Abstract
With the declining use of the pulmonary artery catheter (PAC), transesophageal echocardiography (TEE) has become an appealing alternative to obtain pulmonary artery pressure non-invasively using the simplified Bernoulli equation. The validation of this method in the perioperative setting has been scarce with no clear recommendations about which view is the most accurate to estimate right ventricular systolic pressure (RVSP).
Therefore, we performed a prospective, observer-blinded, diagnostic test accuracy study to assess the difference in systolic pulmonary artery pressure (sysPAP) measuring both, invasively sysPAP and estimated RVSP with TEE in 3 different views: the mid-esophageal (ME) 4Chamber, the ME right ventricular (RV) inflow-outflow and the ME modified bicaval view.
To show a clinically significant difference of at least 10% in RVSP, we included 40 cardiac surgical patients divided into 3 subgroups: Patients with mild to moderate tricuspid regurgitation (TR) and mean PAP <25 mm Hg, patients with mild to moderate TR and mean PAP≥ 25 mm Hg, and patients with severe TR.
For the whole cohort, bias of estimated RVSP compared to measured sysPAP was 5.27 mm Hg, precision was 7.96 mm Hg, limits of agreement were −10.66 to 21.19 mm Hg. The best agreement between the 2 methods was found in patients with severe TR and in the ME RV inflow-outflow and the modified bicaval view. Good Doppler signals were available in 35% and 46% in these views, and in 20% in the ME 4 chamber view.
The estimation of the sysPAP by TEE cannot be considered reliable in the clinical perioperative setting. Only measurements that provide a full Doppler envelope show sufficient precision to provide accurate estimations.
Keywords: pulmonary artery catheter, right ventricular systolic pressure, transesophageal echocardiography
1. Introduction
Pulmonary artery pressure is the key parameter to diagnose and monitor pulmonary hypertension in cardiac surgical patients.[1] However, the use of the pulmonary artery catheter (PAC), which has been declared the gold standard to measure pulmonary artery pressure, has declined over the last decade.[2–4] Because of its association with increased morbidity and mortality the insertion rates dropped below 10% in some institutions.[2–5] However, echocardiography can be used to obtain pulmonary artery pressure non-invasively. The American Society of Echocardiography has published guidelines for the echocardiographic assessment of the right heart. The systolic pulmonary artery pressure (sysPAP) can be achieved by using the simplified Bernoulli equation. Therefore, the tricuspid regurgitant jet velocity is used to obtain a right ventricular to right atrial pressure gradient. Right ventricular systolic pressure (RVSP) can be estimated by adding this pressure gradient to the right atrial pressure. Right ventricular systolic pressure equals sysPAP if pulmonary stenosis or right ventricular outflow obstruction do not apply.[1,6,7] Early literature reports a close correlation between Doppler-derived RVSP and measurements obtained from direct heart catheterization in spontaneously breathing patients,[8,9] but subsequent studies produced conflicting results.[10–13] The majority of these trials compared Doppler-derived RVSP using transthoracic echocardiography (TTE) and the right heart catheterization was performed in outpatients with non-simultaneous measurements, sometimes days or weeks apart.[13] So far, there are only 2 studies comparing RVSP obtained from transesophageal echocardiography (TEE). They also performed simultaneously right heart catheterization measurements under general anesthesia. However, these 2 studies produced conflicting results and used different methodological approaches.[14,15] Cowie et al measured the correlation between RVSP and sysPAP, while Soliman et al evaluated the accuracy of RVSP to predict sysPAP within 10 mm Hg.[10,14,15]
Also, there are no clear recommendations which TEE view is the most accurate to estimate RVSP.
Therefore, this study wanted to assess the difference in systolic pulmonary artery pressure measured invasively with a pulmonary artery catheter and the calculated right ventricular systolic pressure using transesophageal echocardiography in 3 different views: the mid-esophageal (ME) 4 Chamber view, the ME right ventricular (RV) inflow-outflow view and the ME modified bicaval view.
The primary outcome of the study was to determine the bias and precision of estimated RVSP with TEE compared to measured sysPAP with PAC.
As secondary outcomes the differences in bias and precision of estimated RVSP and measured sysPAP between 3 subgroups of patients with different mean pulmonary artery pressure thresholds were investigated. Furthermore, differences of RVSP estimations and TR signal quality in the 3 TEE views were determined.
2. Methods
2.1. Trial design and participants
This prospective, single-center, observer-blinded, diagnostic test accuracy study was performed in accordance with the Declaration of Helsinki and approved by the Ethical Committee of the Medical University Vienna, Austria (registration number: 1113/2017). The study was registered at clinicaltrials.gov, registration number: NCT03117673, Registrar: Ulrike Weber. Written informed consent was obtained from all subjects.
Patients older than 18 years, undergoing elective cardiac surgery under general anesthesia with clinically indicated TEE and PAC were included. Exclusion criteria were right ventricular outflow obstruction and any contraindications for TEE like esophageal disease with known stricture, diverticuli, varices or tumor, prior esophageal or stomach surgery or perforated viscus.
