Abstract
Background:
Rapidly growing coronavirus disease 2019 (COVID-19) pandemic has brought unprecedented challenges to the health system in Nepal. The main objective of this study was to explore the health system preparedness for COVID-19 and its impacts on frontline health-care workers in Nepal.
Methods:
Semi-structured interviews were conducted among 32 health-care workers who were involved in clinical care of COVID-19 patients and four policy-makers who were responsible for COVID-19 control and management at central and provincial level. Interviews were conducted through telephone or Internet-based tools such as Zoom and Skype. All interviews were audio-recorded, transcribed into English, and coded using inductive and deductive approaches.
Results:
Both health-care workers and policy-makers reported failure to initiate pre-emptive control measures at the early stages of the outbreak as the pivot in pandemic control. Although several measures were rolled out when cases started to appear, the overall health system preparedness was low. The poor governance, and coordination between three tiers of government was compounded by the inadequate personal protective equipment for health-care workers, insufficient isolation beds for patients, and poor engagement of the private sector. Frontline health-care workers experienced various degrees of stigma because of their profession and yet were able to maintain their motivation to continue serving patients.
Conclusion:
Preparedness for COVID-19 was affected by the poor coordination between three tiers of governance. Specifically, the lack of human resources, inadequate logistic chain management and laboratory facilities for testing COVID-19 appeared to have jeopardized the health system preparedness and escalated the pandemic in Nepal. Despite the poor preparedness, and health and safety concerns, health-care workers maintained their motivation. There is an urgent need for an effective coordination mechanism between various tiers of health structure (including private sector) in addition to incentivizing the health-care workers for the current and future pandemics.
Keywords: COVID-19, health system, health system preparedness, health workers, Nepal
In December of 2019, a clustered outbreak of pneumonia, later named as coronavirus disease 2019 (COVID-19), was reported in Wuhan, China.1 As of January 3, 2021, over 84 million confirmed cases and nearly 2 million deaths related to COVID-19 have been reported globally.2 The first case of COVID-19 in Nepal was reported on January 13, 2020,3 and in almost a year, there were 261,438 confirmed cases and 1870 deaths reported from the country.2 As of May 2021, Nepal experienced a second wave that has resulted into 460,000 active COVID-19 cases and has claimed more than 5000 lives.2
Nepal’s health system fundamentally suffers from constrained health-care resources including physical infrastructure and skilled human resource.4–6 The fragile health system is struggling to manage the rising COVID-19 pandemic; specifically in adequately screening suspected cases, testing and treating them.7 Although, the country made progress in expanding the number of laboratory testing facilities in the past few months,8 the existing diagnostic facilities were inadequate, and the services at the peripheral parts of the country were few and far between.7 Twenty-five hospitals in Nepal were designated as the hub hospitals with dedicated isolation facilities for COVID-19 patients, but most of them were mostly unprepared for the surge of COVID-19 infections mainly due to the lack of resources that included limited intensive care units (ICUs), isolation wards, human resources,5,7,9 and adequate personal protective equipment (PPE).10 The inadequate preparedness11 was further exposed during the current (second) wave where transmission, severity, and mortality were much higher than in the first wave leading to an overwhelming burden to the health system, and once again under-preparedness was proven fatal for both India and Nepal.12
The constraints occurring at health service and personal level can have a huge psychological impact on health-care workers (HCWs), resulting in stress, anxiety, and depression.13,14 The recent global reports of high infection and deaths among HCWs in addition to stress and pressures at the workplace are alarming and can have devastating consequences to the denominator population. Although the initial surge of COVID-19 pandemic drew massive attention, the progressive decline, specifically in health system’s response in Nepal is noteworthy. For instance, despite the rising cases of COVID-19, Nepal halted the proactive case identification and free testing at public facilities.15 As a result, the incentive for aggressive testing and reporting faltered, and cases went under-reported.16 Under-reporting of COVID-19 cases has multitude of implications, including drawing fallacious disease burden and consequent complacency for management.
Nepal has also been suffering major natural disasters, such as the Gorkha earthquakes in 2015, where public health preparedness was deemed to be sub-optimal; and lessons from the previous disasters are often untranslated into policy and practice.17–19 Possible infectious disease outbreaks of epidemic and pandemic potential always remain major threats in Nepal.7 For example, there have been sporadic cholera outbreaks in Nepal with the earliest reported epidemic that dates back to 1823.20 Nonetheless, the health system preparedness in Nepal toward such infectious disease outbreaks is deemed to be suboptimal due to absence of robust surveillance system, diagnosis and management infrastructure.20 In light of these potential threats, it is critical for the health system of Nepal to learn and use the lessons from current pandemic for the future. The main objective of this study was to explore the characteristics and factors that affected Nepal’s health system preparedness for COVID-19 and its impact on HCWs.
Methods
Study Design
This was a qualitative study with Nepali frontline HCWs and policy-makers and follows a standard consolidated criteria for reporting qualitative studies (COREQ) guideline (see the Online Supplementary Appendix 1).21 To address the research question in this study, a phenomenological approach was used to explore the perspectives of frontline HCWs and policy-makers who were directly involved in the management of the current pandemic. The phenomenological approach allows to describe the phenomena of interest from people who are part of it or have a first-hand experience; refraining from any predesigned framework.22
Study Participants
The researchers (N.S., B.A., B.G., and S.B.M.) prepared the initial list of potential participants from their network and professional contacts. Our sampling approach was based on the basic tenet of qualitative research, where respondents are selected based on their involvement and experience about the phenomena of interest (purposive selection).23 Due to the initial burden of epidemic in Kathmandu (Bagmati province), majority of the respondents in this study were from Bagmati. Participants were contacted by email, social media, and phone. Participants from all the 7 provinces of Nepal, who were directly involved in the clinical (eg, HCWs) or nonclinical (eg, policy-makers) management of COVID-19 outbreak, were included in this study (Table 1). We interviewed 32 HCWs from tertiary health-care institutions and four policy-makers.
