Abstract
Objectives
To investigate the prevalence and severity of external apical root resorption (EARR) volumetrically with clear aligner therapy using cone-beam computed tomography (CBCT) as well as determine the possible risk factors and develop a prediction model for EARR.
Materials and Methods
In this retrospective study, 320 incisors from 40 Class II patients treated with aligners (Invisalign) were included in this study. CBCT images were obtained at pretreatment (T0) and posttreatment (T1). Root volume was calculated by three-dimensional reconstruction of CBCT images, and apical tooth movement was measured from superimposed CBCT images. Changes in root volume were compared using paired t-tests, and the relationship between root volume loss and potential risk factors was analyzed by multiple linear regression.
Results
All of the measured incisors showed root volume loss, with an average of 11.48 ± 6.70 mm3, and the prevalence of severe resorption was 0.625%. The prediction model for EARR included variables of posttreatment sagittal root position (SRP), extraction, tooth type, and apical intrusion and extrusion displacements, with an R2 of 0.51. Age, sex, duration, pretreatment SRP, attachment, advancement, and retraction movements were excluded from the model.
Conclusions
Most incisors showed mild to moderate resorption during aligner treatment; only a minimal percentage showed severe resorption. Posttreatment SRP (which showed the highest association with EARR), extraction, tooth type, and apical intrusion and extrusion displacements were risk factors for EARR.
Keywords: Root resorption, Clear aligners, CBCT, Three-dimensional reconstruction
INTRODUCTION
External apical root resorption (EARR) induced by orthodontic treatment, defined as the permanent loss of root hard tissue, is a common and undesirable complication.1,2 Most previous studies concentrated on EARR with fixed appliances.2–5 More than 90% of the teeth with fixed appliance therapy showed histologically notable EARR, whereas radiographic studies reported a lower percentage.6–9 Between 48% and 66% of teeth showed mild to moderate resorption, and the incidence of severe resorption was between 1% and 5%.7–9 It is widely accepted that maxillary incisors are most prone to resorption, followed by mandibular incisors and first molars.2 However, no consistent conclusions can be drawn for other patient-related and treatment-related factors, such as age, sex, malocclusion, trauma, duration, extraction, and tooth movement.2–5,10
There are few studies on EARR with clear aligners, and their conclusions are still controversial.11 Most of the studies suggested that the incidence and severity of EARR with clear aligners were lower than those with fixed appliances,12–15 whereas Iglesias-Linares et al. found no significant differences between them.16 Intermittent force, light force, and shorter duration may be reasons for the minimal EARR with clear aligners.11 However, many studies on clear aligners have included relatively simple cases, which may also be associated with less resorption.13–15
Most previous studies used panoramic or periapical radiographs to evaluate EARR, which may cause distortion and overestimate or underestimate the extent of resorption. In recent studies, CBCT overcame these shortcomings and improved the accuracy in measuring root length.17,18 However, EARR is a kind of volume loss that irregularly and three-dimensionally occurs at root surfaces. Puttaravuttiporn et al.4 showed that root length may not change significantly when partial volume changes, and Wang et al.19 and Maret et al.20 demonstrated that CBCT in vivo and micro–computed tomography (CT) in vitro provided good comparability of the accuracy in volumetric measurements. Therefore, volumetric measurements using CBCT could be applied to provide more reliable information. In addition, CBCT can achieve more precise measurements of movement of the root apex than lateral cephalograms.21,22
The purpose of the study was to use CBCT to investigate the incidence and severity of EARR volumetrically in clear aligner treatment, determine the associated risk factors, and develop a prediction model for EARR.
MATERIALS AND METHODS
This retrospective study was approved by the Ethics Committee of Wuhan University (2020-B09). The sample size was calculated using PASS software (version 15.0; NCSS Statistical Software, Kaysville, Utah). Based on previous estimates of EARR with fixed appliances (R2 of 0.35), with α = 5% and β = 20%, the sample size needed for multiple linear regression (15 tested variables) was 51.23
The following inclusion criteria were applied: (1) patients had successfully completed treatment with an initial series of aligners; (2) patients showed good quality pretreatment and posttreatment CBCT data; (2) patients were nongrowing; (3) patients had Class II malocclusions; and (4) nonextraction patients had complete permanent dentition, whereas extraction patients had 4 premolars removed.
