Learning objectives.
By reading this article you should be able to:
-
•
Discuss the pathophysiology of immersion pulmonary oedema.
-
•
Explain why cardiac disease increases the risk of immersion pulmonary oedema and decompression sickness.
-
•
Detail the risks of diving with respiratory diseases.
-
•
Define which patients with diabetes can dive.
-
•
Describe the risks of diving with epilepsy or other neurological and neuromuscular disorders.
Key points.
-
•
Immersion pulmonary oedema (IPO) is a major cause of death in scuba divers.
-
•
The incidence of IPO is increased in patients with hypertension and is greater in women than in men.
-
•
Intracardiac and pulmonary right-to-left shunts are important causes of decompression sickness.
-
•
Lung disease can predispose to pulmonary barotrauma and arterial gas embolism.
-
•
Divers must have adequate ventilatory capacity to be able to dive safely and to perform a diver rescue.
Introduction
In the first of our two linked articles on diving medicine we considered the effects of changes of pressure as a diver descends and ascends, with resulting changes in partial pressures of gas breathed and risks of toxic gas effects, decompression sickness (DCS) and barotrauma.1 This second article discusses some medical conditions that affect the ability to dive safely and the aetiology of immersion pulmonary oedema (IPO).
Medical assessment for diving requires the exclusion of diseases that would put a person at greatly increased risk of diving-related illnesses or would result in an increased risk to others who might have to conduct a rescue.
The demands of the type of diving being undertaken must also be considered. An amateur holiday dive for an hour in tropical waters is very different to commercial saturation diving at depths >100 m in the North Sea. A team of saturation divers typically lives for 4 weeks in a chamber pressurised to 11 atmospheres or more on a support ship. It takes a day to get to the bottom pressure as the mixture of breathing gases is gradually changed. Each day the divers lock into a diving bell and are lowered to near the site on the seabed where they will work. When working they have their breathing gas and hot water for their thermal undersuits supplied to them via an ‘umbilical’ (itself a risk factor in diving if it becomes entangled or cut). They are at risk of hypothermia because of long immersion and breathing a gas mixture that is mainly helium, which has a high thermal conductivity, so they are warmed to 32°C, even when in the living chamber. It takes 3 days or more (depending on the depth) to decompress to sea level at the end of the period of work or if a medical emergency occurs.
Cardiovascular disorders
If an average-sized adult is immersed up to the neck in warm water (therefore without cooling) the increased hydrostatic pressure on the legs immediately increases venous return.2 This increases central blood volume by about 700 ml, cardiac filling pressures by about 15 mmHg, and stroke volume by about 30%. The increase in heart size reduces lung volumes and causes release of natriuretic peptides. The resulting natriuresis and secondary diuresis continues until the cardiac filling pressures have returned to the normal level for that person. In cooler water, cold-induced vasoconstriction increases preload further and also raises afterload.
During head-out immersion, respiration is against continuous negative airway pressure equal to the vertical distance between the lung centroid and the water surface. Inspiration requires greater and expiration requires less effort. The vertical distance of the lung centroid below the surface is greater when standing upright than when swimming in a horizontal position, but inspiration always requires an increased negative pressure. If a swimmer breathes out with their head underwater, the expiratory pressure may be positive relative to the lung centroid.
In a submerged scuba diver, the vascular effects are comparable, but the effects of breathing may differ, depending on the type of equipment used by the diver and their attitude in the water.
In a scuba diver using open circuit, the demand valve delivers breathing gas at ambient pressure at the diver's mouth. When the diver is head up in the water when ascending, the diver breathes with an increased negative pressure during all phases of respiration, similar to an individual who is head-out immersed. When head down whilst descending, the diver breathes against CPAP. When swimming horizontally, the mouth is at approximately the same level as the lung centroid; thus, there is little pressure differential.
A closed-circuit rebreather, used by some divers, is analogous to ultra-low flow in an anaesthetic circle circuit. The diver breathes via a closed circuit from a gas reservoir, termed a counter-lung. The carbon dioxide in the expired gas is removed chemically and the decrease in oxygen partial pressure is measured by oxygen sensors and replenished from an oxygen cylinder. The vertical distance between the counter-lung and the diver's lung centroid determines whether the diver is breathing with a negative or positive airway pressure. When a diver is using a back-mounted counter-lung swimming horizontally in the prone position, so that the counter-lung is above the lungs, respiration is with continuous negative airway pressure. When the counter-lung is mounted on the front of the chest, there is CPAP when the diver is prone.
