Abstract
Background.
Carbapenem-resistant Enterobacteriaceae (CRE) spread regionally throughout healthcare facilities through patient transfer and cause difficult-to-treat infections. We developed a state-wide patient-sharing matrix and applied social network analyses to determine whether greater connectedness (centrality) to other healthcare facilities and greater patient sharing with long-term acute care hospitals (LTACHs) predicted higher facility CRE rates.
Methods.
We combined CRE case information from the Illinois extensively drug-resistant organism registry with measures of centrality calculated from a state-wide hospital discharge dataset to predict facility-level CRE rates, adjusting for hospital size and geographic characteristics.
Results.
Higher CRE rates were observed among facilities with greater patient sharing, as measured by degree centrality. Each additional hospital connection (unit of degree) conferred a 6% increase in CRE rate in rural facilities (relative risk [RR] = 1.056; 95% confidence interval [CI], 1.030–1.082) and a 3% increase among Chicagoland and non-Chicago urban facilities (RR = 1.027; 95% CI, 1.002–1.052 and RR = 1.025; 95% CI, 1.002–1.048, respectively). Sharing 4 or more patients with LTACHs was associated with higher CRE rates, but this association may have been due to chance (RR = 2.08; 95% CI, .85–5.08; P = .11).
Conclusions.
Hospitals with greater connectedness to other hospitals in a statewide patient-sharing network had higher CRE burden. Centrality had a greater effect on CRE rates in rural counties, which do not have LTACHs. Social network analysis likely identifies hospitals at higher risk of CRE exposure, enabling focused clinical and public health interventions.
Keywords: healthcare-associated infections, drug-resistant organisms, social network analysis
Extensively drug-resistant organisms (XDROs) are a public health threat because they are nearly untreatable with currently available antibiotics and can spread rapidly throughout a region by interfacility transfer of colonized patients [1–7]. Carbapenem-resistant Enterobacteriaceae (CRE) are increasingly prevalent XDROs associated with up to 50% mortality in infected persons [8, 9]. Klebsiella pneumoniae carbapenemase is the most common carbapenemase reported in the United States and has become a concern because of its propensity for epidemic spread [10]. Infection control interventions [11, 12] and mathematical models [13] have demonstrated that control of such antimicrobial-resistant pathogens requires regional coordination across healthcare facilities [8, 14].
CRE are endemic in Illinois healthcare facilities, especially among patients of a hospital subtype referred to as long-term acute care hospitals (LTACHs) [1]. LTACHs care for chronically critically ill patients who are at high risk of CRE carriage because of greater severity of illness, longer lengths of stay, higher antimicrobial exposure, and increased facility CRE colonization pressure compared with patients in traditional hospitals [15]. LTACHs have played an apparent role in the regional dissemination of CRE to short-term acute care hospitals [2, 3, 16]. To track CRE, the Illinois Department of Public Health (IDPH) made CRE reportable to the XDRO registry (www.xdro.org) in 2013 [14, 17].
Assessing a given hospital’s risk of CRE exposure is critical to targeting surveillance and prevention efforts. Such risk may be driven by patterns of patient movement throughout the healthcare network [13]. The extent to which facilities are linked within a network can be quantified using measures of “centrality,” that is, interconnectedness, derived from social network analysis [18]. Studies have evaluated these connections through simulations; however, relatively few have been able to associate measures of centrality with clinical microbiology results. Degree is a simple count of the number of equally weighted links that a given hospital has with all other hospitals in the network, where a link is defined as 2 hospitals sharing at least 1 patient in the calendar year [18]. Eigenvector centrality is an extension of degree centrality; rather than equally weighting all connections, it gives more weight to connections with more highly connected hospitals [19]. We hypothesized that increased patient sharing with all other hospitals (as defined by degree or eigenvector centrality) and increased patient sharing with LTACHs would each predict higher risk of CRE burden for a given hospital [20–22]. We used the XDRO registry and a state-wide hospital admission history database to evaluate the extent that connectedness to other facilities and, in particular, LTACHs influenced rates of CRE.
