Abstract
Background
Knee instability can arise from various causes and conditions such as neuromuscular disease, central nervous system conditions, and trauma. For people with knee instability, knee orthosis devices are prescribed to help with standing, walking, and performing tasks. We conducted a health technology assessment of stance-control knee–ankle–foot orthoses (SCKAFOs) for people with knee instability, which included an evaluation of the effectiveness, safety, and budget impact of publicly funding SCKAFOs, as well as patient preferences and values.
Methods
We performed a systematic literature search of the clinical evidence. We assessed the risk of bias of each included study using the Risk of Bias in Nonrandomized Studies (RoBANS) tool and the quality of the body of evidence according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Working Group criteria. We performed a systematic economic literature search and also analyzed the budget impact of publicly funding SCKAFOs in people with knee instabilities in Ontario. We did not conduct a primary economic evaluation as there was limited comparative clinical evidence to inform an economic model. Our reference case budget impact analysis was done from the perspective of the Ontario Ministry of Health; it compared the total costs of a basic mechanical SCKAFO and locked KAFO (LKAFO) for people with knee instability. We also performed scenario analyses varying the following parameters: the price of all classes of SCKAFO (mechanical, electronic, and microprocessor), and the uptake of SCKAFO. To contextualize the potential value of SCKAFO, we spoke with people with knee instability.
Results
We included four studies in the clinical evidence review. We are uncertain if SCKAFOs improve walking ability, energy consumption, or activities of daily living compared with LKAFOs (GRADE: Very low). Our economic evidence review identified one costing analysis that suggested that the costs of orthotic devices such as LKAFOs and SCKAFOs are highly variable according to the cost of materials, professional time, and customization required by the individual patient. The budget impact of publicly funding mechanical SCKAFOs in Ontario over the next 5 years (at a full device cost of $10,784) ranged from an additional $0.50 million in year 1 (at an uptake rate of 30% in the target population [429 eligible people]) to $0.83 million in year 5 (at an uptake rate of 50%), with a total budget impact of $3.34 million over 5 years. We found that the greatest increase in budget impact in the scenario analysis came from the microprocessor SCKAFO device, which had an additional cost of $10.07 million in year 1, increasing to $16.78 million in year 5. When we decreased the cost of a mechanical SCKAFO device (to $7,384), this reduced the 5-year budget impact to $0.89 million (vs. $3.34 million in the reference case). The people with knee instability with whom we spoke reported that they preferred a device that would provide a more typical gait, but starting with this type of device would be easier than switching from an existing LKAFO.
Conclusions
We are uncertain if SCKAFOs improve walking ability, reduce energy consumption, or improve activities of daily living compared with LKAFOs. We estimate that the additional cost to provide public funding for a mechanical SCKAFO in people with knee instability would range from about $0.50 million in year 1 to $0.83 million in year 5, yielding a total budget impact of $3.34 million over 5 years. Depending on the class of SCKAFO and the uptake rate for the device, the budget impact may vary. People who met the criteria for the use of a SCKAFO did have a strong preference for it over an LKAFO.
Objective
This health technology assessment evaluates the effectiveness, safety, and cost-effectiveness of stance-control knee–ankle–foot orthoses for people with knee instability. It also evaluates the budget impact of publicly funding stance-control knee–ankle–foot orthoses and the experiences, preferences, and values of people with knee instability.
Background
Health Condition
Knee instability may occur in any of the three anatomical planes of the knee: sagittal, coronal, and transverse.1 The knee extensors are the muscle groups that have a direct effect on knee stability.2 The knee extensors comprise the quadriceps femoris, tensor fasciae latae, and the knee flexors, which include the hamstring group – sartorius, gracilis, and gastrocnemius. Another mechanism that may contribute to knee instability is overactivity remote from the muscles directly affecting the knee. This can be a secondary cause of improper posture.2 Lack of proprioception (sense of self-movement and body position) can also lead to loss of ability to grade movement or sense movement direction. Lastly, spasticity in the muscles acting around the knee can cause knee instability.
Other conditions or injuries affecting the neural supply to these muscles or the proprioceptive feedback of the knee itself could also result in instability. Other morphological abnormalities or injuries to the osseous, ligamentous, and cartilaginous structures of the knee can also adversely affect knee stability.
Overall, the stability of the knee is reliant on the sound inert structures, as well as on intact nervous and functioning muscular systems, that surround the knee. Any adverse changes to these systems and structures can cause muscle weakness and/or changes in biomechanical functioning, which can lead to pain, falls, and a range of mobility issues.2 People with knee instability may walk with a laboured, unsafe gait that can cause fatigue due to the increased energy demands, as well as injuries to the ankle, hip or back from overuse or misuse of the knee and potentially early osteoarthritis.
Clinical Need and Target Population
Several conditions, including neuromuscular disease (NMD) and central nervous system conditions, can lead to knee instability, which are described below.
Neuromuscular disease describes a heterogenous group of conditions (over 150 types) that primarily affect peripheral nerve, muscle, and/or neuromuscular junction.2 Among the NMDs that can cause knee extensor weakness are motor neuron disease, muscular dystrophy, myasthenia gravis, spinal muscular atrophy, poliomyelitis, myopathies, and inclusion body myositis.3 When defining neuromuscular conditions more broadly, they can encompass upper motor neuron conditions that have a common end point of affecting muscle function. All neuromuscular diseases are considered rare or “orphan” diseases. For example, the age- and sex-adjusted incidence of motor neuron disease (which includes spinal muscular atrophy) in Ontario in 2010/11 was 0.024 per 1,000 persons. The crude prevalence in 2010/11 of motor neuron disease for persons aged 0–17, 18–64, and 65 and older was 0.029, 0.052, and 0.254 per 1,000 persons, respectively.4
Central nervous system conditions can cause weakness and/or spasticity in the muscles around the knee, leading to instability and loss of sensation and proprioception in that limb. Conditions include vascular disorders such as stroke, infections such as polio, and structural disorders such as spinal cord injury and peripheral neuropathy.5 The annual age-adjusted incidence rates in Canada for traumatic spinal cord injury was 42.4 and 51.4 per million for people aged 15–64 and 65 and older, respectively.6 The 2010/11 Canadian Community Health Survey3 estimated that approximately 319,000 people were experiencing the effects of stroke, and 118,000 people were living with spinal cord injury. There are currently no national level data in Canada to estimate the number of individuals living with many neurological conditions (e.g., neuromuscular diseases and central nervous system conditions described above).4 Without these relevant data, it is difficult to provide estimates on the needs of this population.
Trauma, such as peripheral nerve injury, peripheral neuropathy, and femoral nerve trauma, and complications from surgery (including from abdominal, hip, and pelvic surgeries) can also lead to knee instability.
Current Treatment Options
A knee–ankle–foot orthosis device is usually prescribed when an ankle–foot orthosis or knee orthosis is insufficient to adequately control knee instability or when control in more than one plane is required.1 Formerly, locked KAFOs (LKAFOs) were made with bulkier materials, such as metal and leather, but modern LKAFOs are made from lighter materials such as thermoplastics or carbon fibre composites, which fit more closely, potentially affording better control of the limb compared with earlier versions of LKAFOs. The LKAFO is custom-made by an orthotist, with some parts (e.g., the knee joint) coming from a medical equipment manufacturer or through central fabrication (made by a manufacturer). Conventional LKAFOs are currently the standard of care in Ontario and they are listed in the Assistive Devices Program (ADP) manual7 (i.e., they are eligible for public funding).
The prescription of an LKAFO is reliant on a person's clinical presentation rather than their diagnosis. Indications for an LKAFO include knee and/or hip flexion contracture up to 20 degrees, and unilateral or bilateral legs with paralysis. Contraindications include knee and/or hip flexion contracture greater than 20 degrees and non-reducible, moderate to severe spasticity and hip abductor strength less than grade 3 (measured on a 0–5 scale, with 0 representing no muscle contraction and 5 representing typical strength).
Conventional LKAFOs provide the wearer with stability while walking by locking the knee joint in a fully extended position during both stance (standing) and swing (moving the leg forward to step) phases. They can be manually unlocked for sitting. LKAFOs require considerable energy consumption as they encourage an atypical gait pattern, such as circumduction (the movement of the leg in a circular manner), hip swinging, and vaulting during gait.8–10 These difficulties can lead to activity avoidance and early onset osteoarthritis in the lower back, opposite hip, knee, and shoulders in wearers who also require a walker or forearm crutches.
Health Technology Under Review
Stance-control KAFOs (SCKAFOs), also known as stance control orthoses, are a newer generation of KAFO that have been developed to prevent knee flexion during the stance phase and permit free knee motion during the swing phase of the wearer's gait.11 By allowing the knee to bend during the swing phase, the SCKAFO provides a more typical gait pattern than with the conventional LKAFO (current standard of care). Patients can walk with much less effort and reduce compensation from other muscle groups. There are three types of SCKAFO that operate in different ways:
Mechanical devices can work in two ways: a system that uses ankle movement to unlock/release during the swing phase or a pendulum system to activate the mechanism that allows a knee joint to be locked and unlocked at specific moments in the user's gait relative to the positioning/angulation of the leg in gait and stance. These devices require a certain range of motion and/or residual function of the ankle and generally cannot accommodate leg-axis deviations more than 10 degrees (varus/valgus—leg bends in the outward or inward direction), knee flexion contractures, or unstable gait patterns. The device can be made for the user by the manufacturer, or it can be fully custom-made in an orthotic clinic (with some parts, such as knee joints, coming from the manufacturer)
Electronic devices are gait activated. They will unlock/release the knee joint based on the position of the leg during the gait cycle. Position sensor–activated devices are one example, where the orthotic knee is locked for the stance phase and unlocked at the end of the stance, when it reaches a pre-set angle relative to the ground or hip of the wearer.12 These devices do not depend on ankle range of motion function and can accommodate leg axis deviations, knee flexion contractures, and, to a certain extent, unstable gait patterns. These devices are generally made for the user by the manufacturer or fully custom-made in an orthotic clinic (with some parts, such as knee joints, coming from the manufacturer)
Advances in electronic devices have made possible microprocessor devices, which are the most complex of the SCKAFOs. The microprocessor technology unlocks/releases based on information received from electronic sensors 100 times per second. It is designed with a carbon fiber strut with integrated ankle movement sensor and a monocentric (single pivot) microprocessor-controlled knee joint. A knee angle sensor provides feedback on knee angle and knee angle velocity. Extension and flexion damping are adjusted at a frequency of 50 Hz by a microprocessor with the ankle movement, the knee angle, the knee angle velocity, and the temperature of the hydraulic as input signals.12 These devices are fully custom-made by the manufacturer
As stated above, indications and contraindications for the use of SCKAFOs are based on the physical presentation of the patient. Table 1 presents a list of indications and contraindications for the use of SCKAFOs, provided by one manufacturer.13
Table 1:
Indications and Contraindications of Stance-Control Knee–Ankle–Foot Orthoses
| Indications | Contraindications |
|---|---|
| Able to fully stabilize the torso and stand freely | Knee or hip flexion contraction > 10 degrees |
| Muscle strength of hip extensors and flexors must permit the controlled swing-through of the affected leg | Genu varum or valguma > 10 degrees |
| Hip muscle strength or compensatory motion must be possible to advance limb | Bilateral user: hip abductor strength 0–3b |
| Successful evaluation with diagnostic trial tool | Leg length discrepancy ≥ 6 inches (15 cm) Body weight > 275 pounds |
Genu varum is characterized by outward bowing of the knee (bow-legged). Genu valgum is a condition in which the knees angle in and touch each other when the legs are straightened (knock-knee).
Rated on a 0–5 scale, with 0 representing no muscle contraction and 5 representing typical strength.
Additional concerns for the use of SCKAFOs include uncontrolled spasticity, progressive worsening of neurological diseases, patients lacking motivation to increase mobility, and diminished cognition. The inability to release spasticity, especially in knee extensors, would also be a barrier to use. Also important is sufficient hip flexor strength, which is necessary to create the swing phase of gait.
Regulatory Information
Locked knee–ankle–foot orthoses and SCKAFOs are Class I devices14 and therefore do not need Health Canada approval. There are a few manufacturers that produce SCKAFOs that are available in Ontario. Below is a list of manufacturers and SCKAFOs:
Table 2:
Manufacturers and Type of SCKAFO and LKAFO Available in Ontario
| Manufacturer | SCKAFO (Type of Device) | LKAFO |
|---|---|---|
| Ottobock | Free Walk (mechanical) E-MAG Active (electronic) C-Brace (microprocessor) |
These three manufacturers all produce a full line of LKAFO knee joint components. Each manufacturer has two lines of knee joints for LKAFOs with several options within each category: 1. Free motion knee joints include single axis, off set, and polycentric 2. Locking knee joints include drop lock, spring assist locking, ratchet lock, and bale lock |
| Becker | SafetyStride (mechanical) FullStride (mechanical) Stride4 (mechanical) UTX (mechanical) |
|
| Fillauer | Swing Phase Lock II (mechanical) |
Abbreviations: LKAFO, locked knee–ankle–foot orthosis device; SCKAFO, stance-control KAFO.
Ontario and Canadian Context
Locked knee–ankle–foot orthoses are publicly funded by the Ontario Ministry of Health, through the ADP. This funding pays for 75% of the cost of the device (100% for those with social assistance benefits, such as the Ontario Disability Support Program).15 However, the ADP has maximum list prices for each individual procedure and component code, and approved orthotists are not permitted to bill more than the approved list price. Eligibility for LKAFOs includes long-term physical disability or a physical condition that requires the use of an orthotic device for 6 months or longer to improve function in daily activities. The ADP does not provide funding for prefabricated or centrally fabricated orthoses (i.e., made by the manufacturer), backup devices (i.e., a device that can be used if the primary device stops functioning properly), or SCKAFOs.
We are aware of one province in Canada (Alberta) that publicly funds one SCKAFO (the Free Walk – mechanical, by Ottobock) and two SCKAFO knee joints (the Swing Phase Lock II – mechanical, by Fillauer, and the Horton Stance Phase, which is currently unavailable in Ontario).16 In October 2020, Quebec approved funding for the C-Brace-microprocessor by Ottobock on a case-by-case basis.
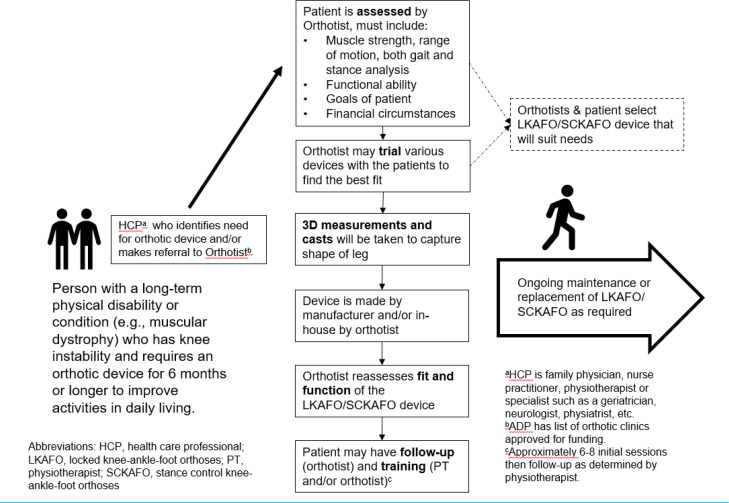
Clinical Pathway
In Ontario, the first stage of the clinical pathway involves the patient presenting with knee instability to their primary health care professional (HCP). If they meet the appropriate criteria (outlined in Figure 1), the HCP will prescribe a knee orthosis and refer the patient to an orthotist. The orthotist uses clinical judgement informed by an evaluation of the patient when choosing the appropriate knee orthosis such as an LKAFO or SCKAFO. Through shared decision-making, including consideration of affordability and ADP funding, the orthotist, patient, and other team members choose the most appropriate device. Once an LKAFO or SCKAFO, if chosen, has been fitted to the patient properly by the orthotist, a referral will be made to a physiotherapist to assist with training in its use. Below is the clinical pathway for a person seeking an LKAFO or SCKAFO.
Figure 1: Clinical Pathway for People with Knee Instability.
Equity
In Ontario, there are two major factors that can impact access to receiving an LKAFO or SCKAFO: socioeconomic status and place of residence (S. Durno, E. Graham, M.Q. Huangfu, A. Lok, A. Moore, M.C. Thiessen, teleconferences, June and July, 2020).
The first factor is that the ADP covers 75% of approved LKAFOs. The other 25% is covered by the patient (if the patient is on the Ontario Disability Support Program, then 100% of the device is covered up to a maximum amount). This coverage alleviates most cost to the patient; however, as described above, the ADP approves only devices or components of a device that do not exceed their set price per individual procedure and component code.7 Many components are more expensive than the set price, and patients may not be able to afford the cost of the entire device or ongoing device maintenance, in addition to the cost of therapy associated with training.
There are other funding sources a patient can access, such as private health insurance, federal government program funding, and provincial worker compensation programs. Access to physiotherapy for assessment of the need for an orthotic device and specialized training in the use of the device would not meet the eligibility criteria for some publicly funded programs. For example, with the Community Physiotherapy Clinic (CPC) program,17 the population included in this review would be excluded because the CPC addresses acute decline, whereas these patients have a chronic condition that requires ongoing maintenance rather than an acute decline, and because they require specialized services that are not widely available within the program. Local hospital-based outpatient programs may be the only publicly funded access points for physiotherapy because they cover patients over 65 years of age.18 Most extended health benefit programs have limited coverage for physiotherapy services for assessment and treatment.
The second factor is that many appointments are necessary to assess the patient's function, fit, as well as function of the device. Training is also needed for a patient to be successful. When a patient lives in a rural or remote community, or away from a city centre, commuting back and forth may not be an option. Barriers can include the cost of specialized transportation if the patient is attending appointments alone, travel time, and loss of work by their caregiver if the patient needs to be accompanied to their appointments.
Access to an LKAFO or SCKAFO may also be impacted by access to referring primary care provider/specialist, access to orthotist and physiotherapist, ability to maintain device, and support to take on and off device by caregiver (depending on the level of impairment of the patient).
Relevant health equity issues contributing to a differential effect of SCKAFOs in people with knee instability across different populations (place of residence and socioeconomic status) will be reported if information is available in the identified studies.
Previous Systematic Reviews
During the scoping phase of this health technology assessment (HTA), we identified several related systematic reviews.1,2 Their research questions were broader than this HTA, in that they evaluated newer LKAFOs compared with older LKAFOs or no comparator. This HTA focuses on evaluating SCKAFO against conventional LKAFOs or no orthoses. They also included other orthotic devices in their reviews (e.g., ankle-foot orthosis and hip knee-ankle-foot orthosis) that were out of scope for this review. The authors of these systematic reviews found that newer LKAFOs (i.e., those made with carbon materials) performed better than older LKAFOs (i.e., those made with metal and leather19). However, they concluded that there was substantial risk of bias in the included studies. They identified a large gap in the evidence on the effectiveness of LKAFOs for managing knee instability.2 The latest systematic review was published in 2017, so rather than using previous systematic reviews to address our research question, we decided to conduct our own literature search to capture any more recent published literature.
Expert Consultation
We engaged with experts in the specialty areas of orthotics and physiatry, and physiotherapists with expertise in neurorehabilitation to help inform our understanding of aspects of the health technology and our methodologies and to contextualize the evidence.
PROSPERO Registration
This health technology assessment has been registered in PROSPERO, the international prospective register of systematic reviews (CRD42020201805), available at https://www.crd.york.ac.uk/PROSPERO.
Clinical Evidence
Research Question
What are the clinical effectiveness and safety of stance-control knee-ankle-foot orthoses (SCKAFOs) compared with locked knee-ankle-foot orthoses (LKAFOs) or with no LKAFO in people with knee instability due to different causes and conditions?
Methods
Clinical Literature Search
We performed a clinical literature search on July 21, 2020, to retrieve studies published from database inception until the search date. We used the Ovid interface in the following databases: MEDLINE, Embase, the Cochrane Central Register of Controlled Trials, the Cochrane Database of Systematic Reviews, the Health Technology Assessment database, and the National Health Service Economic Evaluation Database (NHS EED). We used the EBSCOhost interface to search the Cumulative Index to Nursing & Allied Health Literature (CINAHL).
A medical librarian developed the search strategies using controlled vocabulary (e.g., Medical Subject Headings) and relevant keywords designed to capture the intervention. We created database auto-alerts in MEDLINE, Embase, and CINAHL and monitored them for the duration of the assessment period (July 2020 to February 2021). We also performed a targeted grey literature search of health technology assessment agency websites as well as clinical trial and systematic review registries. See Appendix 1 for our literature search strategies, including all search terms.
Eligibility Criteria
STUDIES
Inclusion Criteria
English-language full-text publications
Studies published from inception to July 21, 2020
-
Health technology assessments, systematic reviews, randomized controlled trials (RCTs), observational studies (e.g., before and after, comparative cohort or case-series)
○ Studies must have at least five patients
Exclusion Criteria
Editorials, commentaries, case reports, conferences abstracts, letters
Animal and in vitro studies
PARTICIPANTS
Inclusion Criteria
Adults (≥ 18 years) with knee instability due to different conditions and causes (e.g., neuromuscular disorders, spinal cord injury, etc.)
Exclusion Criteria
Healthy volunteers, children and adolescents (< 18 years)
INTERVENTIONS
Inclusion Criteria
Any type of stance-control knee–ankle–foot orthosis (e.g., mechanical, electronic, or microprocessor)
Exclusion Criteria
Other orthoses (e.g., hip KAFO, ankle foot orthosis)
COMPARATOR
Inclusion Criteria
Locked KAFO (LKAFO) or no KAFO (i.e., no assistive device)
Exclusion Criteria
Other orthoses (e.g., hip KAFO, ankle foot orthosis)
OUTCOME MEASURES
Condition-specific or generic patient-reported outcomes measuring physical function, level of independence, level of disability, activities of daily living, or quality of life
Pain (self-reported or measured by standardized scales)
Energy consumption and efficiency (measured by changes in pulse rate and oxygen consumption and/or physiological cost index)
Walking ability (e.g., speed of walking measured by velocity, cadence, etc.)
Adverse effects (e.g., falls, tissue damage)
Patient satisfaction
Resource use (e.g., number of follow-up appointments, device malfunctions, access to physiotherapy)
Literature Screening
A single reviewer conducted an initial screening of titles and abstracts using Covidence20 and then obtained the full texts of studies that appeared eligible for review according to the inclusion criteria. A single reviewer then examined the full-text articles and selected studies eligible for inclusion. A single reviewer also examined reference lists and consulted content experts and manufacturers for any additional relevant studies not identified through the search.
Data Extraction
We extracted relevant data on study characteristics and risk-of-bias items using a data form to collect information on the following:
Source (e.g., citation information, study type)
Methods (e.g., study design, study duration and months, reporting of missing data, relevant baseline characteristics [e.g., diagnosis, age, height, weight, body mass index, experience with LKAFOs/SCKAFOs, hip strength, knee strength and ankle strength, equity variables], reporting of outcomes measures used, whether the study compared two or more groups)
Outcomes (e.g., outcomes measured, number of participants for each outcome, number of participants missing for each outcome, outcome definition and source of information, unit of measurement, upper and lower limits [for scales])
Statistical Analysis
We did not undertake any meta-analyses or subgroup analyses because of the small volume of included studies captured in this review, their small sample sizes, and lack of variables reported associated with the subgroup analyses (e.g., equity variables). We undertook a narrative summary of the evidence and presented results in text and tables.
We used WebPlotDigitizer21 to gather point estimates and standard deviations from graphs where available.
Critical Appraisal of Evidence
We assessed risk of bias of non-randomized studies using the Risk of Bias Assessment tool for Non-randomized Studies (RoBANS)22 (Appendix 2).
We evaluated the quality of the body of evidence for each outcome according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Handbook.23 The body of evidence was assessed based on the following considerations: risk of bias, inconsistency, indirectness, imprecision, and publication bias. The overall rating reflects our certainty in the evidence.
