Abstract
Background:
Psychiatric patients or mentally ill patients conform a substantial section of the community deserving special attention. This study aimed to assess the oral health status and treatment needs of psychiatric patients attending District Civil Hospital, Raichur, Karnataka.
Materials and Methods:
The study group comprised 150 outpatients aged 18–64 years, attending the Department of Psychiatry, District Civil Hospital, Raichur. A specific questionnaire was drawn up and was used to record the demographic and medical data and oral hygiene practices. Type III clinical examination was carried out. The WHO Assessment Form 1997 was used to assess the oral health status of the study population.
Results:
Of the 150 patients examined, 90 (60%) were male and 60 (40%) were female. The mean age of the patients was 33.79 ± 10.57 years. The majority (52%) were diagnosed with epilepsy and 18% had anxiety disorder. The prevalence of caries was 87.3%. Periodontal status, according to the Community Periodontal Index scores, was as follows: 54% of the patients had shallow pocket (4 mm–5 mm) and 32% of the patients had 6-mm or more deep pocket.
Conclusion:
This study highlights a substantial need for prevention and treatment of oral health needs among psychiatric patients, and to increase awareness toward oral health.
KEYWORDS: Dental caries, oral health, oral hygiene status, psychiatric patients
INTRODUCTION
Caries and periodontal diseases that are characterized by inflammation are common oral health problems seen in the world. Psychiatric patients form a substantial section of the society needing special attention and are often neglected because of fear, stigma, ignorance, and negative attitudes. Psychiatric or mental disorders affect the general behavior of a person and impair his/her level of functioning and also alter perceptions, leading to improper self-care and poor oral health in them.[1] Psychiatric patients have abundant dental problems due to general self-neglect associated with mental illness and also fear of treatment, high treatment charges, inability to access dental services, and the side effects of medication.[2]
Disability affects over a billion people, which constitutes up to 15% of the world's population.[3] About 12.3% of the global burden of the disease constitutes mental disorders. It has been seen that in such psychiatric patients, oral health is poor and they have large unmet treatment needs. Disability-adjusted life years lost due to mental and behavioral disorders is estimated to increase up to 15% by 2020 which was 11% in 1999.[4]
Psychotropic drugs frequently used to treat these mental disorders result in gland hypofunction due to long-term usage, leading to xerostomia and dry mouth as common side effects, presented by patients and reported by clinicians.[5] The long-term hospitalization of psychiatric patients also leads to poor oral health issues.
Poor oral health in these patients leads to dental caries and periodontal problems. Improper and irregular eating and poor oral hygiene habits along with reduced salivation due to drugs form the causative factors for high caries activity. Oral health behaviors such as tobacco use and irregular brushing habits have been associated with depression and psychological factors. Depression has been consistently associated with smoking and psychological factors, which were significant predictors of plaque accumulation.[6] Among psychotic patients, tooth brushing is most commonly neglected when compared with nonpsychotics.[7]
Psychiatric disorders affecting dental health include dental anxiety, dental phobia, psychosis, eating disorders (anorexia and bulimia nervosa), alcohol and substance abuse, and mood disorders. Those who are dependent on drugs or alcohol often neglect their personal hygiene and dietary needs and may live in poor social conditions, all of which contribute to poor oral health.[8]
Caries and periodontal diseases that are characterized by inflammation are common oral health problems seen in the world. Psychiatric patients form a substantial section of the society needing special attention and are often neglected because of fear, stigma, ignorance, and negative attitudes. Psychiatric or mental disorders affect the general behavior of a person and impair his/her level of functioning and also alter perceptions, leading to improper self-care and poor oral health in them.[1] Psychiatric patients have abundant dental problems due to general self-neglect associated with mental illness and also fear of treatment, high treatment charges, inability to access dental services, and the side effects of medication. Psychiatric patients have abundant dental problems due to general self-neglect associated with mental illness and also fear of treatment, high treatment charges, inability to access dental services, and the side effects of medications.