METHODS
Data Sources
We obtained facility-level CRE case information reported from 1 January 2014 through 31 December 2014 from the Illinois XDRO registry. To minimize surveillance bias, we removed cases only reported from screening cultures (ie, rectal or stool source for the isolate) as not every facility actively screens patients for CRE. Then, we removed duplicate case reports by retaining the earliest CRE report for each patient. Facility-level characteristics such as bed size and number of admissions were obtained from the 2013 IDPH annual hospital questionnaire [23]. The facility list was restricted to short-term acute care hospitals and LTACHs. We focused our evaluation of CRE rates on short-term acute care hospitals.
Social Network Analysis
The social network analysis included all patient admissions in IDPH’s hospital discharge dataset during the first quarter of 2013. An adjacency matrix was built in R (www.r-project.org), with each cell representing the number of unique patients who visited both corresponding facilities during the 3-month period. Because individual patients can be colonized for prolonged periods of time and because most interfacility patient sharing is not through direct transfers, we did not require same-day interfacility transfers. We calculated degree and eigenvector centrality using UCINET (Harvard Analytic Technologies, Inc., Harvard, Massachusetts).
Model Specification
The response variable was the number of facility-level CRE cases per 10 000 patient-days. Predictor variables included the 2 centrality measures (degree and eigenvector), number of beds for each facility, number of patients shared with LTACHs, county type (Chicagoland [Cook and adjacent counties], urban non-Chicago, and rural) based on the Illinois Behavioral Risk Factor Surveillance System designations (Figure 1) [24], with rural counties serving as the referent group. Bivariate associations were examined before constructing multivariable models. We used the Kruskal–Wallis nonparametric test on continuous covariates, and calculated Spearman rank correlations to test for ordinal trends. Both centrality measures were categorized into quintiles, and degree centrality was also evaluated as a discrete variable. The number of patients shared with LTACHs was split into the following 5 interval categories: zero, 1–3, 4–6, 7–9, or 10+ patients. These categories were eventually dichotomized as (<4 or ≥4) based on identifying a readily apparent departure from linearity through locally weighted scatterplot smoothing. Number of beds was evaluated as a discrete variable, and indicator variables were coded for county type. We roughly compared degree and eigenvector centrality using the Akaike information criterion (AIC) to see which measure of centrality better predicted CRE rates.