The work of breathing is also affected by gas density. Density of a gas increases with depth in proportion to the absolute pressure and maximum voluntary ventilation decreases in proportion to the square root of density (and absolute pressure). Therefore, at a depth of 30 m (4 bar, 405.2 kPa, 3040 mmHg) air is four times as dense as at the surface (1 bar, 101.3 kPa, 760 mmHg) and maximum voluntary ventilation is half that at the surface.
Immersion pulmonary oedema
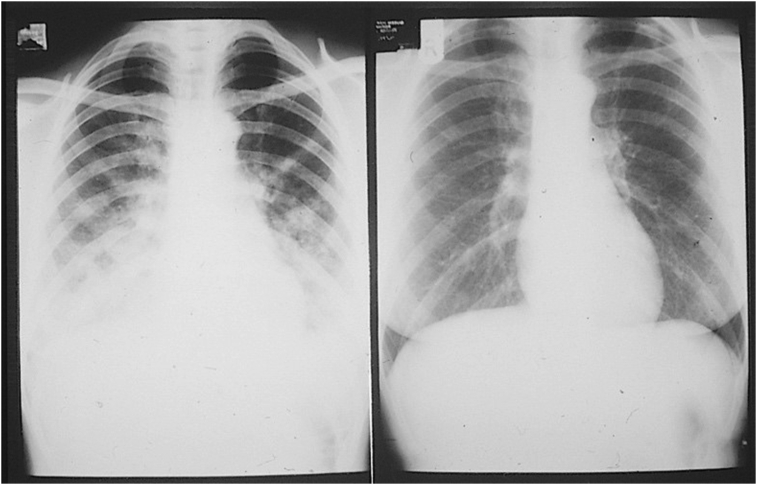
Immersion pulmonary oedema occurs in surface swimmers and divers as a result of the increase in pulmonary capillary pressure and the reduction of airway pressures caused by immersion (Fig. 1).3,4 It is exacerbated by additional increases in pulmonary capillary pressure as a result of cold-induced vasoconstriction with consequent centralisation of blood volume, and by exertion.3
Fig 1.
Chest X-rays from 1977 of the first diver reported to have immersion pulmonary oedema. The left panel shows her X-ray shortly after she surfaced with dyspnoea and frothy haemoptysis. By the time the X-ray was taken she was already feeling better and she refused treatment. A repeat chest X-ray 4 weeks later was normal (right panel). She said that she had had six previous episodes. Cardiac investigations were normal, but she later developed hypertension.
Immersion pulmonary oedema is a leading cause of death in scuba divers. When deaths from equipment failure and diver error are excluded, IPO is probably the most common medical cause of diving deaths. Immersion pulmonary oedema is well described in fit individuals including the special forces and navy divers of many countries. The Israeli Defence Force reported that 70 recruits (aged 18–19 yrs) developed IPO during swimming trials in a 3-yr period (1.8% of trials).5 When recruits drank 5 L of liquid in the 2 h before their swim, eight of 30 developed IPO.6
In the 2016 Vansbro river swimming race in Sweden, 69 of 13,878 (0.5%) had symptoms varying from cough to fulminating pulmonary oedema and 46 were treated with CPAP.7 A total of 58 (84%) of those affected were women. Unfortunately, no breakdown is given of the numbers of women and men participating in the race, but many reports show that IPO occurs considerably more frequently in women than men: the reason for the difference is not known.
The continuous negative airway pressure when divers use rebreathers with back-mounted counter-lungs means that they are at increased risk of IPO. Rebreathers are favoured by military divers because the absence of bubble liberation reduces the probability of detection during a combat swim, but even fit special forces and navy divers are reported to develop IPO when using rebreathers, particularly when they had back-mounted counter-lungs.8 Research in French Navy divers showed that the lung comet score, a grading of interstitial pulmonary oedema, was much increased in prone divers when exercising whilst breathing from a back-mounted counter-lung compared with those exercising using a front-mounted counter-lung or at rest.9
However, IPO is most frequent in amateur divers older than 50 yrs, particular those with hypertension.3 They have higher baseline pulmonary capillary pressures before entering the water, so that the further increases in pulmonary capillary pressure and the negative airway pressures that occur during immersion tip them into IPO.
