Abstract
Background
Thoracic and lumbar spine injuries may require surgical management, particularly AO Spine types B and C injuries. Open reduction and fixation using pedicle screws, with or without fusion and/or decompression, is the gold standard surgical treatment for unstable injuries. Recent advances in instrumentation design have resulted in less-invasive surgeries. However, the literature is sparse about the effectiveness of these procedures for types B and C injuries. The objective is to compare the outcomes of conventional open surgery versus minimally invasive spine surgery (MISS) for the treatment of AO Spine types B and C thoracolumbar injuries.
Methods
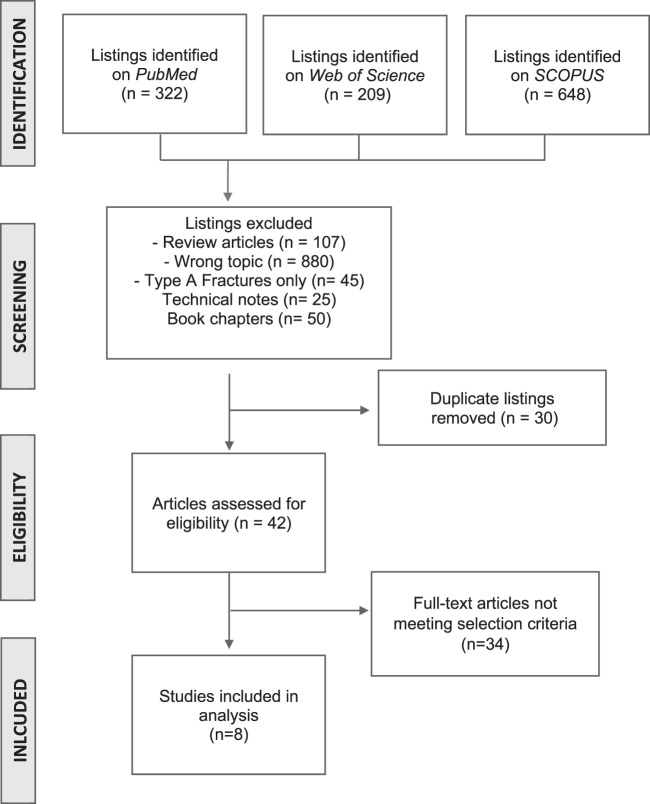
A systematic review of published literature in PubMed, Web of Science, and Scopus was performed to identify studies comparing outcomes achieved with open versus minimally invasive surgery in AO Spine types B and C thoracolumbar injury patients. Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines were used.
Results
Five retrospective case-control studies and 3 prospective studies met selection criteria. In general, most of the studies demonstrated that minimally invasive spine surgery is feasible for types B and C injuries, and associated with potential advantages like reduced blood loss, postoperative pain, and muscle injury, and shorter hospital stays. However, no differences were detected in major outcomes, like neurological status or disability.
Conclusions
Published literature currently suggests that minimally invasive spine surgery is a valid alternative for treating types B and C thoracolumbar injuries. However, further comparative prospective randomized clinical trials are necessary to establish the superiority of one approach over the other.
Level of Evidence
3.
INTRODUCTION
Thoracolumbar spine trauma is common, especially among young adults in urban areas.1 The AO Spine thoracolumbar classification system divides injuries of the thoracic and lumbar spine into 3 main groups, ranked by increasing degree of instability: type A (compression fractures), B (tension band injuries), and C (dislocations).2 Surgery is the treatment of choice to restore spinal stability and normal alignment, together with achieving decompression of neural tissue.3
Traditionally, open reduction and instrumented fusion has been considered the gold standard surgical procedure for treating spinal fractures, as fusion may restore some degree of stability at the treated levels.4,5 Interestingly, in a meta-analysis by Lan et al,6 efficacy and safety were compared between posterior fixation alone (no fusion) and fusion surgery for thoracolumbar burst fractures; of the 5 RCTs and 3 retrospective studies analyzed, incorporating 445 patients, fixation alone was associated with reduced blood loss, operating time, segmental motion, and donor-site pain, but with similar clinical and radiological results.6
Consequently, a less-invasive and safer procedure that also might accomplish the same primary treatment objectives is desirable.7 In some case series, less-invasive procedures have been described for the surgical management of AO Spine types B and C fractures, using percutaneous pedicle screw fixation, with or without facet fusion, to decrease approach-related morbidity, and these also generated clinical results similar to those of open fusion.8 Growing evidence is demonstrating that minimally invasive spine surgery (MISS) has become as effective as open surgery at treating thoracolumbar spine trauma, with advantages like less soft tissue disruption, lower infection rates, less blood loss, shorter operative time, less postoperative pain, and reduced length of hospitalization.9–11 On the other hand, the high degree of instability associated with these injuries may require fusion to restore stability, which could be impaired in MISS due to suboptimal spine preparation and exposure for proper graft insertion. Also, fracture or dislocation reduction and spine realignment may be difficult to achieve using MISS techniques, especially for type C injuries.9,10
Considering the sparse literature on this topic, the aims of this systematic review are 2-fold: (1) to compare the outcomes of AO Spine types B and C thoracolumbar injuries treated with open versus MISS techniques; and (2) to identify the indications for MISS use in patients with these fractures.
