadi EC, Dimitrakakis G, Antoniou CK, Challoumas D, Punjabi N, DImitrakaki IA, et al. Metabolic syndrome and the skin: A more than superficial association. Reviewing the association between skin diseases and metabolic syndrome and a clinical decision algorithm for high risk patients. Diabetol Metab Syndr. 2018;10:9. doi: 10.1186/s13098-018-0311-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cleeman JI. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) J Am Med Assoc. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 4.Leroith D. Pathophysiology of the metabolic syndrome: Implications for the cardiometabolic risks associated with type 2 diabetes. Am J Med Sci. 2012;343:13–6. doi: 10.1097/MAJ.0b013e31823ea214. [DOI] [PubMed] [Google Scholar]
- 5.Karadag AS, Lavery MJ. Skin and the metabolic syndrome. Clin Dermatol. 2018;36:1–2. doi: 10.1016/j.clindermatol.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Armstrong EJ, Harskamp CT, Armstrong AW. Psoriasis and major adverse cardiovascular events: A systematic review and meta-analysis of observational studies. J Am Heart Assoc. 2013;2:1–10. doi: 10.1161/JAHA.113.000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Popa C, Netea MG, van Riel PLCM, van der Meer JW, Stalenhoef AFH. The role of TNF-α in chronic inflammatory conditions, intermediary metabolism, and cardiovascular risk. J Lipid Res. 2007;48:751–62. doi: 10.1194/jlr.R600021-JLR200. [DOI] [PubMed] [Google Scholar]
- 8.Azfar RS, Gelfand JM. Psoriasis and metabolic disease: Epidemiology and pathophysiology. Curr Opin Rheumatol. 2008;20:416–22. doi: 10.1097/BOR.0b013e3283031c99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davidovici BB, Sattar N, Jörg PC, Puig L, Emery P, Barker JN, et al. Psoriasis and systemic inflammatory diseases: Potential mechanistic links between skin disease and co-morbid conditions. J Invest Dermatol. 2010;130:1785–96. doi: 10.1038/jid.2010.103. [DOI] [PubMed] [Google Scholar]
- 10.Fernández-Armenteros JM, Gómez-Arbonés X, Buti-Soler M, Betriu-Bars A, Sanmartin-Novell V, Ortega-Bravo M, et al. Psoriasis, metabolic syndrome and cardiovascular risk factors.A population-based study. J Eur Acad Dermatol Venereol. 2019;33:128–35. doi: 10.1111/jdv.15159. [DOI] [PubMed] [Google Scholar]
- 11.Kokpol C, Aekplakorn W, Rajatanavin N. Prevalence and characteristics of metabolic syndrome in South-East Asian psoriatic patients: A case-control study. J Dermatol. 2014;41:898–902. doi: 10.1111/1346-8138.12614. [DOI] [PubMed] [Google Scholar]
- 12.Praveenkumar U, Ganguly S, Ray L, Nanda SK, Kuruvila S. Prevalence of metabolic syndrome in psoriasis patients and its relation to disease duration: A hospital based case-control study. J Clin Diagn Res. 2016;10:WC01–5. doi: 10.7860/JCDR/2016/17791.7218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Langan SM, Seminara NM, Shin DB, Troxel AB, Kimmel SE, Mehta NN, et al. population-based study in the United Kingdom. J Invest Dermatol. 2012;132:556–62. doi: 10.1038/jid.2011.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rui W, Xiangyu D, Fang X, Long G, Yi Y, Wenjuan W, et al. Metabolic syndrome affects narrow-band UVB phototherapy response in patients with psoriasis. Medicine (Baltimore) 2017;96:e8677. doi: 10.1097/MD.0000000000008677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Giunta A, Babino G, Ruzzetti M, Manetta S, Chimenti S, Esposito M. Influence of body mass index and weight on etanercept efficacy in patients with psoriasis: A retrospective study. J Int Med Res. 2016;44:72–5. doi: 10.1177/0300060515593254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gisondi P, Del Giglio M, Girolomoni G. Considerations for systemic treatment of psoriasis in obese patients. Am J Clin Dermatol. 2016;17:609–15. doi: 10.1007/s40257-016-0211-7. [DOI] [PubMed] [Google Scholar]