The exclusion criteria were the following: (1) previous orthodontic treatment history; (2) additional fixed appliance treatment or surgical treatment; (3) periodontitis, history of trauma, restorative or endodontic treatment on incisors; and (4) mesiodistal angulations of incisors changed greatly in the coronal plane after treatment.
The records of 813 patients treated with aligners (Invisalign, Align Technology, San Jose, Calif) in the Hospital of Stomatology, Wuhan University, from 2015 to 2019 were collected, and the records of 40 patients (n = 320 incisors) were ultimately included in this study (Table 1). All patients received orthodontic treatment with Invisalign aligners and were required to wear each aligner for 14 days for a minimum of 22 hours per day. The incisors were designed with no attachments (n = 265) or optimized attachments (n = 55). The potential risk factors of EARR, including sex, age, treatment duration, extraction or nonextraction, presence or absence of attachment, tooth type, root apex movement, and pretreatment and posttreatment sagittal root position (SRP) relative to the cortical plates were documented.
Table 1.
Clinical Characteristics of Included Participants
| Variable |
Mean, n |
SD, %a |
| Continuous variables | ||
| Age (y) | 24.1 | 5.8 |
| Treatment duration (m) | 21.45 | 7.24 |
| Categorical variables | ||
| Sex | ||
| Male | 20 | 50 |
| Female | 20 | 50 |
| Crowding | ||
| Mild (≦3 mm) | 9 | 22.5 |
| Moderate (4–7 mm) | 17 | 42.5 |
| Severe (>7 mm) | 14 | 35 |
| Deep overbite (>1/3) | 27 | 67.5 |
| Deep overjet (>3 mm) | 22 | 55 |
| Extraction (yes) | 20 | 50 |
| Interproximal reduction (yes) | 14 | 35 |
SD indicates standard deviation.
CBCT was performed before treatment (T0) and after active aligner treatment (T1) with the same device (NewTom VG, Quantitative Radiology, Verona, Italy). The volume data were exported to the DICOM format.
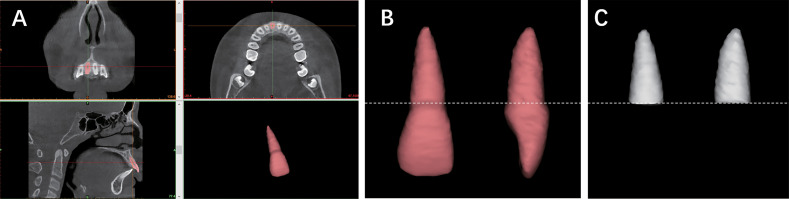
The root volume calculation was performed by three-dimensional (3D) reconstruction in Mimics software (version 20; Materialize, Leuven, Belgium; Figure 1).24 EARR was defined as a root volume loss (mm3) between T0 and T1, and the percentage of EARR was calculated as (root volume loss/original root volume) × 100%. The severity of EARR was divided into the following three degrees according to the percentage of EARR: mild (<10%), moderate (10%–20%), and severe (>20%).
Figure 1.
Measurement of root volume. (A) Thresholding segmentation of a tooth in axial, coronal, and sagittal slices. (B) A reference line was constructed to connect the highest point of the labial to palatal or lingual cementoenamel junction (CEJ), and the root was separated from the line. (C) The 3D reconstruction of the root.