Table 1.
Socio-demographics of participants
| Characteristics | Categories | Frequency (%) |
|---|---|---|
| Age range | Continuous | 24 - 58 y |
| Gender | ||
| Male | 19 (50%) | |
| Female | 18 (50%) | |
| Provinces | ||
| Province-1 | 3 (8%) | |
| Province-2 | 4 (11%) | |
| Bagmati Province | 22 (61%) | |
| Gandaki Province | 3 (8%) | |
| Province-5 | 1 (3%) | |
| Karnali Province | 2 (6%) | |
| Sudurpaschim Province | 1 (3%) | |
| Occupation | ||
| Doctors | 17 (47%) | |
| Nurses | 15 (42%) | |
| Policy-makers | 4 (11%) | |
Data Collection and Interview Guide
Semi-structured interviews were conducted, between March 2020 and May 2020, remotely using telephone or Internet-based tools (Skype, Zoom, and Microsoft Teams). All interviews were audio-recorded. Respondents participated alone in the interviews from either their home or at a peaceful location near their office. Two female research assistants who were pursuing master’s degree in public health: S.B., and Nil.S. conducted the interviews. Before conducting interviews, they were trained in qualitative research by N.S. (MD, PhD), S.B.M. (PhD), and B.A. (MD, DPhil), respectively, with extensive experience and expertise in qualitative research. An interview guide, consisting of a list of relevant topics and corresponding open-ended questions, was developed based on the review of literature24–27 and input from the experts (Online Supporting Information Appendix 2). Authors of this study have diverse background (clinicians, public health experts, and social scientists) who reviewed and refined the topics for the interview guide. The findings in this study used authors’ reflection and interpretations drawing from their lived experience and is an established method in qualitative research.28–31 The interview guide was pilot tested among two potential respondents, one HCW, and policy-makers by N.S. and B.A., and was amended for clarity. The guide helped the interviewers to conduct the interview adhering to the research topics.
Respondents were approached for interviews based on their interest and convenience. Interviewers introduced themselves and briefed the respondents about the study (including study objectives and procedures, and potential benefits and harms in participation) with individual respondents before fixing the appointments. Participants willing to provide verbal consent to participate in the study and audio-record the interview were included in the study. After brief video-interactions with the respondents, the interviews were switched to audio only for quality recording. The interviews were conducted in the local (Nepali) language and lasted between 45 and 60 min. The interviewer also noted down the stresses made on the issues during the interview, which aided the data analysis.
None of the candidates refused to participate, and no repeat interviews were carried out. Based on the principles of “data saturation,” sample size for this study was deemed sufficient when no new data/themes emerged from further interviews.32
Data Analysis
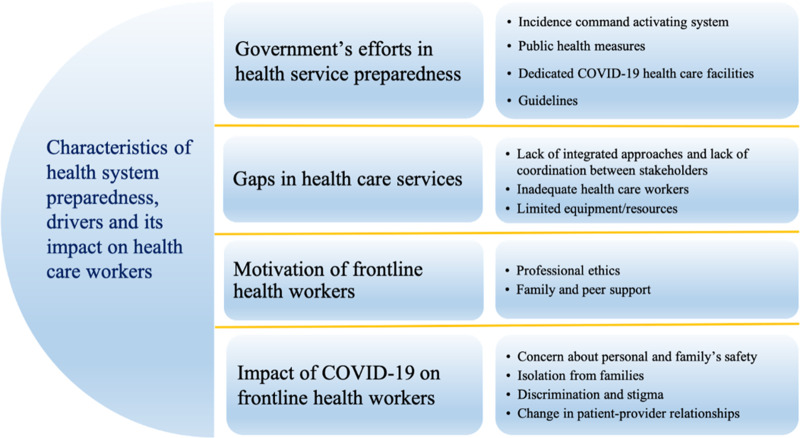
All interviews were transcribed and translated verbatim into English. Transcripts were assessed for accuracy by cross-checking with the audio-recordings. All data were coded line by line in qualitative data analysis software NVivo 12 (QSR International, Doncaster, Australia). The initial codebook was deductively developed based on the interview guide and was revised to include the emerging codes using the inductive approach.33,34 Final codes derived through a mix of deductive and inductive approach were cross-checked between two investigators (B.A. and N.S.). Specifically, four major themes (Figure 1) were derived deductively based on the interview guide/initial codebook while sub-themes corresponding to each of the major themes were derived inductively. Four major themes include:
Government’s efforts in health service preparedness
Gaps in health-care services
Motivation of frontline HCWs and
Impact of COVID-19 on frontline HCWs
Figure 1.
Health system preparedness to tackle the COVID-19 in Nepal: characteristics, drivers, and its impacts on HCWs.
Codes were also independently checked against the transcripts for accuracy. Consensus regarding the nature and coding of final themes was reached through regular team meetings during the data analysis. Regular debriefings were conducted within the study team to discuss the final themes and their interpretations by N.S. and B.A. Findings relevant to the research question are supported by direct quotes of the participants and are presented below.
Results
Characteristics of Participants
Among 36 respondents, 32 were HCWs (17 doctors and 15 nurses) from various tertiary health-care centers across Nepal and four were policy-makers (Table 1). The policy-makers worked in the Ministry of Health and Population at the federal level and the Ministry of Social Development at the provincial level. They were involved in devising or implementing COVID-19 management policies at the respective levels. Age of participants ranged from 24 to 58 years, and half of them were females.
