Abstract
Purpose:
The purpose was to evaluate the difference in crestal bone loss (CBL) around implants with flap and flapless methods followed by early loading.
Materials and Methods:
Twenty implants were placed in twenty patients – ten using flap and ten using flapless techniques. The difference in CBL was measured on standardized digital periapical radiograph taken at 0 week, 6 weeks, 12 weeks, and 6 months.
Results:
The present study showed the mean CBL on proximal surfaces when evaluated at intervals of 0 week, 6 weeks, 12 weeks, and 6 months for flapless method was significantly lower than with flap method the values of which were +0.07 mm against +0.26 mm on mesial side and +0.15 mm against +0.33 mm on distal side at 6 months.
Conclusion:
The flapless approach is a predictable procedure when patient selection and surgical technique are appropriate, and results in lesser CBL.
KEYWORDS: Crestal bone loss, early loading, flapless surgery, implant, osseointegration
INTRODUCTION
Over the course of years, implant dentistry has had the opportunity to observe long-term success and failure with various techniques and devices.[1] Conventionally, osseointegrated dental implantation was performed by raising a flap that involved soft-tissue flap reflection which facilitates visibility and access at the operating site and is considered advantageous in the esthetic zone. However, reflection of mucoperiosteal flap compromises the vascular supply of bone, which may lead to crestal bone loss (CBL) and long-term esthetic complications and demands the introduction of sutures after implant placement.[2,3,4,5]
To address these problems, an alternative technique, that is, flapless implant placement has been introduced for patients with sufficient bone volume in the implant recipient site to minimize postoperative peri-implant tissue loss and to overcome the challenge of soft-tissue management during or after surgery.[6] Flapless implant placement avoids the creation of a flap by minimal removal of soft tissue and creation of osteotomy site, thereby resulting in less postoperative patient discomfort. Furthermore, it leaves the periosteum intact on the buccal and lingual aspects of the ridge so as to maintain a proper blood supply at the implantation site, reducing the possibility of resorption.[1,2]
Although flapless implant placement is advantageous to patients, implant placement with this technique is a blind procedure, and bone perforations are more likely to occur.[7]
Nowadays, the concept of early loading is becoming popular due to reduced patient discomfort and dysfunction.[8,9,10] Early loading protocols demand loading of implants from 1 week to 2 months after insertion.[11,12,13,14,15,16] In light of the various pros and cons of each of the flap and flapless techniques on early loading, it was considered potentially useful to compare the CBL and peri-implant soft tissue by two techniques.
MATERIALS AND METHODS
A total of twenty implants (ten in each group) were placed in the edentulous mandibular posterior region. Ethical clearance was obtained from the ethical committee. After an explanation of the proposed study criteria, including alternative treatment options, potential risks, and benefits, a signed informed consent was obtained from all the selected individuals prior to the dental implant placement.
The selected participants were grouped on the basis of type of surgery during implant placement as: Group I: implants placed by flap technique and Group II: implants placed by flapless technique. This study included patients above 18 years of age who were medically fit in which twenty implants were placed in the posterior mandibular edentulous region, with sufficient amount of bone width of at least 4.5 mm without undercuts of >15° measured radiographically and keratinized tissue of at least 5 mm measured with the help of William's probe.
Detailed patient history was taken before selecting patients for procedure. All vital signs were checked and a complete hemogram was done to evaluate the fitness of the patient for implant placement followed by complete oral prophylaxis.
Preoperative intraoral periapical radiograph and orthopantomogram (OPG) provided the necessary information regarding the available bone and distance of vital structures.
A metal sphere of predetermined diameter (5 mm) was used to calibrate the length and diameter of the dental implant to be placed. The digital OPG obtained was then used to calibrate the dental implant length.
A custom-made polysiloxane putty jig was fabricated for each patient to standardize the radiograph in terms of angulations and position of the film relative to the X-ray beam. The periapical radiographs were made with the long cone paralleling technique using this putty jig for the standardization of the projection and film placement during the follow-up visits.
