Abstract
Background:
We aimed to test the hypothesis that high-impact aerobics programme, combined with pelvic floor muscle training does not impair pelvic floor muscle function in young active women.
Methods:
A randomized control trial was conducted among active nulliparous, sport university students (age 23 ± 3 years, mean ± SD). Experimental group (n = 13) attended high-impact aerobics programme, supplemented by pelvic floor muscle training with one biofeedback session, for 6 weeks. The control group (n = 19) did not get any intervention. Before and after the experiment, we assessed pelvic floor muscle function in both groups with surface electromyography using vaginal probes. In both groups, we assessed the participants’ quality of life related to pelvic floor functions with the Incontinence Impact Questionnaires.
Results:
We recorded no impairments in neuromuscular activity of pelvic floor muscles and in quality of life in women regularly performing high-impact aerobics. What is even more positive, after 6 weeks, experimental group presented better skills both in contracting and relaxing their pelvic floor muscles, although the pre-post intervention EMG change was not statistically significant. All participants maintained good quality of life related to pelvic floor functions.
Conclusions:
High-impact aerobics, supplemented by pelvic floor muscle training can be recommended for active nulliparas.
Keywords: exercise programme, Kegel exercises, prevention, quality of life, stress urinary incontinence, young women
1. Introduction
Maintaining proper pelvic floor muscle function boosts the prevention of disorders like urinary or faecal incontinence, and pelvic organ prolapse. These dysfunctions are multifactorial, significantly impairing the quality of life, both physiologically and mentally.[1] In the long term, weakening of the pelvic floor muscles can lead to social isolation, sleep disorders and even depression. People struggling with such problems are reluctant to engage socially and give up any significant physical exercise.[2] Pelvic floor muscle training owing to the pro-health function is recommended for people of all ages. Regular pelvic floor muscle training should be recommended as both preventive and therapeutic.[2–4] High-impact aerobics include choreographed jumps and running exercises with different phases of flight. While performing individual combinations, participants are asked to move both feet off the ground at the same time, which significantly increases training intensity.[5] This is particularly important for women with high levels of advancement and high exercise capacity, which need high intensity of physical effort to benefit from exercise.[6] However, some authors discuss the potential negative impact of intensive sports activities leading to the deterioration of pelvic floor function. Various authors observed that the highest rate of stress urinary incontinence affects people with high levels of physical activity.[7–9] Increased frequency of urine leakage during high-impact exercises seems to be associated with increased intra-abdominal pressure caused by severe abdominal muscle contraction with inadequate pelvic floor muscle contraction.[8,10] Researchers suggest that intensive physical exertion without adequate pelvic floor muscle contraction can further strain, stretch, and weaken the pelvic floor muscles. Improper condition of this muscle group may expose young females to stress urinary incontinence.[11] Some authors propose the use of “the knack," that is, rapid conscious pelvic floor muscle pre-contraction before jumping, running, lifting heavy objects, as well as before any activities increasing intra-abdominal pressure.[6,12] The experts also recommend informing the participants about the effects of pelvic floor muscle training on the quality of life.[12] So far, the state of knowledge about the impact of physical activity on the pelvic floor is inconsistent. The changes in pelvic floor muscle functions, depending on the exercises introduced, are individually different.[13] The literature review concerning the characteristics of pelvic floor muscle training programmes for nulliparas provides very few preventive exercise recommendations.[14–17] Pelvic floor muscle specialists focus mainly on therapeutic programmes for people with diagnosed dysfunctions[18–20] and people at increased risk (eg, pregnant women[21,22] or postmenopausal women[23,24]). Some authors recommend participation in low-impact sports only to prevent stress incontinence.[9] Modern fitness clubs offer a very wide range of high-impact exercise classes. Safe participation in such forms of physical activities is of crucial importance for women of all ages. In this study we aimed to test a hypothesis that a structured programme of high-impact aerobics supported by pelvic floor muscle education and training improves pelvic floor neuromuscular activity, maintaining good quality of life in respect of urinary incontinence in active nulliparous women.
