Abstract
Objective
To investigate the relationship between late-life duration of poverty exposure and cognitive function and decline among older adults in China.
Methods
Data were from 3,209 participants ≥64 years of age in the Chinese Longitudinal Healthy Longevity Survey (CLHLS). Duration of poverty, defined according to urban and rural regional standards from the China Statistical Yearbook, was assessed according to annual household income from 2005 to 2011 (never in poverty; one-third of the period in poverty; two-thirds or more of the period in poverty). Cognitive function was measured by the Chinese Mini-Mental State Examination (CMMSE) from 2011 to 2018. We used attrition-weighted, multivariable mixed-effects Tobit regression to examine the association of duration of poverty with cognitive function and rate of decline.
Results
A total of 1,162 individuals (36.21%) were never in poverty over the period from 2005 to 2011; 1,172 (36.52%) were in poverty one-third of the period; and 875 (27.27%) were in poverty two-thirds or more of the period. A longer poverty duration was associated with lower subsequent CMMSE scores with a dose-response relationship (one-third vs never in poverty: β = −0.98; 95% confidence interval −1.61 to −0.35; two-thirds or more vs never in poverty: β = −1.55; 95% confidence interval −2.29 to −0.81). However, a longer duration of poverty was associated with a slower rate of CMMSE score decline over time from 2011 to 2018.
Conclusion
These findings provide valuable evidence for the role of cumulative late-life poverty in relation to cognitive health among older adults in a rapidly urbanizing and aging middle-income country. Our findings may support a compensation hypothesis for cognitive reserve in this setting.
More than 50 million people are living with Alzheimer disease and related dementias (ADRD) worldwide, and this number is expected to triple by 2050.1 Maintaining cognitive function is thus crucial for extending the health and well-being of older adults in the context of population aging. Although the association of absolute income measured at a single point in time in relation to ADRD and related outcomes has been well documented,2,3 emerging research has directed attention to longitudinal income trajectories as a potentially salient exposure in ADRD etiology.4-9 For example, sustained poverty over a 15-year period in midlife has been associated with subsequent cognitive function among US adults.6 Other studies have focused on socioeconomic trajectories in childhood, early adulthood, and midlife in relation to cognitive health outcomes.7,10,11
The effects of later-life income trajectories on cognitive outcomes are understudied, resulting in a loss of life-course exposure information on the role of income in ADRD etiology. Nearly all existing studies have focused on high-income countries, where absolute poverty (household income below the level needed to meet basic life necessities) is uncommon.12 There is limited research from low- and middle-income countries13 such as China, which has a large, rapidly aging population and a higher rate of absolute poverty than high-income countries.14,15 Moreover, intergenerational financial exchange is common in China whereby older adults often receive financial support from their adult children, and financial assistance from older parents to financially worse off adult children is also common.16,17 This practice of intergenerational financial exchange increases income volatility among older adults in China.16,17
We aimed to investigate the relationships between duration of poverty over a 6-year period (2005–2011) with cognitive function and decline over a subsequent 7-year period (2011–2018) among adults ≥64 years of age in China. We hypothesized that (1) a longer duration of poverty in later life would be associated with a lower level of cognitive function and that (2) a longer duration of poverty in later life would be associated with a faster subsequent rate of cognitive decline.
Methods
Data Source, Study Design, and Study Sample
Data were from the Chinese Longitudinal Healthy Longevity Survey (CLHLS).18 The CLHLS is an open, nationally representative cohort study that has included >20,000 individuals from 22 provinces in mainland China, with sampling areas covering > 85% of the Chinese population.18 The CLHLS is jointly administered by Duke University and Peking University. The CLHLS was launched in 1998 and conducted follow-up interviews in 2000, 2002, 2005, 2008, 2011, 2014, and 2018, with a response rate >90% for each wave.18 The first 2 waves focused on individuals >80 years of age. Individuals 64 to 80 years of age were enrolled beginning in 2002, and those 40 to 59 years of age were enrolled beginning in 2008. Participants or proxy respondents (usually a spouse or close family member) were asked to self-report information on sociodemographic factors, including sex, ethnicity, lifestyle, disease history, etc. Proxy interviews were conducted for respondents who were too impaired to directly participate in study interviews. Very few participants had full proxy interviews in any given wave (<1% of those <90 years of age, ≈1.5% of those 90 to 99 years of age, <5% of those 100–105 years of age).18 Prior research has ruled out substantial bias due to proxy interviews in the CLHLS.18
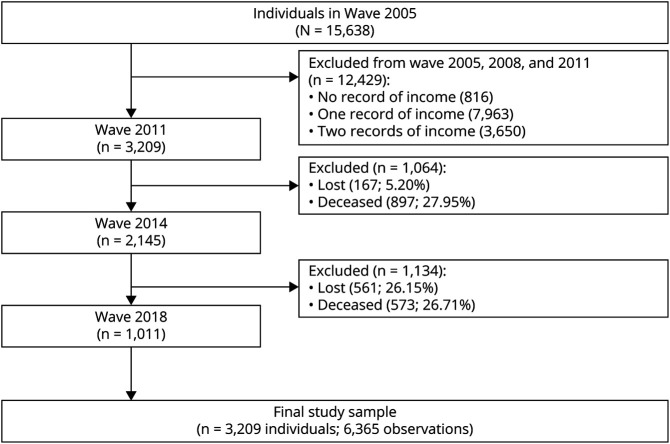
The present study used a longitudinal design among CLHLS participants ≥64 years of age in 2005, with exposure to poverty assessed from 2005 to 2011 and cognitive function assessed from 2011 to 2018. After the exclusion of individuals without all 3 income observations from 2005 to 2011, we included 3,209 individuals ≥64 years of age who contributed 6,365 cognitive function observations from 2011 to 2018 (figure 1).
