Abstract
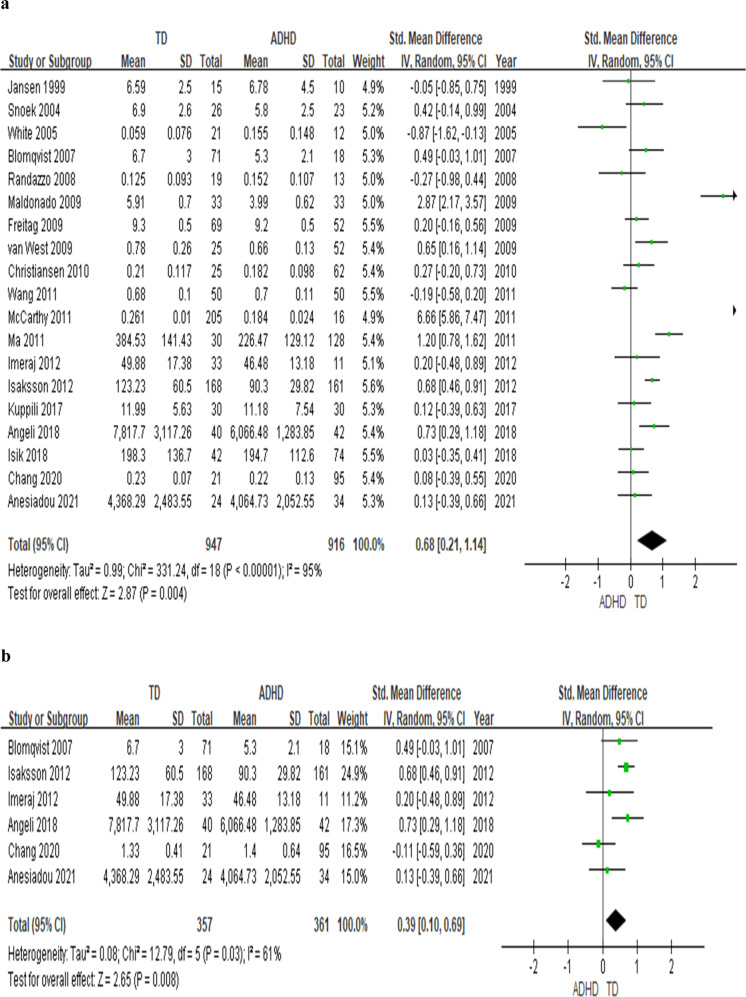
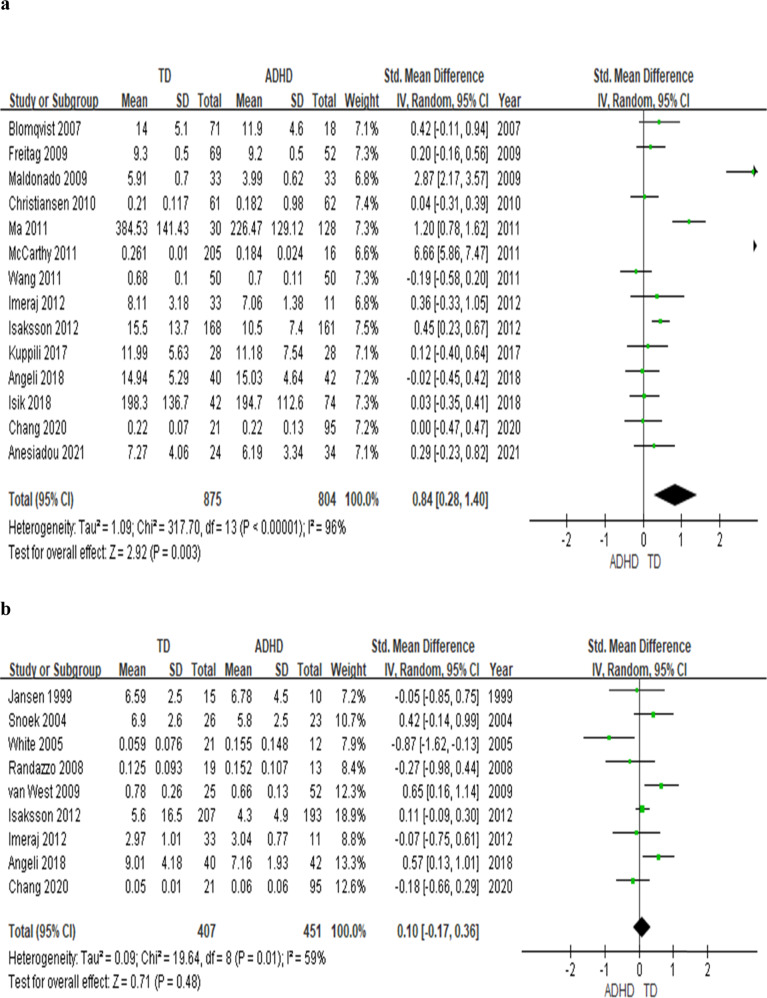
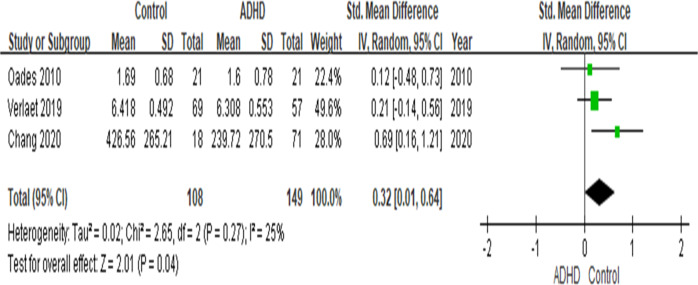
Several studies reported abnormal cortisol and inflammatory biomarker levels in youths with attention deficit hyperactivity disorder (ADHD), but the results have not been conclusive. We conducted a systematic review followed by a meta-analysis of case-control studies assessing blood or saliva cortisol levels and blood levels of inflammatory biomarkers in youth with ADHD. The effect sizes (ES) were synthesized by using a random-effects model. In the 19 studies on cortisol levels (totaling n = 916 youth with ADHD and n = 947 typically developing (TD), healthy youth), youth with ADHD have lower basal cortisol levels at any time-points during the day (effect size: .68; p = 0.004) and lower cumulative levels of cortisol (ES: .39, p = .008) throughout the day than TD youth. Moreover, morning cortisol levels were lower in ADHD youth when compared with TD youth (14 studies, n = 1679, ES: .84, p = 0.003), while there is no difference for the afternoon cortisol levels (p = 0.48). The meta-analysis on inflammation biomarker was conducted on 4 studies (totaling n = 404 youth) showed that Tumour Necrosis Factor-alpha (TNF-α) was lower in ADHD when compared with TD (3 studies, n = 257 youth, p = 0.004), while no differences for Interleukin-1β(IL-1β) (p = 0.21), IL-6 (p = 0.09) and IL-10 (p = 0.77). The lower cortisol in the context of low TNF-α levels may indicate a specific pattern of biomarkers in ADHD, and further investigation is warranted.
Subject terms: Neuroscience, Physiology
Introduction
Hypothalamus-Pituitary-Adrenal (HPA) axis dysfunction and inflammation have been suggested to contribute to the development of attention deficit hyperactivity disorder (ADHD). Steingard et al. were the first to describe abnormalities of the HPA axis in children with ADHD, as they described a higher rate of dexamethasone non suppression in children with ADHD when compared with controls (22.7% vs. 0%) [1]. Subsequently, Kaneko et al. [2]. found that only around 40% of children with ADHD had normal diurnal cortisol rhythm, defined as a diurnal cortisol variation showing a maximum level in the morning and a minimum level at night, as compared with 90% of adult controls and 81% of children with autistic spectrum disorders; moreover, abnormal cortisol rhythms were more frequently found in children with severe ADHD compared with children with mild ADHD [2]. However, subsequent studies have found less consistent findings. For example, one study comparing ADHD and typically developing (TD) children reported a lower morning salivary cortisol level in children with ADHD [3], while another study reported no differences [4]. Moreover, while some studies demonstrated a correlation between low basal cortisol levels and hyperactivity [2, 5] and total ADHD symptoms [5], other studies failed to report such association [6]. There had only been two systematic reviews and meta-analyses of biomarkers, including cortisol, in both children and adults with ADHD: one did not perform subanalysis in regards to the timing of sample collection [7], and the other only included adult subjects [8].
Inflammation has also been suggested to play a crucial role in the pathogenesis of ADHD. Epidemiology, genetic studies, and a recent systematic review have provided support by showing high comorbidity of ADHD with inflammatory and autoimmune disorders and the differences in biomarkers between ADHD and TD youth [9–13]. For example, ADHD is more likely to have allergy associated disorders including asthma, rhinitis, atopic dermatitis and allergic conjunctivitis [9], and psoriasis [10]. Moreover, a personal and maternal history of autoimmune diseases, such as thyrotoxicosis, type 1 diabetes, autoimmune hepatitis, psoriasis, and ankylosing spondylitis, has been associated with an increased risk for ADHD [11].
