Abstract
Objective
The treatment effect of orthoses for hallux valgus (HV) is unclear with little interventional studies, the design involves multiple complex factors, and therefore a systematic analysis with meta-analysis is necessary. The objective of this systematic review and meta-analysis is to determine whether current foot orthoses are effective in treating HV.
Design
Systematic review with meta-analysis.
Data sources
Electronic databases (PubMed, Scopus, Cinahl and Medline) are searched up to February 2020.
Eligibility criteria for selecting studies
Interventional studies with content focus on HV orthosis design and any of the outcomes related to effectiveness for treating HV are included. The standardised mean differences are calculated. The risk of bias in included studies is assessed using the Cochrane Collaboration’s risk of bias tools.
Results
In total, 2066 articles are identified. Among them, nine are selected and quality rated, and data are extracted and closely examined. A meta-analysis is conducted, where appropriate. The main causes of potential bias are missing outcome data and outcome measurement error. The results show that orthosis with a toe separator has the best effect of correcting the HV angle (standardised mean difference: 0.50, 95% CI: 0.189 to 0.803).
Conclusion
The orthoses design with a toe separator or an element that allows for the foot anatomic alignment is critical for reducing the HV angle and relieving foot pain. The results contribute to a better selection of treatment for patients.
PROSPERO registration number
CRD42021260403.
Keywords: foot & ankle, adult orthopaedics, bone diseases, health economics, quality in healthcare, anatomy
Strengths and limitations of this study.
This systematic review with meta-analysis represents, to the best of our knowledge, the most comprehensive examination of the evidence for the characteristics and effectiveness of orthosis in the treatment of hallux valgus.
This study searched articles in large databases including Scopus, Medline, PubMed and Cinahl.
The results highlight the key design features of orthosis and their relevance to hallux valgus angle correction and pain relief.
This study provides evidence on the use of hallux valgus orthoses in angle correction and toe realignment.
There is scarcity of studies on this topic and lack of consistency in the study methods.
Introduction
Hallux valgus (HV) is a common foot deformity, estimated to affect 23% of adults and 35.7% of the elderly.1 It is characterised by the hypermobility and pronation of the first metatarsal ray, which eventually lead to subluxation and pain of the first metatarsophalangeal joint.2 The hallux valgus angle (HVA) and intermetatarsal angle (IMA) are common indicators to objectively measure the degree of the deformity.3 4 HV is not only a prevalent and debilitating condition among the general public, especially women, due to hereditary or improper footwear but also a significant burden on public healthcare with the high demand for foot surgery,5 and its association with foot pain,6–9 which can inhibit the level of mobility and physical activity of those who suffer from the deformity.2 This is especially devastating to athletes, who may acquire the condition due to prolonged periods of training. Previous research work has found that 9.3% of the Muay Thai kickboxers in their study suffer from HV.10–12 Schöffl and Küpper12 and Killian et al13 found that tight climbing shoes exert high pressure load on the forefoot which affects 53% of the long-term high-level climbers. Steinberg et al14 found that 40.0% dancers have bilateral HV and 7.3% have unilateral HV. Contributors to the development of HV include the individual body structure, joint range of motion (ROM), anatomical abnormalities and extensive dance exercises that expose the spine and the lower limb joints to high loads and strains.14–16 Former ballet dancers (73.7%) were also found to have a significantly higher HV incidence rate than the control group (2.6%).15
Extreme cases of HV require surgical intervention, but the recurrence rate is high. Surgical operations may reduce the subsequent mobility of the big toe, and the impact on athletes can be devastating.2 Hence, studies have shown that treatment of HV in athletes should be as conservative as possible.10 The complications related to HV surgical correction such as nerve damage also discourage surgery.17–21 Therefore, non-surgical conservative treatments such as the use of foot orthoses have become a viable and popular option for patients with HV to correct their foot deformity and relieve foot pain.17 22 As described by Charrette,23 HV orthoses act as a means of biomechanical support to reduce the pressure on the first metatarsal joint which would prevent further degeneration of mobility.
HV orthoses are available in a wide range of design features and materials. Ready-made and custom-made are the two main types of foot orthoses.24 While the former is available online or in retail stores and made from standard patterns, the latter is constructed by using footprints or foot moulds based on specifications of the clinician.25 They may or may not have a toe separator, can have different lengths and made of different materials. The design of HV orthoses is multifactorial, however, previous related studies have merely focused on the effectiveness of foot orthoses in patients with HV. This article conducts a systematic study to investigate the effectiveness of these orthoses, and quantitatively synthesises the results based on the best available evidence. The results can provide reference for the clinical selection and future design trends of orthotics to achieve better treatment effects.
Methods
Search methods for identification of studies
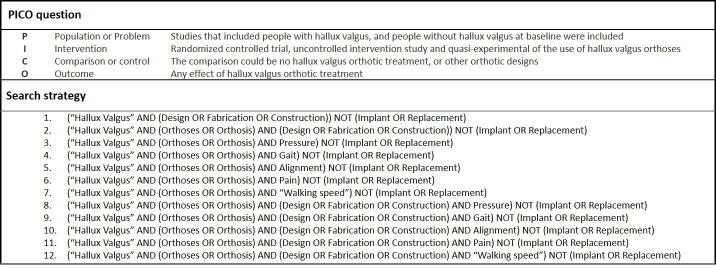
Research articles published in peer-reviewed journals that describe the construction of HV orthoses and/or their effectiveness were searched on PubMed, Scopus, Cinahl and Medline for all years available up to February 2020. The PICO questions designed on the basis of the study selection criteria and a highly sensitive search strategy are reported in figure 1. The keywords include ‘hallux valgus’, ‘orthosis’, ‘design’, ‘fabrication’, ‘construction’, ‘pressure’, ‘gait’, ‘alignment’, ‘pain’ and ‘walking speed’.