Immersion pulmonary oedema recurs, particularly in people who are hypertensive, so those who have had one episode of IPO should not dive again unless the factors causing the IPO in that person are removed.3,4
Other cardiovascular diseases and diving
As described in the first article,1 divers with a right-to-left shunt have an increased risk of DCS after unprovocative dives provided the dive is deep enough and long enough to liberate venous gas bubbles.10, 11, 12 Therefore individuals who have a right-to-left shunt (e.g. cyanotic congenital heart disease, atrial septal defect or a known pulmonary arteriovenous malformation) generally should not dive. Those who might have a right-to-left shunt (e.g. history of cryptogenic stroke at a young age, which is often associated with a large persistent foramen ovale) need careful assessment and advice if they wish to dive.13
Individuals should not dive if they have cardiac disease that might result in incapacity underwater (e.g. serious arrhythmias and coronary artery disease), or may increase the risk of IPO (e.g. cardiomyopathy, significant left heart valve disease), or may increase the risk of DCS (e.g. atrial septal defects, cyanotic heart disease).
Respiratory disorders
The diving physician should ask ‘Does the diver have the necessary ventilatory capacity to carry out diving and a diving rescue safely and is there disease that would increase the risk of pulmonary barotrauma?’
On the surface, a diver must be able to maintain a good exercise level because when submerged, the situation will alter radically.14 The effects of immersion, increased gas density with depth, the constraints of the diving suit and the mechanical resistance associated with breathing equipment conspire to reduce the maximum voluntary ventilation by 50% when at 30 m. Assuming a o2 requirement of about 2.5 L min−1 to swim against a current of 1.2 knots, then on the surface, the minute ventilation required to maintain this would be 75 L min−1; this presents little problem for most people who are reasonably fit: at 30 m underwater, essentially normal pulmonary function is required to maintain the same level of oxygen uptake. With abnormal pulmonary function, the work required to maintain normocapnia when breathing the more dense gas at depth may become excessive.
Common respiratory problems such as asthma and chronic obstructive pulmonary disease (COPD) affect the ventilation/perfusion patterns in the lung, thereby interfering with the efficiency of gas exchange and the possibility of gas trapping in areas of the lung which have an increased gas emptying time. (Note that if an area of lung is completely closed off to gas exchange, the gas in that area will be slowly absorbed).
Theoretical physiological considerations have meant that most diving physicians do not allow people with asthma to dive. However, population surveys of divers show that provided asthma is well-controlled with a combination of one or more inhaled steroids, long-acting β2 agonists, or leukotriene receptor antagonists, diving is safe. In the UK it is recommended that a diver with asthma should measure his or her peak flow daily and must not go diving if peak flow is >15% below their best value when well.
Individuals with a current chest infection should temporarily avoid diving until there is complete recovery.
A history of spontaneous pneumothorax has been considered to be a bar to diving. Occurring mainly in fit young men, the condition frequently recurs if left untreated. Rupture of a bulla underwater may lead to tension pneumothorax, especially on the ascent, or to arterial gas embolism when gas from the bulla invades a pulmonary vein. Pleural stripping or pleurodesis to remove the apical congenital bullae that are usually the cause of the problem may allow the person to dive again, but this is controversial.
Conditions such as sarcoidosis or active tuberculosis will preclude diving until treated. Clinically significant COPD and untreated lung cancer preclude diving altogether.
At present, smokers are permitted to dive, though there is evidence that they have an increased risk of arterial gas embolism caused by pulmonary barotrauma on ascent, even when their spirometry is normal.12,15
Diving for older (aged >65 yrs) and younger people (aged <18 yrs)
Some 49% of people in England aged > 65 yrs take at least five different medications per day. Cardiovascular drugs are the most frequent medication and may indicate diseases that make a person unfit to dive. β-Adrenoceptor antagonists may limit the ability of the heart to respond maximally to exercise. Vasodilating antihypertensive drugs, such as calcium channel blockers and angiotensin-converting enzyme/angiotensin II inhibitors may be acceptable in divers, because they can reduce the risk of IPO. Decreased fitness and reduced muscle mass may prove problematic if the diver has to carry heavy cylinders of breathing gas and weights. Nonetheless, a few people continue diving into their ninth and tenth decades without mishap.
