Abstract
Pre-exposure prophylaxis (PrEP) has limited availability across Latin America, though access is increasing. We explored PrEP uptake in Mexico via an online survey completed by Spanish-speaking, Hornet geosocial networking application (GSN app) users without HIV (n=2,020). Most (81.3%) had heard of PrEP, 3.5% were current users, and 34.2% intended to take PrEP within six months. Current PrEP use was associated with PrEP eligibility (aOR 26.07 [95%CI 13.05–52.09], p<0.001), recent STI testing (aOR 3.79 [95%CI 1.10–13.11], p=0.035), and recent chemsex (aOR 3.02 [95%CI 1.02–8.93], p=0.046). Recent STI testing was associated with hearing about PrEP from a doctor (aOR 3.26 [95%CI 1.98–5.36], p<0.001), and those who lived in large cities were less likely to have learned about PrEP via Hornet (aOR 0.52 [95%CI 0.32–0.85], p=0.009). Interventions to increase PrEP uptake in Mexico should build upon existing health networks and utilize GSN apps for PrEP information dissemination, particularly in less populated areas.
Keywords: pre-exposure prophylaxis, men who have sex with men, HIV, mobile app, Mexico
RESUMEN
La profilaxis pre-exposición (PrEP) tiene disponibilidad limitada en América Latina, aunque su acceso está aumentando. Exploramos el uso de PrEP en México a través de una encuesta en línea para sujetos hispanohablantes sin VIH usuarios de la aplicación de redes geosociales (GSN app) Hornet (n=2,020). La mayoría (81,3%) había escuchado sobre PrEP, el 3,5% eran usuarios actuales, y el 34,2% tenía intención de tomar PrEP en seis meses o menos. El uso actual de PrEP estuvo asociado con la elegibilidad de tomar PrEP (aOR 26.07 [95%CI 13.05–52.09], p<0.001), tener prueba reciente para ITS (aOR 3.79 [95%CI 1.10–13.11], p=0.035), y chemsex reciente (aOR 3.02 [95%CI 1.02–8.93], p=0.046). Tener prueba reciente para ITS se asoció con escuchar sobre PrEP de un médico (aOR 3.26 [95%CI 1.98–5.36], p<0.001), y quienes vivían en ciudades grandes tenían menos probabilidad de conocer acerca de PrEP a través de Hornet (aOR 0.52 [95%CI 0.32–0.85], p=0.009). Las intervenciones para aumentar el uso de PrEP en México deberían basarse en redes de salud existentes y usar las GSN apps para difundir información sobre PrEP, particularmente en áreas menos pobladas.
INTRODUCTION
Pre-exposure prophylaxis (PrEP) with daily oral tenofovir disoproxil fumarate and emtricitabine (TDF-FTC) has been shown to be safe and highly effective in preventing HIV acquisition, with a greater than 90% risk reduction when taken daily (1–4). The World Health Organization (WHO) recommends that oral PrEP be offered as a daily or event-driven prevention option to those at high risk of acquiring HIV (5, 6). Men who have sex with men (MSM) and transgender women (TW) are at a disproportionately high risk of acquiring HIV globally, and could benefit from expanded PrEP availability (7, 8).
In Latin America, there is a need for increased HIV prevention efforts (9). While most regions of the world have seen a decline in recent years in the annual number of new HIV diagnoses, the annual incidence in Latin America has increased, with 120,000 new HIV diagnoses in 2019 among adults age 15 years or older compared to 100,000 in 2010 (10–12). Roughly 74% of the new HIV diagnoses in Latin America in 2019 were in males (12), and at least 40% of diagnoses in 2018 were in MSM (9, 13). Mexico accounts for roughly 14% of new diagnoses in Latin America, ranked second behind Brazil (10). As of 2020, the only Latin American countries, excluding the Caribbean, which had incorporated the WHO oral PrEP recommendations into national guidelines were Brazil and Chile (14, 15), with access elsewhere either non-existent or limited to research studies, private providers, and the internet (7, 9, 14, 16, 17). However, efforts are currently underway via the Implementation PrEP (ImPrEP) Project to increase PrEP uptake among MSM and TW in Mexico, as well as in Brazil and Peru (18).
Mexico is a middle-income country with an estimated population of nearly 130 million people (19). The HIV prevalence among MSM in Mexico is estimated to be as high as 20.7%, compared to 0.2% of the general population (9, 19, 20). Recent studies focusing on MSM in Mexico have demonstrated increasing PrEP awareness, as well as a high willingness to use PrEP (21–24). While these studies primarily explored barriers affecting willingness to take PrEP, there remains a lack of literature exploring existing PrEP uptake as well as the behavioral intention to use PrEP among MSM in Mexico. The present study recruited users from Hornet, a geosocial networking application (GSN app), to further explore associations with PrEP awareness, current use, intention to use, and information source among MSM in Mexico, in order to inform efforts to expand PrEP access across the country.
METHODS
Study Design
This cross-sectional study utilized an internet-based survey; the methodology is described according to the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) (25). The respondents were a convenience sample of adult (≥ 18 years old) users of the Hornet Gay Social Network (Hornet) GSN app recruited between December 2018 and February 2019. As the Hornet GSN app is marketed for gay men, we did not include questions or exclusion criteria pertaining to gender identity or sexual orientation. Recruitment took place via the Hornet direct inbox message system, which requested voluntary participation in “a brief survey which will also connect you with important information for your sexual health.” The recruitment message was sent three times over three months, and survey responses were collected through February 2019. In order to target participants from the Latin America region, the recruitment message was sent to users with Spanish as their primary language and users whose registration location was in Latin America. There was no compensation for participation, and only one survey response per internet protocol (IP) address was permitted.
Survey
This open survey was administered through the SurveyMonkey online survey platform (26). The survey was in Spanish and consisted of 19 questions addressing demographic and sexual health information, as well as awareness of, use of, and intention to use PrEP (Supplemental Document). Respondents were allowed to review and change their answers after proceeding. A completeness check was performed after the submission and compilation of the survey responses. Prior to taking the survey, participants were provided with the following statement on PrEP:
PrEP (pre-exposure prophylaxis) is an effective method to prevent HIV. It is becoming a popular option to help gay men take control of their sexual health. We are helping to collect data in order to recommend and advocate for this HIV prevention tool.
After completion of the survey, respondents were provided with additional information on both PrEP and sexual health, in addition to a list of country-specific PrEP resources and health care providers.
Variables
Demographics
Respondents’ ages were collected as a categorical variable using age ranges: 18–25, 26–30, 31–40, 41–50, 51–60, 61–70, and 70+. The age groups of 41–50, 51–60, 61–70, and 70+ were combined into a 41+ group for analysis. Participants were asked in which country they lived; however, for the present study, only respondents from Mexico were included. Additionally, respondents provided the name of the city in which they lived, which was used to create variables for city population size and border state. City population counts were obtained via the 2010 Mexico national census data, and population size categories were created based on the Organization for Economic Co-operation and Development urban area classifications (27, 28). Respondents were considered to be from a border state if they lived in one of the Mexican states bordering the United States (US), which included Baja California, Sonora, Chihuahua, Coahuila, Nuevo León, and Tamaulipas.
