Abstract
Objective
To examine the effects of a positive deviance intervention on dual-method contraceptive use among married or in-union women.
Design
Open-label cluster randomised controlled trial.
Setting
20 health facilities in Mbarara District, Uganda.
Participants
960 married or in-union women aged 18–49 years using a non-barrier modern contraceptive method.
Interventions
A combination of clinic-based and telephone-based counselling and a 1-day participatory workshop, which were developed based on a preliminary qualitative study of women practising dual-method contraception.
Primary outcome measure
Dual-method contraceptive use at the last sexual intercourse and its consistent use in the 2 months prior to each follow-up. These outcomes were measured based on participants’ self-reports, and the effect of intervention was assessed using a mixed-effects logistic regression model.
Results
More women in the intervention group used dual-method contraception at the last sexual intercourse at 2 months (adjusted OR (AOR)=4.12; 95% CI 2.02 to 8.39) and 8 months (AOR=2.16; 95% CI 1.06 to 4.41) than in the control group. At 4 and 6 months, however, the proportion of dual-method contraceptive users was not significantly different between the two groups. Its consistent use was more prevalent in the intervention group than in the control group at 2 months (AOR=14.53; 95% CI 3.63 to 58.13), and this intervention effect lasted throughout the follow-up period.
Conclusions
The positive deviance intervention increased dual-method contraceptive use among women, and could be effective at reducing the dual risk of unintended pregnancies and HIV infections. This study demonstrated that the intervention targeting only women can change behaviours of couples to practise dual-method contraception. Because women using non-barrier modern contraceptives may be more reachable than men, interventions targeting such women should be recommended.
Trial registration number
UMIN000037065.
Keywords: public health, HIV & AIDS, epidemiology
Strengths and limitations of this study.
The outcomes were measured based on participants’ self-reports and therefore subject to measurement errors because of recall and social desirability biases.
Due to the small number of clusters, several characteristics of the participants were not balanced between the intervention and control groups.
However, mixed-effects logistic regression analysis was performed by controlling the cluster effects and the differences in baseline characteristics to evaluate the intervention’s effects.
This intervention was developed using the positive deviance approach which aimed to promote behaviours of individuals who had achieved rare success to other community members.
Women who used dual-method contraception in the study area contributed the intervention’s development and implementation as peer counsellors.
Introduction
Unintended pregnancy and HIV infection remain major public health concerns in sub-Saharan Africa (SSA). In SSA, almost 30% of pregnancies were unintended, whereas women accounted for 59% of an estimated 980 000 new HIV infections that occurred among adults in 2018.1 2 Sexual intercourse is a major route of HIV transmission, and a significant gender disparity in HIV infection begins when women reach reproductive age.3 Women contract HIV 5–7 years of age earlier than men, and women aged 15–24 years are 2.4 times more likely to become infected with HIV than their male counterparts.2 4 In SSA, therefore, women of reproductive age bear the dual burden of unintended pregnancies and HIV.
Dual-method contraceptive use has been proposed as an effective strategy for preventing unintended pregnancies and sexually transmitted infections (STIs), including HIV.5 It is defined as the use of a non-barrier modern contraceptive method (eg, injectables, implants, oral contraceptive pills, intrauterine devices and sterilisation) in combination with a barrier method, such as male or female condoms.5 Despite the high incidence rate of HIV, dual-method contraception is not commonly practised in SSA, especially among women in long-term relationships.5 6 For instance, only 3.8% of married women in Zimbabwe used dual-method contraception with their partners.6 In South Africa, only 16.2% of married and cohabiting women reported consistent condom use, and they faced several barriers to using condoms, such as infidelity and distrust within relationships.7 Furthermore, women in stable relationships tend to prioritise non-barrier methods over barrier methods and are less likely to use condoms when using other methods.8 9 Although the majority of women understand that condom use is critical for preventing HIV/STIs, they do not practise it.10 Marital sexual intercourse becomes one of the major routes of HIV infection because of inconsistent or no condom use in SSA.11
Several studies examined interventions for promoting dual-method contraceptive use.5 However, few showed a significant effect on the dual-method use, and their impact was often unsustainable.12 To our knowledge, the only intervention that demonstrated a continued effect on the dual-method use over 6 months was a combination of case management and peer leadership programmes among adolescents in the USA.13 In SSA, conditional lottery incentives increased dual-method use among South African women at 3 months but not at 6 months after the intervention.14 Effectiveness of behavioural change interventions on the dual-method use among married or in-union women remains lacking in SSA.5
Uganda is one of the countries most affected by the HIV epidemic, with an adult prevalence (aged 15–64 years) of 6.2% in 2017.15 Like other SSA countries, this rate was higher among women (7.6%) than men (4.7%).15 Uganda has marked a substantial increase in the use of modern contraceptives.16 The prevalence of such use has increased from 14% in 2001 to 35% in 2016 among married or in-union women.16 17 Non-barrier modern contraceptives are the most popular methods, with 32% of currently married or in-union women of reproductive age using them.17 However, condom use remains low in Uganda, especially among women in long-term relationships. That is, only 2% of women reported condom use with regular partners during their last sexual intercourse.17
The positive deviance approach is based on the premise that there are community members who solve problems while many of their peers do not.18 This approach seeks unique behaviours of such exceptional people (positive deviants or PDs) and disseminates these behaviours to the whole community through community-led and peer-based interventions.18 19 We previously conducted a qualitative study to examine the unique behaviours of PDs (ie, women using dual method with marital or in-union partners) in Mbarara District, Uganda.20 These PDs successfully practised dual-method contraception by initiating discussions, educating their partners on sexual risks and condom use and obtaining condoms.20 In this study, we examined the effectiveness of an intervention developed based on those findings to promote dual-method contraceptive use among women in the same area.