2. Materials and methods
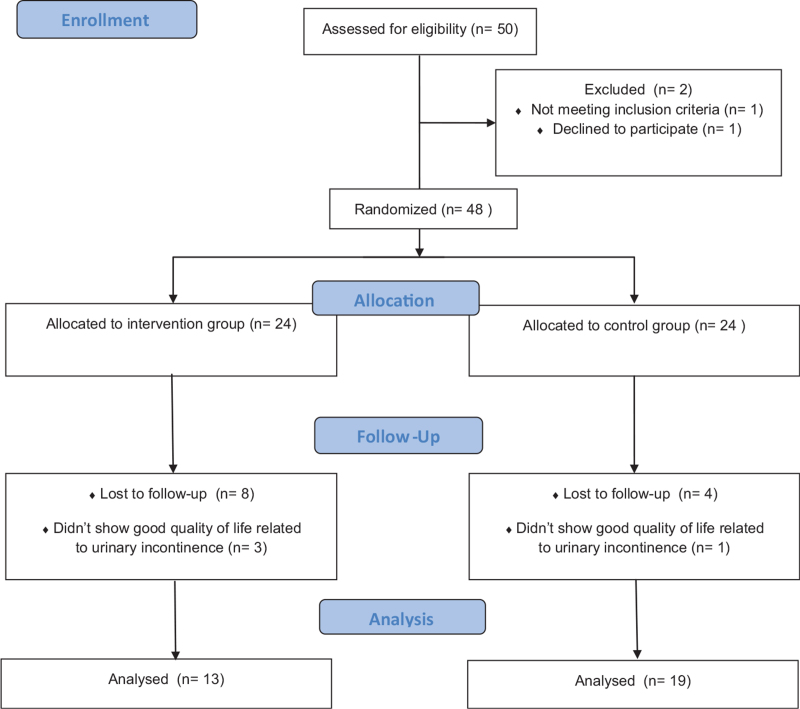
A randomized control trial was conducted among 32 female students from the Gdansk University of Physical Education and Sport, aged between 19 and 28 (22 ± 2 years; mean ± SD), voluntarily participated in the study. They were randomly placed in the experimental or control groups, with the 1:1 ratio. Only women without diagnosed urinary tract problems were eligible for the study. Women in pregnancy, with past births or contraindications to physical activity or allergy to materials used in the study were excluded. The flow of participants throughout the study is presented in Figure 1.
Figure 1.
The flow of participants through the study.
All assessments were conducted in the Laboratory of Physical Effort and Genetics in Sport at Gdansk University of Physical Education and Sport between February and May in 2016. We conducted research interventions according to the principles of the WMA Declaration of Helsinki and with the approval of the Bioethics Commission at the District Medical Chamber in Gdansk (KB - 8/14). The participants signed informed consent before commencing the tests. Research project titled: “Pelvic floor muscle training with surface electromyography" registered by ISRCTN registry at the number ISRCTN92265528, DOI 10.1186/ISRCTN92265528.
Before participating in the electromyography (EMG) assessment, all women took part in an educational lecture given by an expert in the field of pelvic floor muscle function. In a one-off educational session, they were informed about the importance of pelvic floor muscles and the impact of their function on the quality of life. Subsequently, each woman underwent pelvic floor muscle function assessment with EMG using a vaginal probe (self-applied by the participant)[25] and surface electrodes glued to the rectus abdominis muscle, the external oblique muscle, and the gluteus maximus muscle. We performed the assessments of the pelvic floor muscles with surface electromyography based on the Glazer protocol.[26] One EMG test sequence consisted of the following motor tasks: 10-second relaxation (pelvic floor muscle EMG baseline), 5 contractions lasting 10 seconds, each followed by a relaxation lasting 10 seconds, 60-second contraction followed by 10-second relaxation. The experimental group after the first EMG test sequence additionally performed all motor tasks with EMG biofeedback, observing the changes of neuromuscular activity on the computer monitor. Other synergistic muscles should have remained relaxed. Participants received the following commands: “contract" when they were to contract the pelvic floor muscles. At the “relax" command, the participants were asked to relax their entire body including their pelvic floor muscles. The commands were issued by computer software to increase data reliability The tests were carried out by a qualified physiotherapist knowledgeable in urogynaecology, as well as in the use of surface EMG. After 6 weeks of training the women underwent the second pelvic floor muscle assessment. We considered the increase in mean EMG value in contractions and the decrease in mean EMG value in relaxations to be a positive change. We used the Incontinence Impact Questionnaire (IIQ) to assess the impact of incontinence symptoms on the quality of life of participants before and after the experiment.[27] Based on research conducted by Corcos et al we classified a score >70 as low quality of life; a score of 50 to 70 indicated a moderate quality of life, and a score <50 was considered to indicate a good quality of life.[28] During the pre-intervention analysis we excluded women who did not have a good quality of life based on IIQ (Fig. 1). Since we analyzed both the neuromuscular activity of pelvic floor muscles and the impact of urinary incontinence on participants’ quality of life, with reference to these variables we use the common term “pelvic floor muscle function" in the following part of the study. All study participants were tested on the basis of the International Physical Activity Questionnaire (IPAQ) and they were classified as physically active.[29] Before the exercise programme, we assessed the exercise capacity of participants and their exercise heart rate (HR) zones for the intervention. To that end, we conducted cardiopulmonary exercise tests to exhaustion, using an electronically regulated cycle ergometer with gas analyzer (Oxycon Pro, Erich JAEGER GmbH, Hoechberg, Germany) in laboratory conditions. The method and manner of the conducting the test, together with the applied load protocol, were presented by Kostrzewa-Nowak et al.[30] The experimental group reached the following performance parameters at the initial stage before commencing the intervention exercise programme: VO2max (34,8 ± 6,3); HRmax (180 ± 15). Between the first and second pelvic floor muscle function assessments, the experimental group participated in a high-impact aerobics programme, 3 times a week for 6 weeks. We decided to implement a 6-week intervention. In many previous experiments, training effectiveness has been demonstrated after 6 weeks.[31] The individual training session included: 10 minutes aerobic warm-up, 43 minutes of the main part in the form of a choreographic layout using high-impact steps, 7 minutes of stretching and breathing exercises, and 10 minutes of pelvic floor muscle training. Each woman performed exercises with the intensity of 60% to 75% HRmax based on the cardiopulmonary assessments. During the classes, we used the music with a tempo of 140 to 152 BPM (beats per minute).[30] Pelvic floor muscle training was based on “Graduated Strength Training."[32]