Sexual health
Respondents were asked about their HIV status via the question, “Are you HIV positive?” People living with HIV (PLWH) were excluded from this analysis. Participants were also asked about recent (in the previous 12 months) sexually transmitted infection (STI) testing and diagnoses, as well as post-exposure prophylaxis (PEP) use. Recent PEP use and STI diagnosis, both of which are PrEP eligibility criteria in the PAHO guidelines (29), were used to create a new PrEP eligible variable. Drug use during sex (chemsex) was assessed by asking respondents if they had used mephedrone, gamma hydroxybutyrate (GHB)/gamma butyrolactone (GBL), ketamine, or methamphetamine during sex in the previous three months. A five-point Likert scale was used to assess participants’ happiness with their sex life; the answers “very happy” and “happy” were combined into “Happy,” and the answers “unhappy,” and “very unhappy” were combined into “Not Happy.”
PrEP Awareness, Use, Intention to Use, and Information Source
PrEP awareness was assessed via the question “Have you heard about PrEP?” Answer options included “Yes” or “No.” Those who indicated that they had heard of PrEP then selected one of eight options for the question “Where have you heard about PrEP?” PrEP use was assessed by asking “Are you currently taking PrEP?” Answer options included “Yes” or “No.” Those who were currently taking PrEP were then asked where they obtained PrEP. We did not ask about prior PrEP use. Intention to use PrEP was assessed by asking participants’ agreement with the following statement: “It is very likely that I will use PrEP in the next 6 months.” Five-point Likert scale responses were then combined in order to create a bivariate response. The answers “totally agree” and “agree” were combined into “Agree,” and the answers “I don’t know,” “disagree,” and “strongly disagree” were combined into “Do Not Agree.”
Statistical Analysis
Outcomes
The dichotomous variables awareness of PrEP, current use of PrEP, and intention to use PrEP severed as outcomes for this analysis. Additionally, the following four sources of PrEP information were converted into dichotomous outcomes for analysis: internet, doctor, Hornet GSN app, and friends. For example, internet as a source of PrEP information was compared against all other sources, doctor as a source of PrEP information was compared against all other sources, etc.
Analysis and Regression Models
Only completed questionnaires were included in this analysis. All outcome variables were dichotomous and were compared using Pearson’s χ2 statistic, as well as univariable and multivariable odds ratio in logistic regression with 95% confidence intervals (95% CI). For all outcomes, the following “exposures” were analyzed: PrEP eligibility, recent STI testing, and chemsex. City population size was also analyzed as a predictor of source of PrEP information. Individual multivariable logistic regression models were created for each exposure. For each full model, age and city population size were included as confounders, and additional confounding variables were selected based on previous research (23, 30, 31) as well as hypotheses regarding associations. The confounders selected for each regression model are listed as footnotes below each table. Analysis of these data was performed using Stata/IC 16.1.
Ethics
This study received approval from the University of California Los Angeles (UCLA) Institutional Review Board. Respondents provided written consent via the first question of the survey. No identifiable information was collected except for IP address, which is linked to the device or network used to complete the survey. Lastly, our study took advantage of the collaboration with Hornet to disseminate PrEP and sexual health information to MSM across Latin America who may not have otherwise had access to such information.
RESULTS
A total of 4,461 individuals started the survey, with 3,595 completing all of the required questions. For this analysis, we excluded n=1,134 from countries other than Mexico and n=441 PLWH. Consequently, there were 2,020 respondents who met the inclusion criteria and were included in this analysis (Figure 1).
Figure 1:
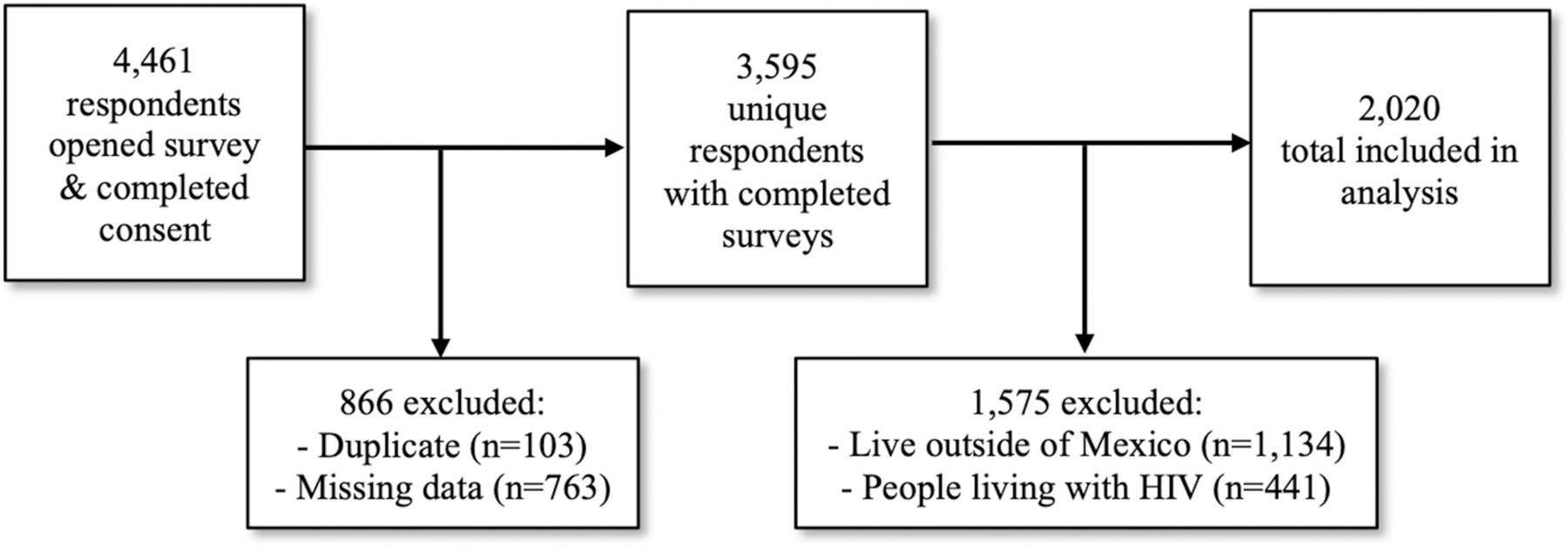
Respondent inclusion flow chart
Table I presents the demographic data as well as the responses to the questions pertaining to sexual health. A majority of the respondents were between 18 and 30 years old (n=1,157, 57.3%). Most (n=1,492, 73.9%) lived in cities with a population of at least 1.5 million inhabitants, largely represented by Mexico City (n=1,315, 65.1%; Figure 2). Only 10.1% (n=205) lived in cities with a population of less than 500,000, and an even smaller percentage (n=66, 3.3%) were from a Mexican state which borders the US. In the previous 12 months, 65.7% (n=1,328) had been tested for an STI, 7.7% (n=156) had received an STI diagnosis, and 5.1% (n=102) had used PEP. Considering recent PEP use and recent STI diagnosis as criteria, n=242 (12.0%) of respondents were technically eligible for PrEP. Few respondents (n=65, 3.2%) reported chemsex in the previous three months, and a majority (n=1,546, 76.5%) indicated that they were either happy or very happy with their sex life.
