Abstract
Introduction
The aim of this study was to compare the fracture resistance of endodontically treated premolars after the application of three restorative materials (i.e., direct composite, indirect composite, and computer aided design/computer aided manufacturing CAD/CAM ceramic inlays) to restore a conservative occluso-mesial cavity preparation.
Materials and methods
sixty sound maxillary premolars were divided into four experimental groups; group A: the control group, where neither root canal treatment nor preparation were performed; group B: teeth were restored with a direct Filtek Z250 composite restorative material; group C: teeth were restored with an indirect inlay Filtek Z250 composite restorative material; group D: teeth were restored with IPS E.Max CAD/CAM monolithic ceramic inlays. Access cavities and root canal treatment procedures were conducted using standard techniques. Then, the cavities were restored with direct composite restorative materials following manufacturer’s instructions. Each group received mesial-occlusal cavities and restored according to the designated group.
Teeth from all groups were exposed to a thermocycling regimen of 500 cycles in water baths at 5–55 °C. Then, each specimen was mounted on a special fixture on a computer controlled Instron Universal Testing Machine. An axial compressive load was applied to the palatal cusp up to failure at an angle of 45°. The force was applied at the rate of 2 mm/min until visible or audible evidence of fracture was observed. The force at fracture was measured in MPa, and the fracture mode was recorded as either favorable [restorable adhesive fracture above the cemento-enamel junction (CEJ)] or unfavorale (non-restorable fractures under CEJ). The obtained data were analyzed using the SPSS version 21.0 statistical software. One-way ANOVA and Tukey's test were used to compare the mean values of maximum load of the four groups. Pearson's Chi-square test was used to compare the distribution of failure mode among the four groups. The p-value of ≤ 0.05 was used to report the statistical significance of results.
Keywords: CAD/CAM, Composite resin, Endodontically treated teeth, Fracture resistance, Restorative dental materials
1. Introduction
More than 70% of fractured teeth were endodontically treated (ET) (Gher et al., 1987). A common belief among the dental community is that root canal treatment weakens the tooth; however, clinical and laboratory studies have shown that endodontic treatment has limited effect on biomechanical characteristics and no effect on the moisture content of the treated tooth (Dietschi et al., 2007, Huang et al., 1992, Papa and Messer, 1994, Sedgley and Messer, 1992). Hence, it is concluded that other important factors greatly affect the strength of ET teeth (e.g., trauma, the amount of remaining tooth structure, and further endodontic and restorative procedures), which makes ET teeth more prone to fracture (Sedgley and Messer, 1992).
According to Reeh et al., 1989a, Reeh et al., 1989b, endodontic procedures caused only a 5% reduction in the relative stiffness of the tooth, while occlusal and mesial-occluso-distal (MOD) cavity preparations caused 20% and 63% reduction in tooth stiffness, respectively. The authors confirmed that the loss of marginal ridges was responsible for the change in tooth stiffness (Reeh et al., 1989a). Several studies have investigated the effect of marginal ridge thickness on the fracture resistance of endodontically treated teeth, and a direct relationship was observed between the two variables (Shahrbaf et al., 2007). Oliveira et al. have concluded that the amount of remaining tooth structure greatly affects the strength of ET teeth (specifically premolars) (Oliveira and Boyer, 1987).
The relationship between the quality of root canal treatment and coronal restoration on the periapical condition of ET teeth was investigated by Ray and Trope. It was determined that teeth with poor endodontic filling but with good coronal restoration showed the absence of peri-radicular inflammation (67.6%). It was concluded that the quality of coronal restoration was essential compared to the quality of root canal treatment (Ray and Trope, 1995).
The fracture mode of endodontically treated teeth restored with different coronal restorations is different than that of intact teeth. Endodontically treated teeth with a MOD cavity preparation had catastrophic non-restorable fractures (Alshiddi and Aljinbaz, 2016, Hannig et al., 2005, Soares et al., 2008).