In the pelvic floor muscle training, we aimed at teaching the participants how to contract and relax pelvic floor muscles properly. During each week of the experiment the training sessions contained a different set of exercises. The participants learned the basic short contraction (so called quick flicks) in the first week. The objective of the exercises in the second week was to activate the pelvic floor muscles more fully through a short gradation of the contraction. One repetition of the exercise consisted of performing 3 increasingly stronger flicks and slowly reducing the contraction until complete relaxation. The next stage of the training focused on muscle endurance by adding constant contraction up to 10 seconds. In the fourth week, 1 repetition of the exercise included: 3 more intense contractions and maintaining constant contraction for 10 seconds, extended by a short pulsation before relaxation. During the fifth week of the training, pelvic floor muscles were activated to improve muscle speed, strength and endurance. The participants repeated three times the sequence of pelvic floor muscle contractions and relaxations, according to the modified Glazer protocol.[26] In the sixth week, the participants repeated exercises from the fourth week. Additionally, to improve their ability to activate their pelvic floor muscles in everyday activities, they were asked to consciously contract their muscles before sneezing, coughing or lifting heavy objects.[32] All training sessions were supervised by a qualified fitness instructor proficient in pelvic floor muscle exercises. The control group has not receive any intervention: nor exercise nor education on pelvic floor muscle training. We asked them to continue their normal lifestyle during the experiment.
Statistical analysis was performed using Statistica 13.1 software (Statsoft, Tulsa, Oklahoma). All values are expressed as mean ± standard deviation (SD). The Shapiro–Wilk test was applied to assess the homogeneity of dispersion from the normal distribution. An unpaired t test analysis was performed to identify significantly different results at baseline. For the remaining results, we used the Mann–Whitney test. The Brown–Forsythe test was used to evaluate homogeneity of variance. We applied analysis of variance. An ANOVA Friedman's test and Dunn-Bonferroni post-hoc test was applied. Additionally, we calculated effect sizes (partial eta squared, ) with 0.01 indicating small, ≥ 0.059 medium and ≥0.138 large effect, respectively. The significance level was set at P < .05.
3. Results
Table 1 illustrates the characteristics of the experimental and control groups. Analysis of selected variables such as age, BMI and IIQ scores showed that the study groups did not statistically differ from each other before the experiment (Table 1). For quantitative analysis, we normalized raw EMG data in μV to the individual maximum voluntary contraction (MVC) of the pelvic floor muscles (expressed as % MVC). The experimental and control groups in their maximum voluntary pelvic floor muscle contractions reached pre-intervention values of 27.09 ± 8.89 μV i 26.93 ± 12.87 μV, respectively. After 6 weeks, these values have risen by 5% in the experimental group and by 2% in the control group.
Table 1.
Characteristics of the study participants.
| Variable at baseline | All participants, n = 32 | Experimental, group n = 13 | Control group, n = 19 | P |
| Age, y | 22 ± 2 | 22 ± 3 | 23 ± 2 | 0.30 |
| BMI, kg/m 2 | 21.56 ± 3.18 | 21.06 ± 1.65 | 22.15 ± 3.67 | 0.59 |
| IIQ score | 2.98 ± 4.49 | 4.4 ± 4.54 | 2 ± 4.29 | 0.10 |
| MVC, μV | 27 ± 11.26 | 27.09 ± 8.89 | 26.93 ± 12.87 | 0.97 |
| 10-s Relaxation before the test (% MVC) | 20.15 ± 14.66 | 18.57 ± 7.38 | 21.22 ± 18.19 | 0.49 |
| Mean of five 10-s maximal contractions (% MVC) | 60.61 ± 16.3 | 54.92 ± 15.74 | 64.5 ± 15.91 | 0.06 |
| Mean of five 10-s relaxations following the 10-s contractions (% MVC) | 22.8 ± 9.89 | 22.2 ± 7.19 | 23.21 ± 11.55 | 0.23 |
| 60-s contraction (% MVC) | 56.89 ± 14.5 | 54.78 ± 14.92 | 58.34 ± 14.43 | 0.88 |
| 10-s relaxation following the 60-s contraction (% MVC) | 16.55 ± 9.99 | 18.97 ± 7.58 | 14.9 ± 11.25 | 0.10 |
Values are means ± SD. The statistical significance level was obtained using Mann–Withney test (the name of a variable in italics) or unpaired t test (the name of a variable in normal font); P < .05 was considered statistically significant. BMI = body mass index, IIQ = Incontinence Impact Questionnaire, MVC = maximal voluntary contraction.