Methods
Study design and settings
A cluster randomised controlled trial was conducted for 8 months (November 2019 to July 2020) in Mbarara District in Southwestern Uganda. The protocol of the trial has been previously published.21 The population of Mbarara District is 472 629 (female=50.6%; male=49.4%), and about a half of the female population (45.7%) are estimated within the reproductive ages (15–49 years).22
The prevalence of HIV is geographically diverse in Uganda, and the Southwestern region has one of the highest prevalence rates of HIV at 7.9% among adults. This rate is higher among women (9.3%) than men (6.3%).15 All public health facilities provide non-barrier modern contraceptives and male condoms free of charge. Male condoms are also available for purchase at pharmacies and markets for US$0.15–US$0.50.20
To recruit a sufficient number of participants, 20 facilities were purposively selected out of 48 public health facilities in Mbarara District.23 All health facilities at the subcounty level or above were selected followed by health facilities at the parish level, which had a high number of outpatients.23 These facilities included 1 general hospital, 3 county-level health centres, 11 subcounty-level health centres and 5 parish-level health centres. Among them, seven facilities were located in urban areas.23
Study participants and enrolment
The inclusion criteria were women (1) aged 18–49 years, (2) having had sexual intercourse in the last 3 months, (3) using non-barrier modern contraceptives, and who (4) desire to avoid pregnancy for 12 months from recruitment, (5) have a husband or live-in sexual partner, and (6) have access to a valid phone number. The exclusion criteria were women who were (1) pregnant, (2) infertile for other reasons, and (3) had been using condoms consistently with a non-barrier modern contraceptive in the last 2 months before the recruitment. The sample size of 960 was calculated based on the effect size of 2.43 reported in a dual-method intervention trial in the USA, considering an intraclass correlation coefficient of 0.006 and a 26% dropout rate.12 13 24 The power of the study was set at 80%, and the significance level was set at 5%. OpenEpi V.3 was used to calculate the sample size.
Convenience sampling method was used to recruit study participants. Female research assistants recruited women at the selected health facilities. They approached every third woman visiting the family planning section at each facility to minimise selection bias and informed them the opportunity to participate in the study. If a woman was interested, they confirmed non-barrier modern contraceptive use with her family planning client record card and asked questions to verify eligibility. The process was repeated until the required sample size was reached.
Randomisation and masking
The 20 health facilities were stratified based on their level and urban or rural status. They were then randomised to either intervention or control group with a 1:1 allocation ratio. Then, 960 women were allocated to the intervention (n=480) or control group (n=480) based on the facilities at which they were recruited. An independent researcher who was not involved in the data collection or analysis carried out the allocation using computer-generated random sequences. Blinding was not feasible in this study due to the nature of the intervention. However, the research assistants who performed the outcome assessment were not informed the intervention allocation.
Intervention
The intervention was developed based on the results of the preliminary study of nine PDs conducted in Mbarara District, Uganda, in October 2019.20 The PDs were identified by screening 150 women using non-barrier modern contraceptives at five health facilities. Then, in-depth interviews were conducted with the PDs. Thematic analysis was performed using the positive deviance framework to identify the unique behaviours associated with dual-method contraceptive use. The findings of the study have been published.20
Out of the nine PDs, four joined the intervention as peer counsellors, whereas the other five were unable to participate due to other commitments. The four PDs demonstrated dual-method contraceptive use at least 2 months before the screening. The mean age of the four PDs was 29.8 years (SD 6.0 years).
Table 1 summarises the intervention, which combined clinic-based and phone-based counselling and a participatory workshop, to disseminate the unique practices of the PDs.20 After the baseline interview on the day of enrolment, women received counselling focusing on dual-method contraception in addition to regular family planning counselling. Trained research assistants delivered the counselling for about 20–30 min. Women received the handout used during the counselling developed either in English or Runyankore and were encouraged to initiate discussions on dual-method contraceptive use with their partners. The handout included several quotes from the PDs, such as ‘If I tell him to use a condom suddenly before having sex, he may get surprised and angry… if he gets mad, it is difficult to keep discussing it. So, I brought up this sensitive topic when he seemed to be in a good mood.’20
Table 1.
Overview of intervention
| Training setting | Duration | Topics covered |
| Clinic-based counselling | 20–30 min |
|
| One-day workshop at a health facility facilitated by PDs | 5 hours |
|
| Bimonthly phone-based counselling | 15–30 min each |
|
*Women in the control group received only these interventions using the existing tool.
PD, positive deviant; STI, sexually transmitted infection.
After 2 weeks of enrolment, women in the intervention group were invited for a 1-day participatory learning workshop at the same health facility where they were recruited. Participation in the workshop was voluntary. The four PDs facilitated the workshop with support from the research assistants. It included role-play exercises to enable women to acquire successful communication skills for discussions with their partners, practice of male condom use and group discussions about the dual risk of unintended pregnancies and HIV/STIs from their partners.
In addition, women in the intervention group received a bimonthly telephone counselling call from the PDs three times (ie, 3, 5 and 7 months after enrolment). It aimed to confirm women’s dual-method contraceptive use and challenges, provide reminders regarding the risk of unintended pregnancies and HIV/STIs and strengthen their capacity to communicate with their partners. In addition, the call included brief health education messages on family planning and HIV/STIs based on an existing tool.25 Each PD provided the same women with counselling each time to build rapport and ensure effective counselling. Each counselling lasted for 15–30 min.
