Abstract
Aim:
The aim of this study was to evaluate the efficacy of various routinely used analgesics in the management of pulpal pain preoperatively.
Materials and Methods:
A total of 150 patients were randomly selected and divided into five groups each. At initial visit, a self-administered questionnaire was given, and patients were asked to mark on the Visual Analog Scale (VAS) indicating severity of pain at that moment which is taken as a pretreatment VAS score. Group I patients received aceclofenac + paracetamol, Group II: ketorolac tromethamine, Group III: lornoxicam + paracetamol, Group IV: tramadol + paracetamol, and Group V: paracetamol. All the patients are requested to record their pain levels at 4 h, 6 h, 8 h, 24 h, and 48 h by means of VAS scores before and after treatment.
Results:
There was no significant decrease in frequency of pain when compared in the first three groups, whereas in Group III and Group IV, the patients experienced an effective reduction in pain because of sustained releasing ability of these drugs. Overall, there was no statistically significant differences among all the groups.
Conclusion:
This study suggests that there was no significant difference in reduction of pain preoperatively. However, lornoxicam + paracetamol and tramadol + paracetamol were effective because of their sustained releasing ability. Ketorolac was effective to reduce the pain for shorter duration. Paracetamol can be advised in compromised patients where safety is concerned.
KEYWORDS: Analgesic time of total pain relief, pain, pulpitis, time of onset of action (tooad) of drug
INTRODUCTION
Pain is the most common problem for which patients seek dental treatment. Pulpitis is the most common cause of odontogenic pain and can be divided into two categories: reversible and irreversible. Reversible pulpitis indicates that pulpal tissues can repair with the removal of the local irritant and restoration of the tooth structure. Irreversible pulpitis has a prolonged duration of pain when stimulated but may also occur spontaneously. The quality of pain may vary based on the vitality of the tooth as well as the extent of inflammation. Following prolonged periods of inflammation, pulpal necrosis may occur. Postoperative pain is an acute type of pain that begins with surgical trauma and gradually decreases with tissue healing,[1,2,3,4,5] whereas in pulpitis, pain is felt due to pressure on walls of tooth rather than inflammatory mediators. Hence, nonsteroidal anti-inflammatory drugs (NSAIDs) which have more analgesic efficacy rather than anti-inflammatory might prove more efficient for pulpitis. There are various pain assessment scales such as Numeric Pain Rating Scale, Wong–Baker FACES Pain Rating Scale, Visual Analog Scale (VAS), and Heft–Parker Scale.
As there are many studies on efficacy of analgesics over post operative pain in endodontics and surgery and very few studies in preoperative pulpal pain. This study is carried out to evaluate the analgesic efficacy of aceclofenac+ paracetamol, lornoxicam+ paracetamol, tramadol+ paracetamol, ketorolac, and paracetamol 650 in management of pulpal pain. This study is planned to compare the analgesic efficacy and their tolerability.[6,7,8,9,10]
MATERIALS AND METHODS
In this study, 150 patients were randomly selected from outpatient attending a private dental college. In this study, patients who came with a complaint of pain and subsequently diagnosed as suffering with irreversible pulpits based on the criteria given below were selected:
Inclusion criteria: Irreversible pulpitis with dull, chronic persistent, and with spontaneous acute pain episodes. Exclusion criteria for this study includes Patients below 18 years of age, pregnancy women, patients with periapical lesions, patients who are asthmatic, patients with gastrointestinal tract problems, patients with known allergic to drugs, and patients on local remedies, previous analgesic intake, and antibiotics for same or other.
Criteria for irreversible pulpitis
Teeth with spontaneous pain, teeth with clinical/radiological pulpal involvement with dental caries, and vital teeth (vitality confirmed by electric pulp testing and thermal testing)
Teeth with clinically no detectable swelling indicating any periapical lesion
Teeth those are not extruded, not tender on percussion, and no pain on vertical pressure
Intraoral periapical (IOPA) revealing any periapical pathologies and discontinuity in the lamina dura were excluded.
The instruction sheet given to the patient consists of a scale rating from 1–10. The pain intensity levels are recorded at 2 h, 4 h, 6 h, 8 h, 24 h, and 48 h, respectively. During the study period, the patients are instructed to avoid taking aggravating factors, for example, cold, hot, and hard food items. Patient consent for this was taken as enclosed in annexure no.