Diagnostic impression and models were made prior to surgery. A diagnostic wax-up of the involved tooth was done and acrylic surgical stent was fabricated based on wax-up to facilitate implant placement. Bone mapping was done followed by surgical stent fabrication to determine the width of the alveolar bone bucco-lingually.
Surgical preparation
Implant placement using flap technique
Local anesthesia was administered, and crestal incision was given for full-thickness flap reflection, to expose the implant site. A surgical stent was then placed and the implant site was marked with the help of a pilot drill. After marking the implant site, an osteotomy site of required dimensions was created. The implants were then inserted into this osteotomy site, which were placed slightly below the level of alveolar crest (1 mm below the crestal bone) [Figure 1]. Healing abutments were then screwed to the implants immediately after implant placement [Figure 2]. Once the healing abutments were placed, the surgical site was thoroughly irrigated and the flap was closed with tight nonresorbable 3-0 silk sutures to achieve water-tight closure. Medications were prescribed followed by surgery and suture placement. Postoperative instructions were given to the patients regarding diet and maintenance of oral hygiene.
Figure 1.

Flap reflection followed by implant placement
Figure 2.

Approximation of flap by 3.0 silk sutures and healing abutment in position
Implant placement using flapless surgeries
Routine presurgical protocol was followed for each patient as with flap technique. The site selection for flapless placement of the implant was done on the basis of bone width of at least 4.5 mm without undercuts of >15°, and keratinized tissue of at least 5 mm. All implants in this technique were inserted after the osteotomy site was created using surgical stents and soft-tissue punch [Figure 3]. After marking the implant site, an osteotomy site was created in which implants were placed. The implants were placed slightly below the level of the alveolar crest (1 mm below the crestal bone). Healing abutments were then screwed to the implants immediately after implant placement [Figure 4]. Postoperative instructions were given to the patient regarding diet and maintenance of oral hygiene. Medications were prescribed thereafter.
Figure 3.

Soft-tissue punch for tissue removal for implant placement
Figure 4.

Healing abutment in place after implant placement with flapless technique which involves soft-tissue removal with punch and no suture placement
After implant placement by both the techniques, the implants were left for osseointegration for a period of 2 months and then early loaded with Porcelain-Fused-to-Metal crown.
The patients were recalled for radiographic evaluation which was made at 6 weeks, 12 weeks, and 6 months of implant placement for evaluation of crestal bone changes. The periapical radiographs were obtained and digitized using Digimizer Image analysis, MedCalc Software version 4.3.5.0, Ostend, Belgium. The known implant length was used to calibrate the images in the computer software. After digitizing the radiograph, the measurements were recorded on proximal sides. Comparative measurements of crestal bone levels of mesial and distal sides adjacent to the implants were made. A minimum of three readings were made for each case, and the average values were used to calculate the change of crestal bone [Figures 5 and 6]. Statistical analysis was done using paired t-test.
Figure 5.
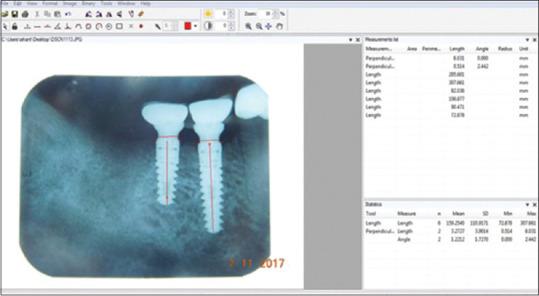
Crestal bone loss measurements on the mesial and distal sides of the implant placed by flap technique after 6 months using software Digimizer Image analysis. Medcalc Software, Version 4.3.5.0
Figure 6.
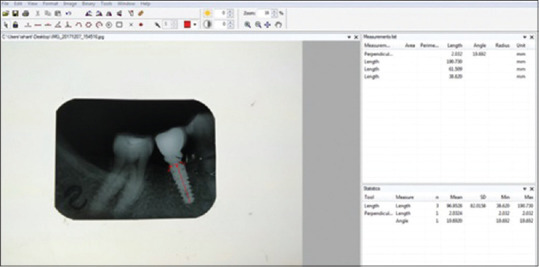
Crestal bone loss measurement on the mesial and distal sides of the implant placed by flapless technique after 6 months using software Digimizer Image analysis. Medcalc Software, Version 4.3.5.0
RESULTS
The study showed that change in the mean for crestal bone on mesial surfaces when evaluated at the interval of 0 week, 6 weeks, 12 weeks, and 6 months for flapless method was significantly lower than that with traditional flap method; the values of which were nil, −0.23, +0.34, and + 0.07 mm, respectively, for flap technique against nil, 0.00, +0.25, and + 0.26 mm, respectively, on the mesial side for flapless technique [Tables 1 and 2].