Figure 1.
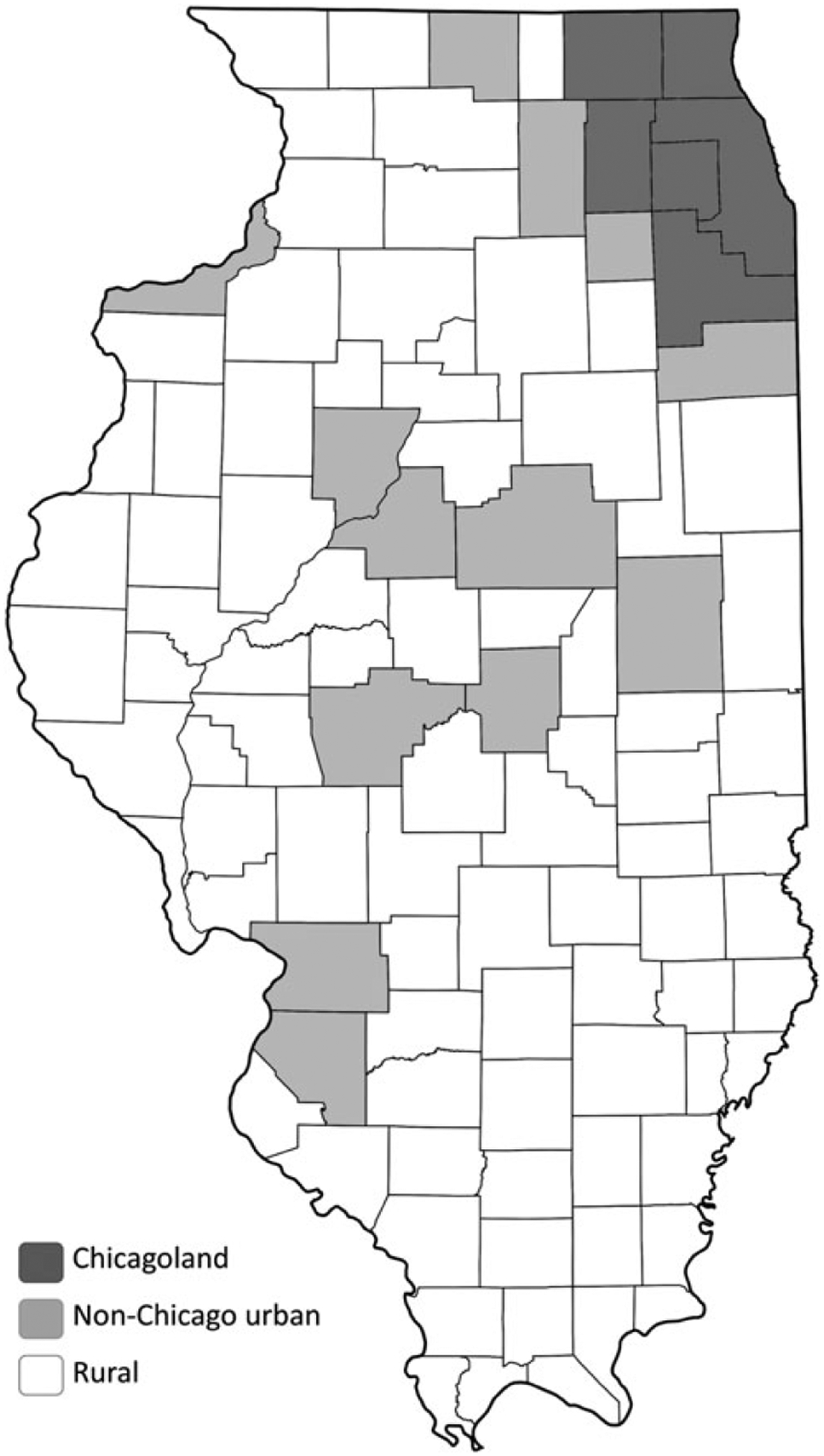
Illinois county types. Note: County types are based on Illinois Behavioral Risk Factor Surveillance System (BRFSS) designations [24]. We defined Chicagoland as Chicago + suburban Cook County + Collar County BRFSS locations.
To account for overdispersion of values, we used negative binomial regression and contrast statements to generate rate ratios across the covariates. We used an offset of log patient-days, which allowed us to interpret our response variable as a rate. It was decided a priori to adjust for number of beds in the final models to better estimate the impact of patient sharing on CRE rates. We constructed separate models for degree and eigenvector centrality and examined all potential 2-way interactions. All analyses, with the exception of the social network analysis, were performed using SAS software, version 9.4 (SAS Institute, Cary, North Carolina).
RESULTS
Of 185 Illinois hospitals, 99 (54%) reported at least 1 CRE case during the study period. There was a mean of 3.5 CRE cases per hospital, or a crude rate of 1.0 CRE case per 10 000 patient-days (Table 1). There was an average of 64 patient-sharing connections (degree) per facility, with a minimum of 1 connection and a maximum of 145 connections (Table 1). The majority of facilities (63%) reporting CRE cases were within Chicagoland counties; 80 (45%) had shared at least 1 patient with an LTACH, and 39 (21%) shared 4 or more patients with LTACHs. Among CRE cases, the mean age was 64 years. Cases were equally distributed among males (50.1%) and females (49.9%). Among case patients for whom race information was reported to the registry (61% of reports), most were African American (44%) or non-Hispanic white (43%).
Table 1.
Characteristics of Short-Term Acute Care Hospitals That Reported at Least 1 Carbapenem-Resistant Enterobacteriaceae Case to the Illinois Extensively Drug-Resistant Organism Registry During, 2014
| Hospital Characteristic | Mean | Median | Interquartile Range |
|---|---|---|---|
| Cases | 3.5 | 1.0 | 0–4 |
| Case rate (per 10 000 patient-days) | 1.0 | 0.2 | 0–1.1 |
| No. of beds | 157 | 126 | 27–234 |
| No. of admissions (per year) | 7388 | 5301 | 1040–10 892 |
| Patient-days | 35 545 | 24 181 | 4618–48 072 |
| No. of patients shared with an LTACH | 2.6 | 0 | 0–3 |
| No. of patients shared with an LTACH (Chicagoland region only) | 7.9 | 5 | 2–11 |
| Patient-Sharing Characteristics | Mean | Minimum | Maximum |
| No. of hospital connections (degree) | 64 | 1 | 145 |
| Degree (Chicagoland) | 92 | 17 | 145 |
| Degree (non-Chicago urban) | 71 | 11 | 138 |
| Degree (rural) | 27 | 1 | 86 |
N = 99.