Table I:
Respondent Demographics and Sexual Health Responses from Mexican GSN App Users in 2018–2019
| Variable | Total, n (%) n=2,020 |
|---|---|
| Age | |
| 18–25 | 657 (32.5) |
| 26–30 | 500 (24.8) |
| 31–40 | 558 (27.6) |
| 41+ | 305 (15.1) |
|
| |
| City Population Size | |
| > 1.5 mil. | 1,492 (73.9) |
| 500,000 – 1.5mil. | 323 (16.0) |
| <500,000 | 205 (10.1) |
|
| |
| Border State with US | |
| Yes | 66 (3.3) |
| No | 1,954 (96.7) |
|
| |
| HIV Status a, b | |
| Uninfected | 1,686 (83.5) |
| Status Unknown | 334 (16.5) |
|
| |
| Recent (12 months) PEP Use | |
| Yes c | 102 (5.1) |
|
| |
| Recent (12 months) STI testing | |
| Yes | 1,328 (65.7) |
|
| |
| Recent (12 months) STI diagnosis | |
| Yes c | 156 (7.7) |
| Not sure | 99 (4.9) |
|
| |
| Recent (3 months) chemsex d | |
| Yes | 65 (3.2) |
|
| |
| Sex Life Happiness | |
| Happy | 1,546 (76.5) |
| Not Happy | 151 (7.5) |
| Not sure | 323 (16.0) |
PLWH were removed from analysis; there were a total of n=441 PLWH from Mexico excluded
Respondents were not asked about timing of most recent HIV test
Recent PEP use and recent STI diagnosis were used to create a new PrEP eligible variable
Survey question specified the following drugs: Mephedrone, GHB/GBL, Ketamine, Methamphetamine. GHB and GBL stand for gamma hydroxybutyrate and gamma butyrolactone, respectively. However only the abbreviation was used in the survey.
Abbreviations: mil. (million), HIV (human immunodeficiency virus), PEP (post-exposure prophylaxis), STI (sexually transmitted infection)
Figure 2:

Map of Mexican cities with at least 10 survey respondents
* Includes respondents who listed Mexico City or one of its 16 municipalities. Cities within the greater Mexico City metropolitan area, such as Cuautitlán Izcalli, Coacalco, Ecatepec, and Nezahualcóyotl, were considered separate.
PrEP uptake was low (Table II); 1,642 (81.3%) respondents had heard about PrEP, the majority of which (n=864, 52.6%) indicated they had heard about PrEP via the internet. Fewer had learned about PrEP from a doctor (n=186, 11.3%), from the Hornet GSN app (n=149, 9.1%), or from friends (n=133, 8.1%). Of those who had heard of PrEP, 3.5% (n=58) were currently taking PrEP, the majority of which (n=51, 87.9%) had acquired PrEP through either a research study or a doctor (Figure 3). Of those aware of PrEP and not currently taking it, 34.2% (n=541) agreed it was likely they would take PrEP in the next six months.
Table II:
PrEP Awareness, Use, and Intention to Use Among Mexican GSN App Users in 2018–2019
| Variable | Total, n (%) n=2,020 |
|---|---|
| Have you heard about PrEP? | |
| Yes | 1,642 (81.3) |
| No | 378 (18.7) |
|
Where have you heard about
PrEP?
n=1,642 a |
|
| Internet | 864 (52.6) |
| Doctor | 186 (11.3) |
| Hornet | 149 (9.1) |
| Friends | 133 (8.1) |
| Dating Applications b | 126 (7.7) |
| 82 (5.0) | |
| Television | 21 (1.3) |
| Other | 81 (4.9) |
|
Are you currently taking PrEP?
n=1,642 a |
|
| Yes | 58 (3.5) |
| No | 1,584 (96.5) |
|
It is very likely I will use PrEP in
the next 6 months
n=1,584 c |
|
| Agree | 541 (34.2) |
| Do not agree | 1,043 (65.8) |
Source of PrEP information and current use of PrEP include only those who responded they had heard of PrEP
No specific application was listed other than Hornet, which was a separate option. This alternative option was “Aplicaciones de citas/Dating applications”
Intention to Use PrEP includes only those who had heard of PrEP and who were not currently taking PrEP
Abbreviations: PrEP (pre-exposure prophylaxis)
Figure 3:
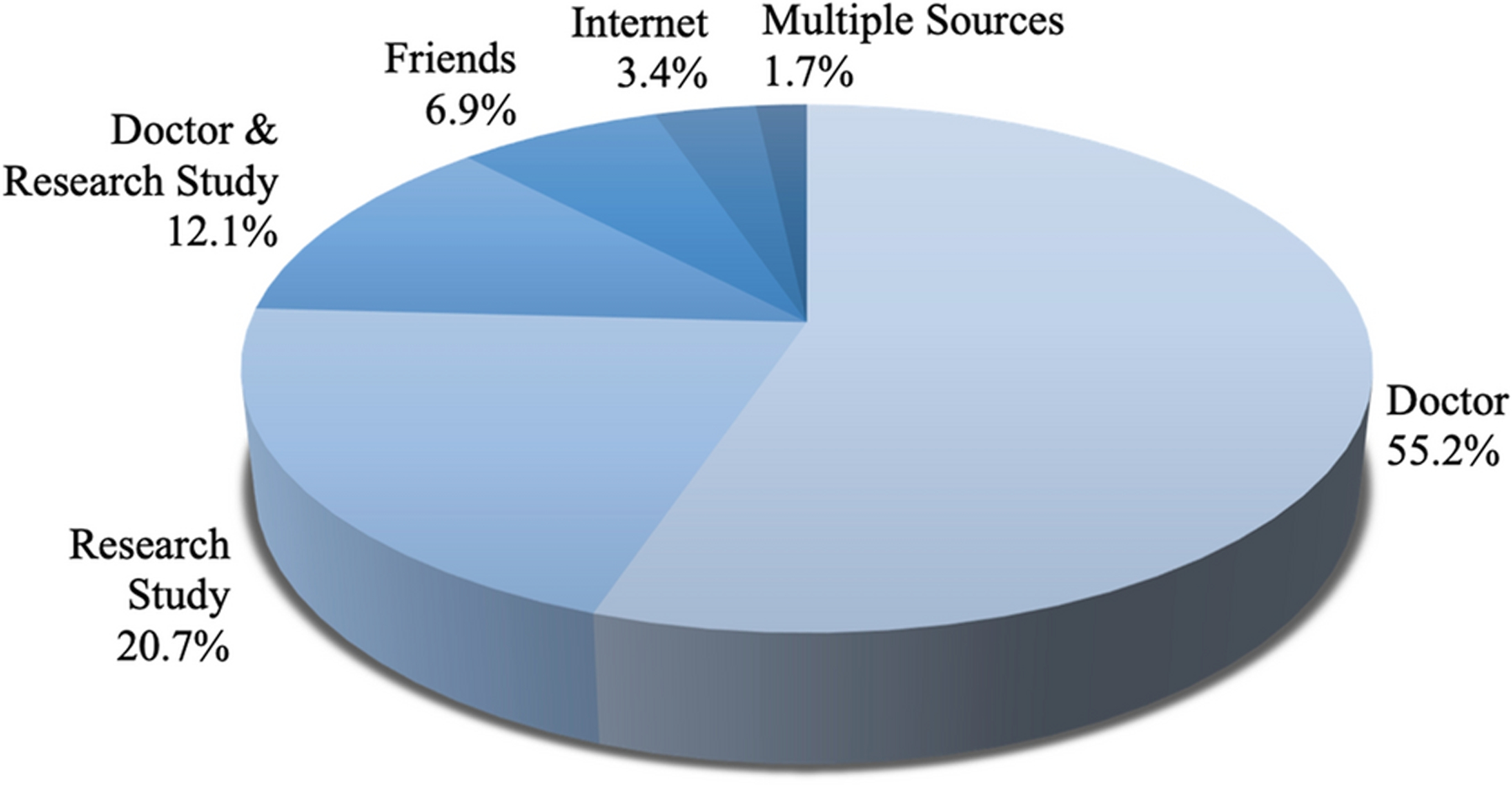
Source of PrEP for current users
Univariable logistic regressions predicting awareness of, current use of, and intention to use PrEP are presented in Table III. Age was associated with PrEP awareness on univariable analysis, with the 26–30 (OR 1.80, [95% CI 1.33–2.46], p<0.001) and 31–40 (OR 1.87 [95% CI 1.38–2.52], p<0.001) age groups being more likely to have heard about PrEP compared to the 18–25 age group. Those in larger population centers were more likely to have heard about PrEP (OR 1.50 [95% CI 1.05–2.13], p=0.024). Having an unknown HIV status was associated with lower PrEP awareness (73.9% vs. 81.4%, OR 0.59 [95% CI 0.45–0.78], p<0.001], but greater intention to use PrEP (40.8% vs. 33.0%, OR 1.40 [95% CI 1.06–1.86], p=0.018) on univariable analysis. Living in a Mexican state on the US/Mexico border, which was only included in univariable analysis, was associated with a greater intention to take PrEP (49.0% vs. 33.7%, OR 1.90 [95% CI 1.08–3.31], p=0.025).