Figure 1.
PICO question and a list of search strategy.
Inclusion and exclusion criteria
The titles and abstracts were then reviewed by two investigators. Full-text articles that assess HV orthosis designs or any of the outcomes related to the effectiveness of HV orthoses were then retrieved for detailed evaluation. The retrieved items were screened based on a two-stage selection process which subsequently considered the titles, abstracts and full text. Assessment of the study eligibility was performed by one investigator.
Quality assessment and risk of bias
The included papers were assessed for methodological quality. The title, journal name and author details were removed to anonymise the articles prior to the rating process. Quality rating was performed by using the epidemiological appraisal instrument (EAI),26–29 which has been validated for the assessment of observational studies. Thirty-one items from the original EAI were used, after removing those that are related to interventions, randomisation, the follow-up period or loss to follow-up that are not applicable to cross-sectional studies. Items were scored as ‘No’ or ‘Unable to determine’ (score=0), ‘Partial’ (score=1), ‘Yes’ (score=2) or ‘Not Applicable’ (item removed from scoring process) and an average score across all items was calculated for each study. Risk of bias was assessed with the use of Cochrane Collaboration tools.
Data management
One investigator recorded the following details for all of the included papers: publication details (author, year, country and study aim), sample characteristics (number of HV cases, number of control subjects, age and sex), study methodology (device, associated factors investigated and orthosis wearing details) and result. The standardised mean differences (SMDs) and 95% CIs were calculated. To calculate the SMDs, the means and SDs of preintervention and postintervention were used.30 The mean difference was divided by the pooled SD.31 The SMDs are calculated with the following formulas:
The interpretation of the SMDs was based on guidelines in previous studies: small effect ≥0.2, medium effect ≥0.5 and large effect ≥0.8.29 32 33 An SMD of ‘0’ means that there is no difference in effect between the groups. SMDs that are ‘>0’ or ‘<0’ indicate that one group is more efficacious than the other, and vice versa. SMDs are usually accompanied by 95% CIs to evaluate the reliability of the comparison.29 32 34
The total variation observed across studies that is due to heterogeneity is denoted as I2. A heterogeneity value of 0%–40% is considered ‘low heterogeneity’; 30%–60% is ‘moderate heterogeneity’; 50%–90% is ‘substantial heterogeneity’; and 75%–100% is ‘considerable heterogeneity’.
Patient and public involvement
Patients and/or the public will not be involved in this study.
Results
Search results
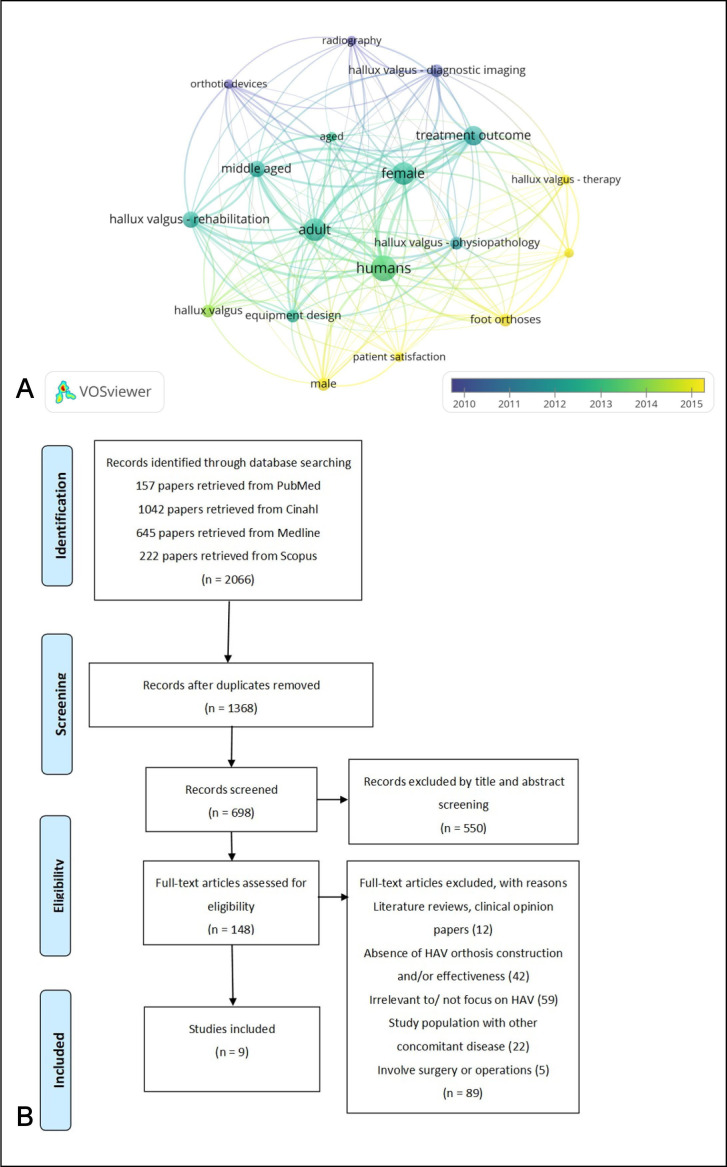
This review adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement and has a registered protocol. The search strategy resulted in 2066 articles from PubMed, Scopus, Cinahl and Medline databases, with 1368 articles removed due to duplications. Then, the title and abstract of 698 articles were screened against the objective of the study, which resulted in the removal of 550 papers as they did not meet the requirements of the study design. The remaining 148 articles were assessed against the inclusion and exclusion criteria by examining the full text and were imported into the VOSviewer (V.1.6.13) to examine the trend of the results. Keywords with fewer than three occurrences were excluded, and general terms were filtered out so that the focus would be on more specific and informative terms.35 Figure 2A visualises the results that among the 148 remaining articles, 18 keywords meet the threshold. The total link strength ranged from 26 to 71, with larger label denoting a higher total link strength. On average, the publication years of the articles ranged from 2010 to 2015, in which ‘male’, ‘patient satisfaction’, ‘foot orthoses’ and ‘hallux valgus-therapy’ are the latest research terms. After the assessment, another 89 articles were removed. The remaining nine studies are discussed in this systematic review. Figure 2B presents a PRISMA flow chart of the article selection process.