Figure 1. Sample Collection.
All participants who survived and remained in the Chinese Longitudinal Healthy Longevity Survey (CLHLS) study or their proxies were directly asked about annual household income. There was a missing rate of 8.83% for income data in the 2005–2011 CLHLS dataset. We excluded participants without complete income data from 2005 to 2011 (those with missing income data in any year of 2005, 2008, and 2011 and those who died or who were lost to follow-up before 2011).
Measures
Exposure: Duration of Poverty From 2005 to 2011
In urban regions in China, the mean annual household income of the lowest income group (bottom quintile of the population income distribution) was 4,290 Chinese yuan renminbi (CNY) (≈US $613) in 2005, 6,560 CNY (≈US $937) in 2008, and 9,785 CNY (≈US $1,398) in 2011. In rural regions, the mean annual household income of the lowest income group was 2,090 CNY (≈US $299) in 2005, 3,072 CNY (≈US $439) in 2008, and 4,421 CNY (≈US $632) in 2011. These population income data are from China Statistical Yearbook published by the National Bureau of Statistics of China and are available from Dryad (table e-1: doi.org/10.5061/dryad.vhhmgqnsk) and online at stats.gov.cn. We defined duration of poverty as the proportion of CLHLS time points from 2005 to 2011 that an individual's household income was below the mean annual income of the bottom quintile income group for that region. The bottom quintile of the population income distribution is defined as the low-income group by the China Statistical Yearbook. We did not use the national absolute poverty line in China in this study because the national poverty line does not account for income and cost of living differences between urban and rural regions. We classified a 3-level variable for the duration of poverty over this period: never in poverty (0 time points), one-third of the time in poverty (1 time point), and two-thirds or more of the time in poverty (2 or all 3 time points).
Outcome: Cognitive Function From 2011 to 2018
Cognitive function was measured in 2011, 2014, and 2018 with the Chinese Mini-Mental State Examination (CMMSE).19 The CMMSE has been validated and used in prior studies.20,21 The CMMSE consists of 24 items across 7 cognitive domains: 5 items for Orientation, 3 items for Registration, 1 item for Naming foods, 5 items for Attention and Calculation, 1 item for Copying a Figure, 3 items for Recall, and 6 items for Language.21 The overall CMMSE scores range from 0 to 30, with higher scores indicating better cognitive function.
Covariates
Covariates were assessed at baseline in 2005 (before income and CMMSE measures) and included sociodemographic characteristics, lifestyle behaviors, and comorbid disease history.6,7 Sociodemographic characteristics were age (in years), sex (female; male), ethnicity (Han; other), marital status (married; widowed; other), and years of schooling. Lifestyle behaviors were smoking history (yes; no), regular physical activity (yes; no), and body mass index (categories of <18.5; 18.5–24.9; 24.9–29.9; >29.9 kg/m2). Self-reported disease history included hypertension (yes; no), diabetes (yes; no), stroke (yes; no), and cardiovascular disease (yes; no).
Statistical Analysis
All statistical analyses were performed with Stata/SE 15.0 (StataCorp, College Station, TX).