IIQ score = item responses are assigned values of 0 for “not at all,” 1 for “slightly,” 2 for “moderately," and 3 for “greatly.” The average score of items responded to is calculated. The average, which was between 0 and 3, was multiplied by 33 1/3 to put scores on a scale of 0to 100.
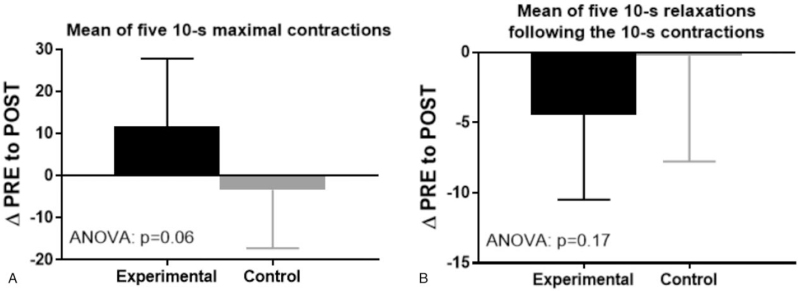
We noticed no statistically significant deterioration in the parameters of neuromuscular activity pelvic floor muscles related to participation in the high-impact aerobics programme. Additionally, in the experimental group we observed a positive trend in the pre-post intervention change in the EMG levels in all motor tasks. The experimental group achieved an increase in the mean EMG values in contractions and presented lower EMG values in relaxations. In the experimental group, we observed the most beneficial pre-post EMG change in 10-second contractions, although it was not statistically significant (P = .06). After 6 weeks, the mean EMG value in this task increased by 21% in the experimental group and decreased by 5% in the control group. We also noted a positive trend in the mean values of five 10-second relaxations following 10-second contractions. In the experimental group, this value decreased by 20%, whereas in the control group by only 1% (Fig. 2).
Figure 2.
Changes in: (A) the mean EMG of the 10-s pelvic floor muscle contractions; (B) following relaxations in the experimental and control groups after 6 weeks of the high-impact aerobics programme. Values expressed as % MVC. EMG = electromyography, MVC = maximal voluntary contraction, POST = post-intervention, PRE = pre-intervention.
In the pre-intervention Incontinence Impact Questionnaire eight women from the experimental group and four from the control group reported some symptoms of urinary incontinence (IIQ score: 4.4 ± 4.54 and 2 ± 4.29, respectively). After 6 weeks, there were six symptomatic women in the experimental group and three in the control group (IIQ score: 3.66 ± 4.82 and 1.75 ± 4.55, respectively). These changes were not statistically significant (Table 2). All women maintained good quality of life in terms of pelvic floor muscle function (IIQ score <50).
Table 2.
The comparison between experimental and control groups in the mean EMG amplitude for pelvic floor muscle activity in selected tasks and in IIQ score.
| Variables | Group | Pre-intervention EMG level (mean ± SD) | Post-intervention EMG level (mean ± SD) | Observed change | P | ES |
| MVC, μV | Experimental | 27.09 ± 8.89 | 28.44 ± 16.84 | +1.35 (+5%) | .82 | 0.00 |
| Control | 26.93 ± 12.87 | 27.51 ± 17.6 | +0.58 (+2%) | |||
| 10-s relaxation before the test (% MVC) | Experimental | 18.57 ± 7.38 | 15.3 ± 10.37 | −3.27 (−18%) | .45 | 0.10 |
| Control | 21.22 ± 18.19 | 17.35 ± 11.64 | −3.87 (−18%) | |||
| Mean of five 10-s maximal contractions (% MVC) | Experimental | 54.92 ± 15.74 | 66.67 ± 7.7 | +11.75 (+21%) | .06 | 0.03 |
| Control | 64.5 ± 15.91 | 61.14 ± 10.14 | −3.36 (−5%) | |||
| Mean of five 10-s relaxations following the 10-s contractions (% MVC) | Experimental | 22.2 ± 7.19 | 17.76 ± 8.45 | −4.44 (−20%) | .17 | 0.09 |
| Control | 23.21 ± 11.55 | 22.98 ± 10.41 | −0.23 (−1%) | |||
| 60-s Contraction (% MVC) | Experimental | 54.78 ± 14.92 | 61.85 ± 9.38 | +7.07 (+13%) | .56 | 0.03 |
| Control | 58.34 ± 14.43 | 59.78 ± 9.42 | +1.44 (+2%) | |||
| 10-s Relaxation following the 60-s contraction (% MVC) | Experimental | 18.97 ± 7.58 | 15.04 ± 10.13 | −3.93 (−21%) | .42 | 0.00 |
| Control | 14.9 ± 11.25 | 16.75 ± 10.22 | +1.85 (+12%) | |||
| IIQ | Experimental | 4.4 ± 4.54 | 3.66 ± 4.82 | −0.74 (−17%) | .69 | 0.01 |
| Control | 2 ± 4.29 | 1.75 ± 4.55 | −0.25 (−13%) |
Values are means ± SD. Analysis of variance (ANOVA) for repeated measures; P < .05 was considered statistically significant. ES (partial eta squared, ) were additionally calculated with ≥ 0.01 indicating small, ≥0.059 medium, and ≥ 0.138 large effect, respectively. ES = effect sizes, IIQ = Incontinence Impact Questionnaire, MVC = maximal voluntary contraction.