Women in the control group received family planning counselling, including dual-method contraceptive use, from female research assistants for 10–20 min, using the existing tool on the day of enrolment.25 However, this group of women did not receive the handout. Furthermore, the research assistants provided bimonthly health education three times (ie, 3, 5 and 7 months after enrolment) by phone. The topics were the same as those for the intervention group. Each call lasted for about 10 min.
Condoms were provided for free, regardless of the allocation at the selected health facilities. Before providing the intervention, the research assistants received a 2-day training on the contents of the existing counselling tool. In addition, the four PDs received a 1-day training on counselling and ethics, including the confidentiality of their clients. The PDs joined the intervention as volunteers but received 30 000 Ugandan shillings (UGX) (equivalent to US$9) per day when they engaged in the workshop and the counselling to compensate for their time and transportation.
Outcomes
The primary outcome was dual-method contraceptive use, which was defined as the application of a male or female condom along with a non-barrier modern contraceptive method.5 Dual-method contraceptive use at the last sexual intercourse and its consistent use in the last 2 months before each follow-up were measured. The former is easier for women to answer accurately than the latter, which requires to estimate the frequency of condom use in the past.26 Nevertheless, consistent dual-method contraceptive use is critical, given that condoms are often used inconsistently.26
Three questions regarding non-barrier modern contraceptive use, condom use at the last sexual intercourse and its frequency in the past 2 months were combined to measure the primary outcome. The following question was posed for non-barrier modern contraceptive use: ‘Apart from condoms, have you been using any other forms of protection against pregnancy during the past two months?’ Condom use at the last sexual intercourse was determined by asking, ‘Did you use a male or female condom the last time you had sexual relations with your husband or live-in sexual partner?’ Women who answered ‘yes’ to both questions were considered to be practising dual-method contraceptive use at the last sexual intercourse. The frequency of condom use was asked with an item: ‘How often did you and your partner use a male or female condom during the past two months?’ Women answered this question using a 4-point scale: ‘every time’, ‘almost every time’, ‘sometimes’ and ‘never’. Women using a non-barrier modern contraceptive and a condom every time were considered practising consistent dual-method contraceptive use.
Other information
The following information was collected at baseline: age, education, religion, employment, wealth index based on the availability of 18 household assets, number of children, respondent’s and partner’s pregnancy intention, history of unintended pregnancy, multiple sex partnership, type of non-barrier modern contraceptives in use, respondent’s and partner’s HIV status, risk perception of HIV/STIs, HIV-related knowledge (the Brief HIV Knowledge Questionnaire: HIV-KQ-18),27 condom use self-efficacy28 and sexual relationship control power (the Sexual Relationship Power Scale).29
Data collection
All research assistants received a 2-day training on data collection and ethics before the baseline data collection. After enrolment, the research assistants interviewed women to identify their baseline characteristics using a pretested structured questionnaire. Each interview lasted approximately 30–45 min.
For outcome assessment, three female research assistants carried out follow-up phone calls bimonthly for 8 months to assess the influence of the intervention on the primary and secondary outcomes (ie, 2, 4, 6 and 8 months after enrolment). The participants received a text message reminding them to answer the next call or call back if they missed the first call. The assistants called each participant up to five times during each follow-up until they answered. The participants received incentives worth UGX20 000 (equivalent to US$6) for their time after the baseline interview.
Data analysis
Χ2 tests and independent sample t-tests were performed to compare the general characteristics between the intervention and control groups at baseline and follow-up. Mixed-effects logistic regression analysis was performed to assess the effects of the intervention on the primary and secondary outcomes. Unadjusted ORs were first estimated by comparing between the control and intervention groups (model 1). Then, in the main model (model 2), the intervention effects were presented with adjusted ORs (AORs) for the interaction term (group×time) after controlling for cluster effects for all health facilities and the individuals and baseline sociodemographic characteristics. The AORs can be interpreted as the difference between the intervention and control groups in the outcome measures between baseline and each follow-up point.
For sensitivity analyses, attrition rates and reasons for dropout were compared between the intervention and control groups using Pearson’s χ2 test. Moreover, differences in baseline characteristics were compared between women lost to follow-up and those who were reached. Analyses were conducted based on the intention-to-treat principle. Significance level was set at 5%. Data were entered using EpiData V.3, and the data processing and statistical analyses were performed using Stata V.14.
Ethics
Participation in this study was voluntary, and the participants provided written informed consent. The protocol was registered at UMIN-CTR clinical trial. The Consolidated Standards of Reporting Trials checklist is available as online supplemental table S1.
bmjopen-2020-046536supp001.pdf (382.3KB, pdf)
Patient and public involvement
The nine PDs were identified from the public, and four of them were involved in the design and conduct of the intervention as peer counsellors. Moreover, the female research assistants were recruited from the study area and contributed to the intervention’s development and implementation. The findings of this study have been shared with them and Mbarara District health authority.
Results
Participant flow
Out of 1956 women screened, 960 were eligible for the trial and allocated to the intervention or control group (figure 1). Of 480 women in the intervention group, 345 (71.9%) attended the 1-day workshop. Moreover, 385 (80.2%), 361 (75.2%) and 369 (76.9%) received counselling at 3, 5 and 7 months after enrolment, respectively.
Figure 1.