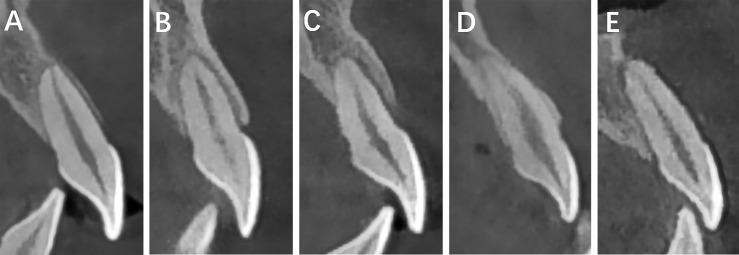
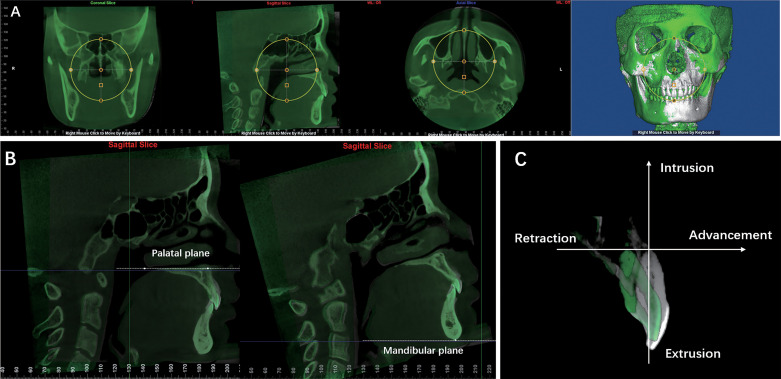
Dolphin Imaging software (version 11.8 premium; Dolphin Imaging & Management Solutions, Chatsworth, Calif) was used to evaluate the SRP and apex movement. SRP was evaluated in the midsagittal view using the classification described by Aman et al. (Figure 2).14 The apex movement was measured by CBCT superimposition (Figure 3).23 To eliminate the effect of resorption on length change, under the assumption that the length was unchanged after treatment, the position of the root apex at T1 was determined by the root length at T0, the incisor edge, and tooth length axis at T1.4
Figure 2.
Classification of root position relative to cortical plates. (A) Class I: the root is positioned against the labial cortical plate. (B) Class II: the root is centered in the alveolar housing without engaging either the labial or palatal cortical plate at the apical third of the root. (C) Class III: the root is positioned against the palatal cortical plate. (D) Class IV: at least two-thirds of the root is engaging both the labial and palatal cortical plates. (E) Class V: the root is positioned outside the labial cortical plate.
Figure 3.
Measurement of root apex movement between T0 and T1. (A) Qualitative visualization of superimposition in the axial, coronal, and sagittal views of CBCT images at T0 and T1. (B) Reference planes were set as the pretreatment palatal plane (ANS-PNS) in the maxilla and as the mandibular plane (Me-Go) in the mandible. (C) Origin of coordinates was the incisor apex at T0, and the x- and y-axes are oriented parallel and perpendicular to the reference plane, respectively. The advancement, retraction, intrusion, extrusion, and total displacement were measured in the coordinate system.
All measurements were made by two blinded observers, and the procedures were repeated for 10% of the sample after 4 weeks.
Statistical Analysis
Statistical analyses were performed using Microsoft Excel (version 2019; Microsoft, Redmond, Wash) and IBM SPSS Statistics (version 25.0; IBM, Armonk, N.Y.). Intraclass correlation coefficients (ICCs) were used to assess the intraoperator and interoperator reliabilities, and the Bland-Altman method was used to assess random errors. Descriptive statistics are reported as mean ± standard deviation. The Shapiro-Wilk test was used to test for normality, and Levene's test was used to assess the equality of variance. Paired t-tests and Wilcoxon signed-rank tests were used to compare the mean root volumes at T0 and T1. Significant variables in univariate analysis and relevant variables based on past studies were screened by multiple linear regression, with the criteria for inclusion and exclusion of variables in the model being α < 0.05 and α > 0.1, respectively.