Furthermore, ADHD has been suggested as the result of an exaggerated central nervous system (CNS) inflammatory response in fetus associated with maternal inflammation [14]. Neonatal infection associated with inflammatory responses and systematic inflammation during the first postnatal month has been shown to be associated with the risk for ADHD at 10 years of age [15]. As for the genetic studies, De Jong et al. [12]. found a similar genetic signature between ADHD and depression in genes related to inflammation. On the other hand, the studies regarding inflammatory biomarkers in ADHD have been inconclusive. For example, some studies reported a higher immunoreactivity and higher levels of a pro-inflammatory cytokine such as IL-6 and anti-inflammatory cytokine such as IL-10 in ADHD children [16, 17], while others found no differences in IL-1b, IL-6, IL-10 levels between ADHD and normal control adults [18, 19]. In addition, there has only been one study reporting higher c-reactive protein (CRP) levels in children with ADHD when compared with TD children [20], while another study reported no association between ADHD symptoms and CRP in a non-ADHD sample [21].
In this study, we have updated the previously published meta-analysis [7] of cortisol levels by including seven recent studies [3, 20, 22–26]. Noteworthy, we assessed also the time of sample collection in potentially explaining the variability in the findings, not considered by the previous meta-analysis [7]. Moreover, to our knowledge there has been no meta-analysis on the inflammatory biomarkers in children with ADHD. Thus, our study also provides the first meta-analystic findings by pulling together all the cross-sectional studies on inflammatory biomarkers in children with ADHD.
Methods
We conducted a systematic review and a meta-analysis in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [27].
Literature search
To identify eligible studies in the systematic review and the meta-analysis, a computerized search was performed for studies available as of 19th of January 2021 in the electronic databases of PubMed at the National Library of Medicine. The search for cortisol levels was performed by using the search terms: (attention deficit hyperactivity disorder OR ADHD) AND cortisol, without special limitation in language. References lists from identified articles and relevant reviews were scrutinized for studies not indexed in the electronic databases. The search for inflammatory biomarkers was performed by using the search terms: (attention deficit hyperactivity disorder OR ADHD) AND inflammation; (attention deficit hyperactivity disorder OR ADHD) AND (c-reactive protein or CRP); (attention deficit hyperactivity disorder OR ADHD) AND interleukin; (attention deficit hyperactivity disorder OR ADHD) AND (tumour necrosis factor-α or TNF-α), without special limitation in language. References lists from identified articles and relevant reviews were scrutinized for studies not indexed in the electronic databases. Our initial search identified 154 studies for the cortisol levels (see Supplementary Fig. S1) and 273 studies for the inflammatory biomarker levels (see Supplementary Fig. S2).
Inclusion criteria of studies in the meta-analysis
The characteristics and references of the included articles are described in Tables 1 and 2.
Table 1.
Characteristics of Studies Included in the Meta-Analysis for Cortisol Levels in Children with ADHD.
| Studies | ADHD, n (male, %) | TD, n (male, %) | Med (%)* | Age (yrs), mean (SD), or age range | Country | Sample Origin, Time |
|---|---|---|---|---|---|---|
| Jansen (1999) [79] | 10 (100) | 15 (86.7) | NS | ADHD: 9.8 (1.5) TD: 10 (2.0) | NL | S, PM |
| Snoek (2004) [80] | 23 (82.6) | 26 (76.9) | 73.9 | ADHD: 9.8 (1.4) TD: 10.3 (1.3) | NL | S, PM |
| White (2005) [81] | 12 (83) | 21 (79) | 0 | ADHD: 5–12 TD: 6–13 | USA | S, PM |
| Blomqvist (2007) [82] | 18 (83.3) | 71 (66.2) | 16.7 | 13 | Sweden | S, AM PM |
| Randazzo (2008) [83] | 13 (61.5) | 19 (31.6) | 0 | Boys: 9–13 Girls: 8–12 | USA | S, PM |
| Freitag (2009) [84] | 52 (79) | 69 (48) | 37$ | ADHD: 9.4 (1.7) TD: 10.0 (1.5) | Germany | S, AM |
| Maldonado (2009) [85] | 33 (45.5) | 33 (57.6) | 0 | ADHD: 6.5 (.15) TD: 6.2 (.13) | Spain | S, AM |
| Van West (2009) [86] | 52 (86.5) | 25 (80) | 0 | ADHD: 8.5 (1.8) TD: 8.9 (1.5) | Belgium | S, PM |
| Christiansen (2010) [87] | 62 (NS) | 61 (NS) | 37.1 | ADHD: 10.6 (2.8) TD: 10.5 (2.7) | Germany | S, AM |
| Ma (2011) [88] | 128 (100) | 30 (100) | NS | ADHD: 9.6 (2.4) TD:10.2 (3.3) | China | B, AM |
| McCarthy (2011) [89] | 28 (66) | 334 (48) | 75.9 | 4–10 | USA | S, AM |
| Wang (2011) [90] | 50 (80) | 50 (80) | 0 | ADHD: 7.6 (1.6) TD:7.8 (1.5) | Taiwan | S, AM |
| Imeraj (2012) [91] | 11 (82) | 33 (79) | 0@ | ADHD: 8.8 (1.5) TD: 8.9 (1.6) | Belgium | S, D |
| Isaksson (2012) [92] | 161 (75.6) | 168 (41.6) | 89 | 6–17 | Sweden | S, D |
| Kuppili (2017) [93] | 30 (93) | 30 (93) | 0 | ADHD: 9.47 (2.43) TD: 10.30 (2.79) | India | B, AM |
| Angeli (2018) [94] | 42 (78.6) | 40 (62.5) | 0 | ADHD: 8.4 (1.9) TD:8.1 (1.7) | Greece | S, D |
| Isik (2018) [95] | 77 (74) | 42 (69) | 0 | ADHD: 10.2 (2.1) TD: 10.9 (2.8) | Turkey | B, AM |
| Anesiadou (2021) [96] | 34 (65) | 24 (67) | 0 | ADHD: 8.79 (1.43) TD: 9.74 (1.98) | Greece | S,D |
| Chang (2020) [97] | 95 (86) | 21 (71) | 0 | ADHD: 9.32 (3.05) TD: 9.19 (2.96) | Taiwan | S, D |
Note, ADHD attention deficit hyperactivity disorder, AM morning, B blood, D diurnal, N number, NL Netherlands, NS not specified, PM afternoon, S saliva, SD standard deviation, TD typically developing youth, yrs years.
*Indicates % of ADHD medication use in ADHD group; $Indicates no meds prior to sampling; @Indicates no meds 72 h prior to sampling.
Table 2.
Characteristics of Studies Included in the Meta-Analysis for Inflammatory Biomarker Levels in Children with ADHD.
| Studies | ADHD, n (male, %) | TD, n (male, %) | Med (%)a | Age (yrs), mean (SD), or age range | Country |
|---|---|---|---|---|---|
| Oades (2010) [98] | 21 (67) | 21 (95) | 0 | ADHD: 9.84 (1.4) TD: 11.0 (1.5) | Germany |
| Verlaet (2019) [99] | 57 (71) | 69 (65) | 0 | ADHD: 8.98 (1.75) TD: 8.37 (1.69) | NL |
| Darwish (2019) [100] | 60 (83) | 60 (68) | 0 | ADHD: 8.4 (1.28) TD: 8.73 (1.89) | Egypt |
| Chang (2020) [101] | 95 (86) | 21 (71) | 0 | ADHD: 9.32 (3.05) TD: 9.19 (2.96) | Taiwan |
Note ADHD attention deficit hyperactivity disorder, N number, NL Netherlands, SD standard deviation, TD typically developing youth, yrs years.
aIndicates % of ADHD medication use in ADHD group.
ADHD and cortisol levels
Our criteria were: the studies (1) measured levels of cortisol of blood or salivary sample; (2) participants were school-aged children (4–12 years) and adolescents (13–17 years) who had a diagnosis of ADHD; (3) the data allowed to calculate an effect size; and (4) the publications were in peer-reviewed journals. Nineteen studies [3–5, 20, 22–26, 28–37] were included in the meta-analysis on cortisol levels.
ADHD and Inflammatory Biomarker Levels
Our criteria were: the studies (1) measured levels of inflammatory biomarkers including C-reactive protein, interleukin (IL)−1β, IL-6, IL-10, and tumour necrosis factor (TNF-)α; (2) participants were school-aged children (4–12 years) and adolescents (13–17 years) who had a diagnosis of ADHD; 3) the data allowed to calculate an effect size; and (4) the publications were in peer-reviewed journals. Four studies [19, 20, 38, 39] were included in the meta-analysis on inflammatory biomarker levels.