2.2. Baseline assessment
All patients received routinely monitoring with an arterial line and a central venous catheter and PAC. The anesthetic technique was general anesthesia with endotracheal intubation. TEE studies were performed in supine position after induction of a propofol and fentanyl based anesthesia, which was maintained with sevoflurane. Standard vital parameters were recorded continuously. The pressure transducers were located in the mid-thoracic position, halfway between the sternum and operating table, as recommended by recent guidelines.[16]
TEE was performed with a Vivid E9 Ultrasound system (GE Vingmed; Horten, Norway) using a cT6 (3.0–8.0 MHz, GE) probe. A standard greyscale 2D image was acquired in every view. Penetration, resolution and gain were optimized for each patient, and the frame rate was 80 frames per second. Imaging frequency ranged between 5 and 7 Megahertz. In patients with atrial fibrillation, the mean of 5 consecutive measurements was used for calculations.
2.3. Interventions and outcomes
All TEE studies and analyses were performed by experienced operators, who were certified by the National Board of Echocardiography. The RVSP was calculated using the modified Bernoulli equation (RVSP = 4 × v2 + RAP), where v is the maximum velocity of the tricuspid valve regurgitation jet measured using continuous wave (CW) Doppler and RAP is the right atrial pressure measured via the central venous line. Windows used to measure the maximal tricuspid regurgitation (TR) velocity were the mid-esophageal (ME) 4 chamber view, the ME right ventricular (RV) inflow-outflow view and the ME modified bicaval view. TR signal quality was classified in every window according to envelope visibility as good (=3, complete envelope), moderate (=2, partial envelope but prone to extrapolation) or poor (=1, unreliable envelope) or no signal (=0).[17] TR severity is assessed as absent, mild, moderate or severe according to the American Society of Echocardiography guidelines.[1,18] Severe TR was defined by the presence of a vena contracta ≥7 mm, reversed systolic hepatic vein flow, proximal iso-velocity surface area (PISA) radius >9 mm, and a very large central jet or eccentric wall impinging jet. Mild TR was defined by a visual small jet, proximal iso-velocity surface area radius <5 mm, and systolic predominance of the hepatic vein flow. Moderate TR was defined as TR not corresponding to the definition of either mild or severe TR.[1,17,18] A predefined value of mean PAP ≥25 mm Hg was considered elevated in agreement with the current guidelines.[19,20] The following routinely acquired right and left ventricular function metrics were also assessed: tricuspid annular plane systolic excursion (TAPSE: <17 mm abnormal) and left ventricular systolic eccentric index (E:I>1.2 defining an abnormal ratio, measured in the transgastric mid-papillary short axis view).[17,21–23]
2.4. Randomization
Patients were divided into 3 groups according to measurement from pulmonary artery catheter:
Patients with mild to moderate TR and normal mean PAP (<25 mm Hg),[19,20] patients with mild to moderate TR and elevated mean PAP (≥25 mm Hg),[19,20] and patients with severe TR; [1,17]
During the whole TEE examination the examiners were blinded to the pulmonary artery pressures measured by PAC. This was done by a patch that covered just the pulmonary artery measurement on the monitor during the TEE examination. After the examination the patch was removed. A study nurse wrote down all hemodynamic measurements which included: systolic, diastolic and mean pulmonary artery pressure, pulmonary artery wedge pressure (PCWP), cardiac output, heart rate, systolic, diastolic and mean arterial blood pressure. Study measurements were performed after induction of anesthesia (before start of surgery, before opening of the sternum and pericardium) and after surgery during skin closure (after closure of sternum and pericardium) in the operation room to allow hemodynamic stable and comparable conditions. All TEE measurements were stored electronically for offline analysis.
2.5. Statistics
The primary outcome of the study was the bias and precision of calculated RVSP with TEE compared to measured sysPAP with PAC. The current literature [8,24–27] provided no information on possible differences in bias and precision of the measurement between patients with normal, and elevated mean PAP, and those with severe TR, so our sample size considerations are based on the whole cohort. Based on currently published RVSP-distributions to show a clinically significant difference of more than 10% [13,14] with a power of 80%, 33 patients in total had to be included. This estimation was based on a one-tailed comparison and a probability of error of first kind of 0.05, and was calculated using G∗Power 3.1.9.2. To allow for dropouts and uncertainty in this calculation, at least 39 patients in total were calculated for inclusion.
All data were tabulated case-wise and pair-wise (i.e., PAC and TEE measurements) Quantitative data are expressed as mean +/- SD if normally distributed or as medians and interquartile ranges (IQRs) if not normally distributed. Qualitative variables are presented as absolute and relative frequencies. Measurements from the best obtainable of the 3 TEE views were used for analysis. According to the method described by Bland and Altman [28] we assessed agreement between measurements: The mean difference (bias, d) as a metric for the systematic measurement error, the SD of the differences (precision, s), and the limits of agreement (d ± 2 s) as metrics for scatter were calculated. Bland-Altman plots were used for graphical representation.
For primary analysis, the whole cohort was used. For secondary analysis, patients with mean PAP <25 mm Hg and mean PAP ≥25 mm Hg, and those with severe TR were analyzed separately. Differences between TR signal quality and of RVSP calculations between the 3 TEE views were analyzed accordingly.
Inter-rater agreement for the maximum velocity of the tricuspid valve regurgitation jet were assessed in all patients independently and offline by an additional echocardiographer. Intra-class correlation coefficient was calculated for each individual view. Inter-observer agreement was calculated by using interclass correlation coefficients (ICCs) and a 95% confidence interval (95% CI).