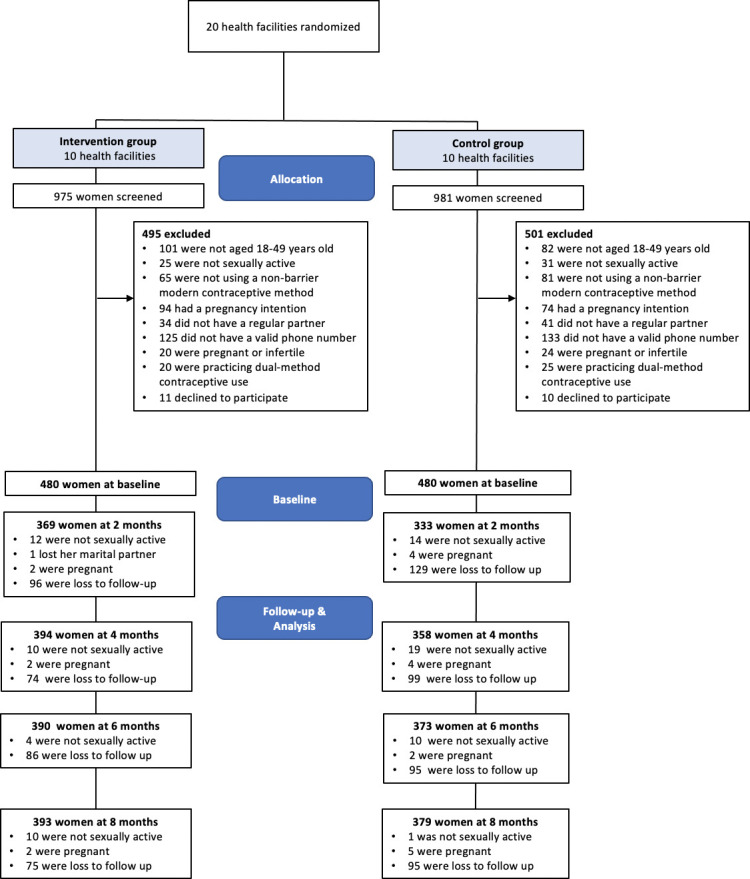
Flow of participants through the study.
The response rates to follow-up surveys ranged from 76.5% at 2 months to 82.3% at 8 months. Women in the intervention group were more likely to respond at 2 months (79.8% vs 73.1%, p=0.015) and 4 months (84.6% vs 79.4%, p=0.036). Most of the baseline characteristics, however, were balanced between women lost to follow-up and those reached in both intervention and control groups. Therefore, the risk of bias was estimated to be low. No statistically significant differences were observed in the response rates between the two groups at 6 and 8 months. Online supplemental table S2 presents the results of the sensitivity analysis.
Participant characteristics
Table 2 presents the sociodemographic characteristics of 960 women at baseline. The mean age was 30.1 (SD 6.7) years. The mean number of children was 3 (SD 1.8). Of 960 women, more than 70% completed primary education. Of all, 9% were HIV positive, 7.6% had an HIV-positive partner and 84.5% perceived a certain level of risk for HIV/STIs. Injectables were the most common family planning method, used by more than half of women (51.9%), followed by implants (31.6%). Characteristics were similar for the intervention and control groups with a few slight imbalances. Specifically, women in the control group were more likely to have primary or higher education (69.8% vs 75.6%; p=0.042), be categorised into the rich quintile (28.3% vs 37.7%; p=0.008) and have fewer children (mean: 3.2 vs 2.9; p=0.041) and less HIV-related knowledge (mean: 11.9 vs 11.3; p<0.001).
Table 2.
Characteristics of women at baseline by intervention group (n=960)
| Variables | Intervention (n=480) | Control (n=480) | Total (n=960) | P value* | |||
| n | % | n | % | n | % | ||
| 1. Sociodemographic characteristics | |||||||
| Age in years, mean (SD) | 30.4 | (6.5) | 29.8 | (6.8) | 30.1 | (6.7) | 0.126 |
| Education | |||||||
| Never | 145 | 30.2 | 117 | 24.4 | 262 | 27.3 | 0.042 |
| Primary and more | 335 | 69.8 | 363 | 75.6 | 698 | 72.7 | |
| Religion | |||||||
| Christian | 450 | 93.8 | 436 | 90.8 | 886 | 92.3 | 0.090 |
| Muslim | 30 | 6.3 | 44 | 9.2 | 74 | 7.7 | |
| Wealth index | |||||||
| Poor | 176 | 36.7 | 158 | 32.9 | 334 | 34.8 | 0.008 |
| Middle | 168 | 35.0 | 141 | 29.4 | 309 | 32.2 | |
| Rich | 136 | 28.3 | 181 | 37.7 | 317 | 33.0 | |
| Number of children, mean (SD) | 3.2 | (1.7) | 2.9 | (1.8) | 3.0 | (1.8) | 0.041 |
| Pregnancy intention | |||||||
| No | 100 | 20.8 | 96 | 20.0 | 196 | 20.4 | 0.822 |
| Yes | 342 | 71.3 | 341 | 71.0 | 683 | 71.2 | |
| Don’t know | 38 | 7.9 | 43 | 9.0 | 81 | 8.4 | |
| Partner’s pregnancy intention | |||||||
| No | 69 | 14.4 | 68 | 14.2 | 137 | 14.3 | 0.776 |
| Yes | 322 | 67.1 | 331 | 69.0 | 653 | 68.0 | |
| Don’t know | 89 | 18.5 | 81 | 16.9 | 170 | 17.7 | |
| History of unintended pregnancy | |||||||
| No | 313 | 65.2 | 335 | 69.8 | 648 | 67.5 | 0.130 |
| Yes | 167 | 34.8 | 145 | 30.2 | 312 | 32.5 | |
| Multiple sex partners | |||||||
| No | 452 | 94.2 | 456 | 95.0 | 908 | 94.6 | 0.568 |
| Yes | 28 | 5.8 | 24 | 5.0 | 52 | 5.4 | |
| 2. HIV-related characteristics | |||||||
| HIV status | |||||||
| Negative | 438 | 91.3 | 436 | 90.8 | 874 | 91.0 | 0.821 |
| Positive | 42 | 8.8 | 44 | 9.2 | 86 | 9.0 | |
| Partner’s HIV status | |||||||
| Negative | 386 | 80.4 | 373 | 77.7 | 759 | 79.1 | 0.587 |
| Positive | 34 | 7.1 | 39 | 8.1 | 73 | 7.6 | |
| Don’t know | 60 | 12.5 | 68 | 14.2 | 128 | 13.3 | |
| Disclosure of HIV status | |||||||
| No | 21 | 4.4 | 19 | 4.0 | 40 | 4.2 | 0.747 |