RESULTS
The study evaluated 320 incisors from 40 patients treated with Invisalign. Table 1 shows the clinical characteristics of the participants. The root apex movement is summarized in Table 2. The ICCs indicated high intraoperator (0.9985 and 0.9984 for root volume, 0.9939 and 0.9947 for displacement) and interoperator reliabilities (0.9984 for root volume and 0.9980 for displacement). Table 3 shows the results of the Bland-Altman analysis.
Table 2.
Movement of Incisors between T0 and T1
| Parameter (mm) |
Mean |
SD |
| Intrusion | 1.13 | 0.86 |
| Extrusion | 0.92 | 0.63 |
| Advancement | 1.27 | 0.96 |
| Retraction | 1.13 | 0.78 |
| Total displacement | 1.68 | 0.97 |
Table 3.
Results of Bland-Altman Analysis for Interoperator and Intraoperator Variabilities
| Parameter |
Mean Difference |
Limits of Agreement |
| Root volume (mm3) | ||
| Inter | 0.121 | −4.3277, 4.5698 |
| Intra1 | −0.3553 | −4.4274, 3.7168 |
| Intra2 | 0.5228 | −3.7232, 4.7688 |
| Displacement (mm) | ||
| Inter | −0.004212 | −0.1671, 0.1586 |
| Intra1 | −0.00625 | −0.1696, 0.1571 |
| Intra2 | 0.001587 | −0.1538, 0.1570 |
All of the teeth showed volume reduction after treatment, with a significant decrease (11.48 ± 6.70 mm3) in the mean root volume. The measurements of each individual incisor are shown in Table 4, and the distribution of EARR severity is shown in Table 5.
Table 4.
Root Volume Loss of Individual Incisors During Orthodontic Treatmenta
| Tooth No. |
Root Volume, mm3 |
Volume Loss, mm3 |
Volume Loss, % |
||
| T0 |
T1 |
P Value |
|||
| 11 | 189.13 ± 38.02 | 174.51 ± 36.56 | < .001*** | 14.62 ± 6.86 | 7.95 ± 3.58 |
| 12 | 152.17 ± 26.84 | 139.50 ± 26.10 | < .001*** | 12.66 ± 6.78 | 8.42 ± 4.64 |
| 21 | 188.97 ± 37.60 | 176.35 ± 35.67 | < .001*** | 12.62 ± 6.40 | 6.67 ± 2.92 |
| 22 | 153.63 ± 26.33 | 141.81 ± 25.17 | < .001*** | 11.82 ± 6.50 | 7.65 ± 4.22 |
| 31 | 107.29 ± 20.92 | 97.20 ± 19.11 | < .001*** | 10.09 ± 5.81 | 9.30 ± 4.96 |
| 32 | 136.58 ± 23.02 | 126.40 ± 22.78 | < .001*** | 10.18 ± 7.28 | 7.43 ± 5.20 |
| 41 | 107.71 ± 21.25 | 98.70 ± 19.48 | < .001*** | 9.01 ± 5.52 | 8.30 ± 4.60 |
| 42 | 134.62 ± 23.79 | 123.77 ± 22.67 | < .001*** | 10.86 ± 7.17 | 8.00 ± 4.82 |
Data are presented as mean ± SD.
*** P < .001.
Table 5.
Classification of EARR Severity
| Severity |
n |
Frequency, % |
| Mild (<10%) | 227 | 70.9375 |
| Moderate (10%–20%) | 91 | 28.4375 |
| Severe (>20%) | 2 | 0.625 |
The prediction model constructed by multiple linear regression was statistically significant (F = 42.228, P < 0.001). The adjusted R2 was 0.51, and the regression coefficients are shown in Table 6. Age, sex, treatment duration, attachment, pretreatment SRP, advancement, retraction, and total apex displacement were excluded from the model after stepwise regression analysis.
Table 6.