Overview of Findings
Although the initial outbreak of COVID-19 in China and elsewhere, as well as its own first confirmed case back in January, provided Nepal with adequate time and opportunity for preparedness, the government of Nepal and health policy-makers did not seem to anticipate the scale of the pandemic in terms of resources and management it required (Figure 1). Few preparedness measures included initiation of Incidence Command Activating System for COVID-19 as a health emergency; implementation of complete lockdown; establishment of COVID-19 dedicated health-care facilities; and preparation of protocols and guidelines for the prevention and management of COVID-19. Nonetheless, the preparedness was deemed futile due to significant gaps that included: 1. lack of integrated approaches and coordination (between a. federal, provincial, and local level; and b. public and private health-care facilities) for management of COVID-19; 2. inadequate number of frontline HCWs; and 3. constraints in equipment/resources, such as space, PPE, and facilities. Despite these constraints, HCWs seem to be incentivized by their professional ethics and support from their family and peers. While health system constraints already jeopardized HCWs’ functionality and motivation, they were further debilitated by the impacts at the personal front with concerns over their own and family’s safety, living isolated from families, perceived discrimination, and stigma from their community. Also, HCWs expressed concerns about the changes in their clinical practice, particularly virtual consultations and application of “don’t touch” measures during clinical examination. Recommendations from HCWs echoed around the need for additional resources for adequate patient management (PPE, human resources, equipment, and infrastructure for isolation and treatment of cases) and additional incentives and security of HCWs. Below we describe each of the components of health system preparedness and its impacts on HCWs.
A. Government’s Efforts in Health Service Preparedness for COVID-19
Initiation of the Incidence Command Activating System
Nepal’s Ministry of Health and Population initiated the Incidence Command Activating System early during the epidemic for a coordinated response against COVID-19 as a health emergency. However, a policy-maker at the federal government acknowledged that there were lapses during the initial phase of crisis management, mainly due to their own inexperience in handling such emergencies.
We do not have any past experience of handling this type of pandemic, so we were not organized in our approaches during January and February. However, starting in March, we have tried our best to be more organized and more systematic using a one-door policy.
(Policy-maker, male, federal government)
Public Health Measures - Social Distancing and Lockdown
The Government of Nepal imposed strict lockdown across the country, cancelled all domestic and international flights, and sealed the open border with India. Despite these measures, there were large influxes of migrant workers through the porous borders. In response, the provincial governments took additional steps by large-scale testing in border districts and deploying border security forces to prevent such influx.
We have been doing testing on a large scale in bordering districts…There is suspicion that some people might have entered Nepal through ‘illegal’ routes
(Policy-maker, male, Province 1)
We have epidemiology division in ministry of health, but they seem to be lost in times of pandemic like this. It’s good that Nepal Government has announced nationwide lockdown and people stay inside. I haven’t seen any other measures being imposed strictly.
(Doctor, male, tertiary hospital, Kathmandu)
Although the policy-makers frequently emphasized the blanket “lockdown” as the government’s major intervention strategy, they less frequently acknowledged the role of population awareness on social distancing and hygiene measures in reducing transmission.
Dedicated COVID-19 Health-Care Facilities
In response to the COVID-19 emergency, the government mapped out all the public hospitals and then categorized them into 3 levels based on their capacity and infrastructures and designated their responsibility.
We have mapped out how many hospitals we have in the nation, their locations, their bed capacity. Secondly, we categorized hospitals in three different categories. We have chosen COVID clinic hospitals and further divided them into three levels: Level 1, Level 2, and Level 3. We have defined the responsibilities of each level of the hospital. While Level 1 hospitals are responsible for managing mild cases of positive COVID cases, Level 2 hospitals are responsible for severe cases where ICUs and ventilators are needed. Level 3 hospitals are responsible for managing the severe cases of COVID with other comorbidities.
(Policy-maker, male, federal government)
The reason behind this categorization of hospitals was reported to prevent and control the overwhelming and unsystematic attendance at hospitals. Nonetheless, none of the policy-makers appreciated the potential transmission of diseases to other patients who may be simply attending the hospital for regular visits or other diseases.
A few policy-makers also shared the government’s plan to expand the resources by partnering with private health-care facilities.
We have set up COVID-19 dedicated hospitals for the increasing number of coronavirus cases. If this is not sufficient, we will use the infrastructure of medical colleges and private facilities in our province for the management of coronavirus patients.
(Policy-maker, male, Gandaki Province)
We have 10 ICU beds in the corona dedicated hospital. We will use ICU beds of medical colleges in case an epidemic breaks out.
(Policy-maker, male, Province 1)
Guidelines for the Management of Suspected COVID-19 Cases
As a part of the preparedness and to ensure the uniformity in the management of COVID-19 cases, Nepal’s health ministry drafted and disseminated the guidelines for clinical and public health management of COVID-19. Policy-makers were vocal about the various guidelines developed and distributed, however, fewer concerns were expressed toward the effective implementation of these protocols.
The government of Nepal has prepared a dozen guidelines for the COVID-19 management, which includes prevention, treatment and control measures, management of quarantine and isolation, and proper use of PPEs. We have shared these guidelines to all our health workers. We regularly conduct meetings using videoconferencing to disseminate information and updates on the situation related to the COVID-19, and best practices followed in the region.
(Policy-maker, male, Gandaki Province)
Although, such preparedness was appreciated by the HCWs, but they accentuated the looming constraints and gaps within the health system that could hinder effective implementation of these guidelines.
B. Gaps in Health-Care/Services Preparedness
Lack of Integrated Approaches and Coordination Among Three Tiers of the Public Health System and Between Public and Private Health-Care Facilities
Among several gaps highlighted by the HCWs, an important gap was the overarching mechanism of functioning in the new federal health system where the coordination between the three tiers of the governmental health system (ie, federal, provincial and local) was “poor,” and the local and provincial healthcare facilities lacked adequate resources to operate effectively and independently. In addition to these operational constraints, lack of trained human resources, also added to the poor management.