Table 1.
Evaluation of mean values, change in mean and P with flap technique on mesial and distal side at 0 weeks, 6 weeks, 12 weeks, and 6 months
| Variables | Mesial | Distal | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Mean±SD | Change in mean±SD | P | Mean±SD | Change in mean±SD | P | |
| 0 weeks | -0.22±0.44 | - | 0.21 (NS) | -0.20±0.71 | - | 0.37 (NS) |
| 6 weeks | -0.45±0.24 | -0.23±0.20 | 0.006 (S) | -0.39±0.52 | -0.19±0.19 | 0.003 (S) |
| 12 weeks | -0.11±0.40 | +0.34±0.16 | 0.24 (NS) | -0.08±0.52 | +0.31±0.01 | 0.009 (NS) |
| 6 months | -0.04±0.047 | +0.07±0.07 | 0.46 (NS) | +0.07±0.73 | +0.15±0.21 | 0.12 (NS) |
SD: Standard deviation, NS: Not significant, S: Significant
Table 2.
Shows evaluation of mean values, change in mean and P with flapless technique on mesial and distal side at 0 weeks, 6 weeks, 12 weeks, and 6 months
| Variables | Mesial | Distal | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Mean±SD | Change in mean±SD | P | Mean±SD | Change in mean±SD | P | |
| 0 weeks | -0.37±0.77 | - | 0.87 (NS) | -0.26±0.67 | - | 0.36 (NS) |
| 6 weeks | -0.37±0.76 | 0.00±0.01 | 0.002 (S) | -0.34±0.71 | -0.08±0.04 | 0.001 (S) |
| 12 weeks | -0.12±0.61 | +0.25±0.15 | 0.003 (S) | -0.01±0.76 | +0.33±0.05 | 0.001 (S) |
| 6 months | +0.14±0.56 | +0.26±0.05 | 0.001 (S) | +0.32±0.79 | +0.33±0.03 | 0.001 (S) |
SD: Standard deviation, NS: Not significant, S: Significant
Similar results were seen in change in the mean for CBL on distal surfaces when evaluated at the interval of 0 week, 6 weeks, 12 weeks, and 6 months; the values of which were nil, −0.19, +0.31, and + 0.15 mm, respectively, for flap technique against nil, −0.08, +0.33, and + 0.33 mm, respectively, on the distal side for flapless technique [Tables 1 and 2].
The mean value showed an increase in crestal bone level for both the techniques over a period of 6 months both at the mesial and distal sides of the implants, but the increase was found to be statistically significant (P < 0.05) and greater for flapless technique when compared with flap technique, which was statistically insignificant.