Table III:
Univariable Regressions Predicting Awareness of, Current Use of, or Intention to Use PrEP Among Mexican GSN App Users in 2018–2019
| Variable | Awareness of
PrEP n=2,020 |
Current Use of
PrEP n=1,642 a |
Intention to Use
PrEP n=1,584 b |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes n (%) |
No n (%) |
OR [95% CI] | p value | Yes n (%) |
No n (%) |
OR [95% CI] | p value | Agree n (%) |
Do Not Agree n (%) |
OR [95% CI] | p value | |
| Age | ||||||||||||
| 18–25 | 504 (76.7) | 153 (23.3) | Ref. | Ref. | 12 (2.4) | 492 (97.6) | Ref. | Ref. | 175 (35.6) | 317 (64.4) | Ref. | Ref. |
| 26–30 | 428 (85.6) | 72 (14.4) | 1.80 [1.33–2.46] | < 0.001 | 17 (4.0) | 411 (96.0) | 1.70 [0.80–3.59] | 0.168 | 154 (37.5) | 257 (62.5) | 1.09 [0.83–1.42] | 0.555 |
| 31–40 | 480 (86.0) | 78 (14.0) | 1.87 [1.38–2.52] | < 0.001 | 16 (3.3) | 464 (96.7) | 1.41 [0.66–3.02] | 0.371 | 142 (30.6) | 322 (69.4) | 0.80 [0.61–1.05] | 0.103 |
| 41+ | 230 (75.4) | 75 (24.6) | 0.93 [0.68–1.28] | 0.658 | 13 (5.7) | 217 (94.3) | 2.46 [1.10–5.47] | 0.028 | 70 (32.3) | 147 (67.7) | 0.86 [0.61–1.21] | 0.393 |
| City Population Size | ||||||||||||
| > 1.5 mil. | 1,239 (83.0) | 253 (17.0) | 1.50 [1.05–2.13] | 0.024 | 45 (3.6) | 1,194 (96.4) | 1.93 [0.59–6.30] | 0.273 | 399 (33.4) | 795 (66.6) | 0.74 [0.53–1.05] | 0.093 |
| 500,000–1.5mil. | 246 (76.2) | 77 (23.8) | 0.98 [0.65–1.48] | 0.911 | 10 (4.1) | 236 (95.9) | 2.18 [0.59–8.03] | 0.244 | 80 (33.9) | 156 (66.1) | 0.76 [0.50–1.16] | 0.202 |
| < 500,000 | 157 (76.6) | 48 (23.4) | Ref. | Ref. | 3 (1.9) | 154 (98.1) | Ref. | Ref. | 62 (40.3) | 92 (59.7) | Ref. | Ref. |
| Border State | ||||||||||||
| Yes | 52 (78.8) | 14 (21.2) | 0.85 [0.47–1.55] | 0.597 | 1 (1.9) | 51 (98.1) | 0.53 [0.07–3.88] | 0.530 | 25 (49.0) | 26 (51.0) | 1.90 [1.08–3.31] | 0.025 |
| No | 1,590 (81.4) | 364 (18.6) | Ref. | Ref. | 57 (3.6) | 1,533 (96.4) | Ref. | Ref. | 516 (33.7) | 1,017 (66.3) | Ref. | Ref. |
| HIV Status | ||||||||||||
| Unknown Status | 247 (73.9) | 87 (26.1) | 0.59 [0.45–0.78] | < 0.001 | 7 (2.8) | 240 (97.2) | 0.77 [0.34–1.71] | 0.520 | 98 (40.8) | 142 (59.2) | 1.40 [1.06–1.86] | 0.018 |
| Negative | 1,395 (82.7) | 291 (17.3) | Ref. | Ref. | 51 (3.7) | 1,344 (96.3) | Ref. | Ref. | 443 (33.0) | 901 (67.0) | Ref. | Ref. |
| PrEP Eligible c | ||||||||||||
| Yes | 218 (90.1) | 24 (9.9) | 2.26 [1.46–3.50] | < 0.001 | 47 (21.6) | 171 (78.4) | 35.31 [17.97–69.37] | < 0.001 | 70 (40.9) | 101 (59.1) | 1.39 [1.00–1.92] | 0.048 |
| No | 1,424 (80.1) | 354 (19.9) | Ref. | Ref. | 11 (0.8) | 1,413 (99.2) | Ref. | Ref. | 471 (33.3) | 942 (66.7) | Ref. | Ref. |
| Recent (12 months) STI Testing | ||||||||||||
| Yes | 1,133 (85.3) | 195 (14.7) | 2.09 [1.66–2.62] | < 0.001 | 55 (4.9) | 1,078 (95.1) | 8.61 [2.68–27.64] | < 0.001 | 366 (34.0) | 712 (66.0) | 0.97 [0.78–1.21] | 0.804 |
| No | 509 (73.6) | 183 (26.4) | Ref. | Ref. | 3 (0.6) | 506 (99.4) | Ref. | Ref. | 175 (34.6) | 331 (65.4) | Ref. | Ref. |
| Recent (3 months) Chemsex d | ||||||||||||
| Yes | 52 (80.0) | 13 (20.0) | 0.92 [0.49–1.70] | 0.787 | 6 (11.5) | 46 (88.5) | 3.86 [1.58–9.44] | 0.003 | 22 (47.8) | 24 (52.2) | 1.80 [1.00–3.24] | 0.050 |
| No | 1,590 (81.3) | 365 (18.7) | Ref. | Ref. | 52 (3.3) | 1,538 (96.7) | Ref. | Ref. | 519 (33.8) | 1,019 (66.2) | Ref. | Ref. |
Bolded ORs had a p value of ≤ 0.05
Current use of PrEP includes only those who had heard of PrEP
Intention to use PrEP includes only those who had heard of PrEP who were not currently taking PrEP
Recent PEP use and STI diagnosis, both of which are PrEP eligibility criteria in the PAHO guidelines (29), were used to create the PrEP eligible variable
Survey question specified the following drugs: Mephedrone, GHB/GBL, Ketamine, Methamphetamine. GHB and GBL stand for gamma hydroxybutyrate and gamma butyrolactone, respectively. However only the abbreviation was used in the survey
Abbreviations: OR (odds ratio), CI (confidence interval), PrEP (pre-exposure prophylaxis), Pop. (population), mil. (million), STI (sexually transmitted infection)