Results of Multiple Linear Regression Predicting the Amount of Root Resorptiona
| Independent Variable |
Regression Coefficient |
Standard Error |
Significance |
| Constant | −0.456 | 1.108 | .681 |
| Posttreatment SRP | |||
| 0000: centered in alveolus | 0 | ||
| 1000: touching labial cortex | 3.104 | 0.842 | < .001*** |
| 0100: touching palatal or lingual cortex | 11.003 | 0.942 | < .001*** |
| 0010: touching both cortices | 4.506 | 1.356 | .001** |
| 0001: outside labial cortex | 8.366 | 0.919 | < .001*** |
| Extraction | |||
| 0: no | |||
| 1: yes | 2.501 | 0.559 | < .001*** |
| Tooth type | |||
| 0: mandibular incisor | |||
| 1: maxillary incisor | 2.542 | 0.543 | < .001*** |
| intrusion distance | 1.269 | 0.356 | < .001*** |
| extrusion distance | 1.451 | 0.515 | .005** |
Dependent variable: root volume change.
** P < .01; *** P < .001.
In conclusion, the EARR amount could be predicted by the following formula:
Root volume change (mm3) = 11.003 (Class III SRP at T1) + 8.336 (Class V SRP at T1) + 3.104 (Class I SRP at T1) + 4.506 (Class IV SRP at T1) + 2.501 (extraction) + 2.542 (maxillary incisors) + 1.269 (intrusion distance) + 1.451 (extrusion distance).
DISCUSSION
This was the first 3D quantitative measurement of root volume loss with Invisalign treatment. Most incisors showed mild to moderate resorption, and only 0.625% had severe resorption. Previous studies using CBCT showed rates of severe resorption (defined as a reduction in root length by more than a quarter) of 0% and 1.25%.12,14
Notably, the prevalence of EARR in this study was much higher than those reported in the literature, specifically higher than 46% reported by Krieger et al.,13 higher than 41.81% in Gay et al.,15 higher than 48.28% in Chang and Liu,25 and higher than 56.30% in Li et al.12 The differences may be attributed to the characteristics of cases and measurement methods. The incidence of EARR was lower in patients with Class I malocclusions than in patients with Class II malocclusions14 and was lower in nonextraction than in extraction cases in previous studies.3,26 The samples in the studies by Krieger et al., Gay et al., and Chang and Li were all nonextraction cases, and all of the patients in the studies by Krieger et al. and Gay et al., and more than 50% of those in the study by Chang and Liu had Class I malocclusions.13–15,25 The participants in the current study all had Class II malocclusions, and half of them had four premolars removed.
The accuracy of EARR diagnosis largely depends on the reliability of radiographic imaging. Micro-CT was considered the standard modality for estimating EARR, and previous studies demonstrated that volumetric measurements using Mimics and micro-CT were equally accurate.18,19,27 Conventional two-dimensional (2D) radiographic images may lead to missed diagnosis, late diagnosis, or underestimation of EARR severity.19,28 Ren et al.17 reported that, for periapical radiography, the correct classification rate of mild resorption on proximal surfaces was 70% and on buccolingual surfaces was 12.5%. Dudic et al.18,29 showed that periapical radiographs detected less than half of the EARR cases that were identified by micro-CT, and the prevalence evaluated by panoramic radiographs was underestimated by more than 20% compared with CBCT. CBCT demonstrated high sensitivity and excellent specificity for the detection of EARR17,29 and was applied in recent studies to measure tooth length.12,14 However, EARR is essentially a kind of volume loss, and using root length loss as the only parameter limited its validity. Thus, the accuracy of 3D quantitative measurement of volume in the present study was superior to that of 2D measurement.
In terms of risk factors, the final regression model included five variables, which were posttreatment SRP, extraction, tooth type, intrusion distance, and extrusion distance. The R2 was 0.51, which showed a stronger predictive power than previous studies, indicating these five risk factors together accounted for 51% of the variability of EARR.23,30 The posttreatment SRP was most strongly associated with EARR, which was in agreement with a previous study.14 Resorption was worst in patients with Class III SRP and least in patients with Class II SRP, which suggested that orthodontists should pay attention to incisor torque and movement in clinical practice.