| Yes | 459 | 95.6 | 461 | 96.0 | 920 | 95.8 | |
| HIV/STI risk perception | |||||||
| No risk at all | 62 | 12.9 | 87 | 18.1 | 149 | 15.5 | 0.124 |
| Small | 177 | 36.9 | 178 | 37.1 | 355 | 37.0 | |
| Moderate | 136 | 28.3 | 124 | 25.8 | 260 | 27.1 | |
| Great | 105 | 21.9 | 91 | 19.0 | 196 | 20.4 | |
| 3. Non-barrier modern contraceptive use | |||||||
| Methods in use | |||||||
| Injectables | 252 | 52.5 | 246 | 51.3 | 498 | 51.9 | 0.599 |
| Implants | 155 | 32.3 | 148 | 30.8 | 303 | 31.6 | |
| IUDs | 43 | 9.0 | 54 | 11.3 | 97 | 10.1 | |
| Contraceptive pill/oral contraceptives | 27 | 5.6 | 31 | 6.5 | 9 | 6.0 | |
| Female sterilisation | 3 | 0.6 | 1 | 0.2 | 4 | 0.4 | |
| Partner’s recognition of contraceptive use | |||||||
| No | 36 | 7.5 | 43 | 9.0 | 79 | 8.2 | 0.411 |
| Yes | 444 | 92.5 | 437 | 91.0 | 881 | 91.8 | |
| Partner’s attitude about contraceptive use | |||||||
| Positive | 432 | 90.0 | 439 | 91.7 | 871 | 90.8 | 0.229 |
| Negative | 36 | 7.5 | 35 | 7.3 | 71 | 7.4 | |
| Don’t know | 12 | 2.5 | 5 | 1.0 | 17 | 1.8 | |
| 4. Other psychosocial characteristics | |||||||
| HIV-related knowledge (HIV-KQ-18), mean (SD) | 11.9 | (2.6) | 11.3 | (3.0) | 11.6 | (2.8) | <0.001 |
| Condom Use Self-Efficacy Scale, mean (SD) | 22.3 | (9.3) | 22.1 | (8.3) | 22.2 | (8.8) | 0.682 |
| Sexual Relationship Power Scale | |||||||
| Low | 173 | 36.0 | 152 | 31.7 | 325 | 33.9 | 0.352 |
| Medium | 168 | 35.0 | 182 | 37.9 | 350 | 36.5 | |
| High | 139 | 29.0 | 146 | 30.4 | 285 | 29.7 | |
P values less than 0.05 are highlighted in a bold font.
*Based on χ2 test for other categorical variables and t-test for continuous variables.
HIV-KQ-18, The Brief HIV Knowledge Questionnaire; IUD, intrauterine device; STI, sexually transmitted infection.
Effect of the intervention
Table 3 demonstrates the outcome data by intervention group and time. More women in the intervention than in the control group used dual-method contraception at the last sexual intercourse and consistently at each follow-up point. These differences were largest at 2 months (dual-method contraceptive use at last sexual intercourse: 42.6% vs 13.8%; p<0.001; consistent dual-method contraceptive use: 15.5% vs 1.5%; p<0.001). The proportion of women practising dual-method contraception in both timeframes gradually decreased over time. At 8 months, more women reported dual-method contraception use in the intervention group compared with the control group (dual-method contraceptive use at last sexual intercourse: 20.9% vs 8.7%; p<0.001; consistent dual-method contraceptive use: 11.2% vs 1.3%; p<0.001).
Table 3.
Dual-method contraceptive use by intervention group and time*
| Outcomes | Intervention | Control | Total | P value† | |||
| n | % | n | % | n | % | ||
| Dual-method contraceptive use at last sexual intercourse | |||||||
| Baseline | 41 | 8.5 | 28 | 5.8 | 69 | 7.2 | 0.104 |
| Month 2 | 157 | 42.6 | 46 | 13.8 | 203 | 28.9 | <0.001 |
| Month 4 | 110 | 27.9 | 55 | 15.4 | 165 | 21.9 | <0.001 |
| Month 6 | 91 | 23.3 | 40 | 10.7 | 131 | 17.2 | <0.001 |
| Month 8 | 82 | 20.9 | 33 | 8.7 | 115 | 14.9 | <0.001 |
| Consistent dual-method contraceptive use | |||||||
| Baseline | – | – | – | – | – | – | – |
| Month 2 | 57 | 15.5 | 5 | 1.5 | 62 | 8.8 | <0.001 |
| Month 4 | 42 | 10.7 | 8 | 2.2 | 50 | 6.7 | <0.001 |
| Month 6 | 32 | 8.2 | 5 | 1.3 | 37 | 4.9 | <0.001 |
| Month 8 | 44 | 11.2 | 5 | 1.3 | 49 | 6.4 | <0.001 |
P values less than 0.05 are highlighted in a bold font.
*Refer to figure 1 for ‘n’ at baseline and follow-up for each group.
†Based on χ2 test.