Table IV presents multivariable logistic regressions predicting awareness of, current use of, and intention to use PrEP for the exposure variables PrEP eligible, recent STI testing, and recent chemsex. PrEP eligibility was associated with PrEP awareness (aOR 1.86 [95% CI 1.19–2.91], p=0.006) and current use of PrEP (aOR 26.07 [13.05–52.09], p<0.001). Recent STI testing was also associated with increased awareness of (aOR 1.79 [95% CI 1.39–2.30], p<0.001) and current use of PrEP (aOR 3.79 [95% CI 1.10–13.11], p=0.035). Chemsex was associated with greater odds of current PrEP use (aOR 3.02 [95% CI 1.02–8.93], p=0.046). When predicting intention to use PrEP, PrEP eligibility (40.9% vs. 33.3%, OR 1.39 [1.00–1.92], p=0.048) and recent chemsex (47.8% vs. 33.8%, OR 1.80 [95% CI 1.00–3.24], p=0.050) were only significantly associated on univariable analysis (Table III); however, both PrEP eligibility and chemsex demonstrated a trend toward significance on multivariable analysis.
Table IV:
Multivariable Regressions Predicting Awareness of, Current Use of, and Intention to Use PrEP Among Mexican GSN App Users in 2018–2019
| Variable | Awareness of
PrEP n=2,020 |
Current Use of
PrEP n=1,642 a |
Intention to Use
PrEP n=1,584 a |
|||
|---|---|---|---|---|---|---|
| aOR [95% CI] | p value | aOR [95% CI] | p value | aOR [95% CI] | p value | |
| PrEP Eligible b,d | ||||||
| Yes c | 1.86 [1.19–2.91] | 0.006 | 26.07 [13.05–52.09] | < 0.001 | 1.37 [0.98–1.91] | 0.062 |
| Recent (12 months) STI Testing e | ||||||
| Yes c | 1.79 [1.39–2.30] | < 0.001 | 3.79 [1.10–13.11] | 0.035 | 1.05 [0.82–1.34] | 0.714 |
| Recent (3 months) Chemsex f,g | ||||||
| Yes c | 0.75 [0.40–1.42] | 0.381 | 3.02 [1.02–8.93] | 0.046 | 1.71 [0.94–3.10] | 0.078 |
Bolded aORs had a p value of ≤ 0.05
Current use of PrEP includes only those who had heard of PrEP (n=1,642); intention to use PrEP includes only those who had heard of PrEP who were not currently taking PrEP (n=1,584)
Recent PEP use and STI diagnosis, both of which are PrEP eligibility criteria in the PAHO guidelines (29), were used to create the PrEP eligible variable
Compared against “No”
Regression models for PrEP eligible included the following confounders: age, city population size, recent STI testing, chemsex, and doctor as source of PrEP information
Regression models for recent STI testing included the following confounders: age, city population size, HIV status, PrEP eligible, chemsex, and doctor as source of PrEP information
Regression models for recent chemsex included the following confounders: age, city population size, PrEP eligible, recent STI testing, and friends as source of PrEP information
Survey question specified the following drugs: Mephedrone, GHB/GBL, Ketamine, Methamphetamine. GHB and GBL stand for gamma hydroxybutyrate and gamma butyrolactone, respectively. However only the abbreviation was used in the survey
Abbreviations: aOR (adjusted odds ratio), CI (confidence interval), PrEP (pre-exposure prophylaxis), STI (sexually transmitted infection)
The multivariable logistic regressions predicting sources of PrEP information for the exposure variables of city population size, PrEP eligibility, recent STI testing, and recent chemsex are presented in Table V. Those who were PrEP eligible were more likely to have heard about PrEP through a doctor (aOR 2.60 [95% CI 1.81–3.75], p<0.001), and less so through the internet (aOR 0.71 [95% CI 0.53–0.95], p=0.023). Similarly, recent STI testing was positively associated with hearing about PrEP from a doctor (aOR 3.26 [95% CI 1.98–5.36], p<0.001), and negatively associated with hearing about PrEP via the internet (aOR 0.76 [95% CI 0.60–0.95], p=0.017). Hornet was less likely to be the source of PrEP information in cities with populations of 1.5 million or greater (aOR 0.52 [95% CI 0.32–0.85], p=0.009), when compared to cities with populations of less than 500,000. Recent chemsex was associated with learning about PrEP through friends (aOR 3.11 [95% CI 1.55–6.24], p=0.001).