Figure 2.
(A) Visualisation of main keywords from 148 papers and (B) flowchart of study selection procedure. HAV, hallux valgus angle.
Study characteristics
The nine studies selected for inclusion in this paper focused on various characteristics and included different demographics (table 1). Of the nine studies included, seven were randomised controlled trials,36–42 and the others were uncontrolled intervention study42 and quasi-experimental,22 respectively. The age of participants ranged from 22.79±1.44 to 60.8±10.8 years old. The publication years of these papers range from 2002 to 2020. The studies evaluated the effects of 11 different types of HV orthoses on angle correction (IMA and HVA), plantar pressure, ROM, pain (Visual Analogue Scale (VAS) and Foot and Ankle Outcome Score (FAOS)), function during daily activities (the American Orthopedic Foot and Ankle Score (AOFAS) and FAOS) and quality of life (FAOS). The number of subjects who suffer from HV ranged from 16 to 69, with mild to moderate HV. Four of the studies involved control groups with 23 to 69 participants. Overall, the majority of the subjects are female.
Table 1.
Selected characteristics of studies included in analysis (nine unique studies)
| Authors(s)/country | Reference no. | Study aim | Method/device | Number of patients with HV |
Age (mean±SD) | Orthosis | Orthosis material/wearing duration | Result |
| Chadchavalpa nichaya et al 2018/Thailand | 36 | To investigate the effect of custom-moulded RTV silicone toe separator to reduce HVA. | Randomised controlled trial/ radiographic measurement and clinical assessment | 45 | HV group: 60.3±9.4 Control group: 60.8±10.8 | Custom-moulded RTV toe separator | Silicone/12 months | Both groups have significant differences in mean HVA with a decrease of 3.3°±2.4° for the study group and increase of 1.9°±1.9° for the control group. Hallux pain of study group is reduced. |
| Doty et al 2015/USA | 37 | To compare the plantar pressure distribution in standard footwear and in the same footwear with orthoses of three different lengths. | Randomised controlled trial/Tactilus Free Form Sensor System | 25 | Mean: 57 | Full-length orthosis | Not Reported/immediate | No significant changes in medial pressure with the addition of any orthosis compared with standard footwear alone. |
| Sulcus-length orthosis | ||||||||
| 3/4-length orthosis | ||||||||
| Farzadi et al 2015/Iran | 22 | To investigate the effect of orthosis with medial arch support on plantar pressure distribution. | Quasi-experimental/Pedar-X in-shoe system | 16 | 26.1±5.7 | Prefabricated arch support foot orthosis | 5 mm thick polypropylene/1 month | The use of the foot orthosis leads to a decrease in peak pressure and maximum force. |
| Moulodi et al 2019/Iran | 38 | To compare the HVA, ROM, FAOS, pain and function in daily activities after the use of orthosis. | Randomised controlled trial/clinical assessment | 24 | 22.79±1.44 | Static orthosis with toe separator | A bar and a single strap/1 month | Both orthoses can reduce HVA up to 3°; significant difference in ROM by using dynamic orthosis. |
| Dynamic orthosis | Firm plastic, straps & a free joint/ 1 month | |||||||
| Plaass et al 2020/Germany | 39 | To analyse the effect of a dynamic orthosis on IMA and HVA. | Randomised controlled trial/radiographic measurement and clinical assessment | 36 | HV group: 53.2±14.0 Control group: 48.5±12.9 |
Dynamic orthosis | Not Reported/3 months | Dynamic orthosis can provide pain relief in patients but showed no effect on HVA. |
| Reina et al 2013/ Spain | 40 | To determine if the use of custom-made foot orthotics prevents the advancement of IMA and HVA. | Randomised controlled trial/radiographic measurement | 23 | HV group: 30.31±9.27 Control group: 30.94±14.06 |
Custom-made foot orthoses | 3 mm thick polypropylene sheet and 3 mm thick polyethylene foam sheet/12 months | Custom-made orthoses appear to have no effect. |
| Tang et al 2002/Taiwan | 43 | To assess the effects of a new foot–toe orthosis on HVA. | Uncontrolled intervention study/radiographic measurement and clinical assessment | 17 | 42.59±16.52 | Total contact orthosis with toe separator | Plastazote poron, microcell pull, plastazote and mineral oil-based polymer gel toe separator/3 months | The new total contact orthosis with fixed toe separator reduces HVA. |
| Tehraninasr et al 2008/Iran | 41 | To compare the effects of wearing an orthosis with toe separator and night-time orthosis on IMA, HVA and foot pain. | Randomised controlled trial/radiographic measurement | 30 | 27±8.91 | Orthosis with toe separator | Polyfoam, polyethylene, plastazote toe separator/3 months | IMA and HVA are reduced in both groups; however, the reduction is not significant; the orthosis with toe separator significantly reduces the pain intensity. |
| Nighttime orthosis | Polyfoam and a rigid polyethylene bar/3 months | |||||||
| Torkki et al 2003/Finland | 42 | To compare the effectiveness of surgical and orthotic treatment with patients on VAS. | Randomised controlled trial/Not Reported | 69 | HV group: 49±10 Control group: 47±9 |
Not Reported | Not Reported/12 months | Orthoses provide short-term symptomatic relief. |
FAOS, Foot and Ankle Outcome Score; HV, hallux valgus; HVA, hallux valgus angle; IMA, intermetatarsal angle; ROM, range of motion; RTV, room temperature vulcanising; VAS, Visual Analogue Scale.