Restorative management of ET teeth is a point of controversy around the world. The placement of a post to reinforce endodontically treated teeth is a widespread practice among local and international dentists (Habib et al., 2014, Naumann et al., 2006). However, dental literature indicates that the use of post is not a necessity in the restoration of all endodontically treated teeth. The use of direct or indirect adhesive restorations without a post was suggested to restore ET teeth with conservative cavity preparations. Oliveira et al. have stated that if a tooth is not fractured or severely damaged by caries before root canal treatment, it may be sufficient to treat the access cavity with a simple adhesive restoration. Moreover, restoring teeth with a resin-based composite coupled with acid etching of enamel and dentin can result in the recovery of tooth stiffness of up to 88% (Dammaschke et al., 2013, Eissmann and Radke, 1987, Monga et al., 2009, Nicheva and Filipov, 2013, Reeh et al., 1989b, Stephen and Bonsor, 2013). In a three-year clinical study, the use of fiber-reinforced posts and direct composite restorations in restoring ET premolars with limited loss of tooth structure was determined to be as successful as full coverage with metal–ceramic crowns (Mannocci et al., 2009).
Thus, if the marginal ridges are intact and most of the natural tooth substance is preserved, the routine use of full crowns on ET teeth may not be necessary.
However, although ceramic restorations are time consuming, expensive, and brittle, these esthetic restorations have many advantages compared to resin-based composites such as color stability and marginal adaptation (Sturdevant et al., 2006).
The aim of this study is to compare the fracture resistance of endodontically treated premolars receiving three restorative materials (i.e., direct composite, indirect composite, and CAD/CAM ceramic inlays) to restore a conservative occluso-mesial cavity preparation.
2. Materials and methods
A total of 60 sound maxillary premolar teeth extracted for orthodontic or periodontal reasons were selected. Teeth affected by caries, developmental anomalies, trauma, fracture, and dehydration were excluded. Teeth hydration was maintained before and during experimental procedures by cleaning and storing them in normal saline at room temperature (25–28 °C).
The teeth were randomly assigned into four experimental groups, i.e., groups A–D. Manufacturer recommendations were carefully followed during the preparation of restorations.
Group A: 15 teeth served as the control group, where neither the root canal treatment nor preparation were performed.
Group B: 15 teeth were restored with a direct Filtek™ Z250 universal restorative composite resin material (3 M ESPE, St. Paul, MN, USA).
Group C: 15 teeth were restored with an indirect inlay Filtek Z250 universal restorative composite resin material (3 M ESPE, St. Paul, MN, USA).
Group D: 15 teeth were restored with IPS E.Max CAD full-contour ceramic inlays (Ivoclar Vivadent AG. Liechtenstein, Switzerland).
For groups B, C, and D, access cavities were prepared using a high-speed handpiece and copious amounts of water; the orifices were enlarged up to size 3 Gates Glidden (JS Dental, Switzerland); then, root canals were instrumented with a rotary PROFILE® endodontic system (Dentsply Sirona, Ballaigues, Switzerland) 0.04–0.06 taper to apical size 35 using the crown down technique. The irrigation and conditioning of canals were performed during instrumentation using standard protocols. After biomechanical preparation, canals were obturated with gutta percha (Diadent, Group International Inc., Cheongju, Korea) and an AH Plus root canal sealer (Dentsply DeTrey, Konstanz, Germany) using cold lateral condensation. Obturation was performed up to 1 mm below the level of the cemento-enamel junction.
Cavities of the tested groups were cleaned, etched with 37% phosphoric acid for 15 s (Total etch, Ivoclar Vivadent, Liechtenstein, Switzerland), irrigated with water for 10 s, and gently dried. Bond (Excite, Ivoclar Vivadent. Liechtenstein, Switzerland) was applied for 20 s and cured for 15 s. A dual cure composite restorative material (MultiCore, Ivoclar Vivadent. Liechtenstein, Switzerland) was applied to fill both the canal orifices and cavities and was cured for 40 s.
Except for group A, an occluso-mesial (OM) cavity preparation was performed on all specimens. Standardized cavity preparation dimensions were followed: the bucco-lingual width of the proximal box was equal to the intercuspal distance, and the width of the occlusal isthmus was 50% of the intercuspal distance. The mesio-distal width of the intact distal marginal ridge was 1.5 mm. The axial wall of the proximal box was prepared at 60–90° to the gingival floor with 6° divergence using a tapered diamond bur. The occlusal isthmus depth was 1.5 mm, and the distance between the gingival floor of the proximal box and CEJ was 1 mm; all measurements were performed using a periodontal probe. Indirect restorations were cemented using a dual cured resin cement (Multilink, Ivoclar Vivadent, Liechtenstein, Switzerland) following the manufacturer’s instructions. The fitting surface of each restoration received a primer (Monobond S, Ivoclar Vivadent, Liechtenstein, Switzerland) for 60 s. Then, the cavity preparation was etched with 37% phosphoric acid (Total etch, Ivoclar Vivadent, Liechtenstein, Switzerland) for 30 s on the enamel and for 15 s on the dentine followed by the application of a bonding agent (Excite, Ivoclar Vivadent, Liechtenstein, Switzerland) for 15 s. Finally, resin cement (Multilink, Ivoclar Vivadent, Liechtenstein, Switzerland) was mixed and applied to the fitting surface of each restoration. Excess cement was removed, and the restoration was cured for 60 s.