METHODS
This review was conducted following the methodological guidelines outlined by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.12 The following clinical question was formulated to guide our review: “Are the results of minimally invasive spinal techniques superior, inferior, or similar to those achieved with traditional open spinal surgery for the treatment of types B and C thoracolumbar spine injuries?”
Literature Search Strategy
PubMed, Web of Science, and Scopus were screened to identify published articles between January 2015 and April 2020 comparing outcomes for open spine surgery versus MISS in patients with either a type B or type C thoracolumbar spine injury who underwent surgery.
For our search, the following combined search terms were used: (thoracic spine fracture OR lumbar spine fracture OR thoracolumbar spine fracture) AND (percutaneous screw fixation OR minimally spine surgery) AND (open screw fixation OR conventional spine surgery).
Titles found in the 3 databases were compared; duplicate records were removed, and the remaining listings screened for inclusion by title and abstract review. Full-text manuscripts were reviewed to ensure that all relevant papers were captured, as were all cross-referenced articles. Eligibility assessments were performed independently in a standardized manner by 3 reviewers (C.C., A.G., and J.Z.). Discrepancies between the 3 reviewer's assessments were discussed with an independent, blinded fourth reviewer (R.Y.) until a consensus was reached. For further search details, please see the PRISMA flow chart in Figure 1.
Figure 1.
Systematic review flowchart, including inclusion and exclusion criteria.
Eligibility Criteria for Study Selection
Selection criteria were as follows:
article published in English,
article published in a peer-reviewed journal,
article describes either a prospective or retrospective clinical trial,
study compares thoracolumbar spine trauma treated with open spine surgery versus MISS, and
study analyzes procedural safety, impairment using the ASIA impairment scale, level of pain, and/or other clinical or radiological outcomes.
Systematic reviews and meta-analyses, letters to the editor, book chapters, commentaries, and papers that did not meet the above inclusion criteria were excluded.
Data Extraction and Analysis
After the exclusion process, the full text of each remaining article was reviewed. Baseline characteristics extracted from each paper included first author, year of publication, study architecture, ASIA impairment scale score, pain severity rated on a visual analog scale (VAS), and clinical and radiological outcomes. Data were compiled and organized using Microsoft Excel 2013 (Microsoft Corp, Redmond, Washington).
Methodological Quality Evaluation
All the studies were analyzed for internal validity and graded for level of evidence, in accordance with the Oxford Center for Evidence-Based Medicine.12
RESULTS
Across the 3 databases, 1179 potentially pertinent articles were identified. After removing duplicates and screening for inclusion and exclusion criteria, 8 studies were deemed eligible for full analysis (Table 1).
Table 1.
Studies included in the analysis.