Psychiatric disturbances and issues are commonplace in the present scenario due to rapid change in lifestyle and increased demands and pressure at workplace.[9] Hence, there is a basic need for dental health education, and lack of access to dental care is also a pertinent issue in towns. Hence, the present study was undertaken on psychiatric outpatients in Raichur city to assess the outcome.
MATERIALS AND METHODS
Psychiatric outpatients visiting the outpatient department of District Civil Hospital, Raichur, Karnataka, were considered to reflect upon their oral health status and treatment needs, and a cross-sectional study was carried out in them.
The WHO Oral Health Assessment Form (1997) was used to assess the patient needs as per the diagnostic criteria described by the WHO.[10] A specific and a structured questionnaire was drawn up and was used to record the demographic variables, medical data such as duration of illness and drug usage, and oral hygiene practices. The examiners explained the questions in their local language and the answers were recorded.
The data obtained from the pilot study were used to arrive at an exact sample size for the present study. The sample was then rounded off to 150. All the patients included in the study were diagnosed by a psychiatrist and classified according to the International Classification of Diseases 10 developed by the World Health Organization in 1992.[10] The patients were checked for oral health status seated in upright position on a chair and examined in adequate natural daylight using Type III clinical examination.
SPSS v16.0 (IBM company, Chicago and United States of America) software was used for data analysis, and P < 0.05 was considered statistically significant.
RESULTS
The patients examined ranged from 18 to 64 years, with a mean age of 33.8 years (standard deviation ± 10.58), A total of 150 patients were examined, out of which 90 (60%) were male and 60 (40%) were female.
In the present study, majority of the patients presented with a normal mucosa and only five cases showed oral submucous fibrosis of the buccal mucosa. No patients presented with any signs and symptoms related to the temporomandibular joint. The mean age of the patients was 33.79 ± 10.57 years. The majority (52%) were diagnosed with epilepsy and 18% had anxiety disorder. The prevalence of caries was 87.3%. Periodontal status, according to the Community Periodontal Index (CPI) scores, was as follows: 54% of the patients had shallow pocket (4 mm–5 mm) and 32% of the patients had 6-mm or more deep pocket.
Dental caries prevalence
Of the 150 psychiatric patients, 133 (88.7%) were with caries and 17 (11.3%) were caries free.
Decayed, missing, and filled component of DMFT
In our study, the mean Decayed, Missing and Filled teeth (DMFT) per person was 4.06 (±3.2) and the mean of its components was 3.4 (±1.2) for decayed teeth, 0.04 (±0.33) for missing teeth, and 0.61 (±1.82) for filled teeth [Table 1].
Table 1.
z Distribution of permanent teeth according to decayed, missing and filled component of decayed, missing and filled teeth
| DMFT component | Number of teeth affected | Mean number of tooth affected per person |
|---|---|---|
| DT | 510 | 3.4 |
| MT | 92 | 0.61 |
| FT | 7 | 0.04 |
| Total (DMFT) | 609 | 4.06 |
DMFT: Decayed, missing and filled teeth, DT: Decayed teeth, MT: Missing teeth, FT: Filled teeth
Treatment needs
Out of the 150 patients, 113 (75.3%) required one tooth surface filling, 28 (18.6%) required two or more tooth surface fillings, 37 (24.7%) required crown for any other reason, and 36 (24%) patients required extraction.
Periodontal status
The percentage of periodontal status of the study patients according to the CPI scores was as follows: bleeding on probing was recorded in 1.3% and calculus was seen in 12.7% of the study patients. Nearly 54% of the patients had shallow pocket (4 mm–5 mm) and 32% of the patients had 6-mm or more deep pocket . No patients had a healthy periodontal condition [Figure 1].
Figure 1.