Table 4 illustrates the effects of the intervention on the primary outcome among women at 2, 4, 6 and 8 months after enrolment. In the main model (model 2), more women in the intervention group reported dual-method contraceptive use at the last sexual intercourse than in the control group at 2 months (AOR=4.12; 95% CI 2.02 to 8.39, p<0.001). The intervention group also reported more dual-method contraceptive use at the last sexual intercourse at 4, 6 and 8 months, although the difference was statistically significant only at 8 months (AOR=2.16; 95% CI 1.06 to 4.41, p=0.034). Moreover, more women in the intervention group practised consistent dual-method contraceptive use than in the control group at 2 months (AOR=14.53; 95% CI 3.63 to 58.13, p<0.001). The intervention effect remained statistically significant at 4, 6 and 8 months.
Table 4.
Effects of intervention on primary outcome among women at 2, 4, 6 and 8 months after enrolment
| Variables | Month 2 | Month 4 | Month 6 | Month 8 | ||||
| Model 1 OR (95% CI) |
Model 2 AOR† (95% CI) |
Model 1 OR (95% CI) |
Model 2 AOR† (95% CI) |
Model 1 OR (95% CI) |
Model 2 AOR† (95% CI) |
Model 1 OR (95% CI) |
Model 2 AOR† (95% CI) |
|
| Dual-method contraceptive use at last sexual intercourse | 4.62*** (3.18 to 6.71) |
4.12*** (2.02 to 8.39) |
2.13*** (1.49 to 3.06) |
1.66 (0.84 to 3.30) |
2.53*** (1.69 to 3.79) |
2.03 (0.99 to 4.14) |
2.76*** (1.79 to 4.26) |
2.16* (1.06 to 4.41) |
| Consistent dual-method contraceptive use | 11.98*** (4.74 to 30.29) |
14.53*** (3.63 to 58.13) |
5.22*** (2.42 to 11.28) |
6.30** (2.20 to 18.03) |
6.58*** (2.53 to 17.07) |
8.04* (1.17 to 55.08) |
9.43*** (3.70 to 24.06) |
10.72** (2.03 to 56.64) |
Table reports effect estimates using OR and adjusted OR (AOR) from multiple logistic regression using the control group as the reference category.
***P<0.001; **p<0.01; *p<0.05.
†Adjusted for cluster effect, individuals, age, education, religion, wealth index, number of children, pregnancy intention, partner’s pregnancy intention, history of unintended pregnancy, multiple sex partnership, non-barrier modern contraceptive methods, HIV status, partner’s HIV status, HIV/STI risk perception, HIV-related knowledge, condom use self-efficacy and sexual relationship control power.
STI, sexually transmitted infection.
The baseline characteristics positively associated with dual-method contraceptive use at the last sexual intercourse include self-efficacy for condom use and multiple sexual partnership. The dual-method use was negatively associated with partner’s pregnancy intention and history of unintended pregnancy. HIV/STI risk perception was associated with its consistent use at 2 months. The complete results are provided in online supplemental tables S3–S10.
Discussion
The positive deviance intervention was effective in promoting the uptake and continued use of dual-method contraception among women in long-term relationships who used non-barrier modern contraceptives. The study observed the largest difference in the dual-method use between the intervention and control groups at the 2-month assessment, which was the closest time point to the baseline counselling and workshop. The number of women using dual-method contraception decreased in the intervention and control groups over time, as observed in previous studies.12 However, the significant difference between the groups remained during the follow-up period.
The observed effect was consistent with a previous intervention study that combined case management and peer education programme for adolescent girls in the USA.13 The intervention illustrated continued effects on the dual-method use at 12 and 24 months after enrolment.13 The peer leadership programme aimed to foster prosocial interaction skills and supportive peer relationships among teenagers.13 The peer supporters were not PDs and provided with intensive standard training.13 Effective communication with partners on sexual health was one of the key topics covered in the sessions.13 Similar to this, the current intervention provided bimonthly counselling tailored to the participants’ individual needs. However, it was provided by the PDs who had overcome barriers to dual-method contraceptive use. Counselling by PDs may be an alternative strategy because it ensures adequate attention to the diverse issues confronting women and prosocial peer influence on their behaviours.
Few intervention studies have demonstrated an increase in dual-method contraceptive use,12–14 and adherence to such practice was frequently low.12 Condom use is often considered a male responsibility and unacceptable in long-term relationships in SSA, especially when women use another contraceptive method.7 9 11 30 The positive deviance intervention can be effective in changing such norms. The PDs who overcame the barriers to dual-method contraceptive use shared their experiences to help other women realise that condom use is normal even among marital or in-union relationships.
Moreover, one of strong predictors of dual-method contraceptive use was self-efficacy for condom use in this study. Self-efficacy for condom use was associated with actual dual-method contraceptive use at the last sexual intercourse throughout the follow-up period. Similar association between self-efficacy and actual condom use was observed among Rwandan adolescents.31 Therefore, it is crucial to increase women’s perceived capability of using condoms skilfully and negotiating their use with partners. The positive deviance intervention could empower women with the skills necessary to play a proactive role in negotiation and condom use with their partners.
Condom use is not an individual action; therefore, a couple-level intervention would be ideal to promote the dual-method use.12 However, reaching out to male partners may be more difficult compared with providing education to women visiting family planning clinics. This study demonstrated that the intervention targeting only women is effective at changing behaviours of couples to practise dual-method contraception. The finding supports the results of a qualitative study of couples using condoms in Uganda; women were more likely to initiate discussion and persuade their male partners to use condoms.32 Considering that women who use modern contraceptives visit health facilities presumably more often than men do, educating them on dual-method contraception can be an effective strategy.