Young people learning to dive is an emotive issue. Occasionally parents request a medical for children as young as 7–8 yrs of age. Physicians need to be cautious in assessing whether a child really understands the risks and wishes to dive, because some requests are the result of parental pressure. Any child who expresses the wish to dive before the age of puberty must have their mental capacity to cope with the demands of a diving incident carefully assessed. A few cases of decompression illness in young teenagers leading to permanent disability have been reported.16 However, most children with responsible adults as buddies will enjoy the freedom and excitement of diving and it is good exercise.
Women and diving
Women scuba divers compose about 27% of UK divers. There are some sex-related physiological differences that are important for diving. Women have a greater percentage of body fat and less muscle mass than men. Therefore female divers may have more difficulty in carrying and lifting their diving equipment but may have some protection against hypothermia. Women have an increased incidence of IPO, but the reason is not known.
There is evidence that the incidence of DCS is increased in women in the first week of the menstrual cycle and that the oral contraceptive may be protective during this time.17 A similar association has been found in US Air Force personnel who were exposed to hypobaric conditions.18 The reason is unclear, but it is probably hormonal.
Diving during pregnancy is very controversial, because of concerns that it may adversely affect the fetus. Many women have dived being unaware that they are pregnant until they later missed a period. It is during this early stage that fetal organogenesis and lateralisation occurs. The observational studies on pregnant women who continued diving are subject to bias. Therefore it is still unclear whether normal diving profiles (which do not involve prolonged periods of decompression or rapid ascents) increase the incidence of fetal abnormalities. Current advice is that women who are planning to become pregnant should not dive, but if a woman discovers that she is pregnant and has been diving, it is not an indication for termination of pregnancy.
Breast implants may absorb nitrogen during diving, but provided rapid decompression is avoided, tissue trauma as a result of the increased volume of the implants does not occur.
Endocrine disorders
Four endocrine disorders are fairly common in potential divers: diabetes mellitus (types I and II), hypothyroidism and hyperthyroidism.
Before 1991, no individual with diabetes was allowed to dive, a worldwide restriction. Since then, the restrictions have relaxed thanks to research and improved medications.19 Divers with diabetes must maintain good control of their diabetes, have no long-term diabetic complications and have annual medical examinations by a diving medical referee. They must also measure their blood glucose immediately before and after each dive if they are taking drugs with the potential to cause hypoglycaemia and carry an emergency kit to treat hypoglycaemia.20
Hypoglycaemia underwater was a major concern for divers with type I diabetes. Such concerns were allayed because fit, healthy divers who have diabetes do not get hypoglycaemia even when strenuously exercising, provided their blood glucose concentrations are slightly increased before diving.19
Some people who have type I diabetes control their blood glucose levels using an insulin pump. Insulin pumps should not be used when diving. Cold and skin pressure (from a wetsuit) may lead to unreliable insulin absorption and no insulin pump has been certified for use under pressure.
People with type II diabetes have a much lower risk of hypoglycaemia underwater. Their main risks are from long-term complications of diabetes (cardiac, neurological, renal). It is estimated that the onset of type II diabetes occurs 4–6 yrs before diagnosis, thus allowing complications to develop.21
People with hypothyroidism and hyperthyroidism can dive provided their symptoms and thyroid status are well controlled.
Neurological disorders
Neurological diseases that significantly increase risk when diving are contraindications. The risks are obvious for some diseases.
Grand mal epilepsy causes a risk of unconsciousness and hence drowning, particularly at depths where high partial pressures of oxygen reduce the threshold for convulsions. In the UK, people with epilepsy must not dive unless they have been free of fits and not taking anticonvulsant medications for >5 yrs, when the risk of a convulsion during a dive is considered to be acceptably low.
Muscle weakness, resulting from impaired central motor control, neuropathy or muscular dystrophy, which impairs the ability to swim or breathe on the surface or under water, is also a contraindication to diving. Sometimes important muscle weakness only becomes apparent when an individual starts diving. For example, diaphragmatic paralysis secondary to phrenic nerve palsy can result in severe breathlessness at the surface because the hydrostatic pressure difference between the abdomen and the mouth results in the diaphragm being pushed up into the chest, thereby reducing lung volumes.
Impaired coordination may cause difficulty using equipment, as can impairment of touch sensation, particularly when visibility is severely impaired, as it often is in UK waters. A diver also needs adequate vision to read their gauges.