Table V:
Multivariable Regressions Predicting Source of PrEP Information Among Mexican GSN App Users in 2018–2019
| Variable | Internet a | Doctor b | Hornet GSN app c | Friends d | ||||
|---|---|---|---|---|---|---|---|---|
| aOR [95% CI] | p value | aOR [95% CI] | p value | aOR [95% CI] | p value | aOR [95% CI] | p value | |
| City Population Size g | ||||||||
| > 1.5 mil | 1.05 [0.75–1.47] | 0.776 | 1.27 [0.72–2.25] | 0.416 | 0.52 [0.32–0.85] | 0.009 | 1.06 [0.57–1.99] | 0.851 |
| 500,000 – 1.5mil | 1.05 [0.70–1.58] | 0.808 | 0.84 [0.41–1.71] | 0.623 | 0.56 [0.30–1.04] | 0.068 | 0.87 [0.40–1.89] | 0.733 |
| < 500,000 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| PrEP Eligible e,h | ||||||||
| Yes f | 0.71 [0.53–0.95] | 0.023 | 2.60 [1.81–3.75] | < 0.001 | 0.63 [0.35–1.15] | 0.135 | 1.21 [0.74–1.98] | 0.447 |
|
Recent (12 months)
STI Testing i |
||||||||
| Yes f | 0.76 [0.60–0.95] | 0.017 | 3.26 [1.98–5.36] | < 0.001 | 0.92 [0.62–1.35] | 0.657 | 1.30 [0.84–2.03] | 0.240 |
| Recent (3 months) Chemsex j | ||||||||
| Yes f | 0.57 [0.32–1.01] | 0.054 | 1.39 [0.65–2.97] | 0.394 | 0.93 [0.33–2.64] | 0.889 | 3.11 [1.55–6.24] | 0.001 |
Bolded aORs had a p value of ≤ 0.05
Internet (n=864, 52.6%) as source of PrEP information compared to all other sources (n=778, 47.4%)
Doctor (n=186, 11.3%) as source of PrEP information compared to all other sources (n=1,456, 88.7%)
Hornet (n=149, 9.1%) as source of PrEP information compared to all other sources (n=1,493, 90.9%)
Friends (n=133, 8.1%) as source of PrEP information compared to all other sources (n=1,509, 91.9%)
Recent PEP use and STI diagnosis, both of which are PrEP eligibility criteria in the PAHO guidelines (29), were used to create the PrEP eligible variable
Compared against “No”
Regression models for city population size included the following confounders: age, recent STI testing, PrEP eligible, and chemsex
Regression models for PrEP eligible included the following confounders: age, city population size, recent STI testing, and chemsex
Regression models for recent STI testing included the following confounders: age, city population size, HIV status, PrEP eligible, and chemsex
Regression models for recent chemsex included the following confounders: age, city population size, PrEP eligible, and recent STI testing
Abbreviations: aOR (adjusted odds ratio), CI (confidence interval), PrEP (pre-exposure prophylaxis), mil. (million), STI (sexually transmitted infection)
DISCUSSION
This study builds upon existing research to further describe the uptake of and intention to use PrEP among MSM in Mexico (22–24). Awareness of PrEP among GSN app users in Mexico was high (81.3%), particularly among respondents aged 26 to 40 when compared to the 18 to 25 age group, and those from large population centers. The internet was the primary source of PrEP information. Notably, PrEP awareness was higher in this study compared to previous reports. Recently reported data from GSN app users in Mexico in 2018 showed that 64.1% were aware of PrEP, while a meta-analysis published in 2017 calculated a pooled PrEP awareness of 29.7% in low- and middle-income countries (23, 31). Our data were collected roughly six months after the previously reported Mexico data, and it is possible that awareness could have increased during this time as a result of the expanding influence of the ImPrEP project (18). One qualitative study of MSM focus groups suggested that PrEP knowledge is higher among GSN app users, which may explain the differences between our data and the low PrEP awareness of 17.0% reported among MSM in Tijuana, Mexico (24). Additionally, our survey was conducted through a single GSN app, and the increased rate of PrEP awareness could represent a more informed user base.
Greater awareness of PrEP, however, does not directly translate to increased PrEP use. Despite high rates of PrEP awareness in our cohort, current use remains low, suggesting a continued need to identify and address barriers to use, such as cost and access (24). Additionally, although previous reports indicated a majority of MSM in Mexico were willing to take PrEP, our data show that a much smaller percentage of respondents intended to take PrEP in the subsequent six months (22, 23). The differentiation between intention and willingness to use PrEP has been explored previously, similarly concluding that larger percentages of respondents were willing to take PrEP compared to those who actually intended to take PrEP in the near future (32). In our study, respondents indicated their intention to use PrEP through agreement with the statement “It is very likely that I will use PrEP in the next 6 months,” which contrasts with other studies that asked if respondents were willing to use PrEP (23, 31, 33, 34). We believe that by specifying the six-month time frame, our question captures respondents who are closer to the action of actually taking PrEP, which is why we chose to label it as intention rather than willingness (32); or, in the terminology of the motivational PrEP cascade, we believe by adding a time frame the question has moved from capturing those in the contemplation stage toward those who may be in the preparation phase (35).
Moving from willingness to intention has been shown to be more likely in those who believe PrEP is efficacious and in those who see themselves as appropriate candidates for PrEP (32). Among Mexican MSM, however, beliefs about PrEP efficacy and side effects continue to be a significant barrier to use, indicating a need for improved counseling on PrEP (23, 36). Our findings demonstrate an existing association between sexual health care and PrEP uptake, as participants who were eligible for PrEP and been tested for STIs were more likely to be aware of PrEP or to be currently taking PrEP. Moreover, while the majority of respondents who were aware of PrEP indicated they had heard of PrEP via the internet, those who were PrEP eligible or had been tested for STIs were less likely to have learned about PrEP via the internet, and more likely to have learned about PrEP from a doctor. Efforts to improve the dissemination of accurate PrEP information and counseling provided to MSM should thus start with points of contact with the health care system. Health care access in Mexico has been increasing in recent years, and is similar to other middle-income countries in Latin America (37). However, not all health care providers are prepared to offer counseling regarding PrEP use, and MSM in Latin America continue to report concern about discrimination from providers regarding their sexual health practices (22, 24, 38). Improving the availability of information about PrEP at points of contact with the health care system is crucial, and efforts to expand PrEP uptake in Mexico should not only work to connect MSM with sexual health services, but also to prepare providers to effectively counsel their patients.
While access to sexual health care would ideally equate with access to PrEP, there remains a lack of widespread availability of PrEP in Mexico, and accessing PrEP through the private market can be expensive (24). A majority of respondents reporting PrEP use in our study obtained their medication from a doctor. However, since PrEP is not publicly available in Mexico, it was likely purchased at a high price (24). Others obtained PrEP through a research study, such as ImPrEP, though this does not guarantee continued access once the study concludes (18). In order to encourage PrEP use in Mexico, especially for those of lower socioeconomic status, it is imperative that a low-cost, generic option be available. In Patrick et al, 87.6% of MSM surveyed stated they would be willing to take PrEP if it were available for free. This number dropped to 59.6% when asked if they would be willing to pay for PrEP, with only 31.0% willing to pay more than 350 pesos (~18.50 USD) per month (22). Similarly, Torres et al found that 72.8% of respondents considered free PrEP as a very important facilitator to them using PrEP (23).
Previous studies in the region have found an association between high risk sexual behaviors and awareness of or willingness to take PrEP (23, 30). Survey questions of recent PEP use and STI diagnosis were used to categorize respondents as PrEP eligible; both PrEP eligibility and recent chemsex were significantly associated current PrEP use, with a trend toward significantly higher intention to use PrEP in the subsequent six months. Interestingly, those who reported chemsex in the previous three months were more likely to have heard about PrEP from friends, suggesting peer networks as another important means by which PrEP information could be disseminated. Percentage of respondents engaging in chemsex was lower in our study (3.2%) compared to Mexican respondents in Torres et al (23) (16.0%); however, we asked about chemsex over a shorter time period (3 months vs. 6 months), listed fewer specific substances, and phrased the question in a different way. Rates of recent PEP use and STI diagnoses between the two studies were similar (23), but the percentage eligible for PrEP was lower in our cohort, likely because our survey lacked additional questions pertaining to sexual risk behaviors which are used to determine PrEP eligibility (29).