Results
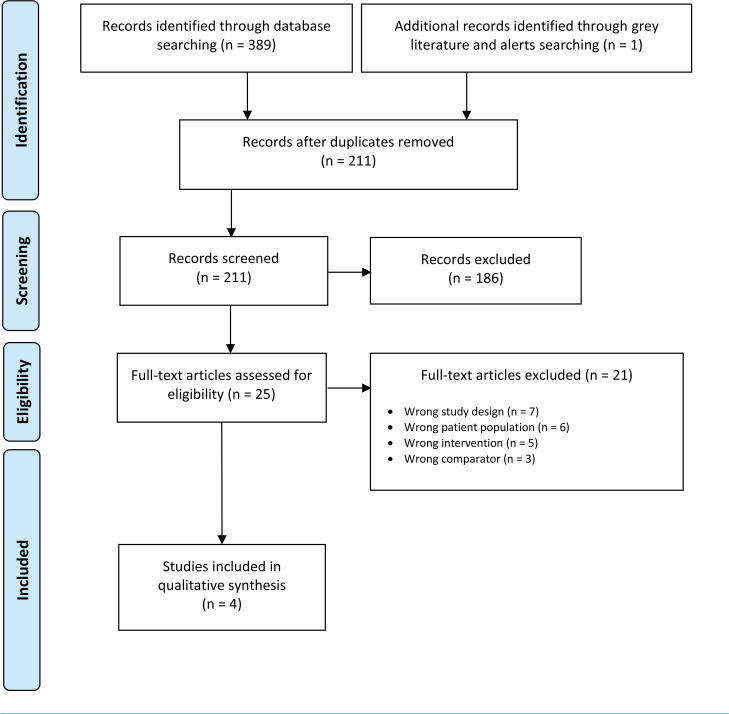
Clinical Literature Search
The database search of the clinical literature yielded 389 citations published from database inception to July 21, 2020. We identified one additional study from the search alert. In total, we identified four studies (before and after designs) that met our inclusion criteria. See Appendix 3 for a list of studies excluded after full-text review. Figure 2 presents the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram for the clinical literature search.
Figure 2: PRISMA Flow Diagram—Clinical Search Strategy.
Source: Adapted from Moher et al.24
Abbreviation: PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-analyses.
Characteristics of Included Studies
Four studies with a before and after design were included.12,25–27 Two studies were conducted in the United States, one in Australia, and one in Germany. The studies were published between 2005 and 2017. Populations included people with various pathologies (e.g., polio, motor neuron disease, inclusion body myositis, incomplete spinal cord injuries, etc.). Previous orthosis experience varied across studies; some people had experience with previous orthoses (e.g., LKAFO, knee brace, posterior offset KAFO), some people had no experience with orthoses, and some used gait aids (e.g., walking sticks, forearm crutches and canes) either in conjunction with orthoses or alone. Where reported, people had between 15 and 28 years of experience with previous orthoses.
Stance-control KAFO (SCKAFO) in the studies included the Dynamic Knee Brace System, Horton Stance Control Knee Joint, SensorWalk, and C-Brace. Two SCKAFOs were mechanical,25,26 one was electronic,27 and one was a microprocessor device.12 Where reported, assessments and fittings took place with orthotists and, in one study, a physiotherapist. Three studies allowed the participants to use the SCKAFO at home for 1–6 months before outcomes were measured and data were collected. The comparator groups were mixed for two studies, so only data comparing SCKAFOs with LKAFOs or no orthoses were collected. The various SCKAFOs were compared to LKAFOs in three studies and no orthoses in one study.
Three studies measured walking ability using metrics such as velocity (cm/sec), cadence (steps/min), and step length (cm). One study measured energy consumption (e.g., oxygen cost, physiological cost index), and one study administered two surveys—one measuring activities of daily living and the other measuring experience with the orthoses. No equity variables were measured in any included studies.
Study and baseline characteristics are reported below in Tables 3 and 4.
Table 3:
Characteristics of Included Studies
| Author, Year, Country | Sample Size | Inclusion Criteria | Intervention and Comparator | Outcomes of Interest |
|---|---|---|---|---|
| Irby et al, 200527 United States | n = 21 | • Primarily dependent on a KAFO for walking and use an orthosis on a daily basis, or does not use an orthosis, but has a collapsing knee that must be stabilized by a hand on the knee and/or forward trunk lean • May use either one or two KAFOs for ambulation • Must require that the KAFO be locked for community ambulation • Must demonstrate ability to walk a minimum of 100 m (crutches or walker can be used, if needed) • Must have sufficient hip flexor strength to advance the limb |
I: Dynamic Knee Brace System C: Locked KAFO |
• Walking ability |
| Davis et al, 201026 Australia | n = 10 | • Regular use of SCO for at least 4 h each day • Able to safely walk (as determined by the treating clinicians) with the knee in stance control mode and in locked mode during clinical consultations • Able to walk a distance of 200 m with the knee in the stance control and locked mode |
I: Horton Stance Control Knee Joint C: Locked KAFO |
• Energy consumption • Walking ability |
| Bernhardt et al, 201125 United States | n = 9 3 lost to follow-up at 6-mo timepoint |
NR | I: SensorWalk C: No orthosis |
• Walking ability |
| Probsting et al, 201712 Germany |
n = 13 (overall sample) n = 5 (included only patients with locked KAFO comparator) |
• Patients used their previous orthoses for at least 6 mo prior to enrollment in the study | I: C-Brace C: Locked KAFO |
• Activities of daily living • Orthosis Evaluation Questionnaire |
Abbreviations: C, comparator; I, intervention; KAFO, knee–ankle–foot orthosis; NR, not reported; SCO, stance control orthoses.
Table 4:
Baseline Characteristics of Patients From Included Studies
| Author, Year | Age (SD) | Height, Weight, and BMI (SD) | Diagnosis | Previous Orthoses, Walking Aids, and Lived Experience | Hip, Knee, and Ankle Strengtha |
|---|---|---|---|---|---|
| Irby et al, 200527 | 53 yr (± 15) Range: 11–76 yr |
Height: NR Weight: 84 kg (± 20) Range: 51–127 kg BMI: 29 ± 6 Range: 19–40 |
Poliomyelitis = 12 Other pathologies or trauma (includes neuropathies, incomplete spinal cord injuries, spina bifida, multiple sclerosis, and muscular dystrophy) = 9 |
Locked KAFO = 13 No assistive = 8 Experience: 28 ± 18 yr Range: 19–40 yr |
Hip extensor: 2.1 Range: 0–4.5 Hip flexor: 2.7 Range: 0–4 Knee extensor: 1.8 Range: 0–5 Knee flexor: NR Ankle dorsiflexion: 2.1 Range 0–5 Ankle plantarflexion: NR |
| Davis et al, 201026 | 61.9 yr Range: 51–72 yr |
Heigh: 163 cm Range 151–182 cm Weight: 71.7 kg Range: 56–111 kg BMI: NR |
Poliomyelitis = 9 Motor neuron disease = 1 |
None = 3 Solid GRAFO = 4 Locked KAFO = 1 Knee brace = 1 Posterior offset KAFO = 1 Walking aidsb: Walking stick = 2 Two walking sticks = 2 Forearm crutch = 1 Two forearm crutches = 1 Experience: 15 yr Range: 0–60 yr |
No average estimates reported |
| Bernhardt et al, 201125 | 60 yr (± 9) | Height: NR Weight: NR BMI: 26.6 (± 4.5) |
All patients had inclusion body myositis | Cane = 4 Experience = None |
NR |
| Probsting et al, 201712 | 54.4 yr | Height: NR Weight: NR BMI: NR |
Poliomyelitis = 4 Incomplete spinal cord injury = 1 |
Locked KAFO = 5 Experience: NR |
No average estimates reported |
Abbreviations: KAFO, knee–ankle–foot orthosis; GRAFO, ground reaction ankle foot orthosis; NR, not reported; SD, standard deviation.
Walking aids were used in conjunction with KAFOs.
Scale from 0–5, with 0 representing no muscle contraction and 5 representing typical strength.
Risk of Bias in the Included Studies
All studies were before and after designs, which means that outcome measurements were taken in the same group of people. Measurements were first taken when the person was using the comparator (i.e., LKAFO or no orthosis), and then measurements were taken when the person was the using SCKAFO. For all included studies, authors did not report the timeframe of when people were recruited or when data were collected on participants. All studies were small, ranging from 5 to 21 participants. Learning effect seemed to be accounted for as one study divided the analysis into “novice” and “experienced” users and the other three studies allowed patients to use the SCKAFO at home before collecting outcome data. Certified orthotists took measurements around patients’ presentation and strength using standardized tools. The orthotists also collected outcome data and both orthotists and participants were not blinded due to the before and after design of the studies. Loss to follow-up was only reported in two of the four studies. Three of four studies had poor reporting, where outcome estimates were only presented in graphs and only partial information on baseline characteristics were reported and details of orthotist assessments were not provided.
Walking Ability
Three of four studies measured outcomes associated with walking ability, including velocity (the speed at which the person walks), cadence (steps per minute), stride length (the size of each step), and swing time (how long it takes to take a step).25–27
One study did not provide estimates in the text,27 so we extracted data from graphs using WebPlotDigitizer.21 Another study did not provide average estimates in the text and graphs, so we reported the outcomes as written in the text of the article.25 Lastly, one study found that three of four outcomes (velocity, cadence, and swing time) favoured the SCKAFO.26 Stride length was shorter in the LKAFO group.
Irby et al27 divided their participants into “experienced” and “novice” groups based on previous device use. The experienced group routinely used an LKAFO for ambulation. The novice group did not use an LKAFO. The authors found that novice users showed significant changes between the LKAFO and SCKAFO conditions for three of the measures (velocity, cadence, and stride length). Velocity increased from 55.3 to 59.0 cm/s (P = s.034). Cadence increased from 76.8 to 84.9 steps/min (P = 0.042). Stride length increased from 86.3 to 99.2 cm (P = .072). Experienced users tended to reduce velocity and cadence during early SCKAFO testing, but this was not significant (P = .10). On aggregate, there were no significant changes between the LKAFO and SCKAFO conditions (see Table 5). The authors hypothesized that experienced LKAFO users had ingrained gait patterns designed to compensate for walking with a standard LKAFO. These patterns may have limited the ability of those users from taking full and immediate advantage of the SCKAFO capabilities.
Table 5:
Outcomes Associated With Walking Ability
| Velocity in cm/s (± SD) | Cadence in steps/min (± SD) | Stride Length in cm (± SD) | Swing Time in sec (± SD) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Author, Year | Sample Size | SCKAFO | LKAFO | SCKAFO | LKAFO | SCKAFO | LKAFO | SCKAFO | LKAFO |
| Irby et al, 200527,a,b | n = 21 | 63.5 (4.5) | 62.5 (4.2) | 75.6 (3.4) | 76.4 (2.1) | NR | NR | NR | NR |
| Davis et al, 201026 | n = 10 | 72.9 (25.7) | 65.0 (24.5)c P = .000107 |
78.9 (17.6) | 73.9 (18.2)c P = .000016 |
55.0 (11.9) | 53.6 (12.0)d | 0.56 (0.10) | 0.64 (0.10)c P = .00067 |
| Bernhardt et al, 201125,e | n = 6 | People walked slower with the SCKAFOf P = .025 |
People walked with a lower cadence with the SCKAFOf P = .007 |
People had a shorter stride length with SCKAFO | NR | NR | |||
Abbreviations: LKAFO, locked knee–ankle–foot orthosis device; NR, not reported; SCKAFO, stance-control knee–ankle–foot orthosis; SD, standard deviation.
These estimates were extracted using WebPlotDigitizer21 for novice and experienced users combined.
Irby et al27 reports standard error, not standard deviation.
This comparison was statistically significantly in favour of SCKAFO.
Stride length in the affected leg.
Poor reporting of data as results were provided by the authors in the text only. Graphs were presented; however, there were no average estimates.
This comparison was statistically significant (in favour of no orthosis).
The quality of the evidence for outcomes associated with walking ability was very low (see Appendix 2, Table A2) and was downgraded for risk of bias and imprecision.
Activities of Daily Living
One study evaluated activities of daily living, comparing SCKAFO with LKAFO.12 There were 45 items on the Activities of Daily Living questionnaire and the scale ranged from 1 to 6, where 1 = very difficult and 6 = very easy. Table 6 shows the items where there was a significant difference between the two groups (in favour of SCKAFO). No items favoured the LKAFO group. Based on the very small sample size (n = 5), there were items that approached significance. These included walking on uneven terrain (P = .07), pushing or pulling a shopping trolley (P = .07), loading or unloading the trunk of a car (P = .07), carrying a heavy object (P = .07), walking with different shoes (P = .07), walking up stairs (P = .07), getting into public transportation (P = .07), and standing for a longer period of time (P = .07).
Table 6:
Activities of Daily Living
| Mean Ratings | ||
|---|---|---|
| Items | SCKAFO (± SD) | LKAFO (± SD)a |
| Family and Social Life | ||
| Going for a walk | 5.0 (1.2) | 3.0 (1.4) |
| Mobility and Transportation | ||
| Stepping on a sidewalk curb | 5.0 (1.2) | 3.6 (1.1) |
| Stepping over minor obstacles | 4.8 (1.3) | 2.8 (1.6) |
| Stepping on minor obstacles like rocks | 4.8 (1.3) | 2.0 (1.7) |
| Walking down stairs | 5.4 (0.9) | 2.6 (1.1) |
| Walking up ramps | 5.2 (0.8) | 2.4 (1.1) |
| Walking on unknown terrain | 4.6 (1.1) | 2.2 (0 (0.8) |
| Walking outside in bad weather | 4.8 (0.8) | 1.8 (0.8) |
| Standing in a crowded bus | 4.4 (1.5) | 2.0 (1.4) |
| Other Activities | ||
| Sitting for a longer period of time | 5.0 (1.4) | 2.6 (0.5) |
| Sitting on a low chair or sofa | 4.8 (1.1) | 2.4 (0.5) |
| Doing something else while walking | 4.4 (1.8) | 2.4 (1.7) |
Abbreviations: LKAFO, locked knee–ankle–foot orthosis device; SCKAFO, stance-control knee–ankle–foot orthosis device; SD, standard deviation.
This comparison was statistically significant (in favour of SCKAFO).
The quality of the evidence for activities of daily living was very low (see Appendix 2, Table A2) and was downgraded for imprecision.
Energy Consumption
One study measured outcomes associated with energy consumption.26 These outcomes measured the following: oxygen cost (calculated by dividing net oxygen consumption by the distance walked in metres per minute) and physiological cost index (calculated as the ratio of heart rate difference [exercise – rest] to walking velocity in metres per minute). This study found no difference in the oxygen cost of walking or the physiological cost index, concluding that SCKAFO did not decrease energy consumption during walking compared to LKAFO.
The quality of the evidence for outcomes associated with energy consumption was very low (see Appendix 2, Table A2) and was downgraded for imprecision.
Table 7:
Outcomes Associated With Energy Consumption
| Author, Year | Sample Size | Oxygen Cost (ml/kg/min) (± SD) | Physiological Cost Index (beats/meter/min) (± SD) | ||
|---|---|---|---|---|---|
| SCKAFO | LKAFO | SCKAFO | LKAFO | ||
| Davis et al, 201026,a | n = 10 | 0.224 (0.069) | 0.213 (0.081) | 0.70 (0.34) | 0.65 (0.32) |
Abbreviations: LKAFO, locked knee–ankle–foot orthosis device; SCKAFO, stance-control knee–ankle–foot orthosis device.
No comparisons were statistically significant.
Patient Satisfaction and Risk of Falls
One study provided only a narrative summary of data collected on patient satisfaction and risk of falls through a non-validated questionnaire. In terms of patient satisfaction, the authors stated that “all participants had complaints about the size, bulk, cosmesis, and noise of the SCKAFO, as well as difficulty donning and doffing the brace.”25 However, it is worth noting that this group did not have an orthosis prior to the study. Considering falls, the authors stated that “some participants felt the SCKAFO was helpful in safeguarding against falls and providing stability.” The quality of the evidence was not assessed for this outcome because outcomes were only described in text.
Other Outcomes
We did not find any data from the included studies on the following pre-specified outcomes:
Pain (self-reported or measured by standardized scales)
Adverse effects (e.g., falls, tissue damage)
Resource use (e.g., number of follow-up appointments, device malfunction, access to physiotherapy)
Discussion
Walking ability was measured in three of the four studies. While it is important to describe the technical measures (e.g., velocity, cadence, oxygen cost, etc.) of the effectiveness of wearing a SCKAFO or LKAFO, these measures do not speak directly to the utility of the devices. Technical measures only assess if a person's walking ability resembles a more typical gait pattern. However, while wearers are unlikely to achieve a completely typical gait pattern, they may see an increase in ease of movement. Therefore, patient-reported outcomes are important to understand the utility of the device. Only one study examined activities of daily living and the authors found that many tasks were significantly easier using a SCKAFO compared with an LKAFO. One study found that “novice” users had better walking ability with SCKAFO compared with LKAFO.27
The included studies are of low quality for various reasons. Studies included in this review had small sample sizes due to the rarity of the conditions (e.g., motor neuron disease), which makes it difficult to recruit a large number of people into a study. However, the studies also suffered from a high risk of bias due to poor study design (e.g., unclear if the samples were representative, no independent outcome assessments, unclear follow-up) and poor reporting. Also, people who are prescribed orthotic devices need training with the device. While some studies allowed people to bring the device home for 1 to 6 months before collecting data, there were no details of proper training with an orthotist or physiotherapist. Previous reviews that are broader in scope and include both comparative and non-comparative studies also reported that the evidence overall is of low quality.1,2,9 It is unlikely that higher quality evidence will be published examining the effects of LKAFO and SCKAFO on outcomes of interest.
Conclusions
We are uncertain if SCKAFOs improve walking ability, energy consumption, or activities of daily living (GRADE: Very low) compared with LKAFOs.
Economic Evidence
Research Question
What is the cost-effectiveness of stance-control knee-ankle-foot orthoses (SCKAFOs) compared with locked knee-ankle-foot orthoses (LKAFO) or with no LKAFO in people with knee instability due to different causes and conditions?
Methods
Economic Literature Search
We performed an economic literature search on July 22, 2020, to retrieve studies published from database inception until the search date. To retrieve relevant studies, we developed a search using the clinical search strategy with an economic and costing filter applied.
We created database auto-alerts in MEDLINE, Embase, and CINAHL, and monitored them for the duration of the assessment period. We also performed a targeted grey literature search of health technology assessment agency websites, clinical trial and systematic review registries, and the Tufts Cost-Effectiveness Analysis Registry. See the Clinical Literature Search section, above, for further details on methods used. See Appendix 1 for our literature search strategies, including all search terms.
Eligibility Criteria
STUDIES
Inclusion Criteria
English-language full-text publications
Studies published from inception to July 22, 2020, and studies identified through database auto-alerts
Studies comparing SCKAFO with LKAFO in people with knee instability due to different causes and conditions
Cost-utility, cost-effectiveness, cost-benefit, cost-consequence, or cost analyses
Exclusion Criteria
None
POPULATION
Inclusion Criteria
Adults (≥ 18 years years) with knee instability due to different causes and conditions
Exclusion Criteria
Healthy volunteers, children (< 18 years)
INTERVENTIONS
Inclusion Criteria
Any type of SCKAFO (e.g., mechanical, electronic, or microprocessor)
Exclusion Criteria
Other KAFO device (e.g., hip KAFO, ankle foot orthosis)
COMPARATOR
Inclusion Criteria
LKAFO or no LKAFO (i.e., no assistive device)
Exclusion Criteria
Other orthosis (e.g., hip KAFO, ankle–foot orthosis)
Outcome Measures
Costs
Health outcomes (e.g., quality-adjusted life-years, adverse events avoided)
Incremental cost
Incremental effectiveness
Cost per incremental quality-adjusted life-year gained
Literature Screening
A single reviewer conducted an initial screening of titles and abstracts using Covidence20 and then obtained the full texts of studies that appeared eligible for review according to the inclusion criteria. A single reviewer then examined the full-text articles and selected studies eligible for inclusion.
Data Extraction
We extracted relevant data on study characteristics and outcomes to collect information about the following:
Source (e.g., citation information, study type)
Methods (e.g., study design, analytic technique, perspective, time horizon, population, intervention[s], comparator[s])
Outcomes (e.g., health outcomes, costs, incremental cost-effectiveness ratios)
Study Applicability and Limitations
We determined the usefulness of each identified study for decision-making by applying a modified quality appraisal checklist for economic evaluations originally developed by the National Institute for Health and Care Excellence (NICE) in the United Kingdom to inform the development of NICE's clinical guidelines.16 We modified the wording of the questions to remove references to guidelines and to make it specific to Ontario. Next, we assessed the applicability of each study to the research question (directly, partially, or not applicable).
Results
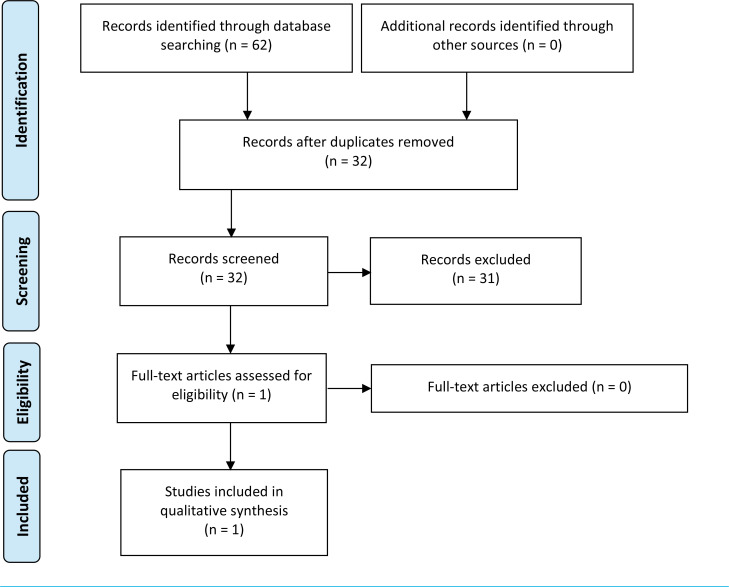
Economic Literature Search
The database search of the economic literature yielded 62 citations published from database inception until July 22, 2020. We did not identify any additional studies from other sources. In total, we identified 32 studies after removing duplicates that met our inclusion criteria. Figure 3 presents the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram for the economic literature search.
Figure 3: PRISMA Flow Diagram—Economic Search Strategy.
Source: Adapted from Moher et al, 2009.24
Abbreviation: PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-analyses.
Overview of Included Economic Studies
We identified one costing analysis2 that met the inclusion criteria. The characteristics and results of the included study is summarized in Table 8.
Table 8:
Results of Economic Literature Review—Summary
| Author, Year, Country of Publication | Analytic Technique, Study Design, Perspective, Time Horizon | Population | Intervention and Comparator | Results | ||
|---|---|---|---|---|---|---|
| Health Outcomes | Costs | Cost-Effectiveness | ||||
| O'Connor et al, 2016,2 United Kingdom | Costing analysis (cross-sectional survey) National Health Service (payer's perspective) NA |
Adult patients with NMD or CNS disorders | Intervention: LKAFO and SCKAFO Comparator: No comparator reported |
NA | Undiscounted, United Kingdom (2015 GBP)a LKAFO: Range: £73 to £3,553 Mean: £484 – £3,144 (depending on the type of KAFO device) SCKAFO: Range: £2,251 to £3,240 Mean: £2,831 |
NA |
Abbreviations: CNS, central nervous system disorders; LKAFO, locked knee–ankle–foot orthosis; NA, not applicable; NMD, neuromuscular disorders; SCKAFO, stance-control knee–ankle–foot orthosis.
The year of the costing survey.
The analysis was included in a health technology assessment conducted by the National Institute for Health Research in the United Kingdom.2 The study population included patients with neuromuscular and central nervous system disorders. Clinical outcomes reported in the health technology assessment were limited and were not included in the costing analysis. The authors conducted a costing survey for health care professionals, such as orthotists, to help estimate the cost of various off-the-shelf or custom-made orthotic devices such as a standard conventional, cosmetic, or carbon fibre LKAFO and a SCKAFO. There was no indication of the type of SCKAFO included in the costing analysis. Cost components considered in this analysis included materials and staffing costs. Unit costs from the National Health Service (NHS) were also considered for prefabricated (off-the-shelf) LKAFO devices. Three scenarios—low, average, and high cost—were analysed to account for the variability in time, staffing, and material costs. Costs (expressed in 2015 GBP) were not reported to be discounted or inflated, and the analysis was conducted from the payer perspective (the NHS).