The incidence of neurological DCS is greatly increased in people with migraine with aura.22 That is because the prevalence of clinically significant right-to-left shunts (across persistent foramen ovale or pulmonary shunts) is approximately 40% in people with migraine with aura compared with 5% in those without migraine with aura.11,22 As stated previously, right-to-left shunts facilitate DCS as a result of paradoxical gas embolism.12,13 Investigations to exclude a significant shunt should be considered in potential divers with a history of migraine with aura.13
Another consideration is whether the manifestations of neurological disease will interfere with diagnosis and treatment if the diver develops neurological DCS after a dive. For example, if a diver with a history of transient ischaemic attacks becomes hemiplegic soon after a dive, the differential diagnosis is another cerebral thromboembolic event or cerebral DCS or cerebral arterial gas embolism secondary to pulmonary barotrauma.
If a diver with pre-existing neurological disease develops neurological DCS, the resulting deficit may be greater. That is particularly so when the diver has spinal disease because the addition of spinal DCS could result in serious disability. In addition, a recompression chamber may continue to treat for residual clinical signs that are not the result of DCS, but are attributable to the prior disease.
However, there are some individuals who dive with serious neurological disability, such as paraplegia, within disabled diver schemes. It is recognised that these divers gain considerable freedom in underwater weightlessness. They are carefully assessed before diving, have restrictions on the diving they can undertake and are cared for underwater by two or more experienced dive buddies.
Serious psychiatric diseases are a contraindication to diving, particularly when they might impair judgement or result in panic if difficulties arise during a dive.
There are concerns that many drugs used to treat neurological and psychiatric diseases adversely potentiate the risk of nitrogen narcosis. In many cases, the concerns are based on theoretical considerations, but some are known to present hazards that will limit the depth to which an individual can dive.
Summary
When diving, the underwater environment and particularly the increased ambient pressure, places unique demands on human physiology, which can cause diving-related diseases with life-threatening consequences. Therefore, it is important to ensure that those with medical conditions that put them at significantly increased risk do not dive.
Declaration of interests
The authors declare that they have no conflicts of interest.
Biographies
Chris Edge PhD AFOM FRCA CChem Cert GStat is a consultant anaesthetist at the Royal Berkshire Hospital and an honorary senior lecturer at the Department of Life Sciences, Imperial College, London. He is past chair of the UK Diving Medical Committee. He is statistical editor of Diving and Hyperbaric Medicine. His major clinical interests are anaesthesia for robotic surgery and research in diabetes in diving medicine. His non-clinical interests include biostatistics.
Peter Wilmshurst BSc FRCP FISM FFSEM is a consultant cardiologist at the Royal Stoke University Hospital and a past chair of the UK Diving Medical Committee. He has conducted research in diving medicine for more than 40 yrs. He was the first to report the role of right-to-left shunts in decompression illness and the first to describe immersion pulmonary oedema in divers and swimmers.
Matrix codes: 1A01, 1A03, 2B01, 3J00
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bjae.2021.05.002.