Studies that included and re-analysed the same data set as previously published studies were not regarded as independent, and in this case only the study with the highest number of participants was included. See Supplementary Fig. S1 and Supplementary Fig. S2 for the flowchart showing the selection of included studies. To assess the quality of the included cross-sectional studies, we used the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Analytical Cross-Sectional Studies [40]. This tool considers the following: (1) definition of the inclusion criteria,(2) description of the study subjects and the settings, (3) valid and reliable measurements of the exposure, (4) objective and standard criteria for measurement, (5) confounding factors, (6) strategies for confounding factors, (7) valid and reliable measures of outcomes, and (8) statistical analysis used. The results of the appraisal were used to inform the synthesis and interpretation of the review results. See Supplementary Tables S1 and S2 for the quality check of the included studies.
Meta-analytic methods
In our analysis, the primary outcomes were comparisons of (1) cortisol levels and (2) levels of IL-1β, IL-6, IL-10, and TN-α, between ADHD and controls. For each identified study, the effect size (ES) expressing the difference in the cortisol levels ((or the area-under-the-curve with respect to the ground (AUCg) if diurnal cortisol was measured in the study) or differences in the inflammatory biomarker levels between ADHD and controls, were described as the standardized mean difference (SMD) on the basis of Hedge’s adjusted g, in which a value lesser than 0 indicated that cortisol levels or inflammatory biomarker levels were higher in ADHD subjects. When these data could not be retrieved from the publications, we contacted the authors to acquire the data of derived ES from other measures of variability. The results of individual studies were synthesized by the random-effects model [41], by which ESs were pooled and 95% confidence intervals (CIs) were calculated. The significance of the pooled effect size was determined by the z test. Sensitivity analyses were performed to determine whether any individual study was responsible for the significant results; moreover, each study was individually removed and the significance was retested. The main results of the meta-analysis did not change after the removal of any one of the included studies. The I2 statistic assessed heterogeneity between studies. Publication bias was assessed using the Egger regression asymmetry tests (and inspection of the regression asymmetry plot) and the Begg adjusted rank correlation test. There was no publication bias in the 19 studies (Begg’s test, p for bias = 0.916; Egger’s test, p for bias = 0.434). Meta-analyses were conducted by applying STATA [42] and Forest Plots were created by using Review Manager 5.3 [43]. Two-sided p values < 0.05 were considered statistically significant.
Results
Youth with ADHD have lower cortisol levels
The meta-analysis on 19 studies comparing basal cortisol levels (saliva and blood) in children with ADHD and TD children showed that ADHD youth have lower basal cortisol levels, independently from the time-point (n = 1863, g = 0.68, p = 0.004) (see Fig. 1a) and lower AUCg (n = 718, g = 0.39, p = 0.008) (see Fig. 1b). In addition, when we analysed the 14 studies that measured the morning cortisol levels, youth with ADHD continue to have a lower cortisol level than TD youth (n = 1679 participants, g = 0.84, p = 0.003) (see Fig. 2a). On the other hand, the subanalysis of 9 studies with the afternoon salivary cortisol levels showed no difference between ADHD and TD groups (n = 858, p = 0.48) (see Fig. 2b).
Fig. 1. Forest plots comparing effect sizes of basal cortisol levels and AUCg between ADHD and TD groups.
Forest plots showing effect sizes (Hedges’s g) and 95% confidence intervals (CIs) from individual studies and pooled results comparing (a) cortisol levels at any time point throughout the day and (b) cortisol AUCg between ADHD population and TD group. Note, ADHD attention deficit hyperactivity disorder, AUCg area-under-the-curve with respect to the ground, CI confidence interval, Std standard, TD typically developing youth.
Fig. 2. Forest plots comparing effect sizes of morning and afternoon cortisol levels between ADHD and TD groups.
Forest plots showing effect sizes (Hedges’s g) and 95% confidence intervals (CIs) from individual studies and pooled results comparing (a) morning and (b) afternoon cortisol levels between ADHD population and TD group. Note, ADHD attention deficit hyperactivity disorder, CI confidence interval, Std standard, TD typically developing youth.
Since salivary sampling is a non-invasive and convenient method to measure cortisol, thus we repeated the analysis after exclusion of three studies that measured blood cortisol (both in the morning), and found again that youth with ADHD have lower salivary cortisol levels than TD youth (n = 1570 g = 0.80, p = 0.006) (see Supplementary Figure S3a). The subanalysis of 11 studies measuring morning salivary cortisol levels (n = 1354, g = 0.99, p = 0.006) and 6 studies measuring awakening salivary cortical levels (n = 750, g = 0.27, p = 0.002) confirmed that youth with ADHD have lower salivary cortisol levels than TD youth (Supplementary Fig. S3b and c). The subanalysis of 3 studies measuring noon salivary cortisol levels (n = 242, p = 0.07) (Supplementary Fig. S4a) and the subanalysis of 5 studies measuring bedtime salivary cortisol levels (n = 704, p = 0.51) showed no differences between youth with ADHD and TD youth (see Supplementary Fig. S4b).
Youth with ADHD have lower TNF-α levels
The meta-analysis on 3 studies comparing TNF-α levels in children with ADHD and TD children showed that ADHD youth have lower TNF-α levels (n = 257, g = 0.32, p = 0.004) (see Fig. 3). However, there were no differences in IL-1β (p = 0.21) or IL-10 (p = 0.77) levels between children with ADHD and TD children (see Supplementary Fig. S5a and c). However, there is a trend showing that ADHD youth have higher IL-6 levels than TD youth (p = 0.09) (see Supplementary Fig. S5b).
Fig. 3. Forest plots comparing effect sizes of TNF-α levels between ADHD and TD groups.
Forest plots showing effect sizes (Hedges’s g) and 95% confidence intervals (CIs) from individual studies and pooled results comparing TNF-α levels between ADHD population and TD group. Note, ADHD, attention deficit hyperactivity disorder, CI confidence interval, Std standard, TD typically developing youth, TNF-α tumour necrosis factor-alpha.
Discussion
The major findings of our meta-analyses are that ADHD youth have lower basal cortisol levels at any time point, lower AUCg, lower morning cortisol levels, and lower TNF-α levels when compared with TD youth. To our knowledge, this is the first meta-analysis of cortisol levels of children with ADHD to include cortisol samples from both blood and saliva and examining sample collection time as a variable, and also the first meta-analysis of inflammatory biomarker levels of children with ADHD.
Morning salivary cortisol level seems to be a potential biomarker for children with ADHD, since it provides a non-invasive alternative to serum cortisol levels which closely correlates with plasma-free cortisol [44]. Overall, our results showing a lower morning cortisol level, especially awakening cortisol level, in ADHD youth may provide a partial explanation of why youth with ADHD may feel tired and have a later rise time in the morning [45], since their cortisol levels may require a longer time to peak. An altered diurnal rhythm of cortisol levels may contribute to the low morning cortisol levels in children with ADHD. A phase delay of cortisol rhythms in ADHD has been further supported by a study of adults with ADHD [46], where adults with ADHD had a delayed phase of cortisol rhythm by 2 h. Incidentally, the lack of difference in the afternoon salivary cortisol levels between youth with ADHD and TD youth may be explained by the higher degree of exposure to stressors, including familial conflicts, in the youth with ADHD throughout the day [47]. For example, children with ADHD often have poor peer and family interactions and encounter stressful scenarios at school and at home [47, 48], which may cause a continuous increase in free cortisol levels. This evidence points at the HPA axis as a potential therapeutic target for ADHD. Medications for ADHD, such as methylphenidate, are able to increase cortisol levels by triggering dopamine release in the central nervous system [49], while glucocorticoids administration improves impulse control in continuous performance tests [50], possibly by enhancing the effects of dopamine in the meso-limbic system [51]. Furthermore, treatment with stimulant medication has been shown to increase baseline cortisol levels [52].
In addition, many other factors may also affect the cortisol levels, such as length of rest period before sample collection, chronic use of nicotine, alcohol, medications, common heterozygous mutations of the 21-hydroxylase gene (a decreased adrenal 21-hydroxylase activity will interfere with cortisol biosynthesis) [53]. However, these factors are often less mentioned in most of the studies. We have carried out a qualitative examination on the aforementioned factors in the included studies of our meta-analysis (see Table 1 and Supplementary Table S3) and found that although most of the studies [3–5, 20, 22–26, 29–34, 36, 37] reported ADHD medication use status except for Jansen et al. [28] and Ma et al. [35], none mentioned about the 21-hydroxylase genetic mutations. In addition, although most of the included studies, other than those collected awakening salivary cortisol levels [3, 20, 22, 23, 26, 32], did not report the resting time required prior to the sample collection, however, they did ask the patients to have at least 30 min to a 90 min gap between brushing their teeth, eating/ drinking and the sample collection; [4, 5, 20, 24, 25, 31, 34–37] and at least a 90 min to a 24 h restriction of strenuous exercises prior to the sample collection [5, 20, 25, 35]. What is more striking is that only 3 studies [5, 20, 25] asked their participants not to drink alcohol or smoke prior to the sample collection or mentioned substance use disorder in the exclusion criteria, although about more than half the studies [3, 20, 24, 25, 30–32, 34, 35, 37] included in the meta-analysis enrolled teenagers with age ≥13, a population relatively at risk for substance use. Therefore, factors such as chronic nicotine or alcohol use and genetic mutation of the 21 hydroxylases should be examined in detail in future studies studying cortisol levels in youth.