Despite the increase in dual-method contraceptive use, it was practised inconsistently, especially among women in the control group. The result is consistent with findings of other intervention studies in the USA and South Africa.12 14 For instance, 32% of women at high risk for unintended pregnancies and STIs initiated dual-method contraception after receiving an individualised computer-based intervention, but only 9% reported its consistent use.12 The inconsistent use may explain the limited effects of dual-method contraception on preventing STIs and unintended pregnancies in the former intervention studies in the USA.12 33 However, unintended pregnancy and STI incidences were significantly lower among HIV-infected women practising dual-method contraception compared with non-users in Nigeria.34 The dual-method use can be effective at reducing such risks if being practised consistently. Although this study did not measure HIV/STI incidence as an outcome, it is expected that the risk was reduced among women who reported consistent dual-method contraceptive use.
The study has several limitations. First, the study measured outcomes based on self-reports from the participants. Therefore, it is subject to measurement errors. Especially, given the information provided, dual-method contraceptive use could have been over-reported, which can lead to overestimating the intervention effect. Nevertheless, over-reporting of outcomes was minimised by assuring the participants of the confidentiality of their responses and conducting interviews by experienced female research assistants. Second, we did not measure HIV/STI incidence as an outcome. It is recommended to measure biological outcomes with behavioural outcomes to evaluate dual-method contraceptive interventions in future research. Lastly, this intervention was developed based on the qualitative study of the PDs in Mbarara District and examined its effectiveness among women in the same area. Merely applying the intervention to other communities might not be effective, as communities’ local solutions might differ.35 Therefore, each community must participate in the process of determining its own solutions. Further research is recommended to assess the effectiveness of the positive deviance approach in a given context with careful attention to its process.
Conclusions
The positive deviance intervention increased dual-method contraceptive use among married or in-union women in Mbarara District, Uganda, by disseminating solutions that exist in the community. This approach could be a potential option to reduce the dual risk of unintended pregnancies and HIV/STIs among women. This study demonstrated that the intervention targeting only women can change behaviours of couples to practise dual-method contraceptive use. Because women using non-barrier modern contraceptives may be more reachable than men, interventions targeting such women should be recommended.
Supplementary Material
Acknowledgments
The authors would like to thank all participants for their time and cooperation and extend their appreciation to the women who joined in the trial as PDs and the research assistants.
Footnotes
Contributors: HK and MJ conceived the study and contributed to funding acquisition. HK, AS, JK, KICO and MJ contributed to the study design. HK conducted the literature review. HK, CM and SM led the development of the data collection instrument, data collection and quality assessment. HK and AS did the statistical analysis. All authors contributed to data interpretation. HK wrote the original draft. AS, JK, KICO, SM, CM and MJ reviewed and revised the manuscript. All authors approved the final version for submission.
Funding: HK received scholarship grant from the Foundation for Advanced Studies on International Development (FASID), Tokyo, Japan.
Disclaimer: The funding source had no role in the design and conduct of this study. SM works at UNICEF Uganda, but the information in this article represents SM’s personal views and opinions and does not necessarily represent UNICEF Uganda’s position.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. The data underlying this study have been uploaded to the Figshare Repository and are accessible at https://doi.org/10.6084/m9.figshare.12936857.v1
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study was approved by the Research Ethics Committee of the Graduate School of Medicine, University of Tokyo (2019085NI), the Institutional Research and Ethics Committee of Mbarara University of Science and Technology (IRB15/06-19) and the Uganda National Council of Science and Technology (HS439ES).
References
- 1.Ameyaw EK, Budu E, Sambah F, et al. Prevalence and determinants of unintended pregnancy in sub-Saharan Africa: a multi-country analysis of demographic and health surveys. PLoS One 2019;14:e0220970. 10.1371/journal.pone.0220970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UNAIDS . UNAIDS data 2019, 2019. Available: https://www.unaids.org/sites/default/files/media_asset/2019-UNAIDS-data_en.pdf [Accessed 21 Mar 2020].
- 3.Kharsany ABM, Karim QA. HIV infection and AIDS in sub-Saharan Africa: current status, challenges and opportunities. Open AIDS J 2016;10:34–48. 10.2174/1874613601610010034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sia D, Onadja Y, Hajizadeh M, et al. What explains gender inequalities in HIV/AIDS prevalence in sub-Saharan Africa? Evidence from the demographic and health surveys. BMC Public Health 2016;16:1136. 10.1186/s12889-016-3783-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lopez LM, Stockton LL, Chen M, et al. Behavioral interventions for improving dual-method contraceptive use. Cochrane Database Syst Rev 2014;3:Cd010915. 10.1002/14651858.CD010915.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mutowo J, Kasu CM. Barriers to use of dual protection among married women in a suburban setting. Nurs Health Sci 2015;4:51–7. [Google Scholar]
- 7.Osuafor GN, Maputle S, Ayiga N, et al. Condom use among married and cohabiting women and its implications for HIV infection in Mahikeng, South Africa. J Popul Res 2018;35:41–65. 10.1007/s12546-017-9195-2 [DOI] [Google Scholar]
- 8.Tsuyuki K, Gipson JD, Urada LA, et al. Dual protection to address the global syndemic of HIV and unintended pregnancy in Brazil. J Fam Plann Reprod Health Care 2016;42:271–9. 10.1136/jfprhc-2015-101175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kosugi H, Shibanuma A, Kiriya J, et al. Consistent condom use among highly effective contraceptive users in an HIV-endemic area in rural Kenya. PLoS One 2019;14:e0216208. 10.1371/journal.pone.0216208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Woodsong C, Koo HP. Two good reasons: women's and men's perspectives on dual contraceptive use. Soc Sci Med 1999;49:567–80. 10.1016/S0277-9536(99)00060-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anglewicz P, Clark S. The effect of marriage and HIV risks on condom use acceptability in rural Malawi. Soc Sci Med 2013;97:29–40. 10.1016/j.socscimed.2013.06.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peipert JF, Zhao Q, Meints L, et al. Adherence to dual-method contraceptive use. Contraception 2011;84:252–8. 10.1016/j.contraception.2011.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sieving RE, McRee A-L, McMorris BJ, et al. Prime time: sexual health outcomes at 24 months for a clinic-linked intervention to prevent pregnancy risk behaviors. JAMA Pediatr 2013;167:333–40. 10.1001/jamapediatrics.2013.1089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Galárraga O, Harries J, Maughan-Brown B, et al. The empower Nudge lottery to increase dual protection use: a proof-of-concept randomised pilot trial in South Africa. Reprod Health Matters 2018;26:67–80. 10.1080/09688080.2018.1510701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ministry of Health, Uganda . Uganda population-based HIV impact assessment (UPHIA) 2016-2017: final report. Kampala: Ministry of Health, 2019. [Google Scholar]
- 16.Bakibinga P, Matanda DJ, Ayiko R, et al. Pregnancy history and current use of contraception among women of reproductive age in Burundi, Kenya, Rwanda, Tanzania and Uganda: analysis of demographic and health survey data. BMJ Open 2016;6:e009991. 10.1136/bmjopen-2015-009991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uganda Bureau of Statistics . Uganda demographic and health survey 2016, 2018. Available: https://dhsprogram.com/pubs/pdf/FR333/FR333.pdf [Accessed 10 Aug 2020].
