Abstract
Brown recluse spiders, also known as Loxosceles reclusa, are endemic to the Southwest and Central Midwestern United States. A bite from this spider can cause a range of clinical manifestations, anywhere from a painless papular lesion to life-threatening reactions. We report a possible spider bite presenting as leukostasis initially suspected to be acute leukemia. A 22-year-old female patient presented to the emergency department with confusion and right upper arm pain, redness, and swelling after a suspected spider bite. Initial labs showed WBC count of 103.5x10e3/µL, hemoglobin of 3.3 g/dL, positive Direct Coombs’ test, creatinine of 1.8 mg/dL, transaminitis, and lactic acid of 20 mmol/L. Acute leukemia with leukostasis was suspected. She was started emergently on hydroxyurea in conjunction with prophylaxis for tumor lysis syndrome. However, peripheral smear showed left-shifted granulocytosis with lymphocytosis, monocytosis, and no blast cells or evidence of myelodysplasia. Bone marrow aspirate showed mildly hypercellular marrow with myeloid hyperplasia and no myelodysplasia. Flow cytometry analysis confirmed a left-shifted myeloid maturation pattern with 0.3% myeloblasts. BCR-ABL1 and JAK2 testing was negative. Hence, she had no evidence of leukemia but rather had leukostasis from a spider bite. Hydroxyurea was stopped and follow-up labs normalized. Sphingomyelinase D in the brown recluse spider venom is unique to Loxosceles and Sicarius and may be responsible for the unique clinical presentation of loxoscelism. The presentation of hyperleukocytosis complicated by shock with an unclear history poses a diagnostic challenge. In diagnostic uncertainty, consider delaying chemotherapy until a diagnosis can be confirmed to avoid potential harm.
Keywords: acute leukemia, brown recluse spider, hematologic emergency, leukostasis, loxoscelism
Introduction
Worldwide, there are more than 42 000 spider species. The tropics host the most incredible variety of spiders, housing nearly a quarter of the world’s 110 families of spiders. No one knows exactly how many different types of spiders exist in North America as our knowledge on this matter is incomplete. In 2019, a total of 3807 species of spiders had been found in the region. Florida has many tropical and subtropical species. California and Texas are large states with considerable topographic and climate variety; thus, it is not surprising that they host many spider species. Interestingly, nearly half of the species in North America never grow to more than 3 mm long (Figures 1-3).1
Figure 1.
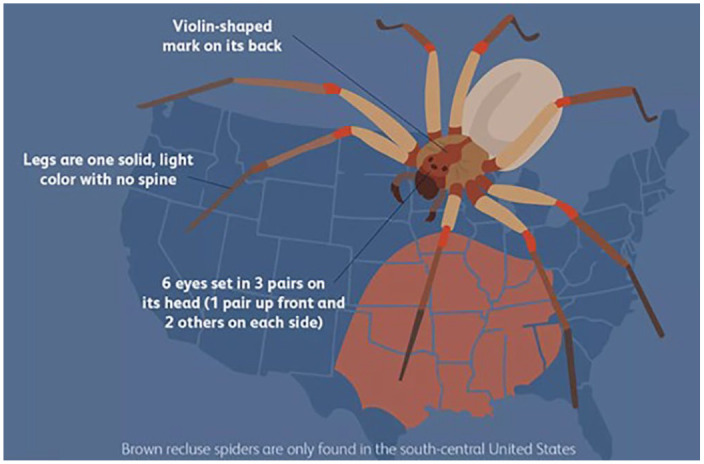
Brown recluse identifying marks and geographic range.
Figure 2.

Brown recluse spiders often have a fiddle-shaped marking.
Figure 3.

Male and female brown recluse.
Source: Common Spiders of North America, by Richard A. Bradley; 2012.1
Brown recluse spiders, also called Loxoscelesreclusa, are restricted to a group of states surrounding American southwest region including a vast area of Texas. They are notorious inhabitants of closets, attics, and basements.2 They usually attack only when they feel jeopardized or disturbed.
Identification
The 6 eyes are in 3 groups of 2; the center group is nearest the front. There is usually a dark violin-shaped mark on the front half of the cephalothorax. The “neck” of the violin is a dark line extending back from the cervical ridge to the back of the cephalothorax. The mark in the head region forms the “body” of the violin, its resemblance enhanced by a series of parallel rows of dark hair, the strings. The abdomen is without any contrast marking and is usually pale in females. The relatively long, thin legs are heavy.1
Several review articles in North America depict most cases to include adult female patients between 20 and 50 years of age during summer months.3 The range of skin manifestations can vary from a completely painless lesion with just a red plaque or papule to extremely painful necrotic lesions with subsequent ulceration and necrosis.4 The location of the bite can easily be misdiagnosed as a skin infection or cellulitis, especially early in the clinical phase when it lacks the typical appearance. Systemic symptoms are infrequent and may include malaise, nausea, and fever. Occasional serious life-threatening complications have also been described, including acute hemolytic anemia, disseminated intravascular coagulopathy, rhabdomyolysis, acute renal failure, shock, or even death in the pediatric population.5 Systemic loxoscelism is a term used to describe a systemic reaction following the Loxosceles reclusa bite. The evidence supporting the use of specific treatments, including antivenom, is lacking, and supportive care remains the mainstay of treatment.3
Hyperleukocytosis (white blood cell [WBC] count >100 × 109/L, or >100 × 103/µL) occurs commonly in leukemia and myeloproliferative disorders. Hyperleukocytosis often causes vascular occlusion and can result in ischemia, hemorrhage, and edema of the involved organs; hyperleukocytosis resulting in systemic complications is referred to as leukostasis. This problem is most commonly observed in acute myelogenous leukemia with high WBC counts. Individuals often clinically present with mental status changes, stroke, and renal or pulmonary insufficiency. If the neutrophil count exceeds 30 000/µL as a reaction to extrinsic factors, such as infection, it is referred to as a leukemoid reaction. We report a case of a severe systemic response to a suspected spider bite with profound hemolytic anemia, hyperleukocytosis, acute kidney injury, and severe lactic acidosis.