| Study |
Fracture Type B
|
Fracture Type C
|
Level of Evidence
|
Follow-Up
|
Results
|
|
|
Operative Time
|
Blood Loss
|
|||||
| Grossbach et al 201319 | n = 38 27 Open 11 PSF | n = 0 | 2 | 13 (9–18) mo | MISS: 195 min Open: 257 min | MISS: 93 mL Open: 498 mL |
| Zhang et al 201620 | n = 10 5 B2 Open 5 B2 PSF | n = 34 17 Open 17 PSF | 2 | 12 mo | MISS: 218 min Open: 190 min | MISS: 302 mL Open: 536 mL |
| Junhui et al 201718 | n = 12 6 Open 6 Wiltse | n = 0 | 2 | 20 (12–36) mo | NA | NA |
| Wang et al 201716 | n = 9 5 Open B1/B2 4 PSF | n = 18 8 Open 10 PSF | 3 | 23 (16–33) mo | MISS: 122 min Open: 180 min | MISS: 99 mL Open: 591 mL |
| Zhang et al 201914 | n = 9 6 B2 Open 3 B2 Wiltse | n = 13 8 Open 5 Wiltse | 3 | 12 mo | MISS:128 min Open:151 min | MISS: 243 mL Open: 437 mL |
| Kreinest et al 201915 | n = 161 45 Open 116 PSF | n = 53 29 Open 24 PSF | 3 | In hospital | NA | NA |
| Lee et al 201917 | n = 13 7 Open 6 PSF | n = 0 | 3 | 9 mo | MISS:138 min Open:189 min | NA |
| Afolabi et al 202013 | n = 82 51 Open 31 PSF | n = 95 81 Open 14 PSF | 3 | In hospital | MISS: 45 min less than open surgery | MISS: 136.5 mL Open: 602 mL |
Abbreviations: CSA, cross-sectional area;MISS, minimally invasive spine surgery; NA, not applicable; ODI, Oswestry disability index; PSF, percutaneous screw fixation; VAS, visual analog scale.
Table 1.
Extended.
|
Results
|
Conclusions
|
|
|
Hospital Stay
|
Others
|
|
| MISS: 7.6 d Open: 11.2 d | Neurologic recovery: no difference | MISS has similar efficacy treating flexion-distraction injuries and allows for reduced blood loss and tissue damage, relative to open surgery. |
| MISS: 18.6 d Open: 27.5 d | Neurologic recovery: no difference x-ray time: MISS 41.6 s vs open 18.0 s VAS: MISS 1.1 vs open 2.4 | MISS as effective as open surgery and minimizes approach-related complications. However, MISS requires greater radiation dose and longer learning curve. |
| NA | CSA: with Wiltse, CSA decreased by 7.6% vs 35.4% with posterior open surgery Pain at last follow-up: 0.9 vs 1.7 (out of 10) | Wiltse approach causes less muscle damage, and less atrophy and fatty infiltration in the multifidus; reduces postoperative low back pain for up to 1 year. |
| MISS: 9.4 d Open: 20.7 d | VAS, ODI: no difference Postoperative complications and neurological recovery: no difference | MISS has a smaller incision, less intraoperative blood loss, and shorter recovery time, and is safer. |
| MISS: 6.6 d Open: 8.5d | Radiographic parameters improved in both groups Relief of canal encroachment: MISS (4.0% ± 3.8% vs open 9.1% ± 6.0%) VAS pain and neurological recovery: no difference | MISS is superior at reducing iatrogenic trauma while achieving similar or even better clinical and radiological outcomes. |
| NA | Misplaced pedicle screws or neurological deficits and need for revision surgery: no difference | Percutaneous surgery using dorsal stabilization permits positioning of pedicle screws as safely as with open surgery during acute care after spinal trauma. |
| MISS: 6.0 d Open: 9.5 d | Fluoroscopic dose: MISS 34 mSv vs open 4 mSv Hemoglobin drop: MISS 12 g/L vs open 21 g/L Kyphoticangulation correction: no difference, but with loss of position greater with open surgery (28% vs 96%) | Combined polyaxial-monoaxial screw MISS constructs demonstrate favorable radiological and clinical outcomes treating unstable thoracolumbar and lumbar fractures among patients who do not require additional decompressive surgery. |
| No difference | Need for transfusion: MISS 37% less than open surgery Mobilization/complications/mortality: no difference | MISS can be used to treat unstable thoracolumbar fractures. |
Among these, there were 5 retrospective13–17 and 3 prospective case-control studies.18–20 All studies compared MISS (percutaneous screws or the Wiltse approach) against traditional open midline surgery. A total of 547 patients were included (334 with type B and 213 with type C thoracolumbar spine fractures) with an average follow-up of 10 months, though some studies only evaluated patients during the initial admission (follow-up time range 0–33 weeks).