Data Imputation
A total of 3,302 observations (51.87%) in our analytic sample over the follow-up period from 2011 to 2018 had missing CMMSE items. Consistent with previous CLHLS analyses using the CMMSE scores, we performed multiple imputation by chained equations on the CLHLS 2005–2018 dataset to impute values for missing CMMSE items.22 Multiple imputation by chained equations is a sequential multivariate regression imputation approach conditional on observed variables as predictors.23 To increase accuracy and to make the missing-at-random assumption more tenable, we conducted item-level imputation using all variables in the final analytic models and produced 5 imputed datasets.7,11,24 We then computed the overall CMMSE scores after item-level imputation.24,25
Primary Analyses
We compared baseline characteristics of the study sample according to duration of poverty using Pearson χ2 tests, analysis of variance, and Kruskal-Wallis rank-sum tests. To account for the ceiling effects of CMMSE scores, we conducted multivariable-adjusted mixed-effects Tobit regression models to examine the association between duration of poverty and subsequent CMMSE scores. Tobit regression, also referred to as censored or truncated regression, assumes that the observed range of the dependent variable y is either left- or right-censored (as with a ceiling effect) and represents an unmeasured latent variable, y*, such that we observe only y = max (0, y*).26,27 The Tobit model modifies the maximum likelihood estimator to estimate the effect of x on the uncensored latent variable y*, where  .26,27 We conducted 3 sets of sequential models. Model set 1 was adjusted for age, sex, race, and marital status (demographic adjustment); model set 2 was additionally adjusted for years of schooling (demographic and education adjustment); and model set 3 was additionally adjusted for all lifestyle behavior and comorbid disease variables (fully adjusted). We included statistical interaction terms between year and duration of poverty to investigate whether duration of poverty was related to rate of change in CMMSE scores over time.
.26,27 We conducted 3 sets of sequential models. Model set 1 was adjusted for age, sex, race, and marital status (demographic adjustment); model set 2 was additionally adjusted for years of schooling (demographic and education adjustment); and model set 3 was additionally adjusted for all lifestyle behavior and comorbid disease variables (fully adjusted). We included statistical interaction terms between year and duration of poverty to investigate whether duration of poverty was related to rate of change in CMMSE scores over time.
To account for any potential bias that could be introduced due to selective attrition or mortality over the follow-up, we generated wave-specific inverse probability weights (IPWs) that jointly incorporated the probabilities of survival and remaining in the study.28,29 Full methodologic details for the creation of the weights are provided in Dryad (e-Methods and tables e-2 and e-3: doi.org/10.5061/dryad.vhhmgqnsk).
Sensitivity Analysis
We performed 3 sensitivity analyses. First, we repeated the modeling analyses with the IPWs trimmed at the 99th percentile (5.31) to exclude any potential outsized effects of the few IPW outliers. Second, to rule out potential reverse causality whereby individuals with preexisting poor cognitive function may be more likely to experience sustained poverty, we repeated the modeling analyses restricted to individuals with CMMSE scores >28 at baseline in 2005. Finally, we repeated the modeling analyses using the dataset without imputed values of CMMSE scores to compare against the results with imputation.
Standard Protocol Approvals, Registrations, and Patient Consents
The CLHLS was approved by the ethics committee of the Peking University (IRB00001052–13074). Written informed consent was obtained from all participants before the investigation.
Data Availability
All data from the CLHLS are publicly available at sites.duke.edu/centerforaging.
Results
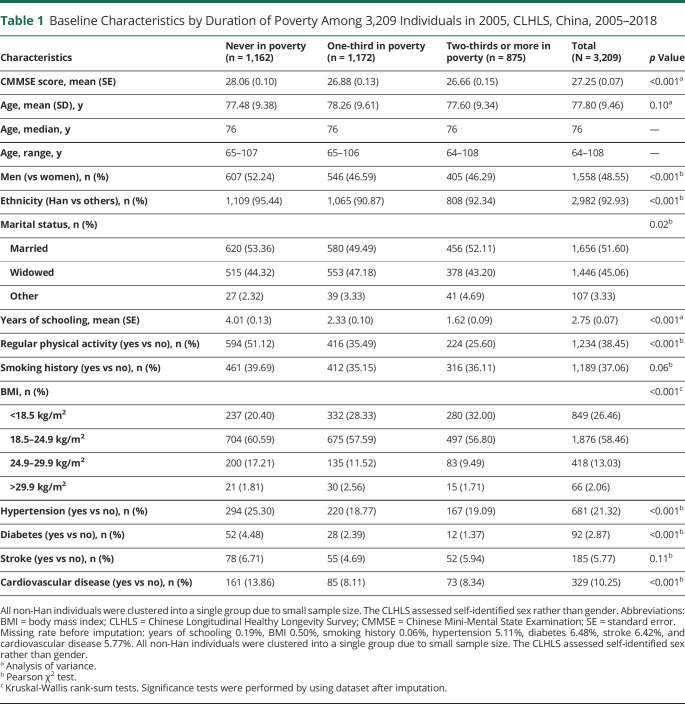
Table 1 presents baseline characteristics of the study sample. A total of 1,162 individuals (36.21%) were never in poverty over the period from 2005 to 2011; 1,172 individuals (36.52%) were in poverty one-third of the time during this period; and 875 individuals (27.27%) were in poverty two-thirds of the time or more during this period (table 1). Individuals who were in poverty one-third and two-thirds or more of the time were more likely to be women, non-Han, poorly educated, and less physically active (table 1). They were also less likely to have higher CMMSE scores, hypertension, diabetes, and cardiovascular disease at baseline (table 1). Table e-4 from Dryad (doi.org/10.5061/dryad.vhhmgqnsk) provides additional information about the distribution of sample characteristics according to the duration of poverty and over time. Baseline characteristic differences between the study sample and excluded individuals are available in table e-5 from Dryad (doi.org/10.5061/dryad.vhhmgqnsk).