Statistical analysis was performed using Stata 12 for Windows (Stata Corp, College Station, TX).
3. Results
Forty cardiac surgical patients were included in this study, who received either valve or coronary artery bypass graft (CABG) procedures or a combination of both. Table 1 presents their baseline characteristics and hemodynamic parameters. Adequate image quality was available in 40 patients before surgery and in 25 patients after surgery. Reasons for inadequate image quality were artefacts from newly inserted mechanical valves during surgery. In these 65 echocardiographic examinations a total of 195 measurements of the right ventricular systolic pressure were performed. Inadequate Doppler signals due to lack of regurgitation jet were detected in 4 out of 195 measurements only for the modified bicaval view.
Table 1.
Baseline characteristics and hemodynamic measurements.
| Factor | All patients n = 40 | Mild to moderate TR and mean PAP <25 mm Hg N = 14 | Mild to moderate TR and mean PAP ≥25 mm Hg N = 17 | Severe TR N = 9 |
| Age (yrs) | 67.2 ± 10.7 (35–83) | 69.6 ± 10.4 (49–83) | 62.1 ± 10.9 (35–77) | 73 ± 6.1 (64–81) |
| Gender m/f | 24/16 | 8/6 | 12/5 | 4/5 |
| Height (cm) | 170.8 ± 9.4 (152–185) | 169.7 ± 10.7 (152–185) | 171.6 ± 9.4 (157–182) | 171.1 ± 7.9 (160–185) |
| Weight (kg) | 78.9 ± 11.9 (53–98) | 77.3 ± 13.6 (53–97) | 78.8 ± 11.7 (63–98) | 81.6 ± 10.4 (65–95) |
| BSA∗ (kg/m2) | 1.9 ± 0.2 (1.5–2.2) | 1.9 ± 0.2 (1.5–2.1) | 1.9 ± 0.2 (1.6–2.2) | 1.9 ± 0.2 (1.7–2.1) |
| ASA† score | 3 ± 0 (3–3) | 3 ± 0 (3–3) | 3 ± 0 (3–3) | 3 ± 0 (3–3) |
| Hemodynamic measurements | ||||
| sysPAP‡ (mm Hg) | 38.2 ± 10.9 (21–68) | 29.3 ± 5.5 (21–42) | 40.4 ± 6.5 (32–58) | 44.8 ± 12.9 (28–68) |
| CVP§ (mm Hg) | 12.7 ± 3.5 (7–27) | 10.4 ± 2.4 (7–15) | 13.6 ± 1.9 (10–16) | 13 ± 2.7 (9–18) |
| PCWP|| (mm Hg) | 15.6 ± 6.8 (2–33) | 10.9 ± 5.4 (2–20) | 16.4 ± 5.1 (7–23) | 21.2 ± 7.3 (12–33) |
| MAP¶ (mm Hg) | 74 ± 13.1 (51–104) | 71.4 ± 10.6 (51–83) | 74.1 ± 14.3 (58–104) | 76.1 ± 14.7 (57–97) |
| Surgical procedure | ||||
| Valve procedure | 29 | 9 | 12 | 8 |
| CABG# | 3 | 1 | 2 | 0 |
| CABG + valve | 8 | 4 | 3 | 1 |
Mean ± standard deviation (minimum – maximum).
BSA = body surface area.
ASA = American Society of Anaesthesiologists.
Systolic pulmonary artery pressure.
Central venous pressure.
Pulmonary capillary wedge pressure.
Mean arterial pressure.
CABG = coronary artery bypass graft.
For the whole cohort, the bias (mean difference) of RVSP calculated from TEE measurements as compared to sysPAP measured by the PAC was 5.27 mm Hg, the precision (standard deviation of the differences) was 7.96mmHg, and limits of agreement were −10.66 to 21.19 mm Hg.