It was also found that extraction increased the risk of EARR, possibly as a result of the large tooth movement and reduction in overjet when closing extraction spaces.3,8,26,31 The EARR of maxillary incisors was greater than that of mandibular incisors, which was consistent with previous studies.32,33
Regarding movement of the apex, Krieger et al.13 reported that only extrusion, and Baumrind et al.23 reported that only retraction, was associated with EARR. However, the current regression model indicated that EARR was positively related to intrusion and extrusion distances. This result was consistent with that of Chang and Liu,25 showing that the vertical movement of anterior teeth was related to root resorption. It was also consistent with the conclusion of Rudolph et al.34 that intrusive and extrusive forces produced the greatest stress at the root apex in a finite element model. Compared with the cephalometric superimposition used in previous studies,4,13,23 CBCT superimposition could better identify the anatomical structures and landmarks, thus achieving more accurate measurements.21 In addition, the current sample of nongrowing patients avoided the effects of maxillary and mandibular growth on superimposition. Although this study suggested that advancement and retraction were not independent risk factors, it is worth noting that excessive retraction may lead to the positioning of roots against the palatal or lingual plate.
No statistically significant relationships were found among root volume loss, age, and sex, which was consistent with the previous literature.3,8,13
It is controversial whether treatment duration is a risk factor. Some researchers reported that greater EARR would occur with the greater tooth movement caused by prolonged treatment time,23,26 whereas the current results agreed with other studies suggesting that duration was not an independent risk factor.3,8,32 Possible explanations are that the tooth movement was considered an independent variable in the current study and that the intermittent force in Invisalign therapy provided the potential for cementum healing.2
No significant association was found with the presence of optimized attachments. Because attachments are related to tooth movement and orthodontic force, it was included as a variable.35
Potential limitations of this study should be discussed. The radiation exposure of CBCT was higher than panoramic radiography, and future studies should try to minimize the radiation dose. This study focused on volume change, and the root surface area, which is important for tooth survival, also merits further study.36
CONCLUSIONS
Most teeth showed mild to moderate resorption after clear aligner treatment, and only a small number of teeth showed severe resorption.
Posttreatment SRP, extraction, tooth type, and intrusion and extrusion displacements were identified as risk factors for root volume loss.
REFERENCES
- 1. .Andreasen J. External root resorption: its implication in dental traumatology. Paedodontics, periodontics, orthodontics and endodontics. Int Endod J. 1985;18:109–118. doi: 10.1111/j.1365-2591.1985.tb00427.x. [DOI] [PubMed] [Google Scholar]
- 2. .Weltman B, Vig KW, Fields HW, et al. Root resorption associated with orthodontic tooth movement: a systematic review. Am J Orthod Dentofacial Orthop. 2010;137:462–476. doi: 10.1016/j.ajodo.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 3. .Artun J, Van 't Hullenaar R, Doppel D, et al. Identification of orthodontic patients at risk of severe apical root resorption. Am J Orthod Dentofacial Orthop. 2009;135:448–455. doi: 10.1016/j.ajodo.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 4. .Puttaravuttiporn P, Wongsuwanlert M, Charoemratrote C, et al. Volumetric evaluation of root resorption on the upper incisors using cone beam computed tomography after 1 year of orthodontic treatment in adult patients with marginal bone loss. Angle Orthod. 2018;88:710–718. doi: 10.2319/121717-868.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. .Sharab LY, Morford LA, Dempsey J, et al. Genetic and treatment-related risk factors associated with external apical root resorption (EARR) concurrent with orthodontia. Orthod Craniofac Res. 2015;18:71–82. doi: 10.1111/ocr.12078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. .Wierzbicki T, El-Bialy T, Aldaghreer S, et al. Analysis of orthodontically induced root resorption using micro-computed tomography (micro-CT) Angle Orthod. 2009;79:91–96. doi: 10.2319/112107-546.1. [DOI] [PubMed] [Google Scholar]
