Recent experience with the development of COVID-19 vaccines might, hopefully, herald a new era for the rapid development and approval of vaccines to confront the still high global burden of disease created by other infectious agents, especially in low-income regions. An example has been set for governments, the pharmaceutical industry, and regulators, that things can be done quickly. Why not build on that experience for other vaccine needs, including the introduction of new technologies, such as the use of synthetic mRNA strands, to speed up the development and manufacture of vaccine products?
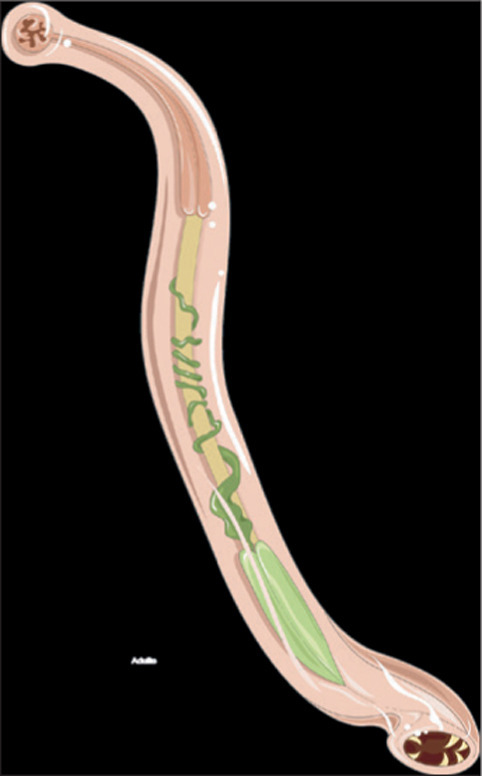
The control of neglected tropical diseases (NTDs) without vaccines remains a challenge. These infections affect many millions of people and are endemic in low-resource settings in Africa, Asia, and South America. In 2010, it was estimated that NTDs collectively caused 26 million disability-adjusted life-years lost worldwide, with helminths the greatest contributors to this burden, at roughly 40% of the total.1 Among the major helminth infections, the soil-transmitted helminths (STHs) Ancylsotoma duodenale, Necator americanus, Ascaris lumbricoides, and Trichuris trichuria, caused 50% of the total disease burden. Today, more than half of the world's population live in places endemic for STH infections,2 and although global control efforts of mass drug administration and improvements in clean water supply, sanitation, and hygiene have greatly reduced the burden of infection, the new WHO roadmap for 2021–30 for the control of NTDs documents the many challenges in making further progress over the next decade.3
The inability of the human host to generate protective immunity to reinfection by helminths means that parasite control can only be achieved by the repeated treatment of individuals. The frequency of administration required varies by helminth infection and depends on parasite life expectancy in the human host and the magnitude of the basic reproductive number, R 0, which measures transmission intensity. For STH infection, biannual or annual treatment is required.4 Considerable progress has been achieved in regions of endemic infection over the past two decades in lowering the prevalence of infection, and concomitantly reducing morbidity. However, pockets of infection remain because treatment coverage does not approach the high levels required to stop transmission (R<1), and in many populations, persistent non-adherence to drug treatment creates reservoirs of infection that maintain community-wide transmission.5 If treatment ceases, infection bounces back to pre-mass drug administration levels. As infection levels fall, maintaining interest in STH control is challenging in the face of other health priorities, especially when resources are scarce. Sustaining interest in NTD control applies not just to ministries of health, but also to the major pharmaceutical companies who, after the London Declaration,6 generously donate drugs for helminth infection control in low-income and middle-income countries. The neverending requirement for mass drug administration in the absence of transmission interruption makes clear the urgent need for other interventions.