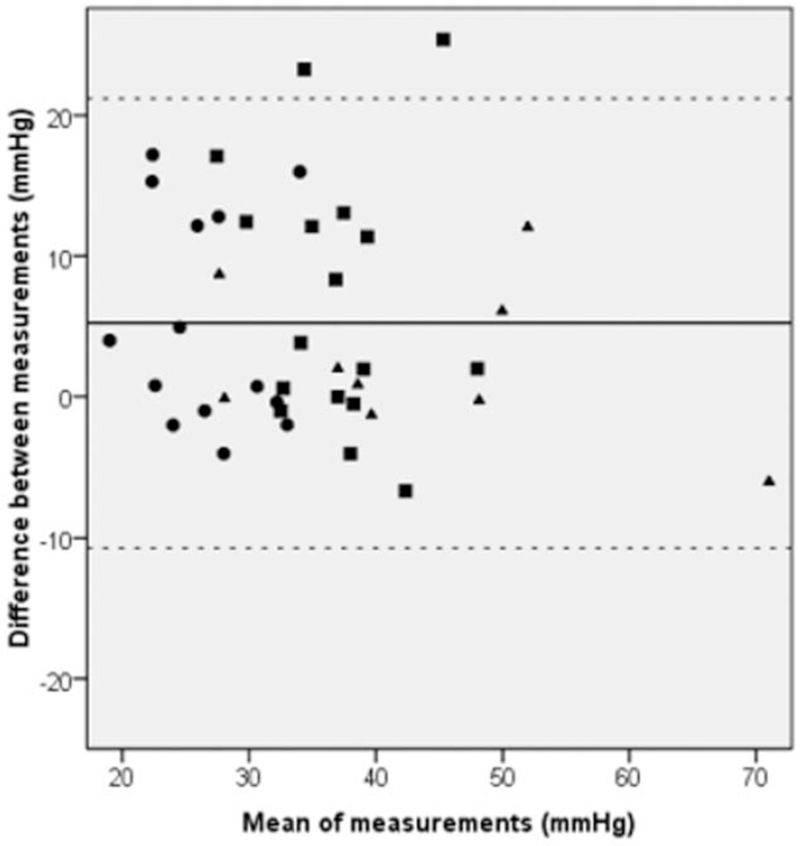
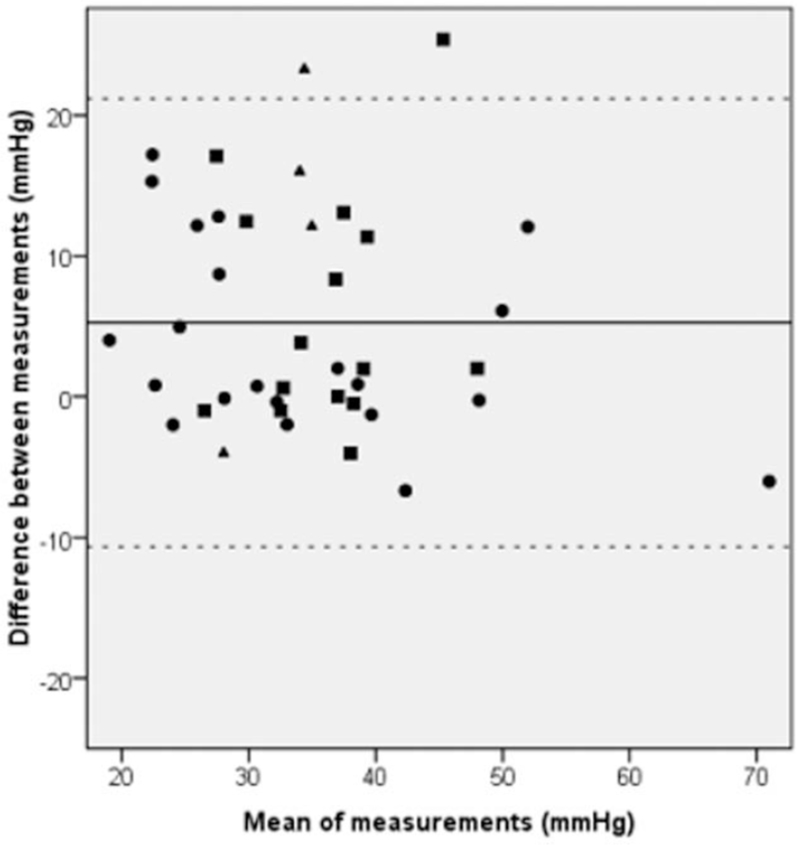
Results revealed relevant differences between groups with mild to moderate TR and mean PAP <25 mm Hg or mean PAP ≥25 mm Hg, and those with severe TR. Measurement in patients with mild to moderate TR and mean PAP <25 mm Hg showed a bias of 4.97 mm Hg, a precision of 7.41 mm Hg, limits of agreement of −9.84 to 19.78 mm Hg, in those with mean PAP ≥25 mm Hg a bias of 6.63mmHg, a precision of 9.07 mm Hg, limits of agreement −11.50 to 24.76 mm Hg, whereas in those with severe TR, a bias of 2.20 mm Hg, a precision of 5.24 mm Hg, limits of agreement of −8.28 to 12.68 mm Hg were found. See Figure 1 for a Bland-Altman plot of results by groups of patients and Figure 2 for a Bland-Altman plot of results by source of best measurement.
Figure 1.
Bland-Altman plot of agreement between right ventricular systolic pressure (RVSP) and systolic pulmonary artery pressure (sysPAP) for the 3 subgroups. Each symbol represents 1 measurement. Dots represent patients with mild to moderate tricuspid regurgitation (TR) and mean pulmonary artery pressure (meanPAP) <25 mm Hg, squares represent patients with mild to moderate TR and meanPAP ≥25 mm Hg, triangles represent patients with severe TR. Solid line marks bias, dotted lines mark limits of agreement.
Figure 2.
Bland-Altman plot of agreement between right ventricular systolic pressure (RVSP) and systolic pulmonary artery pressure (sysPAP) for the 3 different mid-oesophageal standard views. Results by source of best measurement: Each symbol represents 1 patient. Dots represent patients where source of best measurement was the ME RV inflow-outflow view, squares represent the ME 4 chamber view, and triangles represent the ME modified bicaval view. Solid line marks bias, dotted lines mark limits of agreement.
Accuracy improved when only patients with good Doppler signals were included:
In those patients, bias, precision, and limits of agreement were 2.12 mm Hg, 6.62 mm Hg, −11.12 to 15.35 mm Hg for the whole cohort; 1.14 mm Hg, 4.65 mm Hg, −8.16 to 10.44 mm Hg for those with mean PAP <25 mm Hg; 5.14 mm Hg, 8.89 mm Hg, −12.64 to 22.91 mm Hg for those with mean PAP ≥25 mm Hg; −0.69 mm Hg, 2.54 mm Hg, −5.77 mm Hg to 4.38 mm Hg for those with severe TR.