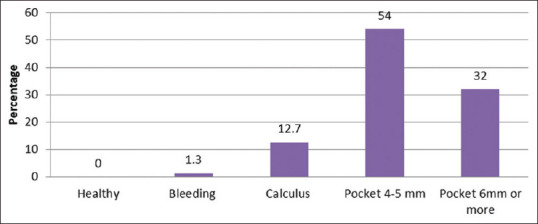
Percentage of patients according to the Community Periodontal Index
Periodontal attachment loss
Of the 150 psychiatric patients, 102 patients (68%) had periodontal attachment loss of 0 mm–3 mm and 48 (32%) patients had attachment loss of 4 mm–5 mm. In the present study, the association between the periodontal attachment loss and age group was found to be highly significant [Figure 2].
Figure 2.
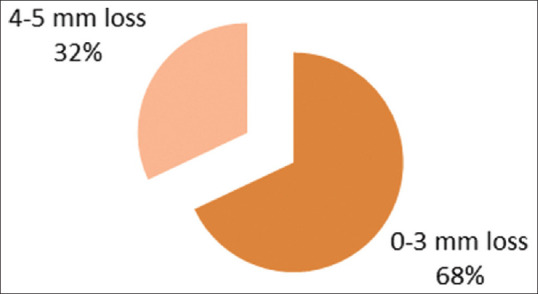
Percentage of patients according to periodontal attachment loss
DISCUSSION
Psychiatric disorders affect the oral health of patients in multiple ways. Psychiatric problems confer a negative impact in the prognosis and treatment plan of various medical illnesses, increase the required duration of treatment, and thus decrease the patient's functional level.[11]
The study results revealed a high caries prevalence among psychiatric patients. Of the 150 study patients examined, 133 (88.7%) had caries and 17 (11.3%) were caries free. The overall caries prevalence in our study was 88.7%, which is similar to the caries prevalence of 89% among psychiatric patients in elderly institutions of Denmark. A high prevalence of caries (75.5% and 73.2%) was seen in other studies, done on hospitalized psychiatric patients in Bengaluru city[1] and Pune, respectively.[12] The findings were in contrast to that of the study conducted on institutionalized psychiatric patients in Davangere with high water fluoride content and thus their caries prevalence was 32.2%.[13]
The mean DMFT score in the present study was 4.06 (±3.2), which is similar to other studies conducted on psychiatric inpatients in Ranchi[6] and Pune, that is, 3.45 (±5.17) and 4.49, respectively.[12]
The average DMFT scores of psychiatric inpatients in Serbia and South Wales were, respectively, 24.4 and 19.1, which are much higher than that of the present study; this might be due to the long-term hospitalization of psychiatric patients. The treatment needs of the study population indicate that majority (94%) of the patients required restorations. Seventy-seven percent of restorative care was recorded in the study conducted on hospitalized psychiatric patients in Bengaluru city. In our study, 24% of the patients required extraction; this finding is consistent with the study conducted on psychiatric inpatients in South Wales,[14] where 27.2% required extraction.
The periodontal tissues of the psychiatric population exhibited different clinical manifestations due to poor oral hygiene practices. The results of our study revealed the presence of higher CPI scores, that is, 54% of shallow pockets and 32% of deep pockets; these findings of our study were consistent with those of another study conducted on hospitalized psychiatric patients in Pune,[12] where 68% had shallow pockets and 32% had deep pockets. In the present study as the age group increased, the percentage of patients with deep pockets also increased, that is, 27% of the patients had deep pockets in 25–34 years' age group and 86% of the patients had deep pockets in 55–64 years' age group. Age-related changes of periodontal tissues such as bleeding gums, calculus deposits, or evidence of gingival pockets clubbed with the psychiatric condition of the patients play a major role in periodontal involvement.[9] The association between poor periodontal health and longer period of hospitalization could be attributed to the accumulated effects of periodontal problems, involving more teeth leading to periodontitis and finally tooth loss as age advances.[15] This could be the reason in the present study, as age increased, the loss of attachment also increased.
Psychiatric or mental disorders affect oral health, leading to high prevalence of oral diseases, especially among elderly age group. The results of the present study evidenced a high prevalence of dental caries and periodontal disease. The study outcome supports the need to develop a balanced oral health system, which will improve the oral health outcomes of these psychiatric patients.