Geography may also have an effect on PrEP uptake. Previous reports found that willingness to take PrEP varied across regions of Mexico, and MSM focus group discussions suggested a difference between urban and rural areas in terms of access to sexual health services and PrEP (23, 24). Our study found that MSM who live in larger population centers were more likely to be aware of PrEP on univariable analysis, though no association was found with current use or intention to use. An increased awareness of PrEP in larger cities may come from larger and more integrated MSM communities, less discrimination, or easier access to health services (39). It is important, then, to consider ways in which information about PrEP can be disseminated to smaller cities and rural areas. Interestingly, we found that those who learned about PrEP via the Hornet GSN app were more likely to be from cities with fewer than 500,000 inhabitants, suggesting GSN apps may be a useful tool for disseminating information to less populated areas. Notably, this includes both smaller cities in rural areas as well as those located within the greater metropolitan area of larger population centers, such as Mexico City. In recent years, GSN apps have been utilized to disseminate sexual health information as well as to recruit for participation in research studies, and these platforms have the potential to provide tailored and targeted information about PrEP to MSM in harder to reach areas (24, 40–43). It is important to note, however, that there are still some in Mexico without internet access who would need to reached by other means (44). An additional geographic difference encountered in our data was an increased intention to use PrEP in the next six months among those who lived in states bordering the US. We did not include living in a border state as an exposure in our multivariable models due to a low number of respondents, but it should be considered for future studies on PrEP uptake in Mexico. Previous research has demonstrated a unique social, cultural, and political environment in regions which border the US, and it is possible that the increased intention to use PrEP in these states is a result of cultural influences from the US where PrEP is more widely available (45).
There are several limitations to this study. First, while the Hornet GSN app is marketed for gay men, an estimated five percent of users are transgender individuals who have sex with men. Since our survey did not include transgender exclusion criteria, it is possible that a small percentage of respondents to this survey were transgender individuals who have sex with men, rather than MSM. Additionally, none of the questions in the survey directly addressed sexual orientation nor sexual practices. As a voluntary, online survey conducted through one of many GSN apps, the sample of respondents is not necessarily representative of the Mexican MSM population, and those with access to a device compatible with Hornet may represent a higher socioeconomic group. Social desirability bias could have influenced respondent answers as well. Our determination of PrEP eligibility per the WHO guidelines lacked data pertaining to condomless anal intercourse or partners with HIV risk factors, and we did not consider respondents’ potential access to PrEP when asking about their current use of or intention to use to PrEP. While we have excluded PLWH from this analysis, we did not include a question on timing of most recent HIV testing, and it is possible some of those included had acquired HIV since their most recent test or had never been tested. We did not include a question on hypothetical willingness to take PrEP, although Rendina et al 2017 recommends surveys include both a question addressing willingness and one for behavioral intention (32). Respondents were provided with a brief statement describing PrEP before initiating the survey, which could have impacted their responses to having heard about PrEP. Our question examining source of PrEP information only permitted one answer choice, which may fail to capture respondents who had heard of PrEP from multiple sources. Lastly, while our survey provided respondents with country-specific information on access to PrEP and sexual health care, the online nature of this survey did not allow for the provision of psychosocial or social service support some may have required.
CONCLUSIONS
This study provides important additional insights into the uptake of and intention to use PrEP among MSM in Mexico, which is highly relevant in the context of the ImPrEP project and the desire to expand access to PrEP across the country. Interventions to increase PrEP uptake in Mexico should build upon and expand access to sexual health care, as well as make use of the various GSN apps to reach MSM in less populated areas of the country.
Supplementary Material
ACKNOWLEDGEMENTS
These data were presented at the 2019 IAS Conference on HIV Science in Mexico City (abstract MOAD0301). This project was funded by the University of California Los Angeles’ South American Program in HIV Prevention Research (SAPHIR) NIMH grant R25MH087222. This work was also supported by the UCLA Center for HIV Identification, Prevention, and Treatment Services (CHIPTS) NIMH grant P30MH58107. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH. Author A.G. is a senior health innovation strategist at Hornet Gay Social Network. The remaining authors (K.J.B., E.R.S, J.L., A.R., S.L.G., V.G.R., J.E.L., J.C., and I.W.H.) have no conflicts of interest to report.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflicts of Interest: Author A.G. is a senior health innovation strategist at Hornet Gay Social Network, which was used for dissemination of the survey used in this study. The content of this paper is solely the responsibility of the authors; Hornet had no influence over the analysis or interpretation of results. The remaining authors (K.J.B., E.R.S, J.L., A.R., S.L.G., V.G.R., J.E.L., J.C., and I.W.H.) have no conflicts of interest to report.
Ethics approval: UCLA Institutional Review Board
Consent to participate: Question 1 of survey (supplemental document)
Consent for publication: N/A
Availability of Data / Code Availability: N/A
Other: These data were presented at the 2019 IAS Conference on HIV Science in Mexico City (abstract MOAD0301).
REFERENCES:
- 1.Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure Chemoprophylaxis for HIV Prevention in Men Who Have Sex with Men. N Engl J Med. 2010;363(27):2587–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34. [DOI] [PubMed] [Google Scholar]
- 3.Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson PL, Glidden DV, Liu A, Buchbinder S, Lama JR, Guanira JV, et al. Emtricitabine-Tenofovir Concentrations and Pre-Exposure Prophylaxis Efficacy in Men Who Have Sex with Men. Science Translational Medicine. 2012;4(151). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Organization WH. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: What’s New. Geneva, Switzerland: World Health Organization; 2015. [Google Scholar]
- 6.WHO. What’s the 2+1+1? Event-Driven Oral Pre-Exposure Prophylasix to Prevent HIV for Men who Have Sex with Men: Update to WHO’s Recommendation on Oral PrEP. WHO; 2019. [Google Scholar]
- 7.Hodges-Mameletzis I, Dalal S, Msimanga-Radebe B, Rodolph M, Baggaley R. Going global: the adoption of the World Health Organization’s enabling recommendation on oral pre-exposure prophylaxis for HIV. Sex Health. 2018;15(6):489–500. [DOI] [PubMed] [Google Scholar]
- 8.Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, et al. Global epidemiology of HIV infection in men who have sex with men. The Lancet. 2012;380(9839):367–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.UNAIDS. Miles to Go: The Response to HIV in Latin America. Geneva, Switzerland: Joint United Nations; 2018. [Google Scholar]
- 10.UNAIDS. Ending AIDS: Progress Towards the 90–90–90 Target. UNAIDS; 2017. [Google Scholar]
- 11.UNAIDS. New HIV infections rising in Latin America - key populations particularly affected. UNAIDS; 2019. 14 Oct 2019. [Google Scholar]
- 12.UNAIDS. AIDSinfo [Available from: https://aidsinfo.unaids.org/.