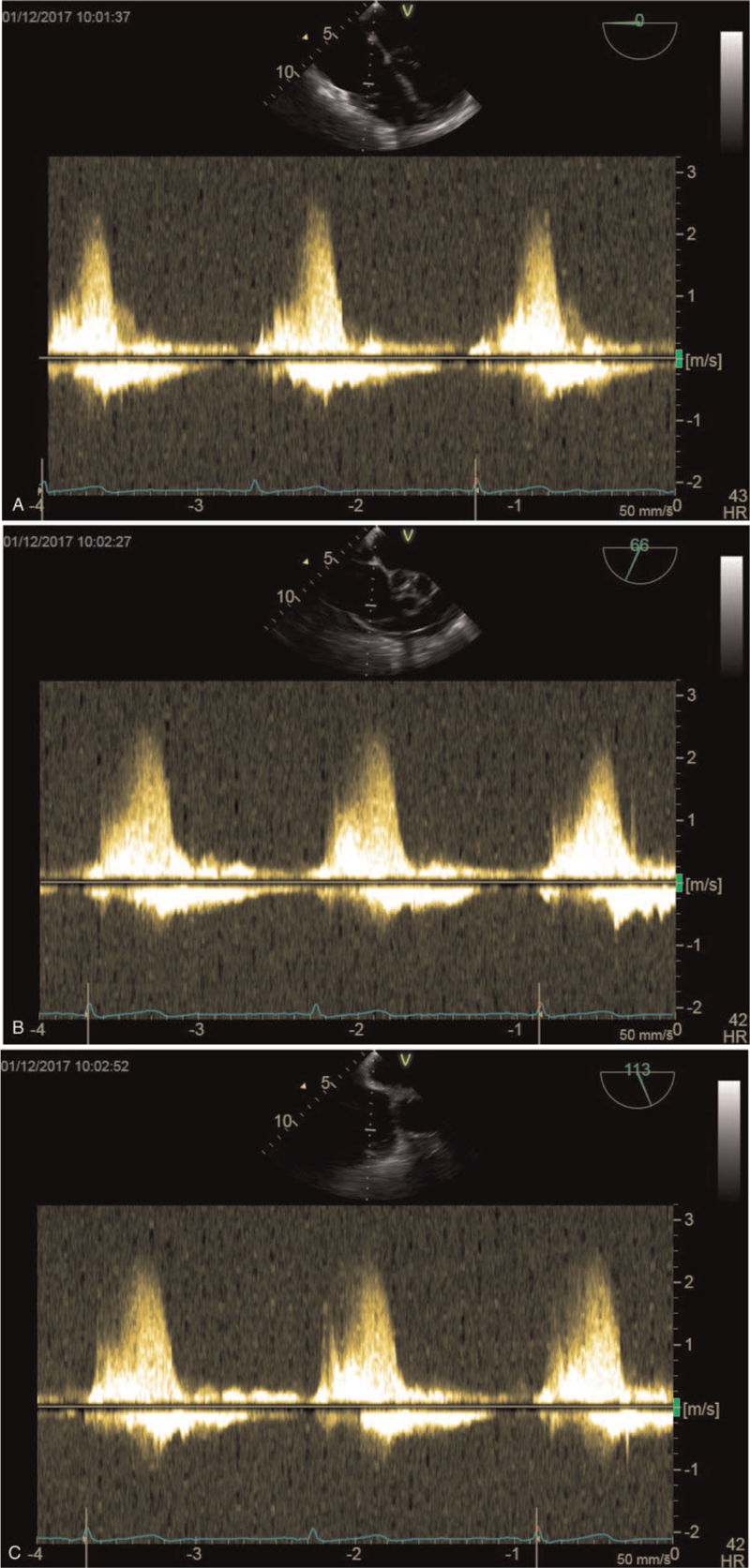
Table 2 presents the signal quality of the tricuspid regurgitation jet in the 3 different TEE views. Figure 3a-c further represents examples of the tricuspid regurgitation jet in all 3 TEE views.
Table 2.
Presents the median tricuspid regurgitation signal quality and the frequency in absolute numbers and proportion (%) of good Doppler signals (3, complete envelope visible) in the 3 different transesophageal echocardiographic views.
| Four chamber view | Right ventricular inflow-outflow view | Modified bicaval view | |
| Mild to moderate TR and mean PAP <25 mm Hg n = 25 | 1 7/25 (28%) | 2 11/25 (44%) | 2.5 12/25 (48%) |
| Mild to moderate TR and mean PAP ≥25 mm Hg n = 29 | 1 4/29 (14%) | 2 6/29 (21%) | 2 12/29 (41%) |
| Severe TR n = 11 | 2 3/11 (27%) | 3 7/11 (64%) | 2.5 6/11 (55%) |
| All n = 65 | 1 13/65 (20%) | 2 23/65 (35%) | 2 30/65 (46%) |
Figure 3.
A–C: Examples of the tricuspid regurgitation jet in the 3 TEE views: the ME 4 chamber view (A), the ME RV inflow-outflow view (B), and the ME modified bicaval view (C).