Among the 5 retrospective studies, 4 evaluated operative time, blood loss, length of hospital stay, complications, and neurological recovery.13,14,16,17 Kreinest et al15 compared misplaced percutaneous versus open pedicle screws, neurological deficits, and the rate of revision surgery for misplaced screws. Two prospective studies compared patients' clinical and radiological outcomes.19,20 The last prospective study, performed by Junhui et al,18 compared Wiltse's procedure against traditional open surgery and measured, as its primary outcome, multifidus cross-sectional area (CSA) on magnetic resonance imaging (MRI) to estimate the extent of muscle atrophy. Just 2 of the prospective studies were randomized.18,20
Summary of the Studies Included in Analysis (Table 1)
Afolabi et al13 compared percutaneous screw fixation (PSF) and open posterior spine surgery for fixation of thoracolumbar fractures in a retrospective case-control study. A total of 255 thoracolumbar fractures were evaluated between January 2007 and May 2011. Distribution of the injuries, by AO type, was A: 71 open and 74 PSF; B1 and B2: 38 open and 20 PSF; B3: 13 open and 11 PSF; and C: 81 open and 14 PSF. The thoracolumbar injury classification and severity score was used to distinguish operative from nonoperative candidates (>3). The choice of open versus MISS technique was per the surgeon's discretion, based on the patient's neurological status and medical history at presentation. Patients in the PSF group averaged a shorter surgical time, a mean 45 minutes less than open surgery (95% confidence interval: −63.03 to 28.36, P < .001). Comparative mean blood loss was 136.5 mL in PSF vs 602 mL in open procedures (P < .001), and there was a lower rate of blood transfusion (37% less in PSF group, P < .001). There were no differences in length of hospital stay or rate of complications/mortality (P = 1.00). The authors did not evaluate fusion rates or neurological outcomes.
Zhang et al14 compared screw placement using the Wiltse approach with canal decompression through the Kambin triangle versus traditional open approaches in a retrospective study. A total of 14 patients were treated using the Wiltse approach versus 29 by conventional open surgery. The distribution of treated injuries was type A: 15 open and 13 Wiltse; type B2: 6 open and 3 Wiltse; and type C: 8 open and 5 Wiltse. The investigators reported that the transmuscular group had a shorter mean operative time than the open surgery group (128 vs 151 minutes), less blood loss (243 vs 437 mL), and a shorter length of hospital stay (6.6 vs 8.5 days). All the radiographic parameters (degree of canal encroachment, sagittal kyphosis angle, and the fractured vertebra's anterior height, as a percentage of normal) improved postoperatively and remained improved in both groups at 12 months follow-up (P < .05).
Kreinest et al15 compared pedicle screw misplacement following open versus percutaneous posterior instrumentation after traumatic spinal fracture in a retrospective case-control study. A total of 169 patients had open surgery versus 322 with PSF. The distribution of injuries, by AO type, was type A: 151 open and 312 PSF; type B2: 45 open and 116 PSF; and type C: 29 open and 24 PSF. The primary outcome was the rate of pedicle screw misplacement. The authors categorized screw position as follows: A, screws positioned within the pedicle; B, laterally or medially breaching the pedicle wall by less than 2 mm; C, laterally or medially encroaching the pedicle wall by 2–4 mm; and D, medially or laterally, all screws breach the pedicle by 4 mm or more. Pedicle screws classified as A or B were determined to be positioned correctly. Of 733 pedicle screws placed during the open surgery procedure, 96.0% were within the safe zone, which was no different than with pedicle screws placed percutaneously (95.3% of 1884 screws). Misplaced pedicle screws were more frequent at spinal levels T7, T8, T12, and L1. In all the other categories of screw position, the number of misplaced screws did not differ between the 2 treatment groups. None of the patients in either treatment group experienced neurological deficits caused by pedicle screw misplacement. Thus, no revision surgery was necessary to replace pedicle screws. No other outcomes were measured.
Wang et al16 retrospectively compared percutaneous and open pedicle screw fixation for thoracolumbar fractures with spinal injuries. A total of 105 thoracolumbar fractures were evaluated, 56 treated with percutaneous screws (42 type A, 2 type B1, 2 type B2, and 10 type C) versus 49 by open pedicle screw fixation (36 type A, 2 type B1, 3 type B2, and 8 type C). Mean follow-up was 23 months (16–33 months). The operative time was significantly less with PSF than open pedicle screw fixation (122 vs 180 minutes, P < .001), as were blood loss (99 vs 591 mL), postoperative drainage (42 vs 343 mL) and length of hospital stay (9.4 vs 20.7 days, P < .001). Other parameters among which there were no statistically significant differences were pain severity (by VAS), Oswestry disability index, and rates of postoperative complications and neurologic recovery.