The patients were instructed to discontinue the medication in case of any allergic reactions and call the emergency mobile number given to them. They were explained about this scale in detailed as enclosed in annexure no.
Visual Analog Scale
At initial visit, a self-administered questionnaire was given and patients were asked to mark on the VAS indicating severity of pain at that moment which is taken as a pretreatment VAS score. Average frequency of pain experienced from past 2-3 days is taken as frequency of pain per day before medication. The electric pulp vitality test and thermal test was carried out to diagnose the status of pulp, and IOPA radiographs were taken to rule out any periapical pathologies. Patients with moderate or severe pain were randomly assigned to different groups of drugs, to administer drugs such as aceclofenac (100 mg) + paracetamol (500 mg), ketorolac (10 mg), tramadol (37.5 mg) + paracetamol (325 mg), lornoxicam (8 mg) + paracetamol (500 mg), and paracetamol 650 mg.
After marking severity of pain on VAS, patients were given any one of the above medications and included in that particular group. They were made to sit in the department for 2 h. Patients were instructed to inform immediately after slight reduction in pain which indicates the time of onset of action of drug. Then, they were also instructed to note the time of complete disappearance of pain, and if there was no complete disappearance of pain even after 4 h, the time at which maximum relief from pain occurs is taken as time of total pain relief which indicates peak effect of the drug.
Patients are followed by telephone to record the VAS scores. All the patients were requested to record their pain levels at 4 h, 6 h, 8 h, 24 h, and 48 h. Their frequency of pain relief and tolerability were also analyzed. The comparison was done both inter- and intragroups between mean VAS scores and expressed in mean ± standard deviation. Then, the data were pooled and analyzed. One-way analysis of variance was applied for which the P value was set as 0.05. Post hoc analysis was also done using Tukey's test. Pearson's Chi-square test was used for overall assessment of frequency and tolerability, and P < 0.001 is considered statistically significant. The tolerability of drugs was assessed with review of questionnaire and case history pro forma which were enclosed in the annexure no.
RESULTS
There was no significant difference in pretreatment mean VAS scores in different groups where P = 0.24. There was a significant difference in mean VAS scores at 2 h, 4 h, 6 h, 24 h, and 48 h among all the groups as shown by P = 0.00 and 0.001. There was no significant difference in mean VAS scores at 8 h in all the groups as shown by P = 0.156 [Figures 1, 2 and Table 1].
Figure 1.
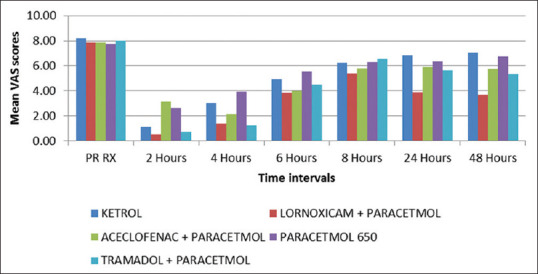
Mean Visual Analog Scale scores before and after medication in all the drug groups
Figure 2.
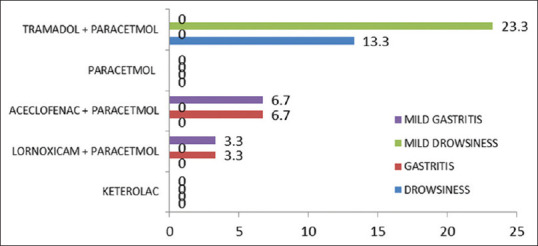
Comparison of tolerability between the drug groups
Table 1.
Comparison of frequency of pain during treatment in all groups
| Groups | Total | χ2 | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Ketorolac | Lornoxicam+ paracetamol | Aceclofenac+ paracetamol | Paracetamol | Tramadol+ paracetamol | |||
| Frequency after, n (%) | |||||||
| 1-2 | 10 (33.30) | 26 (86.70) | 4 (13.30) | 6 (20.00) | 26 (86.70) | 72 (48.00) | 119.871*** |
| 2-3 | 16 (53.30) | 3 (10.00) | 1 (3.30) | 8 (26.70) | 2 (6.70) | 30 (20.00) | |
| 3-4 | 4 (13.30) | 1 (3.30) | 15 (50.00) | 15 (50.00) | 2 (6.70) | 37 (24.70) | |
| 4-5 | 0 | 0 | 8 (26.70) | 1 (3.30) | 0 | 9 (6.00) | |
| 5-6 | 0 | 0 | 2 (6.70) | 0 | 0 | 2 (1.30) | |
| Total, n (%) | 30 (100.00) | 30 (100.00) | 30 (100.00) | 30 (100.00) | 30 (100.00) | 150 (100.00) | |
Difference in mean VAS scores when compared to pretreatment and during different time intervals was statically significant with P = 0.00.