A sensitivity analysis of excluding all patients with atrial fibrillation resulted no relevant changes: bias 6.01 mm Hg, precision 8.08mmHg, limits of agreement −10.15 to 22.18 mm Hg.
Regarding inter-rater reliability, intra-class correlation (ICC) coefficient was 0.989 (95% confidence interval 0.979–0.994) for the ME 4 chamber view, 0.991 (0.983–0.995) for the ME RV inflow-outflow view, and 0.979 (0.959–0.989) for the ME modified bicaval view, and 0.984 (0.971–0.992) for individual best obtainable view in each patient.
No adverse events or hemodynamic instability in any patient were observed.
4. Discussion
Our results indicate that general agreement between systolic pulmonary artery pressure measured by pulmonary artery catheter and transesophageal Doppler echocardiography is rather poor.
The best agreement for the RVSP measured by TEE and the reference standard was found in the subgroup of patients with severe TR. When comparing 3 different mid-esophageal TEE views, the ME RV inflow-outflow and the modified bicaval view showed the best agreement.
TR signal quality was also rated better in the RV inflow-outflow view and in the modified bicaval view compared to the 4 chamber view. However, good Doppler signals with a full TR envelope (signal quality = 3) were only available in 35% and 46% of all measurements in these views, and in 20% in the ME 4 chamber view.
Soliman et al observed in a similar study setting with 33 cardiac surgery patients adequate Doppler signals with a full envelope in 56% of their patients. Adequate signals were most often found in the right ventricular inflow-outflow view and the modified bicaval view, as in our study.[14] Overall, they also reported a poor agreement between TEE and PAC measurements of sysPAP with accurate Doppler-derived measurements in only 55% to 75% of the time.[14] However, they did not distinguish between patients with different mean pulmonary artery pressure thresholds or TR severity.
The fact that the mobility of the echocardiographic probe is limited can complicate obtaining an optimal alignment between the tricuspid regurgitant jet and the Doppler interrogation beam. In our study this became obvious in the ME 4 chamber view, where a near-parallel alignment of the ultrasound beam was more difficult because it resulted in inferior signal quality compared to the other views. Varying chamber dimensions such as left ventricular hypertrophy, but also large volume shift can account for these difficulties.[1,10]
Obviously, signal quality seems to be crucial. The best agreement of RVSP measurements by TEE and sysPAP measurements with the PAC was observed in the subgroup analysis of those measurements with good signal quality (=3) and a full tricuspid regurgitant jet envelope. This subgroup analysis revealed a smaller bias with more narrow limits of agreement than in the overall cohort. Further, the ME RV inflow-outflow and ME modified bicaval view demonstrated better signal quality and also better agreement between the 2 measurement methods compared to the ME 4 chamber view. Also, the subgroup with severe TR also showed better signal quality than the other 2 groups and the best agreement between the TEE and PAC measurements.
Because the modified Bernoulli equation only requires the insertion of the maximal velocity of the tricuspid regurgitant jet, it is also possible to calculate RVSP with moderate (=2, partial envelope but prone to extrapolation) or poor (=1, unreliable envelope) signal quality. Considering our study results and the ones by Soliman et al, the echocardiographer should aim for the best possible signal quality.
However, our results are in contrast to those of Cowie et al They compared 100 measurements of RVSP with TEE with sysPAP from a PAC and demonstrated a strong correlation (r = 0.98) with minimal bias and narrow limits of agreement (−5 to +5 mm Hg) across a broad range of pulmonary pressures. They used a different methodical approach and whether evaluated signal quality or divided the patients into subgroups or defined which and how many views they used for the measurements. Although they stated that they were able to measure RVSP with TEE in all patients.[15]
The strengths of this study include that blinded TEE estimations of RVSP were performed, simultaneously to PAC measurements of sysPAP under general anesthesia. In contrast to the majority of TTE studies, that compared measurements that were taken at different time points hours or days apart.[10,13]
The calculation of RVSP also depends upon an accurate estimate of right atrial pressure. Echocardiographic estimations of right atrial pressure are often inaccurate and may account for the majority of error in RVSP estimation in TTE studies.[10,11,13] Our study used direct central venous measurements as real-time estimate of right atrial pressure. Both the right atrial pressure and pulmonary artery pressure transducers were at the same level and therefore our measurements were independent of transducer position. Accurate and simultaneous measurement of the central venous pressure in the modified Bernoulli equation for estimation of RVSP is crucial to reliable calculation of this parameter.[15] Further, our study accounted for stable hemodynamic conditions with as less direct surgical manipulation as possible, as all measurements were taken under general anesthesia before sternotomy and pericardiotomy and after surgery during skin closure after closure of sternum and pericardium. Nevertheless, our results showed a relatively high bias with wide limits of agreement in our measurements. SysPAP is dependent on cardiac output, heart rate, volume status and pulmonary vascular resistance, a variation of these parameters can happen on a beat-to-beat basis especially under general anesthesia in the operating theatre, because there they are further influenced by volume shifts, surgical manipulation, mechanical ventilation and anesthetic drugs.[14,15,29] Therefore, they could easily account for the reported discrepancy between the 2 measurement methods.