In a prospective, randomized clinical trial, Junhui et al18 compared pedicle screw fixation employing the Wiltse approach versus the conventional posterior open approach, with MRI measurement of the cross-sectional area (CSA) of the multifidus muscles used as the primary outcome. In total, 75 thoracolumbar injuries were treated (35 using a Wiltse approach and 40 by open screw fixation) with 63 type A fractures (29 in the Wiltse group and 34 by conventional open surgery) and 6 type B2 fractures in each group. Multifidus CSA was measured using digital image processing software. To determine the CSA, the region of interest was drawn around the muscles of interest on each side of the spine, taking care to avoid nearby fat, bony structures, and other soft tissues. In the Wiltse group, multifidus CSA decreased by only 7.6% (P > .05) between the preoperative and last follow-up MRI, and there was less fatty infiltration compared to open surgery. In the conventional open approach group, multifidus CSA decreased by 35.4% (P < .05) and there was more fatty infiltration. Multifidus CSA on final follow-up MRI was significantly less in the conventional group (P < .05). Among clinical outcomes, patients in the Wiltse group reported less severe (VAS) pain at the time of last follow-up (mean 20 months, range 12–36 months) than the conventional surgery group (0.9 vs 1.7, P = .013).
Grossbach et al.19 prospectively compared patients with flexion-distraction injuries between May 2003 and March 2013. A total of 38 patients with type B fractures (11 MISS and 27 open surgery) were followed for an average of 13 months (9–18 months). Patients who had undergone MISS had a shorter operative time (195 vs 257 minutes, P = .07) and less blood loss (93 vs 498 mL, P = .003). The other measured parameters (kyphotic angulation correction, length of hospital stay, and neurologic recovery) were no different in the 2 groups.
Lee et al17 retrospectively reviewed 32 patients with thoracolumbar spine fractures who underwent surgery with a percutaneous screw-rod construct versus open transpedicular Schanz screws-rod construct without decompression between July 2014 and July 2017. The MISS group had 13 patients (type A: 7, type B1: 3, and type B2: 3) and the open group 19 (type A: 12, type B1: 6, and type B2: 1). Evaluated outcomes were operative time, hemoglobin drift, fluoroscopic dose, length of hospital stay, and degrees of kyphotic angulation correction at 9 months of follow-up. Mean operative time was 50 minutes shorter in the MISS group, but this difference was not statistically significant (P = .15). Radiation exposure to the patient and surgical team was higher in the MISS group (P = .0007). With respect to kyphotic angulation correction, both groups achieved similar on-table correction; however, at last follow-up, the open surgery group experienced greater reduction than the MISS group (96% vs 28%).
In 2016, Zhang et al20 published the results of a prospective randomized clinical trial comparing 29 patients randomly assigned to MISS (type A: 7, type B2: 5, and type C: 17) and 30 who underwent open surgery (type A: 8, type B2: 5, and type C: 17). Follow-up was 12 months. Operative time was longer in the MISS group (218 vs 190 minutes), but this difference was nonsignificant (P = .165). Blood loss (302 vs 536 mL, P = .011), drainage volume (70.93 vs 310 mL, P < .001), and length of hospital stay (18.6 ± 10.3 vs 27.5 ± 15 days, P = .011) were significantly less in the MISS group. X-ray time was significantly longer in the MISS group (P < .001). The VAS and Japanese Orthopaedic Association (JOA) scores were better in the MISS group, both 1 week and 12 months after surgery (P < .05). By ASIA grade, no difference in the degree of neurological recovery was observed between the 2 groups.
DISCUSSION
For the current review, we analyzed 8 studies in which more severe traumatic injuries (types B and C) were treated with less-invasive procedures, thereby avoiding open posterior midline surgery. Of note, none of the investigative teams reported a high level of evidence evaluating major outcomes like instrumentation failure on longer-term follow-up, or disability or neurological outcomes. In general, certain advantages were observed with less-invasive procedures, like reduced blood loss and postoperative drainage, as well as decreased postoperative pain. However, for major outcomes, like functional status (mostly assessed with the Oswestry disability index, neurological improvement, and the rate of severe complications, there were no differences between the 2 treatment approaches.