There are three tiers of government performing their responsibilities; however, in a situation like now, there is no integrated approach taken. They have different strategies, and I do not think the coordination is quite good as just one level being good is not enough in this situation.
(Doctor, male, tertiary hospital, Kathmandu)
The government staffs are not sufficient; we need participation from the private sector as well. We should move forward, making one team, which is lacking in the current state.
(Doctor, male, tertiary hospital, Kathmandu)
Lack of coordination between the three tiers of government was also strongly echoed by the policy-makers at the provincial level who challenged the current federal system comparing it with the previous integrated system where coordination was more efficient. Against the backdrop of tenet underpinning the devolvement of responsibilities to provincial and local government for the management of current pandemic, policy-makers seem to revive the previous coordination mechanism through personal contacts and communication with the federal government.
……………… It was difficult because, in this federal setup, there is a lack of system anchoring these three tiers of government in health. We relied on our personal relations to navigate the issues of governance. The health of the population should be the responsibility of the central government in this type of epidemic. The health system before the federal setup would have worked more efficiently in this type of epidemic……………….
(Policy-maker, Male, Province 1 Government)
In addition to the inefficient coordination between the three tiers of government, lack of engagement and partnership with private hospitals seemed to be overlooked aspects of the current management of COVID-19 pandemic. The current approach of the government in preparing public health-care facilities alone also seemed to de-functionalize private health-care facilities’ potential capacity and contribution to COVID-19 management. Among several ramifications of obviating the partnerships with private hospitals, high referrals to public health facilities were one of the prominent concerns. In addition, lack of partnerships and delegation to private hospitals have rendered them a paradoxical complacency to defer patients and stay away from the responsibilities to the extent that patients who could be suffering from non-COVID-19 related conditions were simply deferred instead of establishing the diagnosis and providing treatment.
Private hospitals are referring excessively… all cases of fever….you know, [fever] it could be a symptom of 100 other diseases, to our government hospital. Patients are having difficulty in finding immediate service for their ailments. Elderly people without respiratory symptoms, without fever are also finding difficulty in receiving treatment for suspicion of COVID.
(Staff nurse, female, public hospital, Gandaki Province)
Inadequate Number of Frontline HCWs
HCWs endure a dire situation in Nepal, mostly in terms of their vulnerability in finding jobs and appropriate salary. For the current pandemic, the government of Nepal announced short-term (for three months) vacancies, but lack of a single applicant suggests it to be unpopular for most of the clinicians. Historically, Nepal’s health system has faced a shortage of human resources, and permanent positions for doctors and nurses remain unfulfilled. HCWs expressed their dissatisfaction toward health system policy toward HCWs. Aversion among HCWs for government-sponsored jobs, especially during this health crisis, may aggravate the outbreak.
No, the numbers of doctors we have are all working, and if one of them gets infected, we don’t have a substitute. The government also has not been able to add human resources. In the present context, the government has announced a vacancy for three months that almost implies ‘use and throw.’ So, if the government is serious about fighting the situation [current pandemic], ……should hire doctors permanently.
(Medical officer, male, tertiary hospital, Kathmandu)
Limited Equipment/Resources (Space, Equipment, and Facilities)
HCWs expressed grave concerns toward the limited resources such as the numbers of isolation and treatment beds, ICUs and ventilators, and PPEs. Importantly, the existing paucity of infrastructure and equipment was reported to be accentuated during the crisis. Lack of adequate capacity for lab testing and contact tracing were major concerns. The challenges were more prominent in the peripheral regions of the country.
The preparedness of health facilities is not up to the mark even at normal times. …We do not have enough ventilators, even for normal times in our country. The ventilators that we have is not enough for patients with other conditions. We cannot deny ventilators for those patients and use them to treat COVID patients.…. And more importantly, there are no adequate PPEs for clinicians….also, the question remains who should get PPE. What about sweepers and housekeepers? I am also not confident about the current laboratory capacity to meet the tests. The central lab already struggles to meet the test-demands, what about outside Kathmandu?
(Resident doctor, male, tertiary hospital, Kathmandu)
This is a district hospital and we only provide basic health services. We do not have adequate PPEs, medicines, ICUs, and ventilators. We have to refer serious patients to higher facilities which is very far.
(Staff nurse, female, district hospital, Province 1)
In terms of availability of resources, there were a few disconnects and dissonance between HCWs and policy-makers. The policy-makers conceded limited infrastructure to deal with the current crisis but assured that the government is trying its best to procure the necessary equipment.
Although our frontline health workers are well-prepared to deal with COVID-19 cases, there are several logistical challenges at the same time. I must admit that there are not enough PPEs, ventilators, N95 masks, cardiac monitors, and ICU beds in our province.
(Policy-maker, male, Gandaki Province)
C. Motivation of Frontline Health Workers
Professional Ethics
Amid the context of deprived safeguards (such as PPE) for HCWs, their high motivation to work were perceived to be emanating from professional ethics. Also, HCWs believed that their responsibility was irreplaceable and felt a moral obligation to serve the patients.
We are nurses by profession. We have joined this profession to serve ill people. If we do not take care of sick, who else is there to take their care? So, our nursing ethics has motivated us to keep working.
(Staff nurse, female, provincial hospital, Province 2)
I chose a career in health sector knowing I will come in contact with highly infectious disease and there is always possibility I might get infected. So, in situation like this if doctors like me don’t work at frontline then who else will do?
(Medical officer, male, tertiary hospital, Kathmandu)
Global Appreciation of HCWs, Family, and Peer Support
Frontline HCWs also mentioned how they were motivated to work referring to the global appreciation for their work during the pandemic. HCWs also compared their work during the pandemic akin with a frontline warrior during disasters. In addition, the respect and appreciation they garnered from their family and peers who knew their profession and appointment at hospitals also motivated them to work.