Case
A 22-year-old female with a history of asthma presented with lethargy, confusion, hematuria, and severe pain in the right arm (Figures 4 and 5). Nine days prior to admission, she developed pain and rash in her right arm in the mid humerus region after what she suspected to be an insect bite and stated her house was infested with spiders. She had incidentally presented to the emergency department (ED) a week prior to admission due to abdominal symptoms and pain in the right arm. At that time, her laboratory work was normal, and she was treated symptomatically. Finally, she was brought to the ED by her spouse due to lethargy, confusion, severe pain, and bloody urine. History taking was limited time as she had altered mental status and was writhing in pain. She was found to have abnormal laboratory test results: WBC 103.5 × 103/µL, hemoglobin 3.3 mg/dL, platelets 194 000/µL, international normalized ratio 1.35, D-dimer 2.22 mg/L, aspartate transaminase 3335 units/L and alanine transaminase 860 units/L, total bilirubin 9.8 mg/dL, creatinine 1.8 mg/dL, lactate dehydrogenase 3260 units/L, haptoglobin less than 10 mg/dL, fibrinogen 384 mg/dL, and lactic acid 20 mmol/L. Direct Coombs’ (antiglobulin) test was positive for IgG (immunoglobulin G) and complement, and creatine kinase was 1200 U/L with urinalysis revealing red urine, 2+ blood, and no red blood cells. Computed tomography scan of the right humerus revealed cellulitis without abscess formation or osteomyelitis. She was admitted to the intensive care unit with a possible diagnosis of acute leukemia with leukostasis and started on hydroxyurea, broad-spectrum IV (intravenous) antibiotics, and blood product transfusions.
Figure 4.

Right arm lesion at admission—presumed site of envenomation.
Figure 5.

Right arm lesion on day 4 of hospitalization—presumed site of envenomation.
Peripheral blood smear revealed granulocytosis with left shift, lymphocytosis, and circulating basophils with no blasts. Manual cell count showed segmented cells 61%, lymphocytes 19.7%, monocytes 2%, eosinophils 2%, metamyelocytes 5%, myelocytes 6%, promyelocyte 1%, and nucleated red blood cells 5/100 cells without schistocytes or Auer rods. Flow cytometry revealed a left-shifted myeloid maturation pattern with 0.3% myeloblasts. Bone marrow biopsy revealed a mildly hypercellular marrow, myeloid hyperplasia but no evidence of myelodysplasia and an estimated myeloid to erythroid ratio of 8:1 with the myeloid and erythroid series demonstrating normal maturation to completion without evidence of dysplasia and no aggregates of blasts, lymphocytes, or plasma cells. Cytogenetic studies for BCR-ABL1 and JAK2 polymerase chain reaction was negative.
In addition to a history of her home infested with spiders and reports of insect-bite lesions, it was speculated that the likely responsible insect was a brown recluse spider, which has been known to cause Coombs’ positive hemolytic anemia and cellulitis. It was supposed that she likely developed an acute hematological response with hyperleukocytosis to the insect bite leading to hemolysis, severe anemia, acute kidney injury, liver injury, and severe lactic acidosis. The hydroxyurea was stopped, and upon follow-up her laboratory test results normalized.
Discussion
Loxoscelism refers to both local and systemic effects of the brown recluse. The literature surrounding it is generally inadequate because of the lack of documentation of a confirmed spider bite, with only 7% to 14% of cases categorized as confirmed. The spider venom has 3 main enzymes, including Knottin, metalloproteases, and most notably sphingomyelinase D; the toxins expressed in lower quantities are hyaluronidase, a serine protease (serpin), and a translationally controlled tumor protein. The sphingomyelinase D in the brown recluse is unique to Loxosceles and Sicarius and is absent in all other spiders. The sphingomyelinase D may be responsible for the unique clinical presentation of loxoscelism.6 Sphingomyelinase D promotes hemolysis by stimulating erythrocyte activators of the complement system.7
Systemic manifestations typically occur 2 to 3 days following envenomation in contrast to the local skin lesion that may be evident by as early as 12 hours postinoculation.6 In our patient, her systemic symptoms started much sooner than the skin manifestation, which is quite unusual, as her skin lesion developed 9 days later and did not erupt until 11 days later. Of note, severity of skin manifestations does not necessarily correlate with the severity of systemic manifestations. The development of dermonecrosis has varied among studies, ranging from 40% to 70%. Only about 16% of cases of loxoscelism are complicated by hemolytic anemia. Overall, the majority of cases only develop local cutaneous manifestations.7,8 Due to the unusual skin lesion at the time of presentation, establishing the diagnosis was difficult. This is the first reported case of a spider bite causing hyperleukocytosis (WBC counts over 100 × 103/µL).