DISCUSSION
In the present study, a total of 150 patients were enrolled with a mean age of 29.5 years which suggested that symptomatic pulpitis occurred more commonly in young adults. The results of this study showed a faster onset of action in the lornoxicam + paracetamol group when compared to other drug groups. It indicates the peak plasma concentration of the drug. Barden et al. in their systematic review on relative efficacy of analgesics after the third molar extraction used time taken to get at 50% maximum pain relief as time course of the total pain relief. It has the benefit of being intuitively meaningful to patients and professionals as well as being measurable.[4] This study showed an increase in mean VAS scores at 8 h among all the groups indicating the time for remedication. This was because that all the mean VAS scores were taken before the next dose. However, the VAS scores of lornoxicam + paracetamol and aceclofenac + paracetamol were relatively less compared to other groups. Galani Varsha et al. compared the efficacy and tolerability of lornoxicam and diclofenac sodium in patients with acute postoperative pain after spinal surgery.[6] They concluded lornoxicam as a better alternative for diclofenac in acute postoperative after spinal surgery. Das et al. assessed the efficacy and safety of lornoxicam as analgesic after surgery on the head and neck in comparison to tramadol.[6,7,8,9,10] This study showed the aceclofenac + paracetamol group with significant pain relief till 4 h; again, there is an increase in VAS score at the 6th- and at 8th-h time period. This is in par with the pharmacokinetics of aceclofenac which will have duration of action for only 4–6 h. However, when compared to pretreatment VAS, it has reduced pain better than in the ketorolac and paracetamol drug group at 48-h time period. Cliff Ong et al. preformed a systematic literature paracetamol/NSAID combinations versus paracetamol or NSAIDs.[9,10] In our study, tramadol + paracetamol showed a marked reduction in pain in the first 6 h. Though, the duration of action of tramadol is only 3.5-4 hrs when combined with paracetamol its action is prolonged to 6 hrs. At 8-h interval, there was again increase in pain before the next dose of drug.
In the present study, the number of patients with 3–4 times frequency was 16, and after treatment also, there were 15 in that frequency group. This shows that there was no significant difference for frequency of pain relief in the ketorolac drug group as shown by Chi-square value of 4.766. This study showed a significant decrease in frequency of pain after medication with lornoxicam + paracetamol. 23.3% of patients had 4–5 times of pain before medication. They were no patients with 4–5 times frequency after medication. Forty percent of patients had 3–4 times frequency before medication, and only 3.3% of patients had 3–4 times frequency after medication. Twenty-six percent of patients had only 1–2 times frequency after medication. However, the change in frequency of pain for lornoxicam + paracetamol before and after medication was statistically significant (Chi-square = 31.533***). Our study showed a decrease in frequency of pain for paracetamol which was taken t.i.d. 40% of patients had 3–4 times and 3.3% had 1–2 times before medication. 13.3% of patients had 3–4 times and 33.3% had 1–2 times after medication. Ong et al. study a systematic review on analgesic efficacy of acute postoperative pain concluded a combination of paracetamol and an NSAID may offer superior analgesia compared with either drug alone.[8,9]
This study showed a concurrent result with previous studies of tramadol.[10,11,12,13,14] In this study, aceclofenac + paracetamol also showed efficacy less than lornoxicam + paracetamol and tramadol + paracetamol but with better efficacy than ketorolac.