Quality assessment and risk of bias
The inter-rater agreement on the EAI is 95% (14 disagreements out of 279 quality assessment items rated) across all included studies (nine papers). The individual study results for quality appraisal are shown in table 2. All of the studies defined the associated factors investigated and reported the sampling frame and statistical methods (9/9, 100%). Most studies clearly reported their aims and study design (8/9, 89%). More than half of the studies reported the inclusion criteria, sample characteristics, sample size calculations and statistical parameters (7/9, 78%; 6/9, 67%; 7/9, 78%; and 7/9, 78%, respectively). Few studies reported an attempt to blind the assessors towards the group allocation (1/4, 25%), although given the nature of HV deformities, blinding assessors is unlikely to be possible in most studies.
Table 2.
Results of quality assessment of all included papers (nine unique studies)
| Author(s) | Chadchavalpanichaya et al 2018 | Doty et al 2015 | Farzadi et al 2015 | Moulodi et al 2019 | Plaass et al 2020 | Reina et al 2013 | Tang et al 2002 | Tehraninasr et al 2008 | Torkki et al 2003 | Studies scoring ‘yes’ (%) |
| Reference no. | 36 | 37 | 22 | 38 | 39 | 40 | 43 | 41 | 42 | |
| Q1. Reported study aim/objective clearly | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 89 |
| Q2. Associated factors clearly defined | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 100 |
| Q3. HV clearly defined | 1 | 2 | 1 | 0 | 0 | 0 | 0 | 2 | 0 | 22 |
| Q4. Reported study design | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 89 |
| Q5. Reported sampling frame | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 100 |
| Q6. Reported inclusion criteria | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 78 |
| Q7. Reported participation rate | 2 | 0 | 0 | 2 | 1 | 2 | 1 | 0 | 2 | 44 |
| Q8. Reported sample characteristics | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 2 | 67 |
| Q9. Reported statistical methods | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 100 |
| Q10. Reported all basic data | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 11 |
| Q11. Reported variability in data | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 78 |
| Q12. Reported statistical parameters | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 78 |
| Q13. Sample size calculations | 2 | 1 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 78 |
| Q14. Comparability of case/control groups | 2 | – | – | – | 2 | 2 | – | – | 2 | 100 |
| Q15. Adequate participation rate | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 100 |
| Q16. Recruitment period for case/control groups | 2 | – | – | – | 2 | 2 | – | – | 0 | 75 |
| Q17. Non-responder characteristics described | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Q18. Reliability of all associated factors | 2 | 0 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 22 |
| Q19. Validity of all associated factors | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 11 |
| Q20. Standardised assessment of associated factors | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 100 |
| Q21. Blinding of assessors | 2 | – | – | – | 1 | 0 | – | – | 0 | 25 |
| Q22. Reliability of HV assessment | 2 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 22 |
| Q23. Validity of HV assessment | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 11 |
| Q24. Standardised assessment of HV | 2 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 56 |
| Q25. Assessment period for case/control groups | 2 | – | – | – | 2 | 2 | – | – | 2 | 100 |
| Q26. Collected data on HV severity/symptoms | 2 | 0 | 0 | 0 | 2 | 1 | 1 | 1 | 1 | 22 |
| Q27. Adjusted for covariates | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Q28. Reported data for ≥3 levels of associated factors | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 |
| Q29. Reported data for subgroups of subjects | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Q30. Generalisability of results to study population | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Q31. Generalisability of results to other populations | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 2 | 2 | 44 |
| Overall quality score | 1.45 | 0.89 | 0.93 | 1.22 | 1.23 | 1.13 | 0.96 | 1.07 | 1.06 |
Entries in italics indicate ‘Yes’, bold indicates ‘Partial’, bold italic indicates ‘No’ or ‘unable to determine’, ‘–’ indicates ‘not applicable’; that is, items removed from scoring process and not included in % calculations.
HV, hallux valgus.
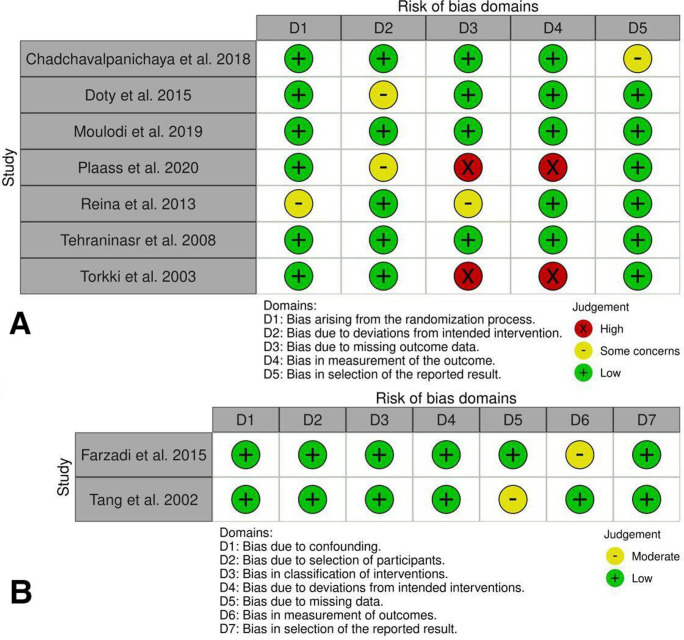
Reliability and validity were considered separately for both the HV assessment and measurement of the associated factors. Only a couple of the studies (2/9; 22%) provided a clear definition of HV by reporting angle values, another couple of studies (2/9; 22%) reported the reliability for the HV angle assessment, and only 11% (1/9) reported the validity of the HV assessment. The risk of bias of the included studies is summarised in figure 3. The main causes of potential bias were missing outcome data and outcome measurement error.