Several treatment options have been used in the treatment of loxoscelism, including antibiotics, steroids, antihistamines, dapsone, and blood product transfusions. While antibiotics may improve skin manifestations and prevent secondary cellulitis, limited evidence supports the use of other treatments due to conflicting evidence.6-11 This patient presented with leukostasis (symptomatic hyperleukocytosis) constituting a medical emergency, and efforts were made to rapidly stabilize the patient, lower the WBC count with hydroxyurea, and provide other supportive measures. However, the unusual presentation and the obscure history of spider-bite initially warranted additional workup to rule out other diagnoses such as acute leukemia. The role of leukapheresis is controversial and typically reserved for patients with symptomatic hyperleukocytosis who must have induction chemotherapy postponed and specifically in hematologic malignancies. Lack of blast cells in the peripheral smear and mostly mature neutrophils pointed against hematologic malignancy and diverted our thought process toward other underlying etiologies. Early recognition and management of atypical findings in brown recluse bites can be challenging to clinicians which may delay diagnosis. The patient was educated about the risks associated with spider bite and various ways to avoid future recurrence.
Conclusion
A recluse bite should be kept in the differential for any patient presenting with hemolytic anemia, leukostasis, atypical skin lesion, potential exposure to insect bite, and geographical location of the recluse itself. Antivenom and other targeted treatments have not been proven to be effective for loxoscelism. At present supportive measures remain the mainstay of therapy. Leukostasis may be challenging to differentiate from acute leukemia and other rare possible causes. However, early diagnostic exclusion may limit potential harmful treatments, and it may be reasonable to delay treatment until the diagnosis is confirmed.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed Consent: Informed consent was obtained from the patient for her anonymized information to be published in this article.
References
- 1.Bradley RA.Common Spiders of North America. University of California Press; 2012. [Google Scholar]
- 2.Rhoads J.Epidemiology of the brown recluse spider bite. J Am Acad Nurse Pract. 2007;19:79-85. [DOI] [PubMed] [Google Scholar]
- 3.Pauli I, Puka J, Gubert IC, Minozzo JC.The efficacy of antivenom in loxoscelism treatment. Toxicon. 2006;48:123-37. [DOI] [PubMed] [Google Scholar]
- 4.Dyachenko P, Ziv M, Rozenman D.Epidemiological and clinical manifestations of patients hospitalized with a brown recluse spider bite. J Eur Acad Dermatol Venereol. 2006;20:1121-1125. [DOI] [PubMed] [Google Scholar]
- 5.Sezerino UM, Zannin M, Coelho LK, et al. A clinical and epidemiological study of Loxosceles spider envenoming in Santa Catarina, Brazil. Trans R Soc Trop Med Hyg. 1998;92:546-548. [DOI] [PubMed] [Google Scholar]
- 6.Anoka IA, Robb EL, Baker MB.Brown Recluse Spider Toxicity. In: StatPearls; 2020. [PubMed] [Google Scholar]
- 7.Repplinger DJ, Hahn I.Arthropods. In: Nelson LS, Howland M, Lewin NA, Smith SW, Goldfrank LR, Hoffman RS, eds. Goldfrank’s Toxicologic Emergencies. 11th ed.McGraw-Hill; 2019. [Google Scholar]
- 8.Lopes PH, Squaiella-Baptistão CC, Marques MOT, Tambourgi DV.Clinical aspects, diagnosis and management of Loxosceles spider envenomation: literature and case review. Arch Toxicol. 2020;94:1461-1477. doi: 10.1007/s00204-020-02719-0 [DOI] [PubMed] [Google Scholar]
- 9.Paixão-Cavalcante D, van den Berg CW, Goncalves-de-Andrade RM, Fernandes-Pedrosa MDF, Okamoto CK, Tambourgi DV.Tetracycline protects against dermonecrosis induced by Loxosceles spider venom. J Invest Dermatol. 2007;127:1410-1418. [DOI] [PubMed] [Google Scholar]
- 10.Berger RS.The unremarkable brown recluse spider bite. JAMA. 1973;225:1109-1111. [PubMed] [Google Scholar]
- 11.Paixão-Cavalcante D, Van den Berg CW, de Freitas Fernandes-Pedrosa M, de Andrade RMG, Tambourgi DV.Role of matrix metalloproteinases in HaCaT keratinocytes apoptosis induced by Loxosceles venom sphingomyelinase D. J Invest Dermatol. 2006;126:61-68. [DOI] [PubMed] [Google Scholar]