Abbreviation: LTACH, long-term acute care hospital.
The association between degree centrality and CRE rate appeared to be linear (Loess smoothing parameter = 1.0), which indicated that specifying degree centrality as a discrete variable was appropriate. In bivariate analysis, each additional hospital connection, defined by degree, corresponded to an absolute rate increase of approximately 0.09 cases per 10 000 patient-days for each additional connection (Table 2). Sharing patients with LTACHs (4 or more patients shared in 3 months) was associated with an increase in CRE rate. CRE rates were significantly different for each county type, with the highest crude rates in Chicagoland counties (Table 2).
Table 2.
Bivariate Associations Between Facility Characteristics and Carbapenem-Resistant Enterobacteriaceae Rates (per 10 000 Patient-days) Among Illinois Acute Care Hospitals During, 2014
| Variable | Absolute Rate Differencea | 95% Confidence Interval | P Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| No. of patients shared with an LTACHb | ||||
| 0 | ref | … | ||
| 1–3 | 0.0 | −.6 | .7 | .94 |
| 4–6 | 1.2 | .1 | 2.3 | .03 |
| 6–9 | 1.2 | .0 | 2.4 | .05 |
| 10+ | 1.3 | .5 | 2.2 | .002 |
| No. of patients shared with an LTACH, dichotomous | ||||
| 0–3 | ref | … | ||
| 4+ | 1.1 | .4 | 1.9 | .003 |
| County location | ||||
| Rural | ref | … | ||
| Non-Chicago urban | 4.6 | 1.3 | 8.0 | <.001 |
| Chicagoland | 6.2 | 1.0 | 11.3 | <.001 |
| Hospital bedsc | ||||
| 0–100 | ref | … | ||
| 101–300 | 0.39 | −.28 | 1.1 | .25 |
| 300+ | −0.08 | −1.05 | .9 | .87 |
| Degree centrality (each additional connection) | 0.09 | .02 | .15 | .009 |
Abbreviation: LTACH, long-term acute care hospital.
The mean rate was 1.0 per 10 000 patient-days; thus, a rate difference of 1.0 is equivalent to a 2-fold increase above the base rate.
P value <.001 for the test of trend across the ordered categories.
P value = .75 for the test of trend.
In multivariable modeling adjusted for hospital bed size and LTACH sharing, we found that hospital degree centrality was an independent predictor CRE rate and that the strength of association varied significantly by county type (Table 3). In Chicagoland, each additional hospital connection (defined by degree centrality) was associated with approximately a 3% increase in CRE rate (Table 3); the association was similar in non-Chicago urban counties. The effect of additional connections was twice as strong in rural counties, with about a 6% increase in CRE rate with each additional connection (Table 3). The rate ratio for sharing 4 or more patients with LTACHs strongly suggested an increase rate for a facility’s exposure to LTACH patients. However, LTACH sharing and degree are strongly correlated variables, and the association with LTACH sharing may have been due to chance (P = .11). We did find that degree centrality was strongly associated with high LTACH sharing (pooled t-test, P < .0001), which suggests collinearity as a reason for the nonsignificant LTACH variable in our model. LTACH sharing was also significant in our multivariate model when we omitted the centrality variable (P = .0004). Degree and eigenvector centrality predicted CRE equally well according to AIC.
Table 3.
Adjusted Associations Between Hospital Characteristics (Centrality and Long-Term Acute Care Hospital Sharing) and Carbapenem-Resistant Enterobacteriaceae Rates (per 10 000 Patient-days) Among Short-Term Acute Care Hospitals in Illinois
| Hospital Characteristic | Rate Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|
| Degree centrality, by regiona | |||
| Chicagolandb | 1.027 | 1.002–1.052 | .03 |
| Non-Chicago urbanb | 1.025 | 1.002–1.048 | .03 |
| Rural countyb | 1.056 | 1.030–1.082 | <.0001 |
| Long-term acute care hospital sharinga | |||
| ≥4 vs <4 patients | 2.08 | .85–5.08 | .11 |
Multivariable model is adjusted for each hospital’s total number of beds and county type–degree centrality interaction.