Table 1.
Baseline Characteristics by Duration of Poverty Among 3,209 Individuals in 2005, CLHLS, China, 2005–2018
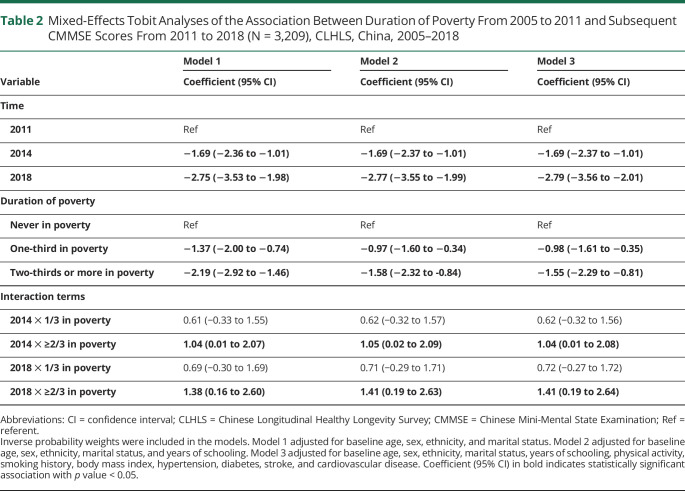
Results from weighted, multivariable-adjusted Tobit regression analyses are provided in table 2. In model 1, individuals who were in poverty one-third of the period from 2005 to 2011 had lower CMMSE scores than those who were never in poverty over that period (β = −1.37, 95% confidence interval [CI] −2.00 to −0.74). A stronger negative association was observed for those in poverty two-thirds or more of the period from 2005 to 2011 compared to those never in poverty over that period (β = −2.19, 95% CI −2.92 to −1.46), indicating a dose-response relationship between duration of poverty and subsequent cognitive function. In the fully adjusted model, these associations were slightly attenuated to −0.98 (95% CI −1.61 to −0.35 for one-third of the period vs never in poverty) and −1.55 (95% CI −2.29 to −0.81 for two-thirds or more of the period vs never in poverty).
Table 2.
Mixed-Effects Tobit Analyses of the Association Between Duration of Poverty From 2005 to 2011 and Subsequent CMMSE Scores From 2011 to 2018 (N = 3,209), CLHLS, China, 2005–2018
Results from the interaction terms suggest that the effect of duration of poverty was modified by time (table 2 and figure 2). In model 1, individuals who were in poverty two-thirds or more of the period from 2005 to 2011 had a slower rate of decline in CMMSE scores compared to those who were never in poverty over that period (β = 1.04, 95% CI 0.01 to 2.07 for 2014 ✕ ≥2/3 in poverty; β = 1.38, 95% CI 0.16 to 2.60 for 2018 ✕ ≥2/3 in poverty). The interaction effect remained statistically significant in the fully adjusted model (β = 1.04, 95% CI 0.01 to 2.08 for 2014 ✕ ≥2/3 in poverty; β = 1.41, 95% CI 0.19 to 2.64 for 2018 ✕ ≥2/3 in poverty), although the 95% CIs were wide due to a lack of precision.
Figure 2. Predicted Trajectories of CMMSE Scores From 2011 to 2018 by Duration of Poverty.