MCQs
The associated MCQs (to support CME/CPD activity) will be accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Edge CJ, Wilmshurst PT. The pathophysiologies of diving diseases. BJA Educ 21;9. [DOI] [PMC free article] [PubMed]
- 2.Arborelius M., Balldin U.I., Lilja B., Lundgren C.E.G. Hemodynamic changes in man during immersion with the head above water. Aerosp Med. 1972;43:592–598. [PubMed] [Google Scholar]
- 3.Wilmshurst P.T., Nuri M., Crowther A., Webb-Peploe M.M. Cold-induced pulmonary oedema in scuba divers and swimmers and subsequent development of hypertension. Lancet. 1989;1:62–65. doi: 10.1016/s0140-6736(89)91426-8. [DOI] [PubMed] [Google Scholar]
- 4.Wilmshurst P.T. Immersion pulmonary oedema: a cardiological perspective. Diving Hyperbar Med. 2019;49:30–40. doi: 10.28920/dhm49.1.30-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adir Y., Shupak A., Gil A. Swimming-induced pulmonary edema: clinical presentation and serial lung function. Chest. 2004;126:394–399. doi: 10.1378/chest.126.2.394. [DOI] [PubMed] [Google Scholar]
- 6.Weiler-Ravell D., Shupak A., Goldenberg I. Pulmonary oedema and haemoptysis induced by strenuous swimming. BMJ. 1995;311:361–362. doi: 10.1136/bmj.311.7001.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eriksson A.B., Hardstedt M. 2017. The “Vansbrosimningen” experience – incidence of swimming induced pulmonary edema (SIPE) and organization of prehospital medical resources. Scienta et Valebrat IV.http://sanma.se/resources/Scientia-et-Valebat-IV-2017.pdf Available from: [Google Scholar]
- 8.Gempp E., Louge P., Blatteau J.E., Hugon M. Descriptive epidemiology of 153 diving injuries with rebreathers among French military divers from 1979 to 2009. Mil Med. 2011;176:446–450. doi: 10.7205/milmed-d-10-00420. [DOI] [PubMed] [Google Scholar]
- 9.Castagna O., Regnard J., Gempp E. The key role of negative pressure breathing and exercise in the development of interstitial pulmonary edema in professional male scuba divers. Sports Med Open. 2018;4:1. doi: 10.1186/s40798-017-0116-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilmshurst P.T., Byrne J.C., Webb-Peploe M.M. Relation between interatrial shunts and decompression sickness in divers. Lancet. 1989;2:1302–1306. doi: 10.1016/s0140-6736(89)91911-9. [DOI] [PubMed] [Google Scholar]
- 11.Wilmshurst P.T. The role of persistent foramen ovale and other shunts in decompression illness. Diving Hyperbar Med. 2015;45:98–104. [PubMed] [Google Scholar]
- 12.Wilmshurst P., Bryson P. Relationship between the clinical features of neurological decompression illness and its causes. Clin Sci. 2000;99:65–75. [PubMed] [Google Scholar]
- 13.Smart D., Mitchell S., Wilmshurst P., Turner M., Banham N. Joint position statement on persistent foramen ovale (PFO) and diving. South pacific underwater medicine society (SPUMS) and United Kingdom sports diving medical committee (UKSDMC) Diving Hyperb Med. 2015;45:129–131. [PubMed] [Google Scholar]
- 14.Neuman T.S. Pulmonary fitness for diving. In: Lundgren C.E., Miller J.N., editors. The lung at depth. Marcel Dekker Inc; New York: 1999. pp. 73–90. [Google Scholar]
- 15.Wilmshurst P.T., Davidson C., O’Connell G., Byrne C. Role of cardiorespiratory abnormalities, smoking and dive characteristics in the manifestations of neurological decompression illness. Clin Sci. 1994;86:297–303. doi: 10.1042/cs0860297. [DOI] [PubMed] [Google Scholar]
- 16.Newton H.B., Padilla W., Burkart J., Pearl D.K. Neurological manifestations of decompression illness in recreational divers – the Cozumel experience. Undersea Hyperb Med. 2007;34:349–357. [PubMed] [Google Scholar]
- 17.Lee V., St Leger Dowse M., Edge C. Decompression sickness in women: a possible relationship with the menstrual cycle. Aviat Space Environ Med. 2003;74:1177–1182. [PubMed] [Google Scholar]
- 18.Rudge F.W. Relationship of menstrual history to altitude chamber decompression sickness. Aviat Space Environ Med. 1990;61:657–659. [PubMed] [Google Scholar]
- 19.Edge C.J., Grieve A.P., Gibbins N. Control of blood glucose in a group of diabetic scuba divers. Undersea Hyperb Med. 1997;24:201–207. [PubMed] [Google Scholar]
- 20.Edge C.J., St Leger Dowse M. Diving with diabetes – the British data. In: Pollock N.W., Uguccioni D.M., Dear GdeL., editors. Diabetes and recreational diving: guidelines for the future. Proc undersea hyperbar med soc/divers alert network 2005 june 19 workshop. Divers Alert Network; Durham, NC: 2005. [Google Scholar]
- 21.Porto M., Curletto G., Cipullo D. Estimating the delay between onset and diagnosis of type 2 diabetes from the time course of retinopathy prevalence. Diabetes Care. 2014;37:1668–1674. doi: 10.2337/dc13-2101. [DOI] [PubMed] [Google Scholar]
- 22.Wilmshurst P., Nightingale S. Relationship between migraine and cardiac and pulmonary right-to-left shunts. Clin Sci. 2001;100:215–220. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.