Vaccines for helminth infections have been produced in the veterinary field for the lung worm Dictyocaulus viviparus in cattle, the nematode Haemonchus contortus in sheep, and the tapeworm Echinococcus granulosus in sheep.7 In the case of human helminth infections, encouraging progress has recently been made for schistosome vaccines with a candidate entering early-stage trials.8
In The Lancet Infectious Diseases, Paul Chapman and colleagues9 assessed the effects of a live attenuated human hookworm vaccine—an interesting step forward. The study involved a trial (part one to assess dosing and part two a randomised, placebo-controlled challenge study) with volunteers being inoculated with a live ultraviolet C light-attenuated N americanus larvae vaccine. Numbers were low in the randomised trial, with five participants in the placebo group and ten in the vaccine group, but no serious adverse events were recorded after vaccination or when the participants were challenged with live hookworm larvae. Clear humoral and cellular immunological markers of exposure to parasite antigens were recorded, but this is also true with people in endemic areas of infection who are repeatedly reinfected. Of greater interest, however, was the observation that larval output in faeces in the vaccinated group was significantly lower than in the placebo group. The vaccine did not fully protect against infection, but it did reduce transmission-stage output. Partially efficacious vaccines that both lower worm burden and reduce transmission would be of great value to augment mass drug administration, provided the duration of the effect is long term (ie, many years).10
Larger studies are required, as are plans to assess the duration of the protective effect, to move to phase 3 studies in areas with natural exposure to infection, and to assess the issues surrounding the manufacture of a vaccine that is based on live attenuated nematode larvae. Research in the field of NTD vaccine development is sparse, but perhaps the recent excitement of the rapid development of SARS-CoV-2 vaccines can act as a stimulant to remedy this situation.
© 2021 Flickr
I was a non-executive director of GlaxoSmithKline for 10 years up to May, 2018.
References
- 1.Freeman MC, Akogun O, Belizario V, Jr, et al. Challenges and opportunities for control and elimination of soil-transmitted helminth infection beyond 2020. PLoS Negl Trop Dis. 2019;13 doi: 10.1371/journal.pntd.0007201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hotez PJ, Alvarado M, Basáñez M-G, et al. The Global Burden of Disease Study 2010: interpretation and implications for the neglected tropical diseases. PLoS Negl Trop Dis. 2014;8 doi: 10.1371/journal.pntd.0002865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO . World Health Organization; 2020. Ending the neglect to attain the sustainable development goals: a road map for neglected tropical diseases 2021–2030.https://www.who.int/neglected_diseases/Ending-the-neglect-to-attain-the-SDGs-NTD-Roadmap.pdf [Google Scholar]
- 4.Anderson RM, May RM. Population dynamics of human helminth infections: control by chemotherapy. Nature. 1982;297:557–563. doi: 10.1038/297557a0. [DOI] [PubMed] [Google Scholar]
- 5.Werkman M, Wright JE, Truscott JE, et al. The impact of community-wide, mass drug administration on aggregation of soil-transmitted helminth infection in human host populations. Parasit Vectors. 2020;13:290. doi: 10.1186/s13071-020-04149-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uniting to Combat Neglected Tropical Diseases The London Declaration on Neglected Tropical Diseases. 2021. https://unitingtocombatntds.org/resource-hub/who-resources/london-declaration-neglected-tropical-diseases/
- 7.Claerebout E, Geldhof P. Helminth vaccines for ruminants. Vet Clin North Am Food Anim Pract. 2020;36:159–171. doi: 10.1016/j.cvfa.2019.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Siddiqui AA, Siddiqui SZ. Sm-p80-based schistosomiasis vaccine: preparation for human clinical trials. Trends Parasitol. 2017;33:194–201. doi: 10.1016/j.pt.2016.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chapman PR, Webster R, Giacomin P, et al. Vaccination of human participants with attenuated Necator americanus hookworm larvae and human challenge in Australia: a dose-finding study and randomised, placebo-controlled, phase 1 trial. Lancet Infect Dis. 2021 doi: 10.1016/S1473-3099(21)00153-5. published online Aug 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kura K, Truscott JE, Toor J, Anderson RM. Modelling the impact of a Schistosoma mansoni vaccine and mass drug administration to achieve morbidity control and transmission elimination. PLoS Negl Trop Dis. 2019;13 doi: 10.1371/journal.pntd.0007349. [DOI] [PMC free article] [PubMed] [Google Scholar]