O'Connor et al2 noted that the cost of an individual LKAFO could be highly variable, ranging from £73 to £3,553 (average: £484 to £3,144, depending on the type of LKAFO), and the cost of a SCKAFO ranged from £2,251 to £3,240 (average: £2,831). An off-the-shelf LKAFO was estimated to cost between £73 and £1,898, and the price for a custom-made LKAFO could range from £2,198 to £3,553. The difference between these cost estimates was attributed to device type and the labour involved in customizing an LKAFO. The largest cost component of a standard (conventional) LKAFO product was for labour (i.e., £2,009 to £2,998 of the £2,220 to £3,189 total cost of an LKAFO), whereas the main cost component for a standard carbon fibre LKAFO and an off the shelf LKAFO was the price of the device (i.e., £2,500 of the £2,564 to £3,553 total cost for a custom cosmetic LKAFO and £900 of the total cost of an off-the-shelf LKAFO). Similarly, the largest cost component of the SCKAFO was the price of the device (£2,187 of the £2,251 to £3,240 total cost of a SCKAFO).
Applicability of the Included Studies
Appendix 5 provides the results of the quality appraisal checklist for economic evaluations applied to the included studies. One study was deemed partially applicable to the research question. None of the studies were conducted from a Canadian perspective.
Discussion
Our literature review showed that the economic evidence of SCKAFO for people with knee instabilities is very limited. Only one study, O'Connor et al,2 met our inclusion criteria; however, the authors did not conduct an economic evaluation or budget impact analysis as a comparison between the two types of the device (e.g., SCKAFO vs. LKAFO). In addition, this analysis was not directly applicable to the Ontario context.
Some other notable strengths of the analysis include multiple costing sources, such as the NHS Supply Chain unit costs compared with expert opinion for off-the-shelf devices.2 The study also conducted lower, average, and upper bound scenarios for all analyses. These methods revealed a large variation in the cost of LKAFOs and SCKAFOs. While material and staffing costs were reported, the analysis did not consider all cost components. For instance, orthotists who participated in the costing survey could not give a clear indication of the cost for lifetime use of the device, or the cost of replacement, if needed. Lastly, it was unclear whether the costs reported for these devices would be partially or fully covered from a payer's perspective. These limitations demonstrate the complexity of costing orthoses used for knee instability, as many of the devices are custom-made.
Conclusions
We identified no studies evaluating the cost-effectiveness of SCKAFOs compared with LKAFOs in people with knee instability. Thus, the cost-effectiveness of using SCKAFOs compared with LKAFOs in Ontario and elsewhere is unknown.
Primary Economic Evaluation
Our analysis sought to understand the economic and clinical outcomes of SCKAFOs compared with LKAFOs in people with knee instabilities. However, there is limited comparative clinical evidence to inform an economic model. While there was some evidence available, we are uncertain if SCKAFOs improve walking ability, energy consumption, or activities of daily living (GRADE: Very low) compared with LKAFOs (see our clinical review, above). The limited and very low quality of evidence on health outcomes that could be used in a cost-effectiveness or cost–utility analysis meant that the clinical evidence did not support economic modelling. To our knowledge, there are no previous economic models evaluating LKAFOs or SCKAFOs. As such, we did not conduct a primary economic evaluation, and we focused on a standalone budget impact analysis for publicly funding SCKAFOs (mechanical, electronic, or microprocessor) in people with knee instability due to different causes and conditions.
Budget Impact Analysis
Research Question
What is the potential 5-year budget impact for the Ontario Ministry of Health of publicly funding stance-control-knee-orthoses (SCKAFOs) for people with knee instability due to different causes and conditions?
Methods
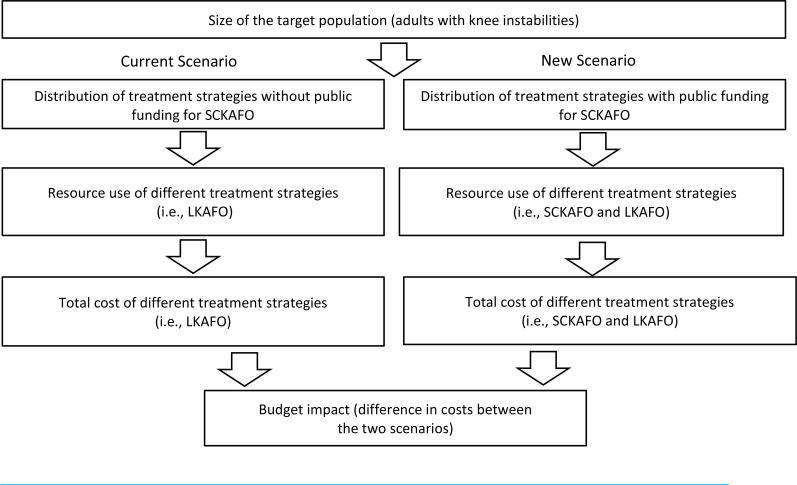
Analytic Framework
We estimated the budget impact of publicly funding SCKAFO devices using the cost difference between two scenarios: (1) current clinical practice without public funding for SCKAFO devices (the current scenario) and (2) anticipated clinical practice with public funding for SCKAFO devices (the new scenario, where there is a mix of SCKAFO and LKAFO). Figure 4 presents the budget impact model schematic.
Figure 4: Schematic Model of Budget Impact.
Abbreviations: LKAFO, locked knee–ankle–foot orthosis; SCKAFO, stance-control knee–ankle–foot orthosis.
We conducted a reference case analysis and sensitivity analyses. Our reference case analysis represents the analysis with the most likely set of input parameters and model assumptions. Our sensitivity analyses will explore how the results are affected by varying input parameters and model assumptions.
Key Assumptions
The target population remains constant over the next 5 years and represents people with an LKAFO (i.e., no gradual uptake of LKAFO), as the number of people requesting these devices in Ontario was constant over the last 5 years
People currently receiving a standard LKAFO are eligible to receive a SCKAFO, and 30% to 50% of people eligible for an LKAFO switch to a SCKAFO over a 5-year period
The mix of populations with different types of SCKAFO devices is unavailable (no data on the proportion of people with a mechanical, electronic, or microprocessor SCKAFO)
The total price estimated for SCKAFOs represents a conservative (maximum) cost estimate for a mechanical SCKAFO
Cost estimates for SCKAFO devices were based on current hourly wages for personnel, materials, and follow-up costs
The cost of follow-up appointments for both devices were included in the Assistive Devices Program (ADP) codes and price estimates used in the reference case and scenario analyses
People who might require a device replacement were included in our target population
The same proportional coverage for funding LKAFO devices is applicable to SCKAFO devices
Target Population
The target population for this analysis included adults (≥ 18 years) with knee instabilities due to different causes and conditions (e.g., neuromuscular disorders, spinal cord injury, etc.), who received an LKAFO in Ontario. To estimate the size of the target population, we first obtained the number of people in Ontario requesting LKAFO devices from the ADP. Based on 2018/2019 fiscal year data, we assumed 429 people have requested devices for LKAFOs, and all of them received funding (ADP, personal communication, May 2020). We did not break down the total population by disease-type or pathology, as subgroups are likely to be small in size and the underlying condition is of limited utility in informing treatment decisions. We assumed that the number of people receiving an LKAFO is constant each year, and that the target population would represent people requiring a new LKAFO, and some receiving a replacement device. More specifically, a person might need a replacement once every 2 to 5 years. Assuming no change in the number of LKAFO requests (i.e., 429) per year, the number of people requiring a replacement is captured in our target population estimate (which reflected incident and some prevalent use of LKAFOs; ADP, personal communication, December 2020). This assumption regarding the estimated target population is consistent with the annual number of referrals received by clinical experts (approximately 400 per year; Ontario Association of Prosthetics and Orthotics [OAPO] Committee, Certified Orthotists, personal communication, January 2021). We also assumed that a gradual uptake of 30% to 50% of people with an LKAFO would be eligible for a SCKAFO (incremental uptake assumed to be 5% per year, starting with 30% in year 1 and reaching 50% in year 5). The remainder would continue to use an LKAFO (OAPO Committee, Certified Orthotists, personal communication, September 2020). For our new scenario, the total number of people using an LKAFO or a SCKAFO was 1,287 and 858, respectively, over the next 5 years. Our approach related to estimating the target population is summarized in Table 9.
Table 9:
Target Population: Number of People With Knee Instabilities Expected to Receive a SCKAFO or an LKAFO in Ontario
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | Total | |
|---|---|---|---|---|---|---|
| Target population/volume of LKAFOsa | 429 | 429 | 429 | 429 | 429 | 2,145 |
| LKAFO volume replaced by SCKAFOs | 30% | 35% | 40% | 45% | 50% | — |
| LKAFO | 300 | 279 | 257 | 236 | 215 | 1,287 |
| SCKAFO | 129 | 150 | 172 | 193 | 214 | 858 |
Abbreviations: LKAFO, locked knee–ankle–foot-orthosis; SCKAFO, stance-control knee–ankle–foot-orthosis.
Data provided by Assistive Devices Program, Personal Communication, May 2020.
Current Intervention Mix
Eligibility for LKAFO devices includes long-term physical disability or a physical condition that requires the use of an orthotic device for 6 months or longer to improve function in daily activities. The ADP typically reimburses 75% of the cost of a prescribed LKAFO device for the majority of eligible people and 100% for those receiving social assistance benefits, to a maximum amount based on the benefits available for the components and procedures of the device that is recommended and approved. Thirty-six percent of people with an LKAFO received 100% funding in the 2018/2019 fiscal year (ADP, personal communication, December 2020). Therefore, in our reference case analysis, we assumed 36% of people received 100% funding from the ADP and the remainder (64%) received 75% funding, as indicated in the administration manual.28 The ADP also cites maximum list prices for device components and services; approved orthotists cannot bill more than the approved list price.
The ADP does not provide funding for SCKAFO devices (ADP, personal communication, 2020). Therefore, we assumed that SCKAFO devices are not funded for knee instability in our current scenario, and that all people receive an LKAFO device.
Uptake of the New Intervention and New Intervention Mix
In our new scenario, in which SCKAFO devices are publicly funded for people with knee instabilities, we assumed that some people would receive a SCKAFO instead of an LKAFO device. Similar to the current scenario, we also assumed that 36% of all people with a SCKAFO device would receive full coverage, and the remainder would receive 75% coverage to a maximum amount provided by the ADP program (ADP, personal communication, December 2020). Based on expert consultations, we assumed that not all people who would have received an LKAFO under the current scenario would receive a SCKAFO under the new scenario (OAPO Committee, Certified Orthotists, personal communication, September 2020). We assumed that 30% to 50% people would opt for a SCKAFO over an LKAFO (see Table 10; OAPO Committee, Certified Orthotists, personal communication, September 2020).
Table 10:
Uptake of People Expected to Receive Full (100%) or Partial (75%) Funding for a SCKAFO or an LKAFO in Ontario
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | Totala | |
|---|---|---|---|---|---|---|
| Target population/volume of people using LKAFOsb | 429 | 429 | 429 | 429 | 429 | 2,145 |
| LKAFO volume replaced by SCKAFOs | 30% | 35% | 40% | 45% | 50% | — |
| LKAFO | 300 | 279 | 257 | 236 | 215 | 1,287 |
| Full coverage (36% of people) b |
108 | 100 | 93 | 85 | 77 | 463 |
| 75% coverage (64% of people) |
192 | 178 | 165 | 151 | 137 | 823 |
| SCKAFO | 129 | 150 | 172 | 193 | 214 | 858 |
| Full coverage (36% of people)c |
46 | 54 | 62 | 69 | 77 | 308 |
| 75% coverage (64% of people)c |
82 | 96 | 110 | 124 | 137 | 549 |
Abbreviations: LKAFO, locked knee-ankle-foot-orthosis; SCKAFO, stance-control knee-ankle-foot-orthosis.
Numbers may be inexact due to rounding.
Data provided by the Assistive Devices Program, personal communications, May and December 2020.
Assumed the same proportions would be applicable to SCKAFO users.
Resources and Costs
Conventional LKAFOs are currently the standard of care in Ontario. They are eligible for public funding and listed in the ADP product manual.7 Our main source of pricing information was provided by orthotists, as suggested by manufacturers and experts, who have experience setting a price to a standard LKAFO using the ADP product manual. This pricing information includes codes for:
Materials
Device components
Professional orthotist time
The ADP does not cover warranty costs for LKAFO devices,28 but extended warranties may be provided by the vendor or purchased out-of-pocket by the individual patient.28 Our overall budget impact estimate includes repair and maintenance costs that are not covered by any warranties that might exist. We also did not include costs of adverse events due to a lack of comparative data on adverse events (see clinical review). A rework factor was already included in ADP codes, which covered all possible errors that can occur such as measurement, cast modification, manufacturing, alignment of joints, materials modifications, knee and ankle joint modifications and more (OAPO Committee, Certified Orthotists, personal communication, October 2020).
LKAFOS
The price of LKAFO and SCKAFO devices can vary greatly. This is mainly due to the cost of customizing the LKAFO device for the individual patient (OAPO Committee, Certified Orthotists, personal communication, September 2020). In consultation with orthotists, we developed a costing strategy to account for the variation in price estimates. We first engaged with experts to obtain commonly used ADP codes to estimate an average price for a standard LKAFO (e.g., $6,151.00 for 100% coverage or $4,613.25 for 75% coverage). We then applied the proportion of people who received 100% and 75% coverage (36% and 64% of people, respectively) to our cost estimates (we based our estimate on the proportion provided by the ADP). We used this estimate in our reference case analysis and assumed it represented the common cost of an LKAFO device. Table 11 outlines the unit cost per component, total cost of KAFOs, and the cost funded by the ADP.
Table 11:
Reference Case Analysis: Price Estimates for a Standard LKAFO
| KAFOa | ||||
|---|---|---|---|---|
| Type of Assessment/Materials/Device Component | Quantity | Unit Price | Total Price | ADP Funding (75%) |
| Tracing/cast/fit—thermoplastic AFO (CNLCF1002) | 1 | 498.00 | 498.00 | 373.50 |
| KAFO—thermoplastic (CNLCF2002) | 1 | 619.00 | 619.00 | 464.25 |
| Thermoplastic hinged AFO (CNLCF1250)b | 1 | 395.00 | 395.00 | 296.25 |
| Thermoplastic thigh cuff (CNLCF2070) | 1 | 236.00 | 236.00 | 177.00 |
| Pad (each) (CNLCF0010) | 8 | 16.00 | 128.00 | 96.00 |
| Pad cover (CNLCF0040) | 8 | 34.00 | 272.00 | 204.00 |
| Installation of uniplanar ankle joints (CNLCF1070) | 2 | 93.00 | 186.00 | 139.50 |
| Reinforced strap (CNLCF0100) | 5 | 42.00 | 210.00 | 157.50 |
| Joint head bending upright (CNLCF1100) | 6 | 82.00 | 492.00 | 369.00 |
| Molded patella cap (CNLCF2190) | 1 | 177.00 | 177.00 | 132.75 |
| Align and install knee joints (CNLCF2010) | 2 | 147.00 | 294.00 | 220.50 |
| External posting to AFO (CNLCF1820) | 1 | 42.00 | 42.00 | 31.50 |
| Multi-layer custom foot bed (CNLCF1730) | 1 | 142.00 | 142.00 | 106.50 |
| Installation of bale lock (CNLCF2040) | 2 | 69.00 | 138.00 | 103.50 |
| Installation of NYU stirrups (CNLCF1071)c | 2 | 152.00 | 304.00 | 228.00 |
| Component Costs | ||||
| Ankle joints (CNLCF3300) | 2 | 137.00 | 274.00 | 205.50 |
| Knee-joint locking (CNLCF3323) | 2 | 393.00 | 786.00 | 589.50 |
| Uprights (lower extremity) (CNLCF3310) | 6 | 142.00 | 852.00 | 639.00 |
| Stirrups (stirrups thermoplastic) (CNLCF3405)c | 2 | 53.00 | 106.00 | 79.50 |
| Total cost of device and time required | 6,151.00d | 4,613.25 | ||
Abbreviations: ADP, assisted devices program; AFO, ankle–foot–orthoses; KAFO, knee AFO.
Source: Ontario Association of Prosthetics and Orthotics, September 2020, Assistive Devices Product Manual.
All costs in 2020 CAD.
Hinged AFO controls and limits subtalar joint motion and allows for free ankle motion.
Stirrups are metal connecting thermoplastic foot shell to ankle joints.
Cost of device for people who have 100% funding by ADP.
We obtained a list of prices that were submitted to the ADP over the 2018/2019 fiscal year that included the following codes for a KAFO with locked knees and hinged ankles (excluding ischial/gluteal weight bearing codes; ADP, personal communication, October 2020):
Thermoplastic or Carbon fibre lamination style LKAFO: including CNLCF1002, CNLCF2002, CNLCF3300, CNLCF3323
A total cost estimate of the LKAFO codes reimbursed by ADP in fiscal 2018/2019 was $667,436.65 (manual calculation; ADP, personal communication, October 2020). Assuming that 429 people received the device per year, we estimated an average cost per person of $1,555.80. We added to this the costs associated with the material and component codes ($3,974, see Table 11) to calculate an average cost of $5,529.80 for each LKAFO for people with 100% coverage and $4,147.35 for people with 75% coverage; see Appendix 6 for full calculations). This estimate was used to validate the average price estimates for a standard LKAFO that we obtained from experts ($6,151.00 and $4,613.25 for people with 100% and 75% coverage, respectively) and was also considered instead of our reference case estimate in one of our sensitivity analyses.
SCKAFOS
We made cost estimates for SCKAFOs based on expert opinion and categorized the estimates by the type of SCKAFO (i.e., mechanical, electronic, or microprocessor; OAPO Committee, Certified Orthotists, personal communication, September 2020). A full list of SCKAFO device prices is shown in Table 12. In our reference case analysis, we used a conservative (maximum) price estimate for a mechanical SCKAFO of $10,784.49 and applied this amount to the 36% of people who received 100% coverage. We adjusted the cost to $8,088.37 for the 64% of people who received 75% coverage (Table 12). We used the maximum price of a mechanical SCKAFO, the most purchased SCKAFO in Ontario, in our reference case analysis (OAPO Committee, Certified Orthotists, personal communication, September 2020). Mechanical SCKAFOs are funded by Alberta Aids to Daily Living (AADL) program, which provides funding for basic medical equipment and supplies for people with chronic health problems. We considered other prices for SCKAFOs in our sensitivity analysis.
Table 12:
Cost Estimates for SCKAFOs Used in Reference and Scenario Analyses
| Type of SCKAFO | Minimuma | ADP Funding,b $ | Maximum,a $ | ADP Funding (75%),b $ |
|---|---|---|---|---|
| Mechanical | ||||
| Labour cost | 3,469.58 | — | 6,434.49 | — |
| Device cost | 3,915 | — | 4,350 | — |
| Total | 7,384.58 | 5,538.44 | 10,784.49c | 8,088.37c |
| Electronic | ||||
| Labour cost | 7,002.24 | — | 11,228.82 | — |
| Device cost | 13,920 | — | 14,500 | — |
| Total | 20,922.24 | 15,691.68 | 25,728.82 | 19,296.62 |
| Microprocessord | ||||
| Total | 83,853.16 | 62,889.87 | 99,296.98 | 74,472.68 |
Abbreviations: ADP, Assistive Devices Program; SCKAFO, stance-control knee–ankle–foot orthosis.
Cost for people who are assumed to receive 100% funding by ADP in 2020 CAD. OAPO Committee, Certified Orthotists, personal communication, October, 2020.
Manual calculation of 75% of full device costs in 2020 CAD.
Costs used in reference case analysis represent costs of a mechanical SCKAFO.
Microprocessor SCKAFOs could not be separated into cost components, as structuring the device is dependent on labour.
Internal Validation
The secondary health economist conducted formal internal validation. This process included checking for errors and ensuring the accuracy of parameter inputs and equations in the budget impact analysis.
Analysis
In the reference case analysis, we calculated the budget impact of publicly funding SCKAFO in adults with knee instabilities in Ontario. The budget impact is the cost difference between estimated total costs of the new scenario (public funding for SCKAFO and LKAFO) and the current scenario (public funding for LKAFO only). We did not present the budget impact broken down by cost type (i.e., labour and device costs) as many ADP codes combined professional time and materials. Our reference case analysis reflected the budget impact associated with publicly funding a basic (mechanical) SCKAFO. All our analyses were done from the perspective of the Ontario Ministry of Health and were expressed in 2020 CAD.
Sensitivity Analyses
Table 13 summarizes all scenarios that we ran as part of our sensitivity analysis to address variability in the costs of LKAFO and SCKAFO and to account for either slower or higher adoption of SCKAFO over the next 5 years. As a part of this analysis, we explored various price estimates.
Table 13:
Cost and Uptake Parameters Used in Scenario Analyses
| Scenario | Reference Case | Sensitivity Analysis |
|---|---|---|
| Cost | ||
| Scenario 1: low cost of a mechanical SCKAFO | ||
| 100% coverage 75% coverage |
$10,784.49a $8,088.37b |
$7,384.58a $5,538.44b |
| Scenario 2: low cost of an electronic SCKAFO | ||
| 100% coverage 75% coverage |
$10,784.49a $8,088.37b |
$20,922.24a $15,691.68b |
| Scenario 3: high cost of an electronic SCKAFO | ||
| 100% coverage 75% coverage |
$10,784.49a $8,088.37b |
$25,728.82a $19,296.62b |
| Scenario 4: low cost of a microprocessor SCKAFO | ||
| 100% coverage 75% coverage |
$10,784.49a $8,088.37b |
$83,853.16a $62,889.87b |
| Scenario 5: high cost of a microprocessor SCKAFO | ||
| 100% coverage 75% coverage |
$10,784.49a $8,088.37b |
$99,296.90a $74,472.68b |
| Uptake | ||
| Scenario 6: slow uptake of SCKAFO | 30% to 50% over 5 y | 30% in y 1, with a 3% annual increase over 5 y (reaching 42% in year 5) |
| Scenario 7: high uptake of SCKAFO | 30% to 50% over 5 y | 50% in y 1, with a 3% annual increase over 5 y (reaching 62% in year 5) |
| Additional Scenarios | ||
| Scenario 8: cost of an LKAFO using ADP submitted prices 100% Coverage 75% Coverage Scenario 9: 100% coverage for LKAFO and SCKAFO |
$6,151.00a $4,613.25a SCKAFO:$8,088.37 Coverage: 36% LKAFO: $4,613.25 Coverage: 64% |
$5,529.80c $4,147.35d SCKAFO: $10,784.49 Coverage: 100% LKAFO: $6,151.00 Coverage: 100% |
Abbreviations: ADP, assistive devices program; LKAFO, locked knee–ankle–foot orthosis; SCKAFO, stance-control knee–ankle–foot orthosis.
Note: scenarios 1–8 assume 36% of people received 100% ADP coverage and 64% of people received 75% ADP coverage.
OAPO Committee, Certified Orthotists, personal communication, 2020; Assistive Devices Product Manual.
Manual calculation of 75% of full price.
Manual calculation based on total ADP payments (Assistive Devices Program, personal communication, October 2020). See Appendix 6 for calculations.
75% of $5,529.80 full cost.
The three key types of SCKAFO device that we costed out were the mechanical, electronic, and microprocessor. The large range of prices for SCKAFO devices may be attributed to the materials and clinical hours needed to customize each class of device. To account for the range in prices in scenarios 1 to 5, we varied the price of the devices using minimum and maximum estimates for each class of SCKAFO (Table 13).
In addition, we explored variation in the uptake rates of SCKAFO (scenarios 6 and 7). In consultation with experts, some people who are eligible for a SCKAFO may choose to not use one, and only a proportion of people using an LKAFO may switch to a SCKAFO. In scenario 6, we modelled a slower uptake (30% in year 1, with a 3% increase each subsequent year, for a total of 772 people who chose a SCKAFO over 5 years) and, in scenario 7, we modelled a larger uptake (50% in year 1, with a 3% increase each year, for a total of 1,201 people who chose a SCKAFO over 5 years), compared to the gradual uptake assumed in our reference case (30% to 50% over 5 years, for a total of 858 people who chose a SCKAFO).