IIQ score = item responses are assigned values of 0 for “not at all,” 1 for “slightly,” 2 for moderately," and 3 for “greatly.” The average score of items responded to is calculated. The average, which was between 0 and 3, was multiplied by 33 1/3 to put scores on a scale of 0 to 100.
4. Discussion
Contrary to numerous reports concerning negative effects of high-impact physical activity on pelvic floor muscle function,[7–9] we did not find any negative changes in neuromuscular activity in nulliparous women participating in high-impact exercise. Our main finding is that high-impact aerobics programme, supplemented by pelvic floor muscle training, does not impair pelvic floor function. What is even more positive, we noted a slight improvement of participants’ skills in contracting and relaxing pelvic floor muscles.
In the experimental group, we observed an increase in EMG values in contractions (10- and 60-second contraction) and a decrease in the EMG values in relaxations (baseline, relaxations following 10- and 60-second contractions), although the pre-post intervention change was not statistically significant. In the control group, some of the analyzed parameters did not demonstrate a positive trend. The effectiveness of our intervention may result from the complexity of implemented pelvic floor muscle training, which aimed at developing various motor skills of this muscle group. Another strength of our intervention was the supervision of training by a specialist qualified in conducting pelvic floor muscle exercises.
An interesting outcome is that the control group, which has not received any intervention, presented a trend to decrease neuromuscular activity of pelvic floor in the 10-second contractions after the experiment. For organizational reasons, the women were informed on their allocation to the groups. Study participants may respond differently if they are aware of their intervention assignment,[33] so the lower EMG level in the control group relative to the experimental group (although not statistically significant) could reflect less motivation to perform proper pelvic floor muscle contraction. However, we did not discourage controls from performing pelvic floor exercises during the experiment, so it is possible that some of them practiced on their own and learned to perform these motor tasks with incorrect technique, for example, contracting synergistic muscles instead of pelvic floor muscles.[12]
Studies conducted by other authors confirm the effectiveness of low-impact aerobics programme, supplemented by pelvic floor muscle training[34,35] or isolated pelvic floor muscle training under the supervision of a qualified therapist in the field of urinary incontinence.[36] However, such exercise programmes do not meet the needs of all populations. It should be remembered that higher intensity of physical activity reduces the risk of non-communicable diseases such as obesity, diabetes, hypertension, ischemic heart disease, sleep disorders, and depression.[37] Bearing in mind the conclusions of numerous studies confirming beneficial changes in the lipid profile of high-impact training,[5,30] women should not be discouraged from participating in such forms of exercise. However, it is important to reduce the risk of its adverse effects.[6] The opportunity for women of all ages to participate in various forms of sports activities is of crucial importance. For some women, low-impact physical activity will not be sufficiently intensive.
A disturbing observation from our study is that young women started experiencing the symptoms of urinary incontinence already. In our study, before the intervention, 38% of the respondents suffered from symptoms associated with uncontrolled urine leakage. However, none of the respondents had any diagnosed dysfunction of the urinary system. Our research corresponded with that of other authors. Twenty-eight percent[38,39] and 23%[9] of young women observed symptoms of stress urinary incontinence in previous studies. A significant part of the respondents (14%) indicated exercise as the circumstances of uncontrolled of uncontrolled urine leakage.[39] Young women are often embarrassed by the problem of urinary incontinence and avoid medical consultations. Therefore, initial screening of high-impact exercise participants with the use of simple questionnaires, like IIQ, may play a key role in the prevention of incontinence development. It should be routinely performed by exercise professionals.