2.1. Procedure for testing samples for fracture resistance and fracture mode
Teeth from all groups were exposed to a thermocycling regimen of 500 cycles in water baths at 5–55 °C; the dwell time was 30 s with a 10-s transfer time between baths. Then, each tooth was vertically mounted with its root embedded into a plastic cylinder of self-curing acrylic resin up to 1 mm below the CEJ and was stored in normal saline at room temperature. The specimen block was mounted on a special fixture on a computer-controlled Instron Universal Testing Machine (Model-4467, Instron Coronation Road, High Wycombe, Buckinghamshire, UK). The axial compressive load was applied to the palatal cusp up to failure at an angle of 45° to its longitudinal axis with a steel obliquely sloping compressive head. The force was applied at the rate of 2 mm/min until visible or audible evidence of fracture or indication of inability of the specimen to withstand a greater load was observed.
The force at fracture was measured in MPa, and the fracture mode was recorded as:
Favorable: restorable adhesive fracture above the cemento-enamel junction (CEJ)
Unfavorable: non-restorable fractures under CEJ.
2.2. Data analysis
The data were collected and analyzed using the SPSS version 21.0 statistical software. Descriptive statistics (i.e., mean, standard deviation, standard error, frequencies, and percentages) were used to describe the outcome variables (i.e., maximum load and failure type). One-way ANOVA analysis of variance was used to compare the mean values of maximum load in relation to the four groups followed by Tukey's test of multiple comparison of mean values. Pearson's Chi-square test was used to compare the distribution of failure mode among the four groups. The p-value of ≤ 0.05 was used to report the statistical significance of results.
3. Results
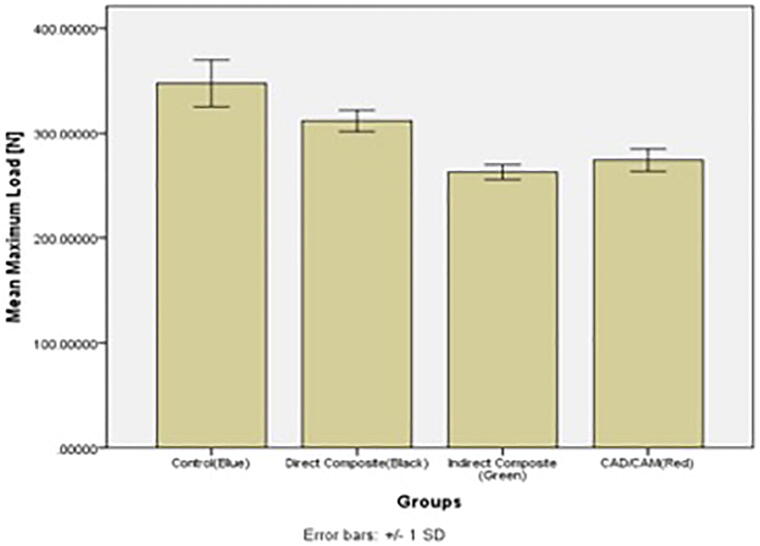
The mean fracture resistance values obtained for each group are shown in Table 1, Table 2 and Fig. 1.
Table 1.
Comparison of the Mean Values of Maximum Load Among the 4 Study Groups.
| Group | Mean of FR (Sd.) | F-value | p-value |
|---|---|---|---|
| Control Direct Composite Indirect Composite CAD/CAM |
347.36 (22.19) 311.77 (10.13) 262.87 (7.10) 274.16 (10.65) |
116.54 | <0.0001 |
Table 2.