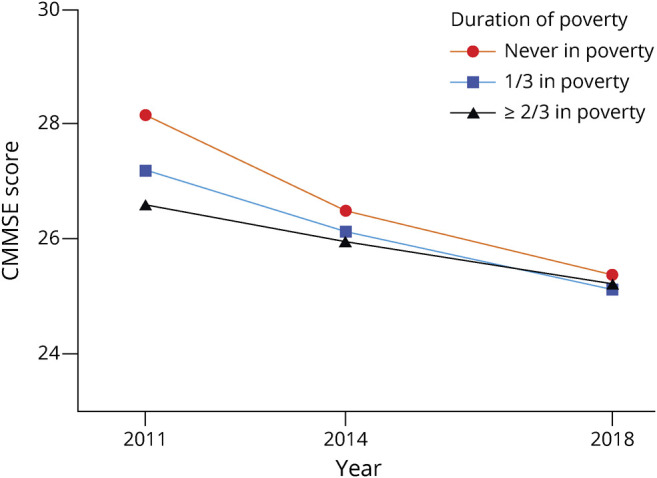
Chinese Mini-Mental State Examination (CMMSE) scores are predicted by estimates in model 3 in table 2. Covariates in model 3 were set to the following levels: age 82 years, male, non-Han, married, zero years of schooling, no regular physical activity, never smoked, body mass index <18.5 kg/m2, no hypertension, no diabetes, no stroke, and no cardiovascular disease.
The sensitivity analyses yielded similar findings to our primary analyses (tables e-6 to e-8 from Dryad: doi.org/10.5061/dryad.vhhmgqnsk). First, the results from models that excluded observations with IPW higher than 5.31 did not differ from our primary findings. Second, the analyses restricted to individuals with CMMSE scores >28 in 2005 (n = 1,918) generated results that were negligibly different from those observed in our main analyses. Finally, when we repeated the modeling analyses without imputed values for missing CMMSE scores, the results were similar to those observed in our main analysis, although the estimates were attenuated in magnitude. The interaction terms between duration of poverty and time were not statistically significant in this analysis, potentially due to loss of precision with the restricted sample size.
Discussion
In this longitudinal study of 3,209 older adults in China from 2005 to 2018, we observed that a longer duration of exposure to poverty in late life was associated with a lower level of subsequent cognitive function in a dose-response fashion. However, we also observed that older adults who experienced poverty two-thirds or more of the time from 2005 to 2011 had a slower rate of subsequent cognitive decline than those never in poverty. Further research on cumulative later-life poverty exposure and cognitive aging in diverse social and economic settings is warranted to better understand the roles of socioeconomic exposures and cognitive reserve in these settings.
Our findings are largely consistent with prior studies indicating that income trajectories are associated with subsequent cognitive function.6,7 Long-term exposure to poverty limits access to adequate nutrition, housing, and health care30; may induce long-lasting psychological stress8,9; and may lead to unhealthy behaviors, including alcohol use, tobacco consumption, and inadequate physical activity.7,8,31,32 Psychological stress has also been associated with dysfunction of hypothalamic-adrenocortical axis,33 an important predictor of hypertension, diabetes, stroke, and cardiovascular disease.34,35 All of these potential mediators may be explanatory mechanisms for our observed associations between poverty duration and subsequent cognitive performance.5,36,37
Our findings expand current knowledge by demonstrating that duration of exposure to poverty in late life may make a difference to older adults' cognitive function in middle-income settings.6,7 Although sustained poverty after the age of 65 years could reflect life-course economic hardship from early childhood to midlife, we included years of schooling and other sociodemographic and health covariates to account for earlier-life socioeconomic status as best as possible.7,38 Previous research that has comprehensively adjusted for early-life and midlife socioeconomic status has still observed associations between late-life socioeconomic conditions and cognitive outcomes.39
Contrary to our second hypothesis, we found that a longer duration of later-life poverty was associated with a slower rate of cognitive decline. These findings are consistent with those from high-income populations demonstrating that higher socioeconomic position and education are associated with a higher level of cognitive function in late life,40,41 while they have also been associated with more rapid memory and cognitive decline once impairment is evident.11,42,43 Education is thought to be a marker of cognitive reserve because it may help older adults to maintain day-to-day cognitive function in the face of brain aging, pathology, or insults.44 Similar to education, income may promote cognitive reserve by providing access to better nutrition, cognitively stimulating activities, social engagement, and health care.11,42,43 Taken together, previous evidence and ours support a compensation hypothesis of cognitive reserve whereby individuals with lower cognitive reserve (those in poverty two-thirds or more of the time) may recruit brain structures or networks to slow the rate of function decline after the deterioration of brain domains earlier than those with higher cognitive reserve (those never in poverty).44,45