Figure 3.
Risk of bias in included studies. (A) Risk of bias for randomised studies. (B) Risk of bias for non-randomised studies.
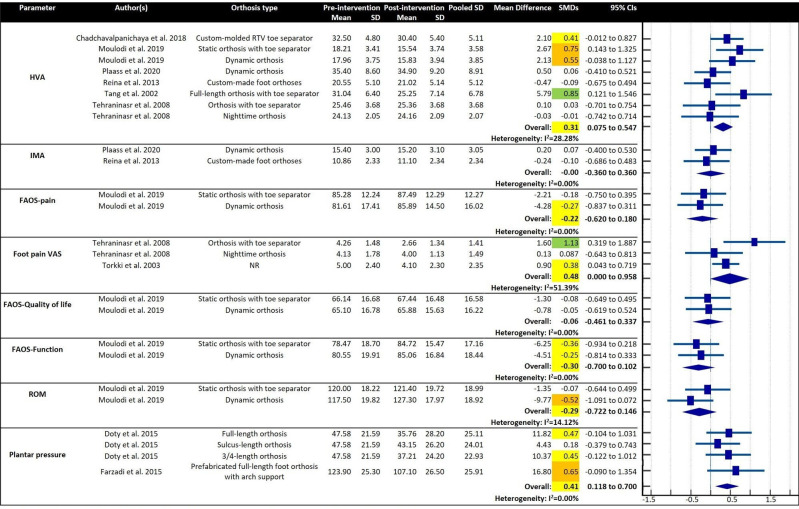
Overview of results from meta-analyses
Figure 4 provides the overall SMDs and SMDs for individual studies in which eight measurement factors before and after intervention in the HV group are compared. The primary function of HV orthosis is to correct the HVA, and a total of six studies investigated the effect of orthosis on the HVA correction. A small effect for HV orthosis in correcting HVA was found (SMD: 0.31, 95% CI: 0.075 to 0.547) with I2 28.28%. Tang et al43 stated that their full-length orthosis with a toe separator provides a significantly positive reduction of the HVA of 5.79° in the HV group (SMD: 0.85, 95% CI: 0.121 to 1.546), which has the highest corrective effect among all the recorded orthoses. The static orthosis with a toe separator tested by Moulodi et al38 also showed a significant positive HVA correction of 2.67° in the HV group (SMD: 0.75, 95% CI: 0.143 to 1.325). Chadchavalpanichaya et al36 developed a custom-moulded room temperature vulcanising (RTV) toe separator, which helps to correct the HVA by 2.1° in the HV group (SMD: 0.41, 95% CI: −0.012 to 0.827). The pooled estimation for orthoses with a toe separator was further investigated that the effect is medium (SMD: 0.50, 95% CI: 0.189 to 0.803) with I2 14.52%. The dynamic orthosis tested also showed a significantly positive reduction of the HVA of 2.13° (SMD: 0.55, 95% CI: −0.038 to 1.127).38 The pooled estimation for dynamic orthoses showed small effect in HVA correction (SMD: 0.27, 95% CI: −0.211 to 0.751) with I2 42.29%.
Figure 4.
Comparison of observations.aSMD ≥0.2 or ≤−0.2 highlighted in yellow; SMDs ≥0.5 or ≤−0.5 in orange and SMDs ≥0.8 or ≤−0.8 in green. FAOS, Foot and Ankle Outcome Score; HVA, hallux valgus angle; IMA, intermetatarsal angle; ROM, range of motion; RTV, room temperature vulcanising; SMD, standardised mean difference; VAS, Visual Analogue Scale.
Three of the studies investigated the pain score with the use of two different types of rating scales. One of them, Tehraninasr et al41 showed that their orthosis with a toe separator can significantly reduce the pain level (SMD: 1.13, 95% CI: 0.319 to 1.887). The level of physical functioning before and after the application of an orthosis have also been compared. A small effect (SMD: −0.30, 95% CI: −0.700 to 0.102) was achieved.
Two other studies investigated the impact of the foot orthosis on plantar pressure. Small effect for HV orthosis in plantar pressure reduction was found (SMD: 0.41, 95% CI: 0.118 to 0.700) with I2 0.00%. It was found that the prefabricated full-length orthosis with an arch support22 can significantly reduce the plantar pressure by 16.8 kPa (SMD: 0.65, 95% CI: −0.090 to 1.354).
Observation of key design features
Customised versus prefabricated
Among the orthoses that showed a significant reduction of the HVA after treatment among the patients with HV, the orthoses developed by Chadchavalpanichaya et al36 and Tang et al43 are custom-made, while those in Moulodi et al38 Tehraninasr et al41 Torkki et al42 Doty et al37 and Farzadi et al22 are prefabricated. This shows that the ability of an orthosis to reduce the severity of HV or its treatment effectiveness might not be related to whether it is customised or prefabricated. However, adjustment and fitting are still key factors, and patients are instructed to adjust the prefabricated orthosis to the best fitting position.39
Static versus dynamic
In terms of HVA reduction, the results are consistent with those of the patients with HV before and after the intervention. Both types of orthoses have a positive effect on treatment effectiveness, while all of the static orthoses that help to reduce the HVA are embedded with the feature of toe separator. Therefore, the toe separator seems to be the key element in correcting the misalignment of the big toe.