Dysfunctions related to urinary incontinence during physical activities are to a large extent related to lack of knowledge about the importance of pelvic floor muscle training. In our previous article, we analyzed the awareness of women about the pelvic floor muscles.[12] According to our research, 51% of respondents had no previous knowledge on that topic. Surprisingly, 43% of women reported that they never performed pelvic floor muscle exercises. The analyses by other authors are even more disturbing: 91% of respondents have never heard of pelvic floor muscle training.[39] The dissemination of education on the importance of pelvic floor muscle training at different levels of social life (school education, exercise professionals) would promote urinary incontinence prevention. Sport university students reported their willingness to implement pelvic floor muscle trainings in specialist courses (89%).[12]
The ability to locate and isolate the pelvic floor muscles correctly can be problematic for women who have not previously performed similar exercises. The awareness of the correct pelvic floor muscle contraction may bring improvement. In the experimental group, in the first EMG assessment, we carried out one additional sequence of exercises using the biofeedback method. The use of EMG biofeedback made it possible to visualize the muscle activation which could be reflected by the consolidation of proper motor patterns.[40] The effectiveness of EMG biofeedback in teaching sport students how to properly contract pelvic floor muscles was described in our previous publication.[12]
The main assumption of our intervention was to make young women more aware of the importance of the pelvic floor muscle training for the prevention of the pelvic floor disorders. In our previous literature review concerning the offer of pelvic floor muscle trainings for healthy women, only 14% of analyzed articles contained a proposal of preventive pelvic floor muscle trainings.[14–17] Owing to the fact that our participants were young women and might want to give birth in the near future, they should start working on improving their pelvic floor function as early as possible. Women planning motherhood must be aware that the changes occurring in pelvic floor during pregnancy might increase the risk of incontinence.[41,42]
5. Conclusions
Owing to numerous speculations about the negative influence of high-impact aerobics programme on pelvic floor muscle function, we conducted this study as a pilot trial. Therefore, the results were obtained from small groups which could result in the paucity of statistical significance. Another weakness of our research is that we used only questionnaires to assess potential pelvic floor dysfunctions. Subjective assessment of urinary incontinence in participants of future studies could be supplemented by a more reliable tool, for example, pad test. Another interesting research issue is carrying out a similar intervention in various populations, for example, including sedentary women.
Acknowledgments
The authors are grateful to the authorities of the Gdansk University of Physical Education and Sport for financial and organizational support. We acknowledge prof. Zbigniew Jastrzębski and his team for the cardiopulmonary assessments of study participants’ and prof. Aleksandra Jażdżewska for the high-impact aerobics programme implementation. We also acknowledge prof. Marcin Dornowski for the support in EMG assessments.
Author contributions
Conceptualization: Magdalena Piernicka, Anna Szumilewicz.
Data curation: Magdalena Piernicka, Anna Szumilewicz.
Formal analysis: Jakub Kortas.
Funding acquisition: Anna Szumilewicz.
Investigation: Magdalena Piernicka, Monika Błudnicka, Anna Szumilewicz.
Methodology: Anna Szumilewicz.
Project administration: Magdalena Piernicka.
Resources: Magdalena Piernicka, Anna Szumilewicz.
Software: Magdalena Piernicka, Jakub Kortas, Anna Szumilewicz.
Supervision: Magdalena Piernicka, Anna Szumilewicz.
Validation: Magdalena Piernicka, Anna Szumilewicz.
Visualization: Magdalena Piernicka, Monika Błudnicka, Jakub Kortas, Anna Szumilewicz.
Writing – original draft: Magdalena Piernicka, Monika Błudnicka, Jakub Kortas, Anna Szumilewicz.
Writing – review & editing: Magdalena Piernicka, Monika Błudnicka, Jakub Kortas, Barbara Duda-Biernacka, Anna Szumilewicz.
Footnotes
Abbreviations: BMI = body mass index, BPM = beats per minute, EMG = electromyography, HR = heart rate, IIQ = Incontinence Impact Questionnaire, IPAQ = International Physical Activity Questionnaire, M = mean, MVC = maximum voluntary contraction, SD = standard deviation.