Managing patients with complex posterior ligamentous injuries, like those with AO Spine type B or type C fractures, usually requires instrumented posterior fusion, as nonoperative management can lead to progressive kyphosis, increased pain, and potential neurological deterioration.21 Palmisani et al22 reported that MISS is generally used to treat type A fractures (more stable injuries), due to limitations achieving fusion using percutaneous screws or paraspinal approaches. Interestingly, the Wiltse approach provides a wider operative field than most MISS approaches, thereby allowing not only screw insertion but also better rod bending, along with the potential to correct kyphosis and indirect decompression, together with some room for posterior bone grafts.
Indications for PSF have progressively increased, as a result of its previously reported advantages (reduced muscle dissection, intraoperative blood loss, and, potentially, postoperative pain).13,14,16–20 Its use was initially limited to treating more stable fractures, due to its limitations achieving decompression, fusion, and spinal realignment. More recent indications include bony Chance fractures (type B1 in the AO Spine classification system), which only require immobilization to obtain fracture healing.23,24 Some surgeons suggest using a funnel or similar device to deliver bone graft around percutaneously inserted screws, which may promote fusion; but is this enough for more severe injury patterns, like types B2 and C injuries?23–25 In this review, some studies identified successful results with MISS treating more unstable spinal fractures.13,20 To treat these severe injuries, combining percutaneous monoaxial and polyaxial screws may add the rigidity necessary to correct some associated deformities. Lee et al,17 for instance, used monoaxial screws in a larger caudal vertebra to create a stable base for leverage, after locking the rod on the cranial polyaxial screws, which may provide good deformity correction. An additional laminectomy can also be performed when required. Zhang et al14 described how they performed a laminectomy without excising the spinous process or posterior ligaments, and reduced bone fragments in the spinal canal using a specific retractor for MISS, similar to an open procedure.
From a technical and practical point of view, we must take into account both the longer learning curve required for MISS and the excessive radiation necessary for proper implant insertion, as surface anatomical landmarks are unavailable, although the advent of navigation may significantly reduce fluoroscopic exposure.17,20 Additionally, costs may be prohibitive in some countries, especially in Latin America, where percutaneous implants are much more expensive than traditional pedicular screw systems. Finally, cross-link insertion, although possible, is challenging with minimal exposures. These limitations should be considered in the long run, as well as implant failure due to a potentially lower fusion rate, given the limitations of proper bone grafting.
Considering technical difficulties, percutaneous screw fixation was associated with higher rates of misplacement at the T4–T8 levels in a study by Youkilis et al,26 potentially due to smaller pedicle dimensions than more caudal levels, and intraoperative radiological difficulties. Similar results were reported for the Kreinest et al15 study included in our review, adding the T12 and L1 levels, once again probably due to the smaller size of the pedicles. The differences in screw misplacement using open versus percutaneous screw did not reach statistical significance, however.
The lower rate of multifidus injury using a Wiltse approach reported by Junhui et al18 could be explained by preservation of the supraspinal and interspinal ligaments when a paraspinal rather than midline approach is adopted. The natural cleavage plane between the multifidus and longissimus muscles preserves its origins, decreasing scar tissue and potentially maintaining muscle function. This also may reduce fatty degeneration and decrease back pain.18,27
Limitations
Our review was limited because of the heterogeneous methodology of the studies available for analysis, as well as the lack of prospective randomized studies evaluating major outcome measurements, like implant failure after longer follow-up, neurological outcomes, and disability. On the other hand, it provides some evidence that less-invasive procedures can be performed even in patients with complex spinal injuries, with potential benefits that include reduced early postoperative pain, reduced blood loss and less soft tissue injury, all of which may be especially useful among patients with important comorbidities such as heart disease, lung disease, or severe associated injuries.
CONCLUSIONS
In this systematic review, we found MISS to be a valid alternative for treating types B and C AO Spine injuries, with potential benefits that include reduced blood loss, soft tissue injury and hospital length of stay. However, comparative prospective randomized blinded studies remain necessary to determine whether MISS is superior or inferior to open surgery, specifically pertaining to major outcomes, like implant and fusion failure rates, disability and neurological outcomes. There are still no clear indications for MISS in patients with types B or C fractures, no consensus techniques, and no long-term results. As such, further development of the technology and techniques for more severe thoracolumbar types B and C fractures remains necessary.