In this trial TEE measurements were performed in all 3 mid-esophageal standard views in every patient and an independent offline analysis was done by an additional echocardiographer to evaluate inter-rater reliability. The intra-class correlation coefficient showed that the TEE measurements are reproducible, with the best values in the ME RV inflow-outflow view, although general agreement between TEE and PAC measurements remained weak. Soliman et al received similar results for intra-class correlation coefficients for peak tricuspid regurgitation velocity, but did not evaluate them for every single TEE view.[14]
This study was also planned according to sound diagnostic test accuracy-methodology, and performed a priori sample-size calculations to avoid type II error of declaring to difference between methods of measurement due to too small sample size.
Further, our study was the first one that performed a subgroup analysis between 3 subgroups of patients with different mean pulmonary artery pressure thresholds and TR severity.
This subgroup analysis demonstrated that severe TR had the best precision regardless of the degree pulmonary artery pressure.
4.1. Limitations
With a pulmonary artery catheter in situ, the incidence of tricuspid regurgitation can be elevated. Studies report an increase of tricuspid regurgitation by 48%, and also TR severity, which may account for our ability to find at least some tricuspid regurgitation in all patients.[15,29]
Only 3 standard mid-esophageal views were evaluated in this study, but no additional transgastric or deep-transgastric views. A recent study showed that these standard views allowed to acquire tricuspid transvalvular blood flow in an orthograde fashion in 51% of their patients, and that the additional transgastric and deep-transgastric views provided no further improvement.[30]
Our study indicates that estimation of sysPAP by transesophageal Doppler echocardiography cannot be considered reliable in the overall clinical perioperative setting in ventilated patients under general anesthesia. Therefore, only TEE measurements that provide a good signal quality with a full Doppler envelope show sufficient precision to provide accurate readings. Our study demonstrated that a good signal quality was only achieved in less than half of our TEE measurement. Transesophageal views with the best signal quality were the ME RV inflow-outflow and modified bicaval view and should therefore used as first line views for estimation of the sysPAP. The results of this study conclude that TEE measurements cannot be used as a diagnostic tool for treatment decisions or used superior to PAC measurements, but may be an important screening tool for pulmonary hypertension intra-operatively. Taking into account that the use of the PAC is vanishing as a standard monitoring during cardiac surgery, we recommend that this information should be combined with further echocardiographic parameters such as right ventricular hypertrophy and dysfunction, valvular disease, left ventricular diastolic failure and the patient's history.[10]
Acknowledgments
We would like to thank all the medical staff at the Division of Cardiothoracic and Vascular Anesthesia and Intensive Care Medicine for their collaboration and assistance.
Author contributions
Conceptualization: Bruno Mora, Dominik Roth, Martin Bernardi, Eva Base, Ulrike Weber.
Data curation: Bruno Mora, Dominik Roth, Martin Bernardi, Ulrike Weber.
Formal analysis: Dominik Roth.
Investigation: Bruno Mora, Dominik Roth, Martin Bernardi, Ulrike Weber.
Methodology: Dominik Roth, Eva Base, Ulrike Weber.
Project administration: Ulrike Weber.
Resources: Ulrike Weber.
Supervision: Eva Base, Ulrike Weber.
Validation: Ulrike Weber.
Writing – original draft: Ulrike Weber.
Writing – review & editing: Bruno Mora, Dominik Roth, Martin Bernardi, Eva Base.
Footnotes
Abbreviations: ME = mid-esophageal, PAC = pulmonary artery catheter, RV = right ventricular, RVSP = right ventricular systolic pressure, sysPAP = systolic pulmonary artery pressure, TEE = transesophageal echocardiography, TR = tricuspid regurgitation.
How to cite this article: Mora B, Roth D, Bernardi MH, Base E, Weber U. Estimation of pulmonary artery pressure with transesophageal echocardiography: an observer-blinded test accuracy study. Medicine. 2021;100:33(e26988).
The authors have no funding and conflicts of interests to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Rudski LG, Lai WW, Afilalo J, Hua L, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography Endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. JASE 2010;23:685–713. [DOI] [PubMed] [Google Scholar]
- [2].Minai OA, Yared JP, Kaw R, Subramaniam K, Hill NS. Perioperative risk and management in patients with pulmonary hypertension. Chest 2013;144:329–40. [DOI] [PubMed] [Google Scholar]
- [3].Cowie BS. Does the pulmonary artery catheter still have a role in the perioperative period? Anaesth Int Care 2011;39:345–55. [DOI] [PubMed] [Google Scholar]
- [4].Chatterjee K. The Swan Ganz catheter: past, present and future. A viewpoint. Circulation 2009;119:147–52. [DOI] [PubMed] [Google Scholar]
- [5].Hoeper MM, Lee SH, Voswinckel R, et al. Complications of right heart procedures in patients with pulmonary hypertension in experienced centers. JACC 2006;48:2546–52. [DOI] [PubMed] [Google Scholar]