DISCUSSION
The present study showed that average CBL on proximal surfaces when evaluated at the intervals of 6 months for flapless method was significantly lower than that with traditional flap method; the values of which were + 0.07 mm against + 0.26 mm on the mesial side and + 0.15 mm against + 0.33 mm on the distal side. This indicates that the loss of bone during the 6-month period was significantly lower with flapless method compared to that with flap method. The present study is in accordance with Sennerby et al., who compared the average marginal bone loss occurring with flap versus flapless implant surgery. The authors reported slightly less bone loss for the flapless approach (–2.1 mm, standard deviation [SD] 1.4 mm; n = 70 implants) versus that of the conventional approach (–2.8 mm, SD 1.5 mm; n = 39 implants).[17]
In another study conducted by Becker et al., implants were placed via the flapless approach with a delayed loading protocol. Probing depths were measured at baseline and up to 1 month after the delivery of the final restoration. The change between those two time points was clinically insignificant (baseline: 2.2 mm [SD 0.9 mm]; up to 1 month: 2.3 mm [SD 0.8 mm]) and is in context with the present study.[18] The explanation of these findings is that when the implant is placed using flap procedures, the implant is positioned closer to the oral environment and plaque accumulation is considerable because of flap elevation and incomplete seal between the flaps due to placement of sutures. In addition, due to difficulty of flap adaptation on the surface of implant and suture loosening, the implant surface is more susceptible to exposure. All these allow the marginal bone to be invaded by the bacteria and harmed by the inflammation process and consequently bone resorption. Kan et al. concluded that to reduce the possibility of postoperative peri-implant tissue loss and to overcome the challenge of soft-tissue management, the concept of flapless implant surgery has been introduced for patients with the sufficient bone volume in the implant recipient site with few prerequisites for FL surgery such as a minimum of 4.5–5.0 mm of keratinized gingival tissue and at least 4–4.5 mm of alveolar bone width without undercuts >15°.[1,6,19,20,21,22,23,24]
Under the guidelines of the present study, the results suggest that flapless surgical approach followed by early loading is a good option for implant placement with less crestal bone resorption when compared with flap technique followed by early loading.
CONCLUSION
Flapless implant placement reduces the possibility of postoperative CBL and peri implant tissue loss and can benefit the patient. The procedure is more congenial because it does not involve raising extensive flaps and placement of sutures. Hence; it results in less bleeding with reduced postoperative discomfort.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hahn J. Single-stage, immediate loading, and flapless surgery. J Oral Implantol. 2000;26:193–8. doi: 10.1563/1548-1336(2000)026<0193:SILAFS>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Rousseau P. Flapless and traditional dental implant surgery: An open, retrospective comparative study. J Oral Maxillofac Surg. 2010;68:2299–306. doi: 10.1016/j.joms.2010.05.031. [DOI] [PubMed] [Google Scholar]
- 3.Campelo LD, Camara JR. Flapless implant surgery: A 10-year clinical retrospective analysis. Int J Oral Maxillofac Implants. 2002;17:271–6. [PubMed] [Google Scholar]
- 4.Gomez-Roman G. Influence of flap design on peri-implant interproximal crestal bone loss around single-tooth implants. Int J Oral Maxillofac Implants. 2001;16:61–7. [PubMed] [Google Scholar]
- 5.Van der Zee E, Oosterveld P, Van Waas MA. Effect of GBR and fixture installation on gingiva and bone levels at adjacent teeth. Clin Oral Implants Res. 2004;15:62–5. doi: 10.1111/j.1600-0501.2004.01005.x. [DOI] [PubMed] [Google Scholar]
- 6.Ozan O, Turkyilmaz I, Yilmaz B. A preliminary report of patients treated with early loaded implants using computerized tomography-guided surgical stents: Flapless versus conventional flapped surgery. J Oral Rehabil. 2007;34:835–40. doi: 10.1111/j.1365-2842.2007.01772.x. [DOI] [PubMed] [Google Scholar]
- 7.Cannizzaro G, Felice P, Leone M, Checchi V, Esposito M. Flapless versus open flap implant surgery in partially edentulous patients subjected to immediate loading: 1-year results from a split-mouth randomised controlled trial. Eur J Oral Implantol. 2011;4:177–88. [PubMed] [Google Scholar]