ACKNOWLEDGMENTS
The authors acknowledge support from the AOSpine Latin America.
Footnotes
Disclosures and COI: The authors have declared no conflicting interest.
REFERENCES
- 1.Tee JW, Chan CH, Fitzgerald MC, Liew SM, Rosenfeld JV. Epidemiological trends of spine trauma: an Australian level 1 trauma centre study. Global Spine J. 2013;3(2):75–84. doi: 10.1055/s-0033-1337124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schnake KJ, Schroeder GD, Vaccaro AR, Oner C. AO. Spine classification systems (subaxial, thoracolumbar) J Orthop Trauma. 2017;31(suppl 4):S14–S23. doi: 10.1097/BOT.0000000000000947. [DOI] [PubMed] [Google Scholar]
- 3.Verheyden AP, Spiegl UJ, Ekkerlein H, et al. Treatment of fractures of the thoracolumbar spine: recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU) Global Spine J. 2018;8(suppl 2):34S–45S. doi: 10.1177/2192568218771668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wood KB, Li W, Lebl DR, Lebl DS, Ploumis A. Management of thoracolumbar spine fractures. Spine J. 2014;14(1):145–164. doi: 10.1016/j.spinee.2012.10.041. [DOI] [PubMed] [Google Scholar]
- 5.O'Toole JE, Kaiser MG, Anderson PA, et al. Congress of Neurological Surgeons systematic review and evidence-based guidelines on the evaluation and treatment of patients with thoracolumbar spine trauma: executive summary. Neurosurgery. 2019;84(1):2–6. doi: 10.1093/neuros/nyy394. [DOI] [PubMed] [Google Scholar]
- 6.Lan T, Chen Y, Hu SY, Li AL, Yang XJ. Is fusion superior to non-fusion for the treatment of thoracolumbar burst fracture? A systematic review and meta-analysis. J Orthop Sci. 2017;22(5):828–833. doi: 10.1016/j.jos.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 7.Court C, Vincent C. Percutaneous fixation of thoracolumbar fractures: current concepts. Orthop Traumatol Surg Res. 2012;98(8):900–909. doi: 10.1016/j.otsr.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 8.Cavanaugh D, Usmani MF, Weir TB, et al. Radiographic evaluation of minimally invasive instrumentation and fusion for treating unstable spinal column injuries. Global Spine J. 2020;10(2):169–176. doi: 10.1177/2192568219856872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pannu CD, Farooque K, Sharma V, Singal D. Minimally invasive spine surgeries for treatment of thoracolumbar fractures of spine: a systematic review. J Clin Orthop Trauma. 2019;10(suppl 1):S147–S155. doi: 10.1016/j.jcot.2019.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tian F, Tu LY, Gu WF, et al. Percutaneous versus open pedicle screw instrumentation in treatment of thoracic and lumbar spine fractures: a systematic review and meta-analysis. Medicine (Baltimore) 2018;97(41):e12535. doi: 10.1097/MD.0000000000012535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McAnany SJ, Overley SC, Kim JS, Baird EO, Qureshi SA, Anderson PA. Open versus minimally invasive fixation techniques for thoracolumbar trauma: a meta-analysis. Global Spine J. 2016;6(2):186–194. doi: 10.1055/s-0035-1554777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Afolabi A, Weir TB, Usmani MF, et al. Comparison of percutaneous minimally invasive versus open posterior spine surgery for fixation of thoracolumbar fractures: a retrospective matched cohort analysis. J Orthop. 2019;18:185–190. doi: 10.1016/j.jor.2019.11.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang B, Zhou F, Wang L, et al. A new decompression technique for upper lumbar fracture with neurologic deficit-comparison with traditional open posterior surgery. BMC Musculoskelet Disord. 2019;20(1):580. doi: 10.1186/s12891-019-2897-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kreinest M, Rillig J, Küffer M, Grützner PA, Tinelli M, Matschke S. Comparison of pedicle screw misplacement following open vs. percutaneous dorsal instrumentation after traumatic spinal fracture. Eur J Trauma Emerg Surg. doi: 10.1007/s00068-019-01245-8. 2021:47(3):727-732. [DOI] [PubMed]