- 13.UNAIDS. New HIV infections rising in Latin America - key populations particularly affected: UNAIDS; 2019. [Available from: https://www.unaids.org/en/resources/presscentre/featurestories/2019/october/20191014_latin-america. [Google Scholar]
- 14.UNAIDS. Laws and Policies Analytics: UNAIDS; [Available from: http://lawsandpolicies.unaids.org/topicresult?i=742. [Google Scholar]
- 15.HIV Policy Lab: Georgetown University; [Available from: https://www.hivpolicylab.org/. [Google Scholar]
- 16.Galea JT, Baruch R, Brown B. ¡PrEP Ya! Latin America wants PrEP, and Brazil leads the way. The Lancet HIV. 2018;5:e110–e2. [DOI] [PubMed] [Google Scholar]
- 17.Luz PM, Veloso VG, Grinsztejn B. The HIV epidemic in Latin America: accomplishments and challenges on treatment and prevention. Curr Opin HIV AIDS. 2019;14(5):366–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Veloso VG, Vega-Ramírez EH, Hoagland B, Konda KA, Bautista-Arredondo S, Guanira JV, et al. , editors. Safety, early continuation and adherence of same day PrEP initiation among MSM and TGW in Brazil, Mexico and Peru: the ImPrEP Study. IAS Conference; 2019; Mexico City, Mexico. [Google Scholar]
- 19.C.I.A. World Factbook - Mexico Washington, DC: Central Intelligence Agency; 2020. [Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/mx.html. [Google Scholar]
- 20.Bautista-Arredondo S, Colchero MA, Romero M, Conde-Glez CJ, Sosa-Rubi SG. Is the HIV epidemic stable among MSM in Mexico? HIV prevalence and risk behavior results from a nationally representative survey among men who have sex with men. PLoS One. 2013;8(9):e72616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Edeza A, Galarraga O, Novak D, Mayer K, Rosenberger J, Mimiaga M, et al. The role of sexual risk behaviors on PrEP awareness and interest among men who have sex with men in Latin America. International Journal of STD & AIDS. 2019;30(6):542–9. [DOI] [PubMed] [Google Scholar]
- 22.Patrick R, Jain J, Harvey-Vera A, Semple SJ, Rangel G, Patterson TL, et al. Perceived barriers to pre-exposure prophylaxis use among HIV-negative men who have sex with men in Tijuana, Mexico: A latent class analysis. PLoS One. 2019;14(8):e0221558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Torres TS, Konda KA, Vega-Ramirez EH, Elorreaga OA, Diaz-Sosa D, Hoagland B, et al. Factors Associated With Willingness to Use Pre-Exposure Prophylaxis in Brazil, Mexico, and Peru: Web-Based Survey Among Men Who Have Sex With Men. JMIR Public Health Surveill. 2019;5(2):e13771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baruch R, Cuadra SM, Arellano J, Sanchez D, Ortega DV, Arredondo A. Pre-exposure prophylaxis and its implications in Mexico: notions of men who have sex with men. Sex Health. 2020. [DOI] [PubMed]
- 25.Eysenbach G Improving the Quality of Web Surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res. 2004;6(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.SurveyMonkey Inc. San Mateo, California, USA: [Available from: www.surveymonkey.com. [Google Scholar]
- 27.OECD. Definition of Functional Urban Areas (FUA) for the OECD metropolitan database. United States: OECD; 2013. [Google Scholar]
- 28.Censo de Población y Vivienda 2010: Instituto Nacional de Estadística y Geografía; [Available from: https://www.inegi.org.mx/programas/ccpv/2010/.
- 29.PAHO. HIV Prevention in the Spotlight: An analysis from the perspective of the health sector in Latin America and the Caribbean. Washington, DC: Pan American Health Organization; 2017. [Google Scholar]
- 30.Assaf RD, Konda KA, Torres TS, Vega-Ramírez EH, Elorreaga OA, Diaz-Sosa D, et al. , editors. Association of Higher Risk and PrEP Awareness Among MSM in Brazil, Mexico, and Peru. CROI; 2019; Seattle, Washington, USA. [Google Scholar]
- 31.Yi S, Tuot S, Mwai GW, Ngin C, Chhim K, Pal K, et al. Awareness and willingness to use HIV pre-exposure prophylaxis among men who have sex with men in low- and middle-income countries: a systematic review and meta-analysis. J Int AIDS Soc. 2017;20(1):21580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rendina HJ, Whitfield TH, Grov C, Starks TJ, Parsons JT. Distinguishing hypothetical willingness from behavioral intentions to initiate HIV pre-exposure prophylaxis (PrEP): Findings from a large cohort of gay and bisexual men in the U.S. Soc Sci Med. 2017;172:115–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Torres TS, De Boni RB, de Vasconcellos MT, Luz PM, Hoagland B, Moreira RI, et al. Awareness of Prevention Strategies and Willingness to Use Preexposure Prophylaxis in Brazilian Men Who Have Sex With Men Using Apps for Sexual Encounters: Online Cross-Sectional Study. JMIR Public Health Surveill. 2018;4(1):e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoagland B, De Boni RB, Moreira RI, Madruga JV, Kallas EG, Goulart SP, et al. Awareness and Willingness to Use Pre-exposure Prophylaxis (PrEP) Among Men Who Have Sex with Men and Transgender Women in Brazil. AIDS Behav. 2017;21(5):1278–87. [DOI] [PubMed] [Google Scholar]
- 35.Parsons JT, Rendina HJ, Lassiter JM, Whitfield TH, Starks TJ, Grov C. Uptake of HIV Pre-Exposure Prophylaxis (PrEP) in a National Cohort of Gay and Bisexual Men in the United States. J Acquir Immune Defic Syndr. 2017;74(3):285–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ofori VB, Assaf RD, Konda KA, Torres TS, Vega-Ramírez EH, Elorreaga OA, et al. , editors. PrEP-Related Barriers Among Men Who Have Sex With Men in Brazil, Mexico, & Peru. CROI; 2019; Seattle, Washington, USA. [Google Scholar]
- 37.Institute For Health Metrics and Evaluation. Healthcare Access and Quality Profile: Mexico. Seattle, WA, USA: University of Washington; 2018. [Google Scholar]
- 38.Magno L, Dourado I, Sutten Coats C, Wilhite D, da Silva LAV, Oni-Orisan O, et al. Knowledge and willingness to use pre-exposure prophylaxis among men who have sex with men in Northeastern Brazil. Glob Public Health. 2019;14(8):1098–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fisher CM, Irwin JA, Coleman JD. LGBT health in the midlands: a rural/urban comparison of basic health indicators. J Homosex. 2014;61(8):1062–90. [DOI] [PubMed] [Google Scholar]
- 40.Newcomb ME, Mongrella MC, Weis B, McMillen SJ, Mustanski B. Partner Disclosure of PrEP Use and Undetectable Viral Load on Geosocial Networking Apps. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2016;71(2):200–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Buttram ME, Kurtz SP. Representations of Pre-exposure Prophylaxis, Informal Antiretroviral Medication Use for HIV Prevention, and Diversion on Geosocial Networking Apps among Men Who Have Sex with Men. AIDS Behav. 2019;23(7):1790–6. [DOI] [PubMed] [Google Scholar]
- 42.Taggart T, Grewe ME, Conserve DF, Gliwa C, Roman Isler M. Social Media and HIV: A Systematic Review of Uses of Social Media in HIV Communication. J Med Internet Res. 2015;17(11):e248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pantalone DW, Holloway IW, Goldblatt AEA, Gorman KR, Herbitter C, Grov C. The Impact of Pre-Exposure Prophylaxis on Sexual Communication and Sexual Behavior of Urban Gay and Bisexual Men. Archives of Sexual Behavior. 2019;49(1):147–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.(INEGI) INdEyG. Information and communication technologies in households [Available from: http://en.www.inegi.org.mx/temas/ticshogares/default.html#Informacion_general.
- 45.Ramos R, Ferreira-Pinto JB, Brouwer KC, Ramos ME, Lozada RM, Firestone-Cruz M, et al. A tale of two cities: Social and environmental influences shaping risk factors and protective behaviors in two Mexico-US border cities. Health Place. 2009;15(4):999–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