Because the price of an LKAFO can vary, we conducted a scenario validating price estimates provided by experts. In scenario 8, we estimated this price based on data from ADP and prices from the ADP product manual.7 See Appendix 6 for full calculations. Lastly, we conducted a scenario (scenario 9) assuming that all patients received 100% funding for LKAFO and SCKAFO devices. For this scenario, we used the full price estimated by Orthotists. Scenario 9 assumes that all patients receive full coverage and includes patients who may have a device that costs more to the ADP than standard SCKAFO and LKAFO devices (patients with only 75% coverage under the current scenario).
Results
Reference Case
The results of our budget impact analysis can be found in Table 14. In our new scenario, we estimated that the total costs for full public funding of SCKAFO would increase from $2.72 million in year 1 (at an uptake rate of 30%) to $3.05 million in year 5 (at an uptake rate of 50%). Given the current spending on LKAFOs, the annual budget impact of funding a mechanical SCKAFO over the next 5 years was estimated to be an additional $0.50 million in year 1, rising to $0.83 million in year 5, for a total of $3.34 million over 5 years. The corresponding SCKAFO-related budget impact would range from $1.17 million to $1.94 million, or a total of $7.77 million over 5 years.
Table 14:
Budget Impact Analysis Results for Reference Case Analysis—LKAFOs Versus Mechanical SCKAFOs
| Budget Impacta,b,c | ||||||
|---|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | Total | |
| Current Scenario | ||||||
| LKAFO 100% | 0.95 | 0.95 | 0.95 | 0.95 | 0.95 | 4.75 |
| LKAFO 75% | 1.27 | 1.27 | 1.27 | 1.27 | 1.27 | 6.33 |
| SCKAFO 100% | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| SCKAFO 75% | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Total SCKAFO | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Total (LKAFO + SCKAFO) | 2.22 | 2.22 | 2.22 | 2.22 | 2.22 | 11.08 |
| New Scenario | ||||||
| LKAFO 100% | 0.66 | 0.62 | 0.57 | 0.52 | 0.47 | 2.85 |
| LKAFO 75% | 0.89 | 0.82 | 0.76 | 0.70 | 0.63 | 3.80 |
| SCKAFO 100% | 0.50 | 0.58 | 0.67 | 0.75 | 0.83 | 3.33 |
| SCKAFO 75% | 0.67 | 0.78 | 0.89 | 1.00 | 1.11 | 4.44 |
| Total SCKAFO | 1.17 | 1.36 | 1.55 | 1.75 | 1.94 | 7.77 |
| Total (LKAFO + SCKAFO) | 2.72 | 2.80 | 2.88 | 2.97 | 3.05 | 14.42 |
| Budget Impact d | 0.50 | 0.58 | 0.67 | 0.75 | 0.83 | 3.34 |
Abbreviations: ADP, assistive devices program; LKAFO, locked knee–ankle–foot orthosis; SCKAFO, stance-control knee–ankle–foot orthosis.
In millions, 2020 CAD.
Numbers may be inexact due to rounding.
Assuming 36% of people received 100% ADP coverage at a cost of $10,784.49 for a SCKAFO and $6,151.00 for an LKAFO; 64% of people received 75% coverage at a cost of $8,088.37 for a SCKAFO and $4,613.25 for an LKAFO.
The budget impact is the difference between the total costs of the new and current scenarios.
Sensitivity Analysis
The total budget impact estimated in each scenario analysis can be found in Table 15 and Appendix 7. We found the greatest increase in budget impact in scenario 5, which assumes that all people switching to a SCKAFO would receive a microprocessor device (5-year budget impact increases from $3.34 million in the reference case to $67.13 million). When we decreased the cost of a mechanical SCKAFO device from $10,784.49 (reference case) to $7,384.58 (scenario 1), this reduced the 5-year budget impact by about 3.75 times, to $0.89 million. The budget impact was also affected by changing the proportion of people eligible for SCKAFO devices (scenarios 6 and 7): $3.01 million (30% uptake, increasing to 42%) to $4.68 million (50% uptake, increasing to 62%) over the next 5 years.
Table 15:
Budget Impact Results for Scenario Analyses—LKAFO Versus Other Classes of SCKAFOS, and Varying Uptake Rates
| Scenario | Budget Impacta,b,c | |||||
|---|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | Total | |
| Reference case | 0.50 | 0.58 | 0.67 | 0.75 | 0.83 | 3.34 |
| Scenario 1: low cost of a mechanical SCKAFO | 0.13 | 0.16 | 0.18 | 0.20 | 0.22 | 0.89 |
| Scenario 2: low cost of an electronic SCKAFO | 1.60 | 1.86 | 2.13 | 2.40 | 2.66 | 10.65 |
| Scenario 3: high cost of an electronic SCKAFO | 2.12 | 2.47 | 2.82 | 3.17 | 3.53 | 14.11 |
| Scenario 4: low cost of a microprocessor SCKAFO | 8.40 | 9.80 | 11.20 | 12.60 | 14.00 | 56.00 |
| Scenario 5: high cost of a microprocessor SCKAFO | 10.07 | 11.75 | 13.43 | 15.10 | 16.78 | 67.13 |
| Scenario 6: slow uptake of SCKAFO | 0.50 | 0.55 | 0.60 | 0.65 | 0.70 | 3.01 |
| Scenario 7: increasing uptake of SCKAFO | 0.83 | 0.88 | 0.94 | 0.99 | 1.04 | 4.68 |
| Scenario 8: cost of an LKAFO using ADP-submitted prices | 0.57 | 0.66 | 0.76 | 0.85 | 0.95 | 3.79 |
| Scenario 9: 100% Coverage | 1.02 | 1.12 | 1.22 | 1.32 | 1.42 | 6.09 |
Abbreviations: ADP, assistive devices program; LKAFO, locked knee–ankle–foot orthosis; SCKAFO, stance-control knee–ankle–foot orthosis.
In millions, 2020 CAD.
Numbers may be inexact due to rounding.
The budget impact is the difference between the total costs of the new and current scenarios.
When we used an average ADP-based cost for an LKAFO, we calculated a lower budget impact of $0.57 in year 1, raising to $0.95 million in year 5, for a total of $3.79 million over 5 years. Results for all scenario analyses can be found in Table 15 and a breakdown of all costs calculated in scenario analyses can be found in Appendix 7.
Discussion
We conducted a standalone budget impact analysis to estimate the additional costs of publicly funding SCKAFOs for people with knee instabilities in Ontario.
In our current scenario (no public funding allocated for SCKAFO), we estimated that it would cost $2.22 million annually to fund LKAFOs in people with knee instabilities due to various pathologies. In our new scenario, if SCKAFO (and LKAFO) were publicly funded, with a gradual uptake rate of 30% to 50% per year (a total of 2,145 people over 5 years), we estimated that the total cost of the new scenario would be $2.72 million in year 1, increasing to $3.05 million in year 5. The estimated budget impact of publicly funding mechanical SCKAFOs for people with knee instability in Ontario would be $0.50 million in year 1, increasing to $0.83 million in year 5. The SCKAFO-related annual budget impact would range from $1.17 to $1.94 million over 5 years. Although funding SCKAFO would result in additional expenditures compared to our current scenario, we assume that LKAFO users would gradually switch to a SCKAFO over time, reducing the costs for LKAFOs as uptake for SCKAFO increases.
Similar to the costing analysis conducted by the NHS, our work shows that orthotic devices can be highly variable in device price and total costs. Therefore, depending on the type SCKAFO used, the budget impact may vary significantly. There is a possibility that the budget impact was underestimated in our reference case analysis. According to orthotists, each class of SCKAFO would need to be analysed on its own, and consequently, an average estimate of the SCKAFO costing may not accurately reflect costs under the new scenario. We accounted for this large range in prices through various scenario analyses. For example, the highest budget impact was observed in instances where all people receive a microprocessor SCKAFO (5-year budget impact of $67.13 million, an approximately 91% cost difference compared to the mechanical SCKAFO used in the reference case analysis). The 5-year SCKAFO-related budget impact for a high-cost microprocessor was $71.15 million, compared to $7.77 million in our reference case scenario. This is expected, as a microprocessor SCKAFO is the most complex of the SCKAFO devices and has the highest material and clinical professional costs among all types of SCKAFO. However, the microprocessor SCKAFO may require specific gait deficits and may be prescribed on a case-by-case basis, as determined by an orthotist. Scenarios where we see the least variation include analyses with a slow uptake of SCKAFOs (with a percentage decrease in budget impact of approximately 5% from the reference case analysis) and with the ADP-based price estimates (with a percentage increase in budget impact of approximately 6% from the reference case analysis). This is likely due to the uptake rate being similar between the reference case and scenario analysis, and the ADP price estimates being similar to the estimate used in our reference case analysis.
Training with a physiotherapist may be necessary to ensure optimal outcomes in some patients requiring a SCKAFO or LKAFO device. Costs of physiotherapy visits were out of scope for this project because there is limited funding for physiotherapy for this specific patient population. Also, specialized training for a device may not meet the eligibility criteria for publicly funded programs, such as the Community Physiotherapy Clinic Program. As such, there could be implications on the costs associated with the device and patient outcomes that need to be examined in future analyses or during implementation (Amanda Smart, Director, Practice, Policy and Member Services, Ontario Physiotherapy Association, personal communication, January 2021).
Strengths and Limitations
To our knowledge, this is the first budget impact analysis conducted in Ontario that evaluates LKAFOs compared with SCKAFOs. Our model also directly and indirectly incorporated many of the components that would be considered during the clinical pathway, such as clinical hours, materials, and price variations that capture cost differences per patient. Moreover, our analysis included the proportion of people receiving 100% social assistance versus 75% ADP coverage, enabling us to provide a budget impact more representative of the target population. While our analysis represents the current environment and future intervention mix in Ontario, we recognized some limitations:
The target population may be slightly larger than that captured in our scenarios, representing people with knee instabilities who currently do not have an LKAFO, but would use a SCKAFO if it were covered. It is challenging to make a precise estimate of the target population for SCKAFOs, as knee instabilities could be caused by numerous pathologies. We consulted with experts and made an assumption that only 30% to 50% of LKAFO users would use a SCKAFO. We tested the effect of this assumption in our sensitivity analyses
The price of an LKAFO can vary greatly, largely due to the cost of customizations, and there is no established average price per device. To mitigate this issue, we obtained from orthotists an example with commonly used ADP codes to best represent a common cost of an LKAFO. We validated this estimate against data provided by experts. Our estimated reference case price of $4,613.25 is compared to an estimated ADP-based price of $4,147.35, with an assumption of 75% reimbursement)
There may be unanticipated costs related to adverse events such as falls or issues with the device, that are challenging to quantify. While it may be possible to estimate a cost for adverse events, our clinical review did not identify outcomes related to adverse events, nor any differences in adverse events between SCKAFO and LKAFO devices. Based on expert consultation, our analysis instead considered a rework factor that was included in the ADP codes. The rework factor covered all possible errors that can occur, such as measurement, cast modification, manufacturing, alignment of joints, materials modifications, knee and ankle joint modification errors, and more (OAPO Committee, Certified Orthotists, personal communication, October 2020)
We did not include costs associated with other professional visits, such as for physiotherapy, because they are not typically considered in the ADP manual as a part of device reimbursement. Other professional visits vary between people, making it challenging to standardize cost for the whole target population
There may be a difference in personnel costs between the LKAFO and SCKAFO estimates. We cannot account for these differences, as the price and cost listings of KAFOs in the ADP product manual are based on established negotiations with the Ministry of Health
We did not conduct a separate scenario analysis comparing SCKAFOs with no LKAFOs because this scenario would only consider costs of a SCKAFO, which is already captured in our reference case analysis. In instances where a patient does not choose an LKAFO, they may select a walker or wheelchair, or they may choose to walk without any assistive device. The cost of other devices in a “no LKAFO” scenario would be out of scope of this analysis
Conclusions
Our analysis examined publicly funding LKAFOs in Ontario for people with knee instabilities. With a gradual uptake of between 30% and 50% per year and a full device cost of $10,784.49, adopting mechanical SCKAFOs would lead to additional costs of $0.50 million in year 1, increasing to $0.83 million in year 5. The total additional costs over 5 years were estimated at about $3.34 million.
Preferences and Values Evidence
Objective
The objective of this analysis was to explore the underlying preference and values of patients and those who have lived experience with knee instability by assessing the values, needs, and priorities, as well as the preferences and perceptions, of both patients and caregivers relating to the use of stance-control knee–ankle–foot orthoses (SCKAFOs) for people with knee instability.
Background
Exploring patient preferences and values provides a unique source of information about people's experiences of a health condition and the health technologies or interventions used to manage or treat that health condition. It includes the impact of the condition and its treatment on the person with the health condition, their family and other caregivers, and the person's personal environment. Engagement also provides insights into how a health condition is managed by the province's health system.
Information shared from lived experience can also identify gaps or limitations in published research (e.g., outcomes important to those with lived experience that are not reflected in the literature).29–31 Additionally, lived experience can provide information and perspectives on the ethical and social values implications of health technologies or interventions.
Because the needs, preferences, priorities, and values of those with lived experience in Ontario are important to consider to understand the impact of the technology in peoples lives, we may speak directly with people who live with a given health condition, including those with experience of the technology or intervention we are exploring. This analysis used direct engagement with patients, their families, and caregivers to examine the perspectives and experiences of people with knee instability, some of whom had used stance control knee ankle foot orthoses.
Direct Patient Engagement
Methods
PARTNERSHIP PLAN
The partnership plan for this health technology assessment focused on consultation to examine the experiences of people with knee instability with the use of stance-control knee–ankle–foot orthoses. We also examined the perspectives of their families and caregivers. We engaged people via one-on-one phone interviews.
We used a qualitative interview, as this method of engagement allowed us to explore the meaning of central themes in the experiences of people with knee instability, as well as those of their families and caregivers.32 The sensitive nature of exploring people's experiences of a health condition and their quality of life are other factors that support our choice of an interview methodology.
PARTICIPANT OUTREACH
We used an approach called purposive sampling,33–36 which involves actively reaching out to people with direct experience of the health condition and health technology or intervention being reviewed. We approached a variety of clinicians, rehabilitation facilities, mental health facilities, community support groups, and partner organizations, including Muscular Dystrophy Canada, March of Dimes Canada, various rehabilitation clinics, community support groups, and clinical experts supporting this review to spread the word about this engagement activity and to contact people who have been assessed for knee instability, and their family members and caregivers.
PARTICIPANTS
Inclusion Criteria
Adults (≥ 18 years) with knee instability due to different causes and conditions (e.g., neuromuscular disorders, spinal cord injury, etc.)
Exclusion Criteria
Healthy volunteers, children and adolescents (<18 years)
INTERVENTIONS
Inclusion Criteria
Any type of SCKAFO (e.g., mechanical, electronic, or microprocessor)
Exclusion Criteria
Other KAFO device (e.g., hip KAFO, ankle foot orthosis)
COMPARATOR
Inclusion Criteria
LKAFO or no KAFO (i.e., no assistive device)
Exclusion Criteria
Other KAFO device (e.g., hip KAFO, ankle foot orthosis)
Participants
For this project, we spoke with a total of 10 participants. Seven had knee instability, including four who had tried a SCKAFO. We also spoke with three caregivers, all of whom had a family member with knee instability. Six participants were from the greater Toronto area, and the remaining four lived in Northern or Northwestern Ontario. Majority of the participants were 50 years old or older.
APPROACH
At the beginning of the interviews and surveys, we explained the role of Ontario Health, the purpose of this health technology assessment, the risks of participation, and how participants’ personal health information would be protected. We gave this information to participants both verbally and in a letter of information (Appendix 8). We then obtained participants’ verbal consent before starting the interview. With participants’ consent, we audio-recorded and then transcribed the interviews.
Interviews lasted approximately 20 to 30 minutes. Each interview was loosely structured and consisted of a series of open-ended questions. Questions were based on a list developed by the Health Technology Assessment International Interest Group on Patient and Citizen Involvement in Health Technology Assessment.37 Questions focused on the impact of major depression on the participants’ quality of life, their experiences with treatments to manage their knee instability, and their experiences, if any, using the SCKAFO, and their perceptions of the benefits or limitations with using this device. Questions to family and caregivers focused on their perceptions of the impact of the knee instability on their quality of life, as well as that of the person with the condition. We also asked about the impact of trying to manage the condition on the family members and caregivers themselves. See Appendix 9 for our interview and survey guide.
DATA EXTRACTION AND ANALYSIS
We used a modified version of a grounded-theory methodology to analyze interview transcripts and survey results. The grounded-theory approach allowed us to organize and compare information on experiences across participants. This method consists of a repetitive process of obtaining information though interviews, documenting and analyzing responses while simultaneously collecting, analyzing, and comparing information.38,39 We used the qualitative data analysis software program NVivo40 to identify and interpret patterns in the data. The patterns we identified allowed us to highlight the preferences and decision-making factors of those who use stance control knee ankle foot orthoses to help with their knee instability.
Results
LIVED EXPERIENCE WITH KNEE INSTABILITY
Participants had different conditions that resulted in their knee instabilities. Most knee instability was the result of polio contracted at a young age. Other causes included trauma to the leg or spine, surgeries that led to damage to the muscles or nerves of the leg, rare genetic diseases impacting nerves, and diseases that impacted participants’ nerves. Most had been living with their condition for a majority of their lives, while others developed knee instability within the last several years. Some had an easier time managing their knee instability, while others were still learning.
Participants used either the LKAFO or the SCKAFO to manage their knee instability. Regardless of which type of knee orthosis they used, they required gait aids. Some of the aids people mentioned using include canes, crutches, walkers, ski poles, wheelchairs, and scooters. Most participants reported needing to use gait aids at all times of the day because of the extent of their instability and overall physical condition. Increased activity required the use of more aids for a longer period or more supportive aids such as wheelchairs or walkers that reduce energy requirements. This was also the case for people who were more tired or in pain. Those with degenerative conditions had to use more stabilizing aids over time to help compensate for their increased lack of stability.
I used the cane with the [locked] KAFO and SCKAFO as well. Well, I only had one cane then. But when…when my knee blew, I had to start using two canes.
It's a little difficult. Our driveway is all rocks, and I would tend to trip on them a lot, but the equipment it makes it a lot easier.
When I go outside. I've got to have my cane on the uneven ground or stone. I've got to be really careful.
IMPACT OF KNEE INSTABILITY
Living with knee instability took a great toll on participants. A lot of their time and energy was spent learning how to manage it. They needed time and assistance to learn how to use the new device and do physiotherapy or other therapies to deal with the pain and discomfort that comes with it. Patients said their knee instability compromised their ability to do regular tasks such as cooking or cleaning.
In some cases, participants had become independent after years of practice using their orthoses and gait aids, and required less support from their caregivers to do their daily tasks.
Oh yeah, he does quite a bit. He can use the lawnmower and tractor. The wheelchair helps him get around on the property. As long as he can do all that, he's pretty independent.
Regardless of how well they had learned to manage their knee instability, all participants complained of pain. This was due either to the way they walked, putting weight on their strong leg to compensate for their weak leg, or to their physical condition, naturally resulting in body aches, pains, and excessive tiredness. Such pains greatly impacted their ability to perform daily activities and made them reliant on their family and caregivers.
I would go to the bathroom and I would have to sleep for 20 minutes because that's how much energy it took to get from the family room to the bathroom and back to the family room. I had no strength.
No, he helps me a lot because I can't stay standing for very long. He does the cooking. He does the laundry. He does everything.
All participants received physiotherapy and massage therapy to help deal with the pain. Many had coverage for these therapies through work; however, some are retired, and their coverage was limited. They made out-of-pocket payments, which had a major impact on their finances. Sometimes they opted to not get the therapies and lived with the pain. These costs come on top of the cost of gait aids and orthoses, as well as the many customizations and adjustments the orthoses require. One participant cited cost as a reason to delay purchasing needed equipment.
At times it's hard for me to even get up from the chair. We're trying to save up to buy a chair that helps me sit down and brings me up standing. It's just too expensive right now.
IMPACT ON CAREGIVERS
People with knee instability talked about the physical and emotional support given by families and caregivers, who help them with daily tasks or take over tasks they are too tired to do. Patients often become emotionally drained from having to deal with their illnesses and conditions, and perform daily tasks while trying to maintain a positive attitude. They said their caregivers played a big role in keeping them motivated and supported.
I realized that the paralysis I faced was a huge wake up call, physically, but the longer lasting effects are the emotional ones. I was lucky in that I was married to someone who I could say, ‘Okay, I can't make this call anymore. I can't fight this fight.’ And she would take over. She kept me motivated.
I have to keep fixing my device because it keeps breaking. Whenever I have issues with it, its hard on my wife because she's got to get tools, and take care of things. And she's got bad knees too, so it's tough on her. It's a tough life. It makes it really hard.
It doesn't just affect the person with the diagnosis, it also affects the people around them, because it's hard for them to see their loved ones go through things. My family's really excited for me to get back and be independent.
EXPERIENCE WITH ORTHOSES
Given that every participant's condition is different, their experience with knee orthoses is also very different. Most people with knee instability have tried KAFOs, and a few have tried SCKAFOs. Many factors were taken into consideration before deciding which device to use.
Patients usually have a consultation with their clinician or orthotist to decide on their best option, get fitted for an orthosis, order the orthosis, wait for it to arrive, and receive physiotherapy to learn how to use the orthosis. Often, the physiotherapy would continue for pain management. Some patients reported needing customizations to their orthoses and sometimes, even with adjustments, an orthosis could not meet their needs and a new orthosis would need to be ordered. Some people required frequent changes to their orthoses. It could take months or years to find a device that met their needs.
It took a long time before I got these braces. At first, they give suggestions [and] describe the different types of braces. They told me which ones would be best for me and I tried and wore those for a little bit. But they were uncomfortable and I wasn't able to walk as far, so I went back to a different version. They had these really skinny ones that are locked that they wanted me to try, but it wasn't enough support for me. So they gave me other ones to try, but those were definitely not for me. And then we found the perfect ones. The ones that I have currently been working good for a while.
It was difficult for most patients to make an appropriate comparison between the LKAFO and SCKAFO devices as they had different physical conditions requiring different levels of support. Some people said they were too weak, not stable enough, or they did not have enough core strength to use the SCKAFO, so they would use the LKAFO instead.
I was getting stronger and I was getting better, but my overall stability, my overall core strength was still weak enough that stance control wasn't on the table at that time.
The final choice of orthosis took a lot of trial and error as there were many factors beyond the simple ability to use the device, that were taken into consideration. Some people who were able to use the SCKAFO or met the physical criteria to use it as determined by their orthotists, preferred it over the LKAFO.
Having casts and going through the process of getting my third [brace], we looked at the possibility of stance control because at that time, my core strength was really good. My stability was really good. My upper body strength was really good.
DECISION-MAKING FACTORS: LKAFO PREFERRED OVER SCKAFO
Some participants who had tried the LKAFO preferred it over the SCKAFO for various reasons. They said that without it they would not be able to walk properly. In some cases, participants could walk a few steps without their orthoses and aids; however, the LKAFO helped them to walk longer distances. They also said the LKAFO allowed for more independence with daily tasks.
I've had issues walking my whole life, but with the surgeries and the equipment, it helps a lot to be able to live my life a little more independently and with less pain using the [locked] KAFO.
I get very tired because I have muscle atrophy in my lower extremities. So the brace helps with not only giving me the ability to walk but also makes up for my little muscle mass. They're basically like my legs. I always joke around saying I have to put my legs on before going anywhere.
I feel a huge difference when I'm wearing the brace. It gives me the ability to walk and it takes away the pain. Now that I've got the brace, there is no pain.
Some patients said they were used to their LKAFO and, because of their old age, physical condition, or stage in life, did not want to go through training to learn how to use a SCKAFO.
I would have had to relearn all of the things that I had taught my body to do in that 8-year period to be able to use the SCKAFO successfully. I am also at an age where it is going to create a level of vulnerability and stress in me that my spouse and I both felt probably wasn't conducive to what I needed or wanted from a device. So even though we entertained using the SCKAFO as a possibility, in the end, for me, we decided it was probably best to stick with the [locked] KAFO and focus instead on raising my kids.
If patients are not properly trained on how to use the SCKAFO, they may have trouble using it as the device may lock and unlock at unexpected or inappropriate times.
This happens occasionally. Sometimes when I'm walking, if I don't put the proper weight on my leg, it stays locked. Sometimes I'll take maybe 10 steps, but then I'll do something and it will stay locked for the next two steps. Apparently, it's because I didn't put my weight on it properly.