- 18.Marsh DR, Schroeder DG, Dearden KA, et al. The power of positive deviance. BMJ 2004;329:1177–9. 10.1136/bmj.329.7475.1177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Herington MJ, van de Fliert E. Positive deviance in theory and practice: a conceptual review. Deviant Behav 2018;39:664–78. 10.1080/01639625.2017.1286194 [DOI] [Google Scholar]
- 20.Kosugi H, Shibanuma A, Kiriya J, et al. Positive deviance for dual-method promotion among women in Uganda: a qualitative study. Int J Environ Res Public Health 2020;17:5009. 10.3390/ijerph17145009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kosugi H, Shibanuma A, Kiriya J, et al. Positive deviance for dual-method promotion among women in Uganda: study protocol for a cluster randomized controlled trial. Trials 2020;21:270. 10.1186/s13063-020-4192-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Uganda Bureau of Statistics . The National population and housing census 2014–Main report, 2016. Available: https://unstats.un.org/unsd/demographic/sources/census/wphc/Uganda/UGA-2016-05-23.pdf [Accessed 31 Aug 2020].
- 23.Ministry of Health, Uganda . National health facility master list 2018. Kampala: Ministry of Health, 2089. [Google Scholar]
- 24.Zhang J, Pals SL, Medley A, et al. Parameters for sample size estimation from a group-randomized HIV prevention trial in HIV clinics in sub-Saharan Africa. AIDS Behav 2014;18:2359–65. 10.1007/s10461-013-0631-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.WHO, Johns Hopkins Bloomberg School of Public Health . Center for communication programs. information and knowledge for optimal health (INFO). Decision-making tool for family planning clients and providers, 2005. Available: https://www.who.int/reproductivehealth/publications/family_planning/9241593229/en/ [Accessed 10 Aug 2019].
- 26.Reynolds HW, Luseno WK, Speizer IS. The measurement of condom use in four countries in East and southern Africa. AIDS Behav 2012;16:1044–53. 10.1007/s10461-012-0146-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carey MP, Schroder KEE. Development and psychometric evaluation of the brief HIV knowledge questionnaire. AIDS Educ Prev 2002;14:172–82. 10.1521/aeap.14.2.172.23902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shaweno D, Tekletsadik E. Validation of the condom use self-efficacy scale in Ethiopia. BMC Int Health Hum Rights 2013;13:22. 10.1186/1472-698X-13-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pulerwitz J, Gortmaker SL, DeJong W. Measuring sexual relationship power in HIV/STD research. Sex Roles 2000;42:637–60. 10.1023/A:1007051506972 [DOI] [Google Scholar]
- 30.Chimbiri AM. The condom is an 'intruder' in marriage: evidence from rural Malawi. Soc Sci Med 2007;64:1102–15. 10.1016/j.socscimed.2006.10.012 [DOI] [PubMed] [Google Scholar]
- 31.Babalola S, Awasum D, Quenum-Renaud B. The correlates of safe sex practices among Rwandan youth: a positive deviance approach. Afr J AIDS Res 2002;1:11–21. 10.2989/16085906.2002.9626540 [DOI] [PubMed] [Google Scholar]
- 32.Williamson NE, Liku J, McLoughlin K, et al. A qualitative study of condom use among married couples in Kampala, Uganda. Reprod Health Matters 2006;14:89–98. 10.1016/S0968-8080(06)28268-5 [DOI] [PubMed] [Google Scholar]
- 33.Berenson AB, Rahman M. A randomized controlled study of two educational interventions on adherence with oral contraceptives and condoms. Contraception 2012;86:716–24. 10.1016/j.contraception.2012.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lawani LO, Onyebuchi AK, Iyoke CA. Dual method use for protection of pregnancy and disease prevention among HIV-infected women in South East Nigeria. BMC Womens Health 2014;14:39. 10.1186/1472-6874-14-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pascale R, Monique S, Sternin J. The power of positive deviance: How unlikely innovators solve the world’s toughest problems. 1st edn. Brighton, Massachusetts: Harvard Business Press, 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-046536supp001.pdf (382.3KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. The data underlying this study have been uploaded to the Figshare Repository and are accessible at https://doi.org/10.6084/m9.figshare.12936857.v1