Comparison of the Mean Values of Maximum Load Among the 4 Study Groups.
| Dependent Variable | (I) Group1 | (J) Group1 | Mean Difference (I-J) | p-value |
|---|---|---|---|---|
| Maximum Load [N] | Control (Blue) | Direct Composite (Black) | 35.59618933* | <0.0001 |
| Indirect Composite (Green) | 84.49970400* | <0.0001 | ||
| CAD/CAM (Red) | 73.20491533* | <0.0001 | ||
| Direct Composite (Black) | Control (Blue) | −35.59618933* | <0.0001 | |
| Indirect Composite (Green) | 48.90351467* | <0.0001 | ||
| CAD/CAM (Red) | 37.60872600* | <0.0001 | ||
| Indirect Composite (Green) | Control (Blue) | −84.49970400* | <0.0001 | |
| Direct Composite (Black) | −48.90351467* | <0.0001 | ||
| CAD/CAM (Red) | −11.29478867 | 0.124 | ||
| CAD/CAM (Red) | Control (Blue) | −73.20491533* | <0.0001 | |
| Direct Composite (Black) | −37.60872600* | <0.0001 | ||
| Indirect Composite (Green) | 11.29478867 | 0.124 |
Fig. 1.
Bar Chart of the Mean Values of Maximum Load Among the 4 Study Groups.
The multiple comparison of mean values indicates that the fracture resistance values are statistically significantly lower in samples of teeth restored by indirect composite and CAD/CAM milled restorations compared with those of teeth restored by direct composite restorations and untreated teeth. There is no significant difference between the mean values of maximum load of indirect composite (262.87) and CAD/CAM (274.16) groups. However, the fracture resistance of the control group (347.36) is statistically significantly higher than that of direct composite restorations (311.77).
The distribution and comparison of fracture mode (favorable and unfavorable) among the four groups shows no statistically significant difference (X2 = 0.754, p = 0.860) (Table 3 and Fig. 2).
Table 3.
Distribution and Comparison of the Failure Mode of the 4 Study Groups.
| Groups | Fracture Mode | Total | X2-value | p-value | |
|---|---|---|---|---|---|
| Unfavorable | Favorable | ||||
| Control Direct Composite Indirect Composite CAD/CAM |
8 (53.3) 8 (53.3) 10 (66.7) 9 (60) |
7 (46.7) 7 (46.7) 5 (33.3) 6 (40) |
15 15 15 15 |
0.754 | 0.860 |
Fig. 2.
Distribution and Comparison of the Failure Mode of the 4 Study Groups.
4. Discussion
Dammaschke et al have concluded that factors such as gender, age, and type and position of tooth (premolar or molar) did not significantly affect the tooth fracture rate (Dammaschke et al., 2013). Furthermore, Nam S-H et al. and Nagasiri et al. showed the superior rigidity of a tooth with an MO or OD cavity to that with an MOD cavity and a significant decrease in fracture resistance if only two or fewer cavity walls remained. Furthermore, the amount of remaining tooth structure and the type of restorative material have significant association with the longevity of ET molars (Nagasiri and Chitmongkolsuk, 2005, Nam et al., 2010).
In this study, the fracture resistance of endodontically treated maxillary premolars with a conservative occluso-mesial access cavity preparation restored with three different restorative materials (i.e., direct Filtek Z250 composite, indirect Filtek Z250 composite, and IPS E.Max CAD/CAM full contour ceramic inlays) was tested.
The obtained results showed a significant difference in the fracture resistance between group A (control group) and group B (teeth resorted with direct composite restoration), which support the conclusion by Shahrbaf et al. that preserving marginal didges had a preferable impact on the fracture resistance of endodontically treated maxillary premolars (Shahrbaf et al., 2007).
Bassir et al. have determined that conservative direct and indirect adhesive restorations in occluso-mesial and occluso-mesio-distal cavities can increase the fracture resistance of endodontically treated premolars to be as high as that of sound teeth (Bassir et al., 2013). However, in this study, there were significant differences between group A (untreated teeth) and other tested groups; the fracture resistance of group B (teeth restored with direct composite restoration) was significantly higher than that of groups C and D (teeth restored with indirect restorations).
Soares et al. conclusions regarding fracture resistance and fracture mode were similar to those in the present study. Specifically, restored teeth showed higher fracture resistance values with greater amount of remaining tooth structure. In addition, a great variation in the mode of fracture appeared among groups in both studies (Soares et al., 2008).