Although the sensitivity analysis showed that the main results of the meta-analysis did not change after the removal of any one of the included studies. Maldonado et al. 2009 [33] and McCarthy et al. 2011 [36] seem to drive the effects in the basal cortisol (Fig. 1a) and morning cortisol analyses (Fig. 2a). Thus, we performed a subanalysis excluding the two studies and found the results for the basal cortisol levels and the morning cortisol levels remained significant (g = 0.27; p = 0.010; g = 0.24; p = 0.020, respectively). The heterogeneity (I2) also decreased (for the basal cortisol levels I2 decreased from 95% to 73.1%; for the morning cortisol levels, I2 decreased from 96–65.5%). These two studies may differ from the rest of the included studies in that they included participants much younger than the rest of the other studies (most of the studies included participants older than 6 years of age), where the participants in Maldonado et al.’s study range from 5–8 years of age and in McCarthy et al.’s study range from 4–10 years of age. Moreover, the inclusion criteria for McCarthy’s study are parental reports of the ADHD diagnosis and the use of stimulants, rather than diagnosis made by clinical professionals or by DSM structured interviews.
Of note, it has been reported that the immunoassays measuring cortisol do not just measure cortisol, but also measure inactive 5α-reduced metabolites of cortisol [54, 55]. Therefore, it may not be low levels of cortisol but rather low levels of the non-active 5α-reduced metabolite of cortisol associated with psychiatric disorders or the severity of the psychiatric disorders [54, 55]. Thus, in order to elucidate the relationship of cortisol in youth with ADHD, the use of mass spectrometry may be necessary to accurately understand the role of cortisol in ADHD.
Our study finding is overall consistent with Scassellati’s meta-analysis of 8 studies of salivary cortisol levels, where patients with ADHD had lower cortisol levels when compared to TD subjects (p = 0.0001) [7]. We have updated this meta-analysis by adding five more recent studies, measuring salivary cortisol levels [3, 20, 22, 23, 26], and also by including three other studies [30, 31, 36], not included by Scassellati et al. meta-analysis. It is also of note that Bonvicini et al.’s meta-analysis of 3 studies of adults with ADHD (n = 117) showed no difference between salivary cortisol levels of ADHD and normal controls (p = 0.13), but there was a numerical trend showing adults with ADHD having lower salivary cortisol levels [8].
Another interesting finding of our meta-analysis is that children with ADHD have a lower level of TNF-α than control children. This finding is different from previous study findings showing no difference in TNF-α levels in ADHD subjects, both youth and adults, and normal controls [18, 19]. On the other hand, lower levels of TNF-α have been positively associated with reaction time (RT) variability in the Continuous Performance Test (indicating inattention) in ADHD [56]. RT variability is the core feature of the hypothesis of glial impairment in ADHD [57] and has been suggested as an endophenotype for ADHD [56]. Moreover, a study addressing the association between ADHD and polymorphism of TNF-α genes in children with ADHD and healthy controls showed that the 308 polymorphism (alleles 1 and 2) at the TNF-α gene is correlated with two attention measures, the hand-eye test of the Neurobehavioral Evaluation System (NES2), which evaluates visual-motor coordination, and sub-test of Shape Discrimination Test (TDTP) [58]. Specifically, individuals without any TNF-α gene allele 2 perform significantly better in the accuracy sub-test of TDTP than individuals with allele 2 (homozygotes or heterozygotes). In addition, a negative correlation has been shown between cortisol awakening response and TNF-α in adults with inattentive type ADHD but not in adults with other subtypes [18]. It has been reported that an imbalance of TNF-α levels, whether too much or too little, can impair cognitive function [59, 60], and the variation of the TNF-α levels may influence the turnover of the monoamines [61]. Thus, inadequate or excess levels of TNF-α may be associated with impaired cognitive performance. More studies with a larger sample will be needed to further clarify the role of TNF-α in ADHD.
Although there is no difference in the interleukin levels between ADHD and TD youth in our meta-analysis, there is a trend showing that IL-6 is higher in ADHD youth than in TD youth. The finding may be not significant due to a lack of power, as genetic, animal, and clinical studies have suggested a potential role of IL-6 in ADHD pathogenesis. For example, one study showed an increased frequency of the C allele at the 174 polymorphism of the IL-6 gene in children with ADHD; moreover, the A and G alleles of the 174 polymorphism have been associated with measures of attention, with people with the IL-6 AA homozygotes performing better than IL-6 homozygotes [58]. Animal studies show that administration of IL-6 in rodent models will alter neurotransmission changes that are similar to the changes seen in ADHD, such as reduced dopamine levels [62]. Moreover, children born prematurely, and with a current or persistent elevation of inflammatory markers, including IL-6, during the first two postnatal weeks, show attention problems at 2 years of age [63]. In addition, a study has shown the decrease in cytokine levels such as IL-6 and CRP, after 8-week omega-3 supplementation, in children with ADHD was correlated with significant improvement in clinical symptoms [64], although our own study did not replicate these findings, and pointed to the need of dividing ADHD children in subgroups based on their biomarker profile [65]. Finally, our systematic review only identified one cross-sectional study comparing CRP levels between ADHD youth and TD youth, where ADHD youth had higher levels of CRP [20]. Thus, more studies on CRP in ADHD are warranted for further investigation. Of note, the situation with high IL-6 and low TNF-α observed in ADHD youth in our study has also been observed in patients with Schizophrenia during both exacerbation and remission [66]. The increase in IL-6 may be associated with the decrease of TNF-α, since IL-6 has been shown to have a suppressive effect on TNF-α production [67], and that they mutually counter-regulate each other during the initial phase of an immune response [68].
A number of biological mechanisms have been proposed to explain the HPA axis and inflammatory abnormalities in ADHD. Youth with ADHD may have an under-active behavioural inhibition system (BIS) [69], and an under-active BIS is closely associated with both lower cortisol levels and deficits in working memory, self-regulation of affect, internalization of speech, and reconstitution of goal-directed behavior in ADHD [70]. ADHD has also been associated with psychosocial adversity and prenatal stress [71], which in turn may lead to low cortisol levels [72, 73] and to hyporeactivity of the HPA axis as one way to adapt to chronic stress [72]. Moreover, youth with ADHD often have a lack of physiological arousal when facing challenges, and this low level of physiological arousal may then drive the child to search for sensations that could eventually trigger a decrease in cortisol response to stressors, after repeated activations [74]. Some evidence suggests a common pathway for the development of both HPA axis and inflammatory abnormalities. ADHD often co-occurs with allergic diseases, and some studies have indicated an association between ADHD and streptococcus-mediated neuropsychiatric disorders [75]. It is possible that a sustained and exaggerated release of inflammatory cytokines in atopic eczema (AE) affected children may impact ADHD relevant brain circuits and affecting behaviour and motor control, emotional regulation, or motivational mechanisms [75]. Moreover, ADHD has been shown to have a higher comorbidity with T-cell mediated neuroinflammation [76, 77], such as celiac diseases and atopic diseases.
The main limitation of our meta-analysis is that we did not control for confounders such as diet and exercise, and that we did not subgroup the subjects into the three ADHD subtypes (inattentive, the hyperactive-impulsive, and the combined subtypes), as these data were not consistently present in the included papers. Moreover, we did not account for the cortisol awakening response, therefore we cannot draw any conclusion on the stress reactivity in ADHD. However, a previous meta-analysis on cortisol reactivity in response to a stressor in ADHD showed no difference between cortisol reactivity and ADHD, but implied that there is significant heterogeneity in the analyses that might serve as moderators of this association [78]. In addition, the heterogeneity of the studies should be considered when interpreting the results of our meta-analyses. For example, as mentioned earlier in the discussion section, when we excluded Maldonado et al. and McCarthy et al. from the analyses, the heterogeneity decreased, which may be attributed to the inclusion of a younger age group (<6 years old) and less rigorous inclusion criteria for the diagnosis of ADHD (self-reports vs structured interviews, in the case of McCarthy et al.’s study). It is also important to point out that there is a limited literature [19, 20, 39] (3 studies) on TNF-α in ADHD, thus more studies in the future are warranted to support the potential role of TNF-α as a biomarker in ADHD.