This study has limitations. First, although we had access to data on income in late life, capturing middle-old and oldest-old age periods, we were able to measure income trajectories taken with 3 measures over only a short period (6 years) compared with prior research (15–20 years).6,38 Second, late-life poverty duration could be, in part, a reflection of childhood and midlife poverty duration, which we were unable to fully take into account. Third, our outcome measure may not fully capture subtle declines in cognitive function, especially at the higher end of the range of function, because the MMSE is designed to detect cognitive impairment and is known to demonstrate ceiling effects.46 However, we used Tobit regression models to help account for these ceiling effects that are observed with the MMSE. At the same time, our results should be interpreted cautiously because results from this mean value–based regression analysis may not be generalized to every CMMSE score quantile if there is heterogeneity in the association between poverty and cognitive function across the distribution of cognitive function. Moreover, missing CMMSE item values for >50% of observations may diminish the robustness of our findings. However, consistent with existing CLHLS research,22 our primary findings using imputed values of CMMSE items were similar to those observed in the nonimputed data. Furthermore, our analysis is subject to selection bias because we required participants to maintain survival and participation in the study from 2005 to 2011 to have complete exposure information on income. We addressed the possibility of this bias as best as possible through applying wave-specific IPWs for survival and study retention across the 2005–2018 CLHLS data collection waves to minimize the likelihood of this bias.7,10 Finally, the scale of our cognitive outcome measures may not be directly comparable with existing studies because we were unable to calculate SDs from the imputed datasets to create standardized cognitive z scores.47,48 Future research is warranted to generalize our findings.
Despite these limitations, the present study has several strengths. First, we used a longitudinal study design and restricted the study sample to cognitive healthy individuals at baseline in a sensitivity analysis, which, to some extent, rules out reverse causality. Second, we provided new evidence of the cumulative effect of later-life poverty exposure on subsequent cognitive function and decline, which is an understudied life-course exposure period. Third, we accounted for urban and rural status in our poverty measurements, which provides a more accurate indicator of socioeconomic welfare in the context of China's urbanization. Finally, we included data from a globally underrepresented but rapidly aging population consisting of middle-old (75–84 years of age) and oldest-old (>84 years of age) adults in China.9,49,50 These data provide valuable evidence on the role of cumulative later-life poverty exposure in relation to cognitive health of older adults in a rapidly aging and urbanizing middle-income country.
Our findings demonstrate the association between duration of poverty in late life and subsequent cognitive function and decline among older adults in China. We found that a longer duration of poverty over a 6-year period in late life was associated with poorer subsequent cognitive function but a slower rate of cognitive decline. In this underrepresented population of older and oldest-old adults in a rapidly aging middle-income country, our findings may support a compensation hypothesis for cognitive reserve, similar to evidence from high-income populations on the role of education in cognitive function and decline. Future research on the cumulative effects of late-life poverty in diverse social and economic settings is warranted.
Acknowledgment
The authors thank Peking University and Duke University for providing CLHLS data. They thank Dr. Fan Xia at the Department of Neurosurgery, West China Hospital, Sichuan University for modifying figure 2.
Glossary
- ADRD
Alzheimer disease and related dementias
- CI
confidence interval
- CLHLS
Chinese Longitudinal Healthy Longevity Survey
- CMMSE
Chinese Mini-Mental State Examination
- CNY
Chinese yuan renminbi
- IPW
inverse probability weight
Appendix. Authors
Study Funding
W.Z. was supported by 1·3·5 Project for Disciplines of Excellence, West China Hospital, Sichuan University (grant ZYJC18010). L.C.K. was supported by the National Institute on Aging at the NIH (grants R01AG069128 and R01AG070953).