Komali et al. conducted a study for comparing analgesic efficacy of diclofenac sodium with ibuprofen. The time to peak effect of ibuprofen was early compared to that of diclofenac sodium.[13]
This study showed that paracetamol can be used as an alternative to NSAIDs in high-risk patients, especially because of low incidence of adverse effects. This is in accordance with Dhusia HL et al. who performed a study to evaluate whether the combination of diclofenac 50 mg and paracetamol 500 mg (Dynapar tablets) twice daily regimen offers superior analgesia than thrice daily regimen of ibuprofen 400 mg tablet in management of dental pain following impacted third molar extraction.[13,14]
CONCLUSION
There was no significant decrease in frequency of pain after ketorolac/aceclofenac + paracetamol. Paracetamol can be advised in compromised patients where safety is concerned as an alternative analgesic to NSAIDs. Lornoxicam + paracetamol is effective with sustain, fast onset of action, and total pain relief when compared to drugs of this study. Patient experienced only 3.3% of gastric irritation which can be reduced by with use of proton pump inhibitors before NSAIDS administration. Tramadol + paracetamol was next to lornoxicam + paracetamol in the efficacy but with drowsiness in 36.6% of patients. This could be an alternative NSAIDs when they are contraindicated.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ingle JI, Dudley H. Glick Differential Diagnosis and Treatment of Dental Pain (Text Book of Ingle) ISBN-10: 1607951924. [Google Scholar]
- 2.Anand KJ, Craig KD. New perspectives on the definition of pain. Pain. 1996;67:3–6. doi: 10.1016/0304-3959(96)03135-1. [DOI] [PubMed] [Google Scholar]
- 3.Balasubramaniam R, Turner LN, Fischer D, Klasser GD, Okeson JP. Non-odontogenic toothache revisited. Open J Stomatology. 2011;1:92–102. [Google Scholar]
- 4.Barden J, Edwards JE, McQuay HJ, Wiffen PJ, Moore RA. Relative efficacy of oral analgesics after third molar extraction. Br Dent J. 2004;197:407–11. doi: 10.1038/sj.bdj.4811721. [DOI] [PubMed] [Google Scholar]
- 5.Hyllested M, Jones S, Pedersen JL, Kehlet H. Comparative effect of paracetamol, NSAIDs or their combination in postoperative pain management: A qualitative review. Br J Anaesth. 2002;88:199–214. doi: 10.1093/bja/88.2.199. [DOI] [PubMed] [Google Scholar]
- 6.Varsha GJ, Nimesh AP, Dave BR, Krishnan A. A comparison of the efficacy and tolerability of lornoxicam and diclofenac sodium in patients with acute postoperative pain after spinal surgery. Am J Phytomed Clin Ther. 2013;1:507–15. [Google Scholar]
- 7.Das SK, Banerjee M, Mondal S, Ghosh B, Ghosh B, Sen S. A comparative study of efficacy and safety of lornoxicam versus tramadol as analgesics after surgery on head and neck. Indian J Otolaryngol Head Neck Surg. 2013;65(Suppl 1):126–30. doi: 10.1007/s12070-013-0617-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ong CK, Seymour RA, Lirk P, Merry AF. Combining paracetamol (Acetaminophen) with nonsteroidal anti-inflammatory drugs: A qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg. 2010;110:1170–9. doi: 10.1213/ANE.0b013e3181cf9281. [DOI] [PubMed] [Google Scholar]
- 9.Ramasamy N, Gopal V, Kumar K. Paracetamol and its combinations in India – An overview. Int Journal of Res Pharm Nano Sci. 2013;2:581–5. [Google Scholar]
- 10.Medve RA, Wang J, Karim R. A scientific report. Tramadol and acetaminophen tablets for dental pain. Anesth Prog. 2001;48:79–81. [PMC free article] [PubMed] [Google Scholar]
- 11.Shaik MM, Kumar J, Mobina S, Satyanarayana N, Sunitha P. Comparative study of tramadol and ketorolac in the pain management of third molar tooth extraction. J Coll Med Sci. 2010;6:135–43. [Google Scholar]
- 12.Komali G. A study of analgesic efficacy of ibuprofen and diclofenac sodium in acute pulpitis patients. J Res Adv Dent. 2014;3:49–54. [Google Scholar]
- 13.Dhusia HL, Bhange PD, Sonar MD, Maroo SH, Patel KR, Ojha RU. Combination of diclofenac with paracetamol offer better pain relief than ibuprofen alone in impacted third molar extraction: A randomized controlled Trial. Int J Res Med. 2013;2:109–14. [Google Scholar]
- 14.Mishra H, Khan FA. A double-blind, placebo-controlled randomized comparison of pre and postoperative administration of ketorolac and tramadol for dental extraction pain. J Anaesthesiol Clin Pharmacol. 2012;28:221–5. doi: 10.4103/0970-9185.94892. [DOI] [PMC free article] [PubMed] [Google Scholar]