Considerations around orthosis length and arch support
In terms of the orthosis length, the full-length orthosis in Tang et al43 has a significant and exceptional corrective effect of HV in the HV group. The full-length orthoses with arch support in Farzadi et al22 can significantly reduce the plantar pressure. These results show that when considering the length of the orthosis for patients with HV, full-length is preferred, and arch support may be important to achieve therapeutic effects.
Discussion
This is the first study to systematically evaluate and synthesise results from the extensive pool of literature that investigates the characteristics of HV orthoses and their effects on different factors. The data obtained from meta-analysis suggest that dynamic orthoses, and static orthoses with a toe separator help to reduce the HVA by approximately 2.1° to 5.79° among patients with HV.36 38 43 The treatment effect of orthoses with a toe separator on HVA correction is larger than that of dynamic orthoses. The full-length orthosis with toe separator developed by Tang et al43 has a significant and exceptional HVA correction effect. The use of orthoses with a toe separator for moderate degree patients with HV can reduce HVA and hallux pain without serious complications.36 41 The studies also showed that the toe separator can greatly alleviate pain by better aligning the big toe and relieving the overstretched collateral ligaments and bone subluxation.41 43 However, due to the ease of use, fit and better appearance, users may be more satisfied with dynamic than static orthoses.38 The dynamic orthoses can reduce the contracture of the first metatarsophalangeal joint and better align the big toe through low torque and prolonged stretching.36 44 45 The freedom of joint movement does not limit the ROM of the big toe, but help to maintain joint mobility and prevent joint stiffness, which seem to have a beneficial effect on the treatment of HV.38
The full-length orthoses with an arch support tested by Farzadi et al22 help to reduce the plantar pressure and forefoot pain significantly. It can be suggested that forefoot pain has an evident relationship with plantar pressure in the metatarsalgia region.24 46 47 This might be associated with better body load distribution by relieving the excessive pressure on the forefoot through metatarsal unloading. By maximising the total contact area of the foot with a full-length orthosis, the peak plantar pressure can be reduced by 30%–40%.48 49 In addition, with adequate arch support, the anatomical alignment of the foot can be restored correctly.41
Both customised and prefabricated orthoses can significantly reduce the symptoms of HV. Ring and Otter50 compared the clinical efficacy of casted foot orthoses and prefabricated foot orthoses in the treatment of plantar heel pain in 67 patients, and found no significant difference in effectiveness between the bespoke or prefabricated orthoses. In addition, compared with the average cost of bespoke devices, the prefabricated orthoses are 38% less expensive per patient. They concluded that prefabricated orthoses could provide benefits that are equivalent to those of casted foot orthoses, but at considerably reduced costs. Since the material properties, thickness and rigidity of the orthoses studied remain unknown, no conclusion can be made on the best material for HVA reduction. However, Chadchavalpanichaya et al36 found that an RTV silicone toe separator is comfortable to wear. Its compliance with treatment is higher than that of the nighttime HV strap.36 The cost of a toe separator made of RTV silicone is only one-tenth of that of medical grade silicone, which can be considered as a clinical and cost-effective option.36
Torkki et al18 pointed out that an orthosis can provide short-term symptomatic relief. However, the wearing duration of the three orthoses in their study ranges from 1 month to 1 year. This may show that orthoses with a toe separator help to reduce the HVA not only for a short period of time but also on a continuous basis. Moreover, the angle reduction did not increase with treatment duration, which may indicate that the treatment reaches its equilibrium result at a certain point of time.
Conclusion
Foot orthoses can be an acceptable treatment option to reduce HV deformity. This systematic review demonstrates a positive relationship between HVA reduction and pain level with orthoses that offer a toe separator. Therefore, it is important to include this element in the conservative treatment of HV deformity, as well as the future development of HV orthoses. It is recommended that a fixed toe separator or a dynamic orthosis is used to maintain the anatomic alignment of the big toe for those who suffer from HV. The results of this study provide patients, practitioners and physicians with important information to help them better understand the characteristics of various HV orthoses and their performance in reducing HV deformity, and contribute to decisions around optimal treatment for patients.
Strengths and limitations
As with any systematic review or meta-analysis, the strength of these results relies on the quality of the studies included. The limitations of this study include the scarcity of studies found on this topic in the literature, lack of consistency in the various study methods, subjects’ conditions and limited consideration of the reliability and validity of the HV assessments in the included studies. Only a few randomised controlled trials are compared and reported in this study and there is limited information on the materials of the orthotics studied. More randomised controlled trials related to HV orthoses are needed, and more research on the material properties of HV orthoses is also required, in order to offer an effective solution for effective and optimal designs of HV orthoses.
Supplementary Material
Footnotes
Contributors: M-YK conceived and wrote this systematic review with meta-analysis. K-LY, JY and C-YT reviewed the protocol and provided extensive feedback. All authors approved the final manuscript.