- 7. .Tieu LD, Saltaji H, Normando D, et al. Radiologically determined orthodontically induced external apical root resorption in incisors after non-surgical orthodontic treatment of Class II division 1 malocclusion: a systematic review. Prog Orthod. 2014;15:48. doi: 10.1186/s40510-014-0048-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. .Sondeijker CFW, Lamberts AA, Beckmann SH, et al. Development of a clinical practice guideline for orthodontically induced external apical root resorption. Eur J Orthod. 2020;42:115–124. doi: 10.1093/ejo/cjz034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. .Walker SL, Tieu LD, Flores-Mir C. Radiographic comparison of the extent of orthodontically induced external apical root resorption in vital and root-filled teeth: a systematic review. Eur J Orthod. 2013;35:796–802. doi: 10.1093/ejo/cjs101. [DOI] [PubMed] [Google Scholar]
- 10. .Dudic A, Giannopoulou C, Meda P, et al. Orthodontically induced cervical root resorption in humans is associated with the amount of tooth movement. Eur J Orthod. 2017;39:534–540. doi: 10.1093/ejo/cjw087. [DOI] [PubMed] [Google Scholar]
- 11. .Elhaddaoui R, Qoraich HS, Bahije L, et al. Orthodontic aligners and root resorption: a systematic review. Int Orthod. 2017;15:1–12. doi: 10.1016/j.ortho.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 12. .Li Y, Deng S, Mei L, et al. Prevalence and severity of apical root resorption during orthodontic treatment with clear aligners and fixed appliances: a cone beam computed tomography study. Prog Orthod. 2020;21:1. doi: 10.1186/s40510-019-0301-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. .Krieger E, Drechsler T, Schmidtmann I, et al. Apical root resorption during orthodontic treatment with aligners? A retrospective radiometric study. Head Face Med. 2013;9:21. doi: 10.1186/1746-160X-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. .Aman C, Azevedo B, Bednar E, et al. Apical root resorption during orthodontic treatment with clear aligners: a retrospective study using cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2018;153:842–851. doi: 10.1016/j.ajodo.2017.10.026. [DOI] [PubMed] [Google Scholar]
- 15. .Gay G, Ravera S, Castroflorio T, et al. Root resorption during orthodontic treatment with Invisalign: a radiometric study. Prog Orthod. 2017;18:12. doi: 10.1186/s40510-017-0166-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. .Iglesias-Linares A, Sonnenberg B, Solano B, et al. Orthodontically induced external apical root resorption in patients treated with fixed appliances vs removable aligners. Angle Orthod. 2017;87:3–10. doi: 10.2319/02016-101.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. .Ren H, Chen J, Deng F, et al. Comparison of cone-beam computed tomography and periapical radiography for detecting simulated apical root resorption. Angle Orthod. 2013;83:189–195. doi: 10.2319/050512-372.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. .Dudic A, Giannopoulou C, Martinez M, et al. Diagnostic accuracy of digitized periapical radiographs validated against micro-computed tomography scanning in evaluating orthodontically induced apical root resorption. Eur J Oral Sci. 2008;116:467–472. doi: 10.1111/j.1600-0722.2008.00559.x. [DOI] [PubMed] [Google Scholar]
- 19. .Wang Y, He S, Yu L, et al. Accuracy of volumetric measurement of teeth in vivo based on cone beam computer tomography. Orthod Craniofac Res. 2011;14:206–212. doi: 10.1111/j.1601-6343.2011.01525.x. [DOI] [PubMed] [Google Scholar]
- 20. .Maret D, Molinier F, Braga J, et al. Accuracy of 3D reconstructions based on cone beam computed tomography. J Dent Res. 2010;89:1465–1469. doi: 10.1177/0022034510378011. [DOI] [PubMed] [Google Scholar]