Disclosure
X. Yu, W. Zhang, and L.C. Kobayashi report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.Alzheimer’s Disease International. World Alzheimer Report 2019: Attitudes to Dementia. Alzheimer’s Disease International;2019. [Google Scholar]
- 2.Lee S, Buring JE, Cook NR, Grodstein F. The relation of education and income to cognitive function among professional women. Neuroepidemiology. 2006;26(2):93-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inouye SK, Albert MS, Mohs R, Sun K, Berkman LF. Cognitive performance in a high-functioning community-dwelling elderly population. J Gerontol. 1993;48(4):M146-M151. [DOI] [PubMed] [Google Scholar]
- 4.Elfassy T, Swift SL, Glymour MM, et al. Associations of income volatility with incident cardiovascular disease and all-cause mortality in a US cohort. Circulation. 2019;139(7):850-859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grasset L, Glymour MM, Elfassy T, et al. Relation between 20-year income volatility and brain health in midlife: the CARDIA Study. Neurology. 2019;93(20):e1890-e1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zeki Al Hazzouri A, Elfassy T, Sidney S, Jacobs D, Perez Stable EJ, Yaffe K. Sustained economic hardship and cognitive function: the Coronary Artery Risk Development in Young Adults study. Am J Prev Med. 2017;52(1):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeki Al Hazzouri A, Haan MN, Kalbfleisch JD, Galea S, Lisabeth LD, Aiello AE. Life-course socioeconomic position and incidence of dementia and cognitive impairment without dementia in older Mexican Americans: results from the Sacramento Area Latino Study on Aging. Am J Epidemiol. 2011;173(10):1148-1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prause J, Dooley D, Huh J. Income volatility and psychological depression. Am J Community Psychol. 2009;43(1-2):57-70. [DOI] [PubMed] [Google Scholar]
- 9.Pool LR, Burgard SA, Needham BL, Elliott MR, Langa KM, Mendes de Leon CF. Association of a negative wealth shock with all-cause mortality in middle-aged and older adults in the United States. JAMA. 2018;319(13):1341-1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang ZX, Plassman BL, Xu Q, et al. Lifespan influences on mid- to late-life cognitive function in a Chinese birth cohort. Neurology. 2009;73(3):186-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haan MN, Zeki Al-Hazzouri A, Aiello AE. Life-span socioeconomic trajectory, nativity, and cognitive aging in Mexican Americans: the Sacramento Area Latino Study on Aging. J Gerontol B Psychol Sci Soc Sci. 2011;66(suppl 1):i102-i110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Townsend P, Gordon D. World Poverty: New Policies to Defeat an Old Enemy. Policy Press; 2002. [Google Scholar]
- 13.Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413-446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zou Q, He X, Li Z, Xu W, Zhang L. The effects of poverty reduction policy on health services utilization among the rural poor: a quasi-experimental study in central and western rural China. Int J Equity Health. 2019;18(1):186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kincannon CL, He W, West LA. Demography of aging in China and the United States and the economic well-being of their older populations. J Cross Cult Gerontol. 2005;20(3):243-255. [DOI] [PubMed] [Google Scholar]
- 16.Zhu H. Adult children's characteristics and intergenerational financial transfers in urban China. Chin J Sociol. 2016;2(1):75-94. [Google Scholar]
- 17.Cong Z, Silverstein M. Intergenerational time-for-money exchanges in rural China: does reciprocity reduce depressive symptoms of older grandparents? Res Hum Dev. 2008;5(1):6-25. [Google Scholar]
- 18.Zeng Y. Introduction to the Chinese Longitudinal Healthy Longevity Survey (CLHLS). In: Healthy Longevity in China Demographic Methods and Population Analysis. Springer; 2008. [Google Scholar]
- 19.Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189-198. [DOI] [PubMed] [Google Scholar]
- 20.Zhang Z, Gu D, Hayward MD. Childhood nutritional deprivation and cognitive impairment among older Chinese people. Soc Sci Med. 2010;71(5):941-949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang Z. Gender differentials in cognitive impairment and decline of the oldest old in China. J Gerontol B Psychol Sci Soc Sci. 2006;61(2):S107-S115. [DOI] [PubMed] [Google Scholar]
- 22.Gao M, Kuang W, Qiu P, Wang H, Lv X, Yang M. The time trends of cognitive impairment incidence among older Chinese people in the community: based on the CLHLS cohorts from 1998 to 2014. Age Ageing. 2017;46(5):787-793. [DOI] [PubMed] [Google Scholar]
- 23.Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20(1):40-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Godin J, Keefe J, Andrew MK. Handling missing Mini-Mental State Examination (MMSE) values: results from a cross-sectional long-term-care study. J Epidemiol. 2017;27(4):163-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burns RA, Butterworth P, Kiely KM, et al. Multiple imputation was an efficient method for harmonizing the Mini-Mental State Examination with missing item-level data. J Clin Epidemiol. 2011;64(7):787-793. [DOI] [PubMed] [Google Scholar]