It is our duty as healthcare providers. Health workers have been called ‘frontline warriors’……. during this pandemic. We are mainly motivated by the exemplary work of paramedics, nurses, and doctors in other countries, as seen on various social media. In fact, peers and family members know where we work, their constant encouragement, and respect for our work, and more so during this time also drives me to work.
(Resident doctor, male, tertiary hospital, Kathmandu)
Despite their high motivation, few HCWs were concerned about the disproportionate burden assigned at work, particularly referring to how seniors and consultants burdened the responsibilities (of patient care) to juniors.
D. Impact of COVID-19 on Frontline HCWs
Concerns About Personal and Family Safety
HCWs reported heightened fear of contracting COVID-19 while attending patients, particularly because of its high infectivity and burgeoning reports of infections and deaths among the frontline HCWs globally. In addition, the potential to transmit the disease to their family members further aggravated their anxiety.
It has impacted my mental health. We hear the news about how COVID-19 is spreading worldwide, and how health workers are contracting the infection, and there is the fear of transmitting to our families if we unknowingly contract the infection.
(Resident doctor, male, tertiary hospital, Kathmandu)
Additionally, the unavailability of PPE was often referred to as the chief stressor in the workplace. Lack of PPE was a serious concern to an extent that they built their makeshift PPEs despite having doubts about its effectiveness. Contrary to the standard protocols for preventing cross-infection that mandate changing into a new set of PPEs before handling another patient/suspected case, many HCWs reported using the same PPE throughout the day while attending different patients due to the shortages.
We haven’t seen how standard PPE looks like. We have PPE made by the hospital that includes plastic gowns, surgical mask, surgical cap, there are no N-95 masks and shoe covers. We are using locally made ones just for the sake of our satisfaction….and we don’t know if it can offer us protection.
(Resident doctor, female, tertiary hospital, Kathmandu)
Isolation From Families
Frontline HCWs feared that they could inadvertently infect their family members. Few HCWs, particularly breastfeeding mothers and those with small kids, were despaired of how they had to restrain themselves from approaching their family members when returning from work.
I have a small child. After returning from [hospital] duty, I cannot go straight away to my child…….
(Staff nurse, female, tertiary hospital, Kathmandu)
Frontline HCWs working at COVID-19 designated health facilities were mandated to live in temporary hostels and could return home only after 14 days of self-isolation, following the last exposure with a COVID-19 patient. If and when these HCWs saw suspected patients more frequently, their quarantine could perpetuate abstaining from visiting their family members.
Our Province 1 government has set up a quarantine hostel for those frontline health workers working in these dedicated hospitals.
(Policy-maker, male, Province 1)
Discrimination and Stigma
HCWs, living in rented dwellings, faced discrimination from their landlords. They were verbally abused, labeled as “disease carriers,” and even asked to vacate the rental unit. Fear of bringing virus from the hospital, infecting the household members, and contaminating the whole property were some of the reasons for such discriminatory acts. Although, the Ministry of Health and Population issued counter orders to stop such discrimination, HCWs continued to struggle against the stigma and discrimination from the community.
My friend lives in a rented room near the hospital. One day after finishing her duty, when she returned to her room, the house owner started washing the gate and the door carpet with soap and water and sprayed some religious powder on the entrance.
(Resident doctor, female, tertiary hospital, Kathmandu)
I live in a rented room, but recently I was asked not to come to my room after working in the hospital all day.
(Medical officer, male, tertiary hospital, Kathmandu)
Change in Patient-Provider Relationships
HCWs have adopted new methods of clinical interactions where their traditional way of examining patients has been challenged due to COVID-19. For instance, the “don’t touch practice” entailed minimizing the physical interactions with patients, which essentially meant that HCWs would have to compromise the proper clinical examination. Such a practice not just discouraged in-person consultations, patients, particularly when febrile, had to visit multiple hospitals for health care.
We are avoiding examination and providing only symptomatic treatment to patients [with fever], and this can affect patients and physicians as well….they [patients] may have to visit other hospitals.
(Doctor, male, tertiary hospital, Kathmandu)
E. Recommendations
The majority of the HCWs and policy-makers stressed that the government needs to ensure adequate stock of PPE and isolation beds. They also emphasized that HCWs must be incentivized and motivated.
Ensuring adequate stock and supply of PPE and other medical equipment, appropriate management of isolation wards, training for frontline health workers, incentives and health insurance of health workers to keep them motivated are some of my recommendations.
(Medical officer, tertiary hospital, Kathmandu)
All participants resonated that the government needs to learn from the current crisis and strengthen the health system to fight effectively against such crises in the future. A HCW also cued toward a chronic problem of failing to learn from the past failures and high acceptance of such a tendency.
We have learnt a huge lesson from this pandemic. The basic step of prevention, which we did not follow properly, has become a routine by now.
(Resident doctor, male, tertiary hospital, Kathmandu)
People, including the political leaders have this newfound awareness about the important [importance] of health and public health efforts. People know that we need to spend on health care infrastructure like ICUs and ventilators, and infection prevention efforts.
(Policy-maker, male, Central Government)
Discussion
Summary of Findings and Current Preparedness
This study illustrated the characteristics of COVID-19 preparedness during the early phase of outbreak in Nepal and explored the impact on HCWs. Although Nepal had adequate time and opportunities for pre-emptive preparedness, the poor anticipation and inadequate preparedness delayed the building of necessary infrastructure, responsibility distribution, and resource allocation. Although activation of Incident Command System, expansion of testing capacities to provincial level, establishment of new centers dedicated for COVID-19 treatment, development of guidelines and protocols, and early implementation of lockdown were identified as important developments, these were conceded to be futile by both policy-makers and frontline HCWs as this preparedness gradually faltered, mostly due to poor systemic coordination among three tiers of governments, poor implementation, and inadequate attention toward expanding testing and treatment capacity. Despite the myriad of challenges of inadequate resources and incentives, discrimination from communities, and isolation from families, HCWs seem to be intrinsically motivated to serve at the frontline. The findings from this study bear urgent implications for health system preparedness toward evolving COVID-19 and potential future disasters in Nepal and other similar settings.