How to cite this article: Piernicka M, Błudnicka M, Kortas J, Duda-Biernacka B, Szumilewicz A. High-impact aerobics programme supplemented by pelvic floor muscle training does not impair the function of pelvic floor muscles in active nulliparous women: A randomized control trial. Medicine. 2021;100:33(e26989).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors report no conflicts of interest.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
References
- [1].Sung V, Hampton B. Epidemiology of pelvic floor dysfunction. Obstet Gynecol Clin N Am 2009;36:421–43. [DOI] [PubMed] [Google Scholar]
- [2].Park S, Kang C, Jang S, et al. Effect of Kegel exercise to prevent urinary and fecal incontinence in an tenatal and postnatal women: systematic review. J Korean Acad Nurs 2013;43:420–30. [DOI] [PubMed] [Google Scholar]
- [3].Chmielewska D, Kwaśna K, Piecha M, et al. Selected methods of conservative treatment of stress urinary incontinence: current views. Part 1. Menopause Rev 2012;4:264–8. [Google Scholar]
- [4].Lemos A, de Souza A, Ferreira A, et al. Do perineal exercises during pregnancy prevent the development of urinary incontinence? A systematic review. Int J Urol 2008;15:875–80. [DOI] [PubMed] [Google Scholar]
- [5].Nowak R, Kostrzewa-Nowak D, Jastrzębski Z, et al. High and low impact aerobic exercise as a method of early prevention of hypercholesterolaemia development among young women. Hum Mov 2016;17:242. [Google Scholar]
- [6].Szumilewicz A, Dornowski M, Piernicka M, et al. High-low impact exercise program including pelvic floor muscle exercises improves pelvic floor muscle function in healthy pregnant women—a randomized control trial. Front Physiol 2019;9:1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Nygaard I, DeLancey J, Arnsdorf L, et al. Exercise and incontinence. Obstet Gynecol 1990;75:848–51. [PubMed] [Google Scholar]
- [8].Almeida MBA, Barra AA, Saltiel F, et al. Urinary incontinence and other pelvic floor dysfunctions in female athletes in Brazil: A cross-sectional study. Scand J Med Sci Sports 2016;26:1109–16. [DOI] [PubMed] [Google Scholar]
- [9].Alves JO, Luz STD, Brandão S, Da Luz CM, Jorge RN, Da Roza T. Urinary incontinence in physically active young women: prevalence and related factors. Int J Sports Med 2017;38:937–41. [DOI] [PubMed] [Google Scholar]
- [10].Harman EA, Frykman PN, Clagett ER, et al. Intra-abdominal and intra-thoracic pressures during lifting and jumping. /Pressions intra-abdominales et intra-thoraciques lors de souleves de poids et de sauts. Med Sci Sports Exerc 1988;20:195–201. [DOI] [PubMed] [Google Scholar]
- [11].Carvalhais A, Natal Jorge R, Bø K. Performing high-level sport is strongly associated with urinary incontinence in elite athletes: a comparative study of 372 elite female athletes and 372 controls. Br J Sports Med 2017;52:586–90. [DOI] [PubMed] [Google Scholar]
- [12].Szumilewicz A, Hopkins WG, Dornowski M, et al. Exercise professionals improve their poor skills in contracting pelvic-floor muscles: a randomized controlled trial. Res Q Exerc Sport 2019;90:641–50. [DOI] [PubMed] [Google Scholar]
- [13].Bø K, Nygaard IE. Is physical activity good or bad for the female pelvic floor? A narrative review. Sports Med 2020;50:471–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Chmielewska D, Stania M, Smykla A, et al. Bioelectrical activity of the pelvic floor muscles after 6-week biofeedback training in nulliparous continent women. Acta Bioeng Biomech 2016;18:105–13. [PubMed] [Google Scholar]
- [15].Pereira-Baldon VS, Avila MA, Dalarmi CB, et al. Effects of different regimens for pelvic floor muscle training in young continent women: randomized controlled clinical trial. J Electromyogr Kinesiol 2018;44:31–5. [DOI] [PubMed] [Google Scholar]
- [16].Pereira VS, de Melo MV, Correia GN, et al. Long-term effects of pelvic floor muscle training with vaginal cone in post-menopausal women with urinary incontinence: a randomized controlled trial. Neurourol Urodyn 2019;32:48–52. [DOI] [PubMed] [Google Scholar]
- [17].Huebner M, Riegel K, Hinninghofen H, et al. Pelvic floor muscle training for stress urinary incontinence: a randomized, controlled trial comparing different conservative therapies. Physiother Res Int 2011;16:133–40. [DOI] [PubMed] [Google Scholar]
- [18].Liu Y-J, Wu W-Y, Hsiao S-M, et al. Efficacy of pelvic floor training with surface electromyography feedback for female stress urinary incontinence. Int J Nurs Pract 2018;24:12696–8. [DOI] [PubMed] [Google Scholar]
- [19].Shin DC, Shin SH, Lee MM, et al. Pelvic floor muscle training for urinary incontinence in female stroke patients: a randomized, controlled and blinded trial. Clin Rehabil 2016;30:259–67. [DOI] [PubMed] [Google Scholar]
- [20].Luginbuehl H, Lehmann C, Baeyens J-P, et al. Involuntary reflexive pelvic floor muscle training in addition to standard training versus standard training alone for women with stress urinary incontinence: study protocol for a randomized controlled trial. Trials 2015;16:524–1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Batista RLA, Franco MM, Naldoni LMV, et al. Biofeedback and the electromyographic activity of pelvic floor muscles in pregnant women. Rev Bras Fisioter 2011;15:386–92. [DOI] [PubMed] [Google Scholar]