The out-of-pocket cost of the device also prevented some people from using the SCKAFO. Customizing their LKAFO made more economic sense.
First, we'll deal with the [locked] KAFO and then maybe look at the SCKAFO the future. We talked about getting the SCKAFO, but we decided at that time that we should just find something that wasn't going to keep breaking, that's more affordable right now.
DECISION-MAKING FACTORS: SCKAFO PREFERRED OVER LKAFO
Most people who tried a SCKAFO device were not sure which type of SCKAFO they had tried. However, those who preferred the SKCAFO over the LKAFO felt the device provided more stability, required less effort to use, and left them with enough energy to engage in more life activities. Participants said they were more independent and less reliant on their caregivers when using the SCKAFO.
The [locked] KAFO required you to use a lot of energy. You use more energy than a normal person walking with the normal gate, like [you do] with the SCKAFO.
The SCKAFO provided more stability than the [locked] KAFO. It takes the weight off the good leg.
My orthotist recommended that we try the SCKAFO, so we tried it for about 2, 3 months. And it was night and day from the other one. I adjusted fairly well. I just needed some training to get used to it.
Patients reported that the SCKAFO material was light and made them feel less tired when they used it. It allows for a more typical gait when walking, which is aesthetically better and also prevents compensation. It is a more compact orthosis compared to the LKAFO, allowing them to wear better fitting clothes.
I can easily wear dress pants or jeans with the SCKAFO. I also like it from a comfort point of view because it eliminated some of the pressure points under my patella.
It really grabs your knee and keeps it steady when you're taking a step forward. It feels like a normal movement when you bend your knee.
The main concern with using the LKAFO was the need to compensate. For most patients, compensating resulted in the overuse of the stronger leg, back, and hip muscles. This caused additional pain, which resulted in a need for additional physiotherapy, interfered with daily activities, and increased cost from additional gait aids.
I use my joints the best I [can], but you compensate, and then you destroy whatever's there eventually because you're overusing it.
I know the locked KAFO doesn't really allow a normal walking pattern. You have to sort of swing your leg around, and you're always using your good leg. I've gotten a lot of use out of it. My ankles have started to hurt, so I've had surgery on them, as well as my hip, back and shoulders. It's become an ongoing thing.
[My orthotist] recommended that I wear a full-length brace with locks on it, so it supported my entire leg. I wore that for a few years and I found it difficult to wear. I wasn't comfortable hiking my hip. I started to develop pain in the hip area and my lower back and I went back to that orthotist and asked him if there was anything he could do about that, because my gate when I walked [was] very uncomfortable. He said no. There was nothing else that he could do.
CHALLENGES WITH FINDING AN ORTHOSIS THAT WORKED
Given that everyone's physical condition was so different, it is difficult to summarize the challenges people faced when considering the SCKAFO alone. Some people were successful and have been using their current orthosis for many years. Others have had to change their orthosis one or more times to find the one that fit their needs or because their physical condition kept changing. Some of the key challenges they faced are described below.
TRAINING
Physical Condition—Severity of Condition
In some cases, the severity of the person's condition prevented them from using certain types of orthoses over others. It also required them to constantly change the type of orthosis they used or require adjustments to their orthoses after short periods time. This meant having to retrain to use a new or adjusted device, sometimes repeatedly.
I know when I tried the [SCKAFO that] I wasn't a candidate because I don't have the ligaments and all that around there to support it. I don't have the muscle mass and the strength, so the training and rehab would have been excruciating.
When I walk, it's like a person running because my movement takes a lot out of my body and, with the polio, my muscles are weakening. So it's pretty tough.
Physical Condition—Age Plus Stage of Life
Some older participants reported that they had the opportunity to use a SCKAFO device, but decided not to because of their age. They did not feel the time and effort it would take to learn how to use the device was worth it, but if they were offered a SCKAFO device a few years earlier, they would have strongly considered it.
You're getting older, and so you never know, right? My leg could pop off at any point. But hopefully not for a few more years.
I was also at an age [where] it was going to create a level of vulnerability and stress in me that we both felt probably wasn't conducive to what I needed or wanted from a device. So even though we entertained that as a possibility. In the end, for me, we decided it was probably best to stick with the status quo.
The girl told me [that] you have to do a lot of rehab. And I'm 70. Maybe if I was 30 I might have done it. But, you know, when you get older you worry about everything else.
Some participants who were not as old echoed the same thought, that if they were at a different stage of life, then they would have certainly considered using the SCKAFO device. These participants were typically parents who wanted to prioritize taking care of their young children over spending time and effort learning how to use a new device.
Physical Condition—Used to Compensating
Some participants who had been using the LKAFO for a long time had become used to it. They had been training their muscles to compensate for so long that doing anything else was too difficult and took too much effort to learn.
My issue…was that I had made so many gains in my muscles because…my body had compensated for the paralysis and for my weaknesses, particularly in my left knee and my pelvis. Now, the possibility of using a [SCKAFO] put me in a physically very vulnerable place because all of my mechanisms for compensating eliminated my ability to walk with a normal gait altogether.
He tried to get her to use the SCKAFO, but she had forgotten how to walk without swinging her leg all around, like she did with the [locked] KAFO.
CUSTOMIZATIONS AND ADJUSTMENTS
Comfort
Because patients wore their orthoses every day, they needed something that would be comfortable. Many said that they had to change the type of orthosis they used (regardless of whether it was an LKAFO or a SCKAFO), the padding inside the orthosis, or the material of the orthosis to feel comfortable wearing it for long periods of time.
I got the material changed for the [locked] KAFO so I could wear regular shoes, but it kept cutting into my leg. I kept trying to wear it because I felt like I was able to live my life. But eventually I told my doctor and orthotist about it, and they suggested that we make a half plastic half old style brace, which was a lot better.
The [locked] KAFO kept rubbing into me around the ankles and underneath the foot. Anytime that there's issues like that, though, I'm able to go and do some adjustments and they add padding, or they remove stuff that needs to be removed. I'm lucky that they'll take me anytime I need adjustment.
Participants said they would often have to get the materials on their orthosis changed to more suit their needs. Typically, participants said they switched to lighter materials because the orthoses were so heavy. This complaint was made more often for LKAFOs than SCKAFOs. However, people who got their LKAFOs made with light plastic material felt the SCKAFO material was too heavy.
They made my [locked] KAFO out of plastic…using the SCKAFO, it [was] difficult to walk on uneven ground because of the weight. I would prefer something lighter and more manageable like the plastic KAFO.
Locking Feature
In some cases, where patients were stable and strong enough to lift their leg and bend it, people had their LKAFO devices customized to remove the locking feature. They said the locking feature prevented them from having a typical gait, made them compensate too much, or caused some other discomfort. Participants said their doctors did not suggest using the SCKAFO. This may be explained by the physical presentation of patients, which may have suggested that the SCKAFO would not work well for them. The various customizations done on their KAFOs made them a better fit. Clinicians may also have been unaware of the SCKAFO device as an option for patients. Regardless, they were still able to make customizations, such as removing the locking feature, to make their LKAFO more comfortable to use.
I had the lock taken off because it was too hard to walk with. I kept having to take out the lock with my hand, so I told them to just remove it so I could bend my leg all the time and they did. I could not walk when it got locked up. I was unstable. I could not even stand up properly. So I had the lock taken off so I could walk better.
We took the lock off the KAFO. It doesn't straighten his leg anymore when he's walking so it's been awkward for him to walk with the lock on, it would throw him off balance.
Frequent Damage to Orthosis
Many people had to get their orthoses fixed because they kept breaking. They said breaking occurred due to missteps, walking on uneven terrain, or because the material of the orthosis was not strong. People who customized their devices to be made of lighter materials like plastic had to deal with frequent breaking, which was unavoidable because they needed the lighter orthosis.
I was popping rivets off my brace all the time. I was at the point where I was becoming really frustrated because I had to make such frequent visits to [my orthotist] to repair the brace. I was still working full time and we had just adopted two kids, when I was 50, so I was really busy and had to deal with this thing breaking all the time.
Getting something fixed and then having [it] break by that afternoon, while you're walking around the office with your colleague is a very frustrating experience.
FEAR OF FALLING
Participants’ general fear of falling prevented them from trying something new. Some participants tried the SCKAFO device, but found its use required a lot of concentration. This was especially the case for people who had been using the LKAFO device for many years. They were worried that this new device would increase their risk of falling. Given that they had already experienced falls that resulted in hospitalizations and long recovery times, they were not willing to accept the risks of starting with a new type of device.
The locks broke on my brace once and I fell straight down and backwards. My brace and my leg bone both broke, so I was off my legs for 6 months.
About 11 years ago, I broke my strong leg, a spiral fracture on the kitchen floor that was slippery.… So now I have a fear of falling. If you said to me, ‘tomorrow we're going to give you this really high-tech brace, it's going to be worth $30,000, and we're going to give you training,’ I guess I'd look at you and say, what's your guarantee that I'm not going to fall and break something?
ACCESS
Some participants said they often had issues with their orthoses, but could not do anything about them because they lived too far from the nearest orthotist to get their orthosis adjusted or customized. Some people said they had to teach themselves how to adjust their orthosis because they could not afford to drive such long distance so often.
My orthotist is about a 5-hour drive and I get discouraged when my [locked] KAFO breaks. I'm so far away from the orthotist's office that I pretty well have to fix it myself.
The [orthotist] is so far, I don't want to have to go there all the time to get my brace fixed. The rivets popped open once and I don't have any rivets at home, so I put some bolts in it. Then the pedal at the bottom of it broke, so I brought it back to the orthotist for them to fix it.
COST
In the Ontario context, people pay out of pocket for a proportion of their orthotic device and for all of their physiotherapy if they do not meet the criteria for publicly funded physiotherapy and have no private coverage. Finances are a significant factor in the choice of device in Ontario. This area of interest was not explored in the included studies. However, the authors of an HTA from the United Kingdom2 interviewed patients and found that people reported that their choice of orthotic device was restricted by “cut backs” in National Health Service funding.
Cost of Orthosis
Some people we interviewed reported that cost was a major barrier to getting an orthosis that helped to stabilize their knees. Some said they did not get the SCKAFO because it was too costly. They instead opted to get customizations done on their LKAFOs or use additional gait aids to help with stability.
They wanted me to get a [SCKAFO] but it's kind of out of my price range. I've got support with the [locked] KAFO, which helps, but the SCKAFO is kind of spring loaded. Every time you take a step, it goes forward, but that's out of my price range.
Cost of Physiotherapy
Patients received physiotherapy to help them use their orthosis properly. Most had to pay some or all physiotherapy costs out of pocket. Most reported that their coverage would allow them to attend only a few sessions or would cover only a small percentage of the total cost on their physiotherapy sessions. Physiotherapy was required every time a patient started using a new orthosis. They would use physiotherapy sessions to learn how to use the orthosis, to manage the pain that came with training new muscle groups to use to the brace, and to manage the pain of their physical condition.
I'm retired now, I had great benefits as a teacher, but once you retire, you don't have benefits anymore. Now I'm seeing an athletic therapist twice a week. And, again, we're just working on core strength and upper body strength, and I'm getting massage therapy every second week still, but I'm paying for everything out of pocket.
Physiotherapy is expensive. That's another expense that is not covered on top of everything else.
Advocating for Coverage Through Insurers
Not all patients had access to coverage and would pay out of pocket for their orthoses. Even patients who had insurance could have trouble paying for their orthoses as their insurance companies may be reluctant to cover the cost. A portion of the cost of the orthosis was covered through the Assistive Devices Program (ADP), while the remainder was expected to be paid out of pocket by patients. Insurance companies sometimes refused coverage because they were unclear about the specificities of the device. Insurance reimbursements often required that patients advocate and get approvals at multiple levels, requiring substantial research.
I was lucky I had good benefits. That helped me a lot with my old brace. But for my new brace I had to appeal to get it covered. When I did, initially, they turned me down. I said, okay, I'm challenging you right now because of you turning me down something that falls under ADP criteria. That is when they turned around and gave me about another $4,000 towards it.
It was a long process to get my brace, and to get it covered. They had to go through funding and everything else. Sent to the insurance to get one portion covered and the other portion of the cost for the price.… It was a long process.
One participant was able to get their SCKAFO device covered through their private insurance after many appeals. The insurance company initially denied the claim as it was not covered through ADP; however, the patient was able to appeal and have a some of the amount covered by their insurer with the remaining payment made out of pocket.
I have good benefits, but I had to appeal to them and make them realize that the SKAFO should be covered. They asked, well what about ADP and I said, look at what ADP only covers—KAFOs. I fought tooth and nail to say SCKAFOs are different in that it's got a computer in the side and it moves with you as your move, and I won the appeal. And they did help me because they realized that there is a difference. They wouldn't cover it in entirety, but they gave me a good chunk.
TIME
The amount of time it took patients to find a solution that worked for them was a major barrier. Orthoses have to be customized. Once a person has been fitted for an orthosis, it can take weeks to receive it. Training and physiotherapy to learn and be comfortable using the orthosis takes additional weeks to months, and if the person decides to go another way, then they have to start over. Once a person settles on an orthosis, getting access to funding takes additional time.
Well, I tried out one brace, but it was totally wrong. It wasn't giving me any support at all, and they took a while to find the kind of brace I needed. Eventually I got one that I could walk better in. I saw my doctor and he said I was much better with this brace than I was with the one before. It was such a long process to get it through. Because they had to find it, then they had to go through funding and everything.
There are many different types of braces. There's the locked ones, there's smaller ones, there's ankle and knee ones.… So, it took a while because we had to try a few.
Before a patient can even start the process of choosing, fitting, and learning to use an orthosis, they have to find a clinician or orthotist who is willing and knowledgeable enough to help. People we interviewed reported that many clinicians they consulted with lacked the knowledge or information about orthoses. They were left to do a lot of their own research or reach out to other orthotists.
It was long and frustrating and complicated, the length of time it took to get even the referral for my first appointment with the orthotist. That year and a half was very difficult.
My clinician wanted to get my knee a little more stable within the existing brace, but it wasn't effective enough. So, I did a lot of research on my own and I found this company…and I looked into that stance control knee brace, and it looked like something I fit the requirement for. So, I thought, I'm going to ask them to help with this and they did.
Preferences
Participants were told about the SCKAFO and the various types available: electronic, mechanical, and sensor controlled. When asked their thoughts on the SCKAFO, they had both positive and negative reflections, based both on their experiences using the SCKAFO and when comparing it with the LKAFO.
POSITIVE
Comfort
Many felt the SCKAFO device would be more comfortable to wear because it would be better fitted and provide more support. The additional support allows for a more typical gate, which makes it more comfortable to wear as well.
Well, it's much more comfortable. I mean it's a little bit more of a break because there's more support and things like that. And it's a little warmer than the one that locks my knee. It's more comfortable because your leg is in a better position.
[With] the [locked] KAFO, I couldn't swing my leg. [With] the SCKAFO I can swing my leg, and I can also put weight on it and it's very comfortable. It makes it easier for me to walk because I can walk like a normal swing…with a normal gate. It's a lot better than the first one.
Less Bulky
Some people reported that the SCKAFO would be less bulky and lighter than their LKAFO device. This would make it easier to wear and would require less effort when walking around, allowing them to walk or otherwise be active for longer periods.
It's far less bulky. I mean, the [locked] KAFO certainly had very strong advantages, but it's still a significant amount of plastic and metal wrapped around my leg. There are advantages but to me the biggest advantage of going with the SCKAFO is far less metal and plastic around my leg.
Some people with LKAFO devices that had been customized with lighter materials disagreed, stating that the SCKAFO was bulkier than their LKAFO.
More Stability
Participants reported that using the SCKAFO device would mean there would be less of a need to compensate using other muscle groups when walking. They expected that the orthosis would do most of the work, so walking would take a lot less effort. They also felt the SCKAFO would provide more stability overall and reduce the need for gait aids.
The SCKAFO would help control the motion of the leg and possibly help to walk without the cane.
If it helps them to walk like you walk, normally and independently, without a cane or a walker, then that means more independence for her. She can do more and she needs me less.
Participants expected that less effort would be exerted using the SCKAFO device, given the extra stability it would provide and the lack of a need for compensation.
That it just looks more normal and I feel like it would be less tiresome to use.
That notion of it helping me to move my leg, instead of it all coming from my back and my hip…it just seems like it would be easier.
Prevent Pain
Participants felt that with the SCKAFO, not needing to compensate with other muscle groups would also reduce pain in their stronger leg, hip, and back, and generally increase comfort when walking.
I think there would be higher rates of medical issues with the locked KAFO. When you're able to bend your knee, like with the SCKAFO, then it's better for you health wise. You'll have [fewer] issues with your other parts.
It would be great to be able to build up the quality of life and to have more independence and more range of motion, compared to regular KAFOs. I think it'd be ideal for people to not have that extra pain in the back so that you're able to walk with control and without discomfort. I think that would be very good thing.
Typical Gait
People reported they felt that using the SCKAFO device would be more aesthetically appealing because they thought it would allow for a more typical gait and allow them the ability have some normalcy, such as having the ability to wear better fitted clothes and shoes, and to walk and move in a more comfortable manner.
They feel far less bulky under my pants. Even at my age, I'm very aware of my style. I have a very strong sense of fashion. So, I mean, once I started getting better and stronger, looking good became something that I was interested in doing.
I'll just feel a little more normal with the SCKAFO. Having something that would bend and move like normal is very appealing.
NEGATIVE
Although people were generally enthusiastic about the SCKAFO device, they still had some reservations. Those who had tried the device, and those who avoided it or who did not fit the criteria to try the device, all had some concerns regarding its use.
Training
Since many of the participants had been using LKAFOs for several years, there were concerns about the difficulty of transitioning to a new kind of device. They believed that training would be difficult and would require a lot of time and effort. However, most of the people we spoke to were older adults who said that, if given the option to train to use a SCKAFO at a younger age, they would have been ok with the time and effort required.
They were talking about 6 weeks of gate training after you started using the SCKAFO, and I made a choice at that point to focus on being a mom over spending years trying to figure out if there's a different way to wear a brace.
Preferences and Values Evidence Discussion
The outreach for this review was robust because it captured many different perspectives, including patients, family, and caregivers. However, insights were obtained only from people who had used an LKAFO device. Most reported using the LKAFO exclusively because their physical condition did not meet the criteria for use of a SCKAFO. Other participants who did meet the physical criteria to use a SCKAFO avoided the device because of their age, cost, comfort, or discomfort over the burden of transitioning to a SCKAFO.
Participants who preferred the SCKAFO had a strong preference for using the SCKAFO over the LKAFO. Reasons cited included comfort, typical gait, stability, and reduced pain. Caregivers supported participant sentiment around SKCAFO because of the increased independence it provided and the accompanying decrease in reliance on assistance.
Participants from Northern Ontario had additional difficulty finding and maintaining an orthosis due to geography as they had to drive long distances to access an orthotist. This was more of a concern for people using LKAFO, as those using SCKAFOs did not mention their devices breaking. However, in both cases, participants said they had to make minor adjustments to their orthoses to suit their comfort, which could change over time depending on their physical condition.
LIMITATIONS
A person's physical condition may limit their ability to use a SCKAFO. As well, we did not interview anyone who had or was using a SCKAFO. This made it difficult for participants to appropriately describe their feelings about the SCKAFO device; a major limitation for this review. Even when describing their preferences, participants had trouble making appropriate conclusions because their conditions made them ineligible for the SCKAFO.
If we could have engaged with more people who had experience with both LKAFO and SCKAFO, we may have been able to compare and contrast the lived experience between these two types of device.
Preferences and Values Evidence Conclusions
People with knee instability require the use of devices such as LKAFOs, SCKAFOs, and other gait aids to help stabilize their knee and help them walk comfortably. The decision-making factors were different for each person, depending on their condition, age, stage of life, and comfort with the current aids. Many participants did not meet the criteria to use the SCKAFO, but those who did had a strong preference for it over the LKAFO. People who had been using the LKAFO for many years and were comfortable with the compensating necessary cited the amount of time and energy required for physiotherapy to learn how to use the SCKAFO as a major deterrent. Many participants who had adapted to using the LKAFO would prefer a device that provides a more typical gait, but starting with this type of device would be easier than switching from an existing LKAFO.
Conclusions of the Health Technology Assessment
We are uncertain if SCKAFOs improve walking ability, energy consumption, or activities of daily living (GRADE: Very low) compared with LKAFOs.
We identified no studies evaluating the cost-effectiveness of SCKAFO compared with LKAFO in people with knee instability. Thus, the cost-effectiveness of using SCKAFO compared to LKAFO in Ontario and elsewhere is unknown. Because the clinical evidence for relevant outcomes was uncertain (GRADE: Very low), we did not conduct a primary economic evaluation. Our budget impact analysis concluded that with a gradual uptake of the SCKAFO device of between 30% and 50% per year and a full device cost of $10,784, funding a mechanical SCKAFO would lead to additional costs of $0.50 million in year 1, increasing to $0.83 million in year 5. The total additional costs over 5 years were estimated at about $3.34 million.
Many of the people we spoke with who could have used a SCKAFO if it were publicly funded had a strong preference for it over LKAFO devices. People who had been using an LKAFO for many years and were comfortable with the compensating necessary cited the amount of time and energy required for physiotherapy necessary to switch to the SCKAFO as a major deterrent. Many participants who had adapted to using an LKAFO would prefer a device that provides a more typical gait, but felt that starting with this type of device would be easier than switching from an existing LKAFO.
Acknowledgments
This report was developed by a multidisciplinary team from Ontario Health. The clinical epidemiologist was Anna Lambrinos, the medical librarian was Corinne Holubowich, the health economics associate was Selena Hussain, the secondary health economist was Olga Gajic-Veljanoski, and the primary patient and public partnership analyst was Aroma Akhund.
The medical editor was Tim Maguire. Others involved in the development and production of this report were Merissa Mohamed, Claude Soulodre, Susan Harrison, Saleemeh Abdolzahraei, Elisabeth Smitko, Sarah McDowell, Vivian Ng, David Wells, Andrée Mitchell, Charles de Mestral, and Nancy Sikich.
We would like to thank the following people, organizations, and manufacturers for lending their expertise to the development of this report:
Nancy Dudek, Faculty of Medicine, University of Ottawa
Scott Durno, Spinal Cord Rehabilitation Program, University Health Network
Eric Graham, Design Prosthetics and Orthotics
MQ Huangfu, Neurocore Physiotherapy
Andrew Lok, Back2feet
Allan Moore, FCBC Orthopedic Bracing Solutions Inc.
Mary Catherine Thiessen, Eagle Orthopaedics, Ontario Association of Prosthetics and Orthotics
Ontario Physiotherapy Association
Ottobock SE & Co.
We also thank our lived experience participants who generously gave their time to share their stories with us for this report.
The statements, conclusions, and views expressed in this report do not necessarily represent the views of those we consulted.
Abbreviations
- ADP
Assistive Devices Program
- CI
Confidence interval
- GRADE
Grading of Recommendations Assessment, Development, and Evaluation
- HTA
Health technology assessment
- KAFO
Knee–ankle–foot orthosis
- LKAFO
Locked knee–ankle–foot orthosis
- NHS
National Health Service
- NICE
National Institute for Health and Care Excellence
- NMD
Neuromuscular disease
- SCKAFO
Stance-control knee–ankle–foot orthosis
Glossary
- Adverse event
An adverse event is an unexpected medical problem that happens during treatment for a health condition. Adverse events may be caused by something other than the treatment.
- Budget impact analysis
A budget impact analysis estimates the financial impact of adopting a new health care intervention on the current budget (i.e., the affordability of the new intervention). It is based on predictions of how changes in the intervention mix will impact the level of health care spending for a specific population. Budget impact analyses are typically conducted for a short-term period (e.g., 5 years). The budget impact, sometimes referred to as the net budget impact, is the estimated cost difference between the current scenario (i.e., the anticipated amount of spending for a specific population without using the new intervention) and the new scenario (i.e., the anticipated amount of spending for a specific population following the introduction of the new intervention).
- Cost–benefit analysis
A cost–benefit analysis is a type of economic evaluation that expresses the effects of a health care intervention in terms of a monetary value so that these effects can be compared with costs. Results can be reported either as a ratio of costs to benefits or as a simple sum that represents the net benefit (or net loss) of one intervention over another. The monetary valuation of the different intervention effects is based on either prices that are revealed by markets or an individual or societal willingness-to-pay value.