Funding: The authors would like to acknowledge the Departmental Grant of Institute of Textiles and Clothing, The Hong Kong Polytechnic University (grant number PolyU RHRM) for funding this project.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplemental information. No additional data are available.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res 2010;3:21. 10.1186/1757-1146-3-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fournier M, Saxena A, Maffulli N. Hallux valgus surgery in the athlete: current evidence. J Foot Ankle Surg 2019;58:641–3. 10.1053/j.jfas.2018.04.003 [DOI] [PubMed] [Google Scholar]
- 3.Hardy RH, Clapham JCR. Observations on hallux valgus. J Bone Joint Surg Br 1951;33-B:376–91. 10.1302/0301-620X.33B3.376 [DOI] [PubMed] [Google Scholar]
- 4.Piqué-Vidal C, Vila J. A geometric analysis of hallux valgus: correlation with clinical assessment of severity. J Foot Ankle Res 2009;2:15. 10.1186/1757-1146-2-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meyr AJ, Adams ML, Sheridan MJ, et al. Epidemiological aspects of the surgical correction of structural forefoot pathology. J Foot Ankle Surg 2009;48:543–51. 10.1053/j.jfas.2009.05.003 [DOI] [PubMed] [Google Scholar]
- 6.Abhishek A, Roddy E, Zhang W, et al. Are hallux valgus and big toe pain associated with impaired quality of life? A cross-sectional study. Osteoarthritis Cartilage 2010;18:923–6. 10.1016/j.joca.2010.03.011 [DOI] [PubMed] [Google Scholar]
- 7.Cho NH, Kim S, Kwon D-J, et al. The prevalence of hallux valgus and its association with foot pain and function in a rural Korean community. J Bone Joint Surg Br 2009;91-B:494–8. 10.1302/0301-620X.91B4.21925 [DOI] [PubMed] [Google Scholar]
- 8.Menz HB, Roddy E, Thomas E, et al. Impact of hallux valgus severity on general and foot-specific health-related quality of life. Arthritis Care Res 2011;63:396–404. 10.1002/acr.20396 [DOI] [PubMed] [Google Scholar]
- 9.Roddy E, Zhang W, Doherty M. Prevalence and associations of hallux valgus in a primary care population. Arthritis Rheum 2008;59:857–62. 10.1002/art.23709 [DOI] [PubMed] [Google Scholar]
- 10.Hunt KJ, McCormick JJ, Anderson RB. Management of forefoot injuries in the athlete. Oper Tech Sports Med 2010;18:34–45. 10.1053/j.otsm.2009.12.001 [DOI] [Google Scholar]
- 11.Vaseenon T, Intharasompan P, Wattanarojanapom T, et al. Foot and ankle problems in Muay Thai kickboxers. J Med Assoc Thai 2015;98:65–70. [PubMed] [Google Scholar]
- 12.Schöffl V, Küpper T. Feet injuries in rock climbers. World J Orthop 2013;4:218. 10.5312/wjo.v4.i4.218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Killian RB, Nishimoto GS, Page JC. Foot and ankle injuries related to rock climbing. The role of footwear. J Am Podiatr Med Assoc 1998;88:365–74. 10.7547/87507315-88-8-365 [DOI] [PubMed] [Google Scholar]
- 14.Steinberg N, Siev-Ner I, Zeev A, et al. The association between hallux valgus and proximal joint alignment in young female dancers. Int J Sports Med 2015;36:67–74. 10.1055/s-0034-1384550 [DOI] [PubMed] [Google Scholar]
- 15.Niek van Dijk C, Lim LSL, Poortman A, et al. Degenerative joint disease in female ballet dancers. Am J Sports Med 1995;23:295–300. 10.1177/036354659502300307 [DOI] [PubMed] [Google Scholar]
- 16.Steinberg N, Hershkovitz I, Peleg S, et al. Morphological characteristics of the young scoliotic dancer. Phys Ther Sport 2013;14:213–20. 10.1016/j.ptsp.2012.07.003 [DOI] [PubMed] [Google Scholar]
- 17.du Plessis M, et al. Manual and manipulative therapy compared to night splint for symptomatic hallux abducto valgus: an exploratory randomised clinical trial. Foot 2010;21:71–8. [DOI] [PubMed] [Google Scholar]
- 18.Torkki M, Malmivaara A, Seitsalo S, et al. Surgery vs orthosis vs watchful waiting for hallux valgus: a randomized controlled trial. JAMA 2001;285:2474–80. 10.1001/jama.285.19.2474 [DOI] [PubMed] [Google Scholar]
- 19.Coetzee JC. Scarf osteotomy for hallux valgus repair: the dark side. Foot Ankle Int 2003;24:29–33. 10.1177/107110070302400104 [DOI] [PubMed] [Google Scholar]
- 20.Sammarco GJ, Idusuyi OB. Complications after surgery of the hallux. Clin Orthop Relat Res 2001;391:59–71. 10.1097/00003086-200110000-00008 [DOI] [PubMed] [Google Scholar]
- 21.Jahss MH. Disorders of the foot & ankle : medical and surgical management. 2nd edn. Philadelphia: Saunders, 1991. [Google Scholar]
- 22.Farzadi M, Safaeepour Z, Mousavi ME, et al. Effect of medial arch support foot orthosis on plantar pressure distribution in females with mild-to-moderate hallux valgus after one month of follow-up. Prosthet Orthot Int 2015;39:134–9. 10.1177/0309364613518229 [DOI] [PubMed] [Google Scholar]
- 23.Charrette M. Bunion formation and orthotic support. Dynamic Chiropractic 2009;2:1–3. [Google Scholar]
- 24.Arias-Martín I, Reina-Bueno M, Munuera-Martínez PV. Effectiveness of custom-made foot orthoses for treating forefoot pain: a systematic review. Int Orthop 2018;42:1865–75. 10.1007/s00264-018-3817-y [DOI] [PubMed] [Google Scholar]