Gaps in Health-Care/Services Preparedness
One of the overarching problems affecting preparedness and response in Nepal was the gaps in coordination among federal, provincial, and local level health system under the federal governance structure.4 This implied a lack of clarity on responsibility division, poor logistic supply chain management, and challenges in skilled human resources at the provincial and local level. While the capacity of public hospitals to provide optimal services to the denominator population before the COVID-19 pandemic was already limited by the lack of resources,4 the government’s failure to engage with the private health sector as well as the nonhealth sector during this crisis seemed even more detrimental. Private health infrastructure in Nepal constitutes a large landscape in Nepal’s health system; thus, engaging and using their space and resources could significantly palliate the burden of public healthcare infrastructure.35,36 Additionally, other available infrastructure could also be temporarily repurposed for COVID-19. Specifically, sharing and devolving testing and tracing, space for quarantine, isolation beds, and intensive care could have been negotiated for the current crisis. For example, Ecuador’s Government collaborated with SENSEable City Laboratory and repurposed shipping containers into temporary makeshift intensive care units.37 In India, government transformed and used the 5231 railway coaches into COVID care centers that spanned across a vast network across the country.38
Health workforce shortages have been a chronic yet constantly overlooked problem in Nepal.5 Nepal has 0.17 doctors and 0.5 nurses per 1000/population, which is well below the WHO’s minimum benchmark of 2.3 doctors, nurses, and midwives per 1000/population.39 This study highlighted how the background deficit in HCWs suddenly appeared as a major foreground hindering the preparedness during the current pandemic. This was further evident from the fact that the short-term vacancies for doctors went unfulfilled and were considered to be exploitative (“use and throw”). Such measures are likely to compound current and future retention of HCWs and their interest in truly serving in public hospitals.
Frontline HCWs in this study who expressed high motivation to serve during such a crisis, however, expressed fear and anxiety largely because of the lack of adequate safety gears, particularly the PPEs. The use of improvised surrogate-PPE out of rain coats, scarfs, and visors made from transparent sheaths connoted vulnerability of frontline HCWs in Nepal.40 While the government of Nepal is quite cognizant about the shortage of health human resources, failure to appreciate it at the budgetary announcement for the current fiscal year 2020/21 has been despairing. The budget has continued to ignore the need for human health resources, professional supervision, and better opportunities for specialized training. Nonetheless, allocating budget for establishing 50-bed hospitals in each province and 300-bed hospitals at the federal level for management of infectious disease outbreaks are appreciable.41
Motivation of the Frontline HCWs and Impact of COVID-19 on Frontline HCWs
HCWs in Nepal have shown a great deal of resilience despite more than a third had anxiety and depression during the current COVID pandemic.42 HCWs identified professional ethics, global appreciation of HCWs’ contribution to the pandemic and importantly, family members and peers’ support and encouragement as major motivating factors for serving patients, even without proper infrastructure and PPE. A previous study from Nepal has also highlighted how the individual determination, a sense of responsibility to the community, and professional duty among HCWs were motivating factors to serve during the crisis.43 Also, HCWs’ sacrifices in terms of how they maintain social distance with their family members, particularly in Kathmandu, where they cram in a rented room/apartment is difficult to imagine and can have psychological and social impact.44 Nonetheless, unfortunately, HCWs in Nepal suffer from a multitude of problems at various levels. While the acts of discrimination toward HCWs from their landlords are quite specific to the current pandemic and has been associated with the fear of infection and transmission, the sporadic incidents of verbal and physical abuse at the health-care institutions even during the nonpandemic context has been horrendous.45 Such discriminatory practices can lead to low self-esteem, stress, and anxiety among HCWs, as shown by studies elsewhere.46
One notable outcome that HCWs seem to express was the new normal in their clinical practice as the way they had to adjust to “don’t touch” practice. Although physical examination and thorough investigation are part of the standard clinical practice, lack of PPE, safety concerns, and subsequent fear of contracting COVID-19 looked discerning. Compounded with lack of sufficient awareness about the disease and importance of distancing, patients may perceive increased social distance with the HCWs as act of malpractice. Crushed between these extremes, HCWs, unfortunately can face the predicament of whether to conduct physical examination (without PPE) or face the allegations of malpractice, which could potentially invite patients’ potential resentment, disappointments, and violence.
Strengths and Limitations
This is to our knowledge the first study to explore the preparedness of Nepal’s health system during COVID-19 pandemic, factors affecting it, and its impact on frontline HCWs. This study used remote interview methods using telephone or Internet-based tools, which may have missed nuances and subtle expressions characteristics of the face-to-face interview. Nonetheless, this remote interview method enabled us to approach and include a diverse range of participants from different geographic locations within Nepal. The sample composition was uneven, with disproportional participation of HCWs from Bagmati province that may have skewed our findings. However, attempts to capture the voice of HCWs from all the provinces were made and the interviews were conducted until theoretical saturation of shared experiences of participants across the country. Other frontline workers, such as dental, public health professionals, laboratory persons, ambulance drivers, and housekeeping staff at the hospital were not interviewed and was beyond the scope of this study. The study was conducted early during the outbreak of COVID-19 in Nepal when little was known about the disease. With the evolution of the knowledge about the virus and the disease, awareness, challenges, priorities, and response strategies of health system has changed over time. The findings presented should be interpreted based on the context of early phase of outbreak in Nepal.