- 8.Meizi E, Meir M, Laster Z. New-design dental implants: A 1-year prospesctive clinical study of 344 consecutively placed implants comparing immediate loading versus delayed loading and flapless versus full thickness flap. Quintessence Int Pub. 2014;29:e14–21. doi: 10.11607/jomi.te37. [DOI] [PubMed] [Google Scholar]
- 9.Branemark PL, Hansson BO, Adell R. Osseointegrated implants in the treatment of edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg. 1977;2:1–13. [PubMed] [Google Scholar]
- 10.Gotfredson K, Hjorting-Hansen E. Histologic and histomorphometric evaluation of submerged and non-submerged titanium implants. In: Laney WR, Tolman DE, editors. Tissue Integration in Oral, Orthopedic and Maxillofacial Reconstruction Quintessence. Chicago: Mansa STM Publishers; 1990. pp. 31–40. [Google Scholar]
- 11.Zhu Y, Zheng X, Zeng G, Xu Y, Qu X, Zhu M, et al. Clinical efficacy of early loading versus conventional loading of dental implants. Sci Rep. 2015;5:15995. doi: 10.1038/srep15995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kwon JY, Kim YS, Kim CW. Assessing changes of peri-implant bone using digital subtraction radiography. J Korean Acad Prosthodont. 2001;39:273–80. [Google Scholar]
- 13.Papaspyridakos P, Chen CJ, Singh M, Weber HP, Gallucci GO. Success criteria in implant dentistry: A systematic review. J Dent Res. 2012;91:242–8. doi: 10.1177/0022034511431252. [DOI] [PubMed] [Google Scholar]
- 14.Sclar AG. Guidelines for flapless surgery. J Oral Maxillofac Surg. 2007;65:20–32. doi: 10.1016/j.joms.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 15.Al-Juboori MJ, Ab Rahman S, Hassan A, Bin Ismail IH, Tawfiq OF. What is the effect of initial implant position on the crestal bone level in flap and flapless technique during healing period? J Periodontal Implant Sci. 2013;43:153–9. doi: 10.5051/jpis.2013.43.4.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Romero-Ruiz MM, Mosquera-Perez R, Gutierrez-Perez JL, Torres-Lagares D. Flapless implant surgery: A review of the literature and 3 case reports. J Clin Exp Dent. 2015;7:e146–52. doi: 10.4317/jced.51985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sennerby L, Rocci A, Becker W, Jonsson L, Johansson LA, Albrektsson T. Short-term clinical results of Nobel direct implants: A retrospective multicentre analysis. Clin Oral Implants Res. 2008;19:219–26. doi: 10.1111/j.1600-0501.2007.01410.x. [DOI] [PubMed] [Google Scholar]
- 18.Becker W, Goldstein M, Becker BE, Sennerby L. Minimally invasive flapless implant surgery: A prospective multicenter study. Clin Implant Dent Relat Res. 2005;7(Suppl 1):S21–7. doi: 10.1111/j.1708-8208.2005.tb00071.x. [DOI] [PubMed] [Google Scholar]
- 19.Flanagan D. Flapless dental implant placement. J Oral Implantol. 2007;33:75. doi: 10.1563/0.797.1. [DOI] [PubMed] [Google Scholar]
- 20.Kan JY, Rungcharassaeng K, Ojano M, Goodacre CJ. Flapless anterior implant surgery: A surgical and prosthodontic rationale. Pract Periodontics Aesthet Dent. 2000;12:467–74. [PubMed] [Google Scholar]
- 21.Xu L, Wang X, Zhang Q, Yang W, Zhu W, Zhao K. Immediate versus early loading of flapless placed dental implants: A systematic review. J Prosthet Dent. 2014;112:760–9. doi: 10.1016/j.prosdent.2014.01.026. [DOI] [PubMed] [Google Scholar]
- 22.Cochran DL, Buser D, Ten Bruggenkate CM, Weingart D, Taylor TM, Bernard JP, et al. The use of reduced healing times on ITI implants with a sandblasted and acid-etched (SLA) surface: Early results from clinical trials on ITI SLA implants. Clin Oral Implants Res. 2002;13:144–53. doi: 10.1034/j.1600-0501.2002.130204.x. [DOI] [PubMed] [Google Scholar]
- 23.Nordin T, Nilsson R, Frykholm A, Hallman M. A 3-arm study of early loading of rough-surfaced implants in the completely edentulous maxilla and in the edentulous posterior maxilla and mandible: Results after 1 year of loading. Int J Oral Maxillofac Implants. 2004;19:880–6. [PubMed] [Google Scholar]
- 24.Jeong SM, Choi BH, Kim J, Xuan F, Lee DH, Mo DY, et al. A 1-year prospective clinical study of soft tissue conditions and marginal bone changes around dental implants after flapless implant surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:41–6. doi: 10.1016/j.tripleo.2010.03.037. [DOI] [PubMed] [Google Scholar]