- 25.Hawke F, Burns J, Radford J, et al. Custom foot orthoses for the treatment of foot pain: a systematic review. J Foot Ankle Res 2008;1:O46. 10.1186/1757-1146-1-S1-O46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Genaidy AM, LeMasters GK. The epidemiological appraisal instrument (EAI): a brief overview. Theor Issue Ergonomic Sci 2006;7:187–9. [Google Scholar]
- 27.Genaidy AM. Cancer risk among firefighters : epidemiological evidence. University of Cincinnati, 2004. [Google Scholar]
- 28.Genaidy AM, Lemasters GK, Lockey J, et al. An epidemiological appraisal instrument - a tool for evaluation of epidemiological studies. Ergonomics 2007;50:920–60. 10.1080/00140130701237667 [DOI] [PubMed] [Google Scholar]
- 29.Faraone SV. Interpreting estimates of treatment effects: implications for managed care. P&T 2008;33:700–11. [PMC free article] [PubMed] [Google Scholar]
- 30.Durlak JA. How to select, calculate, and interpret effect sizes. J Pediatr Psychol 2009;34:917–28. 10.1093/jpepsy/jsp004 [DOI] [PubMed] [Google Scholar]
- 31.Deeks JJ, Higgins JPT, Altman DG. Analysing data and undertaking meta‐analyses. Chichester, UK: John Wiley & Sons, Ltd, 2008: 243–96. [Google Scholar]
- 32.McGough JJ, Faraone SV. Estimating the size of treatment effects: moving beyond P values. Psychiatry 2009;6:21. [PMC free article] [PubMed] [Google Scholar]
- 33.Cohen J. Statistical power analysis for the behavioral sciences. 2nd edn. Hillsdale, NJ: L. Erlbaum Associates, 1988. [Google Scholar]
- 34.Faraone S. Understanding the effect size of ADHD medications: implications for clinical care. Medscape Psychiatry & Mental Health 2003;8. [Google Scholar]
- 35.van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics 2010;84:523–38. 10.1007/s11192-009-0146-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chadchavalpanichaya N, Prakotmongkol V, Polhan N, et al. Effectiveness of the custom-mold room temperature vulcanizing silicone toe separator on hallux valgus: a prospective, randomized single-blinded controlled trial. Prosthet Orthot Int 2018;42:163–70. 10.1177/0309364617698518 [DOI] [PubMed] [Google Scholar]
- 37.Doty JF, Alvarez RG, Ervin TB, et al. Biomechanical evaluation of custom foot Orthoses for hallux valgus deformity. J Foot Ankle Surg 2015;54:852–5. 10.1053/j.jfas.2015.01.011 [DOI] [PubMed] [Google Scholar]
- 38.Moulodi N, Kamyab M, Farzadi M. A comparison of the hallux valgus angle, range of motion, and patient satisfaction after use of dynamic and static orthoses. Foot 2019;41:6–11. 10.1016/j.foot.2019.06.002 [DOI] [PubMed] [Google Scholar]
- 39.Plaass C, Karch A, Koch A, et al. Short term results of dynamic splinting for hallux valgus — a prospective randomized study. Foot and Ankle Surgery 2020;26:146–50. 10.1016/j.fas.2019.01.002 [DOI] [PubMed] [Google Scholar]
- 40.Reina M, Lafuente G, Munuera PV. Effect of custom-made foot orthoses in female hallux valgus after one-year follow up. Prosthet Orthot Int 2013;37:113–9. 10.1177/0309364612447097 [DOI] [PubMed] [Google Scholar]
- 41.Tehraninasr A, Saeedi H, Forogh B, et al. Effects of insole with toe-separator and night splint on patients with painful hallux valgus: a comparative study. Prosthet Orthot Int 2008;32:79–83. 10.1080/03093640701669074 [DOI] [PubMed] [Google Scholar]
- 42.Torkki M, Malmivaara A, Seitsalo S, et al. Hallux valgus: immediate operation versus 1 year of waiting with or without orthoses: a randomized controlled trial of 209 patients. Acta Orthop Scand 2003;74:209–15. 10.1080/00016470310013987 [DOI] [PubMed] [Google Scholar]
- 43.Tang SF, Chen CP, Pan J-L, et al. The effects of a new foot-toe orthosis in treating painful hallux valgus. Arch Phys Med Rehabil 2002;83:1792–5. 10.1053/apmr.2002.34835 [DOI] [PubMed] [Google Scholar]
- 44.Nicholas J. Rehabilitation of patients with rheumatic disorders. Phy Med Rehab 1996:711–27. [Google Scholar]
- 45.John MM. Dynamic splinting for hallux valgus and hallux varus: a pilot study. Foot Ankle J 2009. [Google Scholar]
- 46.Postema K, Burm PE, Zande ME, et al. Primary metatarsalgia: the influence of a custom moulded insole and a rockerbar on plantar pressure. Prosthet Orthot Int 1998;22:35–44. 10.3109/03093649809164455 [DOI] [PubMed] [Google Scholar]
- 47.Kelly A, Winson I. Use of ready-made insoles in the treatment of lesser metatarsalgia: a prospective randomized controlled trial. Foot Ankle Int 1998;19:217–20. 10.1177/107110079801900405 [DOI] [PubMed] [Google Scholar]
- 48.Nouman M, Leelasamran W, Chatpun S. Effectiveness of total contact orthosis for plantar pressure redistribution in neuropathic diabetic patients during different walking activities. Foot Ankle Int 2017;38:901–8. 10.1177/1071100717704427 [DOI] [PubMed] [Google Scholar]
- 49.Kitaoka HB, Luo Z-P, Kura H, et al. Effect of foot orthoses on 3-dimensional kinematics of flatfoot: a cadaveric study. Arch Phys Med Rehabil 2002;83:876–9. 10.1053/apmr.2002.32681 [DOI] [PubMed] [Google Scholar]
- 50.Ring K, Otter S. Clinical efficacy and cost-effectiveness of bespoke and prefabricated foot orthoses for plantar heel pain: a prospective cohort study. Musculoskeletal Care 2014;12:1–10. 10.1002/msc.1053 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplemental information. No additional data are available.