- 21. .Chien PC, Parks ET, Eraso F, et al. Comparison of reliability in anatomical landmark identification using two-dimensional digital cephalometrics and three-dimensional cone beam computed tomography in vivo. Dentomaxillofac Radiol. 2009;38:262–273. doi: 10.1259/dmfr/81889955. [DOI] [PubMed] [Google Scholar]
- 22. .Koerich L, Weissheimer A, de Menezes LM, et al. Rapid 3D mandibular superimposition for growing patients. Angle Orthod. 2017;87:473–479. doi: 10.2319/072316-574.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. .Baumrind S, Korn EL, Boyd RL. Apical root resorption in orthodontically treated adults. Am J Orthod Dentofacial Orthop. 1996;110:311–320. doi: 10.1016/s0889-5406(96)80016-3. [DOI] [PubMed] [Google Scholar]
- 24. .Aras I, Unal I, Huniler G, et al. Root resorption due to orthodontic treatment using self-ligating and conventional brackets: a cone-beam computed tomography study. J Orofac Orthop. 2018;79:181–190. doi: 10.1007/s00056-018-0133-5. [DOI] [PubMed] [Google Scholar]
- 25. .Chang C, Liu Y. Root resorption during orthodontic treatment with aligners. Chin J Orthod. 2018;25:191–195. [Google Scholar]
- 26. .Pastro JDV, Nogueira ACA, Salvatore de Freitas KM, et al. Factors associated to apical root resorption after orthodontic treatment. Open Dent J. 2018;12:331–339. doi: 10.2174/1874210601812010331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. .Kato A, Ohno N. Construction of three-dimensional tooth model by micro-computed tomography and application for data sharing. Clin Oral Invest. 2009;13:43–46. doi: 10.1007/s00784-008-0198-4. [DOI] [PubMed] [Google Scholar]
- 28. .Durack C, Patel S, Davies J, et al. Diagnostic accuracy of small volume cone beam computed tomography and intraoral periapical radiography for the detection of simulated external inflammatory root resorption. Int Endod J. 2011;44:136–147. doi: 10.1111/j.1365-2591.2010.01819.x. [DOI] [PubMed] [Google Scholar]
- 29. .Dudic A, Giannopoulou C, Leuzinger M, et al. Detection of apical root resorption after orthodontic treatment by using panoramic radiography and cone-beam computed tomography of super-high resolution. Am J Orthod Dentofacial Orthop. 2009;135:434–437. doi: 10.1016/j.ajodo.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 30. .Guo Y, He S, Gu T, et al. Genetic and clinical risk factors of root resorption associated with orthodontic treatment. Am J Orthod Dentofacial Orthop. 2016;150:283–289. doi: 10.1016/j.ajodo.2015.12.028. [DOI] [PubMed] [Google Scholar]
- 31. .Deng Y, Sun Y, Xu T. Evaluation of root resorption after comprehensive orthodontic treatment using cone beam computed tomography (CBCT): a meta-analysis. BMC Oral Health. 2018;18:116. doi: 10.1186/s12903-018-0579-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. .Lund H, Grondahl K, Hansen K, et al. Apical root resorption during orthodontic treatment. A prospective study using cone beam CT. Angle Orthod. 2012;82:480–487. doi: 10.2319/061311-390.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. .Castro IO, Alencar AHG, Valladares-Neto J, et al. Apical root resorption due to orthodontic treatment detected by cone beam computed tomography. Angle Orthod. 2013;83:196–203. doi: 10.2319/032112-240.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. .Rudolph DJ, Willes MG, Sameshima GT. A finite element model of apical force distribution from orthodontic tooth movement. Angle Orthod. 2001;71:127–131. doi: 10.1043/0003-3219(2001)071<0127:AFEMOA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 35. .Liu Y, Hu W. Force changes associated with different intrusion strategies for deep-bite correction by clear aligners. Angle Orthod. 2018;88:771–778. doi: 10.2319/121717-864.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. .Yamamoto T, Kinoshita Y, Tsuneishi M, et al. Estimation of the remaining periodontal ligament from attachment-level measurements. J Clin Periodontol. 2006;33:221–225. doi: 10.1111/j.1600-051X.2006.00888.x. [DOI] [PubMed] [Google Scholar]