- Cost–consequence analysis
A cost–consequence analysis is a type of economic evaluation that estimates the costs and consequences (i.e., the health outcomes) of two or more health care interventions. In this type of analysis, the costs are presented separately from the consequences.
- Cost-effective
A health care intervention is considered cost-effective when it provides additional benefits, compared with relevant alternatives, at an additional cost that is acceptable to a decision-maker based on the maximum willingness-to-pay value.
- Cost-effectiveness acceptability curve
In economic evaluations, a cost-effectiveness acceptability curve is a graphical representation of the results of a probabilistic sensitivity analysis. It illustrates the probability of health care interventions being cost-effective over a range of willingness-to-pay values. Willingness-to-pay values are plotted on the horizontal axis of the graph, and the probability of the intervention of interest and its comparator(s) being cost-effective at corresponding willingness-to-pay values is plotted on the vertical axis.
- Cost-effectiveness analysis
Used broadly, “cost-effectiveness analysis” may refer to an economic evaluation used to compare the benefits of two or more health care interventions with their costs. It may encompass several types of analysis (e.g., cost-effectiveness analysis, cost–utility analysis). Used more specifically, “cost-effectiveness analysis” may refer to a type of economic evaluation in which the main outcome measure is the incremental cost per natural unit of health (e.g., life-year, symptom-free day) gained.
- Cost–utility analysis
A cost–utility analysis is a type of economic evaluation used to compare the benefits of two or more health care interventions with their costs. The benefits are measured using quality-adjusted life-years, which capture both the quality and quantity of life. In a cost–utility analysis, the main outcome measure is the incremental cost per quality-adjusted life-year gained.
- Incremental cost
The incremental cost is the additional cost, typically per person, of a health care intervention versus a comparator.
- Knee–ankle–foot orthosis (KAFO)
A KAFO is a brace or assistive device that covers and supports the entire leg. Its purpose is to aid mobility among people who have stability issues or muscle weakness due to one or more of a range of conditions that affect walking ability. Orthoses can be custom made for the individual user by an orthotist (see Orthotist).
- Locked knee–ankle–foot orthosis (LKAFO) Ministry of Health perspective
-
An LKAFO is a type of KAFO that provides stability by locking the knee in an extended position to maintain proper leg alignment during walking.
The perspective adopted in economic evaluations determines the types of costs and health benefits to include. Ontario Health develops health technology assessment reports from the perspective of the Ontario Ministry of Health. This perspective includes all costs and health benefits attributable to the Ministry of Health, such as treatment costs (e.g., drugs, administration, monitoring, hospital stays) and costs associated with managing adverse events caused by treatments. This perspective does not include out-of-pocket costs incurred by patients related to obtaining care (e.g., transportation) or loss of productivity (e.g., absenteeism).
- Orthosis
An orthosis is a brace or other device used to correct a person's posture or provide support for a limb or the spine.
- Orthotist
An orthotist is a health care professional who is trained in assistive walking devices, especially in the design and fabrication of customized orthotic devices (see, for example, Knee–Ankle–Foot Orthosis [KAFO]).
- Proprioception
Proprioception refers to the body's ability to perceive its own position in space such as is needed for person to close their eyes and touch their nose with their index finger. Proprioception allows for coordinated movements such as walking or standing up from a sitting position while maintaining balance and controlling body posture. A proprioception disorder or injury could lead to balance issues, such as having trouble standing on one foot or having frequent falls while walking.
- Quality-adjusted life-year
The quality-adjusted life-year is a generic health outcome measure commonly used in cost–utility analyses to reflect the quantity and quality of life-years lived. The life-years lived are adjusted for quality of life using individual or societal preferences (i.e., utility values) for being in a particular health state. One year of perfect health is represented by one quality-adjusted life-year.
- Reference case
The reference case is a preferred set of methods and principles that provide the guidelines for economic evaluations. Its purpose is to standardize the approach of conducting and reporting economic evaluations, so that results can be compared across studies.
- Scenario analysis
A scenario analysis is used to explore uncertainty in the results of an economic evaluation. It is done by observing the potential impact of different scenarios on the cost-effectiveness of a health care intervention. Scenario analyses include varying structural assumptions from the reference case.
- Sensitivity analysis
Every economic evaluation contains some degree of uncertainty, and results can vary depending on the values taken by key parameters and the assumptions made. Sensitivity analysis allows these factors to be varied and shows the impact of these variations on the results of the evaluation. There are various types of sensitivity analysis, including deterministic, probabilistic, and scenario.
- Stance-control knee–ankle–foot orthosis (SCKAFO)
A SCKAFO is a type of KAFO that allows for a smoother, more comfortable walking gait by allowing free movement of the knee while the leg is in motion and locking to provide extra support for the knee while the leg is straight and in a weight-bearing position.
- Time horizon
In economic evaluations, the time horizon is the time frame over which costs and benefits are examined and calculated. The relevant time horizon is chosen based on the nature of the disease and health care intervention being assessed, as well as the purpose of the analysis. For instance, a lifetime horizon would be chosen to capture the long-term health and cost consequences over a patient's lifetime.
- Utility
A utility is a value that represents a person's preference for various health states. Typically, utility values are anchored at 0 (death) and 1 (perfect health). In some scoring systems, a negative utility value indicates a state of health valued as being worse than death. Utility values can be aggregated over time to derive quality-adjusted life-years, a common outcome measure in economic evaluations.
Appendices
Appendix 1: Literature Search Strategies
Clinical Evidence Search
Search date: July 21, 2020
Databases searched: Ovid MEDLINE, Embase, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, CRD Health Technology Assessment Database, NHS Economic Evaluation Database and EBSCO Cumulative Index to Nursing & Allied Health Literature (CINAHL)
Database segments: EBM Reviews – Cochrane Central Register of Controlled Trials <June 2020>, EBM Reviews – Cochrane Database of Systematic Reviews <2005 to July 16, 2020>, EBM Reviews – Health Technology Assessment <4th Quarter 2016>, EBM Reviews – NHS Economic Evaluation Database <1st Quarter 2016>, Embase <1980 to 2020 Week 29>, Ovid MEDLINE(R) ALL <1946 to July 17, 2020>
Search strategy:
-
1
exp Gait/ (83824)
-
2
exp Gait Disorders, Neurologic/ (16680)
-
3
gait∗.ti,ab,kf. (133179)
-
4
Joint Instability/ (32424)
-
5
(knee∗ adj2 (instabili∗ or stabili∗ or unstabl∗)).ti,ab,kf. (8223)
-
6
or/1-5 (195269)
-
7
Orthotic Devices/ (12963)
-
8
Foot Orthoses/ (2531)
-
9
(orthot∗ or orthos∗).ti,ab,kf. (138026)
-
10
Braces/ (14664)
-
11
(brace or braces).ti,ab,kf. (15635)
-
12
or/7-11 (164846)
-
13
6 and 12 (9112)
-
14
(stance control∗ or SCO or SCOs).ti,ab,kf. (3804)
-
15
13 and 14 (79)
-
16
((stance control∗ adj5 (knee∗ or ankle∗ or foot∗ or ortho∗ or KAFO∗)) or SCKAFO∗).ti,ab,kf. (101)
-
17
((“stance and swing” adj4 (KAFO∗ or knee∗ ankle∗ foot∗ or ortho∗)) or ((swing phase or stance phase) adj2 (lock∗ or unlock∗))).ti,ab,kf. (36)
-
18
(ortho∗ knee unit∗ or swing KAFO∗ or active KAFO∗ or SCOKJ∗ or eknee brace∗ or e knee brace∗).ti,ab,kf. (2)
-
19
(C brace∗ or Cbrace∗ or ottawalk∗).ti,ab,kf. (25)
-
20
((microprocessor∗ adj6 (stance control∗ or swing∗ or knee∗ ankle∗ foot∗ or ortho∗ or KAFO∗)) or MPSSCO∗ or MP SSCO∗).ti,ab,kf. (32)
-
21
(dynamic KAFO∗ or (dynamic knee∗ adj2 (ortho∗ or brace∗))).ti,ab,kf. (46)
-
22
((electronic∗ or electromechanical or electro mechanical) adj4 (KAFO∗ or knee∗ ankle∗ or stance control∗ or (joint∗ adj4 unlock∗) or knee joint∗)).ti,ab,kf. (34)
-
23
((mechanical∗ adj2 control∗ adj2 knee∗) or (mechanical adj2 knee ankle foot ortho∗)).ti,ab,kf. (21)
-
24
((power∗ adj4 (knee∗ ankle∗ foot∗ or (knee adj3 ortho∗) or KAFO∗)) or PKAFO∗).ti,ab,kf. (28)
-
25
(e mag∗ adj2 (control∗ or system∗ or activ∗ or KAFO∗)).ti,ab,kf. (8)
-
26
sensor walk∗.ti,ab,kf. (13)
-
27
((free walk∗ or freewalk∗) adj5 (otto bock∗ or ottobock∗ or KAFO∗ or ortho∗ or stance control∗ or microprocess∗ or mechanic∗ or electronic∗)).ti,ab,kf. (8)
-
28
((otto bock∗ or ottobock∗) adj5 (KAFO∗ or ortho∗ or stance control∗ or microprocess∗ or mechanic∗ or electronic∗ or e mag∗)).ti,ab,kf. (44)
-
29
(Becker adj3 (ortho∗ or e-knee∗ or eknee∗ or stride∗ or fullstride∗ or safety∗ or UTX∗ or mechanic∗ or microprocess∗ or stance control∗ or KAFO∗)).ti,ab,kf. (5)
-
30
((Horton or Fillauer∗) adj4 (stance control∗ or ortho∗ or mechanic∗ or microprocess∗ or electronic∗ or KAFO∗)).ti,ab,kf. (4)
-
31
or/15-30 (334)
-
32
Case Reports/ or Comment.pt. or Editorial.pt. or (Letter not (Letter and Randomized Controlled Trial)).pt. or Congress.pt. (5563712)
-
33
31 not 32 (327)
-
34
33 use medall,cctr,coch,clhta,cleed (155)
-
35
limit 34 to english language [Limit not valid in CDSR; records were retained] (139)
-
36
gait/ (82684)
-
37
exp gait disorder/ (26878)
-
38
gait∗.tw,kw. (136186)
-
39
exp joint instability/ (36672)
-
40
(knee∗ adj2 (instabili∗ or stabili∗ or unstabl∗)).tw,kw. (8465)
-
41
or/36-40 (206348)
-
42
orthotics/ (3485)
-
43
exp orthosis/ (46361)
-
44
(orthot∗ or orthos∗ or brace or braces).tw,kw,dv. (154284)
-
45
or/42-44 (183632)
-
46
41 and 45 (10947)
-
47
(stance control∗ or SCO or SCOs).tw,kw,dv. (3835)
-
48
46 and 47 (82)
-
49
((stance control∗ adj5 (knee∗ or ankle∗ or foot∗ or ortho∗ or KAFO∗)) or SCKAFO∗).tw,kw,dv. (105)
-
50
((“stance and swing” adj4 (KAFO∗ or knee∗ ankle∗ foot∗ or ortho∗)) or ((swing phase or stance phase) adj2 (lock∗ or unlock∗))).tw,kw,dv. (38)
-
51
(ortho∗ knee unit∗ or swing KAFO∗ or active KAFO∗ or SCOKJ∗ or eknee brace∗ or e knee brace∗).tw,kw,dv. (2)
-
52
(C brace∗ or Cbrace∗ or ottawalk∗).tw,kw,dv. (27)
-
53
((microprocessor∗ adj6 (stance control∗ or swing∗ or knee∗ ankle∗ foot∗ or ortho∗ or KAFO∗)) or MPSSCO∗ or MP SSCO∗).tw,kw,dv. (34)
-
54
(dynamic KAFO∗ or (dynamic knee∗ adj2 (ortho∗ or brace∗))).tw,kw,dv. (49)
-
55
((electronic∗ or electromechanical or electro mechanical) adj4 (KAFO∗ or knee∗ ankle∗ or stance control∗ or (joint∗ adj4 unlock∗) or knee joint∗)).tw,kw,dv. (34)
-
56
((mechanical∗ adj2 control∗ adj2 knee∗) or (mechanical adj2 knee ankle foot ortho∗)).tw,kw,dv. (22)
-
57
((power∗ adj4 (knee∗ ankle∗ foot∗ or (knee adj3 ortho∗) or KAFO∗)) or PKAFO∗).tw,kw,dv. (29)
-
58
(e mag∗ adj2 (control∗ or system∗ or activ∗ or KAFO∗)).tw,kw,dv. (9)
-
59
sensor walk∗.tw,kw,dv. (20)
-
60
((free walk∗ or freewalk∗) adj5 (otto bock∗ or ottobock∗ or KAFO∗ or ortho∗ or stance control∗ or microprocess∗ or mechanic∗ or electronic∗)).tw,kw,dv. (10)
-
61
((otto bock∗ or ottobock∗) adj5 (KAFO∗ or ortho∗ or stance control∗ or microprocess∗ or mechanic∗ or electronic∗ or e mag∗)).tw,kw,dv. (50)
-
62
(Becker adj3 (ortho∗ or e-knee∗ or eknee∗ or stride∗ or fullstride∗ or safety∗ or UTX∗ or mechanic∗ or microprocess∗ or stance control∗ or KAFO∗)).tw,kw,dv. (8)
-
63
((Horton or Fillauer∗) adj4 (stance control∗ or ortho∗ or mechanic∗ or microprocess∗ or electronic∗ or KAFO∗)).tw,kw,dv. (6)
-
64
or/48-63 (356)
-
65
Case Report/ or Comment/ or Editorial/ or (letter.pt. not (letter.pt. and randomized controlled trial/)) or conference abstract.pt. or conference review.pt. (11310210)
-
66
64 not 65 (294)
-
67
66 use emez (127)
-
68
limit 67 to english language [Limit not valid in CDSR; records were retained] (120)
-
69
or/35,68 (259)
-
70
69 use medall (112)
-
71
69 use emez (120)
-
72
69 use cctr (27)
-
73
69 use coch (0)
-
74
69 use clhta (0)
-
75
69 use cleed (0)
-
76
remove duplicates from 69 (149)
CINAHL
| # | Query | Results |
| S1 | (MH “Gait+”) | 11,940 |
| S2 | (MH “Gait Disorders, Neurologic+”) | 2,475 |
| S3 | gait∗ | 26,920 |
| S4 | (MH “Joint Instability”) | 9,216 |
| S5 | (knee∗ N2 (instabili∗ or stabili∗ or unstabl∗)) | 2,056 |
| S6 | S1 OR S2 OR S3 OR S4 OR S5 | 38,284 |
| S7 | (MH “Orthoses+”) | 10,460 |
| S8 | orthot∗ or orthos∗ or brace or braces | 18,909 |
| S9 | S7 OR S8 | 19,542 |
| S10 | S6 AND S9 | 2,381 |
| S11 | stance control∗ or SCO or SCOs | 214 |
| S12 | S10 AND S11 | 28 |
| S13 | ((stance control∗ N5 (knee∗ or ankle∗ or foot∗ or ortho∗ or KAFO∗)) or SCKAFO∗) | 51 |
| S14 | ((“stance and swing” N4 (KAFO∗ or knee∗ ankle∗ foot∗ or ortho∗)) or ((swing phase or stance phase) N2 (lock∗ or unlock∗))) | 15 |
| S15 | ortho∗ knee unit∗ or swing KAFO∗ or active KAFO∗ or SCOKJ∗ or eknee brace∗ or e knee brace∗ | 1 |
| S16 | C brace∗ or Cbrace∗ or ottawalk∗ | 13 |
| S17 | ((microprocessor∗ N6 (stance control∗ or swing∗ or knee∗ ankle∗ foot∗ or ortho∗ or KAFO∗)) or MPSSCO∗ or MP SSCO∗) | 14 |
| S18 | (dynamic KAFO∗ or (dynamic knee∗ N2 (ortho∗ or brace∗))) | 10 |
| S19 | ((electromechanical or electro mechanical or electronic∗) N2 (KAFO∗ or knee∗ ankle∗ or stance control∗ or knee joint∗)) | 8 |
| S20 | ((mechanical∗ N2 control∗ N2 knee∗) or (mechanical N2 knee ankle foot ortho∗)) | 9 |
| S21 | ((power∗ N4 (knee∗ ankle∗ foot∗ or (knee N3 ortho∗) or KAFO∗)) or PKAFO∗) | 7 |
| S22 | (e mag∗ N2 (control∗ or system∗ or activ∗ or KAFO∗)) | 1 |
| S23 | sensor walk∗ | 20 |
| S24 | ((free walk∗ or freewalk∗) N5 (otto bock∗ or ottobock∗ or KAFO∗ or ortho∗ or stance control∗ or microprocess∗ or mechanic∗ or electronic∗)) | 2 |
| S25 | ((otto bock∗ or ottobock∗) N5 (KAFO∗ or ortho∗ or stance control∗ or microprocess∗ or mechanic∗ or electronic∗ or e mag∗)) | 18 |
| S26 | (Becker N3 (ortho∗ or e-knee∗ or eknee∗ or stride∗ or fullstride∗ or safety∗ or UTX∗ or mechanic∗ or microprocess∗ or stance control∗ or KAFO∗)) | 3 |
| S27 | ((Horton or Fillauer∗) N4 (stance control∗ or ortho∗ or mechanic∗ or microprocess∗ or electronic∗ or KAFO∗)) | 0 |
| S28 | S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 | 148 |
| S29 | S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 Limiters – English Language | 147 |
| S30 | PT (Case Study or Commentary or Editorial or Letter or Proceedings) | 1,212,586 |
| S31 | S29 NOT S30 | 130 |
Economic Evidence Search
Search date: July 22, 2020
Databases searched: Ovid MEDLINE, Embase, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, Centre for Reviews and Dissemination (CRD) Health Technology Assessment Database, National Health Service (NHS) Economic Evaluation Database and EBSCO Cumulative Index to Nursing & Allied Health Literature (CINAHL)
Database segments: EBM Reviews – Cochrane Central Register of Controlled Trials <June 2020>, EBM Reviews – Cochrane Database of Systematic Reviews <2005 to July 16, 2020>, EBM Reviews – Health Technology Assessment <4th Quarter 2016>, EBM Reviews – NHS Economic Evaluation Database <1st Quarter 2016>, Embase <1980 to 2020 Week 29>, Ovid MEDLINE(R) ALL <1946 to July 21, 2020>
Search strategy:
-
1
exp Gait/ (83845)
-
2
exp Gait Disorders, Neurologic/ (16683)
-
3
gait∗.ti,ab,kf. (133248)
-
4
Joint Instability/ (32433)
-
5
(knee∗ adj2 (instabili∗ or stabili∗ or unstabl∗)).ti,ab,kf. (8226)
-
6
or/1-5 (195354)
-
7
Orthotic Devices/ (12963)
-
8
Foot Orthoses/ (2531)
-
9
(orthot∗ or orthos∗).ti,ab,kf. (138068)
-
10
Braces/ (14666)
-
11
(brace or braces).ti,ab,kf. (15643)
-
12
or/7-11 (164896)
-
13
6 and 12 (9114)
-
14
(stance control∗ or SCO or SCOs).ti,ab,kf. (3808)
-
15
13 and 14 (79)
-
16
((stance control∗ adj5 (knee∗ or ankle∗ or foot∗ or ortho∗ or KAFO∗)) or SCKAFO∗).ti,ab,kf. (101)
-
17
((“stance and swing” adj4 (KAFO∗ or knee∗ ankle∗ foot∗ or ortho∗)) or ((swing phase or stance phase) adj2 (lock∗ or unlock∗))).ti,ab,kf. (36)
-
18
(ortho∗ knee unit∗ or swing KAFO∗ or active KAFO∗ or SCOKJ∗ or eknee brace∗ or e knee brace∗).ti,ab,kf. (2)
-
19
(C brace∗ or Cbrace∗ or ottawalk∗).ti,ab,kf. (25)
-
20
((microprocessor∗ adj6 (stance control∗ or swing∗ or knee∗ ankle∗ foot∗ or ortho∗ or KAFO∗)) or MPSSCO∗ or MP SSCO∗).ti,ab,kf. (32)
-
21
(dynamic KAFO∗ or (dynamic knee∗ adj2 (ortho∗ or brace∗))).ti,ab,kf. (46)
-
22
((electronic∗ or electromechanical or electro mechanical) adj4 (KAFO∗ or knee∗ ankle∗ or stance control∗ or (joint∗ adj4 unlock∗) or knee joint∗)).ti,ab,kf. (34)
-
23
((mechanical∗ adj2 control∗ adj2 knee∗) or (mechanical adj2 knee ankle foot ortho∗)).ti,ab,kf. (21)
-
24
((power∗ adj4 (knee∗ ankle∗ foot∗ or (knee adj3 ortho∗) or KAFO∗)) or PKAFO∗).ti,ab,kf. (28)
-
25
(e mag∗ adj2 (control∗ or system∗ or activ∗ or KAFO∗)).ti,ab,kf. (8)
-
26
sensor walk∗.ti,ab,kf. (13)
-
27
((free walk∗ or freewalk∗) adj5 (otto bock∗ or ottobock∗ or KAFO∗ or ortho∗ or stance control∗ or microprocess∗ or mechanic∗ or electronic∗)).ti,ab,kf. (8)
-
28
((otto bock∗ or ottobock∗) adj5 (KAFO∗ or ortho∗ or stance control∗ or microprocess∗ or mechanic∗ or electronic∗ or e mag∗)).ti,ab,kf. (44)
-
29
(Becker adj3 (ortho∗ or e-knee∗ or eknee∗ or stride∗ or fullstride∗ or safety∗ or UTX∗ or mechanic∗ or microprocess∗ or stance control∗ or KAFO∗)).ti,ab,kf. (5)
-
30
((Horton or Fillauer∗) adj4 (stance control∗ or ortho∗ or mechanic∗ or microprocess∗ or electronic∗ or KAFO∗)).ti,ab,kf. (4)
-
31
or/15-30 (334)
-
32
31 use coch,clhta,cleed (0)
-
33
economics/ (257786)
-
34
economics, medical/ or economics, pharmaceutical/ or exp economics, hospital/ or economics, nursing/ or economics, dental/ (870306)
-
35
economics.fs. (436426)
-
36
(econom∗ or price or prices or pricing or priced or discount∗ or expenditure∗ or budget∗ or pharmacoeconomic∗ or pharmaco-economic∗).ti,ab,kf. (964226)
-
37
exp “costs and cost analysis”/ (603753)
-
38
(cost or costs or costing or costly).ti. (280814)
-
39
cost effective∗.ti,ab,kf. (355202)
-
40
(cost∗ adj2 (util∗ or efficacy∗ or benefit∗ or minimi∗ or analy∗ or saving∗ or estimate∗ or allocation or control or sharing or instrument∗ or technolog∗)).ab,kf. (232667)
-
41
models, economic/ (13764)
-
42
markov chains/ or monte carlo method/ (87361)
-
43
(decision adj1 (tree∗ or analy∗ or model∗)).ti,ab,kf. (46691)
-
44
(markov or markow or monte carlo).ti,ab,kf. (140157)
-
45
quality-adjusted life years/ (43411)
-
46
(QOLY or QOLYs or HRQOL or HRQOLs or QALY or QALYs or QALE or QALEs).ti,ab,kf. (82342)
-
47
((adjusted adj1 (quality or life)) or (willing∗ adj2 pay) or sensitivity analys∗s).ti,ab,kf. (134876)
-
48
or/33-47 (2718008)
-
49
31 and 48 (45)
-
50
49 use medall,cctr (21)
-
51
or/32,50 (21)
-
52
limit 51 to english language [Limit not valid in CDSR; records were retained] (20)
-
53
gait/ (82697)
-
54
exp gait disorder/ (26878)
-
55
gait∗.tw,kw. (136255)
-
56
exp joint instability/ (36681)
-
57
(knee∗ adj2 (instabili∗ or stabili∗ or unstabl∗)).tw,kw. (8467)
-
58
or/53-57 (206430)
-
59
orthotics/ (3485)
-
60
exp orthosis/ (46363)
-
61
(orthot∗ or orthos∗ or brace or braces).tw,kw,dv. (154333)