For degree centrality, rate ratio represents increase in carbapenem-resistant Enterobacteriaceae rate for each additional hospital connection.
DISCUSSION
Using social network analysis, we evaluated the influence of patient sharing on hospital-specific rates of CRE. We found that greater hospital centrality was independently associated with higher CRE rates in the state-wide patient-sharing network. High LTACH connectedness trended toward higher hospital CRE rates, although the association was not statistically significant after adjusting for centrality; this may have been related to the strong correlation between centrality and LTACH sharing. Based on our results and those reported by other investigations, we believe that increased patient sharing with LTACHs confers an increased risk of CRE exposure. The centrality association was stronger for rural counties than for urban counties. Our results provide an important way of identifying hospitals at highest risk of CRE exposure. These findings have immediate public health implications in that early interventions should be focused on the most connected facilities, as well as those with strong connections to LTACHs. Also, centrality could be used to measure a facility’s risk for encountering CRE patients and potentially generate an expected rate of CRE using prediction models as we continue with this work. As such, even single facility outbreaks should prompt early interventions among those facilities that are strongly coupled in terms of patient sharing to try to preempt regional spread, emphasizing the key value of prospectively determining the networks.
Measures of centrality are the key quantitative expression of social network analysis. There are several centrality measures that can be used. Since we could not ascertain directionality with a fully de-identified dataset, we chose to evaluate degree and eigenvector centrality. Both measures reliably predicted an increased CRE rate. Because degree centrality is relatively easy to comprehend and performed as well as eigenvector centrality, we present the results for the degree measure.
During regional outbreaks of multidrug-resistant organism, hospitals routinely perform self-assessments of exposure risk but lack appropriate data to adequately measure such risk. State-wide patient-sharing data, which are now increasingly available through sources like the Healthcare Cost and Utilization Project [25], provide an important way to assess hospital risk of CRE exposure based on its position in regional patient-sharing networks. Studies have shown the utility of identifying the most central facilities in a healthcare network as “sentinel” hospitals, which can facilitate surveillance efforts [26]. A hospital’s awareness of its centrality within a patient-sharing network, as well as awareness of its patient sharing with LTACHs, can also provide important information about risk. Knowledge of the case rates at other facilities, coupled with information about the patient-sharing network, could motivate high-risk hospitals to actively test newly admitted patients for CRE colonization and could be used to prioritize the public health response to the highest-risk hospitals. Public health can play a critical role in identifying tightly connected hospitals and educating personnel at such facilities about their risk and need for enhanced infection control interventions. Enhanced interfacility communication can be facilitated by public health–led health information exchanges such as the Illinois XDRO registry [17].
Most connections were between LTACHs and hospitals that have higher CRE case rates and also relatively high centrality. The association with LTACHs is consistent with prior analyses that have shown the central role LTACHs have in the spread of CRE [2]. We found a threshold effect in that a hospital had to share at least 4 or more patients during our analytic time frame (3 months) to have an elevated CRE rate. This threshold makes sense because we found that many, but not all, LTACH patients are colonized with CRE [1]. Therefore, on average, an acute care hospital would need to share multiple patients with LTACHs before encountering a CRE-colonized individual. Once the threshold of 4 incidents of patient sharing with LTACHs was reached, the crude CRE rate doubled.
A major strength of our study is the novelty of using a social network variable as a predictor of CRE case rates. This has been done in some healthcare settings, for example, examination of sexually transmitted infections through networks [27–30], but social network measures have been used relatively sparingly in other epidemiological areas [20]. In contrast to prior studies of centrality, we were able to access a full year of clinical CRE data from the Illinois XDRO registry, which provides facility-level CRE rates across the entire state. Access to healthcare use data for acute- and LTACHs allowed us to quantify the magnitude of a hospital’s affinity to the network (ie, other facilities in the state). Another strength is that we had access to clinical microbiological data, which allowed us to evaluate the impact of centrality in a real-world setting rather than through simulations.