CONCLUSION
From this study, it has been seen that a special group of patients with psychiatric disorders in the community do suffer from varied oral health issues such as dental caries and periodontal tissue damage. The degree of oral disease prevalence is attributed to the severities of psychiatric disorder of this group of population.
A detailed approach with crisp understanding of the oral health issues of the psychiatric population and a well-planned, coordinated interdisciplinary mode of care involving a team of specialists are necessary to tackle the severe oral health issues in this neglected lot. Proper coordinative efforts of the fraternity of medical, dental, and social care sectors are the need of the hour for oral health well-being of this underprivileged population.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rekha R, Hiremath SS, Bharath S. Oral health status and treatment requirements of hospitalised psychiatric patients in Bangalore city: A comparative study. J Indian Soc Pedod Prev Dent. 2002;20:63–7. [PubMed] [Google Scholar]
- 2.Mirza I, Day R, Phelan M, Wulff V. Oral health of psychiatric in patients. Psychiatr Bull. 2001;25:143–5. [Google Scholar]
- 3.World Health Organization. Disability and Health. [Last accessed on 2012 Nov]. Available from: http://www.who.int/en/
- 4.World Health Organization. Ministerial Round Tables 2001; 54th World health Assembly on Mental Health. Geneva: World Health Organization; 2001. [Google Scholar]
- 5.Smith RG, Burtner AP. Oral side effects of the most frequently used drugs. Spec Care Dentist. 1994;14:96–102. doi: 10.1111/j.1754-4505.1994.tb01112.x. [DOI] [PubMed] [Google Scholar]
- 6.Jyoti B, Muneeshwar PD, Srivastava R, Singh AR, Kiran M, Simlai J. Oral health Status and Treatment needs of Psychiatric inpatients in Ranchi, India. JIAOMR. 2012;24:171–8. [Google Scholar]
- 7.Sayegh F, Dababneh R, Rodan R. Oral health status and dental treatment needs among non institutionalized psychiatric patients. JRMS. 2006;13:27–31. [Google Scholar]
- 8.Cormac I, Jenkins P. Understanding the importance of oral health in psychiatric patients. Adv Psychiatr Treat. 1999;5:53–60. [Google Scholar]
- 9.Jayakumar HL, Jyothi D, Mahesh Chandra K, Pallavi HN. Periodontal health among elderly psychiatric patients in Bangalore City. Pak Oral Dent J. 2011;31:128–36. [Google Scholar]
- 10.World Health Organization. Oral Health Surveys- Basic Methods. 4th ed. Geneva: World Health Organization; 1997. [Google Scholar]
- 11.Little JW, Falace DA, Miller CS, Rhodus NL. Dental Management of the Medically Compromised Patients. 8th ed. China: Elsevier Publisher; 2013. [Google Scholar]
- 12.Gowda EM, Bhat PS, Swamy MM. Dental health requirements for psychiatric patients. Med J Armed Forces India. 2007;63:328–30. doi: 10.1016/S0377-1237(07)80007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar M, Chandu GN, Shafiulla MD. Oral health status and treatment needs in institutionalized psychiatric patients: One year descriptive cross sectional study. Indian J Dent Res. 2006;17:171–7. doi: 10.4103/0970-9290.29868. [DOI] [PubMed] [Google Scholar]
- 14.Lewis S, Jagger RG, Treasure E. The oral health of psychiatric in-patients in south wales. Spec Care Dentist. 2001;21:182–6. doi: 10.1111/j.1754-4505.2001.tb00252.x. [DOI] [PubMed] [Google Scholar]
- 15.Gurbuz O, Alatas G, Kurt E, Dogan F, Issever H. Periodontal Health and treatment needs among hospitalised chronic psychiatric parients in Istanbul, Turkey. Community Dental Health. 2011;28:69–74. [PubMed] [Google Scholar]