-
62
or/59-61 (183682)
-
63
58 and 62 (10949)
-
64
(stance control∗ or SCO or SCOs).tw,kw,dv. (3839)
-
65
63 and 64 (82)
-
66
((stance control∗ adj5 (knee∗ or ankle∗ or foot∗ or ortho∗ or KAFO∗)) or SCKAFO∗).tw,kw,dv. (105)
-
67
((“stance and swing” adj4 (KAFO∗ or knee∗ ankle∗ foot∗ or ortho∗)) or ((swing phase or stance phase) adj2 (lock∗ or unlock∗))).tw,kw,dv. (38)
-
68
(ortho∗ knee unit∗ or swing KAFO∗ or active KAFO∗ or SCOKJ∗ or eknee brace∗ or e knee brace∗).tw,kw,dv. (2)
-
69
(C brace∗ or Cbrace∗ or ottawalk∗).tw,kw,dv. (27)
-
70
((microprocessor∗ adj6 (stance control∗ or swing∗ or knee∗ ankle∗ foot∗ or ortho∗ or KAFO∗)) or MPSSCO∗ or MP SSCO∗).tw,kw,dv. (34)
-
71
(dynamic KAFO∗ or (dynamic knee∗ adj2 (ortho∗ or brace∗))).tw,kw,dv. (49)
-
72
((electronic∗ or electromechanical or electro mechanical) adj4 (KAFO∗ or knee∗ ankle∗ or stance control∗ or (joint∗ adj4 unlock∗) or knee joint∗)).tw,kw,dv. (34)
-
73
((mechanical∗ adj2 control∗ adj2 knee∗) or (mechanical adj2 knee ankle foot ortho∗)).tw,kw,dv. (22)
-
74
((power∗ adj4 (knee∗ ankle∗ foot∗ or (knee adj3 ortho∗) or KAFO∗)) or PKAFO∗).tw,kw,dv. (29)
-
75
(e mag∗ adj2 (control∗ or system∗ or activ∗ or KAFO∗)).tw,kw,dv. (9)
-
76
sensor walk∗.tw,kw,dv. (20)
-
77
((free walk∗ or freewalk∗) adj5 (otto bock∗ or ottobock∗ or KAFO∗ or ortho∗ or stance control∗ or microprocess∗ or mechanic∗ or electronic∗)).tw,kw,dv. (10)
-
78
((otto bock∗ or ottobock∗) adj5 (KAFO∗ or ortho∗ or stance control∗ or microprocess∗ or mechanic∗ or electronic∗ or e mag∗)).tw,kw,dv. (50)
-
79
(Becker adj3 (ortho∗ or e-knee∗ or eknee∗ or stride∗ or fullstride∗ or safety∗ or UTX∗ or mechanic∗ or microprocess∗ or stance control∗ or KAFO∗)).tw,kw,dv. (8)
-
80
((Horton or Fillauer∗) adj4 (stance control∗ or ortho∗ or mechanic∗ or microprocess∗ or electronic∗ or KAFO∗)).tw,kw,dv. (6)
-
81
or/65-80 (356)
-
82
Economics/ (257786)
-
83
Health Economics/ or Pharmacoeconomics/ or Drug Cost/ or Drug Formulary/ (132927)
-
84
Economic Aspect/ or exp Economic Evaluation/ (473674)
-
85
(econom∗ or price or prices or pricing or priced or discount∗ or expenditure∗ or budget∗ or pharmacoeconomic∗ or pharmaco-economic∗).tw,kw. (990932)
-
86
exp “Cost”/ (603753)
-
87
(cost or costs or costing or costly).ti. (280814)
-
88
cost effective∗.tw,kw. (367873)
-
89
(cost∗ adj2 (util∗ or efficac∗ or benefit∗ or minimi∗ or analy∗ or saving∗ or estimate∗ or allocation or control or sharing or instrument∗ or technolog∗)).ab,kw. (244781)
-
90
Monte Carlo Method/ (69116)
-
91
(decision adj1 (tree∗ or analy∗ or model∗)).tw,kw. (50553)
-
92
(markov or markow or monte carlo).tw,kw. (145241)
-
93
Quality-Adjusted Life Years/ (43411)
-
94
(QOLY or QOLYs or HRQOL or HRQOLs or QALY or QALYs or QALE or QALEs).tw,kw. (86249)
-
95
((adjusted adj1 (quality or life)) or (willing∗ adj2 pay) or sensitivity analys∗s).tw,kw. (156041)
-
96
or/82-95 (2336623)
-
97
81 and 96 (52)
-
98
97 use emez (27)
-
99
limit 98 to english language [Limit not valid in CDSR; records were retained] (26)
-
100
52 or 99 (46)
-
101
100 use medall (16)
-
102
100 use emez (26)
-
103
100 use cctr (4)
-
104
100 use coch (0)
-
105
100 use cleed (0)
-
106
100 use clhta (0)
-
107
remove duplicates from 100 (28)
CINAHL
| # | Query | Results |
| S1 | (MH “Gait+”) | 11,944 |
| S2 | (MH “Gait Disorders, Neurologic+”) | 2,475 |
| S3 | gait∗ | 26,923 |
| S4 | (MH “Joint Instability”) | 9,217 |
| S5 | (knee∗ N2 (instabili∗ or stabili∗ or unstabl∗)) | 2,058 |
| S6 | S1 OR S2 OR S3 OR S4 OR S5 | 38,292 |
| S7 | (MH “Orthoses+”) | 10,461 |
| S8 | orthot∗ or orthos∗ or brace or braces | 18,911 |
| S9 | S7 OR S8 | 19,544 |
| S10 | S6 AND S9 | 2,381 |
| S11 | stance control∗ or SCO or SCOs | 214 |
| S12 | S10 AND S11 | 28 |
| S13 | ((stance control∗ N5 (knee∗ or ankle∗ or foot∗ or ortho∗ or KAFO∗)) or SCKAFO∗) | 51 |
| S14 | ((“stance and swing” N4 (KAFO∗ or knee∗ ankle∗ foot∗ or ortho∗)) or ((swing phase or stance phase) N2 (lock∗ or unlock∗))) | 15 |
| S15 | ortho∗ knee unit∗ or swing KAFO∗ or active KAFO∗ or SCOKJ∗ or eknee brace∗ or e knee brace∗ | 1 |
| S16 | C brace∗ or Cbrace∗ or ottawalk∗ | 13 |
| S17 | ((microprocessor∗ N6 (stance control∗ or swing∗ or knee∗ ankle∗ foot∗ or ortho∗ or KAFO∗)) or MPSSCO∗ or MP SSCO∗) | 14 |
| S18 | (dynamic KAFO∗ or (dynamic knee∗ N2 (ortho∗ or brace∗))) | 10 |
| S19 | ((electromechanical or electro mechanical or electronic∗) N2 (KAFO∗ or knee∗ ankle∗ or stance control∗ or knee joint∗)) | 8 |
| S20 | ((mechanical∗ N2 control∗ N2 knee∗) or (mechanical N2 knee ankle foot ortho∗)) | 9 |
| S21 | ((power∗ N4 (knee∗ ankle∗ foot∗ or (knee N3 ortho∗) or KAFO∗)) or PKAFO∗) | 7 |
| S22 | (e mag∗ N2 (control∗ or system∗ or activ∗ or KAFO∗)) | 1 |
| S23 | sensor walk∗ | 20 |
| S24 | ((free walk∗ or freewalk∗) N5 (otto bock∗ or ottobock∗ or KAFO∗ or ortho∗ or stance control∗ or microprocess∗ or mechanic∗ or electronic∗)) | 2 |
| S25 | ((otto bock∗ or ottobock∗) N5 (KAFO∗ or ortho∗ or stance control∗ or microprocess∗ or mechanic∗ or electronic∗ or e mag∗)) | 18 |
| S26 | (Becker N3 (ortho∗ or e-knee∗ or eknee∗ or stride∗ or fullstride∗ or safety∗ or UTX∗ or mechanic∗ or microprocess∗ or stance control∗ or KAFO∗)) | 3 |
| S27 | ((Horton or Fillauer∗) N4 (stance control∗ or ortho∗ or mechanic∗ or microprocess∗ or electronic∗ or KAFO∗)) | 0 |
| S28 | S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 | 148 |
| S29 | (MH “Economics”) | 14,370 |
| S30 | (MH “Economic Aspects of Illness”) | 9,633 |
| S31 | (MH “Economic Value of Life”) | 649 |
| S32 | MH “Economics, Dental” | 145 |
| S33 | MH “Economics, Pharmaceutical” | 2,265 |
| S34 | MW “ec” | 185,606 |
| S35 | (econom∗ or price or prices or pricing or priced or discount∗ or expenditure∗ or budget∗ or pharmacoeconomic∗ or pharmaco-economic∗) | 300,495 |
| S36 | (MH “Costs and Cost Analysis+”) | 120,181 |
| S37 | TI cost∗ | 54,213 |
| S38 | (cost effective∗) | 42,114 |
| S39 | AB (cost∗ N2 (util∗ or efficacy∗ or benefit∗ or minimi∗ or analy∗ or saving∗ or estimate∗ or allocation or control or sharing or instrument∗ or technolog∗)) | 32,895 |
| S40 | (decision N1 (tree∗ or analy∗ or model∗)) | 8,578 |
| S41 | (markov or markow or monte carlo) | 5,863 |
| S42 | (MH “Quality-Adjusted Life Years”) | 4,723 |
| S43 | (QOLY or QOLYs or HRQOL or HRQOLs or QALY or QALYs or QALE or QALEs) | 11,950 |
| S44 | ((adjusted N1 (quality or life)) or (willing∗ N2 pay) or sensitivity analys?s) | 18,686 |
| S45 | S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 | 407,942 |
| S46 | S28 AND S45 | 16 |
| S47 | S28 AND S45 Limiters – English Language |
16 |
Grey Literature
Performed: July 23–27, 2020
Websites searched:
Alberta Health Evidence Reviews, Alberta Health Services, BC Health Technology Assessments, Canadian Agency for Drugs and Technologies in Health (CADTH), Institut national d'excellence en santé et en services sociaux (INESSS), Institute of Health Economics (IHE), McGill University Health Centre Health Technology Assessment Unit, Centre Hospitalier de l'Universite de Quebec-Universite Laval, Health Technology Assessment Database, Agency for Healthcare Research and Quality (AHRQ) Evidence-based Practice Centers, Centers for Medicare & Medicaid Services Technology Assessments, Veterans Affairs Health Services Research and Development, Institute for Clinical and Economic Review, Oregon Health Authority Health Evidence Review Commission, Washington State Health Care Authority Health Technology Reviews, National Institute for Health and Care Excellence (NICE), Healthcare Improvement Scotland, Health Technology Wales, Ireland Health Information and Quality Authority Health Technology Assessments, Australian Government Medical Services Advisory Committee, Council of Australian Governments Health Technologies, Australian Safety and Efficacy Register of New Interventional Procedures -Surgical (ASERNIP-S), Italian National Agency for Regional Health Services (AGENAS), Belgian Health Care Knowledge Centre, Ludwig Boltzmann Institute for Health Technology Assessment, Swedish Agency for Health Technology Assessment and Assessment of Social Services, Ministry of Health Malaysia Health Technology Assessment Section, Tuft's Cost-Effectiveness Analysis Registry, SickKids Paediatric Economic Database Evaluation (PEDE) database, PROSPERO, EUnetHTA, clinicaltrials.gov
Keywords used:
SCKAFO, stance control, orthoses, orthosis, SCO, knee ankle foot, c brace, microprocessor orthoses, microprocessor orthosis, mechanical orthoses, mechanical orthosis, electronic orthoses, electronic orthosis
| Clinical results (included in PRISMA): | 0 |
| Economic results (included in PRISMA): | 0 |
| Ongoing HTAs (PROSPERO/EUnetHTA): | 1 |
| Ongoing clinical trials: | 4 |
Appendix 2: Critical Appraisal of Clinical Evidence
Table A1:
Risk of Biasa Among Nonrandomized Trials (RoBANS Tool)
| Author, Year | Selection of Participants | Confounding Variables | Measurement of Exposure | Blinding of Outcome Assessments | Incomplete Outcome Reporting | Selective Outcome Reporting |
|---|---|---|---|---|---|---|
| Irby et al, 200527 | Unclear | Low | Low | Low | Unclear | High |
| Davis et al, 201026 | Unclear | Low | Low | Low | Low | Low |
| Bernhardt et al, 201125 | Unclear | Low | Low | Low | Low | High |
| Probsting et al, 201712 | Unclear | Low | Low | Low | Unclear | Low |
Possible risk-of-bias levels: low, high, and unclear.
Table A2:
GRADE Evidence Profile for the Comparison of SCKAFO and LKAFO
| Number of Studies (Design)a | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Upgrade Considerations | Quality |
|---|---|---|---|---|---|---|---|
| Walking Ability | |||||||
| Velocity 3 studies25–27 | Serious limitations (–1)b | No serious limitations | No serious limitations | No serious limitations | Undetected | None | ⊕ Very low |
| Cadence 3 studies25–27 | Serious limitations (–1)b | No serious limitations | No serious limitations | No serious limitations | Undetected | None | ⊕ Very low |
| Step Length 2 studies25–27 | Serious limitations (–1)b | No serious limitations | No serious limitations | No serious limitations | Undetected | None | ⊕ Very low |
| Swing Time 1 study26 | No serious limitations | No serious limitations | No serious limitations | Serious limitations (–1)c | Undetected | None | ⊕ Very low |
| Activities of Daily Living | |||||||
| 1 study12 | No serious limitations | No serious limitations | No serious limitations | Serious limitations (–1)d | Undetected | None | ⊕ Very low |
| Energy Consumption | |||||||
| Oxygen cost 1 study26 | No serious limitations | No serious limitations | No serious limitations | Serious limitations (–1)c | Undetected | None | ⊕ Very low |
| Physiological cost index 1 study26 | No serious limitations | No serious limitations | No serious limitations | Serious limitations (–1)c | Undetected | None | ⊕ Very low |
Abbreviations: GRADE, Grading of Recommendations Assessment, Development, and Evaluation; LKAFO, locked knee–ankle–foot orthoses; SCKAFO, stance-control knee–ankle–foot orthoses.
All studies were before and after studies (observational).
Two of the studies did not report results in text. We used software to gather estimates that may not be perfectly accurate.
Small sample size (n = 10) (e.g., not adequately powered) and no sample size calculation was done.
Small sample size (n = 5) (e.g., not adequately powered) and no sample size calculation was done.
Appendix 3: Selected Excluded Studies—Clinical Evidence
For transparency, we provide a list of studies that readers might have expected to see but that did not meet the inclusion criteria, along with the primary reason for exclusion.
| Citation | Primary Reason for Exclusion |
|---|---|
| Andrysek J, Klejman S, Kooy J. Examination of knee joint moments on the function of knee-ankle-foot orthoses during walking. J Appl Biomech. 2013;29(4):474-480. doi:10.1123/jab.29.4.474 | Wrong patient population |
| Arazpour M, Ahmadi F, Bahramizadeh M, Samadian M, Mousavi ME, Bani MA, et al. Evaluation of gait symmetry in poliomyelitis subjects: comparison of a conventional knee-ankle-foot orthosis and a new powered knee-ankle-foot orthosis. Prosthet Orthot Int. 2016;40(6):689–95. doi:10.1177/0309364615596063 | Wrong intervention |
| Arazpour M, Bani AM, Samadian M, Mousavi ME, Hutchins SW, Bahramizadeh M, et al. The physiological cost index of walking with a powered knee-ankle-foot orthosis in subjects with poliomyelitis: a pilot study. Prosthet Orthot Int. 2016;40(4):454–59. doi:10.1177/0309364615592697 | Wrong intervention |
| Arazpour M, Moradi A, Samadian M, Bahramizadeh M, Joghtaei M, Bani MA, et al. The influence of a powered knee-ankle-foot orthosis on walking in poliomyelitis subjects: a pilot study. Prosthet Orthot Int. 2016;40(3):377–383. doi:10.1177/0309364615592703 | Wrong intervention |
| Deems-Dluhy S, Hoppe-Ludwig S, Mummidisetty CK, Semik P, Heinemann AW, Jayaraman A. Microprocessor controlled knee ankle foot orthosis (KAFO) vs Stance Control vs Locked KAFO: a randomized controlled trial. Archives of Physical Medicine & Rehabilitation. 2021;102:233-44. | Wrong comparator |
| Frechtel A, Portnoy S, Raveh E, Schwartz I. Prevention of knee hyperextension in stroke patients using a knee orthosis: 3D computational gait analysis and dynamic EMG. Gait & Posture. 2013; 38(Suppl 1):S85. 10.1016/j.gaitpost.2013.07.178 | Wrong study design |
| Irby SE, Kaufman KR, Mathewson JW, Sutherland DH. Automatic control design for a dynamic knee-brace system. IEEE Trans Rehabil Eng. 1999;7(2):135–39. doi:10.1109/86.769403 | Wrong patient population |
| Irby SE, Bernhardt KA, Kaufman KR. Gait changes over time in stance control orthosis users. Prosthet Orthot Int. 2007;31(4):353–61. doi:10.1080/03093640601076909 | Wrong comparator |
| Jayaraman A, Deems-Dluhy S, Lonini L, Hoppe-Ludwig S. Micro-processor controlled knee-ankle-foot orthosis (C-Brace) vs. stance-control knee-ankle-foot orthosis (SCO) and conventional knee-ankle-foot orthosis (KAFO): functional outcomes in individuals with lower extremity impairments due to neurologic or neuromuscular disease, orthopedic disease or trauma. Prosthet Orthot Int. 2015;39(602):CN-01474600 | Wrong study design |
| Kim ES, Yoon YS, Sohn MK, Kwak SH, Choi JH, Oh JS. Effect of pneumatic compressing powered orthosis in stroke patients: preliminary study. Ann Rehabil Med. 2015;39(2):226–33. doi:10.5535/arm.2015.39.2.226 | Wrong intervention |
| Lemaire ED, Goudreau L, Yakimovich T, Kofman J. Angular-velocity control approach for stance-control orthoses. IEEE Trans Neural Syst Rehabil Eng. 2009;17(5):497-503. doi:10.1109/TNSRE.2009.2023308 | Wrong patient population |
| O'Connor J, McCaughan D, McDaid C, Booth A, Fayter D, Rodriguez-Lopez R, et al. Orthotic management of instability of the knee related to neuromuscular and central nervous system disorders: systematic review, qualitative study, survey and costing analysis. Health Technol Assess. 2016;20(55):1–262. doi:10.3310/hta20550 | Wrong intervention |
| Rafiaei M, Arazpour M, Bahramizadeh M, Farahmand F, Jamshidi N, Samadian M. Feasibility of a powered knee joint in providing stance and swing phase knee flexion when using a knee-ankle-foot orthosis. J Prosthet Orthot. 2017;29:177–82. | Wrong patient population |
| Rafiaei M, Bahramizadeh M, Arazpour M, Samadian M, Hutchins SW, Farahmand F, et al. The gait and energy efficiency of stance control knee-ankle-foot orthoses: a literature review. Prosthet Orthot Int. 2016;40(2):202–14. doi:10.1177/0309364615588346 | Wrong patient population |
| Schmalz T, Probsting E, Stinus H, Kannenberg A. A randomized controlled crossover trial to investigate locomotor capacities when using an electronic stance control orthosis. Prosthet Orthot Int. 2015; 39(604): CN-01131579 | Wrong study design |
| Schmalz T, Pröbsting E, Auberger R, Siewert G. A functional comparison of conventional knee-ankle-foot orthoses and a microprocessor-controlled leg orthosis system based on biomechanical parameters. Prosthet Orthot Int. 2016;40(2):277–86. doi:10.1177/0309364614546524 | Wrong comparator |
| Schmalz T, Pröbsting E. The microprocessor controlled C-Brace orthosis and conventional knee–ankle–foot-orthoses: comparative biomechanical evaluation of functionality. Gait & Posture. 2015;42. | Wrong study design |
| Suga T, Kameyama O, Ogawa R, Matsuura M, Oka H. Newly designed computer controlled knee-ankle-foot orthosis (intelligent orthosis). Prosthet Orthot Int. 1998;22(3):230–39. doi:10.3109/03093649809164488 | Wrong patient population |
| Tian F, Hefzy MS, Elahinia M. State of the art review of knee-ankle-foot orthoses. Ann Biomed Eng. 2015;43(2):427–41. doi:10.1007/s10439-014-1217-z | Wrong study design |
| Yakimovich T, Kofman J, Lemaire E. Design, construction and evaluation of an electromechanical stance-control knee-ankle-foot orthosis. Conf Proc IEEE Eng Med Biol Soc. 2005;2333-40. doi:10.1109/IEMBS.2005.1616934 | Wrong study design |
| Zacharias B, Kannenberg A. Clinical benefits of stance control orthosis systems: an analysis of the scientific literature. J Prosthet Orthot. 2012;24(1):2–7. doi: 10.1097/JPO.0b013e3182435db3 | Wrong study design |
Appendix 4: Selected Excluded Studies—Economic Evidence
For transparency, we provide a list of studies that readers might have expected to see but that did not meet the inclusion criteria, along with the primary reason for exclusion.
| Citation | Primary Reason for Exclusion |
|---|---|
| Cutti AG, Lettieri E, Del Maestro M, Radaelli G, Luchetti M, Verni G, et al. Stratified cost–utility analysis of C-Leg versus mechanical knees: findings from an Italian sample of transfemoral amputees. Prosthet Orthot Int. 2017;41(3):227–236. | Wrong study population: amputees Wrong intervention: C-Leg (prosthetics) |
| Seelen, HAM, Hemmen B, Schmeets AJ, Ament AJH, Evers SMA. Costs and consequences of a prosthesis with an electronically stance and swing phase controlled knee joint. Technol Disabil. 2009;21(1–2):25–34. | Wrong intervention: prosthetics |
| Kuhlmann A, Krüger H, Seidinger S, Hahn A. Cost-effectiveness and budget impact of the microprocessor-controlled knee C-Leg in transfemoral amputees with and without diabetes mellitus. Eur J Health Econ.2020;21(3):437–449. | Wrong study population: amputees Wrong intervention: C-Leg (prosthetics) |
Appendix 5: Results of Applicability Checklist for Studies Included in the Economic Literature Review
Table A3:
Assessment of the Applicability of Studies Evaluating the Cost-Effectiveness of SCKAFOs Versus LKAFOs
| Author, Year, Country | Is the study population similar to the question? | Are the interventions similar to the question? | Is the health care system studied sufficiently similar to Ontario? | Were the perspectives clearly stated? If yes, what were they? | Are all direct effects included? Are all other effects included where they are material? | Are all future costs and outcomes discounted? If yes, at what rate? | Is the value of health effects expressed in terms of quality-adjusted life-years? | Are costs and outcomes from other sectors fully and appropriately measured and valued? | Overall Judgmenta |
|---|---|---|---|---|---|---|---|---|---|
| O'Connor et al, 2016 | Partiallyb | Noc | Yes | Yes, NHS, Payer | Yes | No | NA | No | Partially applicable |
Abbreviations: LKAFO, locked knee–ankle–foot orthosis; NHS, National Health Service; SCKAFO, stance-control knee–ankle–foot orthosis.
Note: response options for all items were “yes,” “partially,” “no,” “unclear,” and “NA” (not applicable).
Overall judgment may be “directly applicable,” “partially applicable,” or “not applicable.”
Study population was limited to people with neuromuscular or central nervous system disorders.
LKAFO was the main intervention in the costing analysis.