Conclusion
We find, in our meta-analysis of existing studies, that children with ADHD have lower basal cortisol levels, especially morning cortisol levels, than TD youth. The lower cortisol levels in ADHD further imply the role of HPA axis hypoactivity in ADHD pathogenesis. In addition, since salivary cortisol levels are often normalized after the child receives treatments with stimulant medications; further attention is warranted for the development of potential treatment strategies involving the normalization of salivary cortisol levels in youth with ADHD. Moreover, we also found that ADHD youth have lower TNF-α levels than TD youth, thus suggesting future studies should investigate TNF-α as a potential biomarker in ADHD.
Supplementary information
Acknowledgements
The work was supported by the following grants: MOST 109–2320-B-038–057-MY3, 109–2320-B-039–066, 110–2321-B-006–004, 110–2811-B-039–507, 110–2320-B-039–048-MY2, and 110–2320-B-039–047-MY3 from the Ministry of Science and Technology, Taiwan; ANHRF109–31 from An Nan Hospital, China Medical University, Tainan, Taiwan; CMRC-CMA-2 from Higher Education Sprout Project by the Ministry of Education (MOE), Taiwan; CMU108-SR-106 from the China Medical University, Taichung, Taiwan; and CMU104-S-16–01, CMU103-BC-4–1, CRS-108–048, DMR-102–076, DMR-103–084, DMR-106–225, DMR-107–204, DMR-108–216, DMR-109–102, DMR-109–244, DMR-HHC-109–11 and DMR-HHC-109–12, DMR-HHC-110–10,DMR-110–124 from the China Medical University Hospital, Taichung, Taiwan. Dr. Pariante and Dr. Mondelli are also supported by the grants “Immunopsychiatry: a consortium to test the opportunity for immunotherapeutics in psychiatry’ (MR/L014815/1) and ‘Persistent Fatigue Induced by Interferon-alpha: A New Immunological Model for Chronic Fatigue Syndrome’ (MR/J002739/1), from the Medical Research Council (UK), and by the National Institute for Health Research Mental Health Biomedical Research Centre in Mental Health at South London and Maudsley NHS Foundation Trust and King’s College London.
Author contributions
JPC and CMP created the concept and designed the study. JPC and VM perform the literature search, data analysis and prepared the manuscript. JPC, KPS, and CMP undertook the interpretation of results and revision of the manuscript. All the authors have approved the final manuscript and take responsibility for the integrity and accuracy of this study.
Competing interests
Dr. Chang and Dr. Su declare no conflict of interest. Dr. Pariante and Dr. Mondelli have received research funding from Janssen Pharmaceutical NV/Janssen Pharmaceutical Companies of Jonhson&Jonhson. Dr. Pariante has also received speaker’s fees from Lundbeck and consultation fees from Consultant to Eleusis Benefit Corporation.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41398-021-01550-0.
References
- 1.Steingard R, Biederman J, Keenan K, Moore C. Comorbidity in the interpretation of dexamethasone suppression test results in children: a review and report. Biol Psychiatry. 1990;28:193–202. doi: 10.1016/0006-3223(90)90574-L. [DOI] [PubMed] [Google Scholar]
- 2.Kaneko M, Hoshino Y, Hashimoto S, Okano T, Kumashiro H. Hypothalamic-pituitary-adrenal axis function in children with attention-deficit hyperactivity disorder. J Autism Dev Disord. 1993;23:59–65. doi: 10.1007/BF01066418. [DOI] [PubMed] [Google Scholar]
- 3.Isaksson J, Nilsson KW, Nyberg F, Hogmark A, Lindblad F. Cortisol levels in children with attention-deficit/hyperactivity disorder. J Psychiatr Res. 2012;46:1398–405. doi: 10.1016/j.jpsychires.2012.08.021. [DOI] [PubMed] [Google Scholar]
- 4.van West D, Claes S, Deboutte D. Differences in hypothalamic-pituitary-adrenal axis functioning among children with ADHD predominantly inattentive and combined types. Eur Child Adolesc Psychiatry. 2009;18:543–53. doi: 10.1007/s00787-009-0011-1. [DOI] [PubMed] [Google Scholar]
- 5.Wang LJ, Huang YS, Hsiao CC, Chiang YL, Wu CC, Shang ZY, et al. Salivary dehydroepiandrosterone, but not cortisol, is associated with attention deficit hyperactivity disorder. World J Biol Psychiatry. 2011;12:99–109. doi: 10.3109/15622975.2010.512090. [DOI] [PubMed] [Google Scholar]
- 6.Pesonen AK, Kajantie E, Jones A, Pyhälä R, Lahti J, Heinonen K, et al. Symptoms of attention deficit hyperactivity disorder in children are associated with cortisol responses to psychosocial stress but not with daily cortisol levels. J Psychiatr Res. 2011;45:1471–6. doi: 10.1016/j.jpsychires.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 7.Scassellati C, Bonvicini C, Faraone SV, Gennarelli M. Biomarkers and attention-deficit/hyperactivity disorder: a systematic review and meta-analyses. J Am Acad Child Adolesc Psychiatry. 2012;51:1003–19 e1020. doi: 10.1016/j.jaac.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 8.Bonvicini C, Faraone SV, Scassellati C. Attention-deficit hyperactivity disorder in adults: a systematic review and meta-analysis of genetic, pharmacogenetic and biochemical studies. Mol Psychiatry. 2016;21:1643. doi: 10.1038/mp.2016.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miyazaki C, Koyama M, Ota E, Swa T, Mlunde LB, Amiya RM, et al. Allergic diseases in children with attention deficit hyperactivity disorder: a systematic review and meta-analysis. BMC Psychiatry. 2017;17:120. doi: 10.1186/s12888-017-1281-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hegvik TA, Instanes JT, Haavik J, Klungsoyr K, Engeland A. Associations between attention-deficit/hyperactivity disorder and autoimmune diseases are modified by sex: a population-based cross-sectional study. Eur Child Adolesc Psychiatry. 2018;27:663–75. doi: 10.1007/s00787-017-1056-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nielsen PR, Benros ME, Dalsgaard S. Associations between autoimmune diseases and attention-deficit/hyperactivity disorder: a nationwide study. J Am Acad Child Adolesc Psychiatry. 2017;56:234–40 e231. doi: 10.1016/j.jaac.2016.12.010. [DOI] [PubMed] [Google Scholar]
- 12.de Jong S, Newhouse SJ, Patel H, Lee S, Dempster D, Curtis C, et al. Immune signatures and disorder-specific patterns in a cross-disorder gene expression analysis. Br J Psychiatry. 2016;209:202–8. doi: 10.1192/bjp.bp.115.175471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anand D, Colpo GD, Zeni G, Zeni CP, Teixeira AL. Attention-deficit/hyperactivity disorder and inflammation: what does current knowledge tell us? A systematic review. Front Psychiatry. 2017;8:228. doi: 10.3389/fpsyt.2017.00228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leffa DT, Torres ILS, Rohde LA. A review on the role of inflammation in attention-deficit/hyperactivity disorder. Neuroimmunomodulation. 2018;25:328–33. doi: 10.1159/000489635. [DOI] [PubMed] [Google Scholar]
- 15.Allred EN, Dammann O, Fichorova RN, Hooper SR, Hunter SJ, Joseph RM, et al. Systemic inflammation during the first postnatal month and the risk of attention deficit hyperactivity disorder characteristics among 10 year-old children born extremely preterm. J Neuroimmune Pharm. 2017;12:531–43. doi: 10.1007/s11481-017-9742-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Donfrancesco R, Nativio P, Di Benedetto A, Villa MP, Andriola E, Melegari MG, et al. Anti-Yo antibodies in children with ADHD: first results about serum cytokines. J Atten Disord. 2020;24:1497–502. doi: 10.1177/1087054716643387. [DOI] [PubMed] [Google Scholar]