- 17.Singh S, Bhansali A. Randomized placebo control study of insulin sensitizers (Metformin and Pioglitazone) in psoriasis patients with metabolic syndrome (Topical Treatment Cohort) BMC Dermatol. 2016;16:12. doi: 10.1186/s12895-016-0049-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Trong HN, Nguyen TT, Nguyen ATT, Uyen NP, Van TN, Hau KT, et al. Efficacy of adding oral simvastatin to topical therapy for treatment of psoriasis: The vietnamese experience. Open Access Maced J Med Sci. 2019;7:237–42. doi: 10.3889/oamjms.2019.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Panda S, Das A, Lahiri K, Chatterjee M, Padhi T, Rathi S, et al. Facial acanthosis nigricans: A morphological marker of metabolic syndrome. Indian J Dermatol. 2017;62:591–7. doi: 10.4103/ijd.IJD_545_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ayaz T, Sahin SB, Sahin OZ. Relation of acanthosis nigricans to metabolic syndrome in overweight and obese women. Metab Syndr Relat Disord. 2014;12:320–3. doi: 10.1089/met.2013.0145. [DOI] [PubMed] [Google Scholar]
- 21.Monfrecola G, Lembo S, Caiazzo G, Vita VD, Caprio RD, Balato A, et al. Mechanistic target of rapamycin (mTOR) expression is increased in acne patients' skin. Exp Dermatol. 2016;25:153–5. doi: 10.1111/exd.12885. [DOI] [PubMed] [Google Scholar]
- 22.Melnik BC. Dietary intervention in acne: Attenuationof increased mTORC1 signaling promoted by Western diet. Dermatoendocrinol. 2012;4:20–32. doi: 10.4161/derm.19828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nagpal M, De D, Handa S, Pal A, Sachdeva N. Insulin resistance and metabolic syndrome in young men with Acne. JAMA Dermatol. 2016;152:399–404. doi: 10.1001/jamadermatol.2015.4499. [DOI] [PubMed] [Google Scholar]
- 24.Kartal D, Yildiz H, Ertas R, Borlu M, Utas S. Association between isolated female acne and insulin resistance: A prospective study. G Ital Dermatol Venereol. 2016;151:353–7. [PubMed] [Google Scholar]
- 25.Fabbrocini G, Izzo R, Faggiano A, Del Prete M, Donnarumma M, Marasca C, et al. Low glycaemic diet and metformin therapy: A new approach in male subjects with acne resistant to common treatments. Clin Exp Dermatol. 2016;41:38–42. doi: 10.1111/ced.12673. [DOI] [PubMed] [Google Scholar]
- 26.Marson JW, Baldwin HE. Rosacea: A wholistic review and update from pathogenesis to diagnosis and therapy. Int J Dermatol. 2020;59:e175–82. doi: 10.1111/ijd.14757. [DOI] [PubMed] [Google Scholar]
- 27.Duman N, Ersoy Evans S, Atakan N. Rosacea and cardiovascular risk factors: A case control study. J Eur Acad Dermatol Venereol. 2014;28:1165–9. doi: 10.1111/jdv.12234. [DOI] [PubMed] [Google Scholar]
- 28.Rainer BM, Fischer AH, Luz Felipe Da Silva D, Kang S, Chien AL. Rosacea is associated with chronic systemic diseases in a skin severity-dependent manner: Results of a case-control study. J Am Acad Dermatol. 2015;73:604–8. doi: 10.1016/j.jaad.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 29.Belli AA, Gok SO, Akbaba G, Etgu F, Dogan G. The relationship between rosacea and insulin resistance and metabolic syndrome. Eur J Dermatol. 2016;26:260–4. doi: 10.1684/ejd.2016.2748. [DOI] [PubMed] [Google Scholar]
- 30.Vinkel C, Thomsen SF. Hidradenitis suppurativa: Causes, features, and current treatments. J Clin Aesthet Dermatol. 2018;11:17–23. [PMC free article] [PubMed] [Google Scholar]
- 31.Tzellos T, Zouboulis CC, Gulliver W, Cohen AD, Wolkenstein P, Jemec GBE. Cardiovascular disease risk factors in patients with hidradenitis suppurativa: A systematic review and meta-analysis of observational studies. Br J Dermatol. 2015;173:1142–55. doi: 10.1111/bjd.14024. [DOI] [PubMed] [Google Scholar]