Appendix 6: Calculations for ADP LKAFO Cost Estimates
Step 1: Calculate the Total Payments for ADP codes CNLCF1002; CNLCF2002; CNLCF3300, and CNLCF3323 (Assuming Full Coverage).
| CNLCF1002 | CNLCF2002 | CNLCF3300 | CNLCF3323 | Total | |
|---|---|---|---|---|---|
| Total ADP payments | $235,456.00 | $263,094.25 | $25,633.49 | $143,252.91 | $667,436.65∗ |
Step 2: Divide the Total Cost by Target Population (N = 429)
$667,436.65/429 = $1,555.80
Step 3: Calculate the Cost of the Remainder of ADP Codes Provided by Experts, Excluding CNLCF1002; CNLCF2002; CNLCF3300, and CNLCF3323 (Assuming Full Coverage)
| KAFO | ||||
|---|---|---|---|---|
| Type of Assessment/Materials/Device Components | Quantity | Unit Pricea | Total Pricea,b | ADP Funding (75%) |
| Tracing/Cast/Fit-thermoplastic AFO (CNLCF1002) | ||||
| KAFO–thermoplastic (CNLCF2002) | ||||
| Thermoplastic hinged AFO (CNLCF1250)c | 1 | 395.00 | 395.00 | 296.25 |
| Thermoplastic thigh cuff (CNLCF2070) | 1 | 236.00 | 236.00 | 177.00 |
| Pad (each) (CNLCF0010) | 8 | 16.00 | 128.00 | 96.00 |
| Pad cover (CNLCF0040) | 8 | 34.00 | 272.00 | 204.00 |
| Installation of uniplanar ankle joints (CNLCF1070) | 2 | 93.00 | 186.00 | 139.50 |
| Reinforced strap (CNLCF0100) | 5 | 42.00 | 210.00 | 157.50 |
| Joint head bending upright (CNLCF1100) | 6 | 82.00 | 492.00 | 369.00 |
| Molded patella cap (CNLCF2190) | 1 | 177.00 | 177.00 | 132.75 |
| Align and install knee joints (CNLCF2010) | 2 | 147.00 | 294.00 | 220.50 |
| External posting to AFO (CNLCF1820) | 1 | 42.00 | 42.00 | 31.50 |
| Multi-layer custom foot bed (CNLCF1730) | 1 | 142.00 | 142.00 | 106.50 |
| Installation of bale lock (CNLCF2040) | 2 | 69.00 | 138.00 | 103.50 |
| Installation of NYU stirrups (CNLCF1071) | 2 | 152.00 | 304.00 | 228.00 |
| Component costs | ||||
| Ankle joints (CNLCF3300) | ||||
| Knee-joint locking (CNLCF3323) | ||||
| Uprights (lower extremity) (CNLCF3310) | 6 | 142.00 | 852.00 | 639.00 |
| Stirrups (thermoplastic) (CNLCF3405)d | 2 | 53.00 | 106.00 | 79.50 |
| Total cost of device and time required (without codes CNLCF1002, CNLCF2002, CNLCF3300, and CNLCF3323) | 3,974.00 | |||
Abbreviations: ADR, assistive devices program; AFO, ankle–foot orthosis; KAFO, knee–ankle–foot orthosis.
Note: data retrieved from Ontario Association of Prosthetics and Orthotics, September 2020, Assistive Devices Product Manual.
All costs in 2020 CAD.
Cost of device for people who have 100% funding by ADP.
Hinged AFO controls and limits subtalar joint motion and allows for free ankle motion.
Stirrups: metal connecting thermoplastic foot shell to ankle joints.
Step 4: Add Step 2 and Step 3
$1,555.80 + $3,974.00 = $5,529.80
Total calculated with ADP submitted prices:
100% coverage: $5,529.80
75% coverage: $4,147.30
Appendix 7: Scenario Analyses—Budget Impact Analysis Results
Table A4:
Scenario Analyses—Budget Impact Analysis Results (Varying SCKAFO, Uptake, and LKAFO Parameters)
| Budget Impacta,b, c | ||||||
|---|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | Total | |
| Current Scenario | ||||||
| LKAFO 100% | 0.95 | 0.95 | 0.95 | 0.95 | 0.95 | 4.75 |
| LKAFO 75% | 1.27 | 1.27 | 1.27 | 1.27 | 1.27 | 6.33 |
| SCKAFO 100% | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| SCKAFO 75% | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Total SCKAFO | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Total (LKAFO + SCKAFO) | 2.22 | 2.22 | 2.22 | 2.22 | 2.22 | 11.08 |
| Scenario 1: New Scenario, Low Cost of a Mechanical SCKAFO | ||||||
| LKAFO 100% | 0.66 | 0.62 | 0.57 | 0.52 | 0.47 | 2.85 |
| LKAFO 75% | 0.89 | 0.82 | 0.76 | 0.70 | 0.63 | 3.80 |
| SCKAFO 100% | 0.34 | 0.40 | 0.46 | 0.51 | 0.57 | 2.28 |
| SCKAFO 75% | 0.46 | 0.53 | 0.61 | 0.68 | 0.76 | 3.04 |
| Total SCKAFOd | 0.80 | 0.93 | 1.06 | 1.20 | 1.33 | 5.32 |
| Total (LKAFO + SCKAFO) | 2.35 | 2.37 | 2.39 | 2.42 | 2.44 | 11.97 |
| Budget impact e | 0.13 | 0.16 | 0.18 | 0.20 | 0.22 | 0.89 |
| Scenario 2: New Scenario, Low Cost of an Electronic SCKAFO | ||||||
| LKAFO 100% | 0.66 | 0.62 | 0.57 | 0.52 | 0.47 | 2.85 |
| LKAFO 75% | 0.89 | 0.82 | 0.76 | 0.70 | 0.63 | 3.80 |
| SCKAFO 100% | 0.97 | 1.13 | 1.29 | 1.45 | 1.62 | 6.46 |
| SCKAFO 75% | 1.29 | 1.51 | 1.72 | 1.94 | 2.15 | 8.62 |
| Total SCKAFOd | 2.26 | 2.64 | 3.02 | 3.39 | 3.77 | 15.08 |
| Total (LKAFO + SCKAFO) | 3.81 | 4.08 | 4.35 | 4.61 | 4.88 | 21.73 |
| Budget impacte | 1.60 | 1.86 | 2.13 | 2.40 | 2.66 | 10.65 |
| Scenario 3: New Scenario, High Cost of an Electronic SCKAFO | ||||||
| LKAFO 100% | 0.66 | 0.62 | 0.57 | 0.52 | 0.47 | 2.85 |
| LKAFO 75% | 0.89 | 0.82 | 0.76 | 0.70 | 0.63 | 3.80 |
| SCKAFO 100% | 1.19 | 1.39 | 1.59 | 1.79 | 1.99 | 7.95 |
| SCKAFO 75% | 1.59 | 1.85 | 2.12 | 2.38 | 2.65 | 10.60 |
| Total SCKAFOd | 2.78 | 3.25 | 3.71 | 4.17 | 4.64 | 18.54 |
| Total (LKAFO + SCKAFO) | 4.33 | 4.69 | 5.04 | 5.39 | 5.74 | 25.19 |
| Budget impact e | 2.12 | 2.47 | 2.82 | 3.17 | 3.53 | 14.11 |
| Scenario 4: New Scenario, Low Cost of a Microprocessor SCKAFO | ||||||
| LKAFO 100% | 0.66 | 0.62 | 0.57 | 0.52 | 0.47 | 2.85 |
| LKAFO 75% | 0.89 | 0.82 | 0.76 | 0.70 | 0.63 | 3.80 |
| SCKAFO 100% | 3.89 | 4.53 | 5.18 | 5.83 | 6.48 | 25.90 |
| SCKAFO 75% | 5.18 | 6.04 | 6.91 | 7.77 | 8.63 | 34.53 |
| Total SCKAFOd | 9.07 | 10.58 | 12.09 | 13.60 | 15.11 | 60.43 |
| Total (LKAFO + SCKAFO) | 10.62 | 12.02 | 13.42 | 14.82 | 16.22 | 67.08 |
| Budget impact e | 8.40 | 9.80 | 11.20 | 12.60 | 14.00 | 56.00 |
| Scenario 5: New Scenario, High Cost of a Microprocessor SCKAFO | ||||||
| LKAFO 100% | 0.66 | 0.62 | 0.57 | 0.52 | 0.47 | 2.85 |
| LKAFO 75% | 0.89 | 0.82 | 0.76 | 0.70 | 0.63 | 3.80 |
| SCKAFO 100% | 4.60 | 5.37 | 6.13 | 6.90 | 7.67 | 30.67 |
| SCKAFO 75% | 6.13 | 7.16 | 8.18 | 9.20 | 10.22 | 40.89 |
| Total SCKAFOd | 10.73 | 12.52 | 14.31 | 16.10 | 17.89 | 71.57 |
| Total (LKAFO + SCKAFO) | 12.29 | 13.96 | 15.64 | 17.32 | 19.00 | 78.21 |
| Budget impact | 10.07 | 11.75 | 13.43 | 15.10 | 16.78 | 67.13 |
| Scenario 6: New Scenario, Slow Uptake of a SCKAFO | ||||||
| LKAFO 100% | 0.66 | 0.64 | 0.61 | 0.58 | 0.55 | 3.04 |
| LKAFO 75% | 0.89 | 0.85 | 0.81 | 0.77 | 0.73 | 4.05 |
| SCKAFO 100% | 0.50 | 0.55 | 0.60 | 0.65 | 0.70 | 3.00 |
| SCKAFO 75% | 0.67 | 0.73 | 0.80 | 0.87 | 0.93 | 4.00 |
| Total SCKAFOd | 1.17 | 1.28 | 1.40 | 1.52 | 1.63 | 7.00 |
| Total (LKAFO + SCKAFO) | 2.72 | 2.77 | 2.82 | 2.87 | 2.92 | 14.09 |
| Budget impact e | 0.50 | 0.55 | 0.60 | 0.65 | 0.70 | 3.01 |
| Scenario 7: New Scenario, Increasing Uptake of a SCKAFO | ||||||
| LKAFO 100% | 0.47 | 0.45 | 0.42 | 0.39 | 0.36 | 2.09 |
| LKAFO 75% | 0.63 | 0.60 | 0.56 | 0.52 | 0.48 | 2.79 |
| SCKAFO 100% | 0.83 | 0.88 | 0.93 | 0.98 | 1.03 | 4.66 |
| SCKAFO 75% | 1.11 | 1.18 | 1.24 | 1.31 | 1.38 | 6.22 |
| Total SCKAFOd | 1.94 | 2.06 | 2.18 | 2.29 | 2.41 | 10.88 |
| Total (LKAFO + SCKAFO) | 3.05 | 3.10 | 3.15 | 3.20 | 3.25 | 15.76 |
| Budget impact | 0.83 | 0.88 | 0.94 | 0.99 | 1.04 | 4.68 |
| Scenario 8: New Scenario, Cost of KAFO Using ADP Estimates | ||||||
| LKAFO 100% | 0.60 | 0.56 | 0.51 | 0.47 | 0.43 | 2.56 |
| LKAFO 75% | 0.80 | 0.74 | 0.68 | 0.63 | 0.57 | 3.42 |
| SCKAFO 100% | 0.50 | 0.58 | 0.67 | 0.75 | 0.83 | 3.33 |
| SCKAFO 75% | 0.67 | 0.78 | 0.89 | 1.00 | 1.11 | 4.44 |
| Total SCKAFOd | 1.17 | 1.36 | 1.55 | 1.75 | 1.94 | 7.77 |
| Total (LKAFO + SCKAFO) | 2.56 | 2.66 | 2.75 | 2.84 | 2.94 | 13.75 |
| Budget impact e | 0.57 | 0.66 | 0.76 | 0.85 | 0.95 | 3.79 |
| Scenario 9: 100% Coverage | ||||||
| LKAFO 100% | 1.85 | 1.72 | 1.58 | 1.45 | 1.32 | 7.92 |
| LKAFO 75% | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| SCKAFO 100% | 1.39 | 1.62 | 1.85 | 2.08 | 2.31 | 9.25 |
| SCKAFO 75% | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Total SCKAFOd | 1.39 | 1.62 | 1.85 | 2.08 | 2.31 | 9.25 |
| Total (LKAFO + SCKAFO) | 3.24 | 3.33 | 3.43 | 3.53 | 3.63 | 17.17 |
| Budget impact e | 1.02 | 1.12 | 1.22 | 1.32 | 1.42 | 6.09 |
Abbreviations: ADP, assistive devices program; knee-ankle-foot orthosis; LKAFO, locked KAFO; SCKAFO, stance-control KAFO.
In millions, 2020 CAD.
Numbers may be inexact due to rounding.
Assuming 36% of people received 100% ADP coverage at a cost of $10,784.49 for a SCKAFO and $6,151.00 for an LKAFO; 64% of people received 75% coverage at a cost of $8,088.37 for a SCKAFO and $4,613.25 for an LKAFO.
SCKAFO-related budget impact.
The budget impact is the difference between the total costs of the new and current scenarios.
Appendix 8: Letter of Information
Appendix 9: Interview Guide
Author contributions
This report was developed by a multidisciplinary team from Ontario Health. The clinical epidemiologist was Anna Lambrinos, the medical librarian was Corinne Holubowich, the health economics associate was Selena Hussain, the secondary health economist was Olga Gajic-Veljanoski, and the primary patient and public partnership analyst was Aroma Akhund.
Key Messages
What Is This Health Technology Assessment About?
The stability of the knee is reliant on sound anatomical structures as well as an intact nervous system and an adequate muscular system around the knee. Any adverse changes to these systems that cause muscle weakness, anatomical instability, or loss of perception of limb in space can alter knee movement, resulting in pain, falls, and limited mobility. Adverse changes that can cause knee instability include neuromuscular disease, central nervous system conditions, and trauma.
For people with knee instability, knee orthosis devices are prescribed to help with standing, walking, and performing tasks. Conventional knee–ankle–foot orthoses provide stability by locking the knee in a fully extended (i.e., straight leg) position while standing and walking; however, this creates atypical gait patterns. Stance-control knee–ankle–foot orthoses allow the knee to bend while walking to provide a more typical gait, improving stability.
This health technology assessment looked at how safe and effective stance-control knee–ankle–foot orthoses are for people with knee instability. It also looked at the budget impact of publicly funding stance-control knee–ankle–foot orthoses and at the experiences, preferences, and values of people with knee instability.
What Did This Health Technology Assessment Find?
We are uncertain if stance-control knee–ankle–foot orthoses improve walking ability, energy consumption, or activities of daily living compared with locked knee–ankle–foot orthoses.
We estimated that the additional cost to provide public funding for mechanical stance-control knee–ankle–foot orthoses in people with knee instability would range from about $0.50 million in year 1 to $0.83 million in year 5, for a total of about $3.34 million over the next 5 years.
The decision-making factors for people with knee instability varied depending on their condition, age, stage of life, and comfort with their current aids. While participants interviewed had adapted to using a locked knee–ankle–foot orthosis, many preferred a device that would provide a more typical gait. The major deterrent was the amount of time and energy required for physiotherapy.
Contributor Information
Ontario Health (Quality):
Anna Lambrinos, Corinne Holubowich, Selena Hussain, Olga Gajic-Veljanoski, and Aroma Akhund
About Us
Ontario Health is an agency of the Government of Ontario. Our mandate is to connect and coordinate our province's health care system in ways that have not been done before to help ensure that Ontarians receive the best possible care. We work to support better health outcomes, patient experiences, provider experiences and value for money spent.
For more information about Ontario Health, visit ontariohealth.ca
References
- (1).McDaid C, Fayter D, Booth A, O'Connor J, Rodriguez-Lopez R, McCaughan D, et al. Systematic review of the evidence on orthotic devices for the management of knee instability related to neuromuscular and central nervous system disorders. BMJ Open. 2017;7(9):e015927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (2).O'Connor J, McCaughan D, McDaid C, Booth A, Fayter D, Rodriguez-Lopez R, et al. Orthotic management of instability of the knee related to neuromuscular and central nervous system disorders: systematic review, qualitative study, survey and costing analysis. Health Technology Assessment (Winchester, England). 2016;20(55):1–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (3).Statistics Canada. Canadian community health survey: neurological conditions prevalence files, 2010/2011 [Internet]. 2012. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/120918/dq120918d-eng.pdf
- (4).Public Health Agency of Canada. Neurological conditions [Internet]. Ottawa: Government of Canada; 2016. [updated July 6 2016. Available from: https://cbpp-pcpe.phac-aspc.gc.ca/chronic-diseases/neurological-conditions [Google Scholar]
- (5).Johns Hopkins Medicine. Overview of nervous system disorders [Internet]. The Johns Hopkins University; 2020. [Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/overview-of-nervous-system-disorders [Google Scholar]
- (6).Pickett GE, Campos-Benitez M, Keller JL, Duggal N. Epidemiology of traumatic spinal cord injury in Canada. Spine (Phila Pa 1976). 2006;31(7):799–805. [DOI] [PubMed] [Google Scholar]
- (7).Ministry of Health and Long-Term Care. Orthotic devices product manual [Internet]. Toronto (ON): Queen's Publisher for Ontario; 2014. Available from: https://www.health.gov.on.ca/en/pro/programs/adp/information_technology/docs/orthotic_devices_manual.pdf [Google Scholar]
- (8).Lemaire ED, Goudreau L, Yakimovich T, Kofman J. Angular-velocity control approach for stance-control orthoses. IEEE Trans Neural Syst Rehabil Eng. 2009;17(5):497–503. [DOI] [PubMed] [Google Scholar]
- (9).Rafiaei M, Bahramizadeh M, Arazpour M, Samadian M, Hutchins SW, Farahmand F, et al. The gait and energy efficiency of stance control knee-ankle-foot orthoses: A literature review. Prosthet Orthot Int. 2016;40(2):202–14. [DOI] [PubMed] [Google Scholar]
- (10).Sulzer JS, Gordon KE, Dhaher YY, Peshkin MA, Patton JL. Preswing knee flexion assistance is coupled with hip abduction in people with stiff-knee gait after stroke. Stroke. 2010;41(8):1709–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (11).Rasmussen AA, Smith KM, Damiano DL. Biomechanical evaluation of the combination of bilateral stance-control knee-ankle-foot orthoses and a reciprocating gait orthosis in an adult with a spinal cord injury. Journal of Prosthetics & Orthotics (JPO). 2007;19(2):42–7. [Google Scholar]
- (12).Probsting E, Kannenberg A, Zacharias B. Safety and walking ability of KAFO users with the C-BraceR Orthotronic Mobility System, a new microprocessor stance and swing control orthosis. Prosthet Orthot Int. 2017;41(1):65–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (13).Ottobock. Ottobock advanced orthotics: stance control KAFOs and unilateral joints [Internet]. Germany: Ottobock; 2017. [cited 2020 Sep 16]. Available from: https://media.ottobock.com/orthotics/_general/files/kafo-family-brochure.pdf [Google Scholar]
- (14).2011 June status report of the Auditor General of Canada: chapter 6—regulating medical devices—Health Canada [Internet]. Ottawa (ON): Office of the Auditor General of Canada; 2021. [cited 2021 Apr 15]. Available from: https://www.oag-bvg.gc.ca/internet/english/parl_oag_201106_06_e_35374.html [Google Scholar]
- (15).Glanville JM, Arber M, Garcia S, Veale T. Sensitivity of a search filter designed to identify studies reporting health state utility values [abstract]. 2016. In: Mosaic ‘16 Paper Abstracts [Internet]. Forest Hill (MD): CadmiumCD. Available from: https://www.eventscribe.com/2016/mla/assets/Paper_Abstracts_Updated.pdf [Google Scholar]
- (16).National Institute for Health and Care Excellence. Process and methods guides. Appendix I: Quality appraisal checklist–economic evaluations [Internet]. London: The Institute; 2012. [cited 2016 Jan]. Available from: https://www.nice.org.uk/process/pmg4/chapter/appendix-i-quality-appraisal-checklist-economic-evaluations [Google Scholar]
- (17).Ministry of Health and Long-Term Care. Ontario community physiotherapy clinic program: patient information [Internet]. Toronto (ON): Queen's Publisher for Ontario; c2021. [cited 2021 March 23]. Available from: https://opa.on.ca/wp-content/uploads/CPC-Patient-Information-Sheet-2018-03-05-EN.pdf [Google Scholar]
- (18).Get government-funded physiotherapy [Internet]. Toronto (ON): Queen's Printer for Ontario; c2012-21. [updated 2021. Apr 1; cited 2021 Apr 16]. Available from: https://www.ontario.ca/page/get-physiotherapy [Google Scholar]
- (19).Brehm MA, Beelen A, Doorenbosch CA, Harlaar J, Nollet F. Effect of carbon-composite knee-ankle-foot orthoses on walking efficiency and gait in former polio patients. J Rehabil Med. 2007;39:651–7. [DOI] [PubMed] [Google Scholar]
- (20).Covidence systematic review software. Veritas Health Innovation. Melbourne (Australia). Available at: https://www.covidence.org/home.
- (21).Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2015. [Google Scholar]
- (22).Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013;66(4):408–14. [DOI] [PubMed] [Google Scholar]
- (23).Schünemann H, Brożek J, Guyatt G, Oxman A, editors. GRADE handbook [Internet]. Hamilton (ON): GRADE Working Group; 2013. [cited 2017 Dec]. Available from http://gdt.guidelinedevelopment.org/app/handbook/handbook.html [Internet]. [Google Scholar]
- (24).Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(6):e1000097. [PMC free article] [PubMed] [Google Scholar]
- (25).Bernhardt K, Oh T, Kaufman K. Stance control orthosis trial in patients with inclusion body myositis. Prosthet Orthot Int. 2011;35(1):39–44. [DOI] [PubMed] [Google Scholar]
- (26).Davis PC, Bach TM, Pereira DM. The effect of stance control orthoses on gait characteristics and energy expenditure in knee-ankle-foot orthosis users. Prosthet Orthot Int. 2010;34(2):206–15. [DOI] [PubMed] [Google Scholar]
- (27).Irby SE, Bernhardt KA, Kaufman KR. Gait of stance control orthosis users: the dynamic knee brace system. Prosthet Orthot Int. 2005;29(3):269–82. [DOI] [PubMed] [Google Scholar]
- (28).Ministry of Health and Long-Term Care. Orthotic devices: policy and administration manual [Internet]. Toronto (ON): Queen's Printer for Ontario; 2019. Available from: https://www.health.gov.on.ca/en/pro/programs/adp/policies_procedures_manuals/docs/orthotic_devices_manual.pdf [Google Scholar]
- (29).Barham L. Public and patient involvement at the UK National Institute for Health and Clinical Excellence. Patient. 2011;4(1):1–10. [DOI] [PubMed] [Google Scholar]
- (30).Messina J, Grainger DL. A pilot study to identify areas for further improvements in patient and public involvement in health technology assessments for medicines. Patient. 2012;5(3):199–211. [DOI] [PubMed] [Google Scholar]
- (31).Ontario Health Technology Advisory Committee Public Engagement Subcommittee. Public engagement for health technology assessment at Health Quality Ontario—final report from the Ontario Health Technology Advisory Committee Public Engagement Subcommittee [Internet]. Toronto (ON): Queen's Printer for Ontario; 2015. Apr [cited 2018 Apr 30]. Available from: http://www.hqontario.ca/Portals/0/documents/evidence/special-reports/report-subcommittee-20150407-en.pdf [Google Scholar]
- (32).Kvale S. Interviews: an introduction to qualitative research interviewing. Thousand Oaks (CA): Sage; 1996. [Google Scholar]
- (33).Kuzel AJ. Sampling in qualitative inquiry. In: Miller WL, Crabtree BF, editors. Doing qualitative research. Thousand Oaks (CA): Sage; 1999. p. 33–45. [Google Scholar]
- (34).Morse J. Emerging from the data: cognitive processes of analysis in qualitative research. In: Morse J, editor. Critical issues in qualitative research methods. Thousand Oaks (CA): Sage; 1994. p. 23–41. [Google Scholar]
- (35).Patton MQ. Qualitative research and evaluation methods. 3rd ed.Thousand Oaks (CA): Sage; 2002. [Google Scholar]
- (36).Strauss AL, Corbin JM. Basics of qualitative research: techniques and procedures of developing a grounded theory. 2nd ed.Thousand Oaks (CA): Sage; 1998. [Google Scholar]
- (37).Health Technology Assessment International. Introduction to health technology assessment [Internet]. Edmonton (AB): Health Technology Assessment International; 2015. [cited 2018 Apr 30]. Available from: http://www.htai.org/fileadmin/HTAi_Files/ISG/PatientInvolvement/v2_files/Resource/PCISG-Resource-Intro_to_HTA__KFacey__Jun13.pdf [Google Scholar]
- (38).Strauss AL, Corbin JM. Grounded theory research: procedures, canons, and evaluative criteria. Qual Sociol. 1990;13(1):3–21. [Google Scholar]
- (39).Strauss AL, Corbin JM. Grounded theory methodology: an overview. In: Denzin NK, Lincoln YS, editors. Handbook of qualitative research. Thousand Oaks (CA): Sage; 1994. p. 273–85. [Google Scholar]
- (40).NVivo qualitative data analysis software. QSR International. Doncaster, Victoria (Australia). Available at: https://www.qsrinternational.com/nvivo/home.