Conclusion
One of the prominent lessons learned from the COVID-19 pandemic that could be relevant for Nepal and elsewhere is to have pre-emptive and adequate preparedness early on. Although a few preparedness measures were implemented in Nepal, such as the designation of COVID-19 specific hospitals and lockdown, the maintenance and sustainability of these measures were not forethought. The identified gaps in Nepal’s health service preparedness against COVID-19 identified in this study emerged from (a) systemic lack of coordination between the governance system and (b) a severe shortage of resources (human and nonhuman), to tackle the pandemic at all levels. Specifically, the lack of human resources, inadequate logistic chain management and laboratory facilities for testing COVID-19 appeared to have jeopardized the health system preparedness and escalated the pandemic in Nepal. Despite health and safety concerns, HCWs have shown a great deal of resilience and motivation to serve to their capacities.
Acknowledgments
We are deeply grateful to all the respondents of this study who have been relentlessly contributing their efforts to curb the pandemic at various capacities.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/dmp.2021.204.
click here to view supplementary material
Data availability statement
Data cannot be shared publicly because of the nature of qualitative data; it contains personal quotes and clues that may potentially lead to participants’ identification. However, in compliance with the data access policy outlined by the Institutional Review Committee of Manmohan Memorial Institute of Health Sciences (https://www.mmihs.edu.np/irc.php), data are available upon reasonable request to the chair of the research department (e-mail: drdharmakhanal@gmail.com).
Conflict of interest
The authors declare that they have no competing interests.
Ethical standards
The Institutional Review Board (IRB) at Manmohan Memorial Institute of Health Sciences (MMIHS), Kathmandu, Nepal (Registration number: 76/133) approved the study. All participants were briefed about the study objectives and procedures, and of potential benefits and harms in participation. Participants were informed of voluntary participation and their rights to withdraw from the interview at any point or to refuse to answer any questions. Because of the COVID-19 pandemic, verbal consent was deemed appropriate for the interviews by the IRB of MMIHS. Participants who provided verbal consent and permission to audio-record the interview were included in the study. Data were de-identified, and any identifying contents were replaced with specific codes throughout the transcription process to ensure participants’ anonymity and confidentiality.
References
- 1.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Worldometer. COVID-19 coronavirus pandemic. 2020. https://www.worldometers.info/coronavirus/#countries. Accessed July 4, 2020.
- 3.Bastola A, Sah R, Rodriguez-Morales AJ, et al. The first 2019 novel coronavirus case in Nepal. Lancet Infect Dis. 2020;20(3):279-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghimire U, Shrestha N, Adhikari B, et al. Health system’s readiness to provide cardiovascular, diabetes and chronic respiratory disease related services in Nepal: analysis using 2015 health facility survey. BMC Public Health. 2020;20(1):1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adhikari B, Mishra SR.Urgent need for reform in Nepal’s medical education. Lancet. 2016;388(10061):2739-2740. [DOI] [PubMed] [Google Scholar]
- 6.Mishra SR, Khanal P, Karki DK, et al. National health insurance policy in Nepal: challenges for implementation. Glob Health Action. 2015;8:28763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pokharel S, Raut S, Rijal KR, et al. Coronavirus disease 2019 pandemic - public health preparedness in Nepal and one health approach. Disaster Med Public Health Prep. 2020. May 29:1-2. [DOI] [PMC free article] [PubMed]
- 8.Ministry of Health and Population Nepal. Situation report COVID-19 #109 (as of 28 May 2020). 2020. https://heoc.mohp.gov.np/update-on-novel-corona-virus-covid-19/. Accessed June 29, 2021.
- 9.Ministry of Health and Population Nepal. COVID-19 Update. 2020. https://covid19.mohp.gov.np/#/. Accessed June 13, 2020.
- 10.Nepali Times. Protecting those who protect us from the epidemic. 2020. https://www.nepalitimes.com/here-now/protecting-those-who-protect-us-from-the-epidemic/. Accessed March 28, 2020.
- 11.Rayamajhee B, Pokhrel A, Syangtan G, et al. How well the government of Nepal is responding to COVID-19? An experience from a resource-limited country to confront unprecedented pandemic. Front Public Health. 2021;9:597808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Basnyat B. How Nepal can survive 2nd covid wave. Nepali Times. 2021. https://www.nepalitimes.com/opinion/how-nepal-can-survive-2nd-covid-wave/. Accessed May 18, 2021.
- 13.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bahadur BCU, Pokharel S, Munikar S, Wagle CN, et al. Anxiety and depression among people living in quarantine centers during COVID-19 pandemic: a mixed method study from western Nepal. medRxiv. 2020.11.05.20224436. doi: 10.1101/2020.11.05.20224436 [DOI] [PMC free article] [PubMed]
- 15.Awale S. Why Nepal’s Covid-19 figures are deceptive. Nepali Times. 2020. https://www.nepalitimes.com/here-now/why-nepals-covid-19-figures-are-deceptive/. Accessed December 28, 2020.
- 16.The Himalayan Times. Nepal Government not to bear costs of Covid-19 test, treatment. 2020. https://www.hindustantimes.com/world-news/nepal-government-not-to-bear-costs-of-covid-19-test-treatment/story-RwN56cSag0QVn7n9Fh1E0M.html. Accessed December 28, 2020.