Our study has several limitations. First, although CRE reports were obtained from a mandatory surveillance system (XDRO registry), it is possible that case reporting was incomplete. Incomplete reporting could bias our findings either toward or away from the null, depending on whether underreporting was random or associated with centrality. Second, we did not have directional social network measures (ie, we know that the same patient visited 2 facilities during the time period but did not know which facility was visited first). Despite this potential limitation, we found that strong connections to the network were associated with a high rate of CRE, and we were able to evaluate patient sharing beyond simple direct transfers. Third, we did not have admissions data for nursing homes, which would have allowed us to quantify associations to the network across the broader continuum of care. Finally, variability in case rates may be related to differences in clinical culture-acquisition practices or seasonal differences in patient transfer patterns.
Combining surveillance data with social network measures such as centrality can guide large-scale interventions by identifying at-risk facilities in the network. Our work shows that by using widely available patient-sharing data, hospitals and public health officials can identify which facilities are at highest risk of CRE exposure. There is urgency for such analyses in order to intervene early and prevent the spread of XDROs.
Acknowledgments.
M. J. R. had full access to all study data and takes responsibility for data integrity and accuracy of the data analysis. We acknowledge Strengthening Health Systems through Interprofessional Education (Project SHINE) and the Illinois Department of Public Health, Division of Patient Safety and Quality. We acknowledge Kruti Doshi, Collaborative Research Unit, Cook County Health and Hospitals System, for her help with social network analysis.
Financial support.
This study was funded by the Centers for Disease Control and Prevention (CDC) cooperative agreement U54-CK000161 for the CDC Prevention Epicenter Program.
Footnotes
Potential conflicts of interests. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Lin MY, Lyles-Banks RD, Lolans K, et al. The importance of long-term acute care hospitals in the regional epidemiology of Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae. Clin Infect Dis 2013; 57:1246–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Won SY, Munoz-Price LS, Lolans K, et al. Emergence and rapid regional spread of Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae. Clin Infect Dis 2011; 53:532–40. [DOI] [PubMed] [Google Scholar]
- 3.Prabaker K, Lin MY, McNally M, et al. Transfer from high-acuity long-term care facilities is associated with carriage of Klebsiella pneumoniae carbapenemase–producing Enterobacteriaceae: a multihospital study. Infection Control 2012; 33:1193–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karkada UH, Adamic LA, Kahn JM, Iwashyna TJ. Limiting the spread of highly resistant hospital-acquired microorganisms via critical care transfers: a simulation study. Intensive Care Med 2011; 37:1633–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lesosky M, McGeer A, Simor A, Green K, Low DE, Raboud J. Effect of patterns of transferring patients among healthcare institutions on rates of nosocomial methicillin-resistant Staphylococcus aureus transmission: a Monte Carlo simulation. Infect Control Hosp Epidemiol 2011; 32:136–47. [DOI] [PubMed] [Google Scholar]
- 6.Donker T, Wallinga J, Grundmann H. Patient referral patterns and the spread of hospital-acquired infections through national health care networks. PLoS Comput Biol 2010; 6:e1000715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donker T, Wallinga J, Slack R, Grundmann H. Hospital networks and the dispersal of hospital-acquired pathogens by patient transfer. PLoS One 2012; 7:e35002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee BY, McGlone SM, Song Y, et al. Social network analysis of patient sharing among hospitals in Orange County, California. Am J Public Health 2011; 101:707–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. CRE toolkit: guidance for control of carbapenem-resistant Enterobacteriaceae (CRE). Atlanta, Georgia: CDC, 2012. [Google Scholar]