- 26.Amemiya T. Tobit models: a survey. J Econom 1984;24(1):3-61. [Google Scholar]
- 27.McDonald JF, Moffitt RA. The uses of Tobit analysis. Rev Econ Stat. 1980;62(2):318-321. [Google Scholar]
- 28.Weuve J, Tchetgen Tchetgen EJ, Glymour MM, et al. Accounting for bias due to selective attrition: the example of smoking and cognitive decline. Epidemiology. 2012;23(1):119-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Glymour MM, Tzourio C, Dufouil C. Is cognitive aging predicted by one's own or one's parents' educational level? Results from the Three-City Study. Am J Epidemiol. 2012;175(8):750-759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marmot M. The influence of income on health: views of an epidemiologist. Health Aff. 2002;21(2):31-46. [DOI] [PubMed] [Google Scholar]
- 31.Yang S, Lynch JW, Raghunathan TE, Kauhanen J, Salonen JT. Socioeconomic and psychosocial exposures across the life course and binge drinking in adulthood: population-based study. Am J Epidemiol. 2007;165(2):184-193. [DOI] [PubMed] [Google Scholar]
- 32.Boen C, Yang YC. The physiological impacts of wealth shocks in late life: evidence from the Great Recession. Soc Sci Med. 2016;150:221-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brunner E. Socioeconomic determinants of health: stress and the biology of inequality. BMJ. 1997;314(7092):1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.al'Absi M, Arnett DK. Adrenocortical responses to psychological stress and risk for hypertension. Biomed Pharmacother. 2000;54(5):234-244. [DOI] [PubMed] [Google Scholar]
- 35.Rosmond R, Björntorp P. The hypothalamic-pituitary-adrenal axis activity as a predictor of cardiovascular disease, type 2 diabetes and stroke. J Intern Med. 2000;247(2):188-197. [DOI] [PubMed] [Google Scholar]
- 36.Hamer M, Molloy GJ, Stamatakis E. Psychological distress as a risk factor for cardiovascular events: pathophysiological and behavioral mechanisms. J Am Coll Cardiol. 2008;52(25):2156-2162. [DOI] [PubMed] [Google Scholar]
- 37.Matthews KA, Katholi CR, McCreath H, et al. Blood pressure reactivity to psychological stress predicts hypertension in the CARDIA study. Circulation. 2004;110(1):74-78. [DOI] [PubMed] [Google Scholar]
- 38.Elfassy T, Glymour MM, Kershaw KN, et al. Association between sustained poverty and changes in body mass index, 1990-2015: the Coronary Artery Risk Development in Young Adults study. Am J Epidemiol. 2018;187(6):1240-1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marden JR, Tchetgen Tchetgen EJ, Kawachi I, Glymour MM. Contribution of socioeconomic status at 3 life-course periods to late-life memory function and decline: early and late predictors of dementia risk. Am J Epidemiol. 2017;186(7):805-814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Clouston SAP, Smith DM, Mukherjee S, et al. Education and cognitive decline: an integrative analysis of global longitudinal studies of cognitive aging. J Gerontol B Psychol Sci Soc Sci. 2020;75(7):e151-e160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zahodne LB, Glymour MM, Sparks C, et al. Education does not slow cognitive decline with aging: 12-year evidence from the Victoria Longitudinal Study. J Int Neuropsychol Soc 2011;17(6):1039-1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Avila JF, Rentería MA, Jones RN, et al. Education differentially contributes to cognitive reserve across racial/ethnic groups. Alzheimers Dement. 2021;17(1):70-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mungas D, Gavett B, Fletcher E, Farias ST, DeCarli C, Reed B. Education amplifies brain atrophy effect on cognitive decline: implications for cognitive reserve. Neurobiol Aging. 2018;68:142-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stern Y, Arenaza-Urquijo EM, Bartrés-Faz D, et al. Whitepaper: defining and investigating cognitive reserve, brain reserve, and brain maintenance. Alzheimers Dement. 2020;16(9):1305-1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reuter-Lorenz PA, Cappell KA. Neurocognitive aging and the compensation hypothesis. Curr Dir Psychol Sci. 2008;17(3):177-182. [Google Scholar]
- 46.Anstey K, Christensen H. Education, activity, health, blood pressure and apolipoprotein E as predictors of cognitive change in old age: a review. Gerontology. 2000;46(3):163-177. [DOI] [PubMed] [Google Scholar]
- 47.Kobayashi LC, Glymour MM, Kahn K, et al. Childhood deprivation and later-life cognitive function in a population-based study of older rural South Africans. Soc Sci Med. 2017;190:20-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wu Q, Tchetgen Tchetgen EJ, Osypuk TL, White K, Mujahid M, Maria Glymour M. Combining direct and proxy assessments to reduce attrition bias in a longitudinal study. Alzheimer Dis Assoc Disord. 2013;27(3):207-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zizza CA, Ellison KJ, Wernette CM. Total water intakes of community-living middle-old and oldest-old adults. J Gerontol A Biol Sci Med Sci. 2009;64(4):481-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bould S, Sanborn B, Reif L. Eighty-Five Plus: The Oldest Old. Wadsworth Pub Co; 1989. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data from the CLHLS are publicly available at sites.duke.edu/centerforaging.