- [6].Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a comprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. Anesth Analg 2014;118:21–68. [DOI] [PubMed] [Google Scholar]
- [7].Flachskampf FA, Wouters PF, Edvardsen T, et al. Recommendations for transesophageal echocardiography: EACVI update 2014. Eur Heart J Cardiovasc Imaging 2014;15:353–65. [DOI] [PubMed] [Google Scholar]
- [8].Yock PG, Popp RL. Noninvasive estimation of right ventricular systolic pressure by Doppler ultrasound in patients with tricuspid regurgitation. Circulation 1984;70:657–62. [DOI] [PubMed] [Google Scholar]
- [9].Skjaerpe T, Hatle L. Diagnosis and assessment of tricuspid regurgitation with Doppler ultrasound. Develop Cardiovasc Med 1981;13:299–304. [Google Scholar]
- [10].Silverton N, Meineri M, Djaiani G. The controversy of right ventricular systolic pressure: is it time to abandon the pulmonary artery catheter? Anaesthesia 2015;70:241–57. [DOI] [PubMed] [Google Scholar]
- [11].Fisher MR, Forfia PR, Chamera E, et al. Accuracy of Doppler echocardiography in the hemodynamic assessment of pulmonary hypertension. Am J Resp Crit Care Med 2009;179:615–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Rich JD. Counterpoint: can Doppler echocardiography estimates of pulmonary artery systolic pressures be relied upon to accurately make the diagnosis of pulmonary hypertension? No. Chest 2013;143:1536–9. [DOI] [PubMed] [Google Scholar]
- [13].Taleb M, Khunder S, Tinkel J, Khouri S. The diagnostic accuracy of Doppler echocardiography in assessment of pulmonary artery systolic pressure: a meta-analysis. Echocardiography 2013;30:258–65. [DOI] [PubMed] [Google Scholar]
- [14].Soliman D, Bolliger D, Skarvan K, Kaufmann BA, LuratiBuse G, Seeberger MD. Intra-opertive assessment of pulmonary artery pressure by transesophageal echocardiography. Anaesthesia 2015;70:264–71. [DOI] [PubMed] [Google Scholar]
- [15].Cowie B, Kluger R, Rex S, Missant C. The utility of transesophageal echocardiography for estimating right ventricular systolic pressure. Anaesthesia 2015;70:258–63. [DOI] [PubMed] [Google Scholar]
- [16].Kovacs G, Avian A, Olschewski A, Olschewski H. Zero reference level for right heart catheterisation. Eur Resp J 2013;42:1586–94. [DOI] [PubMed] [Google Scholar]
- [17].Amsallem M, Sternbach JM, Adigopula S, et al. Addressing the controversy of estimating pulmonary arterial pressure by echocardiography. JASE 2016;29:93–102. [DOI] [PubMed] [Google Scholar]
- [18].Howard LS, Grapsa J, Dawson D, et al. Echocardiographic assessment of pulmonary hypertension: standard operating procedure. Eur Resp Rev 2012;21:239–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].McLaughlin VV, Archer SL, Badesch DB, et al. ACCF/AHA 2009 expert consensus document on pulmonary hypertension. JASE 2009;53:1573–619. [DOI] [PubMed] [Google Scholar]
- [20].Galie N, Hoeper MM, Humbert M, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J 2009;30:2493–537. [DOI] [PubMed] [Google Scholar]
- [21].Vonk MC, Sander MH, van den Hoogen FHJ, van Riel PLCM, Verheugt FWA, van Dijk APJ. Right ventricle Tei-index: a tool to increase the accuracy of non-invasive detection of pulmonary arterial hypertension in connective tissue diseases. Eur J Echocardiogr 2007;8:317–21. [DOI] [PubMed] [Google Scholar]
- [22].Tei C, Nishimura RA, Seward JB, Tajik AJ. Noninvasive Doppler-derived myocardial performance index: correlation with simultaneous measurements of cardiac catheterization measurements. JASE 1997;10:169–78. [DOI] [PubMed] [Google Scholar]
- [23].Dambrauskaite V, Delcroix M, Claus P, et al. The evaluation of pulmonary hypertension using right ventricular myocardial isovolumic relaxation time. JASE 2005;18:1113–20. [DOI] [PubMed] [Google Scholar]
- [24].Arcasoy SM, Christie JD, Ferrari VA, et al. Echocardiographic assessment of pulmonary hypertension in patients with advanced lung disease. Am J Resp Crit Care Med 2003;167:735–40. [DOI] [PubMed] [Google Scholar]
- [25].Laaban JP, Diebold B, Zelinski R, Lafay M, Raffoul H, Rochemaure J. Noninvasive estimation of systolic pulmonary artery pressure using Doppler echocardiography in patients with chronic obstructive pulmonary disease. Chest 1989;96:1258–62. [DOI] [PubMed] [Google Scholar]
- [26].Brecker SJD, Gibbs SR, Fox KM, Yacoub MH, Gibson DG. Comparison of Doppler derived haemodynamic variables and simultaneous high fidelity pressure measurements in severe pulmonary hypertension. Br Heart J 1994;72:384–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].D’Alto M, Romeo E, Argiento P, et al. Accuracy and precision of echocardiography versus right heart catheterization for the assessment of pulmonary hypertension. Int J Cardiology 2013;168:4058–62. [DOI] [PubMed] [Google Scholar]
- [28].Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307–10. [PubMed] [Google Scholar]
- [29].Stewart D, Leman RB, Kaiser J, Mann DL. Catheter-induced tricuspid regurgitation. Incidence and clinical significance. Chest 1991;99:651–5. [DOI] [PubMed] [Google Scholar]
- [30].Kasper J, Bolliger D, Skarvan K, Buser P, Filipovic M, Seeberger MD. Additional cross-sectional transesophageal echocardiography views improve perioperative right heart assessment. Anesthesiology 2012;117:726–34. [DOI] [PubMed] [Google Scholar]