- 16.Wang B, Fan Y, Dong J, et al. A retrospective study comparing percutaneous and open pedicle screw fixation for thoracolumbar fractures with spinal injuries. Medicine (Baltimore) 2017;96(38):e8104. doi: 10.1097/MD.0000000000008104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee YC, Selby M, Zotti M, Roy D, Freeman B. Minimally invasive stabilization for thoracolumbar and lumbar fractures: a comparative study with short segment open Schanz screw constructs. J Spine Surg. 2019;5(1):13–18. doi: 10.21037/jss.2019.01.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Junhui L, Zhengbao P, Wenbin X, et al. Comparison of pedicle fixation by the Wiltse approach and the conventional posterior open approach for thoracolumbar fractures, using MRI, histological and electrophysiological analyses of the multifidus muscle. Eur Spine J. 2017;26(5):1506–1514. doi: 10.1007/s00586-017-5010-1. [DOI] [PubMed] [Google Scholar]
- 19.Grossbach AJ, Dahdaleh NS, Abel TJ, Woods GD, Dlouhy BJ, Hitchon PW. Flexion-distraction injuries of the thoracolumbar spine: open fusion versus percutaneous pedicle screw fixation. Neurosurg Focus. 2013;35(2):E2. doi: 10.3171/2013.6.FOCUS13176. [DOI] [PubMed] [Google Scholar]
- 20.Zhang W, Li H, Zhou Y, et al. Minimally invasive posterior decompression combined with percutaneous pedicle screw fixation for the treatment of thoracolumbar fractures with neurological deficits: a prospective randomized study versus traditional open posterior surgery. Spine (Phila Pa 1976) 2016;41(suppl 19):B23–B29. doi: 10.1097/BRS.0000000000001814. [DOI] [PubMed] [Google Scholar]
- 21.Joaquim AF, Schroeder GD, Patel AA, Vaccaro AR. Clinical and radiological outcome of non-surgical management of thoracic and lumbar spinal fracture-dislocations—a historical analysis in the era of modern spinal surgery. J Spinal Cord Med. 2020;43(1):3–9. doi: 10.1080/10790268.2018.1474692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Palmisani M, Gasbarrini A, Brodano GB, et al. Minimally invasive percutaneous fixation in the treatment of thoracic and lumbar spine fractures. Eur Spine J. 2009;18(Suppl 1):71–74. doi: 10.1007/s00586-009-0989-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beringer W, Potts E, Khairi S, Mobasser JP. Percutaneous pedicle screw instrumentation for temporary internal bracing of nondisplaced bony Chance fractures. J Spinal Disord Tech. 2007;20(3):242–247. doi: 10.1097/BSD.0b013e31802d839c. [DOI] [PubMed] [Google Scholar]
- 24.Schizas C, Kosmopoulos V. Percutaneous surgical treatment of chance fractures using cannulated pedicle screws. Report of two cases. J Neurosurg Spine. 2007;7(1):71–74. doi: 10.3171/SPI-07/07/071. [DOI] [PubMed] [Google Scholar]
- 25.Ni WF, Huang YX, Chi YL, et al. Percutaneous pedicle screw fixation for neurologic intact thoracolumbar burst fractures. J Spinal Disord Tech. 2010;23(8):530–537. doi: 10.1097/BSD.0b013e3181c72d4c. [DOI] [PubMed] [Google Scholar]
- 26.Youkilis AS, Quint DJ, McGillicuddy JE, Papadopoulos SM. Stereotactic navigation for placement of pedicle screws in the thoracic spine. Neurosurgery. 2001;48(4):771–778. doi: 10.1097/00006123-200104000-00015. discussion 778–779. [DOI] [PubMed] [Google Scholar]
- 27.Fan SW, Hu ZJ, Fang XQ, Zhao FD, Huang Y, Yu HJ. Comparison of paraspinal muscle injury in one-level lumbar posterior inter-body fusion: modified minimally invasive and traditional open approaches. Orthop Surg. 2010;2(3):194–200. doi: 10.1111/j.1757-7861.2010.00086.x. [DOI] [PMC free article] [PubMed] [Google Scholar]