- 32.Theut P, Saunte DM, Benhadou F, Marmol VD, Guillem P, El-Domyati M, et al. Low and high body mass index in hidradenitis suppurativa patients—different subtypes? J Eur Acad Dermatol Venereol. 2018;32:307–12. doi: 10.1111/jdv.14599. [DOI] [PubMed] [Google Scholar]
- 33.Kromann CB, Ibler KS, Kristiansen VB, Jemec GBE. The influence of body weight on the prevalence and severity of hidradenitis suppurativa. Acta Derm Venereol. 2014;94:553–7. doi: 10.2340/00015555-1800. [DOI] [PubMed] [Google Scholar]
- 34.Verdolini R, Clayton N, Smith A, Alwash N, Mannello B. Metformin for the treatment of hidradenitis suppurativa: A little help along the way. J Eur Acad Dermatol Venereol. 2013;27:1101–8. doi: 10.1111/j.1468-3083.2012.04668.x. [DOI] [PubMed] [Google Scholar]
- 35.Banger HS, Malhotra SK, Singh S, Mahajan M. Is early onset androgenic alopecia a marker of metabolic syndrome and carotid artery atherosclerosis in young Indian male patients? Int J Trichology. 2015;7:141–7. doi: 10.4103/0974-7753.171566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abdelmawla MY, Esawy A, Khater E, Khalifa N. Insulin resistance in androgenetic alopecia and acne vulgaris. Egypt J Dermatol Venerol. 2019;39:83. [Google Scholar]
- 37.El Sayed MH, Abdallah MA, Aly DG, Khater NH. Association of metabolic syndrome with female pattern hair loss in women: A case-control study. Int J Dermatol. 2016;55:1131–7. doi: 10.1111/ijd.13303. [DOI] [PubMed] [Google Scholar]
- 38.Su LH, Chen THH. Association of androgenetic alopecia with metabolic syndrome in men: A community-based survey. Br J Dermatol. 2010;163:371–7. doi: 10.1111/j.1365-2133.2010.09816.x. [DOI] [PubMed] [Google Scholar]
- 39.Dreiher J, Shapiro J, Cohen AD. Lichen planus and dyslipidaemia: A case-control study. Br J Dermatol. 2009;161:626–9. doi: 10.1111/j.1365-2133.2009.09235.x. [DOI] [PubMed] [Google Scholar]
- 40.Arias-Santiago S, Buenda-Eisman A, Aneiros-Fernndez J, Giron-Prieto MS, Gutierrez-Salmeron MT, Mellado VG, et al. Cardiovascular risk factors in patients with lichen planus. Am J Med. 2011;124:543–8. doi: 10.1016/j.amjmed.2010.12.025. [DOI] [PubMed] [Google Scholar]
- 41.Lee JH, Jung HM, Han K Do, Lee SH, Lee JY, Park YG, et al. Association between metabolic syndrome and atopic dermatitis in Korean adults. Acta Derm Venereol. 2017;97:77–80. doi: 10.2340/00015555-2441. [DOI] [PubMed] [Google Scholar]
- 42.Holzer G, Straßegger B, Volc-Platzer B. Cutaneous manifestations of metabolic syndrome. Hautarzt. 2016;67:982–8. doi: 10.1007/s00105-016-3891-2. [DOI] [PubMed] [Google Scholar]
- 43.Imamoglu B, Hayta SB, Guner R, Akyol M, Ozcelik S. Metabolic syndrome may be an important comorbidity in patients with seborrheic dermatitis. Arch Med Sci Atheroscler Dis. 2016;1:e158–61. doi: 10.5114/amsad.2016.65075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ambiel MV, Roselino AM. Prevalence of metabolic syndrome and its components in a Brazilian sample of pemphigus patients. An Bras Dermatol. 2014;89:752–6. doi: 10.1590/abd1806-4841.20142930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nagase T, Akase T, Sanada H, Minematsu T, Ibuki A, Huang L, et al. Aging-like skin changes in metabolic syndrome model mice are mediated by mineralocorticoid receptor signaling. Aging Cell. 2013;12:50–7. doi: 10.1111/acel.12017. [DOI] [PubMed] [Google Scholar]
- 46.Penington AJ, Morrison WA. Skin graft failure is predicted by waist-hip ratio: A marker for metabolic syndrome. ANZ J Surg. 2007;77:118–20. doi: 10.1111/j.1445-2197.2006.03989.x. [DOI] [PubMed] [Google Scholar]