- 17.Passarelli F, Donfrancesco R, Nativio P, Pascale E, Di Trani M, Patti AM, et al. Anti-Purkinje cell antibody as a biological marker in attention deficit/hyperactivity disorder: a pilot study. J Neuroimmunol. 2013;258:67–70. doi: 10.1016/j.jneuroim.2013.02.018. [DOI] [PubMed] [Google Scholar]
- 18.Corominas-Roso M, Armario A, Palomar G, Corrales M, Carrasco J, Richarte V, et al. IL-6 and TNF-alpha in unmedicated adults with ADHD: Relationship to cortisol awakening response. Psychoneuroendocrinology. 2017;79:67–73. doi: 10.1016/j.psyneuen.2017.02.017. [DOI] [PubMed] [Google Scholar]
- 19.Oades RD, Dauvermann MR, Schimmelmann BG, Schwarz MJ, Myint AM. Attention-deficit hyperactivity disorder (ADHD) and glial integrity: S100B, cytokines and kynurenine metabolism-effects of medication. Behav Brain Funct. 2010;6:29. doi: 10.1186/1744-9081-6-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang JP, Mondelli V, Satyanarayanan SK, Chiang YJ, Chen HT, Su KP, et al. Cortisol, inflammatory biomarkers and neurotrophins in children and adolescents with attention deficit hyperactivity disorder (ADHD) in Taiwan. Brain Behav Immun. 2020;88:105–13. doi: 10.1016/j.bbi.2020.05.017. [DOI] [PubMed] [Google Scholar]
- 21.Vogel SWN, Bijlenga D, Verduijn J, Bron TI, Beekman A, Kooij J, et al. Attention-deficit/hyperactivity disorder symptoms and stress-related biomarkers. Psychoneuroendocrinology. 2017;79:31–39. doi: 10.1016/j.psyneuen.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 22.Imeraj L, Antrop I, Roeyers H, Swanson J, Deschepper E, Bal S, et al. Time-of-day effects in arousal: disrupted diurnal cortisol profiles in children with ADHD. J Child Psychol Psychiatry. 2012;53:782–9. doi: 10.1111/j.1469-7610.2012.02526.x. [DOI] [PubMed] [Google Scholar]
- 23.Angeli E, Korpa T, Johnson EO, Apostolakou F, Papassotiriou I, Chrousos GP, et al. Salivary cortisol and alpha-amylase diurnal profiles and stress reactivity in children with attention deficit hyperactivity disorder. Psychoneuroendocrinology. 2018;90:174–81. doi: 10.1016/j.psyneuen.2018.02.026. [DOI] [PubMed] [Google Scholar]
- 24.Kuppili PP, Pattanayak RD, Sagar R, Mehta M, Vivekanandhan S. Thyroid and cortisol hormones in attention deficit hyperactivity disorder: a case-control study. Asian J Psychiatr. 2017;28:73–77. doi: 10.1016/j.ajp.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 25.Isik U, Bilgic A, Toker A, Kilinc I. Serum levels of cortisol, dehydroepiandrosterone, and oxytocin in children with attention-deficit/hyperactivity disorder combined presentation with and without comorbid conduct disorder. Psychiatry Res. 2018;261:212–9. doi: 10.1016/j.psychres.2017.12.076. [DOI] [PubMed] [Google Scholar]
- 26.Anesiadou S, Makris G, Michou M, Bali P, Papassotiriou I, Apostolakou F, et al. Salivary cortisol and alpha-amylase daily profiles and stress responses to an academic performance test and a moral cognition task in children with neurodevelopmental disorders. Stress Health. 2021;37:45–49. doi: 10.1002/smi.2971. [DOI] [PubMed] [Google Scholar]
- 27.Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jansen LM, Gispen-de Wied CC, Jansen MA, van der Gaag RJ, Matthys W, van Engeland H. Pituitary-adrenal reactivity in a child psychiatric population: salivary cortisol response to stressors. Eur Neuropsychopharmacol. 1999;9:67–75. doi: 10.1016/S0924-977X(98)00003-0. [DOI] [PubMed] [Google Scholar]
- 29.Snoek H, Goozen Van, Matthys SH, Buitelaar W, van Engeland JK, Stress H. responsivity in children with externalizing behavior disorders. Dev Psychopathol. 2004;16:389–406. doi: 10.1017/S0954579404044578. [DOI] [PubMed] [Google Scholar]
- 30.White BP, Mulligan SE. Behavioral and physiologic response measures of occupational task performance: a preliminary comparison between typical children and children with attention disorder. Am J Occup Ther. 2005;59:426–36. doi: 10.5014/ajot.59.4.426. [DOI] [PubMed] [Google Scholar]
- 31.Randazzo WT, Dockray S, Susman EJ. The stress response in adolescents with inattentive type ADHD symptoms. Child Psychiatry Hum Dev. 2008;39:27–38. doi: 10.1007/s10578-007-0068-3. [DOI] [PubMed] [Google Scholar]
- 32.Freitag CM, Hänig S, Palmason H, Meyer J, Wüst S, Seitz C. Cortisol awakening response in healthy children and children with ADHD: impact of comorbid disorders and psychosocial risk factors. Psychoneuroendocrinology. 2009;34:1019–28. doi: 10.1016/j.psyneuen.2009.01.018. [DOI] [PubMed] [Google Scholar]
- 33.Maldonado EF, Trianes MV, Cortes A, Moreno E, Escobar M. Salivary cortisol response to a psychosocial stressor on children diagnosed with attention-deficit/hyperactivity disorder: differences between diagnostic subtypes. Span J Psychol. 2009;12:707–14. doi: 10.1017/S1138741600002079. [DOI] [PubMed] [Google Scholar]
- 34.Christiansen H, Oades RD, Psychogiou L, Hauffa BP, Sonuga-Barke EJ. Does the cortisol response to stress mediate the link between expressed emotion and oppositional behavior in attention-deficit/hyperactivity-disorder (ADHD)? Behav Brain Funct. 2010;6:45. doi: 10.1186/1744-9081-6-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ma L, Chen YH, Chen H, Liu YY, Wang YX. The function of hypothalamus-pituitary-adrenal axis in children with ADHD. Brain Res. 2011;1368:159–62. doi: 10.1016/j.brainres.2010.10.045. [DOI] [PubMed] [Google Scholar]
- 36.McCarthy AM, Hanrahan K, Scott LM, Zemblidge N, Kleiber C, Zimmerman MB. Salivary cortisol responsivity to an intravenous catheter insertion in children with attention-deficit/hyperactivity disorder. J Pediatr Psychol. 2011;36:902–10. doi: 10.1093/jpepsy/jsr012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Blomqvist M, Holmberg K, Lindblad F, Fernell E, Ek U, Dahllöf G. Salivary cortisol levels and dental anxiety in children with attention deficit hyperactivity disorder. Eur J Oral Sci. 2007;115:1–6. doi: 10.1111/j.1600-0722.2007.00423.x. [DOI] [PubMed] [Google Scholar]
- 38.Darwish AH, Elgohary TM, Nosair NA. Serum Interleukin-6 level in children with attention-deficit hyperactivity disorder (ADHD) J Child Neurol. 2019;34:61–67. doi: 10.1177/0883073818809831. [DOI] [PubMed] [Google Scholar]
- 39.Verlaet AAJ, Breynaert A, Ceulemans B, De Bruyne T, Fransen E, Pieters L, et al. Oxidative stress and immune aberrancies in attention-deficit/hyperactivity disorder (ADHD): a case-control comparison. Eur Child Adolesc Psychiatry. 2019;28:719–29. doi: 10.1007/s00787-018-1239-4. [DOI] [PubMed] [Google Scholar]
- 40.Moola, S et al. Chapter 7: Systematic review of etiology and risk. In Joanna Briggs Institute Reviewer’s Manual (eds Aromataris, E & Munn, Z)(The Joanna Briggs Institute, 2017).
- 41.Shadish, WR & Haddock, CK Combining estimates of effect size. in The Handbook of Research Synthesis (eds Cooper, H, & Hedges, LV)(Russell Sage Foundation, New York, 1994).
- 42.Stata Statistical Software: Release 15. [computer program]. College Station, TX: StatCorp; 2017.
- 43.Review Manager (RevMan) (Version 5.3) [computer program]. Copenhagen: The Nordic Chocrane Centre; 2014.