The limitation of this study was that only intact teeth were used in the control group, and there was no negative control group which should have consisted of prepared teeth without restorations. Hence, this issue should be considered in future studies. In addition, of note, this study was performed under in vitro conditions. Thus, the conditions in this study are not identical to the real intra-oral conditions, although an attempt was made to simulate the oral environment. Therefore, the obtained results cannot be applied directly in the clinical practice. The applied load was only in one direction; one point and continually increasing load was applied to teeth, which did not simulate many ways of masticatory force exertion and parafunctional forces. Thus, further studies on the longevity of restorative techniques simulating the clinical conditions and the possible influence of parafunctional forces in addition to clinical studies to verify in vitro results are recommended.
Because this study showed that the direct composite restoration group exhibited the highest fracture resistance values among the groups compared to the intact teeth group, its use is recommended to restore the two-wall access cavity preparation of endodontically treated maxillary premolars rather than indirect composite or CAD/CAM ceramic restorations.
5. Conclusion
A significant difference between the control group and other groups was observed. Direct composite restorations showed the highest fracture resistance followed by CAD/CAM ceramic restorations and indirect composite restorations. There was no significant difference in fracture resistance between CAD/CAM and indirect composite restorations. No significant difference was observed in the fracture mode between all groups.
Ethical statement
This study was performed using only extracted teeth and did not include humans or animals. Therefore, ethical approval was not required.
Disclosure statement
The authors do not have any financial interest in the companies whose materials are included in this article.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
The authors would like to acknowledge the CDRC and Deanship of Scientific Research at the College of Dentistry at King Saud University for their valuable and continuous support.
Footnotes
Peer review under responsibility of King Saud University.
Contributor Information
Salwa Omar Bajunaid, Email: sbajunaid@ksu.edu.sa.
Norah Omar AlSadhan, Email: Noalsadhan@gmail.com.
Noura AlBuqmi, Email: nourabuqmi@gmail.com.
References
- Alshiddi I., Aljinbaz A. Fracture resistance of endodontically treated teeth restored with indirect composite inlay and onlay restorations – An in vitro study. Saudi Dent. J. 2016;28(1):49–55. doi: 10.1016/j.sdentj.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassir M., Labibzadeh A., Mollaverdi F. The effect of amount of lost tooth structure and restorative technique on fracture resistance of endodontically treated premolars. J. Conserv. Dent. 2013;16(5):413–417. doi: 10.4103/0972-0707.117494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dammaschke, T., Nykiel, K., Sagheri, D., Schäfer, E., 2013. Influence of coronal restorations on the fracture resistance of root canal-treated premolar and molar teeth: a retrospective study. Aust. Endod. J. 39, 2, 48–56. [DOI] [PubMed]
- Dietschi D., Duc O., Krejci I., Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature—part 1: composition and micro- and macrostructure alterations. Quint. Int. 2007;38(9):733–743. [PubMed] [Google Scholar]
- Eissmann, H.F., Radke, R.A. Jr., 1987. Post Endodontic restoration. Cohen S, Burns RC, eds. Pathways of the pulp. Fourth ed. St Louis: Mosby; 640–643.