- [22].Bhat C, Khan M, Ballala K, et al. Reduced pelvic floor muscle tone predisposes to persistence of lower urinary tract symptoms after puerperium. Scientifica 2016;01–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Bertotto A, Schvartzman R, Uchôa S, et al. Effect of electromyographic biofeedback as an add-on to pelvic floor muscle exercises on neuromuscular outcomes and quality of life in postmenopausal women with stress urinary incontinence: a randomized controlled trial. Neurourol Urodyn 2017;36:2142–7. [DOI] [PubMed] [Google Scholar]
- [24].Alves FK, Riccetto C, Adami DBV, et al. A pelvic floor muscle training program in postmenopausal women: a randomized controlled trial. Maturitas 2015;81:300–5. [DOI] [PubMed] [Google Scholar]
- [25].Halski T, Słupska L, Dymarek R, et al. Evaluation of bioelectrical activity of pelvic floor muscles and synergistic muscles depending on orientation of pelvis in menopausal women with symptoms of stress urinary incontinence: a preliminary observational study. BioMed Res Int 2014;274938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Glazer HI, Marinoff SC, Sleight IJ. Web-enabled Glazer surface electromyographic protocol for the remote, real-time assessment and rehabilitation of pelvic floor dysfunction in vulvar vestibulitis syndrome. A case report. J Reprod Med 2002;47:728–30. [PubMed] [Google Scholar]
- [27].Uebersax J, Wyman J, Shumaker S, et al. Short forms to assess life quality and symptom distress for urinary incontinence in women: the incontinence impact questionnaire and the urogenital distress inventory. continence program for women research group. Neurourol Urodyn 1995;14:131–9. [DOI] [PubMed] [Google Scholar]
- [28].Corcos J, Behlouli H, Beaulieu S. Identifying cut-off scores with neural networks for interpretation of the incontinence impact questionnaire. Neurourol Urodyn 2002;21:198–203. [DOI] [PubMed] [Google Scholar]
- [29].Booth M. Assessment of physical activity: an international perspective. Res Q Exerc Sport 2000;71:114–20. [DOI] [PubMed] [Google Scholar]
- [30].Kostrzewa-Nowak D, Nowak R, Jastrzębski Z, et al. Effect of 12-week-long aerobic training programme on body composition, aerobic capacity, complete blood count and blood lipid profile among young women. Biochem Med 2015;25:103–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Piernicka M, Duda-Biernacka B, Bludnicka M, Szumilewicz A. The characteristics of the pelvic floor muscle training programs used in experimental studies with surface electromyography in non-pregnant women: a systematic review. Iran J Public Health 2020;49:1022–32. [Google Scholar]
- [32].University of Michigan, Miller M. On Pelvic Floor Muscle Function and Stress Urinary Inocntinence: Effects of Posture, Parity and Volitional Control, Dissertation. 2013;145–157. [Google Scholar]
- [33].Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Dtsch Med Wochenschr 2011;136:E26–126. [Google Scholar]
- [34].Stafne SN, Salvesen K, Romundstad PR, et al. Does regular exercise including pelvic floor muscle training prevent urinary and anal incontinence during pregnancy? A randomised controlled trial. Int J Gynaecol Obstet 2012;119:1270–80. [DOI] [PubMed] [Google Scholar]
- [35].Pelaez M, Gonzalez-Cerron S, Montejo R, et al. Pelvic floor muscle training included in a pregnancy exercise program is effective in primary prevention of urinary incontinence: a randomized controlled trial. Neurourol Urodyn 2014;33:67–71. [DOI] [PubMed] [Google Scholar]
- [36].Sangsawang B, Sangsawang N. Is a 6-week supervised pelvic floor muscle exercise program effective in preventing stress urinary incontinence in late pregnancy in primigravid women?: a randomized controlled trial. Eur J Obstet Gynecol Reprod Biol 2016;197:103–10. [DOI] [PubMed] [Google Scholar]
- [37].Bouchard C, Shepbard R, Stephens T. Physical activity, fitness, and henlth: intematioval proceedings and consensus statement champaign. Human Kinetics Inc 1994;167–76. [Google Scholar]
- [38].Nygaard IE, Thompson FL, Svengalis SL, et al. Urinary incontinence in elite nulliparous athletes. Obstet Gynecol 1994;84:183–7. [PubMed] [Google Scholar]
- [39].Carls C. The prevalence of stress urinary incontinence in high school and college-age female athletes in the Midwest: implications for education and prevention. Urol Nurs 2007;27:21–4. [PubMed] [Google Scholar]
- [40].Arnouk A, De E, Rehfuss A, et al. Physical, complementary, and alternative medicine in the treatment of pelvic floor disorders. Curr Urol Rep 2017;18:47–8. [DOI] [PubMed] [Google Scholar]
- [41].Ghetti C. Pelvic floor changes in first pregnancy: how do they affect quality of life? OB/GYN Clinical Alert 2017;34:03–4. [Google Scholar]
- [42].Boyles S, Li H, Mori T, et al. Effect of mode of delivery on the incidence of urinary incontinence in primiparous women. Obstet Gynecol 2009;113:134–41. [DOI] [PubMed] [Google Scholar]