- 44.Calixto C, Martinez FE, Jorge SM, Moreira AC, Martinelli CE., Jr Correlation between plasma and salivary cortisol levels in preterm infants. J Pediatr. 2002;140:116–8. doi: 10.1067/mpd.2002.120765. [DOI] [PubMed] [Google Scholar]
- 45.Chiang HL, Gau SS, Ni HC, Chiu YN, Shang CY, Wu YY, et al. Association between symptoms and subtypes of attention-deficit hyperactivity disorder and sleep problems/disorders. J Sleep Res. 2010;19:535–45. doi: 10.1111/j.1365-2869.2010.00832.x. [DOI] [PubMed] [Google Scholar]
- 46.Baird AL, Coogan AN, Siddiqui A, Donev RM, Thome J. Adult attention-deficit hyperactivity disorder is associated with alterations in circadian rhythms at the behavioural, endocrine and molecular levels. Mol Psychiatry. 2012;17:988–95. doi: 10.1038/mp.2011.149. [DOI] [PubMed] [Google Scholar]
- 47.Chang JP, Gau SS. Mother-child relationship in youths with attention-deficit hyperactivity disorder and their siblings. J Abnorm Child Psychol. 2017;45:871–82. doi: 10.1007/s10802-016-0218-9. [DOI] [PubMed] [Google Scholar]
- 48.Gau SS, Chang JP. Maternal parenting styles and mother-child relationship among adolescents with and without persistent attention-deficit/hyperactivity disorder. Res Dev Disabil. 2013;34:1581–94. doi: 10.1016/j.ridd.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 49.Wilens TE. Effects of methylphenidate on the catecholaminergic system in attention-deficit/hyperactivity disorder. J Clin Psychopharmacol. 2008;28:S46–53. doi: 10.1097/JCP.0b013e318173312f. [DOI] [PubMed] [Google Scholar]
- 50.Wang LJ, Huang YS, Hsiao CC, Chen CK. The trend in morning levels of salivary cortisol in children with ADHD During 6 months of methylphenidate treatment. J Atten Disord. 2017;21:254–61. doi: 10.1177/1087054712466139. [DOI] [PubMed] [Google Scholar]
- 51.Marinelli M, Piazza PV. Interaction between glucocorticoid hormones, stress and psychostimulant drugs. Eur J Neurosci. 2002;16:387–94. doi: 10.1046/j.1460-9568.2002.02089.x. [DOI] [PubMed] [Google Scholar]
- 52.Kariyawasam SH, Zaw F, Handley SL. Reduced salivary cortisol in children with comorbid attention deficit hyperactivity disorder and oppositional defiant disorder. Neuro Endocrinol Lett. 2002;23:45–48. [PubMed] [Google Scholar]
- 53.Rasmusson AM, Vythilingam M, Morgan CA. The neuroendocrinology of posttraumatic stress disorder: new directions. CNS Spectr. 2003;8(Sep):651–7. doi: 10.1017/S1092852900008841. [DOI] [PubMed] [Google Scholar]
- 54.Yehuda R, Bierer LM, Andrew R, Schmeidler J, Seckl JR. Enduring effects of severe developmental adversity, including nutritional deprivation, on cortisol metabolism in aging Holocaust survivors. J Psychiatr Res. 2009;43:77–83. doi: 10.1016/j.jpsychires.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yehuda R, Bierer LM, Sarapas C, Makotkine I, Andrew R, Seckl JR. Cortisol metabolic predictors of response to psychotherapy for symptoms of PTSD in survivors of the World Trade Center attacks on September 11, 2001. Psychoneuroendocrinology. 2009;34:1304–13. doi: 10.1016/j.psyneuen.2009.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Oades RD, Myint AM, Dauvermann MR, Schimmelmann BG, Schwarz MJ. Attention-deficit hyperactivity disorder (ADHD) and glial integrity: an exploration of associations of cytokines and kynurenine metabolites with symptoms and attention. Behav Brain Funct. 2010;6:32. doi: 10.1186/1744-9081-6-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Russell VA, Oades RD, Tannock R, Killeen PR, Auerbach JG, Johansen EB, et al. Response variability in Attention-Deficit/Hyperactivity Disorder: a neuronal and glial energetics hypothesis. Behav Brain Funct. 2006;2:30. doi: 10.1186/1744-9081-2-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Drtilkova I, Sery O, Theiner P, Uhrova A, Zackova M, Balastikova B, et al. Clinical and molecular-genetic markers of ADHD in children. Neuro Endocrinol Lett. 2008;29:320–7. [PubMed] [Google Scholar]
- 59.Medeiros R, Figueiredo CP, Pandolfo P, Duarte FS, Prediger RD, Passos GF, et al. The role of TNF-alpha signaling pathway on COX-2 upregulation and cognitive decline induced by beta-amyloid peptide. Behav Brain Res. 2010;209:165–73. doi: 10.1016/j.bbr.2010.01.040. [DOI] [PubMed] [Google Scholar]
- 60.McAfoose J, Koerner H, Baune BT. The effects of TNF deficiency on age-related cognitive performance. Psychoneuroendocrinology. 2009;34:615–9. doi: 10.1016/j.psyneuen.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 61.Hayley S, Brebner K, Lacosta S, Merali Z, Anisman H. Sensitization to the effects of tumor necrosis factor-alpha: neuroendocrine, central monoamine, and behavioral variations. J Neurosci. 1999;19:5654–65. doi: 10.1523/JNEUROSCI.19-13-05654.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zalcman S, Green-Johnson JM, Murray L, Nance DM, Dyck D, Anisman H, et al. Cytokine-specific central monoamine alterations induced by interleukin-1, -2 and -6. Brain Res. 1994;643:40–49. doi: 10.1016/0006-8993(94)90006-X. [DOI] [PubMed] [Google Scholar]
- 63.O’shea TM, Joseph RM, Kuban KC, Allred EN, Ware J, Coster T, et al. Elevated blood levels of inflammation-related proteins are associated with an attention problem at age 24 mo in extremely preterm infants. Pediatr Res. 2014;75:781–7. doi: 10.1038/pr.2014.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hariri M, Djazayery A, Djalali M, Saedisomeolia A, Rahimi A, Abdolahian E. Effect of n-3 supplementation on hyperactivity, oxidative stress and inflammatory mediators in children with attention-deficit-hyperactivity disorder. Malays J Nutr. 2012;18:329–35. [PubMed] [Google Scholar]
- 65.Chang JP, Su KP, Mondelli V, Satyanarayanan SK, Yang HT, Chiang YJ, et al. High-dose eicosapentaenoic acid (EPA) improves attention and vigilance in children and adolescents with attention deficit hyperactivity disorder (ADHD) and low endogenous EPA levels. Transl Psychiatry. 2019;9:303. doi: 10.1038/s41398-019-0633-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dunjic-Kostic B, Jasovic-Gasic M, Ivkovic M, Radonjic NV, Pantovic M, Damjanovic A, et al. Serum levels of interleukin-6 and tumor necrosis factor-alpha in exacerbation and remission phase of schizophrenia. Psychiatr Danub. 2013;25:55–61. [PubMed] [Google Scholar]
- 67.Yimin, Kohanawa M, Minagawa T. Up-regulation of granulomatous inflammation in interleukin-6 knockout mice infected with Rhodococcus aurantiacus. Immunology. 2003;110:501–6. doi: 10.1111/j.1365-2567.2003.01762.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yimin, Kohanawa M. A regulatory effect of the balance between TNF-alpha and IL-6 in the granulomatous and inflammatory response to Rhodococcus aurantiacus infection in mice. J Immunol. 2006;177:642–50. doi: 10.4049/jimmunol.177.1.642. [DOI] [PubMed] [Google Scholar]
- 69.Quay HC. Inhibition and attention deficit hyperactivity disorder. J Abnorm Child Psychol. 1997;25:7–13. doi: 10.1023/A:1025799122529. [DOI] [PubMed] [Google Scholar]
- 70.Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull. 1997;121:65–94. doi: 10.1037/0033-2909.121.1.65. [DOI] [PubMed] [Google Scholar]
- 71.Biederman J, Milberger S, Faraone SV, Kiely K, Guite J, Mick E, et al. Family-environment risk factors for attention-deficit hyperactivity disorder. A test of Rutter’s indicators of adversity. Arch Gen Psychiatry. 1995;52:464–70. doi: 10.1001/archpsyc.1995.03950180050007. [DOI] [PubMed] [Google Scholar]
- 72.Moss HB, Vanyukov M, Yao JK, Kirillova GP. Salivary cortisol responses in prepubertal boys: the effects of parental substance abuse and association with drug use behavior during adolescence. Biol Psychiatry. 1999;45:1293–9. doi: 10.1016/S0006-3223(98)00216-9. [DOI] [PubMed] [Google Scholar]
- 73.Yehuda R, Engel SM, Brand SR, Seckl J, Marcus SM, Berkowitz GS. Transgenerational effects of posttraumatic stress disorder in babies of mothers exposed to the World Trade Center attacks during pregnancy. J Clin Endocrinol Metab. 2005;90:4115–8. doi: 10.1210/jc.2005-0550. [DOI] [PubMed] [Google Scholar]