- 10.Gupta N, Limbago BM, Patel JB, Kallen AJ. Carbapenem-resistant Enterobacteriaceae: epidemiology and prevention. Clin Infect Dis 2011; 53:60–7. [DOI] [PubMed] [Google Scholar]
- 11.Ostrowsky BE, Trick WE, Sohn AH, et al. Control of vancomycin-resistant enterococcus in health care facilities in a region. N Engl J Med 2001; 344:1427–33. [DOI] [PubMed] [Google Scholar]
- 12.Schwaber MJ, Carmeli Y. An ongoing national intervention to contain the spread of carbapenem-resistant Enterobacteriaceae. Clin Infect Dis 2014; 58:697–703. [DOI] [PubMed] [Google Scholar]
- 13.Kallen M, Ricks P, Edwards J, et al. Vital signs: carbapenem-resistant Enterobacteriaceae. MMWR Morb Mortal Wkly Rep 2013; 62:165–70. [PMC free article] [PubMed] [Google Scholar]
- 14.Slayton RB, Toth D, Lee BY, et al. Vital signs: estimated effects of a coordinated approach for action to reduce antibiotic-resistant infections in health care facilities—United States. MMWR Morb Mortal Wkly Rep 2015; 64:826–31. [PMC free article] [PubMed] [Google Scholar]
- 15.Gould CV, Rothenberg R, Steinberg JP. Antibiotic resistance in long-term acute care hospitals: the perfect storm. Infect Control 2006; 27:920–5. [DOI] [PubMed] [Google Scholar]
- 16.Guh AY, Limbago BM, Kallen AJ. Epidemiology and prevention of carbapenem-resistant Enterobacteriaceae in the United States. Expert Rev Anti Infect Ther 2014; 12:565–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trick WE, Lin MY, Cheng-Leidig R, et al. Electronic public health registry of extensively drug-resistant organisms, Illinois, USA. Emerg Infect Dis 2015; 21:1725–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Borgatti SP, Everett MG, Johnson JC. Analyzing social networks. London: SAGE Publications Limited, 2013:163–9. [Google Scholar]
- 19.Bonacich P Some unique properties of eigenvector centrality. Soc Networks 2007; 29:555–64. [Google Scholar]
- 20.Simmering JE, Polgreen LA, Campbell DR, Cavanaugh JE, Polgreen PM. Hospital transfer network structure as a risk factor for Clostridium difficile infection. Infect Control Hosp Epidemiol 2015; 36:1031–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Borgatti S, Halgin D, De Jordy R. An introduction to UCINET and NetDraw. In: NIPS UCINET & NetDraw Workshop. Harvard University, MA, 2008. [Google Scholar]
- 22.Borgatti SP. Centrality and AIDS . Connections 1995; 18:112–4. [Google Scholar]
- 23.Illinois Health Facilities and Services Review Board. Hospital Profiles and Annual Bed Reports, 2014. Available at: http://www.hfsrb.illinois.gov/HospProf_ABR.htm.Accessed15 September 2015.
- 24.Illinois Behavioral Risk Factor Surveillance System. Strata Map, 2016. Available at: http://app.idph.state.il.us/brfss/.Accessed15 September 2015.
- 25.NIS, HCUP Nationwide Inpatient Sample. Healthcare cost and utilization project (HCUP) Rockville, MD: Agency for Healthcare Research and Quality, 2006. [PubMed] [Google Scholar]
- 26.Ciccolini M, Donker T, Grundmann H, Bonten MJ, Woolhouse ME. Efficient surveillance for healthcare-associated infections spreading between hospitals. Proc Natl Acad Sci USA 2014; 111:2271–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liljeros F, Edling CR, Amaral LAN. Sexual networks: implications for the transmission of sexually transmitted infections. Microb Infect 2003; 5:189–96. [DOI] [PubMed] [Google Scholar]
- 28.Doherty IA, Padian NS, Marlow C, Aral SO. Determinants and consequences of sexual networks as they affect the spread of sexually transmitted infections. J Infect Dis 2005; 191(suppl 1):S42–54. [DOI] [PubMed] [Google Scholar]
- 29.Ghani AC, Garnett GP. Risks of acquiring and transmitting sexually transmitted diseases in sexual partner networks. Sex Transm Dis 2000; 27:579–87. [DOI] [PubMed] [Google Scholar]
- 30.Schneeberger A, Mercer CH, Gregson SA, et al. Scale-free networks and sexually transmitted diseases: a description of observed patterns of sexual contacts in Britain and Zimbabwe. Sex Transm Dis 2004; 31:380–7. [DOI] [PubMed] [Google Scholar]