- Gher M.E., Jr., Dunlap R.M., Anderson M.H., Kuhl L.V. Clinical survey of fractured teeth. J. Am. Dent. Assoc. 1987;114(2):174–177. doi: 10.14219/jada.archive.1987.0006. [DOI] [PubMed] [Google Scholar]
- Habib S.R., Al Rifaiy M.Q., Alkunain J., Alhasan M., Albahrani J. Concepts of restoring endodontically treated teeth among dentists in Saudi Arabia. Saudi. J. Dent. Res. 2014;5(1):15–20. [Google Scholar]
- Hannig Ch., Westphal Ch., Becker K., Attin T. Fracture resistance of endodontically treated maxillary premolars restored with CAD/CAM ceramic inlays. The J. Prosth. 2005;94(4):342–349. doi: 10.1016/j.prosdent.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Huang T.-J., Schilder H., Nathanson D. Effects of moisture content and endodontic treatment on some mechanical properties of human dentin. J. Endodon. 1992;18(5):209–215. doi: 10.1016/S0099-2399(06)81262-8. [DOI] [PubMed] [Google Scholar]
- Mannocci F., Bertelli E., Sherriff M., Watson T.F., Ford T.R. Three-year clinical comparison of survival of endodontically treated teeth restored with either full cast coverage or with direct composite restoration. Int. Endod. J. 2009;42(5):401–405. doi: 10.1111/j.1365-2591.2009.01559.x. [DOI] [PubMed] [Google Scholar]
- Monga P., Sharma V., Kumar S. Comparison of fracture resistance of endodontically treated teeth using different coronal restorative materials: An in vitro study. J. Conserv. Dent. 2009;12(4):154–159. doi: 10.4103/0972-0707.58338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagasiri R., Chitmongkolsuk S. Long-term survival of endodontically treated molars without crown coverage: a retrospective cohort study. J. Prosth. Dent. 2005;93(2):164–170. doi: 10.1016/j.prosdent.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Nam S.H., Chang H.S., Min K.S., Lee Y., Cho H.W., Bae J.M. Effect of the number of residual walls on fracture resistance, failure patterns, and photoelasticity of simulated premolars restored with or without fiber-reinforced composite posts. J. Endod. 2010;36(2):297–301. doi: 10.1016/j.joen.2009.10.010. [DOI] [PubMed] [Google Scholar]
- Naumann M., Kiessling S., Seemann R. Treatment concepts for restoration of endodontically treated teeth: A nationwide survey of dentists in Germany. J. Prosth. Dentistry. 2006;96(5):332–338. doi: 10.1016/j.prosdent.2006.08.028. [DOI] [PubMed] [Google Scholar]
- Nicheva S., Filipov I. Restoration of endodontically treated posterior teeth with direct and indirect composite – 6-month results. J. IMAB. Annual. Proceeding. 2013;19(4):396–400. [Google Scholar]
- Oliveira Fde, Boyer D.B. Fracture resistance of endodontically prepared teeth using various restorative materials. J. Am. Dent. Ass. 1987;115(1):57–60. doi: 10.14219/jada.archive.1987.0212. [DOI] [PubMed] [Google Scholar]
- Papa C. Cain, Messer H. Moisture content of vital vs endodontically treated teeth. Endodon. Den. Trauma. 1994;10(2):91–93. doi: 10.1111/j.1600-9657.1994.tb00067.x. [DOI] [PubMed] [Google Scholar]
- Reeh E.S., Messer H.H., Douglas W.H. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J. Endodon. 1989;15(1):512–516. doi: 10.1016/S0099-2399(89)80191-8. [DOI] [PubMed] [Google Scholar]
- Reeh E.S., Douglas W.H., Messer H.H. Stiffness of endodontically treated teeth related to restoration technique. J. Dent. Res. 1989;68(1):1540–1544. doi: 10.1177/00220345890680111401. [DOI] [PubMed] [Google Scholar]
- Ray H.A., Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int. Endo. J. 1995;28(1):12–18. doi: 10.1111/j.1365-2591.1995.tb00150.x. [DOI] [PubMed] [Google Scholar]
- Sedgley C., Messer H. Are endodontically treated teeth more brittle? J. Endodon. 1992;18(7):332–335. doi: 10.1016/S0099-2399(06)80483-8. [DOI] [PubMed] [Google Scholar]
- Shahrbaf S., Mirzakouchaki B., Oskoui S.S., Kahnamoui M.A. The Effect of Marginal Ridge Thickness on the Fracture Resistance of Endodontically-treated. Composite Restored Maxillary Premolars. Oper. Dent. 2007;32(3):285–290. doi: 10.2341/06-83. [DOI] [PubMed] [Google Scholar]
- Soares P.V., Santos-Filho P.C., Queiroz E.C., Araújo T.C., Campos R.E., Araújo C.A., Soares C.J. Fracture resistance and stress distribution in endodontically treated maxillary premolars restored with composite resin. J. Prosth. 2008;17(2):114–119. doi: 10.1111/j.1532-849X.2007.00258.x. [DOI] [PubMed] [Google Scholar]
- Stephen J., Bonsor Gavin Pearson. Elsevier; 2013. A Clinical Guide to Applied Dental Materials; p. 98. Chapter 7. [Google Scholar]
- Sturdevant, C.M., Roberson, M.A., Heymann, H., 2006. Sturdevant's Art and Science of Operative Dentistry. Elsevier Health Sciences. Swift EJ, Fifth Edition. chapter 4. 141–143.