- 74.Alink LR, van Ijzendoorn MH, Bakermans-Kranenburg MJ, Mesman J, Juffer F, Koot HM. Cortisol and externalizing behavior in children and adolescents: mixed meta-analytic evidence for the inverse relation of basal cortisol and cortisol reactivity with externalizing behavior. Dev Psychobiol. 2008;50:427–50. doi: 10.1002/dev.20300. [DOI] [PubMed] [Google Scholar]
- 75.Verlaet AA, Noriega DB, Hermans N, Savelkoul HF. Nutrition, immunological mechanisms and dietary immunomodulation in ADHD. Eur Child Adolesc Psychiatry. 2014;23:519–29. doi: 10.1007/s00787-014-0522-2. [DOI] [PubMed] [Google Scholar]
- 76.Gungor S, Celiloglu OS, Ozcan OO, Raif SG, Selimoglu MA. Frequency of celiac disease in attention-deficit/hyperactivity disorder. J Pediatr Gastroenterol Nutr. 2013;56:211–4. doi: 10.1097/MPG.0b013e318272b7bc. [DOI] [PubMed] [Google Scholar]
- 77.Schmitt J, Buske-Kirschbaum A, Roessner V. Is atopic disease a risk factor for attention-deficit/hyperactivity disorder? A systematic review. Allergy. 2010;65:1506–24. doi: 10.1111/j.1398-9995.2010.02449.x. [DOI] [PubMed] [Google Scholar]
- 78.Kamradt JM, Momany AM, Nikolas MA. A meta-analytic review of the association between cortisol reactivity in response to a stressor and attention-deficit hyperactivity disorder. Atten Defic Hyperact Disord. 2018;10:99–111. doi: 10.1007/s12402-017-0238-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jansen LM, Gispen-de Wied CC, Jansen MA, van der Gaag RJ, Matthys W, van Engeland H. Pituitary-adrenal reactivity in a child psychiatric population: salivary cortisol response to stressors. Eur Neuropsychopharmacol. 1999;9:67–75. doi: 10.1016/S0924-977X(98)00003-0. [DOI] [PubMed] [Google Scholar]
- 80.Snoek H, Van Goozen SH, Matthys W, Buitelaar JK, van Engeland H. Stress responsivity in children with externalizing behavior disorders. Dev Psychopathol. 2004;16:389–406. doi: 10.1017/S0954579404044578. [DOI] [PubMed] [Google Scholar]
- 81.White BP, Mulligan SE. Behavioral and physiologic response measures of occupational task performance: a preliminary comparison between typical children and children with attention disorder. Am J Occup Ther. 2005;59:426–36. doi: 10.5014/ajot.59.4.426. [DOI] [PubMed] [Google Scholar]
- 82.Blomqvist M, Holmberg K, Lindblad F, Fernell E, Ek U, Dahllof G. Salivary cortisol levels and dental anxiety in children with attention deficit hyperactivity disorder. Eur J Oral Sci. 2007;115:1–6. doi: 10.1111/j.1600-0722.2007.00423.x. [DOI] [PubMed] [Google Scholar]
- 83.Randazzo WT, Dockray S, Susman EJ. The stress response in adolescents with inattentive type ADHD symptoms. Child Psychiatry Hum Dev. 2008;39:27–38. doi: 10.1007/s10578-007-0068-3. [DOI] [PubMed] [Google Scholar]
- 84.Freitag CM, Hanig S, Palmason H, Meyer J, Wust S, Seitz C. Cortisol awakening response in healthy children and children with ADHD: impact of comorbid disorders and psychosocial risk factors. Psychoneuroendocrinology. 2009;34:1019–28. doi: 10.1016/j.psyneuen.2009.01.018. [DOI] [PubMed] [Google Scholar]
- 85.Maldonado EF, Trianes MV, Cortes A, Moreno E, Escobar M. Salivary cortisol response to a psychosocial stressor on children diagnosed with attention-deficit/hyperactivity disorder: differences between diagnostic subtypes. Span J Psychol. 2009;12:707–14. doi: 10.1017/S1138741600002079. [DOI] [PubMed] [Google Scholar]
- 86.van West D, Claes S, Deboutte D. Differences in hypothalamic-pituitary-adrenal axis functioning among children with ADHD predominantly inattentive and combined types. Eur Child Adolesc Psychiatry. 2009;18:543–53. doi: 10.1007/s00787-009-0011-1. [DOI] [PubMed] [Google Scholar]
- 87.Christiansen H, Oades RD, Psychogiou L, Hauffa BP, Sonuga-Barke EJ. Does the cortisol response to stress mediate the link between expressed emotion and oppositional behavior in attention-deficit/hyperactivity-disorder (ADHD)? Behav Brain Funct. 2010;6:45. doi: 10.1186/1744-9081-6-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ma L, Chen YH, Chen H, Liu YY, Wang YX. The function of hypothalamus-pituitary-adrenal axis in children with ADHD. Brain Res. 2011;1368:159–62. doi: 10.1016/j.brainres.2010.10.045. [DOI] [PubMed] [Google Scholar]
- 89.McCarthy AM, Hanrahan K, Scott LM, Zemblidge N, Kleiber C, Zimmerman MB. Salivary cortisol responsivity to an intravenous catheter insertion in children with attention-deficit/hyperactivity disorder. J Pediatr Psychol. 2011;36:902–10. doi: 10.1093/jpepsy/jsr012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang LJ, Huang YS, Hsiao CC, Chiang YL, Wu CC, Shang ZY, et al. Salivary dehydroepiandrosterone, but not cortisol, is associated with attention deficit hyperactivity disorder. World J Biol Psychiatry. 2011;12:99–109. doi: 10.3109/15622975.2010.512090. [DOI] [PubMed] [Google Scholar]
- 91.Imeraj L, Antrop I, Roeyers H, Swanson J, Deschepper E, Bal S, et al. Time-of-day effects in arousal: disrupted diurnal cortisol profiles in children with ADHD. J Child Psychol Psychiatry. 2012;53:782–9. doi: 10.1111/j.1469-7610.2012.02526.x. [DOI] [PubMed] [Google Scholar]
- 92.Isaksson J, Nilsson KW, Nyberg F, Hogmark A, Lindblad F. Cortisol levels in children with attention-deficit/hyperactivity disorder. J Psychiatr Res. 2012;46:1398–405. doi: 10.1016/j.jpsychires.2012.08.021. [DOI] [PubMed] [Google Scholar]
- 93.Kuppili PP, Pattanayak RD, Sagar R, Mehta M, Vivekanandhan S. Thyroid and cortisol hormones in attention deficit hyperactivity disorder: a case-control study. Asian J Psychiatr Aug. 2017;28(Aug):73–77. doi: 10.1016/j.ajp.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 94.Angeli E, Korpa T, Johnson EO, Apostolakou F, Papassotiriou I, Chrousos GP, et al. Salivary cortisol and alpha-amylase diurnal profiles and stress reactivity in children with attention deficit hyperactivity disorder. Psychoneuroendocrinology. 2018;90:174–81. doi: 10.1016/j.psyneuen.2018.02.026. [DOI] [PubMed] [Google Scholar]
- 95.Isik U, Bilgic A, Toker A, Kilinc I. Serum levels of cortisol, dehydroepiandrosterone, and oxytocin in children with attention-deficit/hyperactivity disorder combined presentation with and without comorbid conduct disorder. Psychiatry Res. 2018;261:212–9. doi: 10.1016/j.psychres.2017.12.076. [DOI] [PubMed] [Google Scholar]
- 96.Anesiadou S, Makris G, Michou M, Bali P, Papassotiriou I, Apostolakou F, et al. Salivary cortisol and alpha-amylase daily profiles and stress responses to an academic performance test and a moral cognition task in children with neurodevelopmental disorders. Stress Health. 2021;37:45–49. doi: 10.1002/smi.2971. [DOI] [PubMed] [Google Scholar]
- 97.Chang JP, Mondelli V, Satyanarayanan SK, Chiang YJ, Chen HT, Su KP, et al. Cortisol, inflammatory biomarkers and neurotrophins in children and adolescents with attention deficit hyperactivity disorder (ADHD) in Taiwan. Brain Behav Immun. 2020;88:105–13. doi: 10.1016/j.bbi.2020.05.017. [DOI] [PubMed] [Google Scholar]
- 98.Oades RD, Dauvermann MR, Schimmelmann BG, Schwarz MJ, Myint AM. Attention-deficit hyperactivity disorder (ADHD) and glial integrity: S100B, cytokines and kynurenine metabolism-effects of medication. Behav Brain Funct. 2010;6:29. doi: 10.1186/1744-9081-6-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Verlaet AAJ, Breynaert A, Ceulemans B, De Bruyne T, Fransen E, Pieters L, et al. Oxidative stress and immune aberrancies in attention-deficit/hyperactivity disorder (ADHD): a case-control comparison. Eur Child Adolesc Psychiatry. 2019;28:719–29. doi: 10.1007/s00787-018-1239-4. [DOI] [PubMed] [Google Scholar]
- 100.Darwish AH, Elgohary TM, Nosair NA. Serum Interleukin-6 level in children with attention-deficit hyperactivity disorder (ADHD) J Child Neurol. 2019;34:61–67. doi: 10.1177/0883073818809831. [DOI] [PubMed] [Google Scholar]
- 101.Chang JP, Mondelli V, Satyanarayanan SK, Chiang YJ, Chen HT, Su KP, et al. Cortisol, inflammatory biomarkers and neurotrophins in children and adolescents with attention deficit hyperactivity disorder (ADHD) in Taiwan. Brain Behav Immun. 2020;88:105–13. doi: 10.1016/j.bbi.2020.05.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.