- 17.Adhikari B, Ozaki A, Marahatta SB, et al. Earthquake rebuilding and response to COVID-19 in Nepal, a country nestled in multiple crises. J Glob Health. 2020;10(2):020367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mishra SR, Adhikari B.Planetary health in Nepal’s post-earthquake rebuilding agenda: progress and future directions. Lancet Planet Health. 2019;3(2):e55-e56. [DOI] [PubMed] [Google Scholar]
- 19.Adhikari B, Mishra SR, Babu Marahatta S, et al. Earthquakes, fuel crisis, power outages, and health care in Nepal: implications for the future. Disaster Med Public Health Prep. 2017;11(5):625-632. [DOI] [PubMed] [Google Scholar]
- 20.Rhee C, Gupta B, Lal B, et al. Mapping the high burden areas of cholera in Nepal for potential use of oral cholera vaccine: an analysis of data from publications and routine surveillance systems. Asian Pac J Trop Med. 2020;13:107. [Google Scholar]
- 21.Tong A, Sainsbury P, Craig J.Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349-357. [DOI] [PubMed] [Google Scholar]
- 22.Groenewald T.A phenomenological research design illustrated. Int J Qual Methods. 2004;3(1):42-55. [Google Scholar]
- 23.Sargeant J.Qualitative research part II: Participants, analysis, and quality assurance. J Grad Med Educ. 2012;4(1):1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu Q, Luo D, Haase JE, et al. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob Health. 2020;8(6):e790-e798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McMahon SA, Ho LS, Brown H, et al. Healthcare providers on the frontlines: a qualitative investigation of the social and emotional impact of delivering health services during Sierra Leone’s Ebola epidemic. Health Policy Plan. 2016;31(9):1232-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Raven J, Wurie H, Witter S.Health workers’ experiences of coping with the Ebola epidemic in Sierra Leone’s health system: a qualitative study. BMC Health Serv Res. 2018;18(1):251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Singh DR, Sunuwar DR, Shah SK, et al. Impact of COVID-19 on health services utilization in Province-2 of Nepal: a qualitative study among community members and stakeholders. BMC Health Serv Res. 2021;21(1):174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abimbola S, Pai M.Will global health survive its decolonisation? Lancet. 2020;396(10263):1627-1628. [DOI] [PubMed] [Google Scholar]
- 29.Khan M, Abimbola S, Aloudat T, et al. Decolonising global health in 2021: a roadmap to move from rhetoric to reform. BMJ Glob Health. 2021;6(3):e005604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Adhikari B, Pokharel S, Raut S, et al. Why do people purchase antibiotics over-the-counter? A qualitative study with patients, clinicians and dispensers in central, eastern and western Nepal. BMJ Global Health. 2021;6(5):e005829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Adhikari B, Mishra SR, Dirks KN.Green space, health, and wellbeing: considerations for South Asia. Lancet Planet Health. 2020;4(4):e135-e136. [DOI] [PubMed] [Google Scholar]
- 32.Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893-1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Crabtree B, Miller W.A template approach to text analysis: developing and using codebooks. In Crabtree BF, Miller WL, eds. Doing Qualitative Research in Primary Care: Multiple Strategies. Newbury Park, CA: Sage Publications; 1992:93-109. [Google Scholar]
- 34.Fereday J, Muir-Cochrane E.Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. 2006;5(1):80-92. [Google Scholar]
- 35.Acharya S, Ghimire S, Jeffers EM, et al. Health care utilization and health care expenditure of nepali older adults. Front Public Health. 2019;7:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Singh DR, Sunuwar DR, Adhikari B, et al. The perils of COVID-19 in Nepal: implications for population health and nutritional status. J Glob Health. 2020;10(1):010378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Bank Group. Global responses to COVID-19 in slums and cities. 2020. http://pubdocs.worldbank.org/en/359311591302725959/June1-Response-to-COVID-in-Slums-and-cities.pdf. Accesed June 15, 2020.
- 38.Patel CK, Selvam VK, Sahu DK.Railway anaesthesiologists and Indian railway COVID-19 management system. Indian J Anaesth. 2020;64(Suppl 2):S132-S135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ministry of Health and Population Nepal. Human resources for health Nepal country profile. 2013. https://bit.ly/2YxdZl3. Accessed June 13, 2020.
- 40.Shrestha GS.COVID-19 pandemic: shortage of personal protective equipment, use of improvised surrogates, and the safety of health care workers. J Nepal Health Res Counc. 2020;18(1):150. [DOI] [PubMed] [Google Scholar]
- 41.The Kathmandu Post. Nepal’s budget: not quite all there. 2020. https://kathmandupost.com/editorial/2020/05/28/nepal-s-budget-not-quite-all-there. Accessed June 13, 2020.
- 42.Khanal P, Devkota N, Dahal M, et al. Mental health status among health workers in Nepal during COVID-19 pandemic (Policy brief). Pulic Health Update. 2020. https://bit.ly/3dYiSdr. Accessed June 13, 2020.
- 43.Raven J, Baral S, Wurie H, et al. What adaptation to research is needed following crises: a comparative, qualitative study of the health workforce in Sierra Leone and Nepal. Health Res Policy Syst. 2018;16(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.The Kathmandu Post. Health workers deployed at Covid-19 frontline deprived of their allowances. 2020. https://kathmandupost.com/national/2020/06/07/health-workers-deployed-at-covid-19-frontline-deprived-of-their-allowances. Accessed June 13, 2020.
- 45.My República. Doctors ‘manhandled’ at Nepal Medical College. 2020. https://bit.ly/2XZpnXO. Accessed June 13, 2020.
- 46.Lanctôt N, Guay S.The aftermath of workplace violence among healthcare workers: a systematic literature review of the consequences. Aggress Violent Behav. 2014;19(5):492-501. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/dmp.2021.204.
click here to view supplementary material
Data Availability Statement
Data cannot be shared publicly because of the nature of qualitative data; it contains personal quotes and clues that may potentially lead to participants’ identification. However, in compliance with the data access policy outlined by the Institutional Review Committee of Manmohan Memorial Institute of Health Sciences (https://www.mmihs.edu.np/irc.php), data are available upon reasonable request to the chair of the research department (e-mail: drdharmakhanal@gmail.com).